Abstract
Background
Hot flushes are the most common menopausal vasomotor symptom. Hormone therapy (HT) has frequently been recommended for relief of hot flushes, but concerns about the health risks of HT have encouraged women to seek alternative treatments. It has been suggested that acupuncture may reduce hot flush frequency and severity.
Objectives
To determine whether acupuncture is effective and safe for reducing hot flushes and improving the quality of life of menopausal women with vasomotor symptoms.
Search methods
We searched the following databases in January 2013: the Cochrane Menstrual Disorders and Subfertility Group Specialised Trials Register, the Cochrane Central Register of Controlled Trials (CENTRAL), PubMed, EMBASE, CINAHL, PsycINFO, Chinese Biomedical Literature Database (CBM), Chinese Medical Current Content (CMCC), China National Knowledge Infrastructure (CNKI), VIP database, Dissertation Abstracts International, Current Controlled Trials, Clinicaltrials.gov, National Center for Complementary and Alternative Medicine (NCCAM), BIOSIS, AMED, Acubriefs, and Acubase.
Selection criteria
Randomized controlled trials comparing any type of acupuncture to no treatment/control or other treatments for reducing menopausal hot flushes and improving the quality of life of symptomatic perimenopausal/postmenopausal women were eligible for inclusion.
Data collection and analysis
Sixteen studies, with 1155 women, were eligible for inclusion. Three review authors independently assessed trial eligibility and quality, and extracted data. We pooled data where appropriate and calculated mean differences (MDs) and standardized mean differences (SMDs) with 95% confidence intervals (CI). We evaluated the overall quality of the evidence using Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria.
Main results
Eight studies compared acupuncture versus sham acupuncture. No significant difference was found between the groups for hot flush frequency (MD ‐1.13 flushes per day, 95% CI ‐2.55 to 0.29, 8 RCTs, 414 women, I2 = 70%, low‐quality evidence) but flushes were significantly less severe in the acupuncture group, with a small effect size (SMD ‐0.45, 95% CI ‐0.84 to ‐0.05, 6 RCTs, 297 women, I2 = 62%, very‐low‐quality evidence). There was substantial heterogeneity for both these outcomes. In a post hoc sensitivity analysis excluding studies of women with breast cancer, heterogeneity was reduced to 0% for hot flush frequency and 34% for hot flush severity and there was no significant difference between the groups for either outcome.
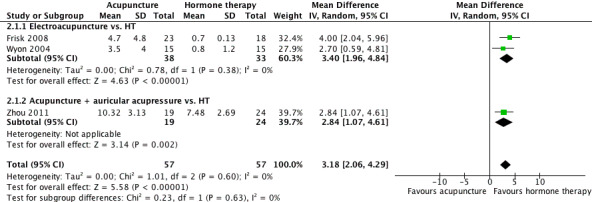
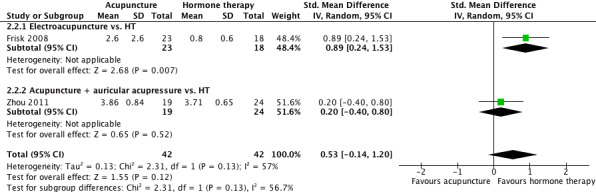
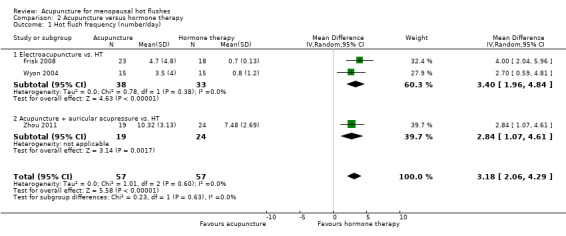
Three studies compared acupuncture versus HT. Acupuncture was associated with significantly more frequent hot flushes than HT (MD 3.18 flushes per day, 95% CI 2.06 to 4.29, 3 RCTs, 114 women, I2 = 0%, low‐quality evidence). There was no significant difference between the groups for hot flush severity (SMD 0.53, 95% CI ‐0.14 to 1.20, 2 RCTs, 84 women, I2 = 57%, low‐quality evidence).
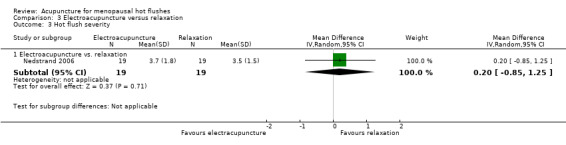
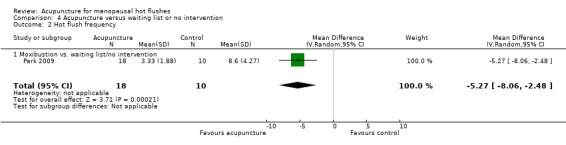
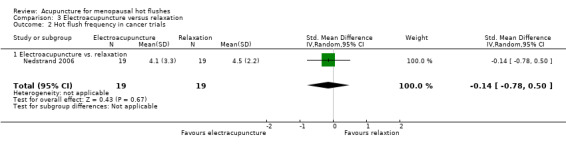
One study compared electroacupuncture versus relaxation. There was no significant difference between the groups for either hot flush frequency (MD ‐0.40 flushes per day, 95% CI ‐2.18 to 1.38, 1 RCT, 38 women, very‐low‐quality evidence) or hot flush severity (MD 0.20, 95% CI ‐0.85 to 1.25, 1 RCT, 38 women, very‐low‐quality evidence).
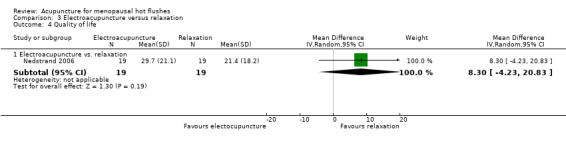
Four studies compared acupuncture versus waiting list or no intervention. Traditional acupuncture was significantly more effective in reducing hot flush frequency from baseline (SMD ‐0.50, 95% CI ‐0.69 to ‐0.31, 3 RCTs, 463 women, I2 = 0%, low‐quality evidence), and was also significantly more effective in reducing hot flush severity (SMD ‐0.54, 95% CI ‐0.73 to ‐0.35, 3 RCTs, 463 women, I2 = 0%, low‐quality evidence). The effect size was moderate in both cases.
For quality of life measures, acupuncture was significantly less effective than HT, but traditional acupuncture was significantly more effective than no intervention. There was no significant difference between acupuncture and other comparators for quality of life. Data on adverse effects were lacking.
Authors' conclusions
We found insufficient evidence to determine whether acupuncture is effective for controlling menopausal vasomotor symptoms. When we compared acupuncture with sham acupuncture, there was no evidence of a significant difference in their effect on menopausal vasomotor symptoms. When we compared acupuncture with no treatment there appeared to be a benefit from acupuncture, but acupuncture appeared to be less effective than HT. These findings should be treated with great caution as the evidence was low or very low quality and the studies comparing acupuncture versus no treatment or HT were not controlled with sham acupuncture or placebo HT. Data on adverse effects were lacking.
Keywords: Female, Humans, Middle Aged, Acupuncture Therapy, Estrogen Replacement Therapy, Hot Flashes, Hot Flashes/drug therapy, Quality of Life
Plain language summary
Acupuncture for menopausal hot flushes
Review question: Is acupuncture safe and effective for reducing hot flushes and improving the quality of life of menopausal women with hot flushes?
Background: Hot flushes are the most common symptoms related to perimenopause and menopause. Hormone therapy (HT) is considered to be the most effective treatment for symptoms. However, studies have reported that hormone therapies may have some negative health effects and many women are now choosing not to use these and are looking for alternatives such as acupuncture. Cochrane review authors examined the evidence, which is current to January 2013.
Study characteristics: Sixteen randomized controlled trials, with 1155 women, were included in the review. Most were small and of short duration. 15 of the 16 included studies reported their funding sources.
Key findings: When acupuncture was compared with sham acupuncture, there was no evidence of any difference in their effect on hot flushes. When acupuncture was compared with no treatment, there appeared to be a benefit from acupuncture, but acupuncture appeared to be less effective than HT.
Quality of the evidence: These findings should be treated with great caution as the evidence was low or very low quality and the studies comparing acupuncture with no treatment or HT were not controlled with sham acupuncture or placebo HT. Data on adverse effects were lacking.
Summary of findings
Summary of findings for the main comparison. Acupuncture versus sham acupuncture for menopausal hot flushes.
| Acupuncture versus sham acupuncture for menopausal hot flushes | ||||
| Population: women with menopausal hot flushes Intervention: acupuncture versus sham acupuncture | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Acupuncture versus sham acupuncture | ||||
| Hot flush frequency (number/day) | The mean hot flush frequency in the intervention groups was 1.13 flushes per day lower (2.55 lower to 0.29 higher) | 414 (8 studies) | ⊕⊕⊝⊝ low1,2 | There was no significant difference between the groups in the mean number of hot flushes per day |
| Hot flush severity | The mean hot flush severity in the intervention groups was 0.45 standard deviations lower (0.84 to 0.05 lower) | 297 (6 studies) | ⊕⊝⊝⊝ very low3,4 | Hot flushes were significantly less severe in the acupuncture group. The size of the effect was small. SMD ‐0.45 (‐0.84 to ‐0.05) |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; SMD: standardized mean difference. | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1 Only 2/8 studies described appropriate methods of randomization and allocation concealment, one of which had very high attrition. 2 Heterogeneity 70%. 3 Heterogeneity 68%. 4 Small total sample (n = 297).
Summary of findings 2. Acupuncture compared to hormone therapy for menopausal hot flushes.
| Acupuncture versus hormone therapy for menopausal hot flushes | ||||
| Population: women with menopausal hot flushes Intervention: acupuncture Comparison: hormone therapy | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Acupuncture versus hormone therapy | ||||
| Hot flush frequency (number/day) | The mean hot flush frequency in the intervention groups was 3.18 flushes per day higher (2.06 to 4.29 higher) | 114 (3 studies) | ⊕⊕⊝⊝ low1,2 | Hot flushes were significantly more common in the acupuncture group than in the hormone therapy group |
| Hot flush severity | The mean hot flush severity in the intervention groups was 0.53 standard deviations higher (0.14 lower to 1.2 higher) | 84 (2 studies) | ⊕⊕⊝⊝ low1,2 | There was no significant difference between the groups in the mean severity of hot flushes SMD 0.53 (‐0.14 to 1.2) |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; SMD: standardized mean difference. | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1 None of studies described method of allocation concealment. 2 Total sample only 114 women.
Summary of findings 3. Electroacupuncture versus relaxation for menopausal hot flushes.
| Electroacupuncture versus relaxation for menopausal hot flushes | ||||
| Population: women with menopausal hot flushes Intervention: electroacupuncture versus relaxation | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Electroacupuncture versus relaxation | ||||
| Hot flush frequency (number/day) | The mean hot flush frequency in the intervention groups was 0.4 flushes per day lower (2.18 lower to 1.38 higher) | 38 (1 study) | ⊕⊝⊝⊝ very low1,2,3 | There was no significant difference between the groups in the frequency or severity of hot flushes |
| Hot flush severity | The mean hot flush severity in the intervention groups was 0.2 higher (0.85 lower to 1.25 higher) | 38 (1 study) | ⊕⊝⊝⊝ very low1,2,3 | |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval. | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1 Methods of randomization and allocation concealment not described in sufficient detail. 2 Single study conducted in women treated for breast cancer. 3 Very small sample (n = 38).
Summary of findings 4. Acupuncture versus waitlist or no intervention for menopausal hot flushes.
| Acupuncture versus waitlist or no intervention for menopausal hot flushes | ||||
| Population: women with menopausal hot flushes Intervention: acupuncture versus waiting list or no intervention | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Acupuncture versus wait listing or no intervention | ||||
| Change in frequency of hot flushes from baseline to end of study | The mean change in frequency of hot flushes from baseline to end of study in the intervention groups was 0.5 standard deviations lower (0.69 to 0.31 lower) | 463 (3 studies) | ⊕⊕⊝⊝ low1 | Acupuncture significantly reduced the frequency and severity of hot flushes compared to waiting list or no intervention The effect size was moderate in both cases Frequency: SMD ‐0.5 (‐0.69 to ‐0.31) Severity: SMD ‐0.54 (‐0.73 to ‐0.35) |
| Change in hot flush severity from baseline to end of study | The mean change in hot flush severity from baseline to end of study in the intervention groups was 0.54 standard deviations lower (0.73 to 0.35 lower) | 463 (3 studies) | ⊕⊕⊝⊝ low1 | |
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; SMD: standardized mean difference. | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1 Only 1/3 studies described satisfactory methods of randomization and allocation concealment; 2/3 unblinded.
Background
Menopause is said to have occurred once a period of 12 months of amenorrhoea (no menstrual periods) has elapsed. Perimenopause is the time period prior to menopause and ends 12 months after the final menstrual period (Soules 2001). This menopausal transition reflects a period of changing ovarian function, which may precede the final menstrual period by between two and eight years (Greendale 1999). Postmenopause is defined as all the years after the last menstrual period (Soules 2001). The menopause is brought about by a decrease in ovarian hormone secretion (Soules 2001). It can occur naturally as the result of aging or from surgical removal of the ovaries, radiotherapy, or chemotherapy. Most women experience natural menopause between 40 and 58 years of age (NIH 2005).
From perimenopause to late postmenopause, some women experience problems such as vasomotor and vaginal symptoms, urinary stress incontinence, sexual dysfunction, impaired quality of life, mood disturbance, depression, and cognitive difficulties (NAMS 2012). Vasomotor symptoms are highly prevalent across menopausal stages in most societies (Freeman 2007).
Description of the condition
Hot flushes (or hot flashes) are the most common vasomotor symptom related to menopause and perimenopause. Hot flushes are thought to result from the brain's response to diminished hormones and hormonal fluctuations during the menopause transition, with instability of the thermoregulatory mechanisms that regulate temperature homeostasis in the hypothalamus (Freeman 2007).
They are characterized by a sensation of intense heat in the face, neck, or chest accompanied by objective signs of cutaneous vasodilation and a subsequent drop in core temperature (Stearns 2002). Women may also experience sweating, flushing, palpitations, anxiety, irritability, and night sweats (Stearns 2002). The reported prevalence of hot flushes varies from 13% to 79% (median 41%) among perimenopausal women and from 8% to 80% (median 41.5%) in postmenopausal women.
It is reported that almost two‐thirds of postmenopausal women experience hot flushes, and 10% to 20% of these find them very distressing (Borud 2009). They are often accompanied by sweating, and can cause disruption of sleep patterns, irritability, and disturbance of daily activity.
Description of the intervention
Hormone therapy (HT) (oestrogen or combined oestrogen‐progestogen therapy) is the most common treatment for hot flushes, and the North American Menopause Society (NAMS 2012) supports its use for treating moderate‐to‐severe vasomotor symptoms. However, an increased risk of cardiovascular disease and breast cancer has been observed in healthy menopausal women treated with HT (Marjoribanks 2012). The publication of the Women's Health Initiative study, which highlighted these risks, has resulted in reduced use of HT. Among French‐speaking women in Quebec, the total number of women on long‐term HT and new users has declined by 28% and 50%, respectively (Guay 2007).
Due to lack of confidence in pharmacological interventions, many menopausal women are trying complementary and alternative medicines (CAM). More than half of peri‐ and postmenopausal women use some type of CAM, including dietary and herbal therapies, stress management, acupuncture, and massage therapy (Newton 2002; Wathen 2006; Gold 2007).
Acupuncture has been proposed for various indications including dental pain, fibromyalgia, nausea, vomiting, knee osteoarthritis, insomnia, epicondylitis, chronic back pain, idiopathic headache, resolution of breech presentation, and as an aid during gastrointestinal endoscopy (Ernst 2006). Estimates of the prevalence of acupuncture use by mid‐life women ranges from 1% to 10.4% (Newton 2002; Wathen 2006; Gold 2007).
Acupuncture is defined as the practice of inserting a needle or needles into certain points in the body for therapeutic purposes (Nasir 2002). Manual pressure (acupressure), small electric currents through the inserted needles (electroacupuncture), and lasers can also stimulate these points. Laser acupuncture is defined as the stimulation of traditional acupuncture points with low‐intensity, non‐thermal laser irradiation (Whittaker 2004).
Types of acupuncture include the following:
traditional Chinese medicine (TCM) acupuncture involves the insertion of needles into body acupoints for therapeutic purposes;
electroacupuncture involves passing small electric currents through the inserted acupuncture needles;
acupressure is a technique that involves manual pressure on the acupoints;
laser acupuncture is defined as the stimulation of traditional acupuncture points with low‐intensity, non‐thermal laser irradiation;
ear acupuncture uses acupuncture needles, seeds, or magnetic pearls to stimulate the acupoints located on the ear;
moxibustion uses the heat generated by burning herbal preparation to stimulate acupuncture points;
scalp acupuncture involves the use of acupuncture needles along the surface of the head.
It has been suggested that acupuncture may have the potential to reduce hot flush frequency and severity.
How the intervention might work
The mechanism by which acupuncture might affect health or menopausal symptoms is not completely understood. Two explanations (Western and Eastern) have been proposed. According to the Western view, luteinizing hormone (LH) pulsatility indicates that β‐endorphin activity is low after the menopause and is increased by oestrogen therapy. Nappi and colleagues found a lower concentration of β‐endorphin in the cerebrospinal fluid of postmenopausal women than in women of fertile age (Nappi 1990). Low levels of central β‐endorphin activity after menopause may contribute to elevated levels of LH and lability in thermoregulation. During oestrogen treatment, increased central opioid activity may account for a decrease in vasomotor symptoms. Acupuncture may act in the same way as HT, by increasing the activity of hypothalamic β‐endorphin (Wyon 2004). It has also been observed that acupuncture may affect the nervous system by modulating the levels of several neurotransmitters and neuropeptides and may also have an immunomodulatory effect (Cabyoglu 2006).
The Eastern view of acupuncture is based on Chinese medical philosophy. Through the stimulation of specific points, acupuncture tries to re‐establish the energy balance in order to treat disease. According to Chinese medicine theory, energy (qi) flows through the body along meridians and the disruption of this flow causes disease (Pearl 1999). TCM acupuncture stimulates the qi at points along the body meridians that pass through major organs. It effectively opens blocked gates to increase energy flow and balance Yin and Yang. This enables the person to achieve optimal health. Acupuncture specific to menopausal symptoms is designed to correct a condition known as deficient heat. This condition is a deficiency in Yin energy and is characterized by "five palm sweats", night sweats, and a general mental agitation. Acupuncture points specific to menopausal symptoms balance the kidney qi by subduing kidney Yang, nourish the heart, and quieten the spirit (Cohen 2003).
Acupuncture treatment might also have additional physical and mental health benefits for perimenopausal and menopausal women, such as improving quality of sleep and decreasing feelings of fatigue.
Why it is important to do this review
If shown to be effective, acupuncture could be used to treat menopausal hot flushes and improve quality of life, offering an alternative to HT. A systematic review is required to determine whether acupuncture is effective and safe for reducing menopausal vasomotor symptoms.
Objectives
To determine whether acupuncture is effective and safe for reducing hot flushes and improving the quality of life of menopausal women with vasomotor symptoms.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomized controlled trials (RCTs) in the review. Studies using cross‐over designs were included only if pre‐cross‐over data were available. We excluded quasi‐RCTs.
Types of participants
We included perimenopausal, menopausal, and postmenopausal women of any age recruited from any healthcare setting in the review. Only women experiencing hot flushes at baseline were included. We defined menopausal status according to the Stages of Reproductive Aging Workshop (STRAW) criteria (Soules 2001). We defined menopause as occurring after 12 months of amenorrhoea; perimenopause as the time period prior to menopause, ending 12 months after the final menstrual period; and postmenopause as all the years beyond the last menstrual period. Trials that included women with menopause due to surgical removal of ovaries, radiation, or chemotherapy were eligible.
Types of interventions
Trials of any type of acupuncture were eligible, including TCM acupuncture, electroacupuncture, acupressure, laser acupuncture, ear acupuncture, moxibustion, and scalp acupuncture, regardless of the duration of treatment.
Control groups could receive no intervention (e.g. wait list), placebo acupuncture, sham acupuncture, HT, or any other active therapy. We defined placebo acupuncture as a needle not penetrating the skin but placed over the same acupuncture points and sham acupuncture as a needle located outside of acupuncture points, or shallow needling.
We considered acupuncture interventions combined with other interventions, provided both interventions were given to both comparison groups.
Types of outcome measures
Primary outcomes
Hot flush
Change in hot flushes (with or without night sweats): change in frequency or severity, evaluated subjectively by participants, using daily diaries, any validated objective scoring system, or other generic measures of vasomotor symptoms.
Secondary outcomes
Quality of life
Evaluated with any validated quality of life instrument (e.g. the Menopause‐Specific Quality of Life (Hilditch 1996), Women's Health Questionnaire (WHQ) (Hunter 1992), or other generic measures of quality of life.
Adverse events
All adverse events (e.g. needling pain, bleeding at the site of needling, trauma to internal organs).
Search methods for identification of studies
We searched for all published and unpublished RCTs of acupuncture for hot flushes, without language restriction and in consultation with the Menstrual Disorders and Subfertility Group (MDSG) Trials Search Co‐ordinator. Searches were first conducted in 2008 and then again in January 2013.
Electronic searches
We searched the Cochrane Menstrual Disorders and Subfertility Group Trials Register, the Cochrane Central Register of Controlled Trials (CENTRAL), PubMed, EMBASE, CINAHL, PsycINFO, Chinese Biomedical Literature Database (CBM), Chinese Medical Current Content (CMCC) (www.cmcc.org.cn), China National Knowledge Infrastructure (CNKI), VIP database, Dissertation Abstracts International, Current Controlled Trials (controlled‐trials.com), Clinicaltrials.gov (clinicaltrials.gov), National Center for Complementary and Alternative Medicine (NCCAM) (nccam.nih.gov/clinicaltrials/alltrials.htm), BIOSIS, AMED (The Allied and Complementary Medicine Database), Acubriefs, and Acubase (see the Appendix 1; Appendix 2; Appendix 3; Appendix 4; Appendix 5; Appendix 6; Appendix 7; and Appendix 8 for search strategies).
We searched the following clinical trial registries for ongoing trials:
Australian and New Zealand Clinical Registry (www.anzctr.org.au/);
Chinese Clinical Trial Register (www.chictr.org);
Current Controlled Trials (controlled‐trials.com);
Clinical trials.gov (clinicaltrials.gov);
ISRCTN (www.isrctn.org/);
NCCAM (nccam.nih.gov/clinicaltrials/alltrials.htm);
WHO International Clinical Trial Registration Platform search portal (www.who.int/trialsearch/).
Searching other resources
We handsearched relevant journals, conference abstracts, and the reference lists of studies identified.
Data collection and analysis
We conducted data collection and analysis in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Selection of studies
Three review authors (SD, GA, and CB) undertook trial selection. One review author (WT) searched the Chinese databases. GA and CB screened the titles and abstracts of articles found in the search and discarded trials that were clearly ineligible.
SD, GA, and CB independently assessed whether the trials met the inclusion criteria, with disagreements resolved by discussion. When articles contained insufficient information to make a decision about eligibility, CB attempted to contact authors of the original reports to obtain further details; if there was no response, CB sent a reminder.
Data extraction and management
Two review authors (GA and CB) independently extracted data using a form designed by the review authors for this purpose. We resolved discrepancies by discussion or in consultation with a third review author (SD). For each included trial, we collected information regarding the location of the trial, methods of the trial, risk of bias, participants (age range, eligibility criteria), type of interventions, and effect of interventions.
Assessment of risk of bias in included studies
Two review authors (CV and JP) independently assessed risk of bias using The Cochrane Collaboration's 'Risk of Bias' tool (Higgins 2011). We resolved any disagreements between review authors by discussion or with a third party. For each study, the seven domain‐based criteria were: random sequence generation, quality of allocation concealment, blinding of participants and personnel, blinding of outcome assessors, completeness of outcome data, risk of selective outcome reporting, and other potential bias. The review authors assessed each domain as at high, low, or unclear risk of bias. See Characteristics of included studies.
Measures of treatment effect
All data were continuous. If all studies reported exactly the same outcomes we calculated mean difference (MDs) between treatment groups. If similar outcomes were reported on different scales, we calculated the standardized mean difference (SMD). We presented 95% confidence intervals (CI) for all estimates.
Unit of analysis issues
We planned to use only first‐phase data from cross‐over studies, had any cross‐over studies been eligible.
Dealing with missing data
We analyzed the data on an intention‐to‐treat basis as far as possible and we attempted to obtain missing data from the original trialists. Where these were unobtainable, we analyzed only the available data.
Assessment of heterogeneity
We considered whether the clinical and methodological characteristics of the included studies were sufficiently similar for meta‐analysis to provide a clinically meaningful summary.
We examined heterogeneity between the results of different trials informally by the overlap in their CIs. Poor overlap generally indicates the presence of statistical heterogeneity. In additon, more formally, we employed the results of the Chi2 test to determine the strength of evidence that heterogeneity was genuine. A low P value (or a large Chi2 statistic relative to the degree of freedom) suggests heterogeneity of effects (variation in effect estimates beyond chance).
An I2 statistic was also calculated and interpreted as:
0% to 40% might not be important;
30% to 60% represents moderate heterogeneity;
50% to 90%, represents substantial heterogeneity;
75% to 100%, represents considerable heterogeneity (Higgins 2011).
Assessment of reporting biases
In view of the difficulty of detecting and correcting for publication bias and other reporting biases, the review authors aimed to minimize the potential impact of reporting bias by ensuring a comprehensive search for eligible studies and by being alert for duplication of data.
Data synthesis
We combined data from included studies using random‐effects models in the following comparisons:
acupuncture versus sham‐acupuncture;
acupuncture versus HT;
electroacupuncture versus relaxation;
acupuncture versus waitlist or no intervention.
We stratified analyses by type of acupuncture.
Subgroup analysis and investigation of heterogeneity
We performed subgroup analyses for the primary outcome to determine the separate evidence for:
acupuncture in cancer trials;
acupuncture in trial less of 12 weeks duration;
acupuncture in trial of 12 weeks and more.
Sensitivity analysis
We conducted sensitivity analyses for the primary outcome, to investigate the impact of:
restricting eligibility to studies without high risk of bias;
adopting a fixed‐effect model.
Overall quality of the body of evidence: 'Summary of findings' table
Summary of findings tables were generated using GRADEPRO software. These tables evaluated the overall quality of the body of evidence for primary review outcomes for comparisons of acupuncture versus sham acupuncture, using GRADE criteria (study limitations (i.e. risk of bias), consistency of effect, imprecision, indirectness, and publication bias).
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
We identified and screened 384 references. We excluded 322 references based on the title and abstract, and retrieved 62 references for more detailed evaluation. From these, we excluded 46 publications, and included 16 publications (Figure 1).
1.
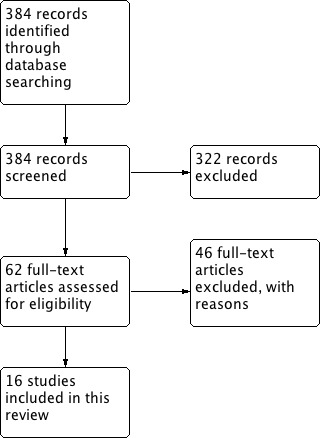
Study flow diagram.
Included studies
Sixteen RCTs with 1155 participants met the inclusion criteria. Ten studies compared acupuncture versus sham acupuncture (Avis 2008; Bokmand 2013; Deng 2007; Hervik 2009; Kim 2011; Nir 2007; Painovich 2012; Venzke 2010; Vincent 2007; Wyon 2004). Two RCTs compared acupuncture versus HT (Frisk 2008; Zhou 2011). One RCT compared acupuncture versus relaxation (Nedstrand 2006). Five RCTs compared acupuncture versus wait list or no intervention (Bokmand 2013; Borud 2009; Kim 2010; Painovich 2012; Park 2009). We presented full descriptions of the studies in the Characteristics of included studies table.
Study design
All of the trials were parallel‐group RCTs.
Trials took place in China (Zhou 2011), Korea (Kim 2010; Kim 2011; Park 2009), Norway (Borud 2009; Hervik 2009), Sweden (Frisk 2008; Nedstrand 2006; Wyon 2004), Denmark (Bokmand 2013), and the US (Avis 2008; Deng 2007; Nir 2007; Painovich 2012; Venzke 2010; Vincent 2007). Five of the studies were multicentred Avis 2008; Borud 2009; Frisk 2008; Kim 2010; (Nedstrand 2006).
Only four studies reported the use of intention‐to‐treat analysis Borud 2009; Kim 2010; Kim 2011; (Vincent 2007). Five studies reported use of power calculations for estimating their sample size (Bokmand 2013; Borud 2009; Deng 2007; Kim 2011; Vincent 2007).
Participants
The range of mean participant age was 51 to 57 years. In seven studies, participants were recruited through newspaper advertisements (Borud 2009; Kim 2011; Nir 2007; Park 2009; Venzke 2010; Wyon 2004; Zhou 2011); in one study they were recruited through local newspaper advertisements, hospital posting, and notifications in the community meeting (Kim 2010); in seven studies via cancer centres or clinic centres (Avis 2008; Bokmand 2013; Deng 2007; Frisk 2008; Hervik 2009; Nedstrand 2006; Vincent 2007), and in one study by mailing advertisements near the medical centre and via the medical centre intranet (Painovich 2012).
All studies included perimenopausal or postmenopausal women, or both. Six studies used follicle‐stimulating hormone or serum oestradiol levels (or both) for confirming the menopausal status of participants (Borud 2009; Kim 2010; Nir 2007; Park 2009; Venzke 2010; Wyon 2004). Six studies determined menopausal status by self reported levels of hot flushes (Avis 2008; Hervik 2009; Kim 2011; Nedstrand 2006; Painovich 2012; Vincent 2007). Three studies did not state how menopausal status was determined (Bokmand 2013; Deng 2007; Frisk 2008). One study included women who had received a bilateral ovariectomy (Zhou 2011).
All women had vasomotor symptoms at baseline. Seven studies did not specify a minimum number of hot flushes as an inclusion criterion (Bokmand 2013; Frisk 2008; Hervik 2009; Kim 2011; Nedstrand 2006; Wyon 2004; Zhou 2011). Other studies required had 3 to 15 hot flushes daily as an inclusion criterion.
Only one study did not report the demographic characteristics of participants at baseline (Nedstrand 2006). In all others, the study groups were well balanced and no significant differences in demographic characteristics were reported at baseline.
Five trials enrolled women with breast cancer who had previously completed their treatment and experienced hot flushes (Bokmand 2013; Deng 2007; Frisk 2008; Hervik 2009; Nedstrand 2006). In one study, women were treated with the oestrogen antagonist, tamoxifen (Hervik 2009).
Interventions
The duration of acupuncture treatment varied considerably between studies. It ranged from four to five weeks (Bokmand 2013; Deng 2007; Kim 2010; Park 2009; Vincent 2007), seven to eight weeks (Avis 2008; Kim 2011; Nir 2007), 10 weeks (Hervik 2009; Vincent 2007), and 12 weeks (Borud 2009; Frisk 2008; Nedstrand 2006; Painovich 2012; Venzke 2010; Zhou 2011).
Traditional acupuncture was performed in 11 trials (Avis 2008; Bokmand 2013; Borud 2009; Deng 2007; Hervik 2009; Kim 2010; Kim 2011; Nir 2007; Painovich 2012; Venzke 2010; Vincent 2007), electroacupuncture in three trials (Frisk 2008; Nedstrand 2006; Wyon 2004), acupuncture and auricular acupressure (Zhou 2011), and moxibustion in one trial (Park 2009). The acupuncture points used differed across studies. In three trials, the acupuncturists administered individualized acupuncture treatment for each participant (Borud 2009; Nir 2007; Venzke 2010) and 13 trials used a standardized formula with the number of acupuncture points selected ranging from 4 to 13 points (Avis 2008; Bokmand 2013; Deng 2007; Frisk 2008; Hervik 2009; Kim 2010; Kim 2011; Painovich 2012; Nedstrand 2006; Park 2009; Vincent 2007; Wyon 2004; Zhou 2011).
All trials provided data on compliance with the intervention(s).
Outcomes
Vasomotor symptoms
All studies assessed vasomotor symptoms by self report. Five assessed only vasomotor symptoms such as hot flush frequency and severity ( Avis 2008; Deng 2007; Kim 2011; Vincent 2007;Zhou 2011). Climacteric symptoms were assessed by the Menopause Rating Scale (MRS) (Kim 2010; Kim 2011), WHQ (Borud 2009), Greene Climateric Scale (Venzke 2010), Modified Kupperman's Index (Frisk 2008; Hervik 2009; Nedstrand 2006; Wyon 2004), visual analogue scale (VAS) (Bokmand 2013; Nedstrand 2006; Park 2009; Wyon 2004), and Hot Flash Related Daily Interference Scale (HFRDIS) (Avis 2008).
The diary of vasomotor symptoms was the most commonly used tool to quantify hot flush frequency and severity. For all RCTs, the frequency of hot flushes was based on the number of hot flushes recorded by day. Few authors calculated a mean daily hot flush score from seven days of values. More recent studies evaluated the mean reduction in average 24‐hour hot flush frequency and severity from baseline to the end of the study. The different hot flush severity scores used and results of frequency and severity recalls by women complicated the comparison among trials in regards of the severity results. Severity was evaluated according to different rating scales ranging from 1 to 3 (mild to severe symptoms), 1 to 4 (mild to very severe symptoms), by VAS of 1 to 10, and according to log transformation of the severity scores obtained.
Quality of life
Quality of life was assessed in three studies, which used the Menopausal‐Specific Quality of Life Scale (MENQoL) (Nir 2007; Park 2009; Painovich 2012).
Excluded studies
We excluded 46 trials (see Characteristics of excluded studies). The most common reason for exclusion was that participants did not meet the inclusion criteria for the intervention studies; for example, qualitative and observational research, case history and abstract of annual meeting with no further scientific publication of their results (Mingling 1991; Ji 1998; Towlerton 1999; Gui‐e 2000; Cummins 2000; Tukmachi 2000; Zhenya 2001; De Valois 2003; Xu 2004; Hu 2005; Perez 2005; Xiaoming 2005; Zhou 2006; Walker 2007; Huazhang 2008; Walker 2008; Guévin 2009; Hervik 2010; Borud 2010; De Valois 2010; Otte 2011; Castelo Branco 2011; Azizi 2011; Spetz Holm 2012; Kao 2012; Lesi 2012). We excluded eight studies due to insufficient data information related to vasomotor symptoms in order to meet the review inclusion criteria (Wyon 1995; Cohen 2003; Huo 2004; Li 2005; Jin 2007; Xia 2008; O'Brien 2010; Walker 2010). One study did not assess hot flushes outcome in their psychological distress study (Sandberg 2002). Two studies assessed only acupuncture techniques (Facchinetti 1989; Grilli 1989). Four studies were a duplicate of an included trial (Nedstrand 2005; Huang 2006; Zaborowska 2007; Frisk 2012). We excluded five studies because they were not randomized (Davies 2001; Harris 2002; Porzio 2002; Zhang 2006; Sunay 2011).
Risk of bias in included studies
For further details, see the methodological quality summary (Figure 2) and methodological quality graph (Figure 3).
2.
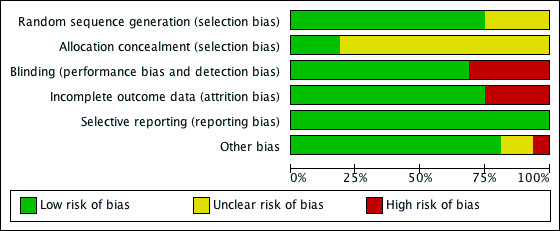
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.
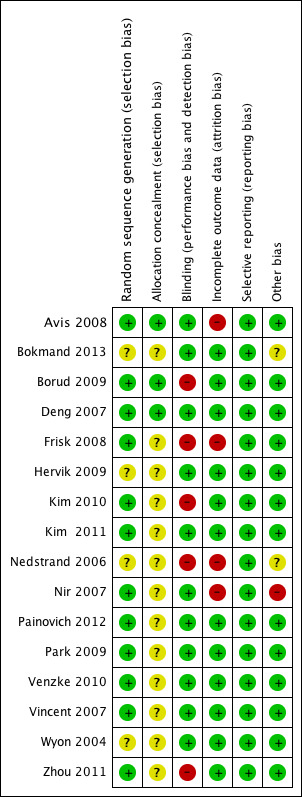
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
Generation of random sequence
We rated 12 studies as at low risk of bias related to sequence generation; these studies used computer‐generated randomization, randomization tables, or fully‐described drawing of lots. We rated the other four studies as at unclear risk of this bias.
Allocation concealment
We rated three studies as at low risk of bias related to allocation concealment; these studies used remote allocation. We rated the other 13 studies as at unclear risk of bias because they did not describe an acceptable method of allocation concealment; this included several studies that used envelopes for allocation concealment but did not state whether the envelopes were sealed, opaque and sequentially numbered.
Blinding
As our primary review outcome was self assessed, we considered that lack of participant blinding could influence outcome measures. We rated 11 studies as at low risk of bias because participants (at least) were blinded. We rated five as at high risk of bias because participants were not blinded.
Incomplete outcome data
We assessed 12 of the 16 studies as at low risk of attrition bias. We considered four studies to be at high risk of attrition bias due to high dropout rates.
Selective reporting
We evaluated each study for the possible risk of selective reporting bias. We considered all studies to have a low risk of selective reporting bias.
Other potential sources of bias
We considered 13 of the studies to be free of other potential sources of bias. One study was at unclear risk of bias due to lack of information about the baseline characteristics of participants (Nedstrand 2006), one study was at high risk due to reported differences in the baseline characteristics of the two groups of women (Nir 2007), and one was at unclear risk because during the project period some women received another type of treatment (which had no effect on the acupuncture according to the authors) (Bokmand 2013).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
1. Acupuncture versus sham acupuncture
Primary outcome
Hot flushes
Eight studies compared traditional acupuncture (Avis 2008; Deng 2007; Hervik 2009; Kim 2011; Nir 2007; Vincent 2007) or electroacupuncture (Wyon 2004) versus sham acupuncture, and reported hot flush frequency or severity.
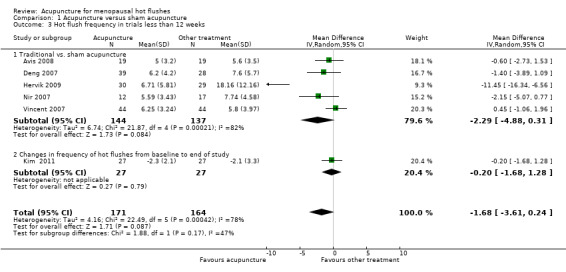
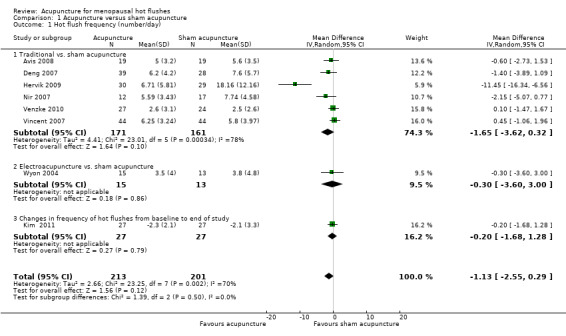
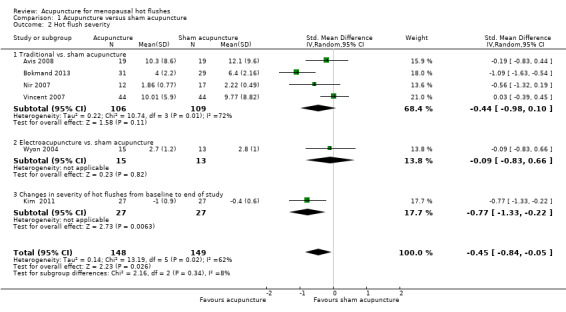
No significant difference was found between the groups for hot flush frequency (MD ‐1.13 flushes per day, 95% CI ‐2.55 to 0.29, 8 RCTs, 414 women, I2 = 70%) (Figure 4), but flushes were significantly less severe in the acupuncture group, with a small effect size (SMD ‐0.45, 95% CI ‐0.84 to ‐0.05, 6 RCTs, 297 women, I2 = 62%) (Figure 5).
4.
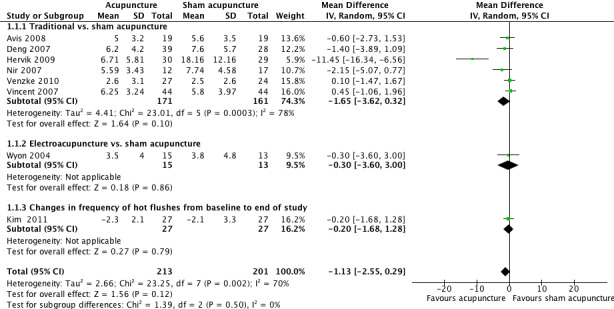
Forest plot of comparison: 1 Acupuncture versus sham acupuncture, outcome: 1.1 Hot flush frequency (number/day).
5.
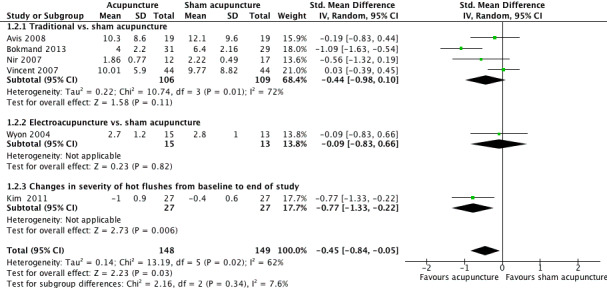
Forest plot of comparison: 1 Acupuncture versus sham acupuncture, outcome: 1.2 Hot flush severity.
There was substantial heterogeneity for both these outcomes. We considered clinical and methodological differences between the studies that might explain the heterogeneity and noted that a post‐hoc analysis excluding studies of women with cancer eliminated heterogeneity for hot flush frequency (MD 0.15 flushes per day, 95% CI 0.61 to 0.91, 6 studies, 188 women, I2 = 0%) and reduced heterogeneity for the analysis of hot flush severity (MD ‐0.29, 95% CI ‐0.62 to 0.04, 5 studies, 237 women, I2 = 34%). There was no longer a significant difference between the groups for hot flush severity when we excluded the single study of women with cancer.
No significant difference was found between the groups in subgroup or sensitivity analysis of hot flush frequency (Analysis 1.3; Analysis 1.4; Analysis 1.5; Analysis 1.8), but acupuncture significantly reduced hot flush severity compared to sham acupuncture in a study of women with cancer (Analysis 1.6) and in studies of less than 12 weeks' duration (Analysis 1.7).
1.3. Analysis.
Comparison 1 Acupuncture versus sham acupuncture, Outcome 3 Hot flush frequency in trials less than 12 weeks.
1.4. Analysis.

Comparison 1 Acupuncture versus sham acupuncture, Outcome 4 Hot flush frequency in trials of 12 weeks and more.
1.5. Analysis.
Comparison 1 Acupuncture versus sham acupuncture, Outcome 5 Hot flush frequency in cancer trials.
1.8. Analysis.
Comparison 1 Acupuncture versus sham acupuncture, Outcome 8 Hot flush severity in trials of 12 weeks and more.
1.6. Analysis.
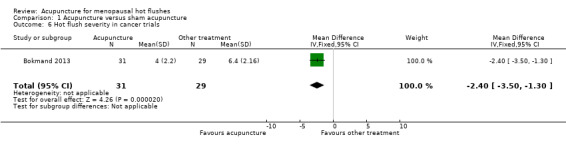
Comparison 1 Acupuncture versus sham acupuncture, Outcome 6 Hot flush severity in cancer trials.
1.7. Analysis.
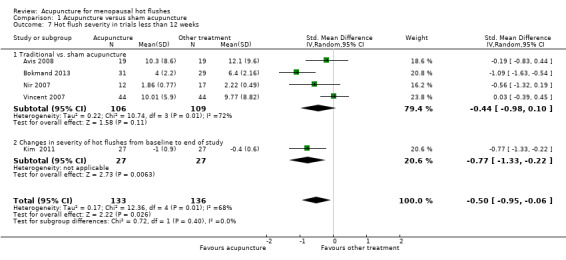
Comparison 1 Acupuncture versus sham acupuncture, Outcome 7 Hot flush severity in trials less than 12 weeks.
Secondary outcomes
Quality of life
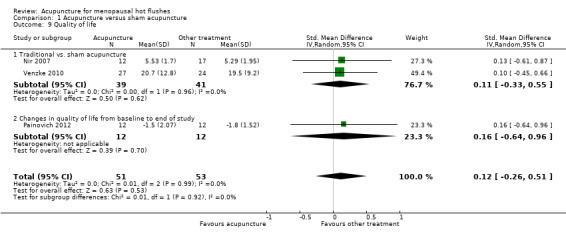
Two studies compared traditional acupuncture versus sham acupuncture and reported quality of life. No significant difference was found between the groups (SMD 0.11, 95% CI ‐0.33 to 0.55, 2 RCTs, 80 women, I2 = 0%) (Analysis 1.9).
1.9. Analysis.
Comparison 1 Acupuncture versus sham acupuncture, Outcome 9 Quality of life.
No significant difference was found between the groups for any of subgroup analyses (Analysis 1.10; Analysis 1.11).
1.10. Analysis.
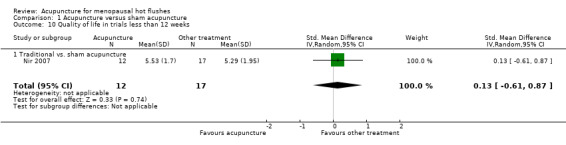
Comparison 1 Acupuncture versus sham acupuncture, Outcome 10 Quality of life in trials less than 12 weeks.
1.11. Analysis.
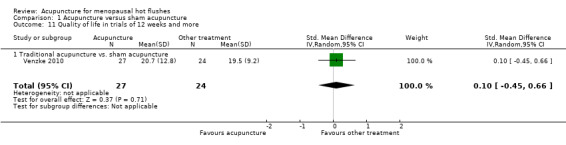
Comparison 1 Acupuncture versus sham acupuncture, Outcome 11 Quality of life in trials of 12 weeks and more.
Adverse events
Three studies reported no adverse events (Venzke 2010; Vincent 2007; Wyon 2004), and three noted some minor adverse effects, such as slight bruising at the needle site (Deng 2007; Kim 2011; Nir 2007). Three trials did not report this outcome (Avis 2008; Hervik 2009; Painovich 2012).
2. Acupuncture versus hormone therapy
Primary outcome
Hot flushes
Three studies compared electroacupuncture (Frisk 2008; Wyon 2004), or acupuncture plus auricular acupressure (Zhou 2011), versus HT and reported hot flush frequency or severity. When these studies were pooled, acupuncture was associated with significantly more hot flushes per day than HT (MD 3.18 flushes per day, 95% CI 2.06 to 4.29, 3 RCTs, 114 women, I2 = 0%) (Figure 6). No significant difference was found between the groups for hot flush severity (SMD 0.53, 95% CI ‐0.14 to 1.20, 2 RCTs, 84 women, I2 = 57%) (Figure 7). There was moderate heterogeneity for hot flush severity: the study of electroacupuncture found a significant difference between the groups (Frisk 2008), while the study of acupuncture plus auricular acupressure found no significant difference (Zhou 2011).
6.
Forest plot of comparison: 2 Acupuncture versus hormone therapy, outcome: 2.1 Hot flush frequency (number/day).
7.
Forest plot of comparison: 2 Acupuncture versus hormone therapy, outcome: 2.2 Hot flush severity.
Subgroup and sensitivity analyses did not affect the main findings (Analysis 2.3).
2.3. Analysis.

Comparison 2 Acupuncture versus hormone therapy, Outcome 3 Hot flush severity in cancer trials.
Secondary outcomes
Quality of life
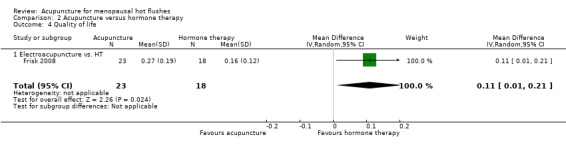
One study compared electroacupuncture versus HT and reported quality of life (Frisk 2008). Quality of life was significantly higher in the HT group (MD 0.11, 95% CI 0.01 to 0.21, 1 RCT, 41 women) (Analysis 2.4).
2.4. Analysis.
Comparison 2 Acupuncture versus hormone therapy, Outcome 4 Quality of life.
Adverse events
No serious adverse events were reported in the two studies.
3. Acupuncture versus relaxation
Primary outcome
Hot flushes
One study compared electroacupuncture versus relaxation and reported hot flush frequency and severity (Nedstrand 2006). There was no significant difference between the groups for either hot flush frequency (MD ‐0.40 flushes per day, 95% CI ‐2.18 to 1.38, 1 RCT, 38 women) (Analysis 3.1) or hot flush severity (MD 0.20, 95% CI ‐0.85 to 1.25, 1 RCT, 38 women) (Analysis 3.3).
3.1. Analysis.
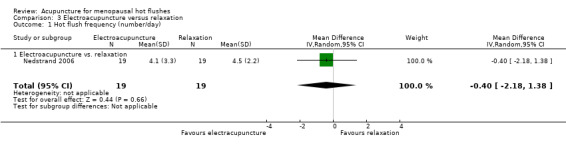
Comparison 3 Electroacupuncture versus relaxation, Outcome 1 Hot flush frequency (number/day).
3.3. Analysis.
Comparison 3 Electroacupuncture versus relaxation, Outcome 3 Hot flush severity.
Secondary outcomes
Quality of life
One study compared electroacupuncture versus relaxation and reported quality of life (Nedstrand 2006). There was no significant difference between the groups (MD 8.30, 95% CI ‐4.23 to 20.83, 1 RCT, 38 women) (Analysis 3.4).
3.4. Analysis.
Comparison 3 Electroacupuncture versus relaxation, Outcome 4 Quality of life.
Adverse events
No adverse events were mentioned in the study.
4. Acupuncture versus wait list or no intervention
Primary outcome
Hot flushes
Four studies compared traditional acupuncture (Borud 2009; Kim 2010; Painovich 2012), or moxibustion (Park 2009), versus wait list or no intervention and reported hot flush frequency or severity.
Traditional acupuncture was significantly more effective than wait list or no intervention in reducing hot flush frequency from baseline (SMD ‐0.50, 95 CI ‐0.69 to ‐0.31, 3 RCTs, 463 women, I2 = 0%) (Analysis 4.1). The effect size was moderate. Moxibustion was significantly more effective than wait list or no intervention in reducing the number of hot flushes per week (MD ‐5.27, 95% CI ‐8.06 to ‐2.48, 1 RCT, 28 women) (Analysis 4.2).
4.1. Analysis.

Comparison 4 Acupuncture versus waiting list or no intervention, Outcome 1 Change in frequency of hot flushes from baseline to end of study.
4.2. Analysis.
Comparison 4 Acupuncture versus waiting list or no intervention, Outcome 2 Hot flush frequency.
Traditional acupuncture was significantly more effective than wait list or no intervention in reducing hot flush severity from baseline (SMD ‐0.54, 95% CI ‐0.73 to ‐ 0.35, 3 RCTs, 463 women, I2 = 0%) (Analysis 4.3). The effect size was moderate. Similarly, acupuncture and moxibustion were significantly more effective than wait list or no intervention in reducing hot flush severity (SMD ‐1.35, 95% CI ‐1.81 to ‐0.89, 2 RCTs, 93 women, I2 = 0%) (Analysis 4.4).
4.3. Analysis.

Comparison 4 Acupuncture versus waiting list or no intervention, Outcome 3 Change in hot flush severity from baseline to end of study.
4.4. Analysis.
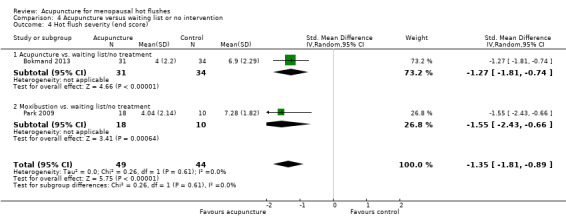
Comparison 4 Acupuncture versus waiting list or no intervention, Outcome 4 Hot flush severity (end score).
Subgroup and sensitivity analyses did not affect the main findings.
Secondary outcomes
Quality of life
Four studies compared traditional acupuncture (Borud 2009; Kim 2010; Painovich 2012), or moxibustion (Park 2009), versus wait list or no intervention and reported quality of life.
Traditional acupuncture improved quality of life from baseline significantly more than wait list or no intervention (SMD ‐0.93, 95% CI ‐1.20 to ‐0.67, 3 RCTs, 463 women, I2 = 32%) (Analysis 4.5). There was no significant difference between the moxibustion and controls groups for quality of life (MD ‐0.46, 95% CI ‐5.98 to 5.06, 1 RCT, 30 women) (Analysis 4.6).
4.5. Analysis.
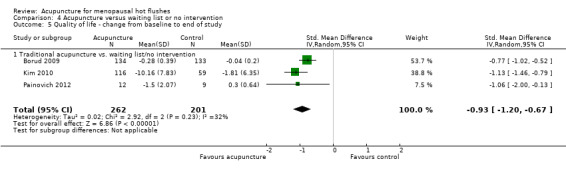
Comparison 4 Acupuncture versus waiting list or no intervention, Outcome 5 Quality of life ‐ change from baseline to end of study.
4.6. Analysis.

Comparison 4 Acupuncture versus waiting list or no intervention, Outcome 6 Quality of life (end score).
Adverse events
Two studies reported mild side effects, including skin burns related to moxibustion and bruising around the needle site (Park 2009; Kim 2010). One trial reported no adverse effects (Borud 2009), and one did not report adverse effects (Painovich 2012).
Discussion
Summary of main results
This review assessed the effectiveness of acupuncture on vasomotor symptoms in RCTs.
Studies that compared acupuncture versus sham acupuncture did not provide sufficient evidence to show whether acupuncture is an effective treatment for vasomotor symptoms. It is debatable as to whether sham acupuncture is a suitable placebo intervention due to the possibility that sham acupuncture has an active effect related to peripheral sensory stimulation.
Three small studies comparing acupuncture with HT indicated that HT was superior to acupuncture for reducing the frequency of hot flushes.
One small study compared acupuncture with relaxation and showed no significant difference between the groups.
However, comparisons of acupuncture with wait list or no treatment or control groups indicated that acupuncture reduced the frequency and severity of hot flushes from baseline to end of study and also improved quality of life.
Currently there is insufficient evidence to determine whether acupuncture is effective as a treatment for hot flushes, as there are still few studies comparing acupuncture to other treatments and the quality of some of the studies is poor. Further high‐quality studies are needed to determine the effect of acupuncture on vasomotor symptoms.
Overall completeness and applicability of evidence
Most of the included studies reported hot flush frequency, hot flush severity and quality of life, but data on adverse events were poorly reported or lacking.
Interventions were usually well described but were of limited applicability as they often used protocols requiring the acupuncturist to select acupuncture points during the intervention, based on their past experience.
There was some indication that effects may differ in studies of women with cancer, but this was unclear.
Quality of the evidence
The 16 studies included in this systematic review were published from 2004 to 2012. This suggests that acupuncture has been the subject of more studies in the last decade than previously. However, most had small sample sizes and questionable methodological quality. Many had an inadequate level of blinding and no intention‐to‐treat analysis. Meta‐analyses were generally underpowered and there was moderate‐to‐high heterogeneity in some cases. We graded the overall quality of the evidence for the primary outcomes as low to very low, using GRADE criteria (Table 1; Table 2; Table 3; Table 4). There was some indication that effects may differ in studies of women with cancer, but this was unclear.
Potential biases in the review process
This review was limited by methodological heterogeneity between the included studies, which used a variety of measures for hot flush frequency and severity. This meant that we were unable to pool some of the data. In most cases, we had no access to the original data, and some studies reported their results in tabular form. Many primary study authors failed to respond to our requests for missing data.
A strength of the review was that we made strong efforts to retrieve all RCTs on acupuncture.
Agreements and disagreements with other studies or reviews
Our results and those presented in recent reviews support our conclusion that there is currently insufficient randomized evidence to show whether acupuncture is an effective treatment for menopausal hot flushes and that further evaluation of the effects of acupuncture on vasomotor symptoms in placebo‐controlled trials is justified.
Authors' conclusions
Implications for practice.
We found insufficient evidence to determine whether acupuncture is an effective treatment for controlling vasomotor menopausal symptoms. When we compared acupuncture with sham acupuncture, there was no evidence of any significant difference in their effect on menopausal vasomotor symptoms. When we compared acupuncture with no treatment there appeared to be a benefit from acupuncture, but acupuncture appeared to be less effective than hormone therapy (HT). These findings should be treated with great caution as the evidence was of low or very low quality and the studies comparing acupuncture versus no treatment or HT were not controlled with sham acupuncture or placebo HT. Data on adverse effects were lacking.
Implications for research.
More large randomized controlled trials (RCTs) on acupuncture versus placebo control or other types of intervention are required, and should investigate whether effects differ in women with cancer. Future RCTs should use standardized protocols and outcome measures to enable comparison across studies.
What's new
| Date | Event | Description |
|---|---|---|
| 31 July 2013 | Amended | Additional author Elizabeth Maunsell added |
History
Protocol first published: Issue 4, 2008 Review first published: Issue 7, 2013
| Date | Event | Description |
|---|---|---|
| 14 April 2008 | New citation required and major changes | Substantive amendment |
Acknowledgements
We are grateful for the help of Carole Thiébaut for conducting the electronic searches and to Geneviève Asselin, a research assistant, who performed the selection of the included articles. We also acknowledge the assistance of the Menstrual Disorders and Subfertility Review Group editorial team.
Appendices
Appendix 1. Menstrual Disorders and Subfertility Group keywords search
MSDG Search XH941 15 Jan 2013
Keywords CONTAINS "acupoint" or "acupressure" or "acupressure‐acupuncture therapy" or "acupuncture" or "electro‐acupuncture" or "electroacupuncture" or "moxibustion" or "ear electroacupuncture" or "ear point pressing" or "ear point tapping" or Title CONTAINS "acupoint" or "acupressure" or "acupressure‐acupuncture therapy" or "acupuncture" or "electro‐acupuncture" or "electroacupuncture" or "moxibustion" or "ear electroacupuncture" or "ear point pressing" or "ear point tapping"
AND
Keywords CONTAINS "climacteric " or "climacteric depression" or "climacteric symptoms" or "climacteric symptoms‐outcome" or "climacteric symptoms ‐ vasomotor" or "climacteric symptoms" or "climacteric symptoms ‐ urogenital" or "climacteric symptoms‐psychological" or "menopausal symptoms" or "menopausal symptoms" or "Menopause" or "menopause‐surgical" or "menopausal transition" or "vasomotor", "vasomotor symptoms" or "vasomotor symptoms" or Title CONTAINS "climacteric " or "climacteric depression" or "climacteric symptoms" or "climacteric symptoms‐outcome" or "climacteric symptoms ‐ vasomotor" or "climacteric symptoms" or "climacteric symptoms ‐ urogenital" or "climacteric symptoms‐psychological" or "menopausal symptoms" or "menopausal symptoms" or "Menopause" or "menopause‐surgical" or "menopausal transition" or "vasomotor", "vasomotor symptoms" or "vasomotor symptoms"
Appendix 2. EMBASE search
1 exp "menopause and climacterium"/ or exp climacterium/ or exp early menopause/ or exp menopause/ or exp postmenopause/ or exp premenopause/ (78,582) 2 exp Menopause Related Disorder/ (18,824) 3 (surgical adj3 menopaus$).tw. (889) 4 (climacter$ or menopaus$).tw. (47,547) 5 (premenopaus$ or perimenopaus$).tw. (19,567) 6 post*menopaus$.tw. (48,978) 7 exp anovulation/ or exp premature ovarian failure/ (5772) 8 or/1‐7 (120,987) 9 exp acupuncture/ or exp electroacupuncture/ or exp acupressure/ or exp shiatsu/ or exp tui na/ (28,296) 10 acupuncture.tw. (18,348) 11 (shiatsu or tui na).tw. (100) 12 (acupressure$ or electroacupunctur$).tw. (3374) 13 (meridian$ or moxi$).tw. (9682) 14 exp moxibustion/ (1211) 15 acup$ point$.tw. (1726) 16 or/9‐15 (37,056) 17 8 and 16 (490) 18 Clinical Trial/ (875,392) 19 Randomized Controlled Trial/ (334,840) 20 exp randomization/ (60,305) 21 Single Blind Procedure/ (16,822) 22 Double Blind Procedure/ (112,519) 23 Crossover Procedure/ (35,869) 24 Placebo/ (211,086) 25 Randomi?ed controlled trial$.tw. (82,375) 26 Rct.tw. (10,694) 27 random allocation.tw. (1197) 28 randomly allocated.tw. (18,120) 29 allocated randomly.tw. (1854) 30 (allocated adj2 random).tw. (714) 31 Single blind$.tw. (12,916) 32 Double blind$.tw. (133,133) 33 ((treble or triple) adj blind$).tw. (296) 34 placebo$.tw. (183,316) 35 prospective study/ (222,307) 36 or/18‐35 (1,298,972) 37 case study/ (18,200) 38 case report.tw. (236,726) 39 abstract report/ or letter/ (854,525) 40 or/37‐39 (1,104,568) 41 36 not 40 (1,263,189) 42 17 and 41 (222) 43 2012$.em. (1,289,170) 44 42 and 43 (23)
Appendix 3. PsycINFO
1 exp menopause/ (2728) 2 (climacter$ or menopaus$).tw. (3664) 3 (premenopaus$ or perimenopaus$).tw. (1081) 4 postmenopaus$.tw. (1804) 5 or/1‐4 (5169) 6 exp acupuncture/ (1022) 7 acupuncture.tw. (1385) 8 acupressure$.tw. (97) 9 electroacupuncture.tw. (188) 10 (meridian$ or moxi$).tw. (695) 11 Acupuncture Point$.tw. (101) 12 acup$ point$.tw. (110) 13 or/6‐12 (2196) 14 5 and 13 (16) 15 limit 14 to yr="2012 ‐Current" (1)
Appendix 4. AMED search
1 exp climacteric/ or exp menopause/ (504) 2 exp postmenopause/ (36) 3 (climacter$ or menopaus$).tw. (687) 4 (premenopaus$ or perimenopaus$).tw. (103) 5 post*menopaus$.tw. (379) 6 exp amenorrhea/ (34) 7 (ovar$ adj3 fail$).tw. (6) 8 or/1‐7 (950) 9 exp acupuncture/ (3191) 10 acupuncture.tw. (8654) 11 exp acupuncture therapy/ or exp acupoints/ or exp neiguan/ or exp acupressure/ or exp acupuncture analgesia/ or exp ear acupuncture/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/ or exp needling/ or exp scalp acupuncture/ (6584) 12 acupressure$.tw. (337) 13 electroacupuncture.tw. (847) 14 (meridian$ or moxi$).tw. (1092) 15 acupoint$.tw. (1696) 16 needling.tw. (726) 17 or/9‐16 (9591) 18 8 and 17 (72) 19 limit 18 to yr="2012 ‐Current" (1)
Appendix 5. CENTRAL search
1 exp climacteric/ or exp menopause/ or exp menopause, premature/ or exp perimenopause/ or exp postmenopause/ or exp premenopause/ (5209) 2 (surgical adj3 menopaus$).tw. (94) 3 (climacter$ or menopaus$).tw. (3977) 4 (premenopaus$ or perimenopaus$).tw. (2031) 5 post*menopaus$.tw. (7511) 6 exp anovulation/ or exp menopause, premature/ or exp ovarian failure, premature/ (185) 7 (ovar$ adj3 fail$).tw. (143) 8 or/1‐7 (11,761) 9 exp Acupuncture/ (106) 10 acupuncture.tw. (4327) 11 exp acupuncture therapy/ or exp acupressure/ or exp acupuncture, ear/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/ (2301) 12 acupressure$.tw. (259) 13 electroacupuncture.tw. (481) 14 (meridian$ or moxi$).tw. (1167) 15 exp Acupuncture Points/ (836) 16 acup$ point$.tw. (436) 17 or/9‐16 (5918) 18 8 and 17 (82) 19 limit 18 to yr="2012 ‐Current" (2)
Appendix 6. MEDLINE
1 exp climacteric/ or exp menopause/ or exp menopause, premature/ or exp perimenopause/ or exp postmenopause/ or exp premenopause/ (45,986) 2 (surgical adj3 menopaus$).tw. (650) 3 (climacter$ or menopaus$).tw. (35,372) 4 (premenopaus$ or perimenopaus$).tw. (15,613) 5 post*menopaus$.tw. (37,791) 6 exp anovulation/ or exp menopause, premature/ or exp ovarian failure, premature/ (4033) 7 (ovar$ adj3 fail$).tw. (3007) 8 or/1‐7 (85,165) 9 exp Acupuncture/ (1102) 10 acupuncture.tw. (13,101) 11 exp acupuncture therapy/ or exp acupressure/ or exp acupuncture, ear/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/ (15,238) 12 acupressure$.tw. (500) 13 electroacupuncture.tw. (2237) 14 (meridian$ or moxi$).tw. (7810) 15 exp Acupuncture Points/ (3325) 16 acup$ point$.tw. (1089) 17 or/9‐16 (24,584) 18 8 and 17 (206) 19 randomized controlled trial.pt. (337,979) 20 controlled clinical trial.pt. (84,988) 21 randomized.ab. (255,104) 22 placebo.tw. (143,633) 23 clinical trials as topic.sh. (161,830) 24 randomly.ab. (186,796) 25 trial.ti. (108,840) 26 (crossover or cross‐over or cross over).tw. (55,103) 27 or/19‐26 (830,147) 28 (animals not (humans and animals)).sh. (3,656,512) 29 27 not 28 (765,528) 30 18 and 29 (97) 31 2012$.ed. (1,039,918) 32 30 and 31 (14)
Appendix 7. PubMed search
1 "acupuncture"[MeSH Terms] OR ("acupuncture therapy"[TIAB] NOT Medline[SB]) OR "acupuncture therapy"[MeSH Terms] OR Acupunctur*[Text Word] 2 "electroacupuncture"[MeSH Terms] OR electroacupuncture[Text Word] 3 ("acupuncture points"[TIAB] NOT Medline[SB]) OR "acupuncture points"[MeSH Terms] OR Acupoints[Text Word] 4 "acupressure"[MeSH Terms] OR acupressure[Text Word] 5 "meridians"[MeSH Terms] OR meridians[Text Word] 6 "moxibustion"[MeSH Terms] OR moxibustion[Text Word] 7 1 OR 2 OR 3 OR 4 OR 5 OR 6 8 ("menopause"[TIAB] NOT Medline[SB]) OR "menopause"[MeSH Terms] OR menopausal[Text Word] OR menopause[Text Word] 9 ("hot flashes"[MeSH Terms] OR hot flashes[Text Word]) OR (("hot flashes"[TIAB] NOT Medline[SB]) OR hot flushes[Text Word]) OR hot flush[Text Word] OR hot flash[Text Word] OR ("flushing"[MeSH Terms] OR flushing[Text Word]) OR "night sweats"[All Fields] 10 "premature ovarian failure"[Text Word] OR "ovarian failure, premature"[MeSH Terms] OR ovarian failure[Text Word] 11 "perimenopause"[MeSH Terms] OR perimenopause[Text Word] OR peri‐menopause[All Fields] 12 "postmenopause"[MeSH Terms] OR postmenopause[Text Word] ("postmenopause"[TIAB] NOT Medline[SB]) OR post‐menopause[Text Word] 13 vasomotor disorder[All Fields] OR vasomotor disorders[All Fields] 14 "climacteric"[MeSH Terms] OR climacteric[Text Word] 15 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 16 7 AND 15
Appendix 8. CINAHL
1 exp climacteric/ or exp menopause/ or exp menopause, premature/ or exp perimenopause/ or exp postmenopause/ or exp premenopause/ (6152) 2 (surgical adj3 menopaus$).tw. (76) 3 (climacter$ or menopaus$).tw. (3447) 4 (premenopaus$ or perimenopaus$).tw. (1238) 5 post*menopaus$.tw. (3331) 6 exp anovulation/ or exp menopause, premature/ or exp ovarian failure, premature/ (156) 7 (ovar$ adj3 fail$).tw. (96) 8 or/1‐7 (8677) 9 exp Acupuncture/ (4351) 10 acupuncture.tw. (3103) 11 exp acupuncture therapy/ or exp acupressure/ or exp acupuncture, ear/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/ (4689) 12 acupressure$.tw. (221) 13 electroacupuncture.tw. (131) 14 (meridian$ or moxi$).tw. (333) 15 exp Acupuncture Points/ (497) 16 acup$ point$.tw. (200) 17 or/9‐16 (5262) 18 8 and 17 (49) 19 exp clinical trials/ (58,044) 20 Clinical trial.pt. (32,026) 21 (clinic$ adj trial$1).tw. (13,186) 22 ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$3 or mask$3)).tw. (7966) 23 Randomi?ed control$ trial$.tw. (9743) 24 Random assignment/ (18,278) 25 Random$ allocat$.tw. (1144) 26 Placebo$.tw. (9960) 27 Placebos/ (4416) 28 Quantitative studies/ (3995) 29 Allocat$ random$.tw. (73) 30 or/19‐29 (80,696) 31 18 and 30 (12) 32 from 31 keep 1‐12 (12)
Data and analyses
Comparison 1. Acupuncture versus sham acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hot flush frequency (number/day) | 8 | 414 | Mean Difference (IV, Random, 95% CI) | ‐1.13 [‐2.55, 0.29] |
| 1.1 Traditional vs. sham acupuncture | 6 | 332 | Mean Difference (IV, Random, 95% CI) | ‐1.65 [‐3.62, 0.32] |
| 1.2 Electroacupuncture vs. sham acupuncture | 1 | 28 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐3.60, 3.00] |
| 1.3 Changes in frequency of hot flushes from baseline to end of study | 1 | 54 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.68, 1.28] |
| 2 Hot flush severity | 6 | 297 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐0.84, ‐0.05] |
| 2.1 Traditional vs. sham acupuncture | 4 | 215 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.98, 0.10] |
| 2.2 Electroacupuncture vs. sham acupuncture | 1 | 28 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.83, 0.66] |
| 2.3 Changes in severity of hot flushes from baseline to end of study | 1 | 54 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐1.33, ‐0.22] |
| 3 Hot flush frequency in trials less than 12 weeks | 6 | 335 | Mean Difference (IV, Random, 95% CI) | ‐1.68 [‐3.61, 0.24] |
| 3.1 Traditional vs. sham acupuncture | 5 | 281 | Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐4.88, 0.31] |
| 3.2 Changes in frequency of hot flushes from baseline to end of study | 1 | 54 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.68, 1.28] |
| 4 Hot flush frequency in trials of 12 weeks and more | 3 | 103 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐1.11, 1.40] |
| 4.1 Traditional vs. sham acupuncture | 1 | 51 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐1.47, 1.67] |
| 4.2 Electroacupuncture vs. sham acupuncture | 1 | 28 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐3.60, 3.00] |
| 4.3 Changes in frequency of hot flushes from baseline to end of study | 1 | 24 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐2.13, 3.33] |
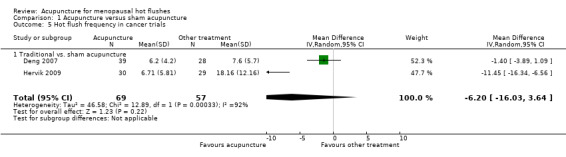
| 5 Hot flush frequency in cancer trials | 2 | 126 | Mean Difference (IV, Random, 95% CI) | ‐6.20 [‐16.03, 3.64] |
| 5.1 Traditional vs. sham acupuncture | 2 | 126 | Mean Difference (IV, Random, 95% CI) | ‐6.20 [‐16.03, 3.64] |
| 6 Hot flush severity in cancer trials | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.40 [‐3.50, ‐1.30] |
| 7 Hot flush severity in trials less than 12 weeks | 5 | 269 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.95, ‐0.06] |
| 7.1 Traditional vs. sham acupuncture | 4 | 215 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.98, 0.10] |
| 7.2 Changes in severity of hot flushes from baseline to end of study | 1 | 54 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐1.33, ‐0.22] |
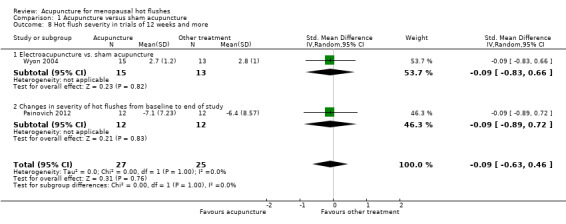
| 8 Hot flush severity in trials of 12 weeks and more | 2 | 52 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.63, 0.46] |
| 8.1 Electroacupuncture vs. sham acupuncture | 1 | 28 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.83, 0.66] |
| 8.2 Changes in severity of hot flushes from baseline to end of study | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.89, 0.72] |
| 9 Quality of life | 3 | 104 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.26, 0.51] |
| 9.1 Traditional vs. sham acupuncture | 2 | 80 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.33, 0.55] |
| 9.2 Changes in quality of life from baseline to end of study | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.64, 0.96] |
| 10 Quality of life in trials less than 12 weeks | 1 | 29 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.61, 0.87] |
| 10.1 Traditional vs. sham acupuncture | 1 | 29 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.61, 0.87] |
| 11 Quality of life in trials of 12 weeks and more | 1 | 51 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.45, 0.66] |
| 11.1 Traditional acupuncture vs. sham acupuncture | 1 | 51 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.45, 0.66] |
1.1. Analysis.
Comparison 1 Acupuncture versus sham acupuncture, Outcome 1 Hot flush frequency (number/day).
1.2. Analysis.
Comparison 1 Acupuncture versus sham acupuncture, Outcome 2 Hot flush severity.
Comparison 2. Acupuncture versus hormone therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hot flush frequency (number/day) | 3 | 114 | Mean Difference (IV, Random, 95% CI) | 3.18 [2.06, 4.29] |
| 1.1 Electroacupuncture vs. HT | 2 | 71 | Mean Difference (IV, Random, 95% CI) | 3.40 [1.96, 4.84] |
| 1.2 Acupuncture + auricular acupressure vs. HT | 1 | 43 | Mean Difference (IV, Random, 95% CI) | 2.84 [1.07, 4.61] |
| 2 Hot flush severity | 2 | 84 | Std. Mean Difference (IV, Random, 95% CI) | 0.53 [‐0.14, 1.20] |
| 2.1 Electroacupuncture vs. HT | 1 | 41 | Std. Mean Difference (IV, Random, 95% CI) | 0.89 [0.24, 1.53] |
| 2.2 Acupuncture + auricular acupressure vs. HT | 1 | 43 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.40, 0.80] |
| 3 Hot flush severity in cancer trials | 1 | 41 | Std. Mean Difference (IV, Random, 95% CI) | 0.89 [0.24, 1.53] |
| 3.1 Electroacupuncture vs. HT | 1 | 41 | Std. Mean Difference (IV, Random, 95% CI) | 0.89 [0.24, 1.53] |
| 4 Quality of life | 1 | 41 | Mean Difference (IV, Random, 95% CI) | 0.11 [0.01, 0.21] |
| 4.1 Electroacupuncture vs. HT | 1 | 41 | Mean Difference (IV, Random, 95% CI) | 0.11 [0.01, 0.21] |
2.1. Analysis.
Comparison 2 Acupuncture versus hormone therapy, Outcome 1 Hot flush frequency (number/day).
2.2. Analysis.

Comparison 2 Acupuncture versus hormone therapy, Outcome 2 Hot flush severity.
Comparison 3. Electroacupuncture versus relaxation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hot flush frequency (number/day) | 1 | 38 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐2.18, 1.38] |
| 1.1 Electroacupuncture vs. relaxation | 1 | 38 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐2.18, 1.38] |
| 2 Hot flush frequency in cancer trials | 1 | 38 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.78, 0.50] |
| 2.1 Electroacupuncture vs. relaxation | 1 | 38 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.78, 0.50] |
| 3 Hot flush severity | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Electroacupuncture vs. relaxation | 1 | 38 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.85, 1.25] |
| 4 Quality of life | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Electroacupuncture vs. relaxation | 1 | 38 | Mean Difference (IV, Random, 95% CI) | 8.3 [‐4.23, 20.83] |
3.2. Analysis.
Comparison 3 Electroacupuncture versus relaxation, Outcome 2 Hot flush frequency in cancer trials.
Comparison 4. Acupuncture versus waiting list or no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in frequency of hot flushes from baseline to end of study | 3 | 463 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.69, ‐0.31] |
| 1.1 Traditional acupuncture vs. waiting list/no intervention | 3 | 463 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.69, ‐0.31] |
| 2 Hot flush frequency | 1 | 28 | Mean Difference (IV, Random, 95% CI) | ‐5.27 [‐8.06, ‐2.48] |
| 2.1 Moxibustion vs. waiting list/no intervention | 1 | 28 | Mean Difference (IV, Random, 95% CI) | ‐5.27 [‐8.06, ‐2.48] |
| 3 Change in hot flush severity from baseline to end of study | 3 | 463 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.54 [‐0.73, ‐0.35] |
| 3.1 Traditional acupuncture vs. waiting list/no intervention | 3 | 463 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.54 [‐0.73, ‐0.35] |
| 4 Hot flush severity (end score) | 2 | 93 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.35 [‐1.81, ‐0.89] |
| 4.1 Acupuncture vs. waiting list/no treatment | 1 | 65 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.27 [‐1.81, ‐0.74] |
| 4.2 Moxibustion vs. waiting list/no treatment | 1 | 28 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.55 [‐2.43, ‐0.66] |
| 5 Quality of life ‐ change from baseline to end of study | 3 | 463 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.20, ‐0.67] |
| 5.1 Traditional acupuncture vs. waiting list/no intervention | 3 | 463 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.20, ‐0.67] |
| 6 Quality of life (end score) | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐5.98, 5.06] |
| 6.1 Moxibustion vs. waiting list/no intervention | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐5.98, 5.06] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Avis 2008.
| Methods | 2‐site clinical trial using 3‐arm prospective, randomized, single‐blind, sham‐control design; UC, SA, and TA | |
| Participants | 37 perimenopausal or postmenopausal women aged 42‐55 years experiencing at least 4 moderate‐to‐severe hot flushes per day and not having used HT, a selective oestrogen‐receptor modulator, an aromatase inhibitor, clonidine, Bellergal, antidepressant therapy, or gabapentin in the past 12 weeks; not having received chemotherapy; not having used acupuncture for any reason within the past 4 weeks; not having any previous acupuncture treatment for hot flushes; having no significant psychiatric disorder and untreated thyroid disease; not having been diagnosed with bleeding or clotting problem other than heavy periods; not currently taking any prescribed medications that increase the risk of bleeding (warfarin, enoxaparin, or clopidogrel) Setting: Massachusetts General Hospital and University of North Carolina. Women were recruited through newspaper advertisements, radio announcements, and hospital postings |
|
| Interventions | TA: 30‐minutes, standardized and individualized treatment according to TCM designed to tone or reinforce the kidney essence, balance yin/yang, and control hot flushes and night sweats, 2 times per week for 8 weeks. Treatments were given by experienced acupuncturists trained in TCM. No more than 16 acupuncture points were needled during any treatment. The 'De Qui' sensation was the elicited response. Type of needle used: Vinco 34‐gauge, 1‐inch (0.22 x 25 mm) and 30‐gauge, 1.5‐inch (0.30 x 40 m). Acupuncture points for the standardized treatment were CV 4, KI 3 (bilateral), SP 6(bilateral), BL 23(bilateral), HT 6 (bilateral), and KI 7 (bilateral), and the possible additional points (based on a person’s TCM diagnostic category or based on acupuncturist clinical judgement were KI 6, KI 10, GV 4, GV 20, CV 6, CV 15, BL 15, BL 18, BL 52, LR 3, LR 8, GB 13, GB 20, PC 7, HT 7, HT 8, yintang and taiyang SA: 30‐minutes treatment 2 times per week for 8 weeks were given by experienced acupuncturists trained in TCM. Non‐acupuncture points sites (sites where minimal effects on hot flushes) were needled shallowly, without attempting to elicit the 'De Qui' sensation. 12 needles were inserted, 6 on both side of the body (right and left). Point locations were: 3.5 cun below GB‐34; mid‐way between GB and BL channels; 2 cun above the lateral malleolus; 3 cun lateral to the navel; in the depression proximal to the metacarpal‐phalangeal joint between the index and middle fingers; approximately 1‐1.5 inches above or proximal to the third and fourth toe web space between the third and fourth metatarsals; and 3 cun lateral to the lower border of the spinous process of the fourth lumbar vertebra UC: There had been no initiation of treatment for their hot flushes for 2 months, but participants could continue with any non‐pharmacological treatment they were currently using |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
|
|
| Source of funding | National Cancer Institute, Massachusetts General Hospital, National Institutes of Health, National Center for Research Resources, General Clinical Research Centers Program, University of North Carolina at the Verne S. Caviness General Clinical Research Center at UNC School of Medicine | |
| Notes | Follow‐up: 8 weeks (after completion of treatment) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Treatment assignment was generated using a randomisation computer program and a computer file was kept at each clinic with their respective randomisation list. The acupuncturist accessed it from his/her PC and a paper copy of the randomisation assignments was kept at each clinical centre and by the Biostatistics and Data Management group at Wake Forest University for easy access in case of computer malfunction" (from the author) |
| Allocation concealment (selection bias) | Low risk | "The study coordinator and/or other personnel administering the questionnaires did not have access to the randomisation list to remain masked" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Study staff who administered questionnaires were blinded to which form of acupuncture that the women received" "The acupuncturists were blinded to the participant's treatment group until after making the TCM diagnosis" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Study retention was excellent with all women remaining in the study. However, not all women completed all study procedures. Eight (42%) of the women in the TA group and 10 (56%) in the SA group completed at least (80%) of the 16 treatments. Furthermore, two women in the UC group did not complete any follow‐up diaries, one in the SA group, and three in the TA group" Nothing reported about reasons for treatment withdrawal/not completing all study procedures Analyses were conducted with an ITT approach Nothing mentioned about imputation method |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | The study appeared free of other sources of bias |
Bokmand 2013.
| Methods | Randomized, subject‐blinded trial. 3 groups: true acupuncture, SA and no treatment | |
| Participants | 94 women in the postoperative period from 6 months to 5 years Perimenopausal or postmenopausal women aged 43‐76 years, treated for breast cancer, experiencing hot flushes and disturbed night sleep. Not having HT treatment or known metastatic disease Setting: Vejle Hospital and Herlev Hospital, Copenhagen University Hospital. Women were recruited through advertisement at the breast centre waiting room for mammography control and in the outpatient clinics |
|
| Interventions | 2 experienced acupuncturists gave either acupuncture in the selected acupuncture points or in the sham points True acupuncture: Predetermined bilateral points for 15‐20 minutes once a week for 5 consecutive weeks 4 acupuncture points were needled; Hc6, Ki3, Sp6, and Lr3. These points are located on the wrist, ankle, and foot SA: 4 predetermined bilateral non‐acupuncture points outside the meridians, but in the same region as the true points No treatment: Received no acupuncture To our knowledge none of the participants had acupuncture before |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
|
|
| Source of funding | "The study funds have no role in the study." The authors were supported by funds from Vejle Hospital: “Udviklingsfonden” and “Forskningsrådet”. |
|
| Notes | The study appeared free of other sources of bias | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The randomization was done by the acupuncturist. The participant personally drew a sealed envelope from a plastic bag and was randomly allocated to either of the three groups." No further details reported |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The randomization was done by the acupuncturist. The participant personally drew a sealed envelope from a plastic bag and was randomly allocated to either of the three groups." No further details reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Group acupuncture and sham‐acupuncture were both patient ‐ and investigator blinded" "Participants of no treatment group were not blinded" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropout |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Unclear risk | During the project period, some women received other type of treatment, which had no effect on neither the treatment nor acupuncture according to the authors. These women were divided in the 3 groups |
Borud 2009.
| Methods | Multicentre, randomized, controlled trial with 2 parallel arms; TA + self care advice, self care only | |
| Participants | 267 postmenopausal women experiencing on average, 7 or more hot flushes per 24 h for 7 consecutive days within the 2‐week qualifying period They were excluded if they had surgical menopause, history of cancer within the past 5 years (including use of tamoxifen), heart valve disease, poorly controlled hypertension, poorly controlled diabetes mellitus, organ transplant, mental disease, drug or alcohol dependency; used anticoagulant medication, and had inability to complete study forms. Women were recruited by newspaper advertisements and media coverage Setting: Oslo, Bergen and Tromso in Sweden |
|
| Interventions | TA + self‐care advice (1 page information): 10 individualized TCM acupuncture treatments were given for 12 consecutive weeks by 10 different acupuncturists having at least 2500 h of training and at least 3 years of clinical experience. The intervention could be extended 2 weeks if needed. The minimum number of session accepted as 'per protocol' was 6. Acupuncturist was instructed to see the participant within 1 week. Participants were treated according to the syndrome diagnosis. Point location was not standardized in the study but was left to the acupuncturists to decide. The 'De Qui' sensation was the elicited response. Moxibustion (heated needles) could be added if indicated in co‐intervention. They also received the 1‐page leaflet with information about self care strategies to relieve menopausal symptoms, and they were free to use any of these. Advice about sufficient sleep and rest, reduction in physical and psychological stress, regular exercise, healthy food, limited tobacco smoking and limited alcohol intake. There was a washout period for participants who had already taken HT: for systemic HT and SSRIs/SNRIs an 8‐week washout period was required; for local prescription HT 4‐week washout period was required. Self care advice only: Participants were not prescribed any medical treatment for menopausal symptoms but they were free to use any over‐the‐counter medication and self provided non‐pharmaceutical interventions, guided by the self‐care information leaflet (the same than in the acupuncture group). The intervention lasted 12 consecutive weeks. There was a washout period for participants who had already taken HT: for systemic HT and SSRIs/SNRIs an 8‐week washout period was required; for local prescription HT 4‐week washout period was required |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
|
|
| Source of funding | The Research Council of Norway and University Hospital of North Norway | |
| Notes | Follow‐up: 12 months (after the beginning of the study) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization lists were computer generated (blocked randomization, random block size) and stratified by centre |
| Allocation concealment (selection bias) | Low risk | Quote: "After enrolment, the local coordinator telephoned the central randomization unit at the University Hospital of North Norway (UNN) to obtain group allocation" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "All researchers remained blinded throughout the study. A person blinded to group allocation entered data on hot flashes and sleep into the database. The randomization code was broken only after the analyses of the primary outcomes were completed" "Participants were not blinded because they had acupuncture or a one page information of self‐care menopausal symptoms" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Missing data were handled by single imputation of missing values. Missing data on hot flash frequency and intensity of sleep at 12 weeks were substituted with the mean value of the entries in the diary of at least 3 days data had been recorded. If less than 3 days’ data were recorded, the data were considered missing. Single imputation is considered fairly accurate if the proportion of missing values is small (<5%). and replacing the missing values by the mean value is considered a valid strategy" "Missing data on hot flash frequency and intensity or sleep were found in a total of 16 hot flash diaries at week 12. The rate of missing information was 1.5%. Missing values for 1 day were substituted with the mean of the reported data in 10 diaries, for 2 days in two diaries, for 3 days in 2 diaries, and 4 days in 2 diaries" Few dropouts and reasons for withdrawal are reported. No serious adverse effects were reported |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | This study appeared free of other sources of bias |
Deng 2007.
| Methods | Randomized, controlled, subject‐blinded trial. 2 groups: true acupuncture and SA | |
| Participants | 71 women undergoing treatment for breast cancer at Memorial Sloan‐Kettering Cancer Center having a Karnofsky's performance score > 60 and experiencing an average of 3 or more hot flushes per day for 1‐week period with baseline diary Women planning surgery, chemotherapy, radiotherapy, immunotherapy; having initiated or ceased HT during the trial or within 3 weeks before the trial; using pharmacological treatment of hot flushes or SSRIs (unless dose remained stable for 4 weeks prior to study); having skin infection; having received acupuncture treatment in the 6 weeks prior to study or acupuncture given specifically for the treatment of hot flushes in the previous 6 months were excluded Setting: Memorial Sloan‐Kettering Cancer Center, New York, USA |
|
| Interventions | True acupuncture: Treatment given 2 times per week for 4 weeks by several licensed acupuncturists having 3 years of normal postgraduate training and 3 to 25 years of continuous practice Needles (stainless‐steel filiform 0.20 x 30 mm manufactured by Seiring Corp, Shizuoka, Japan) were inserted 0.25 to 0.5 inches into the skin at 19 acupuncture points (DU14, GB20, BL13, PC7, H6, K7, ST36, SP6, ear shen men, ear sympathetic point) for 20 minutes, and were manually stimulated. The 'De Qui' sensation was the elicited response SA: Treatment given 2 times per week for 4 weeks by several licensed acupuncturists having 3 years of normal postgraduate training and 3 to 25 years of continuous practice Needles (Streitberger sham needles 0.30 x 30 mm manufactured by Asjamed, Pullach, Germany) were applied a few centimetres away from the true acupuncture points for 20 minutes. Rather than penetrating the skin, the needle retracted inside its handle after insertion through an adhesive tape placed on a plastic supporting ring |
|
| Outcomes | Frequency of hot flushes per day using a diary | |
| Source of funding | National Cancer Institute | |
| Notes | Follow‐up: 6 months after initiation of treatment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random assignment of participants was accomplished using a secure, password‐protected, institutional computer system that stratified by using permuted blocks of random length" |
| Allocation concealment (selection bias) | Low risk | Quote: "The system is designed to ensure that allocation cannot be guessed before a patient is registered and cannot be changed afterwards, thus ensuring full allocation concealment.” "After participant registration and random assignment, a research assistant who was otherwise unconnected with the trial accessed allocation and telephoned the acupuncturist with the details of allocation" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Patients, researchers, and others involved in patient care were blind to study group; only acupuncturists and the designated research assistant were aware of which patients received true and which received placebo treatment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few dropouts and lost of follow‐up (true acupuncture, 2%; SA, 7%). Reason for missing outcome data unlikely to be related to true outcome. No ITT analysis |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | The study appeared free of other sources of bias |
Frisk 2008.
| Methods | Randomized, controlled study, part of the multicentre study HABITS (Hormonal replacement therapy After Breast cancer ‐ is IT Safe?). 2 groups: EA and HT | |
| Participants | 45 postmenopausal women having previously completed treatment for breast cancer in situ, T1 and T2 tumours with 4 or fewer lymph nodes positive for metastasis, T3 tumours without metastasis; having no clinical or mammographic signs of recurrence; having vasomotor symptoms needing treatment according to the woman herself Women planning surgery, chemotherapy, radiotherapy, immunotherapy; having initiated or ceased HT during the trial or within 3 weeks before the trial; taking pharmacological treatment of hot flushes; using of SSRIs (unless dose remained stable for 4 weeks prior to study); having skin infection; having received acupuncture treatment in the 6 weeks prior to study; and having received acupuncture specifically for the treatment of hot flushes in the previous 6 months were excluded "The women were referred from breast surgeons or oncologists because they suffered from breast cancer and vasomotor symptoms severe enough to merit therapy" Setting: this study was part of an international, multicentre study, HABITS, involving women from 3 centres in Sweden (Kalmar, Linkoping, Norrkoping). EA treatments were given both at hospitals and private practices |
|
| Interventions | EA: 30‐minute treatment given by 6 different physiotherapists educated and experienced in acupuncture for 12 weeks (twice per week for the first 2 weeks and once a week for 10 other weeks). Physiotherapists were instructed orally and in writing about the acupuncture points. Participants received EA at 2 Hz in 4 and 'classical acupuncture' in 8 of the acupuncture points: UB 15, 23, 32 (bilateral) and GV 20, H7, P6, LIV 3, SP6, SP9 (unilateral). The needles were inserted and rotated to elicit the sensation Teh Chi. At depths of 1.25‐2.5 cm this sensation was usually obtained. The procedure used was according to TCM acupuncture HT: There were 3 options for this treatment: women less than 2 years after menopause were given a sequential oestrogen/progestogen combination; women more than 2 years after menopause were given continuous combined oestrogen/progestogen; and post‐hysterectomy women received unopposed oestrogen. The treatment was given over 24 months |
|
| Outcomes |
|
|
| Source of funding | The country Council of Ostergotland | |
| Notes | Follow‐up (for EA): 24 months (after start of treatment) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The computerized randomization in blocks of eight for the HABITS study occurred at the University of Uppsala" "In all, 27 women were randomised to non‐hormonal and 18 to hormonal treatment; the groups were uneven because the three centres did not filled each of their block" |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote of author: "So, the patients knew which treatment (pills of HT or acupuncture) they were getting. All women, no matter if they were offered HT or acupuncture, chose to start the treatment they were randomized to" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Missing data were completed in the log books and for the KI, by taking the mean of the previous and the following measurements for that specific patient (logbook data in 8 cases (3%), when including women with another period of acupuncture in 12 cases (5%), KI data in 3 cases (1%), when including women with another period of acupuncture in 6 cases (3%))" Quote: "By the end of the study, 12/23 (52%) had asked for no other treatment than EA for 24 months." Therefore, 47.8% dropout for the EA group at 24 months Quote: "Eleven out of 18 women completed 24 months of HT." Therefore, 38.9% of dropouts for the HT An ITT approach was used to conducted the analyses High dropout rate during treatment Reasons for dropouts are reported |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes. However, the number of hot flushes per 24 h, as well as the Kupperman index score, was reported as mean changes and medians. The author provided the data for the 12 weeks for hot flushes frequency and severity for both groups No table for distress and not much detail for HT group (distress, number...) |
| Other bias | Low risk | The study appeared free of other sources of bias |
Hervik 2009.
| Methods | Randomized, single‐blind study of women following a breast cancer surgery. 2 groups: TA and SA | |
| Participants | 59 postmenopausal women (no menstruation for at least 3 months) having finished treatment for breast cancer (chemotherapy or radiotherapy), treated with oestrogen antagonist, tamoxifen, for at least 3 months after chemotherapy or radiotherapy, and complaining of hot flushes (no severity limits) Women taking medication for hot flushes either prior to, or during the treatment and follow‐up period; having received previous acupuncture treatment; being treated with other complementary or alternative therapies simultaneously; having serious endocrine or vascular disorders; suffering from psychological problems; and having hypertension (diastolic blood pressure over 95 mm Hg) were excluded Setting: The Breast Centre at Vestfold Central Hospital in Norway |
|
| Interventions | TA: 30‐minute treatment were given for 10 consecutive weeks (twice per week the 5 first weeks and once per week the remaining 5 weeks) by a physiotherapist (the same for both TA and SA groups) having 3 years' certified training course and 15 years' practice. 8 needles (0.30 mm) were inserted 0.5‐3 cm deep at 8 points along meridians in TCM (LIV3, GB20, LU7, KI3, Sp6, REN4, P7 and LIV8, unilateral) and manually stimulated. The 'De qui' sensation was the elicited response SA: 30‐minute treatment were given for 10 consecutive weeks (twice per week the 5 first weeks and once per week the remaining 5 weeks) by a physiotherapist (the same for both TA and SA group) having 3 years' certified training course and 15 years' practice. 8 needles (identical to TA group) were inserted 2‐3 mm deep at 8 points well away from acupuncture and trigger points (bilateral) |
|
| Outcomes |
|
|
| Source of funding | The Norwegian Acupuncture Association (NAFO), University of Tromso (NAFKAM), and Vestfold Central Hospital | |
| Notes | Follow‐up: 12 weeks (after completion of treatment). Additional data obtained from author by personal communication | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomized, using a sealed envelope technique, to receive either TA or SA" Comment: does not mention the randomization method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were randomized, using a sealed envelope technique, to receive either TA or SA" Comments: not mentioned whether the envelopes were sequentially numbered and opaque |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Patients were blinded to the type of acupuncture received" "A neutral attitude towards the patients and potential treatment effects was attempted, and all data was handled by a secretary blinded to the treatment group" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All patients completed treatment"; "Number of hot flashes was recorded in all but one patient (SA group), the KI was obtained from all patients throughout the study period" No dropout Use of ITT approach or imputation method not mentioned Comments: unclear about what have been done with the missing data |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | The study appeared free of other sources of bias |
Kim 2011.
| Methods | Randomized, single‐blind study of perimenopausal or postmenopausal women with moderate or severe hot flushes. 2 groups: TKM acupuncture and SA | |
| Participants | 54 perimenopausal and postmenopausal women (no menstruation for at least 3 months) having desired to receive treatment for hot flushes and complaining of moderate (able to continue activities) and severe hot flushes (not able to continue activities) Women taking medication for hot flushes within the 8 weeks prior to the study; history of cancer within 5 years; having total hysterectomy and serious endocrine or vascular disorders; suffering from psychological problems; and having medical conditions such as uncontrolled hypertension, diabetes mellitus or vaginal bleeding of unknown origin within 6 weeks were excluded Setting: The Dongguk University Ilsan Korean Medicine Hospital in South Korea |
|
| Interventions | TKM acupuncture: 20‐minute treatments were given for 7 consecutive weeks (twice per week the 4 first weeks and once per week the remaining 3 weeks) by a traditional Korean medicine doctor (the same for both TA and SA group) having more than 4 years of clinical experience and certified by the Korean Ministry of Health and Welfare. 13 needles (0.30 mm) were inserted 0.2‐10 mm deep at 7 points and manually stimulated. The 'de qi' sensation was the elicited response SA: 20‐minute treatments were given for 7 consecutive weeks (twice per week the 4 first weeks and once per week the remaining 3 weeks) by a TKM doctor (the same for both TA and SA group) having more than 4 years of clinical experience and certified by the Korean Ministry of Health and Welfare. 12 needles (identical to TA group) were inserted on 7 predefined non‐acupuncture points without stimulation, to not elicit the 'de qi' sensation For both groups, all participants were in a separate room with an eye bandage and no patient‐practitioner communication was allowed |
|
| Outcomes |
|
|
| Source of funding | The Korean Institute of Oriental Medicine | |
| Notes | Follow‐up: 15 weeks (8 weeks after completion of treatment) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random allocation software V1.0 (Department of Anaesthesia, Isfanhan University of Medical Science) was used to randomise patients into two groups. A block size of 4 was used" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The allocation of each patient was concealed by placing each random code in an opaque, sealed envelope. These envelopes were opened after the enrolment of the patient" Comments: not mentioned if the envelopes were sequentially numbered |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Patients were blinded to the type of acupuncture received. All participants were in a separate room with an eye bandage and no‐patient‐practitioner communication was allowed" "All data was collected by a blinded assessor" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few dropouts and lost of follow‐up (TA, 2 women; SA, 4 women). An ITT approach was used to conduct the analyses |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | The study appeared free of other sources of bias |
Kim 2010.
| Methods | Multicentre, randomized, controlled trial. 2 groups: acupuncture plus UC and UC alone | |
| Participants | 175 peri‐ and postmenopausal women aged 45‐60 years having a mean daily hot flush scores (daily frequency x severity) of 10 or higher for 1 week before screening visit Perimenopausal was defined as menstrual irregularity or amenorrhoea of 3‐11 months and postmenopausal as 1 of the following: 12 months of spontaneous amenorrhoea; 6 months of spontaneous amenorrhoea with FSH levels > 40 mIU/mL; 6 weeks' postsurgical bilateral oophorectomy with or without hysterectomy; or hysterectomy with at least 1 intact ovary Women were excluded if they had uncontrolled hypertension, diabetes mellitus, required insulin injections, any type of thyroid dysfunction, past or present malignant tumours, severe dyslipidaemia, other infectious diseases, or systemic diseases, and if they were using hormones, antidepressants, gabapentin, SSRIs, or sedatives Women were recruited through local newspaper advertisements, hospital postings, and notification in the community meeting Setting: Kang‐nam Kyung Hee Oriental Medical Center (Seoul), Dongguk International Hospital (Ilsan), Semyung University Hospital (Jecheon), Dong‐Eui Medical Center (Busan), Korea |
|
| Interventions | Acupuncture plus UC: Treatments were given by TKM physicians registered by the government with 3 years of clinical experience, 3 times per week for 4 consecutive weeks. Acupuncture points were selected according to recommendations of TKM clinical experts and are ST36, SP6, LI4, PC6, HT7, HT8, and CV4 and the 'De Qui' sensation were the elicited response. Needles were inserted 3‐15 mm depending on the point selected, remained in place for 20 minutes, and were manipulated manually (intermittently). Needles used were 40 x 0.25 mm. Participants and physicians could communicate freely about participant's symptoms and general conditions Follow‐up at weeks 6 and 8. UC consisted of the use of non‐prescription drugs for episodic or minor symptoms that were not related to hot flushes or supplements (including evening primrose oil, phyto‐oestrogens, omega‐3 fatty acids, calcium, and vitamins. UC: UC alone group received no acupuncture treatment for the 4‐week study period and could use non‐prescription drugs for episodic or minor symptoms that were not related to hot flushes or supplements (including evening primrose oil, phyto‐oestrogens, omega‐3 fatty acids, calcium, and vitamins Additional acupuncture treatment, herb prescriptions, or therapeutic interventions by another TKM physician were not allowed during the treatment period for both groups Follow‐up at weeks 6 and 8 |
|
| Outcomes | Primary outcome:
Secondary outcome:
Timing of assessment of the main outcome: at baseline, and at week 1, 2, 3, 4, 6, and 8 after randomization |
|
| Source of funding | Acupuncture, Moxibustion, and Meridian Research Project (K09050) of the Korean Institute of Oriental Medicine | |
| Notes | Follow‐up: 2 weeks (after completion of treatment, i.e. weeks 6 and 8) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A separate randomization sequence was computer generated at the central coordinating centre and provided for each local treatment centre" |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "This was an open trial, so patient blinding was unavailable. We failed to blind the assessor to assignment of patient. Instead, all outcomes were self‐administered by patients, and the researcher who was separated from the treatment procedure collected the data. Data were sent to the central research centre, and personal who were independent of this study entered the data" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data are not balanced across intervention groups (acupuncture plus UC, dropouts 7%; UC, dropouts 19%) and reasons for missing data differ Analyses were conducted with an ITT approach Missing data were replaced with the last observation value |
| Selective reporting (reporting bias) | Low risk | This study appeared free from selective reporting |
| Other bias | Low risk | This study appeared free from other bias |
Nedstrand 2006.
| Methods | Randomized, controlled trial in women treated for breast cancer. 2 groups: AR and EA | |
| Participants | 38 women treated for breast cancer aged 30‐64 years, with treatment‐induced or spontaneous menopause, that had last menstruation at least 6 months prior, experiencing at least 2 flushes per 24 h and regarding the flushes severe enough to require treatment, and wishing to receive treatment for vasomotor symptoms Women that took HT in the last 6 months; had severe metabolic, endocrine, or thromboembolic disease; had uncontrolled hypertension and used sedatives daily; and taken anxiolytic or antidepressant medication were excluded Study setting: the outpatient clinics at the Departments of Oncology and Breast Surgery at the Linköping University Hospital in Sweden |
|
| Interventions | AR: Weekly 60‐minute group sessions (5‐6 in each group) for a 12‐week period given by a physician familiar with AR having undergone training but not having formal education in behaviour therapy. This instructor was self trained to use technique of AR, and was supervised by a certified clinical psychologist. Participants were asked to train at home twice daily, to discuss the results of training each week at the group session and were given information about menopause and theories of hot flushes. The following components were explored during the AR programme: progressive relaxation, cue‐controlled relaxation, differential relaxation, and rapid relaxation. EA: 30‐minutes treatment given twice per week the first 2 weeks and once a week for another 10 weeks by a physiotherapist experienced and skilled in acupuncture treatment. 12 sterile stainless‐steel needles were inserted 5‐20 mm into the skin and were twirled to elicit the 'De qui' sensation. 4 of them were in the lower back, BL23 and 32 bilaterally, and were attached to an electrical stimulator giving a low burst frequency of 2 Hz alternating current stimulation. A non‐painful local muscle stimulation. |
|
| Outcomes |
Timing of assessment: at baseline; after 4, 8, and 12 weeks of therapy; and at 3 and 6 months after completion of therapy for the first 4 outcomes cited above; 2 weeks prior to treatment, daily for the 12‐week treatment period, and for the 6‐month follow‐up in daily every fourth week for hot flushes frequency |
|
| Source of funding | The Swedish Medical Research Council, The Swedish Foundation for Health Care Sciences and Allergy Center, Cancer and Trafikskadades Förbund, and The Lions Foundation | |
| Notes | Follow‐up: 6 month (after completion of treatment) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of generating random sequence not reported |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomization to AR or EA was performed using identical, opaque, sealed envelopes containing a label naming the treatment." Not reported whether envelopes were sequentially numbered |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants and therapists were not blinded because of 2 different therapies applied Comments: not reported if the others involved in the research were blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout rate (AR, 26%; EA, 11%) Reasons for withdrawal mentioned Quote: "Missing values were compensated for by the mean of the score from the time before and after in each case" No mention of ITT approach Number of women analysed at week 12 and at the end of the 6‐month follow‐up is unclear |
| Selective reporting (reporting bias) | Low risk | This study appeared free from selective reporting |
| Other bias | Unclear risk | Few information about characteristics of participants at baseline |
Nir 2007.
| Methods | Randomized, placebo‐controlled pilot study. 2 groups: active acupuncture and SA | |
| Participants | 29 postmenopausal women aged 45‐65 having: no menstrual period for at least 6 months or at least 6 weeks post‐bilateral oophorectomy; a baseline oestradiol concentration of less than 50 pg/mL and normal TSH level; a mean of at least 7 moderate‐to‐severe hot flushes/24 h or a mean of at least 70 hot flushes per week during the screening/baseline phase Women having endocrine disorders, including unstable thyroid disease, known or suspected oestrogen‐dependent neoplasia, known psychiatric disorders, abnormal results on a laboratory TSH test, a baseline oestrogen level higher than 50 pg/mL; having received any treatment for hot flushes, including black cohosh, phyto‐oestrogens, or acupuncture for 6 weeks before the study; having any unstable medical conditions; using any medication known to affect vasomotor symptoms (e.g. clonidine, veralipride, SSRIs); and having received acupuncture within the past year were excluded Women were recruited through advertisements at community clinics Setting: community clinics of San Francisco Bay Area, US |
|
| Interventions | Active acupuncture: 9 acupuncture sessions, twice weekly for the first 2 weeks and once weekly for the remaining 5 weeks. Disposable, stainless‐steel filiform needles (appearing identical to placebo) were inserted for 20 minutes at 5‐7 active treatment points (3‐6 points according to participant's primary TCM‐defined pattern for hot flushes, and 1 or 2 points according to secondary TCM‐defined pattern). Stimulation was manual and the 'De qui' sensation was the elicited response. 5 licensed acupuncturists provided both active and placebo treatments. They received training to maintain a standardized interaction with all participants. Follow‐up: 1 month SA: 9 acupuncture sessions, twice weekly for the first 2 weeks and once weekly for the remaining 5 weeks. Disposable, stainless‐steel filiform needles (appearing identical to active needles and having blunt tips that touch the skin before retracting up into a hollow shaft handle) were used at 5‐7 sham points among 10 non‐valid points located off any acupuncture channels. There was no skin penetration and stimulation was manual. Follow‐up: 1 month |
|
| Outcomes | Primary:
Timing of assessment of the main outcome: at baseline, every week for the 7‐week treatment, at the end of treatment, at the end of the 1‐month follow‐up Secondary:
|
|
| Source of funding | Not reported | |
| Notes | Follow‐up: 1 month (after completion of treatment) There were no significant differences between groups at baseline in severity, frequency, body mass index, age at menopause, years since last menstrual period, history of or time on HT but there was a significant difference in age |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "In order to balance the number of placebo and active treatments among the acupuncturists, we created a separate randomization table for each acupuncturist by generating a random string of permutations of two elements (blocked randomization)" |
| Allocation concealment (selection bias) | Unclear risk | Quote(from the author): "The subjects underwent the same protocol for the first acupuncture visit (anamnesis, questions regarding the hot flashes etc.) nature which determined which points would be used and only after this session they were divided to the treatment and placebo group using a sealed envelope with allocation. Not reported whether envelopes opaque, sealed and sequentially numbered" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote (from the report): "To minimize the potential confounding effect of the acupuncturist’s awareness of which treatment participants were receiving, acupuncturists were trained to maintain a standardized interaction with all participants. All sessions were audio‐taped, of which five percent were randomly selected and reviewed for adherence to the standardized protocol by an independent rater who remained blind to the type of treatment received" Quote (from the author): "Placebo treatment included none acupuncture points but to the inexperienced patient these are very similar (proximal) to actual points and similar in number to the treatment group. The acupuncturists were instructed on how to verbally conduct the session, to avoid any conversation other than the pre determined protocol. This included length of the session and wording. Investigators were not aware of the allocation of the patients to treatment or placebo group during the study when meeting with the patients in the first session as well as when reviewing hot flash log data" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout rate (active acupuncture, 17%; SA, 24%) Reasons mentioned but some are likely to be related to true outcome (dissatisfied with treatment). The total number of women analyzed was 12 in the active acupuncture group and 17 in the SA (according to the participant flow diagram). ITT approach and imputation method not reported |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | High risk | There was a significant difference in age between the 2 groups at baseline Source of funding not mentioned |
Painovich 2012.
| Methods | Pilot, randomized, single‐blind, placebo‐controlled trial. 3 groups: TA, SA, and waiting list control | |
| Participants | 21 women older than 40 years with menopause‐related vasomotor symptoms. Inclusion criteria included at least 7 hot flushes per day and at least 1 missed menstrual cycle or spontaneous or medically induced menopause. Exclusion criteria included concomitant illness with reasonable likelihood of limiting survival to less than 1 year; current substance abuse; known, suspected, or planned pregnancy in the next year; other concomitant menopause treatment; participating in acupuncture treatment or formal psychological stress management programme within the last year; participating in another treatment of vasomotor symptoms, unless willing to stop it 4 weeks in advance of participation; human immunodeficiency virus infection; chronic or active hepatitis; or other blood‐borne illness Setting: Cedars‐Sinai Heart Institute, Los Angeles, CA, US |
|
| Interventions | Intervention period was 3 months; participants received treatment 3 times per week for a maximum total of 36 treatments. Data and specimen collections were carried out at weeks 0, 5, and 12 TA: 11 front points, which were placed with the women lying supine, and 7 back points, which were accessed in prone position. The needles were inserted 0.5‐1.5 inches and then manually stimulated to reach 'de‐qi' and then retained for 30 minutes. The needles were secure with adhesive tape SA: The sham points were selected by the team to be proximate to the TA site. The disposable acupuncture needle and plastic needle tube were placed on the sham points, manipulated without skin penetration and secure with adhesive tape Waiting list control: The women received no treatment for 3 months, underwent exit testing, and subsequently had the option of 1 month of complimentary TA |
|
| Outcomes |
|
|
| Source of funding | National Institutes of Health ‐ National Center for Alternative and Complementary Medicine and General Clinical Research Center grant from the National Center for Research Resources | |
| Notes | Study approved by the Cedars‐Sinai Institutional Review Board | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were allocated to 1 of 3 study arms with equal probability using a randomized block design after signing the consent form |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | The participants were blinded as to the randomization status, the waiting list control group necessarily knew their randomization status. Both TA and SA groups were required to wear eye covers throughout the treatment The treating acupuncturists were unblinded, to know whether to deliver TA or SA Comments: nothing mentioned concerning the blinding of the outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 27 dropped out, 16 before treatment began, 8 in each acupuncture group and 11 from the waiting control despite being offered free acupuncture after the 3‐month waiting period |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | The study appeared free from other bias |
Park 2009.
| Methods | Randomized, clinical trial. 3 groups: moxibustion 1, moxibustion 2, and waiting list | |
| Participants | 28 perimenopausal or postmenopausal women aged 45‐60 years experiencing at least 5 moderate (warm sensation with a transient and insignificant impact on the participant's activity) to severe (hot sensation with sweating that caused significant disruption to a participant's daily activity) hot flushes every 24 h and had natural or surgical menopause Women having uncontrolled hypertension, diabetes mellitus requiring insulin injections, any type of thyroid dysfunction, past or current malignant tumours, severe dyslipidaemia, other infectious diseases or systemic diseases; using hormones, antidepressants, gabapentin, SSRIs, or sedatives; using transdermal HT within 4 weeks or oral hormone medication within 8 weeks were excluded Women were recruited from Daejeon, South Korea using local newspaper advertisements and notices posted at various clinics Setting: South Korea |
|
| Interventions | Moxibustion 1: Moxibustion capsules formulated as a disposable adhesive, and were composed of a moxa pillar attached to the base of the device. Total length of the moxibustion device was 25 mm, of which 18 mm constituted the moxa pillar. Acupoints used were consistent with evidence from clinical practice. There were 4 acupoints: CV12, CV4, bilateral ST36, SP6. 5 moxibustion capsules used at each point in a single session. Treatment procedures were identical in Moxa 1 and Moxa 2. Treatments were given for 4 weeks (4 times per week for the first 2 weeks and 3 times per week for the 2 remaining weeks) by a qualified acupuncture doctor licensed in the Republic of Korea having had 6 years of training in acupuncture and moxibustion Moxibustion 2: The same moxibustion capsules were used in Moxa 1 and Moxa 2. Acupoints used were consistent with evidence in published literature. 5 moxibustion capsules were used at each point in a single session. There were 4 acupoints: GV4, CV3, CV6, bilateral UB23. Participants received this type of acupuncture 4 times per week for the first 2 weeks and 3 times per week for the 2 remaining weeks. Treatments were given for 4 weeks (4 times per week for the first 2 weeks and 3 times per week for the 2 remaining weeks) by a qualified acupuncture doctor licensed in the Republic of Korea having had 6 years of training in acupuncture and moxibustion Waiting list: The 10 participants in this group did not received any treatment for 5 weeks (including the 1‐week follow‐up period) |
|
| Outcomes | Primary outcomes:
Time of assessment of the main outcomes: at baseline, during treatment (at 1, 2, and 3 weeks), at the end of treatment (week 4), and for a 2‐week follow‐up period (week 6) Secondary outcomes:
|
|
| Source of funding | Korea Institute of Oriental Medicine (K08010) | |
| Notes | Follow‐up: 2 weeks (after completion of treatment); and 1 week for the waiting list group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed by the study coordinator using a computerized list with an assignment ratio of 2:2:1 (Moxa 1/Moxa 2/control)” |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "All analyses were conducted blind to group allocation” "[The participants] were not told which treatment they would received. In addition, to eliminate observation bias, the two assessors were blind to the intervention group before analysis of data" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Analyses were performed with the ''intention to treat'' population for which all participants were randomised at least once after moxibustion treatment (missing data were replaced with the last observation value)'' Moderate dropout rate (10% for both moxibustion group 1 and 2; 0% for the waiting list) Reasons for dropouts are mentioned |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | This study appeared to be free of other sources of bias |
Venzke 2010.
| Methods | Randomized, single‐blind, controlled clinical trial. 2 groups: TCM acupuncture and SA | |
| Participants | 51 postmenopausal women having vasomotor symptoms (hot flushes, night sweats) more than 14 events of any severity per week, or more than 5 moderate‐to‐severe events (waking up soaked, needed to change clothing); having no menstrual period for at least 12 months; having natural menopause; not using ET/HT or herbal treatment for menopausal symptoms for at least 3 months before enrolment; and not having received acupuncture treatments within the last 6 months; able to keep regular appointment Women having artificial menopause (due to surgery, radiotherapy, or medication), a pacemaker, an history of heart disease, an history of active alcohol or drug abuse within the last year before enrolment; human immunodeficiency virus disease, fibromyalgia, uncontrolled thyroid disease, uncontrolled hypertension and any systematic illness, condition, or personal situation (such as an unstable living situation) that might render the person unable to complete the study, fulfil the demands of the study, interfere with data interpretation, or create undue risk were excluded Women were recruited through advertisements in the local newspaper, brochures displayed in local physician's surgery, and by word of mouth Setting: Sky Lake Medical Center in a small city, Klamath Falls, in rural area of Eastern Oregon, US |
|
| Interventions | TCM acupuncture: 25‐minute treatment given for 12 weeks twice a week for 4 weeks and once a week for 8 weeks) by a licensed acupuncturist trained in TCM‐style acupuncture and having expertise in hot flushes with menopausal women and women with breast cancer. TCM pattern differentiation and selection of acupuncture points were based on several TCM sources. Stimulations received were manual and electrical. Hwato needles (1 inch/34 gauge and 1.1/2 inch/32 gauge) without tubes were used. During each treatment, 6‐12 acupuncture points were selected among the following: UB23‐20‐15‐17, Du9‐4‐24, Sp9‐6, right Lu7, left Ki6, Ki3‐7, H6‐7, Liv3, and GB20. The 'De Qui' sensation was the response elicited. For electrical stimulation, acupuncturist used 4 needles (bilateral UB23 and SP6) connected to an EA device (ITO, model IC 1107) and stimulated at a frequency of 2 Hz. For manual stimulation, the remaining needles were stimulated again manually after 15 minutes. The needle retention time was 25 minutes. Advice regarding diet and exercise was also given to women SA: 25‐minute treatment given for 12 weeks (twice a week for 4 weeks and once a week for 8 weeks) by a licensed acupuncturist trained in TCM‐style acupuncture and having expertise in hot flushes with menopausal women and women with breast cancer. Streitberger and Kleinhenz needles as well as small plastic rings for no penetration of the skin were used (2 on the back, 2 on the lower legs, and 2 on the forearms). 4 of the placebo needles were connected to a disabled acupuncture device (ITO, model IC 1107). The other 2 placebo needles had manual stimulation. The specific points were away any acupuncture meridians. The acupuncturist had expertise in hot flushes with menopausal women and women with breast cancer. Advice regarding diet and exercise were also given to women |
|
| Outcomes | Primary outcomes:
Timing of assessment of the main outcome: at baseline, at week 4 during treatment, and at week 13 and 24 after treatment |
|
| Source of funding | Merle West Center for Medical Research (Klamath Falls, Oregon) | |
| Notes | Follow‐up: 12 weeks (after completion of treatment) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "At the start of the study, randomization was then accomplished by asking study subjects to draw an envelope. In each envelope there was a small piece of paper with the typed letter A or B. Subjects who drew an A were randomised to the PA [placebo acupuncture] group; subjects who drew B were randomised to RA [real acupuncture] group" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "At the start of the study, randomization was then accomplished by asking study subjects to draw an envelope. In each envelope there was a small piece of paper with the typed letter A or B. Subjects who drew an A were randomised to the PA [placebo acupuncture] group; subjects who drew B were randomised to RA [real acupuncture] group" Rationale for judgement: unclear whether allocation might be predictable as envelopes ran out |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "This study was designed as a single‐blind, randomised, controlled clinical trial" "During the final visit study subjects were asked to guess whether they had received placebo or real acupuncture, and at what stage they came to that conclusion. This helped us assess how successful our blinding was" Comments: participants blinding only |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "A total of 56 subjects were randomised and 51 of these completed the study." "RA was given to 27 and PA to 24 of the 51 subjects who completed the study." (Total dropout rate was 9%) Reasons for dropouts are not reported Imputation method and use of an ITT approach to conduct analyses are not reported |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | The study appeared free of other sources of bias |
Vincent 2007.
| Methods | Prospective, randomized, single‐blind, sham‐controlled trial. 2 groups: medical acupuncture and SA | |
| Participants | 103 perimenopausal (3 or more months of self reported menstrual irregularity or amenorrhoea) and postmenopausal (amenorrhoea for 12 or more months) women aged 45‐59 years and experiencing a mean of 5 or more hot flushes per day. Women using oestrogen, soy, progesterone, vitamin E, or black cohosh; using non‐prescription drugs, gabapentin, or antidepressants specifically for the treatment of hot flushes within the previous month; using warfarin; having skin disorders with skin breakdown such as eczema or psoriasis; having a pacemaker or prosthetic joints; having active chemotherapy; and suffering of diabetic neuropathy were excluded Setting: Mayo Clinic General Clinical Research Center, US |
|
| Interventions | Medical acupuncture: Treatments were given twice per week for 5 weeks by an acupuncturist (the same for both medical and SA) licensed by the Minnesota Board of Medical Practice and having 5000 h of experience. The needling was administered in 12 acupuncture points (SP4 unilateral, SP6 bilateral, He7 bilateral, Ll11 bilateral, Liv2 bilateral, Ki6 unilateral, LU7 unilateral right, PC6 unilateral left, GB34 bilateral, Liv3 bilateral, Ren4, GB20 bilateral). Needles were inserted 0.5‐3 cm into the skin, and the 'De qui' sensation was the elicited response Follow‐up: 7 weeks SA: Needling administered in non‐acupuncture, non‐meridian areas, whenever possible 5 cm or more away from the actual acupuncture point. Treatments were given twice a week for 5 weeks Follow‐up: 7 weeks |
|
| Outcomes | Primary: daily hot flush score (frequency x severity) using a diary Timing of assessment: at baseline, and every week for the 5‐week treatment and for the 7‐week follow‐up period |
|
| Source of funding | Mayo Foundation Award | |
| Notes | Follow‐up: 7 weeks (after completion of treatment) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized to medical or sham acupuncture using a stratified randomization schedule. Stratification was done using menopausal status to ensure equal distribution of peri‐ and postmenopausal women among the two groups. A blocked size of four was used" |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote (from the author): "Patients were blinded to the group assignment. We also did not include any patients who had previous acupuncture so they would not know if it was actual or sham acupuncture. We did not blind the investigators" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rate was about 10% (SA: 13%; medical acupuncture: 10%) Reasons for attrition were reported (not related to true outcome) Quote: "The last observation carried forward was used for imputing missing data per an intention‐to‐treat model" |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | The study appeared free of other sources of bias |
Wyon 2004.
| Methods | Randomized controlled trial. 3 groups: EA, SNI, and ET | |
| Participants | 28 postmenopausal women aged 48‐63 years with vasomotor symptoms and a spontaneous menopause at least 6 months previously. Women were excluded if they had a severe metabolic, thromboembolic, or endocrine disease; they had uncontrolled hypertension (> 95 mmHg diastolic); they were using sedative, anxiolytic, or antidepressant medication; if they were using narcotics; they were doing regular exercise more than once per week Setting: gynaecological outpatient clinic of the Linköping University Hospital in Sweden |
|
| Interventions | EA: 30‐minute treatment given by an experienced physiotherapist skilled in acupuncture for 12 weeks (twice per week for the first 2 weeks and once a week for the next 10 weeks). 12 needles (stainless‐steel, Hwato 0.25 mm diameter, 15 mm long, and 0.30 mm diameter and 30 mm long) were inserted 5‐20 mm into the skin at different point locations (bilaterally, B15‐23‐32; unilaterally, HT7, SP6‐9, LR3, PC6, GV20). 4 needles in lower back were attached to an electrical stimulator (IC‐1107, Ito Co., Ltd, Japan) with a burst frequency of 2 Hz alternating current stimulation. The 'De qui' and a non‐painful local muscle contractions were the elicited responses Follow‐up: once a week for the next 6 month after treatment SNI: 30‐minute treatment given by an experienced physiotherapist skilled in acupuncture for 12 weeks (twice per week for the first 2 weeks and once a week for the next 10 weeks). Small‐dimension needles (Hwato, 0.25 mm diameter, 15 mm long) were inserted parallel to the skin 1‐5 cm away from EA points. 3 needles (BL15‐23‐32) were moved laterally on the back about 10‐15 cm. No additional stimulation after insertion was elicited Follow‐up: once a week for the next 6 months after treatment ET: Women were given oral 2 mg 17β‐oestradiol for 12 weeks. They were suggested to continue their ET with additional sequential progestogens given monthly Follow‐up: once a week for the next 6 month after treatment |
|
| Outcomes | Primary:
Timing of assessment of the main outcome: before treatment; after 4, 8, and 12 weeks of treatment; and 12 and 24 weeks after the end of therapy Secondary:
|
|
| Source of funding | The Swedish Medical Research Council grant to K2001‐72x‐12651‐O4B, The Swedish Foundation for Health Care Sciences and Allergy Research and Cancer and Trafikskadades Förbund, The Lions Foundation | |
| Notes | No significant difference of groups at baseline except that women in the oestrogen group were slightly younger Follow‐up: 6 month (after completion of treatment) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomization was performed by the use of identical, opaque, sealed envelopes, containing label to determine the treatment." Not reported whether envelopes sequentially numbered |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "The gynaecologists and nurses evaluating the patients were blind to treatments, i.e. at evaluation, the physician and research nurse did not know which acupuncture treatment each women had and not until after analysis of the results did we unveil the treatment modalities. Furthermore, the patients were only informed that two different modalities were used but not that we expected one to be more efficient" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All women randomized to electro‐acupuncture and estradiol therapy completed the 12 weeks of treatment" At 6 months, few dropouts and exclusions (EA :4, SNI :1, ET:6) Reasons for withdrawals reported No ITT analysis |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | The study appeared free of other sources of bias |
Zhou 2011.
| Methods | Randomized controlled trial. 2 groups: acupuncture, auricular acupressure, and HT | |
| Participants | Bilaterally ovariectomized Chinese women suffering from menopausal hot flushes presenting a normal TSH level and oestradiol concentration < 50 pg/mL. They were excluded if they were under other medical treatment during the research period, had metabolic, renal, anaphylactic, or endocrine disease, or suffered from primary hypertension, primary hypotension, chronic anaemia, tuberculosis, a mental disorder, or a chronic condition; body mass index more than 24, or cigarette smoker. Women were recruited by advertisement. Setting: Zhejiang University, University of Chinese Medicine, Liaoning University of Chinese and Colorado School of Traditional Chinese Medicine |
|
| Interventions | Acupuncture: 40‐minute treatment given twice a week for 12 weeks. 8 points were selected: SP6, GB20, LI4, LI11, CV4, GV14, KI7, and EX‐CA1. The needles were manipulated twice during the treatment using a twirling technique in a small range. The manipulation lasted 30 seconds for each acupoint. Sterilized disposable needles (0.35 mm x 40 mm) were inserted using the double hand‐needle insertion technique. The depth of insertion was adjusted based on the woman's body size and the permissible depth of insertion of the specific acupoint Auricular acupressure: Height auricular acupoints were selected: AH6a, TF4, TG2p, AT4, CO18, CO10, CO15, and Co12. Pieces of plaster with magnetic beads of proper size and good quality were stuck to the acupoints, which were then pressed slightly until the person had an aching pain, numbness, distension, and a warm sensation. The participants were asked to press the acupoints by themselves 6 times a day for a 3‐minute duration each time. The auricular acupressure was alternatively conducted on both ears every 2 days. The plaster was changed once a week HT: The participants were prescribed with oral Livial (tibolone) of 1 tablet a day (2.5 mg/tablet) for 12 consecutive weeks |
|
| Outcomes | Primary outcomes:
Time of assessment: at baseline, at the end of treatment, and after a 4‐week follow‐up period Secondary outcomes:
|
|
| Source of funding | Natural Medicine Research UK, China Postdoctoral Science Foundation, Zhejiang Traditional Chinese Medicine Foundation, Zhejiang Provincial Postdoctoral Science Foundation, Outstanding Young Medical Scientist Foundation of Zhejiang Province | |
| Notes | Follow‐up: 4 weeks (after completion of treatment) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were randomized to either the acupuncture and auricular acupressure group or the HT group with the use of a randomization chart constructed in Microsoft Excel that randomized numbers into two groups" |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants knew which treatment (acupuncture + auricular acupressure or HT) they were getting. The acupuncturist was not blinded to the treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Three subjects were considered missing cases during the study and were excluded from analysis" Reasons for withdrawals reported No ITT analysis |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes |
| Other bias | Low risk | This study appeared free from other bias |
AR: applied relaxation; EA: electroacupuncture; ET: oestrogen therapy; FSH: follicle‐stimulating hormone; HT: hormone therapy; ITT: intention to treat; LH: luteinizing hormone; MRS: Menopausal Rating Scale; SA: sham acupuncture; SNI: superficial needle insertion; SNRI: serotonin‐noradrenaline reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor; TA: traditional acupuncture; TCM: traditional Chinese medicine; TKM: traditional Korean medicine; TSH: thyroid‐stimulating hormone; UC: usual care; VAS: visual analogue scale.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Azizi 2011 | Combination of treatments |
| Borud 2010 | Not an RCT |
| Castelo Branco 2011 | No washout period between interventions |
| Cohen 2003 | Data on vasomotor symptoms |
| Cummins 2000 | Not an RCT |
| Davies 2001 | Not an RCT |
| De Valois 2003 | Not an RCT |
| De Valois 2010 | Not an RCT |
| Facchinetti 1989 | Data on acupuncture techniques |
| Frisk 2012 | Data on vasomotor symptoms were the same presented in Frisk's study in 2008 |
| Grilli 1989 | Data on acupuncture techniques |
| Gui‐e 2000 | The trial does not include perimenopausal, menopausal, or postmenopausal women who experiencing hot flushes at baseline |
| Guévin 2009 | Not an RCT |
| Harris 2002 | Not an RCT |
| Hervik 2010 | Not an RCT |
| Hu 2005 | Not an RCT |
| Huang 2006 | Data are identical to Nir's study in 2006 |
| Huazhang 2008 | There is no comparison between acupuncture intervention and placebo, control or other treatment |
| Huo 2004 | No data on menopausal hot flushes or on other menopausal symptoms |
| Ji 1998 | Not an RCT |
| Jin 2007 | Data on vasomotor symptoms |
| Kao 2012 | No data on hot flushes |
| Lesi 2012 | Meeting abstract. Uncontrolled experimental pilot study |
| Li 2005 | Data on vasomotor symptoms |
| Mingling 1991 | Not an RCT |
| Nedstrand 2005 | Data are identical to Nedstrand's study in 2006 |
| O'Brien 2010 | Data on vasomotor symptoms |
| Otte 2011 | Not an RCT |
| Perez 2005 | Meeting abstract |
| Porzio 2002 | Not an RCT |
| Sandberg 2002 | No assessment of hot flushes |
| Spetz Holm 2012 | Not an RCT |
| Sunay 2011 | Not an RCT |
| Towlerton 1999 | Not an RCT |
| Tukmachi 2000 | Not an RCT |
| Walker 2007 | Not an RCT |
| Walker 2008 | Meeting abstract. Data are identical to Walker's study in 2010 |
| Walker 2010 | Data on vasomotor symptoms |
| Wyon 1995 | Data on vasomotor symptoms |
| Xia 2008 | Data on vasomotor symptoms |
| Xiaoming 2005 | Not an RCT |
| Xu 2004 | Complex therapy included acupuncture, traditional Chinese medicine drug, and Nieji were used in treatment group |
| Zaborowska 2007 | Duplicate of Wyon's study in 2004 |
| Zhang 2006 | Not an RCT |
| Zhenya 2001 | Not an RCT |
| Zhou 2006 | Not an RCT |
RCT: randomised controlled trial.
Differences between protocol and review
We increased the scope of the search for the 2013 update, using the strategy described in Appendix 1.
Contributions of authors
Sylvie Dodin (SD) wrote the protocol. Joalee Paquette (JP), Caroline Vaillancourt (CV), and Claudine Blanchet (CB) selected and classified the studies to be included, with SD if a consensus was needed. JP, CV, and CB extracted the data, carried out the risk of bias assessment, and discussed it with SD. Wu Taixiang (WT) searched for and selected the trials from the Chinese databases. Elisabeth Maunsell, Isabelle Marc and Edzard Ernst co‐drafted the protocol and earlier version of the review. CB wrote the first draft of the review under SD's supervision.
Sources of support
Internal sources
None, Not specified.
External sources
None, Not specified.
Declarations of interest
None.
Edited (no change to conclusions)
References
References to studies included in this review
Avis 2008 {published and unpublished data}
- Avis NE, Legault C, Coeytaux RR, Pian‐Smith M, Shifren JL, Chen W, et al. A randomized, controlled pilot study of acupuncture treatment for menopausal hot flashes. Journal of the North American Menopause Society 2008;15(6):1070‐8. [DOI] [PubMed] [Google Scholar]
Bokmand 2013 {published data only}
- Bokmand S, Flyger H. Acupuncture relieves menopausal discomfort in breast cancer patients: a prospective, double blinded, randomized study. Breast 2013;22(3):320‐3. [DOI] [PubMed] [Google Scholar]
Borud 2009 {published data only}
- Borud EK, Alraek T, White A, Fonnebo V, Eggen AE, Hammar M, et al. The acupuncture on hot flashes among menopausal women (ACUFLASH) study, a randomized controlled trial. Journal of the North American Menopause Society 2009;16(3):484‐93. [DOI] [PubMed] [Google Scholar]
Deng 2007 {published data only}
- Deng G, Vickers AJ, Yeung KS, D'Andrea GM, Xiao H, Heerdt AS, et al. Randomized, controlled trial of acupuncture for the treatment of hot flashes in breast cancer patients. Journal of Clinical Oncology 2007;23(6):5584‐90. [DOI] [PubMed] [Google Scholar]
Frisk 2008 {published and unpublished data}
- Frisk J, Carlhall S, Kallstrom A‐C, Lindh‐Astrand L, Malmstrom A, Hammar M. Long‐term follow‐up of acupuncture and hormone therapy on hot flushes in women with breast cancer: a prospective, randomized, controlled multicenter trial. Climacteric 2008;11(2):166‐74. [DOI] [PubMed] [Google Scholar]
Hervik 2009 {published and unpublished data}
- Hervik J, Mjåland O. Acupuncture for the treatment of the hot flashes in breast cancer patients, a randomized, controlled trial. Breast Cancer Research and treatment 2009;116(2):311‐6. [DOI] [PubMed] [Google Scholar]
Kim 2010 {published data only}
- Kim KH, Kang KW, Kim DI, Kim HJ, Yoon HM, Lee JM, et al. Effects of acupuncture on hot flushes in perimenopausal and postmenopausal women‐a multicenter randomized clinical trial. Journal of the North American Menopause Society 2010;17(2):269‐80. [DOI] [PubMed] [Google Scholar]
Kim 2011 {published data only}
- Kim DI, Jeong JC, Kim KH, Rho JJ, Choi MS, Yoon SH, et al. Acupuncture for hot flushes in perimenopausal and postmenopausal women: a randomised, sham‐controlled trial. Acupuncture in Medicine 2011;29(4):249‐56. [DOI] [PubMed] [Google Scholar]
Nedstrand 2006 {published data only}
- Nedstrand E, Wyon Y, Hammer M, Wijma K. Psychological well‐being improves in women with breast cancer after treatment with applied relaxation or electro‐acupuncture for vasomotor symptom. Journal of Psychosomatic Obstetrics & Gynecology 2006;27(4):193‐9. [DOI] [PubMed] [Google Scholar]
Nir 2007 {published and unpublished data}
- Nir Y, Huang MI, Schnyer R, Chen B, Manber R. Acupuncture for postmenopausal hot flashes. Maturitas: The European Menopausal Journal 2007;56(4):383‐95. [DOI] [PubMed] [Google Scholar]
Painovich 2012 {published and unpublished data}
- Painovich JM, Shufelt CL, Azziz R, Yang Y, Goodarzi MO, Braunstein GD, et al. A pilot randomized, single‐blind, placebo‐controlled trial of traditional acupuncture for vasomotor symptoms and mechanistic pathways of menopause. Menopause 2012;19(1):54‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2009 {published and unpublished data}
- Park JE, Lee MS, Jung S, Kim A, Kang K, Choi J, et al. Moxibustion for treating menopausal hot flashes: a randomized clinical trial. Journal of the North American Menopause Society 2009;16(4):660‐5. [DOI] [PubMed] [Google Scholar]
Venzke 2010 {published data only}
- Venzke L, Calvert JF Jr, Gilbertson B. A randomized trial of acupuncture for vasomotor symptoms in post‐menopausal women. Complementary Therapies in Medicine 2010;18(2):59‐66. [DOI] [PubMed] [Google Scholar]
Vincent 2007 {published and unpublished data}
- Vincent A, Barton DL, Mandrekar JN, Cha SS, Zais T, Wahner‐Roedler DL, et al. Acupuncture for hot flashes: a randomized, sham‐controlled clinical study. Journal of the North American Menopause Society 2007;14(1):45‐52. [DOI] [PubMed] [Google Scholar]
Wyon 2004 {published and unpublished data}
- Wyon Y, Wilma K, Nedstrand E, Hammar M. A comparison of acupuncture and oral estradiol treatment of vasomotor symptoms in postmenopausal women. Climacteric 2004;7(2):153‐64. [DOI] [PubMed] [Google Scholar]
Zhou 2011 {published data only}
- Zhou J, Qu F, Sang X, Wang X, Nan R. Acupuncture and auricular acupressure in relieving menopausal hot flashes of bilaterally ovariectomized Chinese women: a randomized controlled trial. Evidence‐Based Complementary and Alternative Medicine 2011;2011:713274. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Azizi 2011 {published data only}
- Azizi H, Liu YF, Du L, Wang CH, Bahrami‐Taghanaki H, Esmaily HO, et al. Menopause‐related symptoms: traditional Chinese medicine vs hormone therapy. Alternatives Therapies 2011;17(4):48‐53. [PubMed] [Google Scholar]
Borud 2010 {published data only}
- Borud EK, Alraek T, White A, Grimsgaard S. The acupuncture on hot flashes among menopausal women study: observational follow‐up results at 6 and 12 months. Menopause: The Journal of the North American Menopause Society 2010;17(2):262‐8. [DOI] [PubMed] [Google Scholar]
Castelo Branco 2011 {published data only}
- Castelo Branco de Luca A, Maggio da Fonseca A, Carvalho Lopes CM, Bagnoli VR, Soares JM, Baracat EC. Acupuncture‐ameliorated menopausal symptoms: single‐blind, placebo‐controlled, randomized trial. Climacteric 2011;14:140‐5. [DOI] [PubMed] [Google Scholar]
Cohen 2003 {published data only}
- Cohen SM, Rousseau ME, Carey BL. Can acupuncture ease the symptoms of menopause?. Holistic Nursing Practice 2003;17(6):295‐9. [DOI] [PubMed] [Google Scholar]
Cummins 2000 {published data only}
- Cummins SM, Brunt MA. Does acupuncture influence the vasomotor symptoms experienced by breast cancer patients taking tamoxifen?. Acupuncture in Medicine 2000;18(1):28. [Google Scholar]
Davies 2001 {published data only}
- Davies FM. The effect of acupuncture treatment on the incidence and severity of hot flushes experienced by women following treatment for breast cancer: a comparison of traditional and minimal acupuncture. European Journal of Cancer 2001;37 Suppl 6:S438. [Google Scholar]
De Valois 2003 {published data only}
- Valois B, Young T, Hunter M, Lucey H, Maher HJ. Using traditional acupuncture for hot flushes and night sweats in women taking tamoxifen ‐ a pilot study. Focus on Alternative and Complementary Therapies 2003;8(1):134‐5. [Google Scholar]
De Valois 2010 {published data only}
- Valois BA, Young TE, Robinson N, McCourt C, Maher EJ. Using traditional acupuncture for breast cancer‐related hot flashes and night sweats. Journal of Alternative and Complementary Medicine 2010;16(10):1047‐57. [DOI] [PubMed] [Google Scholar]
Facchinetti 1989 {published data only}
- Facchinetti F, Lanzani A, Nappi G, Pironti T, Genazzani AR. [Mediation opioïdes des effets de l'acupuncture et des techniques derivées dans le traitement des troubles de la ménopause]. Revue Française de Médecine Traditionnelle Chinoise 1989;133:72‐5. [Google Scholar]
Frisk 2012 {published data only}
- Frisk J, Kallstrom AC, Wall N, Fredrikson M, Hammar M. Acupuncture improves health‐related quality‐of‐life (HRQoL) and sleep in women with breast cancer and hot flushes. Support Care Cancer 2012;20(4):715‐24. [DOI] [PubMed] [Google Scholar]
Grilli 1989 {published data only}
- Grilli M, Lamma A, Macchiagodena C, Moroni M, Roncuzzi A, Savorani G, et al. [L'emploi thérapeutique de l'acupuncture dans la ménopause]. La Revue Francaise de Médecine Traditionelle Chinoise 1989;133:65‐6. [Google Scholar]
Guévin 2009 {published data only}
- Guévin F, Lambert B. Acupuncture and menopausal hot flashes. Medical Acupuncture 2009;21(4):243‐5. [Google Scholar]
Gui‐e 2000 {published data only}
- Gui‐e S, Ren‐hai M. Acupuncture treatment of premature ovarian failure: observation of 76 patients. International Journal of Clinical Acupuncture 2000;11(1):11‐4. [Google Scholar]
Harris 2002 {published data only}
- Harris PF, Remington PL, Trentham‐Dietz A, Allen CI, Newcomb PA. Prevalence and treatment of menopausal symptoms among breast cancer survivors. Journal of Pain and Symptom Management 2002;23(6):501‐9. [DOI] [PubMed] [Google Scholar]
Hervik 2010 {published data only}
- Hervik J, Mjaland O. Quality of life of breast cancer patients medicated with anti‐estrogens, 2 years after acupuncture treatment: a qualitative study. International Journal of Women's Health 2010;2:319‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hu 2005 {published data only}
- Hu J. Acupuncture treatment of menopausal syndrome. Journal of traditional Chinese Medicine 2005;25(1):78‐80. [PubMed] [Google Scholar]
Huang 2006 {published data only}
- Huang MI, Nir Y, Chen B, Schnyer R, Manber R. A randomized controlled pilot study of acupuncture for postmenopausal hot flashes: effect on nocturnal hot flashes and sleep quality. Fertility and Sterility 2006;86(3):700‐10. [DOI] [PubMed] [Google Scholar]
Huazhang 2008 {published data only}
- Huazhang T, Chunyan Z. The combined use of acupuncture and Chinese medicines for treatment of menopausal syndrome ‐ a clinical report of 63 cases. Journal of Traditional Chinese Medicine 2008;28(1):3‐4. [DOI] [PubMed] [Google Scholar]
Huo 2004 {published data only}
- Huo ZJ, Zhang WB. Acupuncture treatment of 51 cases of menopausal perspiration. Journal of Acupuncture and Tuina Science 2004;2(4):27‐8. [Google Scholar]
Ji 1998 {published data only}
- Ji P, Ma RH, Wang ZX. Body acupuncture plus ear pressing in the treatment of menopausal syndrome. International Journal of Clinical Acupuncture 1998;9(4):471‐3. [Google Scholar]
Jin 2007 {published data only}
- Jin H, Liu TT, Wang R. Clinical observation on acupuncture at the five‐zangshu for treatment of perimenopausal syndrome. Zhongguo Zhen Jiu 2007;27(8):572‐4. [PubMed] [Google Scholar]
Kao 2012 {published data only}
- Kao CL, Chen CH, Lin WY, Chiao YC, Hsieh CL. Effect of auricular acupressure on peri‐ and early postmenopausal women with anxiety: a double‐blinded, randomized, and controlled pilot study. Evidence‐Based Complementary and Alternative Medicine 2012;2012:567639. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lesi 2012 {published data only}
- Lesi G, Gramenzi A, Garavini CM, Cardini F. Acupuncture in the management of menopausal symptoms in women diagnosed with breast cancer: an uncontrolled experimental pilot study. European Journal of Integrative Medicine 2012;4S:9‐123. [Google Scholar]
Li 2005 {published data only}
- Li P. Influence of auricular points sticking and pressing on the symptoms and serum endocrine hormone of menopausal women. Chinese Journal of Clinical Rehabilitation 2005;9(15):140‐1. [Google Scholar]
Mingling 1991 {published data only}
- Mingling W. 42 cases of climacteric syndrome treated with auricular pellet pressure. Journal of Traditional Chinese Medicine 1991;11(3):196‐8. [PubMed] [Google Scholar]
Nedstrand 2005 {published data only}
- Nedstrand E, Wijma K, Wyon Y, Hammar M. Vasomotor symptoms decrease in women with breast cancer randomized to treatment with applied relaxation or electro‐acupuncture: a preliminary study. Climacteric 2005;8(3):243‐50. [DOI] [PubMed] [Google Scholar]
O'Brien 2010 {published data only}
- O'Brien KA, Varigos E, Black C, Komesaroff PA. Laser acupuncture does not improve menopausal symptoms. Menopause 2010;17(3):636‐41. [DOI] [PubMed] [Google Scholar]
Otte 2011 {published data only}
- Otte JL, Carpenter JS, Zhong X, Johnstone PAS. Feasibility study of acupuncture for reducing sleep disturbances and hot flashes in postmenopausal breast cancer survivors. Clinical Nurse Specialist 2011;Sept‐Oct:228‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perez 2005 {published data only}
- Perez AT, Sear A, Frankel C, Franco SX, Tan‐Chiu E, Gokce F, et al. Acupuncture for the management of hot flashes in women with early stage breast cancer treated with tamoxifen or an aromatase inhibitor: a pilot study of efficacy, safety and feasibility. Journal of Clinical Oncology 2005;23(16S):703. [Google Scholar]
Porzio 2002 {published data only}
- Porzio G, Trapasso T, Martelli S, Sallusti E, Piccone C, Mattei A, et al. Acupuncture in the treatment of menopause‐related symptoms in women taking tamoxifen. Tumori 2002;88(2):128‐30. [DOI] [PubMed] [Google Scholar]
Sandberg 2002 {published data only}
- Sandberg M, Wijma K, Wyon Y, Nedstrand E, Hammar M. Effects of electro‐acupuncture on psychological distress in postmenopausal women. Complementary Therapies in Medicine 2002;10:161‐9. [DOI] [PubMed] [Google Scholar]
Spetz Holm 2012 {published data only}
- Spetz Holm AE, Frisk J, Hammar ML. Acupuncture as treatment of hot flashes and the possible role of calcitonin gene‐related peptide. Evidence‐Based Complementary and Alternative Medicine 2012:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sunay 2011 {published data only}
- Sunay D, Ozdiken M, Arslan H, Seven A, Aral Y. The effect of acupuncture on postmenopausal symptoms and reproductive hormones: a sham controlled clinical trial. Acupuncture in Medicine 2011;29:27‐31. [DOI] [PubMed] [Google Scholar]
Towlerton 1999 {published data only}
- Towlerton G, O'Brien M, Duncan A. Acupuncture in the control of vasomotor symptoms caused by tamoxifen. Palliative Medicine 1999;13:445. [DOI] [PubMed] [Google Scholar]
Tukmachi 2000 {published data only}
- Tukmachi E. Treatment of hot flushes in breast cancer patients with acupuncture. Acupuncture in Medicine 2000;18(1):22‐7. [Google Scholar]
Walker 2007 {published data only}
- Walker G, Valois B, Davies R, Young T, Maher J. Ear acupuncture for hot flushes ‐ the perceptions of women with breast cancer. Complementary Therapies in Clinical Practice 2007;13:250‐7. [DOI] [PubMed] [Google Scholar]
Walker 2008 {published data only}
- Walker EM, Rodriguez AI, Kohn B, Pegg J, Bell RM, Levine RA. Acupuncture for the treatment of vasomotor symptoms in breast cancer patients receiving hormone suppression treatment. International Journal of Radiation Oncology, Biology, Physics 2008;72 Suppl 1:S103. [Google Scholar]
Walker 2010 {published data only}
- Walker EM, Rodriguez AI, Kohn B, Ball RM, Pegg J, Pococl JR, et al. Acupuncture versus venlafaxine for the management of vasomotor symptoms in patients with hormone receptor‐positive breast cancer: a randomized controlled trial. Journal of Clinical Oncology 2010;28(4):634‐40. [DOI] [PubMed] [Google Scholar]
Wyon 1995 {published data only}
- Wyon Y, Lindgren R, Lundeberg T, Hammar M. Effects of acupuncture on climacteric vasomotor symptoms, quality of life, and urinary excretion of neuropeptides among postmenopausal women. Menopause 1995;2(1):3‐12. [Google Scholar]
Xia 2008 {published data only}
- Xia XH, Hu L, Qin ZY, Zhou J, Meng L, Li WL, et al. Multicentral randomized controlled clinical trials about treatment of perimenopausal syndrome with electroacupuncture of sanyinjiao (SP 6). Zhen Ci Yan Jiu 2008;33(4):262‐6. [PubMed] [Google Scholar]
Xiaoming 2005 {published data only}
- Xiaoming S, Yuanhao D, Li Y, Yang X, Hong Y, Guiru H, et al. Acupuncture for treatment of climacteric syndrome ‐ a report of 35 cases. Journal of Traditional Chinese Medicine 2005;25(1):3‐6. [PubMed] [Google Scholar]
Xu 2004 {published data only}
- Xu Z. Nie Ji, Acupuncture and Bushen Yinao capsule in the treatment of 100 women with menopause. Chinese Manipulation & Qi Gong Therapy 2004;20(5):12‐3. [Google Scholar]
Zaborowska 2007 {published data only}
- Zaborowska E, Brynhildsen J, Damberg M, Fredriksson M, Lindh‐Astrand L, Nedstrand E, et al. Effects of acupuncture, applied relaxation, estrogens and placebo on hot flushes in postmenopausal women: an analysis of two prospective, parallel, randomized studies. Climacteric 2007;10(1):38‐45. [DOI] [PubMed] [Google Scholar]
Zhang 2006 {published data only}
- Zhang H. Influence of acupuncture on the clinical manifestation and beta‐endorphin level in female patients with menopausal symptoms. Chinese Journal of Clinical Rehabilitation 2006;10(31):1‐3. [Google Scholar]
Zhenya 2001 {published data only}
- Zhenya J, Changdu L, Li X. Menopausal syndrome treated by cupping along channels: 48 cases. International Journal of Clinical Acupuncture 2001;12(4):363‐4. [Google Scholar]
Zhou 2006 {published data only}
- Zhou J, Qin ZY, Li WL, Zhang CP, Tian LY, Zhang YJ, et al. Clinical observation on therapeutic effect of electroacupuncture at Sanyinjiao (SP 6) on peri‐menopausal syndrome. Zhongguo Zhen Jiu 2006;26(9):617‐20. [PubMed] [Google Scholar]
Additional references
Cabyoglu 2006
- Cabyoglu MT, Ergene N, Tan U. The mechanism of acupuncture and clinical applications. International Journal of Neuroscience 2006;116(2):115‐25. [DOI] [PubMed] [Google Scholar]
Ernst 2006
- Ernst E. Acupuncture ‐ a critical analysis. Journal of Internal Medicine 2006;259(2):125‐37. [DOI] [PubMed] [Google Scholar]
Freeman 2007
- Freeman EW, Sherif K. Prevalence of hot flushes and night sweats around the world: a systematic review. Climacteric 2007;10(3):197‐214. [DOI] [PubMed] [Google Scholar]
Gold 2007
- Gold EB, Bair Y, Zhang G, Utts J, Greendale GA, Upchurch D, et al. Cross‐sectional analysis of specific complementary and alternative medicine (CAM) use by racial/ethnic group and menopausal status: the Study of Women's Health Across the Nation (SWAN). Menopause 2007;14(4):612‐23. [DOI] [PubMed] [Google Scholar]
Greendale 1999
- Greendale GA, Lee NP, Arriola ER. The menopause. Lancet 1999;353:571‐80. [DOI] [PubMed] [Google Scholar]
Guay 2007
- Guay MP, Dragomir A, Pilon D, Moride Y, Perreault S. Changes in pattern of use, clinical characteristics and persistence rate of hormone replacement therapy among postmenopausal women after the WHI publication. Pharmacoepidemiology and Drug Safety 2007;16(1):17‐27. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hilditch 1996
- Hilditch JR, Lewis J, Peter A, Maris B, Ross A, Franssen E, et al. A menopause‐specific quality of life questionnaire: development and psychometric properties. Maturitas 1996;24(3):161‐75. [DOI] [PubMed] [Google Scholar]
Hunter 1992
- Hunter MS. The Women's Health Questionnaire: a measure of mid‐aged women's perceptions of their emotional and physical health. Psychology & Health 1992;7(1):45‐54. [Google Scholar]
Marjoribanks 2012
- Marjoribanks J, Farquhar C, Roberts H, Lethaby A. Long term hormone therapy for perimenopausal and postmenopausal women. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD004143.pub4] [DOI] [PubMed] [Google Scholar]
NAMS 2012
- The North American Menopause Society. The 2012 Hormone Therapy Position Statement of the North American Menopause Society. Menopause 2012;19(3):257‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nappi 1990
- Nappi C, Petralgia F, Gambardella A, Masellis G, Carlo C, Genazzani AR, et al. Relationship between cerebrospinal fluid β‐endorphin and plasma pituitary‐gonadal hormone levels in women. Journal of Endocrinological Investigation 1990;13:149‐53. [DOI] [PubMed] [Google Scholar]
Nasir 2002
- Nasir LS. Acupuncture. Primary Care 2002;29(2):393‐405. [DOI] [PubMed] [Google Scholar]
Newton 2002
- Newton KM, Buist DS, Keenan NL, Anderson LA, LaCroix AZ. Use of alternative therapies for menopause symptoms: results of a population‐based survey. Obstetrics and Gynecology 2002;100(1):18‐25. [DOI] [PubMed] [Google Scholar]
NIH 2005
- National Institutes of Health. NIH State‐of‐the‐Science Conference Statement on management of menopause‐related symptoms. NIH Consensus and State‐of‐the‐Science Statements 2005;22(1):1‐38. [PubMed] [Google Scholar]
Pearl 1999
- Pearl D, Schrollinger E. Acupuncture: its use in medicine. Western Journal of Medicine 1999;171(3):176‐80. [PMC free article] [PubMed] [Google Scholar]
Soules 2001
- Soules MR, Sherman S, Parrott E, Rebar R, Santoro N, Utian W, et al. Executive summary: Stages of Reproductive Aging Workshop (STRAW). Climacteric 2001;4(4):267‐72. [PubMed] [Google Scholar]
Stearns 2002
- Stearns V, Ullmer L, Lopez JF, Smith Y, Isaacs C, Hayes D. Hot flushes. Lancet 2002;360(9348):1851‐61. [DOI] [PubMed] [Google Scholar]
Wathen 2006
- Wathen CN. Alternatives to hormone replacement therapy: a multi‐method study of women's experiences. Complementary Therapies in Medicine 2006;14(3):185‐92. [DOI] [PubMed] [Google Scholar]
Whittaker 2004
- Whittaker P. Laser acupuncture: past, present, and future. Lasers in Medical Science 2004;19(2):69‐80. [DOI] [PubMed] [Google Scholar]


