Abstract
Background
Intraperitoneal adhesions are associated with considerable co‐morbidity and have large financial and public health repercussions. They have secondary effects that include chronic pelvic pain, dyspareunia, subfertility and bowel obstruction. In women with adhesions, subsequent surgery is more difficult, often takes longer, and is associated with a higher complication rate (Broek 2013). The significant burden of adhesions has led to the development of several anti‐adhesion agents, although there is disagreement as to their relative effectiveness.
Objectives
To summarise evidence derived from Cochrane systematic reviews on the clinical safety and effectiveness of solid agents, gel agents, liquid agents and pharmacological agents, used as adjuvants to prevent formation of adhesions after gynaecological pelvic surgery.
Methods
The Cochrane Database of Systematic Reviews was searched using the keyword 'adhesion' up to August 2014. The Cochrane information management system was also searched for any titles or protocols of reviews in progress. Two review authors independently extracted information from the reviews, with disagreements being resolved by a third review author. The quality of the included reviews was described in a narrative manner, and the AMSTAR tool was used to formally assess each review included in this overview. The quality of evidence provided in the original reviews was described using GRADE methods.
Main results
We included two reviews, one with 18 studies comparing solid agents (oxidised regenerated cellulose expanded polytetrafluoroethylene, sodium hyaluronate and carboxymethylcellulose, and fibrin sheets) with control or with each other. The other review included 29 studies which compared liquid agents (4% icodextrin, 32% dextran, crystalloids), gel agents (carboxymethylcellulose and polyethylene oxide, polyethylene glycol gels, hyaluronic acid based gel, 0.5% ferric hyaluronate gel, sodium hyaluronate spray) and pharmacological agents (gonadotrophin‐releasing hormone agonist, reteplase plasminogen activator, N,O‐carboxymethyl chitosan, steroid agents, intraperitoneal noxytioline, intraperitoneal heparin, systemic promethazine) with control or each other. Both reviews met all of the criteria of the AMSTAR assessment.
The reviews included as outcomes both the primary outcomes of this overview (pelvic pain, pregnancy, live birth rate and quality of life (QoL)) and our secondary outcomes (adverse effects, presence or absence of adhesions at second–look laparoscopy (SLL) and adhesion score). However, neither of the reviews identified any primary studies of solid, gel or pharmacological agents that reported any of our primary outcomes. The only studies in either review that reported any of our primary outcomes were studies comparing liquid agents versus control (saline or Hartmann's solution), which reported pelvic pain (two studies), live birth (two studies) and pregnancy (three studies).
An external source of funding was stated for 25 of the 47 studies across both reviews; in 24 of these studies the funding was commercial.
Solid agents (18 studies)
None of our primary outcomes were reported. Adverse events were reported as an outcome by only 9 of the 18 studies. These reported no adverse events.
Liquid agents (nine studies)
There was no evidence of a difference between liquid agents and control (saline or Hartmann's solution) with respect to pelvic pain (odds ratio (OR) 0.65, 95% confidence interval (CI) 0.37 to 1.14, 1 study, n = 286, moderate quality evidence), pregnancy rate (OR 0.64, 95% CI 0.36 to 1.14, 3 studies, n = 310, moderate quality evidence) or live birth rate (OR 0.67, 95% CI 0.29 to 1.58, 2 studies, n = 208, moderate quality evidence). No studies of liquid agents reported QoL. Adverse events were not reported as an outcome by any of the nine studies.
Gel agents (seven studies)
None of our primary outcomes were reported. Adverse events were not reported as an outcome by any of the seven studies.
Pharmacological agents (seven studies)
None of our primary outcomes were reported. Adverse events were reported as an outcome by only one of the seven primary studies. This study reported no evidence of difference in ectopic pregnancy rates between intraperitoneal noxytioline and no treatment (OR 4.91, 95% CI 0.45 to 53.27, 1 study, n = 33, low quality evidence).
Authors' conclusions
There is insufficient evidence to allow us to draw any conclusions about the effectiveness and safety of anti‐adhesion agents in gynaecological surgery, due to the lack of data on pelvic pain, fertility outcomes, quality of life or safety. A substantial proportion of research in this field has been funded by private companies that manufacture these agents, and further high powered, independent trials will be needed before definitive conclusions can be made.
Plain language summary
Agents that prevent the development of abdominal adhesions following surgery: an overview of Cochrane reviews
Background
Abdominal adhesions are web like structures that commonly form following abdominal or pelvic surgery. They are a result of damage to the lining of the abdomen and can cause multiple conditions such as chronic pelvic pain and infertility. Many types of solid, liquid, gel and pharmacological agents have been developed which, when applied during surgery, supposedly reduce the chance that adhesions will develop. However, there has been considerable disagreement as to which agent is more effective. We aimed to summarise the evidence from Cochrane Reviews regarding anti‐adhesion agents in gynaecological surgery.
Search results
Our search up to 31 August 2014 identified two Cochrane reviews. One focused on solid agents, while the other focused on liquid and gel anti‐adhesion agents as well as drugs that may prevent adhesions from forming. All reviews were high quality, though the quality of specific comparisons in each review ranged from low to high as a result of the limitations of the original studies. The characteristics of the women who underwent the trials were recorded poorly among the trials.
Overview of the effectiveness of different anti‐adhesion agents
There was no evidence of a difference between liquid agents compared to no treatment or placebo on pelvic pain, pregnancy rates or live birth rates following surgery (moderate quality of evidence). There were no studies that investigated other anti‐adhesion agents in preventing pelvic pain or infertility directly. Adverse events were reported as an outcome by only 10 of the 47 primary studies. These reported no adverse events.
An external source of funding was stated for 25 of the 47 studies across both reviews; in 24 of these studies the funding was commercial.
The lack of studies investigating the effect of these agents on pelvic pain and fertility means that it is impossible to judge whether the reduction in adhesions produced by these agents translates to any benefit to the patient. Furthermore, the multiple different ways in which adhesions were measured made it difficult to combine studies. A substantial proportion of research in this field has been funded by private companies that manufacture these agents, and further high powered, independent trials will be needed before definitive conclusions can be made.
Background
Intraperitoneal adhesions are associated with considerable co‐morbidity and have large financial and public health repercussions. They are the most common complication of gynaecological surgery, forming in 50% to 100% of women (diZerega 1994). Secondary effects of adhesions include chronic pelvic pain, dyspareunia, subfertility and bowel obstruction (ten Broek 2013; SRS 2007). In women with adhesions, subsequent surgery is more difficult, often takes longer, and is associated with a higher complication rate (ten Broek 2013). The significant burden of adhesions has led to the development of several anti‐adhesion agents, although there is no agreement as to which is the most effective. A Cochrane systematic review has been carried out to investigate intraperitoneal prophylactic anti‐adhesion agents in non‐gynaecological surgery (Kumar 2009) but, as yet, no review has summarised their role in gynaecological surgery.
Description of the condition
Adhesions are fibrin bands that form as the result of aberrant peritoneal healing (Cheong 2011). Normally, peritoneal damage causes an inflammatory response, which activates the coagulation cascade. This leads to formation of a fibrin plug over the damaged mesothelium, which is then broken down to reveal regenerated peritoneum. However, with adhesion formation fibrinolysis of the fibrin plug is decreased and, consequently, a fibrin matrix develops. Adhesions may be defined as 'de novo', meaning that they have formed at a location that was previously free from adhesions, or 're‐formed', which indicates that adhesions have recurred post‐adhesiolysis. In addition to surgery, causes of adhesions include endometriosis, infection (particularly pelvic inflammatory disease) and ischaemia (Diamond 2001). Although the aetiologies are different, the basic pathogenesis of these adhesions is similar.
Description of the interventions
Adhesions can be surgically removed although, because of the high propensity for adhesions to re‐form, the clinical effectiveness of adhesiolysis has been controversial (Hammoud 2004). Thus the focus of adhesion management is now prevention. Various measures can be taken to prevent adhesions from forming. One of the best recognised measures is careful surgical technique, as tissue trauma and bacterial infection have strong links to the condition. Likewise, more traumatic forms of surgery, such as laparotomy, lead to increased risk of damage. This leads to an increased risk of adhesion formation compared to less invasive procedures such as laparoscopy (Robertson 2010). Adhesiolytic agents may be used to prevent the formation of adhesions primarily through one of two methods, by creating an inert barrier that allows peritoneal healing to occur, or by modifying the processes surrounding adhesion formation.
Agents that act as a barrier include solid agents, liquid agents (hydroflotation agents) and gel agents. Several solid agents with different characteristics are commercially available. These include oxidised regenerated cellulose, expanded polytetrafluoroethylene and fibrin sheet. On the other hand, liquid agents are commonly made up of a non‐viscous high molecular weight glucose polymer that is used as an intraperitoneal irrigant or instillant. Gel agents commonly include derivatives of hyaluronic acid. Hyaluronic acid is a linear polysaccharide with repeating disaccharide units composed of sodium D‐glucuronate and N‐acetyl‐D‐glucosamine; it is a major supportive and protective component of body tissues (Johns 2001). Another gel agent was ferric hyaluronate gel 0.5% (Intergel); this product is no longer available.
Pharmacological agents include steroids, which have been used to prevent adhesions. They can be administered in several ways that include systemically before, during and after surgery, as well as intraperitoneally during surgery and via hydrotubation postoperatively. Other pharmacological agents used to prevent adhesions include noxytioline, an antibacterial agent; promethazine, an antihistamine; and reteplase, a thrombolytic drug (all of which are instilled intraperitoneally); as well as heparin, an anticoagulant that is used intraoperatively for irrigation. A nasal gonadotrophin‐releasing hormone agonist (GnRHa) has also been used preoperatively and postoperatively.
How the intervention might work
Liquid agents such as icodextrin and dextran work by hydroflotation, whereby the liquids separate raw opposing surfaces until the healing process has been completed. Liquid agents are believed to remain in the peritoneal cavity for several days, which may be considered a sufficient time given that adhesions form within eight days of surgery (Diamond 2001; Hosie 2001). Steroids and antihistamines (for example promethazine) act as immunomodulating agents and have been used in the belief that they promote fibrinolysis during healing, without hindering the healing process. GnRHa may work by decreasing estrogen‐related growth factors and promoting fibroblasts.
Gel agents include polyethylene glycol (PEG), which is a polymer of hyaluronic acid. When two PEG‐containing liquids are sprayed simultaneously, they form a cross‐linked gel that prevents denuded tissues from coming in contact with each other. This theoretically prevents the occurrence of adhesions.
With regards to solid agents, oxidised regenerated cellulose was the first tested synthetic mechanical barrier to cover traumatised peritoneum in the pelvis. Oxidised regenerated cellulose (Interceed, Johnson & Johnson, Cincinnati, USA) can be cut as necessary and is absorbable. It is applied over raw tissue surfaces at the end of surgery, after haemostasis has been achieved. It forms a gelatinous coat which, according to manufacturers, protects against adhesions within eight hours of application. It is broken down into its monosaccharide constituents and is absorbed within two weeks.
The other commercially available solid agent is expanded polytetrafluoroethylene (Gore‐Tex) surgical membrane (W.L. Gore & Associates, Arizona, USA). It must be sutured in place and is inert and permanent. Other products include Seprafilm (Genzyme Corporation, Cambridge, USA), an adhesion barrier composed of chemically derived sodium hyaluronate and carboxymethylcellulose. It is absorbed from the peritoneal cavity within seven days and is completely excreted from the body within 28 days (Diamond 1996).
Another solid agent called the fibrin sheet (TachoComb, Torii Pharmaceutical, Tokyo, Japan) is a sheet‐type fibrin sealant with a solid layer of human fibrinogen, thrombin and aprotinin coating the active surface of equine collagen stained with riboflavin. It has been suggested that this fibrin sheet may offer adhesion prevention effects following myomectomy (Mais 1995; Pellicno 2003).
Adverse effects of barrier agents have been reported, including abscess formation, foreign body reaction and the possibility of actually inducing adhesions rather than preventing them. However, these reactions are thought to be rare and evidence is limited to isolated case reports (ten Broek 2014; Diamond 2012).
Why it is important to do this overview
Adhesions negatively impact women in a variety of ways following pelvic surgery. Symptomatically, adhesions may present with dyspareunia, subfertility and bowel obstruction. Adhesions have also been linked with chronic pelvic pain, although this association remains controversial because the extent of the adhesions does not always correlate with the level of pelvic pain, and reports have been mixed as to whether treatment of adhesions actually improves symptoms (Cheong 2014; Swank 2003).
Nevertheless, these consequences can greatly decrease a woman’s well‐being and necessitate further surgery. Subsequent surgery in women with adhesions is more difficult, often takes longer and is associated with a higher complication rate. In 2002 it was estimated that the cost of adhesion‐related readmissions in the UK during the first year after lower abdominal surgery was £24.2 million, which increased to £95.2 million in the subsequent nine years (Wilson 2002). The Surgical and Clinical Adhesions Research study (SCAR) found that 5% (n = 245) of readmissions 10 years after open gynaecological surgery were due to adhesions (Lower 2000; Lower 2004). An English study estimated that the National Health Service (NHS) could save £700,000 per year if an anti‐adhesion agent that reduced adhesions by 25% and cost £110 was used; at worst, its use would be cost‐neutral (Cheong 2011).
Considerable disagreement about the effectiveness of adhesion prevention agents can be found in the literature, in part because studies investigating these agents base their results on different endpoints, such as severity of adhesions or the area in which they may form. Indeed many adhesion scoring systems have been developed to help clinicians grade the severity of adhesions and obtain a measure of treatment effect. However, it has been shown that the extent of adhesions does not always correlate with reduction in clinically relevant symptoms (Liakakos 2001). This overview will explore the various endpoints identified in the individual studies and will aim to determine the extent to which surrogate markers are used in the literature.
This overview also seeks to provide an up‐to‐date and coherent document that will guide clinicians and policy makers regarding the efficacy of solid, liquid, gel and pharmacological agents, and to clarify which adhesion prevention agents are most effective.
Objectives
To summarise evidence derived from Cochrane systematic reviews on the clinical safety and effectiveness of solid, liquid, gel and pharmacological agents used as adjuvants to prevent formation of intraperitoneal adhesions after gynaecological pelvic surgery.
Methods
Criteria for considering reviews for inclusion
Only published Cochrane reviews and Cochrane reviews and titles in preparation were considered for inclusion in this overview.
Types of participants
Women in any age group undergoing gynaecological pelvic surgery (laparoscopy or laparotomy).
Types of interventions
Solid, liquid and gel agents and pharmacological agents used in gynaecological surgery to prevent adhesions were considered. Any agent was compared with any other agent or with no treatment, if available. These included the following.
Solid agents
Oxidised regenerated cellulose (Interceed)
Expanded polytetrafluoroethylene (Gore‐Tex)
Sodium hyaluronate and carboxymethylcellulose (Seprafilm)
Above agents versus each other
Other agents
Liquid agents
Icodextrin 4% (Adept)
Dextran 32%
Above agents versus each other
Other agents
Gel agents
Carboxymethylcellulose and polyethylene oxide (Oxiplex)
Polyethylene glycol gels (Spraygel)
Hyaluronic acid based gel (Hyalobarrier)
Ferric hyaluronate gel 0.5% (Intergel)
Above agents versus each other
Other agents
Pharmacological agents
Gonadotrophin‐releasing hormone agonist (GnRHa)
Other pharmacological agents
Types of outcome measures
-
Primary outcomes
Pelvic pain (new pain, change in severity of pain, improvement in pain)
Pregnancy rate
Live birth rate.
Quality of life (QoL), measured using validated tools
-
Secondary outcomes
Adverse outcomes, local and systemic, including adverse fertility outcomes (e.g. miscarriage, ectopic pregnancy) and need for removal of barrier agents.
-
Change in adhesions:
presence or absence of adhesions at second–look laparoscopy (SLL) (bimodal outcome);
-
adhesion score:
mean adhesion score at SLL (non‐parametric continuous data),
change in adhesion score, as a bimodal outcome (for studies reviewing adhesion re‐formation prevention strategies).
Search methods for identification of reviews
The Cochrane Database of Systematic Reviews was searched using the keyword 'adhesion' up to August 2014. The term was restricted to the title, abstract or keywords. The Cochrane information management system (Archie) was also searched for any titles or protocols of reviews in progress. We planned that any relevant protocols and titles that were found would be considered for future incorporation into the overview.
Data collection and analysis
Selection of reviews
Reviews addressing the use of anti‐adhesion agents for prevention in gynaecological surgery were identified by one review author (AH) and confirmed by a second review author (LB). Disagreements were resolved by consensus or by discussion with a third review author.
Data extraction and management
Two review authors (AH, LB) independently selected studies, assessed quality, and extracted information from the reviews. The data were transferred into an Excel spreadsheet to allow review authors to combine and re‐format information in the results and discussion sections and in figures. Disagreements were resolved by a third review author (GA or AW). When data were missing, the original study authors were contacted for assistance. Data were managed within a Microsoft Access database before being input into RevMan. The statistical package RevMan 5.2, provided by The Cochrane Collaboration, was used to analyse and synthesise data. Evidence was sought that the review authors made attempts to retrieve missing data from the original trial authors. If this was not documented, we aimed to contact trial authors directly to retrieve the information.
Assessment of methodological quality of included reviews
Quality of included reviews
The quality of the included reviews was described in a narrative manner, and the AMSTAR tool was used to formally assess each review included in this overview.
Quality of evidence in included reviews
Risk of bias assessments for the original trials were derived from each systematic review. The quality of evidence provided in the original reviews was described, and GRADEPro 'Summary of findings' tables were produced to indicate the quality of the evidence for each comparison.
Data synthesis
A narrative description of the included trials was provided. We planned that indirect comparison analyses would be undertaken, if possible.
Results
Description of included reviews
Design and setting
Our search identified two systematic reviews published in The Cochrane Library, both of which matched the inclusion criteria set out in a pre‐published protocol for this review (Hindocha 2014). One study primarily investigated liquid and pharmacological agents in adhesion prevention. It included 29 randomised controlled trials and was last updated in 2014 (Ahmad 2014(b)). The other review focused on solid agents in adhesion prevention during gynaecological surgery. It included 18 randomised controlled trials and was last updated in 2014 (Ahmad 2014(a)). The individual characteristics of both these reviews have been summarised in Table 1, and the PRISMA flow chart can be seen in Figure 1. No protocols or titles were identified by searching the Cochrane information management system.
1. Characteristics of included studies table.
| Review | Date assessed as up to date | Population | Interventions | Comparison Interventions | Outcomes for which data was reported | Review limitations |
| Ahmad 2008 | 07/04/2014 | Female patients of any age undergoing either open or laparoscopic pelvic surgery for a gynaecological reason. | Hydroflotation, Gel or Pharmacological agents. | Placebo, No treatment or compared to different physical barrier agent included in the interventions. |
Primary: Pelvic pain, live birth rate Secondary: Improvement, Worsening, and mean adhesion score at SLL, Adhesion incidence at SLL, Clinical pregnancy rate, ectopic pregnancy rate and improved QoL at SLL, Adverse outcomes. |
Only 5 of the 13 trials detailed adequate allocation concealment, while only 6 trials were deemed to be at low risk for reporting bias. In all other cases, the risk of bias in the included trials for randomisation, allocation concealment, blinding or selective reporting was deemed unclear. |
| Ahmad 2014 | 19/12/2007 | Female patients of any age undergoing either open or laparoscopic pelvic surgery for a gynaecological reason. Women undergoing rectal surgery were not included. |
Included: Physical Barrier agents, including Oxidised Regenerated Cellulose, Expanded Polytetrafluoroethylene, Sodium Hyaluronate and Carboxymethylcellulose, Fibrin Sheet. Excluded: Fibrin glue and Sepracoat as they are not physical barriers. |
Placebo, No treatment or compared to a different physical barrier agent included in the interventions. |
Primary: Pregnancy rate, reduction in pelvic pain. Secondary: Area and incidence of adhesions post‐operatively, change in adhesion score on SLL, Adverse outcomes. |
18 of 29 trials deemed low risk for random sequence generation, 11 of 29 trials considered low risk for allocation concealment and 16 of 29 trials considered to be of low risk in terms of blinding. Furthermore, 23 of 29 considered low risk in terms of attrition bias, and 25 of 20 deemed to be at low risk of selective reporting bias. |
1.
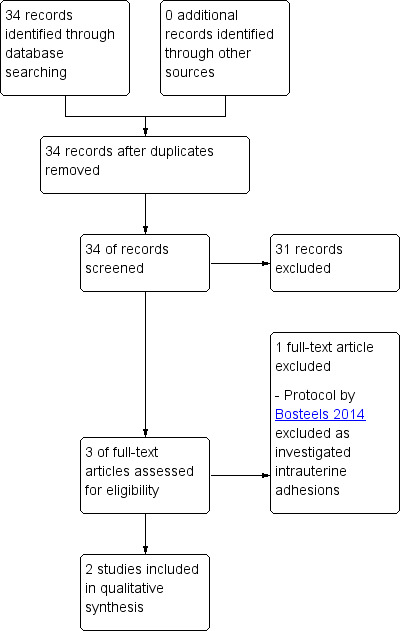
Overview flow diagram.
In terms of design, both were Cochrane systematic reviews and meta‐analyses, and both undertook searches of the Menstrual Disorders and Subfertility Group (MDSG) Specialised Register, CENTRAL, MEDLINE, PsycINFO and Cumulative Index to Nursing and Allied Health Literature using Ovid software. Both reviews also searched the World Health Organization International Clinical Trials Registry Platform, ClinicalTrials.gov and the grey literature. Both studies investigated adhesion agents in the setting of gynaecological surgery.
In terms of study location, Ahmad 2014(a) reported that the studies investigating oxidised regenerated cellulose versus no treatment or control at laparoscopy took place in European centres, with two studies from Germany, three studies from Italy and one study from the UK. Studies investigating oxidised regenerated cellulose versus no treatment or control at laparotomy were more internationally distributed, with studies taking place in North America, Sweden, Australia, UK, Denmark, Finland, Japan and the Netherlands. The trials investigating Gortex or sodium hyaluronate and carboxymethylcellulose versus no treatment both took place in the USA. Only one study was identified that investigated fibrin sheets versus no treatment, and this was a multi‐centre trial taking place in Canada.
In Ahmad 2014(b), three of the seven studies included in the analysis investigating liquid agents versus no treatment took place in the USA. One study took place in Australia, two studies took place in Europe, and one did not state its location. Conversely, four of the five studies investigating gel agents versus placebo or no treatment took place in Europe (Italy, Germany, France and the Netherlands), with one study not stating its location. The analysis comparing steroids versus no steroids included studies from Australia, the Netherlands and France. Studies investigating the other interventions and comparisons in this review took place across the USA, Sweden, Italy, Germany, Canada, Antillies, Australia and the Netherlands. Three studies did not state their location.
Exclusion criteria for individual studies were inconsistently reported in each review. Furthermore, the exclusion criteria varied widely between the studies that did have them detailed, with some studies excluding participants with diabetes (Mettler 2008 in the Ahmad 2014(b) review), while other studies excluded participants based on a history of pelvic inflammatory disease (Mettler 2008 in the Ahmad 2014(b) review). This was the case across both Ahmad 2014(a) and Ahmad 2014(b) and may explain a degree of heterogeneity in each of their analyses.
Participants
Patient characteristics were reported inconsistently across the studies in the reviews. In Ahmad 2014(b), only seven trials had a documented mean age, ranging from 26.8 to 34.97 years. Seven trials did not have an age recorded, while the remaining 15 trials stated that only women more than 18 years old were recruited. In Ahmad 2014(a),11 trials had a documented mean age, ranging from 28 to 34.1 years. Three trials stated that the age range was females of reproductive age more than 18 years old, while the remaining five trials did not have a documented age characteristic in the review. Ethnicity, weight, or other general population characteristics were not described for individual studies in either review.
Participant numbers varied widely between studies in both reviews, with control and intervention groups in each study covering between 4 and 203 participants. This and other characteristics are broken down in the summary of findings tables (Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10; Table 11; Table 12; Table 13; Table 14).
2. Oxidised Regenerated Cellulose versus No Treatment at Laporoscopy for adhesion prevention after gynaecological surgery.
| Oxidised Regenerated Cellulose versus No Treatment at Laporoscopy for adhesion prevention after gynaecological surgery (Ahmad 2014(a)) | ||||||
| Patient or population: Women undergoing laparoscopy Settings: Gynaecological surgery Intervention: Oxidised Regenerated Cellulose versus No Treatment at Laparoscopy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Oxidised Regenerated Cellulose | |||||
| Pelvic Pain | Not Reported | |||||
| Pregnancy Rate | Not Reported | |||||
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
| Incidence of adhesions ‐ De novo Follow‐up: 2‐14 weeks | 333 per 1000 | 200 per 1000 (130 to 290) | OR 0.5 (0.3 to 0.83) | 360 (3 studies) | ⊕⊝⊝⊝ very low1,2,3 | |
| Incidence of adhesions ‐ Reformation (or mixture) Follow‐up: 8‐30 weeks | 700 per 1000 | 284 per 1000 (140 to 489) | OR 0.16 (0.07 to 0.41) | 100 (3 studies) | ⊕⊕⊝⊝ low3,4 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
|
1 One of three studies was at unclear risk of selection bias and one of three studies was at unclear risk of allocation bias. One of three studies was also deemed to be at high risk of attrition bias, with the other two studies having an unclear risk. All three studies were at unclear risk for reporting bias, performance bias and detection bias. Therefore, the quality of the result was downgraded.
2 Heterogeneity evident as I2 value was 85%, there was poor overlap of confidence intervals on visual examination and Chi2 p‐value was <0.05. The reason for the heterogeneity was likely due to differences in the methods (such as the different follow up times, and the different types of surgery that participants had to undergo) 3 There was potential publication bias, with Ahmad 2014(a) reporting that there was evidence of duplicate publication data and the existence of unreported data. The specific evidence for this was not detailed in the paper, though they do state that they had contacted the initial authors. 4 Two of the three trials were deemed to be at high risk of randomisation bias, one trial was deemed to be high risk of allocation concealment bias, while one trial was at unclear risk. Finally, one trial was deemed high risk of attrition bias, while the other two trials were at unclear risk of attrition bias. The evidence was therefore downgraded. | ||||||
3. Oxidised Regenerated Cellulose versus No Treatment at Laparotomy for adhesion prevention after gynaecological surgery.
| Oxidised Regenerated Cellulose versus No Treatment at Laporoscopy for adhesion prevention after gynaecological surgery (Ahmad 2014(a)) | ||||||
| Patient or population: Women undergoing laparotomy Settings: Gynaecological surgery Intervention: Oxidised regenerated cellulose versus no treatment/control at laparotomy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Oxidised Regenerated Cellulose | |||||
| Pelvic Pain | Not Reported | |||||
| Pregnancy Rate | Not Reported | |||||
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
| Incidence of adhesions ‐ De novo Incidence at second look laparoscopy | 282 per 1000 | 220 per 1000 (141 to 329) | OR 0.72 (0.42 to 1.25) | 271 (1 study) | ⊕⊕⊝⊝ low1,2 | |
| Incidence of adhesions ‐ Reformation (or mixture) Incidence at second look laparoscopy | 746 per 1000 | 528 per 1000 (451 to 618) | OR 0.38 (0.27 to 0.55) | 554 (6 studies) | ⊕⊕⊝⊝ low2,3 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
| 1 The one study investigating this comparison was at high risk of attrition bias, with a 22% dropout rate. It was also at unclear risk of selection, performance or detection bias. Therefore, the quality of the result was downgraded. 2 There was potential publication bias, with Ahmad 2014(a) reporting that there was evidence of duplicate publication data and the existence of unreported data. The specific evidence for this was not detailed in the paper, though they do state that they had contacted the initial authors. 3 Five of The six studies were at unclear risk of selection bias, performance bias and detection bias. One study was deemed at high risk of attrition bias, with two studies at unclear risk. One study was deemed at high risk of reporting bias, with the other five being at unclear risk. Therefore, the quality of the result was downgraded. | ||||||
4. Expanded Polytetrafluoroethylene and Carboxymethylcellulose versus No Treatment for adhesion prevention after gynaecological surgery.
| Expanded Polytetrafluoroethylene and Carboxymethylcellulose versus No Treatment for adhesion prevention after gynaecological surgery (Ahmad 2014(a)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological Surgery Intervention: Expanded Polytetrafluoroethylene and Carboxymethylcellulose versus No Treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Expanded Polytetrafluoroethylene and Carboxymethylcellulose versus No Treatment | |||||
| Pelvic Pain | Not Reported | |||||
| Pregnancy Rate | Not Reported | |||||
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
| Incidence of adhesions ‐ De novo | 905 per 1000 | 666 per 1000 (322 to 892) | OR 0.17 (0.03 to 0.94) | 42 (1 study) | ⊕⊕⊝⊝ low1,2 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
| 1 The trial was at an unclear risk of randomisation bias and was unclear on the method of blinding. 2 Evidence was downgraded due to serious imprecision, with only 1 study reporting on a small number of participants. | ||||||
5. Oxidised Regenerated Cellulose vs Expanded Polytetrafluoroethylene for adhesion prevention after gynaecological surgery.
| Oxidised Regenerated Cellulose vs Expanded Polytetrafluoroethylene for adhesion prevention after gynaecological surgery (Ahmad 2014(a)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological surgery Intervention: Oxidised Regenerated Cellulose vs Expanded Polytetrafluoroethylene | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Oxidised Regenerated Cellulose | Expanded Polytetrafluoroethylene | |||||
| Pelvic Pain | Not Reported | |||||
| Pregnancy Rate | Not Reported | |||||
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
| Adhesion Score Non‐validated score out of 11 at SLL | The mean adhesion score was ‐3.79 lower (5.12 to 2.46 lower) | 58 (1 study) | ⊕⊝⊝⊝ very low1,2,3 | |||
| Incidence of adhesions ‐ De novo Incidence at second look laparoscopy | 455 per 1000 | 437 per 1000 (178 to 740) | OR 0.93 (0.26 to 3.41) | 38 (1 study) | ⊕⊝⊝⊝ very low1,2 | |
| Incidence of adhesions ‐ Reformation (or mixture) Incidence at second look laparoscopy | 750 per 1000 | 281 per 1000 (57to 706) | OR 0.13 (0.02 to 0.8) | 23 (1 study) | ⊕⊝⊝⊝ very low1,2,4 | The confidence interval crossed the line of no effect when a risk ratio rather than an odds ratio was calculated (RR 0.36, 95% CI 0.13, to 1.01). |
| *The basis for the assumed risk is the mean control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 The 1 trial investigating this outcome had an unclear risk of bias for its randomisation method, blinding, allocation concealment, attrition bias and selective reporting, and at high risk of performance/detection bias. The evidence was downgraded as a result
2 This comparison was limited to 1 study with a wide confidence interval that crossed the line of appreciable benefit. Therefore, the evidence was downgraded due to very serious imprecision
3 Non‐validated score used 4 Serious imprecision: low event rate. Findings sensitive to choice of effect estimate.
6. Sodium Hyaluronate plus Carboxymethylcellulose versus No Treatment for adhesion prevention after gynaecological surgery.
| Sodium Hyaluronate and Carboxymethylcellulose versus No Treatment for adhesion prevention after gynaecological surgery (Ahmad 2014(a)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological surgery Intervention: Sodium Hyaluronate and Carboxymethylcellulose versus No Treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Sodium Hyaluronate and Carboxymethylcellulose versus No Treatment | |||||
| Pelvic Pain | Not Reported | |||||
| Pregnancy Rate | Not Reported | |||||
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
|
Adhesion Score Non‐validated score out of 4 at SLL |
The mean adhesion score in the intervention groups was 0.49 lower (0.53 to 0.45 lower) | 127 (1 study) | ⊕⊕⊕⊝ moderate1 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
| 1 This 1 trial had unclear risk of selective reporting bias. The scale used in this trial was also not validated. Therefore, the evidence was downgraded. | ||||||
7. Fibrin Sheet versus No treatment at Laporoscopic Myomectomy for adhesion prevention after gynaecological surgery.
| Fibrin Sheet versus No treatment at Laporoscopic Myomectomy for adhesion prevention after gynaecological surgery (Ahmad 2014(a)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological surgery Intervention: Fibrin Sheet versus No treatment at Laporoscopic Myomectomy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Fibrin Sheet versus No treatment at Laporoscopic Myomectomy | |||||
| Pelvic Pain | Not Reported | |||||
| Pregnancy Rate | Not Reported | |||||
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
| Incidence of adhesion per patient Follow‐up: 13‐19 weeks | 625 per 1000 | 667 per 1000 (412 to 850) | OR 1.2 (0.42 to 3.41) | 62 (1 study) | ⊕⊝⊝⊝ very low1,4 | |
|
Adhesion Score Non‐validated score out of 4 at SLL |
The mean adhesion score was 0.14 lower (0.67 lower to 0.39 higher) |
62 (1 study) |
⊕⊝⊝⊝ very low1,2,3 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
|
1 Only one trial which was at unclear risk of randomisation bias, allocation concealment, blinding, attrition bias or selective reporting. Therefore, results were downgraded 2 Non validated scoring method used 3 Imprecision, with few participants and wide confidence intervals 4Downgraded for very serious imprecision, with a low event rate, and findings being compatible with clinically meaningful benefit in either group, or with no effect | ||||||
8. Gel agents vs no treatment for adhesion prevention after gynaecological surgery.
| Gel agents vs no treatment for adhesion prevention after gynaecological surgery (Ahmad 2014(b)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological surgery Intervention: gel agents vs no treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control or no treatment | Oxidised Regenerated Cellulose versus No Treatment at Laporoscopy | |||||
| Pelvic Pain | Not Reported | |||||
| Pregnancy Rate | Not Reported | |||||
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
| Number of participants with adhesions at second‐ look laparoscopy | 766 per 1000 | 450 per 1000 (264‐647) | OR 0.25 (0.11‐0.56) | 134 (4 studies) | ⊕⊕⊕⊕ high |
|
| Mean adhesion score at second‐look laparoscopy | Mean adhesion score at second‐look laparoscopy in the intervention groups was 0.13 standard deviations lower (0.65 lower‐0.39 higher) | 58 (2 studies) | ⊕⊕⊕⊝ moderate1 | SMD ‐0.13 (‐0.65 to 0.39)3 | ||
| Number of participants with an improvement in adhesion score Follow‐up: 2‐14 weeks | 43 per 1000 | 147 per 1000 (27 to 515) | OR 3.78 (0.61‐23.32) | 58 (2 studies) | ⊕⊕⊕⊝ moderate1 | |
| Number of participants with worsening adhesion score Follow‐up: 8‐30 weeks | 826 per 1000 | 432 per 1000 (160‐730) | OR 0.16 (0.04‐0.57) | 58 (2 studies) | ⊕⊕⊕⊝ moderate2 | |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
| 1 Outcome was downgraded due to imprecision, as the number of participants in the analysis was low, and the confidence interval was wide (and arguably crossing the line of appreciable benefit) 2 Outcome was downgraded due to imprecision, as the number of events in the analysis was low, and the confidence interval was wide (and arguably crossing the line of appreciable benefit) 3 Standardized mean difference (SMD) was used due to the variety of different scoring systems between studies. A lower SMD adhesion score equates to an improvement in adhesions compared to control. | ||||||
9. Liquid agents vs no hydroflotation agents for adhesion prevention after gynaecological surgery.
| Liquid agents vs no hydroflotation agents for adhesion prevention after gynaecological surgery (Ahmad 2014(b)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological surgery Intervention: Hydroflotation agents vs no hydroflotation agents | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control or No treatment | Hydroflotation agents | |||||
| Pelvic pain in participants at second look laparoscopy | 806 per 1000 | 730 per 1000 (606‐826) | OR 0.65 (0.37‐1.14) | 286 (1 study) | ⊕⊕⊕⊝ moderate1 | |
| Clinical pregnancy rate | 234 per 1000 |
163 per 1000 (99‐258) |
OR 0.64 (0.36‐1.14) | 310 (3 studies) | ⊕⊕⊕⊝ moderate1 | |
| Live birth rate | 140 per 1000 | 98 per 1000 (45‐205) | OR 0.67 (0.29‐1.58) | 208 (2 studies) | ⊕⊕⊕⊝ moderate1 | |
| Quality of Life | Not Reported | |||||
| Number of participants with adhesions at second‐ look laparoscopy | 836 per 1000 | 635 per 1000 (529‐738) | OR 0.34 (0.22‐0.55) | 566 (4 studies) | ⊕⊕⊕⊕ High | |
| Mean adhesion score at second‐look laparoscopy | The mean adhesion score at second‐look laparoscopy in the intervention groups was 0.06 standard deviations lower (0.2 lower‐0.09 higher) | 722 (4 studies) | ⊕⊕⊕⊕ High | SMD ‐0.06 (‐0.2 to 0.09)4 | ||
|
Number of participants with an improvement in adhesion score |
437 per 1000 | 496 per 1000 (380‐614) | OR 1.27 (0.79‐2.05) | 665 (4 studies) | ⊕⊕⊕⊝ moderate1,2 | |
| Number of participants with worsening adhesion score | 308 per 1000 | 111 per 1000 (30‐350) | OR 0.28 (0.07‐1.21) | 53 (1 study) | ⊕⊕⊕⊝ moderate1,3 | |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
|
1 Outcome was downgraded due to imprecision, as the number of participants in the analysis was low, and the confidence interval was wide (and arguably crossing the line of appreciable benefit)
2 The outcome had moderate levels of heterogenety, with an I2 38%, though the Chi2 P value was 0.18, and there was good overlap of the confidence interval.
3 Outcome was downgraded due to imprecision, due to the small number of events. 4Standardized mean difference (SMD) was used due to the variety of different scoring systems between studies. A lower SMD adhesion score equates to an improvement in adhesions compared to control. | ||||||
10. Gel agents compared with hydroflotation agents when used as an instillant for adhesion prevention after gynaecological surgery.
| Gel agents compared with hydroflotation agents when used as an instillant for adhesion prevention after gynaecological surgery (Ahmad 2014(b)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological surgery Intervention: Hydroflotation agents used as an instillant vs Gel agents | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
|
Hydroflotation agents used as an instillant |
Gel agents | |||||
| Pelvic Pain | Not Reported | |||||
| Pregnancy Rate | Not Reported | |||||
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
| Number of participants with adhesions at second‐ look laparoscopy | 225 per 1000 |
95 per 1000 (52‐163) |
OR 0.36 (0.19‐0.67) | 342 (2 studies) | ⊕⊕⊕⊕ high | |
| Mean adhesion score at second‐look laparoscopy | Mean adhesion score at second‐look laparoscopy in the intervention groups was 0.79 lower (0.79‐0.79 lower) | 77 (1 study) | ⊕⊕⊕⊝ moderate2 | SMD ‐0.13 (‐0.65 to 0. 39)3 | ||
|
Number of participants with an improvement in adhesion score |
110 per 1000 | 161 per 1000 (92‐265) | OR 1.55 (0.82‐2.92) | 342 (2 studies) | ⊕⊕⊕⊝ moderate1 | |
| Number of participants with worsening adhesion score | 139 per 1000 | 43 per 1000 (19‐96) | OR 0.28 (0.12‐0.66) | 342 (2 studies) | ⊕⊕⊕⊕ high | |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
| 1 Outcome was downgraded due to imprecision, as the number of participants in the analysis was low, and the confidence interval was wide (and arguably crossing the line of appreciable benefit) 2Ahmad 2014(b) advised caution on interpreting this result, as the SD was very narrow for a study containing only 38 participants in each arm. 3 Standardized mean difference (SMD) was used due to the variety of different scoring systems between studies. A lower SMD adhesion score equates to an improvement in adhesions compared to control. | ||||||
11. Steroids (any route) vs no steroids for adhesion prevention after gynaecological surgery.
| Steroids (any route) vs no steroids for adhesion prevention after gynaecological surgery (Ahmad 2014(b)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological surgery Intervention: Steroids (any route) vs no steroids | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control or No treatment | Steroid agents | |||||
| Pelvic Pain | Not Reported | |||||
| Clinical pregnancy rate | 297 per 1000 | 299 per 1000 (218‐396) | OR 1.01 (0.66‐1.55) | 410 (3 studies) | ⊕⊕⊕⊝ moderate1,2 | |
| Ectopic pregnancy rate | 195 per 1000 | 140 per 1000 (19‐580) | OR 0.67 (0.08‐5.7) | 83 (3 studies) | ⊕⊕⊕⊝ moderate3 | |
| Live birth rate | 112 per 1000 | 76 per 1000 (32‐170) | OR 0.65 (0.26‐1.62) | 223 (2 studies) | ⊕⊕⊕⊝ moderate1 | |
| Quality of Life | Not Reported | |||||
|
Number of participants with an improvement in adhesion score |
462 per 1000 | 805 per 1000 (594‐921) | OR 4.83 (1.71‐13.65) | 75 (1 study) | ⊕⊕⊝⊝ low2 | |
| Number of participants with worsening adhesion score | 343 per 1000 | 124 per 1000 (59‐233) | OR 0.27 (0.12‐0.58) | 176 (2 studies) | ⊕⊕⊝⊝ low1,2 | |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
| 1 Outcome was downgraded due to imprecision, as the number of participants in the analysis was low, and the confidence interval was wide (and arguably crossing the line of appreciable benefit) 2 Study was unpublished, with little information regarding the charachteristics of the study provided by the authors. Therefore, caution should be employed with these results. 3 Outcome was downgraded due to heterogeneity. While there was confidence interval overlap and a Chi2 p value of 0.08, the I2 value was 60% and there was substantial variation in the point estimate. | ||||||
12. Intraperitoneal noxytioline vs no treatment for adhesion prevention after gynaecological surgery.
| Intraperitoneal noxytioline vs no treatment for adhesion prevention after gynaecological surgery (Ahmad 2014(b)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological surgery Intervention: Intraperitoneal noxytioline vs no treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Hydroflotation agents | |||||
| Pelvic Pain | Not Reported | |||||
| Clinical pregnancy rate | 302 per 1000 | 222 per 1000 (115‐388) | OR 0.66 (0.3‐1.47) | 126 (1 study) | ⊕⊕⊕⊝ moderate1 | |
| Ectopic pregnancy rate | 53 per 1000 | 214 per 1000 (24‐747) | OR 4.91 (0.45‐53.27) | 33 (1 study) | ⊕⊕⊝⊝ low2 | |
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
| Number of participants with worsening adhesion score | 205 per 1000 | 124 per 1000 (42‐312) | OR 0.55 (0.17‐1.76) | 87 (1 study) | ⊕⊕⊕⊝ moderate1 | |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
|
1 Outcome was downgraded due to imprecision, as the number of participants in the analysis was low, and the confidence interval was wide (and arguably crossing the line of appreciable benefit)
2Outcome was downgraded due to imprecision, as the number of participants in the analysis was low, and the confidence interval was wide (and arguably crossing the line of appreciable benefit). Due to the size of the confidence interval, the authors deemed this to be very serious and downgraded the results | ||||||
13. Intraperitoneal heparin solution vs no intraperitoneal heparin for adhesion prevention after gynaecological surgery.
| Intraperitoneal heparin solution vs no intraperitoneal heparin for adhesion prevention after gynaecological surgery (Ahmad 2014(b)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological surgery Intervention: Intraperitoneal heparin vs control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Intraperitoneal Heparin | |||||
| Pelvic Pain | Not Reported | |||||
| Pregnancy Rate | Not Reported | |||||
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
|
Number of participants with an improvement in adhesion score |
571 per 1000 | 537 per 1000 (299‐758) | OR 0.87 (0.32‐2.35) | 63 (1 study) | ⊕⊕⊝⊝ low1,2 | |
| Number of participants with worsening adhesion score | 396 per 1000 | 454 per 1000 (268‐656) | OR 1.27 (0.56‐2.91) | 92 (1 study) | ⊕⊕⊝⊝ low1,2 | |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
|
1 Outcome was downgraded as hydrocortisone was added to the irrigation of the first 46 patients entered into the trial, though was not used for the other patients. The authors state that the reason for this was due to published reports pof possible adverse effects 2 Outcome was downgraded due to imprecision, as the number of participants in the analysis was low, and the confidence interval was wide (and arguably crossing the line of appreciable benefit) | ||||||
14. Systemic promethazine vs no promethazine for adhesion prevention after gynaecological surgery.
| Systemic promethazine vs no promethazine for adhesion prevention after gynaecological surgery (Ahmad 2014(b)) | ||||||
| Patient or population: Women undergoing gynaecological surgery Settings: Gynaecological surgery Intervention: Systemic promethazine vs no promethazine | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Systematic promethazine | |||||
| Pelvic Pain | Not Reported | |||||
| Pregnancy Rate | Not Reported | |||||
| Live Birth Rate | Not Reported | |||||
| Quality of Life | Not Reported | |||||
|
Number of participants with an improvement in adhesion score |
692 per 1000 | 558 per 1000 (331‐763) | OR 0.56 (0.22‐1.43) | 75 (1 study) | ⊕⊕⊝⊝ low1,2 | |
| Number of participants with worsening adhesion score | 391 per 1000 | 275 per 1000 (138‐477) | OR 0.59 (0.25‐1.42) | 93 (1 study) | ⊕⊕⊝⊝ low1,2 | |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
| 1 Data was obtained directly from the study author after reading results in a review article. Many charachteristics of the result was unclear. 2 Outcome was downgraded due to imprecision, as the number of participants in the analysis was low, and the confidence interval was wide (and arguably crossing the line of appreciable benefit) | ||||||
Finally, it should be noted that seven trials in Ahmad 2014(a) were exclusively carried out on participants having treatment for infertility. Of these, four trials reported fertility outcomes. Fertility outcomes were reported by one further study in this review and were limited to a subgroup of patients with infertility that were recruited into the trial (Ahmad 2014(a)).
Interventions and comparisons
Ahmad 2014(a) included trials comparing the use of solid agents such as oxidised regenerated cellulose, expanded polytetrafluoroethylene, sodium hyaluronate and carboxymethylcellulose, and fibrin sheet with any other barrier agent or no treatment or control. Studies of fibrin glue and Sepracoat were excluded from this study as they are not solid agents.
Ahmad 2014(b) included trials comparing the use of liquid agents, gel agents, steroid agents (including systemic, intraperitoneal, preoperative and postoperative steroids), intraperitoneal noxytioline, intraperitoneal heparin, systemic promethazine, GnRHa, reteplase plasminogen activator and N,O‐carboxymethyl chitosan. All of these were compared to no treatment or control. Gel agents were also compared to liquid agents when used as an instillant.
Ahmad 2014(a) split the analysis of the interventions based on whether participants had a laparoscopic procedure or a laparotomy. These comparisons were further divided into subgroups based on whether the trials were investigating new (de novo) adhesion formation in patients or whether they were investigating re‐formation of adhesions following surgery (this subgroup also included those studies which mixed de novo adhesions and re‐formation adhesions into one study group). Reasons for surgery in studies in the review investigating de novo adhesions included uterine fibroids, polycystic ovary syndrome and infertility, and surgical types carried out included myomectomy and ovarian cautery. For studies across the review investigating re‐formation adhesions, reasons for surgery included chronic pelvic pain, infertility, endometriosis and pre‐existing adhesions. The surgical types carried out all involved adhesionolysis, with concomitant tubal, ovarian, or endometriosis treatment. It should be noted that three trials were restricted to women undergoing treatment for infertility, although none of these trials had fertility as an outcome.
Ahmad 2014(b) did not distinguish between laparoscopy and laparotomy in their analysis. Studies were only analysed based on their outcomes: either the primary outcomes of pelvic pain and live birth rate following surgery, or secondary outcomes (1. improvement in adhesion score at SLL with the agent, 2. preventing a worsening of adhesion score at SLL with the agent, 3. the presence of adhesions at SLL with the agent, 4. the mean adhesion score at SLL with the agent, 5. the clinical pregnancy rate, 6. the miscarriage rate, 7. the ectopic pregnancy rate, 8. the QoL on SLL).
On scrutinising this analysis of Ahmad 2014(b) , the comparison between liquid agents and control agents mainly contained studies where laparoscopy was carried out (adhesionolysis, combined with treatment for either endometriosis, tubal or ovarian pathology). However, two studies (Adhesion SG 1983, Diamond 1998) investigated the effect of liquid agents versus control in open surgery. These results were still incorporated into the comparisons investigating the effect of liquid agents on adhesion score, pregnancy rate and the incidence of adhesions.
The comparison for gel agents versus placebo in Ahmad 2014(b) was also predominantly made up of participants undergoing laparoscopy (including laparoscopic myomectomy, adhesionolysis or other treatments for benign gynaecological diseases, infertility or recurrent miscarriages, chronic pelvic pain, or endometriosis). However, one trial (Mettler 2004) investigating the agents in laparotomy (for fibroids) was incorporated into the analysis. The results for this trial were incorporated into all the comparisons of gel agents versus control that looked at changes in adhesion scores or adhesion incidence. With regards to other adhesion agents investigated by Ahmad 2014(b), the studies included a mix of participants undergoing either laparoscopic or open surgery for tubal obstruction, chronic pelvic pain, infertility, endometriosis or benign gynaecological diseases.
Furthermore, Ahmad 2014(b) did not distinguish between primary prevention of de novo adhesions and secondary prevention of adhesions following adhesionolysis. This was because too few of the included studies differentiated between the two outcomes.
Outcomes
Ahmad 2014(a) and Ahmad 2014(b) reported the following as primary outcomes.
Pelvic pain (improvement, worsening, no change in pain at second‐look laparoscopy (SLL)), measured by a validated pain scale.
Live birth rate, relevant only to studies investigating the use of anti‐adhesion agents in procedures to improve fertility.
Ahmad 2014(a) and Ahmad 2014(b) reported the following as secondary outcomes.
Number of participants with adhesions at SLL.
Clinical pregnancy rate (pregnancy confirmed with ultrasound scan), relevant only to studies investigating the use of anti‐adhesion agents in procedures to improve fertility.
Miscarriage rate, defined as the loss of pregnancy before 24 weeks of gestation.
Ectopic pregnancy rate.
Number of participants with an improvement in quality of life (QoL) at SLL, recorded on whichever scale was chosen by the original study authors.
Adverse outcomes, local and systemic, thought to be due to the anti‐adhesion agent.
Ahmad 2014(b) reported on three further secondary outcomes.
Improvement in adhesion score at SLL, with preference given to the modified American Fertility Score (mAFS).
Worsening in adhesion score at SLL, with preference given to the mAFS.
Mean adhesion score at SLL per participant, with preference given to the mAFS.
Ahmad 2014(a), on the other hand, combined these three secondary outcomes into one outcome: adhesion score at SLL, with preference given to the mAFS.
In both Ahmad 2014(a) and Ahmad 2014(b), it was stated that articles which met the inclusion criteria but did not report any of the stated outcomes were also included within the qualitative analysis.
Methodological quality of included reviews
Review quality
We assessed the reviews using the AMSTAR tool as outlined in the methods (Table 15).
15. AMSTAR assessment of included systematic reviews.
| AMSTAR assessment items | Ahmad 2014(a) | Ahmad 2014(b) | |
| Was an ‘a priori’ design provided? | Yes | Yes | |
| Was there duplicate study selection and data extraction? | Yes | Yes | |
| Was a comprehensive literature search performed? | Yes | Yes | |
| Was the status of the publication used as an inclusion criterion? | Yes | Yes | |
| Was a list of studies (included and excluded) provided? | Yes | Yes | |
| Were the characteristics of the included studies provided? | Yes | Yes | |
| Was the scientific quality of the included studies assessed and documented? | Yes | Yes | |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | Yes | Yes | |
| Were the methods used to combine the findings of studies appropriate? | Yes | Yes | |
| Was the likelihood of publication bias assessed | Unable due to the small number of studies | Unable due to the small number of studies | |
| Was conflict of interest included? | Yes | Yes |
Yes in the AMSTAR table represents that, in the authors' opinion, the study was acceptable in meeting the requirements of the AMSTAR criteria.
Both reviews provided an a priori design.
Both reviews conducted study selection and data extraction in duplicate.
Both reviews conducted a comprehensive literature search.
Both studies stated that they searched the grey literature, and included studies regardless of their publication type.
Both reviews listed included and excluded studies.
Both reviews described the characteristics of the included studies.
Both reviews assessed the quality of studies included in the review.
Both reviews did explicitly consider the scientific quality of the studies in formulating their conclusions. Though the original published version of Ahmad 2014(a) did not explicitly state how the scientific quality of the included studies influenced its conclusions, the authors have addressed this in the most recent version.
Both reviews combined the studies using appropriate methods, and heterogeneity was assessed adequately.
Neither of the reviews was able to formally assess the possibility of publication bias due to the small number of studies in each comparison.
Both reviews addressed the potential for conflict of interest.
The searches in Ahmad 2014(a) and Ahmad 2014(b) both took into account all trials up until April 2014.
Although both reviews met all AMSTAR criteria, we noted the following limitations.
Ahmad 2014(b) included studies in the meta‐analysis that used Ringer's lactate, normal saline or phosphate buffered saline (PBS) as a control agent. For example, all of the studies investigating liquid agents versus control or no treatment used one of these solutions as the control agent. However, one of the comparisons in Ahmad 2014(b) investigated gel agents versus liquid agents when used as an instillant. Two studies were investigated in this comparison, both of which compared Intergel to Ringer's lactate (which rather than a control was classed as a liquid agent in this comparison). Arguably, if the authors had considered this solution as a control agent in the other comparisons, they should apply the same thinking to these comparisons and thus incorporated these studies into the meta‐analysis that compared gel treatments to control or no treatment (rather than analysing the studies separately).
Both reviews (Ahmad 2014(a); Ahmad 2014(b)) combined a number of studies into their meta‐analyses. However, there were significant differences, across reviews, between the methods of the individual included studies. Specifically, the timing for the SLL (to assess adhesions) varied widely between individual studies, from six days in some studies to six months in other studies. One study was even reported as having its second‐look surgery at 2.3 to 2.6 years following the initial surgery (Tinelli 2011 in Ahmad 2014(a)). As postoperative adhesions have been shown to evolve and change over time (Bakkum 1995), the decision to not segregate studies into subgroups based on their SLL time may lead to increased heterogeneity in the results and could arguably reduce the power of the analyses.
Finally, the meta‐analysis from Ahmad 2014(b) did not make any distinction between studies in terms of the type of surgery that had been undertaken. There is a proven link between surgical trauma and peritoneal adhesions (Mais 2014) and thus one could argue that the meta‐analysis should be subgrouped based on the type of surgery. Whlie there is no definitive evidence that the efficacy of anti‐adhesion agents is affected by the surgery type, it is possible that any benefit seen in less traumatic surgery would be reduced compared to the more traumatic surgery as there will be more scope for improvement in the latter.
Included study quality
In Ahmad 2014(a), the quality of evidence for most comparisons was downgraded due to risk of bias assessment in individual studies. Specifically, only 5 of the 18 included trials showed adequate random sequence generation, while only two studies were at low risk of performance or detection bias. Only 5 of 18 studies adequately protected against attrition bias, while only 1 of the 18 trials detailed adequate allocation concealment. No trials were definitively considered to be at low risk for reporting bias. In most other cases, the risk of bias was deemed unclear.
With regards to Ahmad 2014(b), a smaller proportion of trials had the quality of their evidence downgraded for risk of bias (see summary of findings table). This was as 18 of 29 trials were deemed to be low risk for random sequence generation, 11 of 29 trials were low risk for allocation concealment, and 16 of 29 trials were low risk in terms of blinding. Furthermore, 23 of 29 trials were low risk in terms of attrition bias, and 25 of 29 trials were at low risk of selective reporting bias.
Although both reviews were unable to assess publication bias, due to the relatively small numbers of studies in each comparison, a significant portion of studies in both reviews had some form of external funding from a pharmaceutical/medical company. In Ahmad 2014(b), 15 of the 29 studies stated that they had some form of external funding from a private company, while Ahmad 2014(a) stated that 10 of the 18 studies had some form of external funding. Evidence has shown that studies funded by private companies tend to favour the intervention rather than the control (Bhandari 2004; Lexchin 2003). A possible reason for this is that private companies may discourage negative studies of their intervention, as has been evident in the past (see Rennie 1997). This in itself is a form of publication bias. As such, while it is impossible to assess for publication bias due to the small number of studies, the high number of privately funded studies in both reviews must be taken into account when interpreting the conclusions of this overview.
Ahmad 2014(a) mentioned that duplicate publication of data might have biased their analysis. They reported that 8 of the 15 included studies in their review had evidence of duplicate publications in the literature, five of which investigated oxidised regenerated cellulose versus no treatment. While they tried to contact the original authors of the studies, they could not rule out that further trials included in the systematic review were not influenced by publication bias caused by duplication of study results. Ahmad 2014(b) did not raise any concerns that duplication of study results affected their review.
Effect of interventions
1 Solid agent versus treatment or control
1.1 Oxidised regenerated cellulose (solid agent) versus control or no treatment
Primary outcomes
a. Pelvic pain
No review found any trials that investigated the effect of oxidised regenerated cellulose on postoperative pelvic pain.
b. Pregnancy rate
No review found any trials that investigated the effect of oxidised regenerated cellulose on postoperative pregnancy rate.
c. Live birth rate
No review found any trials that investigated the effect of oxidised regenerated cellulose on postoperative live birth rate.
d. Quality of life (QoL) measures
No review found any trials that investigated the effect of oxidised regenerated cellulose on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
Ahmad 2014(a) identified 5 out of 13 studies which stated the presence or absence of adverse outcomes for oxidised regenerated cellulose in laparotomy. In the 225 participants receiving the intervention in these studies, none reported adverse effects related to the agent.
b. Change in adhesion score
i) Following laparoscopic surgery, Ahmad 2014(a) found that oxidised regenerated cellulose reduced the incidence of adhesions when compared to no treatment for both de novo adhesions (odds ratio (OR) 0.50, 95% confidence interval (CI) 0.30 to 0.83, 3 studies, n = 360, I2 = 75%, very low quality evidence) and re‐formation adhesions (OR 0.16, 95% CI 0.07 to 0.41, 3 studies, n = 100, I2 = 36%, low quality evidence). Following laparotomy, Ahmad 2014(a) found there was no evidence of a difference between oxidised regenerated cellulose compared to no treatment for de novo adhesions (OR 0.72, 95% CI 0.42 to 1.25, 1 study, n = 271, I2 = not applicable (N/A), low quality evidence). However, meta‐analysis showed some benefit for re‐formation adhesions (OR 0.38, 95% CI 0.27 to 0.55, 6 studies, n = 554, I2 = 41%, low quality evidence).
ii) No reviews found any studies that assessed the effect of oxidised regenerated cellulose on the mean adhesion score at SLL.
iii) No reviews found any studies that assessed the effect of oxidised regenerated cellulose on improving or preventing deterioration of the adhesion score at SLL (bimodal outcome).
1.2 Expanded polytetrafluoroethylene versus no treatment or control
Primary outcomes
a. Pelvic pain
No review found any trials that investigated the effect of expanded polytetrafluoroethylene on postoperative pelvic pain.
b. Pregnancy rate
No review found any trials that investigated the effect of expanded polytetrafluoroethylene on postoperative pregnancy rate.
c. Live birth rate
No review found any trials that investigated the effect of expanded polytetrafluoroethylene on postoperative live birth rate.
d. Quality of life (QoL) measures
No review found any trials that investigated the effect of expanded polytetrafluoroethylene on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
Ahmad 2014(a) identified only one trial that investigated the adverse effects of expanded polytetrafluoroethylene, with a total of 21 participants treated with the agent. No adverse effects secondary to the agent were reported.
b. Change in adhesion score
i) Ahmad 2014(a) identified only one trial that investigated the effect of expanded polytetrafluoroethylene on adhesion formation at laparotomy. They found a reduced incidence of de novo adhesion formation compared to no treatment (OR 0.17, 95% CI 0.03 to 0.94, 1 study, n = 42, I2 = N/A, low quality evidence).
ii) No reviews found any studies that assessed the effect of expanded polytetrafluoroethylene on the mean adhesion score at SLL.
iii) No reviews found any studies that assessed the effect of expanded polytetrafluoroethylene on improving or preventing deterioration of adhesion score at SLL (bimodal outcome).
1.3 Sodium hyaluronate and carboxymethylcellulose versus control or no treatment
Primary outcomes
a. Pelvic pain
No review found any trials that investigated the effect of sodium hyaluronate and carboxymethylcellulose on postoperative pelvic pain.
b. Pregnancy rate
No review found any trials that investigated the effect of sodium hyaluronate and carboxymethylcellulose on postoperative pregnancy rate.
c. Live birth rate
No review found any trials that investigated the effect of sodium hyaluronate and carboxymethylcellulose on postoperative live birth rate.
d. Quality of life (QoL) measures
No review found any trials that investigated the effect of sodium hyaluronate and carboxymethylcellulose on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
Ahmad 2014(a) identified only one trial that investigated the adverse effects of sodium hyaluronate and carboxymethylcellulose, with a total of 59 participants treated with the agent. No adverse effects secondary to the agent were reported.
b. Change in adhesion score
i) No reviews found any studies that assessed the effect of sodium hyaluronate and carboxymethylcellulose on the incidence of adhesions at SLL.
ii) Ahmad 2014(a) identified one trial that investigated the effect of sodium hyaluronate and carboxymethylcellulose on the mean adhesion score. They found that sodium hyaluronate and carboxymethylcellulose significantly reduced the mean adhesion score when compared to no treatment (mean difference (MD) ‐0.49, 95% CI 0.53 to 0.45, 1 study, n = 127, I2 = N/A, moderate quality evidence). It should be noted that the adhesion score that was used was a non‐validated score out of 4.
iii) No reviews found any studies that assessed the effect of sodium hyaluronate and carboxymethylcellulose on improving or preventing deterioration of the adhesion score at SLL (bimodal outcome).
It should be noted that other outcomes were reported by this study, though the authors of Ahmad 2014(a) judged that inappropriate statistical analysis had been used to analyse those outcomes. This was because, even though it wasn't treated as such in the study, the data from this study appeared to be positively skewed after calculating the standard deviations (SDs) from the standard errors of the means (SEMs). Therefore, the authors judged that inappropriate statistical tests had been used, and thus the other outcomes were not incorporated as part of the analysis.
1.5 Fibrin sheet versus no treatment or control
Primary outcomes
a. Pelvic pain
No review found any trials that investigated the effect of a fibrin sheet on postoperative pelvic pain.
b. Pregnancy rate
No review found any trials that investigated the effect of a fibrin sheet on postoperative pregnancy rate.
c. Live birth rate
No review found any trials that investigated the effect of a fibrin sheet on postoperative live birth rate.
d. Quality of life (QoL) measures
No review found any trials that investigated the effect of a fibrin sheet on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
Ahmad 2014(a) identified only one study which stated the presence or absence of adverse outcomes for fibrin sheets. In the 30 participants receiving the intervention in this study, none reported adverse effects related to the agent.
b. Change in adhesion score
i) Ahmad 2014(a) identified one study that compared fibrin sheets to no treatment in on the incidence of adhesion SLL. They found no evidence of a difference between the fibrin sheet group and the no treatment group (OR 1.2, 95% CI 0.42 to 3.41, 1 study, n = 62, I2 = N/A, very low quality evidence).
ii) Ahmad 2014(a) identified one study that compared fibrin sheets to no treatment in on the mean adhesion score at SLL. They found no evidence of a difference between the fibrin sheet group and the no treatment group (MD ‐0.14, 95% CI ‐0.67 to 0.39, 1 study, n = 62, I2 = N/A, very low quality evidence). It should be noted that the adhesion score that was used was a non‐validated score out of 4.
iii) No reviews found any studies that assessed the effect of fibrin sheets on improving or preventing deterioration of the adhesion score at SLL (bimodal outcome).
1.6 Expanded polytetrafluoroethylene versus oxidised regenerated cellulose
Primary outcomes
a. Pelvic pain
No review found any trials that investigated the effect of expanded polytetrafluoroethylene versus oxidised regenerated cellulose on postoperative pelvic pain.
b. Pregnancy rate
No review found any trials that investigated the effect of expanded polytetrafluoroethylene versus oxidised regenerated cellulose sheet on postoperative pregnancy rate.
c. Live birth rate
No review found any trials that investigated the effect of expanded polytetrafluoroethylene versus oxidised regenerated cellulose sheet on postoperative live birth rate.
d. Quality of life (QoL) measures
No review found any trials that investigated the effect of expanded polytetrafluoroethylene versus oxidised regenerated cellulose sheet on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
Ahmad 2014(a) identified only one out of two studies which stated the presence or absence of adverse outcomes for oxidised regenerated cellulose versus expanded polytetrafluoroethylene. Twelve participants received the intervention in this study (nine treated with oxidised regenerated cellulose, three treated with expanded polytetrafluoroethylene) with no reported adverse effects related to the agent.
b. Change in adhesion score
i) Ahmad 2014(a) identified one study which compared expanded polytetrafluoroethylene versus oxidised regenerated cellulose in reducing de novo adhesions following laparoscopic myomectomy. There was no evidence of a difference between the two agents (OR 0.93, 95% CI 0.26 to 3.34, 1 study, n = 38, I2 = N/A, low quality evidence). Ahmad 2014(a) identified one study which compared both these agents in reducing re‐formation adhesions following laparotomy for adhesionolysis. They found that expanded polytetrafluoroethylene was more effective than oxidised regenerated cellulose in reducing the incidence of adhesion re‐formation on SLL (OR 0.13, 95% CI 0.02 to 0.80, 1 study, n = 23, I2 = N/A, low quality evidence).
ii) No reviews found any studies that assessed the effect of oxidised regenerated cellulose versus expanded polytetrafluoroethylene on the mean adhesion score at SLL.
iii) No reviews found any studies that assessed the effect of oxidised regenerated cellulose versus expanded polytetrafluoroethylene on improving or preventing deterioration of the adhesion score at SLL (bimodal outcome)
2. Liquid agents versus versus control or no treatment
Primary outcomes
a. Pelvic pain
Ahmad 2014(b) found one study which investigated the effect of 4% icodextrin in reducing pelvic pain when used during laparoscopy for adhesionolysis. They found that, compared to normal saline, there was no evidence that 4% icodextrin reduced postoperative pelvic pain caused by adhesions (OR 0.65, 95% CI 0.37 to 1.14, 1 study, n = 286, moderate quality evidence).
b. Pregnancy rate
Ahmad 2014(b) found that there was no evidence of a difference between 32% dextran and placebo (either Hartmann's solution or saline) on pregnancy rates (OR 0.64, 95% CI 0.36 to 1.14, 3 studies, n = 310, moderate quality evidence). Miscarriages and ectopic pregnancy rates were not assessed by any of the studies included in the reviews.
c. Live birth rate
Ahmad 2014(b) identified two studies which investigated 32% dextran compared to either Hartmann's solution or saline on live birth rates following gynaecological surgery. Meta‐analysis revealed no evidence of a difference between 32% dextran and no treatment (OR 0.67, 95% CI 0.29 to 1.58, 2 studies, n = 208, moderate quality evidence).
d. Quality of life (QoL) measures
No review found any trials that investigated the effect of liquid agents on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
Adverse outcomes were not reported by any of the studies included in the reviews.
b. Change in adhesion score
i) Ahmad 2014(b) found on meta‐analysis that the incidence of adhesions was significantly reduced when using liquid agents (either 32% dextran, 0.4% hyaluronic acid or 4% icodextrin) compared to control (either saline, phosphate buffered solution or Hartmann's solution) at SLL (OR 0.34, 95% CI 0.22 to 0.55, 4 studies, n = 566, I2 = 0%, high quality evidence).
ii) Ahmad 2014(b) found four studies which reported the mean adhesion score on SLL after using liquid agents (either 32% dextran or 4% icodextrin). On meta‐analysis, there was no significant difference in the mean adhesion score at SLL when compared to saline (OR ‐0.06, 95% CI ‐0.20 to 0.09, 4 studies, n = 722, I2 = 0%, high quality evidence).
iii) On analysis of four studies that looked at adhesion scores in a bimodal fashion, there was no evidence of a difference between liquid agents (either 32% dextran or 4% icodextrin) and control (saline or Hartmann's solution) on causing an improvement in adhesion scores (OR 1.27, 95% CI 0.79 to 2.05, 4 studies, n = 665, I2 = 38%, moderate quality evidence) (Ahmad 2014(b)). Only one study was included by Ahmad 2014(b) that specifically investigated worsening of adhesion scores on SLL with liquid agents. They found no evidence of a difference between liquid agents (4% icodextrin) and saline on worsening adhesion scores at SLL (OR 0.28, 95% CI 0.07 to 0.21, 1 study, n = 53, I2 = N/A, moderate quality evidence).
3a. Gel agents versus no treatment or control
Primary outcomes
a. Pelvic pain
No reviews found any studies that assessed the effect of gel agents on pelvic pain.
b. Pregnancy rate
No reviews found any studies that assessed the effect of gel agents on pregnancy rate.
c. Live birth rate
No reviews found any studies that assessed the effect of gel agents on live birth rate.
d. Quality of life (QoL) measures
No review found any studies that investigated the effect of gel agents on post‐operative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
No reviews found any studies that reported the adverse outcomes from the use of gel agents.
b. Change in adhesion score
i) Ahmad 2014(b) found on analysis of four studies that gel based agents were associated with a significant reduction in the incidence of adhesions at SLL when compared to no treatment (OR 0.25, 95% CI 0.11 to 0.56, 4 studies, n = 134, I2 = 0%, high quality evidence). Of the four studies, one study investigated this using polyethylene glycol gel, two studies used auto‐crosslinked hyaluronic acid gel and one study used sodium hyaluronate spray.
ii) On analysis of two studies, Ahmad 2014(b) found no evidence of a difference in the mean adhesion score at SLL between gel based agents and no treatment (standardised mean difference (SMD) ‐0.13, 95% CI ‐0.65 to 0.39, 2 studies, n = 58, I2 = 0%, moderate quality evidence). One study in the analysis investigated using hyaluronic acid based gel, and the other investigated using sodium hyaluronate spray.
iii) On analysis of two studies, Ahmad 2014(b) found no evidence of a difference with gel based agents when compared to no treatment in improving adhesion scores on SLL (OR 3.78, 95% CI 0.61 to 23.32, 2 studies, n = 58, I2 = 0%, moderate quality evidence). However, gel based agents were found to significantly prevent worsening of adhesion scores at SLL when compared to no treatment (OR 0.16, 95% CI 0.04 to 0.57, 2 studies, n = 58, I2 = 0%, moderate quality evidence). The gel agents used in these two studies included carboxymethylcellulose and polyethylene oxide gel, and polyethylene glycol gel alone.
3b. Gel agents versus liquid agents
Primary outcomes
a. Pelvic pain
No reviews found any studies that compared the effect of gel agents to liquid agents on pelvic pain.
b. Pregnancy rate
No reviews found any studies that compared the effect of gel agents to liquid agents on pregnancy rate.
c. Live birth rate
No reviews found any studies that compared the effect of gel agents to liquid agents on live birth rate.
d. Quality of life (Qol) measures
No review found any studies that investigated the effect of gel agents, compared to liquid agents, on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
No reviews found any studies that compared the adverse outcomes from the use of gel agents to liquid agents.
b. Change in adhesion score
i) Analysis of two studies by Ahmad 2014(b) revealed that 0.5% ferric hyaluronate gel was associated with a significantly reduced incidence of adhesions at SLL compared to saline when used as an instillant (OR 0.36, 95% CI 0.19 to 0.67, 2 studies, n = 342, I2 = 0%, high quality evidence).
ii) One study was identified that reported a significantly lower mean adhesion score at SLL with 0.5% ferric hyaluronate gel compared to saline when used as an instillant (MD ‐0.79, 95% CI ‐0.79 to ‐0.79, 1 study, n = 77, I2 = NA, moderate quality evidence), though Ahmad 2014(b) deemed that these results should be interpreted with caution due to the narrow reported SD of a study with only 38 participants in each arm.
iii) Ahmad 2014(b) identified two trials which both compared 0.5% ferric hyaluronate gel to saline on adhesion scores at SLL. On analysis, there was no evidence of a difference between the two agents (OR 1.55, 95% CI 0.82 to 2.92, 2 studies, n = 342, I2 = 0%, moderate quality evidence). Two studies were also identified that compared 0.5% ferric hyaluronate gel to saline in preventing worsening of adhesion score at SLL. On meta‐analysis, 0.5% ferric hyaluronate gel was found to reduce the chance of patient’s adhesion score worsening at SLL compared to saline (OR 0.28, 95% CI 0.12 to 0.66, 2 studies, n = 342, I2 = 0%, high quality evidence).
4. Pharmacological agents
1. GnRHa versus no GnRHa or control
Ahmad 2014(b) stated that no study was found to be eligible for inclusion in the meta‐analysis. One study showed no evidence of benefit in adhesion scores from a group receiving GnRHa compared to those who did not receive GnHRa, although this was not included in the final meta‐analysis.
2. Reteplase plasminogen activator versus no reteplase plasminogen activator or control
Ahmad 2014(b) stated that no study was found to be eligible for inclusion in the meta‐analysis. Two studies showed no evidence of benefit on adhesion scores from reteplase plasminogen activator use compared to those who did not receive reteplase plasminogen activator, although this finding was not included in the final meta‐analysis.
3. N,O‐carboxymethyl chitosan versus no N,O‐carboxymethyl chitosan or control
Ahmad 2014(b) stated that no study was found to be eligible for inclusion in the meta‐analysis.
4. Steroid agents (including systemic, intraperitoneal, pre and postoperative) versus no steroids or control
Primary outcomes
a. Pelvic pain
No reviews found any studies that assessed the effect of steroid agents on pelvic pain.
b. Pregnancy rate
No reviews found any studies that assessed the effect of steroid agents on pregnancy rate.
c. Live birth rate
Meta‐analysis of two studies by Ahmad 2014(b) found no evidence of a difference between steroid agents and control or no treatment on live birth rates (OR 0.65, 95% CI 0.26 to 1.62, two studies, n = 223, I2 = 0%, moderate quality evidence) or clinical pregnancy rates (OR 1.01, 95% CI 0.66 to 1.55, 3 studies, n = 410, I2 = 0%, moderate quality evidence). However, it is important to note that in one of these studies intravenous hydrocortisone, oral prednisolone and intraperitoneal hydrocortisone were used and were compared to no treatment. The other study only used intraperitoneal hydrocortisone and compared the results to a control (intraperitoneal saline administration). Despite this, the review authors combined the trials.
d. Quality of life (QoL) measures
No review found any studies that investigated the effect of steroid agents on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
No reviews found any studies that reported the adverse outcomes from the use of steroid agents.
b. Change in adhesion score
i) No reviews found any studies that assessed the effect of steroid agents on the incidence of adhesions.
ii) No reviews found any studies that assessed the effect of steroid agents on the mean adhesion score.
iii) Ahmad 2014(b) identified one study which found that steroids compared to no treatment were associated with a significant improvement in adhesion score (OR 4.83, 95% CI 1.71 to 13.65, 1 study, n = 75, low quality evidence). This result should be interpreted with caution as the data were unpublished and were provided by the study author without detailed information regarding the methods of this study. Ahmad 2014(b) Identified two studies which looked at the effect of steroids on preventing worsening of adhesion score at SLL. They found that steroids significantly prevented worsening of the adhesion score compared to no treatment (OR 0.27, 95% CI 0.12 to 0.58, 2 studies, n = 187, I2 = 0%, low quality evidence).
4.1 Intraperitoneal noxytioline versus no noxytioline or control
Primary outcomes
a. Pelvic pain
No reviews found any studies that assessed the effect of intraperitoneal noxytioline on pelvic pain.
b. Pregnancy rate
Ahmad 2014(b) found one study which showed no evidence of a difference between the group receiving intraperitoneal noxytioline and the control group on clinical pregnancy rate (OR 0.66, 95% CI 0.30 to 1.47, 1 study, n = 126, I2 = N/A, moderate quality evidence).
c. Live birth rate
No reviews found any studies that assessed the effect of intraperitoneal noxytioline on live birth rate.
d. Quality of life (QoL) measures
No review found any trials that investigated the effect of Intraperitoneal noxytioline on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
There was no evidence of a difference on ectopic pregnancy rates between participants who received intraperitoneal noxytioline and those who did not (OR 4.91, 95% CI 0.45 to 53.27, P = 0.19, 1 study, n = 33, low quality evidence) (Ahmad 2014(b)). No other adverse effects were reported as outcomes in any studies.
b. Change in adhesion score
i) No reviews found any studies that assessed the effect of intraperitoneal noxytioline on the incidence of adhesions at SLL.
ii) No reviews found any studies that assessed the effect of intraperitoneal noxytioline on the mean adhesion score at SLL.
iii) Ahmad 2014(b) found one study which showed no evidence of a difference between those women receiving intraperitoneal noxytioline and those who did not, in preventing worsening of the adhesion score (OR 0.55, 95% CI 0.17 to 1.76, 1 study, n = 87, I2 = N/A, moderate quality evidence).
4.2 Intraperitoneal heparin versus no heparin (or placebo)
Primary outcomes
a. Pelvic pain
No reviews found any studies that assessed the effect of intraperitoneal heparin on pelvic pain.
b. Pregnancy rate
No reviews found any studies that assessed the effect of intraperitoneal heparin on clinical pregnancy rate.
c. Live birth rate
No reviews found any studies that assessed the effect of intraperitoneal heparin on live birth rate.
d. Quality of life (QoL) measures
No review found any trials that investigated the effect of intraperitoneal heparin on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
No reviews found any studies that reported adverse outcomes from the use of intraperitoneal heparin.
b. Change in adhesion score
i) No reviews found any studies that assessed the effect of intraperitoneal heparin on the incidence of adhesions at SLL.
ii) No reviews found any studies that assessed the effect of intraperitoneal heparin on the mean adhesion score at SLL.
iii) Ahmad 2014(b) found one study which found no evidence of a difference between participants who received intraperitoneal heparin and those who did not in either improving adhesion scores at SLL (OR 0.87, 95% CI 0.32 to 2.35, 1 study, n = 63, I2 = NA, low quality evidence) or preventing worsening of adhesion scores at SLL (OR 1.27, 95% CI 0.56 to 2.91, 1 study, n = 92, I2 = 0%, low quality evidence).
4.3 Systemic promethazine versus no promethazine (or placebo)
Primary outcomes
a. Pelvic pain
No reviews found any studies that assessed the effect of systemic promethazine on pelvic pain.
b. Pregnancy rate
No reviews found any studies that assessed the effect of systemic promethazine on clinical pregnancy rate.
c. Live birth rate
No reviews found any studies that assessed the effect of systemic promethazine on live birth rate.
d. Quality of life (QoL) measures
No review found any trials that investigated the effect of systemic promethazine on postoperative QoL using validated tools.
Secondary outcomes
a. Adverse outcomes
No reviews found any studies that reported the adverse outcomes from the use of systemic promethazine.
b. Change in adhesion score
i) No reviews found any studies that assessed the effect of systemic promethazine on the incidence of adhesions at SLL.
ii) No reviews found any studies that assessed the effect of systemic promethazine on the mean adhesion score at SLL.
iii) Ahmad 2014(b) found one study which showed no evidence of a difference between participants who received systemic promethazine compared to those who did not in improving adhesion scores at second‐look surgery (OR 0.56, 95% CI 0.22 to 1.43, 1 study, n = 75%, I2 = N/A, low quality evidence), and no evidence of preventing worsening of adhesion scores at second‐look surgery (OR 0.59, 95% CI 0.25 to 1.42, 1 study, n = 93, I2 = 0%, low quality evidence).
Discussion
Summary of main results
Primary outcomes
No reviews identified any studies that investigated the effect of solid, gel or pharmacological agents on pelvic pain, pregnancy rate, live birth rate or QoL, which were our primary outcomes.
There was no conclusive evidence of a difference between liquid agents and control with regard to pelvic pain (moderate quality evidence), pregnancy rate (moderate quality evidence) or live birth rate (moderate quality evidence). No reviews identified any studies that investigated the effect of liquid agents on QoL.
Secondary outcomes:
Adverse events were reported as an outcome by only 10 of the 47 primary studies in these reviews. Although these reported no adverse events, data were insufficient to reach any conclusions with regard to the safety of these interventions.
Oxidised regenerated cellulose during laparoscopy was associated with a reduction in the incidence of de novo adhesions and re‐formation adhesions, though the evidence ranged from very low to low quality.
During laparotomy, oxidised regenerated cellulose was associated with a reduction in the incidence of re‐formation adhesions compared with control, though the evidence was low quality.
Expanded polytetrafluoroethylene during laparotomy was associated with a reduction in the incidence of de novo adhesions compared with control, though the evidence was low quality.
There was no conclusive evidence of a difference in the incidence of adhesions between sodium hyaluronate and carboxymethylcellulose and control. However, sodium hyaluronate and carboxymethylcellulose were associated with a reduction in the mean adhesion score compared to control on SLL, though the evidence was of moderate quality.
There was no conclusive evidence of a difference between fibrin sheets and control on the incidence of adhesions (moderate quality evidence) or on the mean adhesion score (very low quality evidence).
Liquid agents were associated with a reduction in the incidence of adhesions at SLL compared to no treatment or control (high quality evidence). However, there was no evidence of a difference between liquid agents and control on mean adhesion scores (high quality evidence) or in improving adhesion scores as a bimodal outcome (moderate quality evidence).
Gel agents were associated with a reduction in the incidence of adhesions at SLL when compared to no treatment (high quality evidence).
For pharmacological agents, steroids were associated with a significant improvement in adhesion scores compared to control (low quality evidence). There was no evidence of a difference in adhesion scores between intraperitoneal noxytioline and control (moderate quality evidence), intraperitoneal heparin and control (low quality evidence) or systemic promethazine (low quality evidence) and control.
Overall completeness and applicability of evidence
One of the most important conclusions derived from this overview is that there is a general lack of trials that have investigated clinically relevant endpoints. The overwhelming majority of trials instead focused on surrogate markers such as adhesion scores and the incidence of adhesions on SLL. Only 8 studies out of 47 across both reviews investigated the effect of anti‐adhesion agents on our primary outcomes of pelvic pain, pregnancy rate, live birth rate and QoL (Ahmad 2014(a); Ahmad 2014(b)). There is controversy as to the use of adhesion scores in assessing outcomes. While there is a link between adhesion scores or incidence and factors such as pain, fertility and QoL (Diamond 2010), a reduction in adhesions does not directly lead to improved outcomes in all patients. This is in part due to the multi‐factorial aetiology of diseases such as chronic pelvic pain and infertility. As a result, trials that investigate outcomes such as pelvic pain and infertility are required to be large, well controlled and adjusted for confounding factors. This is often beyond the capability of many research teams, which is why surrogate endpoints such as adhesion scores are used. Nonetheless, readers should note that an improvement in adhesion score or incidence does not always translate to improvement for women in clinical practice, and this severely limits the applicability of the evidence in this overview.
It is difficult to make conclusions regarding the applicability of the included reviews to other clinical settings. This is because, apart from age, other aspects of participant characteristics (such as race, previous gynaecological surgery etc.) were not detailed by the reviews. However, every study (across both Ahmad 2014(a) and Ahmad 2014(b)) was carried out in the clinical setting. Furthermore, studies were distributed across centres in Europe, North America, Australia and Japan. While certain comparisons only contained studies from one region (for example oxidised regenerated cellulose versus no treatment or control only included studies from European centres), there is no evidence to suggest that outcomes would have been markedly different should they have taken place in other developed countries. It should, however, be noted that there is a lack of studies covering regions in the developing world, and thus care must be taken before applying this overview to those regions.
We envisage no issues in the applicability of the interventions covered in this review. It should be noted that there was little usable evidence regarding the adverse effects of the anti‐adhesion agents included in this overview. Therefore, though some of these agents may be associated with an improved adhesion score, this benefit may not necessarily outweigh the adverse effects from the intervention. While anti‐adhesion agents have traditionally been associated with a low side effect profile, this overview cannot make definitive conclusions as to whether this side effect profile outweighs the benefits of their use. Furthermore, no trials were identified that did a cost benefit analysis with any of the interventions. This could be an area of possible future research with these interventions. This overview also did not examine the effect of anti‐adhesion agents on surgical time. Some anti‐adhesion agents are required to be sutured into place, and may prolong surgical time, which in turn may increase the problems associated with the procedure. While it was not part of our initial protocol, we found no usable evidence in either Ahmad 2014(a) or Ahmad 2014(b) that investigated this.
We believe that the most common forms of anti‐adhesion agents have been covered across both reviews included in this overview. However, there were no randomised controlled trials identified for newer anti‐adhesion agents that are formed from lactic acid derived polymers (Surgiwrap) or polyethylene glycol mixtures (Coseal), both of which could be considered for inclusion in Ahmad 2014(a). No studies were reported as eligible for inclusion that investigated GnRHa, reteplase plasminogen activator or non‐steroidal anti‐inflammatory drugs, which would have been considered for inclusion in Ahmad 2014(b). Further research will be needed in these areas before conclusions can be made about their efficacy. No other classes of anti‐adhesion agents, to the authors' knowledge, have been produced that would not be eligible for inclusion in either Ahmad 2014(a) or Ahmad 2014(b).
It should be noted that while Ahmad 2014(a) distinguished between studies investigating de novo adhesions following surgery from studies investigating re‐formation adhesions following adhesionolysis, Ahmad 2014(b) did not. The authors of Ahmad 2014(b) stated that this was because too few studies distinguished between de novo adhesions and re‐formation adhesions in their review. It is believed to be easier to demonstrate benefit with re‐formation adhesions compared to de novo adhesions, mainly due to the higher baseline adhesion scores in the former. This is because the scope for deterioration in the score is smaller with a higher baseline score, while the scope for improvement is greater. Therefore, combining the two may affect the internal validity of the results.
To enhance the completeness of this review, there should be further high powered studies investigating interventions such as sodium hyaluronate and carboxymethylcellulose, expanded polytetrafluoroethylene and other interventions where the evidence has been limited to one or two trials (these are further outlined in the summary of findings table). Further research testing these interventions in different clinical settings would enhance both the quality and applicability of the evidence. The important factor of surgical time should also be investigated in future trials so that this can be addressed in future updates of this overview.
Quality of the evidence
In both Ahmad 2014(a) and Ahmad 2014(b), the quality of evidence for most comparisons was downgraded due to risk of bias in individual studies. Specifically, only 23 of 47 included trials showed adequate random sequence generation (5 of the 18 in Ahmad 2014(a), 18 of the 29 in Ahmad 2014(b)), while only 12 out of the 47 trials detailed adequate allocation concealment (1 of the 18 trials in Ahmad 2014(a), 11 of 29 trials in Ahmad 2014(b)). Only 28 out of 47 trials were considered low risk for attrition bias (5 of 18 studies in Ahmad 2014(a), 23 of 29 trials in Ahmad 2014(b)), while 18 out of 47 studies were deemed low risk for performance or detection bias (2 out of 18 trials in Ahmad 2014(a), 16 of 29 trials in Ahmad 2014(b)). 25 out of 47 trials were at low risk for selection bias (0 out of 18 in Ahmad 2014(a), 25 out of 29 in Ahmad 2014(b)). In most other cases the risk of bias was deemed unclear.
Only one comparison in Ahmad 2014(a) (oxidised regenerated cellulose compared to no treatment at laparoscopy) had the quality downgraded due to high levels of heterogeneity. This was determined by the poor confidence interval overlap between studies in this comparison, an I2 of 75% and a Chi2 P value of 0.02. We identified multiple factors that could contribute to this heterogeneity. For instance, the timing until reassessment was different between these studies, and the type of surgery carried out was also different between the three trials. Some trials had a high dropout rate (up to 22%) compared to the other studies. There were a number of other differences between the three trials that may also have contributed to the inconsistency (patient characteristics, pre‐existing adhesions, etc.), and further studies will be needed before any firm conclusions can be made regarding oxidised regenerated cellulose in preventing de novo adhesions following laparoscopy. Other comparisons in Ahmad 2014(a) were either not at high risk of heterogeneity or were limited to one study. In Ahmad 2014(b), most comparisons with more than one trial were deemed to be at low risk of heterogeneity, with good overlap of the confidence intervals, a non‐significant Chi2 result, and a low I2 statistic. Only the comparison of liquid agent versus no treatment or control, improvement in adhesion score at SLL, showed moderate levels of heterogeneity with an I2 = 38%. However, there was still good overlap of the confidence intervals between studies, and the Chi2 P value was non‐significant. Nonetheless, like Ahmad 2014(a), the timing until reassessment was different between studies and the type of surgery carried out between the included trials differed quite markedly. This would have contributed to some of the heterogeneity seen in this comparison.
In Ahmad 2014(a), imprecision was apparent for the comparisons involving fibrin sheets, expanded polytetrafluoroethylene, and sodium hyaluronate and carboxymethylcellulose versus no treatment or control. The analyses for these comparisons were limited to only one trial each, with participant numbers in each trial ranging from 41 to 127 patients. Confidence intervals were also wide, and further high powered trials investigating these interventions are needed before we can make firm conclusions on the point estimate of these interventions. Imprecision was evident for a number of comparisons in Ahmad 2014(b) that were limited to only one study with a small study population (see summary of finding table for details). Further high powered trials investigating these interventions are needed before we can make firm conclusions on the point estimate of these interventions.
Comparisons investigating adhesion scores in Ahmad 2014(a) were downgraded as they did not use validated adhesion scores. Only three studies reported adhesion scores in this review (Diamond 1996; Haney 1995; Tackeuchi 2005). However, only data from non‐validated scores were able to be included in the meta‐analysis. One study (Tackeuchi 2005) reported a validated score (the modified American Fertility Score (mAFS)), though due to the way the results were presented the authors of Ahmad 2014(a) were unable to incorporate these data in their analysis.
Publication bias was impossible to assess formally in either Ahmad 2014(a) or Ahmad 2014(b) as there were too few studies per comparison to make any meaningful conclusions. However, 25 of 47 studies across both reviews had some form of external funding from a private company. As outlined above, publication bias favouring the intervention can occur in meta‐analyses that include a large number of privately funded trials (Bhandari 2004; Lexchin 2003). This could, in part, be due to privately funded companies discouraging the publication of trials that show no benefit for their intervention (Rennie 1997). Therefore, the conclusions of this overview must be considered within this context. Ahmad 2014(a) also found that there was duplication of study data amongst different publications. This was especially evident for the comparison of oxidised regenerated cellulose versus no treatment or control at either laparoscopy or laparotomy, with five of the included studies having duplicate data in other publications. The comparison of expanded polytetrofluoroethylene versus no treatment also contained one study whose results had been duplicated across publications. While these were identified in the review, it is impossible to rule out that this may not have been the case for other studies in the reviews. Finally, it is stated in Ahmad 2014(a) that there was evidence that UK centres in the 1990s were randomising patients for a trial investigating oxidised regenerated cellulose. However, only results from Sheffield (Li 1994) were ever published. As such, taking all these factors into consideration, we would argue that the potential for publication bias is high across this overview and this should almost certainly be considered when interpreting the results.
While Ahmad 2014(a) distinguished between studies investigating 'de novo' adhesions following surgery from studies investigating re‐formation adhesions (following adhesionolysis), Ahmad 2014(b) did not. This is because too few studies distinguished between de novo adhesions and re‐formation adhesions in Ahmad 2014(b). It is believed to be easier to demonstrate benefit with interventions for patients who suffer re‐formation adhesions. This is because the higher baseline adhesion scores make the scope for a deterioration in the score smaller; they also make the scope for an improvement in the adhesion score greater. As such, combining trials that investigate de novo adhesions with those that investigate re‐formation adhesions may have affected the internal validity of the results.
Furthermore, Ahmad 2014(b) did not distinguish between different types of liquid agents, with dextran, 0.4% hyaluronic acid and icodextrin all being analysed in the same meta‐analysis. As there is little evidence as to whether there is a difference between these agents in terms of superiority, it is difficult to gauge whether a possible beneficial effect seen by one of these agents was masked by the lack of beneficial effect seen in the other agents.
In both reviews, many studies excluded participants at SLL if they were pregnant. While this is fully understandable with regards to the increased risk to the participant, it should be noted that participants who are able to conceive are likely to have less severe adhesions. Therefore, by excluding these participants, the studies may have introduced bias into the results by increasing the mean severity of adhesion scores across the included population.
As a final note, it is important to draw attention to the fact that adhesion scores were reported in an inconsistent manner across studies in both Ahmad 2014(a) and Ahmad 2014(b). Adhesions were reported in terms of incidence, change in adhesion score, improvement in adhesion score (bimodal), worsening of adhesion score, adhesion formation per site, extent of adhesions, and area covered by adhesions. This reduces the power of a meta‐analysis as some trials looking at the same intervention cannot be compared like for like. Furthermore, this opens up the potential for selection bias in the results. Specifically, as there appears to be no accepted standardised method of judging adhesions, it is possible that outcomes were picked based on the type of intervention used, which would be a form of selection bias. Finally, it opens up the risk in all studies looking at multiple outcomes in that it increases the risk of a 'significant' result occurring by chance. There is no way that we can judge the effect this had on our results, though further high powered trials looking at standardised clinically relevant endpoints will give us a better indication in the future.
Potential biases in the overview process
A potential bias that should be considered is that this overview limits itself to published Cochrane reviews. As such, the search did not seek to include systematic reviews not published by The Cochrane Collaboration. Therefore, the conclusions of this overview should take into account that well designed non‐Cochrane systematic reviews are not included.
Agreements and disagreements with other studies or reviews
One systematic review has recently been published in the Lancet looking at the benefits of certain adhesion preventing agents in all forms of surgery (ten Broek 2014). The specific agents investigated included sodium hyaluronate and carboxymethylcellulose, oxidised regenerated cellulose, icodextrin 4% and polyethylene glycol. The majority of their conclusions were similar to those of this overview with regards to gynaecological surgery. They found that oxidised regenerated cellulose was associated with a possible reduced incidence of adhesions in gynaecological surgery on meta‐analysis. They also found no evidence for polyethylene glycol gel based products on improving the incidence of adhesions in their meta‐analysis.
However, ten Broek 2014 found that the mean adhesion score improved with polyethylene glycol gel versus no treatment. This partially contradicts the results of Ahmad 2014(b), which found no benefit with gel based agents on the mean adhesion score at SLL. There are several reasons for this discrepancy. Firstly, ten Broek 2014 included the results of the study Mettler 2008 in this analysis, which looked at polyethylene glycol gels in preventing adhesions at either laparoscopy or laparotomy during gynaecological surgery (where it was assigned 78.4% weighting). Ahmad 2014(b), on the other hand, argued that the high risk of selection bias in Mettler 2008 meant that including it would undermine the quality of the evidence. Mettler 2008, in their initial protocol, stated that they would grade adhesions by taking an average mAFS score from all those sites that had been treated. However, they state that "In hindsight, it became apparent that use of this score would have biased the interpretation of results" in favour of the control. Therefore, they changed their study after "review of the myomectomy surgery record" to only include scores from the posterior uterus. Ahmad 2014(b) seems to argue that, though the initial protocol may have biased the results, the change in the protocol was done primarily to favour the intervention and thus led this study to being at a high risk of selection bias. ten Broek 2014 also seemed to recognise a high risk of selection bias in Mettler 2008, though they still included the study. However, they too warn that "the studies assessing these outcomes had a high risk of random error" (ten Broek 2014).
Another reason why the analysis differed is that the Ahmad 2014(a) review included one study that investigated hyaluronic acid gels (Mais 1995), as per their review protocol. ten Broek 2014 on the other hand did not include the study by Mais 1995 as it did not look at polyethylene glycol, which was the focus of their analysis. One could reasonably argue that polyethylene glycol should be analysed separately from other gel materials, as per ten Broek 2014. Of the other studies that looked at polyethylene glycol, in both reviews, one found benefit for the intervention (Mettler 2008) while one found no benefit for the intervention (ten Broek 2012).
Another important discrepancy between ten Broek 2014 and this overview is that ten Broek 2014 had more confidence in the results of their meta‐analysis, stating that "Oxidised regenerated cellulose and hyaluronate carboxymethylcellulose can safely reduce clinically relevant consequences of adhesions" (ten Broek 2014). The conclusions of this overview, however, are much more tentative. This is possibly due to two reasons. Firstly, ten Broek 2014 assessed the risk of bias of their included studies more leniently than either Ahmad 2014(a) or Ahmad 2014(b). For example, three of seven trials rated by ten Broek 2014 as having low risk random sequence generation were rated as having unclear risk by Ahmad 2014(a). Likewise, four out of seven trials rated as having a low risk allocation concealment method by ten Broek 2014 were rated as having unclear sequence generation by Ahmad 2014(a). This is despite Ahmad 2014(a), Ahmad 2014(b) and ten Broek 2014 all using the Cochrane Collaboration tool for assessing risk of bias (It should be noted that many of the authors involved in extracting the data in Ahmad 2014(a) were also involved in extracting the data from Ahmad 2014(b)). The reason for this discrepancy is difficult to ascertain as the justifications for the scores have not been published by ten Broek 2014. We are currently in discussions with the authors of ten Broek 2014 regarding this, and will update the overview should we decide to change our rating assessments.
Our overview has also judged that the large number of funded studies mean that there is a risk of publication bias affecting our results, even though it could not be formally assessed. ten Broek 2014, however, argued that there is a low risk that publication bias has influenced their results. They argue that the results of unpublished studies match those of published reports, and that the funnel plots for their analysis show no evidence of publication bias. Conversely, however, one could argue that ten Broek 2014 only identified one unpublished trial investigating anti‐adhesion agents in gynaecological surgery (De Wilde 2014). Furthermore, one could argue that the funnel plots are not applicable to most of their comparisons investigating gynaecological surgery. This is because all of their comparisons for anti‐adhesion agents in gynaecological surgery contained less than 10 studies each, with the majority containing only two or three studies. Their largest comparison looking at gynaecological surgery involved eight trials, though six of the eight trials had a similar standard error. This was also true for their second largest analysis which contained six trials (adhesion score during SLL for oxidised regenerated cellulose), with five of the trials having similar standard errors. One could argue that it is difficult to look or test for asymmetry in the funnel plots when the number of trials is small and there is a similar standard error between the trials.
On the other hand, ten Broek 2014 convincingly argued that there is no direct evidence that publication bias does exist in the meta‐analysis. Furthermore, a large number of privately funded trials in a meta‐analysis cannot be the sole basis of writing off the results of a review, as it is largely unclear as to what impact this will have. Ultimatelly, this is a controversial topic and readers will need to take this into account when interpreting the conclusions of this overview.
Authors' conclusions
Implications for practice.
There is insufficient evidence to allow us to draw any conclusions about the effectiveness and safety of anti‐adhesion agents in gynaecological surgery, due to lack of data on pelvic pain, fertility outcomes, quality of life or safety. A substantial proportion of research in this field has been funded by private companies that manufacture these agents, and further high powered, independent trials will be needed before definitive conclusions can be made.
Implications for research.
Further high powered trials investigating clinically relevant endpoints, such as pelvic pain, fertility and quality of life, are needed to assess whether the improvement seen in the adhesion scores with some of the interventions translates to clinical benefit. Furthermore, detailed cost benefit analysis is needed to justify the use of anti‐adhesion agents in clinical practice.
Studies evaluating adhesions need to assess adhesions in a consistent manner using validated adhesion scores. The multiple methods of assessing adhesions (such as incidence of adhesions, worsening of adhesion score, mean adhesion score etc.) make it difficult to combine data in a meta‐analysis, and thus make it difficult to form meaningful conclusions from the results. The adverse effects of anti‐adhesion agents, and the effect they have on different subgroups of patients, also need to be further investigated.
Notes
None
Acknowledgements
Currently, two Cochrane reviews (Ahmad 2014(a); Ahmad 2014(b)) have assessed the effectiveness of adhesion prevention agents. Several of the authors of the present overview contributed to both of these reviews. Ahmad 2014(b) evaluated liquid, gel and pharmacological agents; and Ahmad 2014(a) analysed solid agents.
We acknowledge the contributions of Dr Helena O'Flynn to early drafts of this protocol.
Appendices
Appendix 1. Abbreviations
SLL = Second‐look laparoscopy
CI = Confidence interval
n = Number of participants
OR = Odds ratio
SMD = Standard mean difference
QoL = Quality of life
Contributions of authors
AH drafted the protocol, helped extract the data and wrote the review.
GA conceived the idea, helped draft the protocol, supervised AH throughout the overview, and commented on draft and final versions of the review.
SD helped with planning the data analysis, and commented on draft and final versions of the review.
LB assisted in drafting the protocol, extracting data, writing the report, and commented on drafts and final versions of the review.
AW helped in developing the protocol idea, and commented on drafts and final versions of the overview, and supervised the co‐authors.
Sources of support
Internal sources
There were no sources of support, Other.
External sources
National Institute of Health Research, UK, £5,000, UK.
Declarations of interest
Overview authors Akshay Hindocha, Sofia Dias, Andrew Watson and Gaity Ahmad are authors of the included Cochrane systematic reviews.
New
References
References to included reviews
Ahmad 2014(a)
- Ahmad G, Duffy JMN, Farquhar C, Watson A. Barrier agents for adhesion prevention after gynaecological surgery. Cochrane Database of Systematic Reviews 2014, Issue 11. [DOI] [PubMed] [Google Scholar]
Ahmad 2014(b)
- Ahmad G, Mackie FL, Iles DA, O'Flynn H, Dias S, Metwally M, Watson A. Fluid and pharmacological agents for adhesion prevention after gynaecological surgery. Cochrane Database of Systematic Reviews 2014, Issue 7. [DOI: 10.1002/14651858] [DOI] [PubMed] [Google Scholar]
Additional references
Adhesion SG 1983
- Adhesion Study Group (Buttram V, Malinak R, Cleary R, Cohen S, Cowan B, Daniell J, et al). Reduction of postoperative pelvic adhesions with intraperitoneal 32% dextran 70: a prospective, randomized clinical trial. Fertility and Sterility 1983;40:612‐9. [DOI] [PubMed] [Google Scholar]
Bakkum 1995
- Bakkum EA, Trimbos‐Kemper TC. Natural course of postsurgical adhesions. Microsurgery 1995;16(9):650‐4. [DOI] [PubMed] [Google Scholar]
Bhandari 2004
- Bhandari M, Busse JW, Jackowski D, Montori VM, Schünemann H, Sprague S, et al. Association between industry funding and statistically significant pro‐industry findings in medical and surgical randomized trials. Canadian Medical Association Journal 2004;170:477‐80. [PMC free article] [PubMed] [Google Scholar]
Bosteels 2014
- Bosteels J, Weyers S, Kasius J, Broekmans FJ, Mol BWJ, D’Hooghe TM. Anti‐adhesion therapy following operative hysteroscopy for treating female subfertility. Cochrane Database of Systematic Reviews May 2014, Issue 1. [Google Scholar]
Cheong 2011
- Cheong Y, Laird S, Li T, Shelton K, Ledger W, Cooke I. Peritoneal healing and adhesion formation/reformation. Human Reproduction Update 2011;7:556‐66. [DOI] [PubMed] [Google Scholar]
Cheong 2014
- Cheong Y, Reading I, Bailey S, Sadek K, Ledger W, LI T. Should women with chronic pelvic pain have adhesiolysis?. BMC Women's Health 2014;14:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Wilde 2014
- Wilde RL. Post market study for an adhesion barrier following laparoscopic myomectomy. http://clinicaltrials.gov/show/NCT00891657.
Diamond 1996
- Diamond MP. Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL‐F): a blinded, prospective, randomized, multicenter clinical study. Seprafilm Adhesion Study Group. Fertility and Sterility 1996;66(6):904‐10. [PubMed] [Google Scholar]
Diamond 1998
- Diamond MP. Reduction of de novo postsurgical adhesions by intraoperative pre coating with Sepracoat (HAL‐C) solution: a prospective, randomized, blinded, placebo controlled multicenter study. Fertility and Sterility 1998;69(6):1067‐74. [DOI] [PubMed] [Google Scholar]
Diamond 2001
- Diamond M, Freeman M. Clinical implications of postsurgical adhesions. Human Reproduction Update 2001;7:567‐76. [DOI] [PubMed] [Google Scholar]
Diamond 2010
- Diamond M, Wexner S, diZereg G, Korell M, Zmora O, Goor H, Kamar M. Adhesion prevention and reduction: Current status and future recommendations of a Multinational Interdisciplinary Consensus Conference. Surgical Innovation 2010;17(3):183‐8. [DOI] [PubMed] [Google Scholar]
Diamond 2012
- Diamond M, Burns E, Accomando B, Mian S, Holmdahl L. Seprafilm® adhesion barrier: a review of the clinical literature on intraabdominal use. Gynecological Surgery 2012;9(3):247‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
diZerega 1994
- diZerega G. Contemporary adhesion prevention. Fertility and Sterility 1994;61:219‐35. [DOI] [PubMed] [Google Scholar]
Hammoud 2004
- Hammoud A, Gago L, Diamond M. Adhesions in patients with chronic pelvic pain: a role for adhesiolysis?. Fertility and Sterility 2004;82:1483‐91. [DOI] [PubMed] [Google Scholar]
Haney 1995
- Haney A, Hesla J, Hurst B, Kettel M, Murphy A, Rock J, et al. Prevention of pelvic side wall adhesion reformation using surgical barriers: Expanded polytetrafluororethylene (Gore‐Tex surgical membrane) is superior to oxidised regenerated cellulose (Interceed TC7). Fertility and Sterility 1994;210:265. [PubMed] [Google Scholar]
Hindocha 2014
- Hindocha A, Beere L, Dias S, Watson A, Ahmad G. Adhesion prevention agents for gynaecological surgery: an overview of Cochrane reviews. Cochrane Database of Systematic Reviews 05/08/2014, Issue 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hosie 2001
- Hosie K, Gilbert JA, Kerr D, Brown CB, Peers EM. Fluid dynamics in man of an intraperitoneal drug delivery solution: 4% icodextrin. Drug Delivery 2001;8(1):9‐12. [DOI] [PubMed] [Google Scholar]
Johns 2001
- Johns DB, Keyport GM, Hoehler F, Zerega GS. Reduction of postsurgical adhesion with Intergel adhesion prevention solution: a multicenter study of safety and efficacy after conservative gynaecologic surgery. Fertility and Sterility 2001;76(3):595‐604. [DOI] [PubMed] [Google Scholar]
Kumar 2009
- Kumar S, Wong P, Leaper D. Intra‐peritoneal prophylactic agents for preventing adhesions and adhesive intestinal obstruction after non‐gyneacological abdominal surgery. Cochrane Database of Systematic Reviews 2009, Issue 1, DOI 10.1002/14651858.CD005080. [DOI] [PubMed] [Google Scholar]
Lexchin 2003
- Lexchin J, Bero LA, Djulbegovic B, Clark O. Pharmaceutical industry sponsorship and research outcome and quality: systematic review. BMJ 2003;326:1167‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 1994
- Li TC, Cooke ID. The value of an absorbable adhesion barrier, Interceed, in the prevention of adhesion reformation following microsurgical adhesiolysis. British Journal of Obstetrics and Gynaecology 1994;101(4):335‐9. [DOI] [PubMed] [Google Scholar]
Liakakos 2001
- Liakakos T, Thomakos N, Fine PM, Dervenis C, Young R. Peritoneal adhesions: Etiology, pathophysiology, and clinical significance. Digestive Surgery 2001;18:260‐73. [DOI] [PubMed] [Google Scholar]
Lower 2000
- Lower AM, Hawthorn RJS, Emeritus HE, O'Brien F, Buchan S, Crowe AM. The impact of adhesions on hospital readmissions over ten years after 8849 open gynaecological operations: an assessment from the Surgical and Clinical Adhesions Research Study. British Journal of Obstetrics and Gynaecology 2000;107:855‐62. [DOI] [PubMed] [Google Scholar]
Lower 2004
- Lower AM, Hawthorn RJ, Clark D, Boyd JH, Finlayson AR, Knight AD, et al. Surgical and Clinical Research (SCAR) Group. Adhesion‐related readmissions following gynaecological laparoscopy or laparotomy in Scotland: an epidemiological study of 24 046 patients. Human Reproduction 2004;19(8):1877‐85. [DOI] [PubMed] [Google Scholar]
Mais 1995
- Mais V, Ajossa S, Marongiu D, Peiretti R, Guerriero S, Melis G. Reduction of adhesion reformation after laparoscopic endometriosis surgery: a randomised trial with an oxidized regenerated cellulose absorbable barrier. Obstetrics and Gynecology 1995;86(4, Pt 1):512‐5. [DOI] [PubMed] [Google Scholar]
Mais 2014
- Mais V. Peritoneal adhesions after laparoscopic gastrointestinal surgery. World Journal of Gastroenterology 2014;20(17):4917‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mettler 2004
- Mettler L, Audebert A, Lehmann‐Willenbrock E, Schive‐Peterhansi K, Jacobs V. A randomized prospective,controlled, multicenter clinical trial of a sprayable, site specific adhesion barrier system in patients undergoing myomectomy. Fertility and Sterility 2004;82(2):398‐404. [DOI] [PubMed] [Google Scholar]
Mettler 2008
- Mettler L, Hucke J, Bojahr B, Tinneberg HR, LeylandN, Avelar R. A safety and efficacy study of a resorbable hydrogel for reduction of post‐operative adhesions following myomectomy. Human Reproduction 2008;23(5):1093‐100. [DOI] [PubMed] [Google Scholar]
Pellicno 2003
- Pellicno M, Bramamte S, Cirillo D. Effectiveness of auto‐cross linked hyaluronic acid gel after laparoscopic myomectomy in infertile patients: a prospective randomised controlled study. Fertility and Sterility 2003;80:441‐4. [DOI] [PubMed] [Google Scholar]
Rennie 1997
- Rennie D. Thyroid storms. JAMA 1997;277:1238‐43. [PubMed] [Google Scholar]
Robertson 2010
- Robertson D, Lefebvre G. Adhesion prevention in gynaecological surgery. Journal of Obstetrics and Gynaecology Canada 2010;32:598‐608. [DOI] [PubMed] [Google Scholar]
SRS 2007
- Practice Committee of the American Society for Reproductive Medicine: Society of Reproductive Surgeons. Pathogenesis, consequences and control of peritoneal adhesions in gynaecological surgery. Fertility and Sterility 2007;88:21‐6. [DOI] [PubMed] [Google Scholar]
Swank 2003
- Swank DJ, Swank‐Bordewijk SC, Hop WC, Erp WF, Janssen IM, Bonjer HJ, et al. Laparoscopic adhesiolysis in patients with chronic abdominal pain: a blinded randomised controlled multi‐centre trial. Lancet 2003;12(361(9365)):1247‐51. [DOI] [PubMed] [Google Scholar]
Tackeuchi 2005
- Takeuchi H, Kitade M, Kikuchi I, Shimanuki H, Kumakri J, Kmoshita K. Adhesion prevention effects of fibrin ceilings after laparoscopic myomectomy as determined by second look laparoscopy: a prospective randomised, controlled study. Journal of Reproductive Medicine 2005;50(8):571‐7. [PubMed] [Google Scholar]
ten Broek 2012
- Broek R, Kok‐Krant N, Verhoeve HR, Goor H, Bakkum EA. Efficacy of polyethylene glycol adhesion barrier after gynaecological laparoscopic surgery: results of a randomized control pilot study. Gynaecological Surgery 2012;9:29‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
ten Broek 2013
- Broek R, Issa Y, Santbrink E, Bouvy N, Kruitwagen R, Jekeel J, et al. Burden of adhesions in abdominal and pelvic surgery: a systematic review and meta‐analysis. BMJ 2013;347:f5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
ten Broek 2014
- Broek R, Stommel M, Stirk C, Laarhoven C, Keus F, Goor H. Benefits and harms of adhesion barriers for abdominal surgery: a systematic review and meta‐analysis. Lancet 2014;383(9911):48‐59. [DOI] [PubMed] [Google Scholar]
Tinelli 2011
- Tinelli A, Malvasi A, Guido M, Tsin DA, Hudelist G, Hurs B, et al. Adhesion formation after intracapsular myomectomy with or without adhesion barrier. Fertility and Sterility 2011;95(5):1780–5. [DOI] [PubMed] [Google Scholar]
Wilson 2002
- Wilson MS, Menzies D, Knight AD, Crowe AM. Demonstrating the clinical and cost effectiveness of adhesion reduction strategies. Colorectal Disease 2002;4(5):355‐60. [DOI] [PubMed] [Google Scholar]


