Abstract
Background
Sexual offending is a serious social problem, a public health issue, and a major challenge for social policy. Victim surveys indicate high incidence and prevalence levels and it is accepted that there is a high proportion of hidden sexual victimisation. Surveys report high levels of psychiatric morbidity in survivors of sexual offences.
Biological treatments of sex offenders include antilibidinal medication, comprising hormonal drugs that have a testosterone‐suppressing effect, and non‐hormonal drugs that affect libido through other mechanisms. The three main classes of testosterone‐suppressing drugs in current use are progestogens, antiandrogens, and gonadotropin‐releasing hormone (GnRH) analogues. Medications that affect libido through other means include antipsychotics and serotonergic antidepressants (SSRIs).
Objectives
To evaluate the effects of pharmacological interventions on target sexual behaviour for people who have been convicted or are at risk of sexual offending.
Search methods
We searched CENTRAL (2014, Issue 7), Ovid MEDLINE, EMBASE, and 15 other databases in July 2014. We also searched two trials registers and requested details of unidentified, unpublished, or ongoing studies from investigators and other experts.
Selection criteria
Prospective controlled trials of antilibidinal medications taken by individuals for the purpose of preventing sexual offences, where the comparator group received a placebo, no treatment, or 'standard care', including psychological treatment.
Data collection and analysis
Pairs of authors, working independently, selected studies, extracted data, and assessed the risk of bias of included studies. We contacted study authors for additional information, including details of methods and outcome data.
Main results
We included seven studies with a total of 138 participants, with data available for 123. Sample sizes ranged from 9 to 37. Judgements for categories of risk of bias varied: concerns were greatest regarding allocation concealment, blinding of outcome assessors, and incomplete outcome data (dropout rates in the five community‐based studies ranged from 3% to 54% and results were usually analysed on a per protocol basis).
Participant characteristics in the seven studies were heterogeneous, but the vast majority had convictions for sexual offences, ranging from exhibitionism to rape and child molestation.
Six studies examined the effectiveness of three testosterone‐suppressing drugs: cyproterone acetate (CPA), ethinyl oestradiol (EO), and medroxyprogesterone acetate (MPA); a seventh evaluated two antipsychotics (benperidol and chlorpromazine). Five studies were placebo‐controlled; in two, MPA was administered as an adjunctive treatment to a psychological therapy (assertiveness training or imaginal desensitisation). Meta‐analysis was not possible due to heterogeneity of interventions, comparators, study designs, and other issues. The quality of the evidence overall was poor. In addition to methodological issues, much evidence was indirect.
Primary outcome: recividism. Two studies reported recidivism rates formally. One trial of intramuscular MPA plus imaginal desensitisation (ID) found no reports of recividism at two‐year follow‐up for the intervention group (n = 10 versus one relapse within the group treated by ID alone). A three‐armed trial of oral MPA, alone or in combination with psychological treatment, reported a 20% rate of recidivism amongst those in the combined treatment arm (n = 15) and 50% of those in the psychological treatment only group (n = 12). Notably, all those in the 'oral MPA only' arm of this study (n = 5) dropped out immediately, despite treatment being court mandated.
Two studies did not report recidivism rates as they both took place in one secure psychiatric facility from which no participant was discharged during the study, whilst another three studies did not appear directly to measure recividism but rather abnormal sexual activity alone.
Secondary outcomes:The included studies report a variety of secondary outcomes. Results suggest that the frequency of self reported deviant sexual fantasies may be reduced by testosterone‐suppressing drugs, but not the deviancy itself (three studies). Where measured, hormonal levels, particularly levels of testosterone, tended to correlate with measures of sexual activity and with anxiety (two studies). One study measured anxiety formally; one study measured anger or aggression.
Adverse events: Six studies provided information on adverse events. No study tested the effects of testosterone‐suppressing drugs beyond six to eight months and the cross‐over design of some studies may obscure matters (given the 'rebound effect' of some hormonal treatments). Considerable weight gain was reported in two trials of oral MPA and CPA. Side effects of intramuscular MPA led to discontinuation in some participants after three to five injections (the nature of these side effects was not described). Notable increases in depression and excess salivation were reported in one trial of oral MPA. The most severe side effects (extra‐pyramidal movement disorders and drowsiness) were reported in a trial of antipsychotic medication for the 12 participants in the study. No deaths or suicide attempts were reported in any study. The latter is important given the association between antilibidinal hormonal medication and mood changes.
Authors' conclusions
We found only seven small trials (all published more than 20 years ago) that examined the effects of a limited number of drugs. Investigators reported issues around acceptance and adherence to treatment. We found no studies of the newer drugs currently in use, particularly SSRIs or GnRH analogues. Although there were some encouraging findings in this review, their limitations do not allow firm conclusions to be drawn regarding pharmacological intervention as an effective intervention for reducing sexual offending.
The tolerability, even of the testosterone‐suppressing drugs, was uncertain given that all studies were small (and therefore underpowered to assess adverse effects) and of limited duration, which is not consistent with current routine clinical practice. Further research is required before it is demonstrated that their administration reduces sexual recidivism and that tolerability is maintained.
It is a concern that, despite treatment being mandated in many jurisdictions, evidence for the effectiveness of pharmacological interventions is so sparse and that no RCTs appear to have been published in two decades. New studies are therefore needed and should include trials with larger sample sizes, of longer duration, evaluating newer medications, and with results stratified according to category of sexual offenders. It is important that data are collected on the characteristics of those who refuse and those who drop out, as well as those who complete treatment.
Keywords: Adolescent; Adult; Aged; Child; Humans; Male; Middle Aged; Androgen Antagonists; Androgen Antagonists/adverse effects; Androgen Antagonists/therapeutic use; Antipsychotic Agents; Antipsychotic Agents/adverse effects; Antipsychotic Agents/therapeutic use; Child Abuse, Sexual; Child Abuse, Sexual/prevention & control; Desensitization, Psychologic; Desensitization, Psychologic/methods; Exhibitionism; Exhibitionism/drug therapy; Exhibitionism/prevention & control; Libido; Libido/drug effects; Randomized Controlled Trials as Topic; Rape; Rape/prevention & control; Recurrence; Sex Offenses; Sex Offenses/prevention & control; Sex Offenses/psychology; Sexual Behavior; Sexual Behavior/drug effects
Plain language summary
Drug treatments for sexual offenders or those at risk of offending
Background
Victim surveys suggest that sexual offending is common, and survivors experience psychological problems. However, much offending goes undetected because of under‐reporting and failure to successfully prosecute offenders.
Medications used to treat sex offenders ('antilibidinal' medications) act by limiting the sexual drive (libido). There are two types, those which work by suppressing testosterone (e.g., progestogens, antiandrogens, and gonadotropin‐releasing hormone (GnRH) analogues), and those that reduce sexual drive by other mechanisms (i.e., antipsychotics and serotonergic antidepressants (SSRIs)).
We reviewed evidence for the effectiveness of such drugs in people who were convicted or thought to be at risk of committing sexual offences.
Search date
The evidence in this review is current to July 2014.
Study characteristics
We found seven randomised trials involving 138 participants, which provided data on 123. All were male, aged between 16 and 68 years. Offending ranged from very serious (e.g., rape) to minor criminality (e.g., exhibitionism). Comparators included placebo (five studies), psychological treatment (one study), and a combination of psychological and pharmacological treatment (one study). Five studies took place in the community and two in a secure hospital. Duration varied between three and 13 months.
Six studies examined the effectiveness of three testosterone‐suppressing drugs: cyproterone acetate (CPA), ethinyl oestradiol (EO), and medroxyprogesterone acetate (MPA). In two of these studies, MPA was given alongside a psychological therapy (assertiveness training or imaginal desensitisation). The seventh study assessed the effectiveness of two antipsychotics (benperidol and chlorpromazine) versus placebo. Meta‐analysis was not possible due to heterogeneity of interventions, comparator groups, study designs, and other issues.
Results
Two studies reported reoffending rates formally. One trial of intramuscular MPA plus imaginal desensitisation (ID) found no reoffending at two‐year follow‐up for the intervention group (n = 10 versus one relapse within the group treated by ID alone). A three‐armed trial of oral MPA, alone or in combination with psychological treatment, reported a 20% rate of reoffending amongst those in the combined treatment arm (n = 15) and 50% of those in the psychological treatment only group (n = 12). Notably, all those in the 'oral MPA only' arm (n = 5) dropped out immediately, despite treatment being court mandated. Two studies did not report reoffending rates as they both took place in a secure psychiatric facility from which none were discharged. Three community studies did not formally report reoffending at all, focusing largely on 'abnormal sexual activity'.
Secondary outcomes: Studies reported a variety of secondary outcomes. Results suggested that the frequency of self reported deviant sexual fantasies may be reduced by testosterone‐suppressing drugs, but not the deviancy itself. Where measured, hormonal levels, particularly levels of testosterone, tended to correlate with measures of sexual activity and anxiety. One study measured anxiety formally; one study measured anger/aggression.
Adverse events: Six studies provided information on adverse events and none tested the effects of testosterone‐suppressing drugs beyond six to eight months. The most severe were reported in a trial of antipsychotic medication. Reported side effects in two trials of oral MPA and CPA included considerable weight gain. Side effects of intramuscular MPA led to discontinuation in some participants. Important increases in depression and excess salivation were reported in one trial of oral MPA. No deaths and no suicide attempts were reported in any study.
We conclude that these seven trials (published more than 20 years ago), examining only a limited number of drugs, provide a poor evidence base to guide practice. Not only were the trials small, they were of short duration, included varied participants, and none trialled the newer drugs currently in use, particularly SSRIs or GnRH analogues. The results of this review, therefore, do not allow firm conclusions to be drawn regarding pharmacological interventions as an effective intervention for reducing sexual offending.
New studies are needed that address these deficits. Data should also be collected on the characteristics of those who refuse, drop out, and complete treatment.
Quality of the evidence
Overall, the quality of the evidence was poor. We had concerns about: number of participants leaving studies, blinding of those who measured outcomes, ways in which investigators concealed allocation of treatment to those delivering it, and reporting of our primary outcome: reoffending.
Background
Description of the condition
Sexual offending is a legal construct which overlaps, but is not necessarily congruent with, the clinical constructs of disorders of sexual preference as described in the ICD‐10 Classification of Mental and Behavioural Disorders (WHO 1992), or paraphilias as described in the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition‐Revised) (APA 1994). Most, but not all, sexual offences are disorders of sexual preference and most, but not all, disorders of sexual preference are sexual offences. For instance, clinically defined sexual behaviours such as paedophilia, voyeurism, frotteurism, exhibitionism, zoophilia, and necrophilia also meet the rubric for sexual offences but, for instance, fetishism and transvestic fetishism do not, in many jurisdictions. Crimes such as rape and incest with consenting adult participants are not of themselves classified as disorders of sexual preference or paraphilias (Grubin 2008).
The true prevalence of sexual offending is unknown. Sexual offending accounts for only 1% of crimes recorded in England and Wales (Eastman 2012). In the US, 9.7% of prisoners have a history of sexual offending (Greenfeld 1997), with a figure of 13.3% reported in Australia (Gelb 2007). These figures are similar to the 10% reported by Taylor et al (Taylor 1998) and Duggan et al (Duggan 2013) for high security and medium security hospitals in the UK. They represent significant underestimates of the extent of the problem as many sexual offences are not reported or, if they are reported, the allegations are often subsequently withdrawn. The true proportion of offenders in custody may be only 0.7% of those responsible for offences (Farrow 2012) ‐ see Figure 1 (Gelb 2007). Surveys and reviews show a high incidence of victimisation (Hood 2002; Edwards 2003; Chapman 2004; Barth 2013; Abrahams 2014), as well as high levels of psychiatric morbidity (McCauley 1997; Hill 2000; Molnar 2001; Swanston 2003; Chapman 2004; Mchichi 2004).
1.
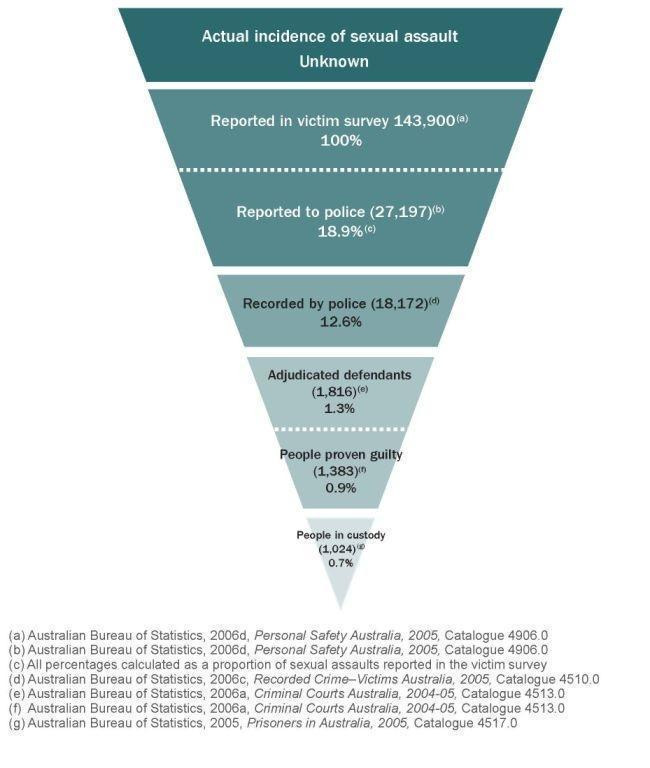
From Gelb 2007 (used with permission of the Sentencing Advisory Council, Melbourne, Victoria, Australia)
Legislative provisions reflect widespread societal concern. For instance, in the UK, provisions in the Sexual Offences Act 2003 include substantial increases in sentence length and state control, in terms of notification requirements and supervision, for up to 10 years after a sentence has been spent (Great Britain 2003). Again, in England and Wales, the Mental Health Act was amended in 2008 so that sexual deviancy was no longer excluded as a criterion for compulsory detention (DOH 2008). In Germany, penal reform in 1998 made the treatment of sexual offenders mandatory for such offenders receiving a prison sentence of more than two years (Lösel 2005). Similarly, the treatment of mentally disordered offenders in the US includes state‐specific sexual predator laws that allow for the preventative detention of those believed to be at high risk of sexually offending in the future. Finally, also in the US, there is Megan's Law, which allows information on registered sex offenders against children to be made available to the community; a similar law is now in force in the UK (AML 2007; Lipscombe 2012). While this concern is understandable, other commentators have argued that exaggerating the danger that sexual offenders pose is problematic as it may increase public fear, and stigmatise and hinder rehabilitation of offenders who have changed their lifestyles, while wasting valuable resources on unnecessary surveillance (Soothill 2000).
Although therecorded pattern of sexual reoffending is relatively infrequent, with reported rates of 13.4% over four to five years' follow‐up (Hanson 1998), long‐term follow‐up studies demonstrate that recividism may persist over a long period, especially for paedophilia (Prentky 1997). This has two significant consequences for the design of trials and their interpretation. First, its low frequency means that the difference between the two trial conditions has to be substantial in order for an effect to be demonstrated. Second, since reoffending can occur many years after release, follow‐up needs to be long‐term in order to capture data from all of those who reoffend.
The literature also recognises that those convicted of a sexual offence are not homogeneous: the most common distinction is drawn between rapists and child molesters, as these are deemed to have different aetiologies, presenting characteristics, and likelihood of reoffending over different time periods (Prentky 1997; Firestone 2000). Another important confounder in the interpretation of trial data is the degree of psychopathy possessed by the sexual offender, as those with high levels are less likely to benefit from treatment and more likely to reoffend (Seto 1999; Hildebrand 2004).
Description of the intervention
A companion review of psychological interventions for those who have sexually offended or are at risk of offending has recently been updated (Kenworthy 2003; Dennis 2012), and it is important to note the underlying difference between the psychological and antilibidinal approaches with which this review is concerned (see below). The objective of psychological interventions is, in general, to change the sexual behaviour of the offender while leaving libido intact, whilst encouraging a change from non‐consensual to consensual sexual activity, with partners of appropriate (legal) age. In contrast, many (although not all) antilibidinal interventions, such as the pharmacological interventions reviewed here, are administered to diminish or altogether eradicate sexual desire and capacity (Abel 2000), either temporarily (to provide a 'window' in which psychological treatments may be attempted) or permanently.
Surgical antilibidinal interventions, such as orchiectomy or orchidectomy (male castration) or neurosurgery, require a separate review.
Medication
Antilibidinal medications broadly fall within two categories, namely those hormonal medications that have a testosterone‐suppressing effect, and non‐hormonal medications that affect libido through other mechanisms.
Hormonal drug therapy
The three main classes of testosterone‐suppressing drugs used today include progestogens, antiandrogens, and gonadotropin‐releasing hormone (GnRH) analogues. Prior to the 1960s, oestrogens were prescribed in North America to treat sexually aggressive men but this practice has been discontinued (Grubin 2008).
The commonly used testosterone‐suppressing drugs include medroxyprogesterone acetate (MPA), cyproterone acetate (CPA), triptorelin, and goserelin.
Non‐hormonal drug therapy
Non‐hormonal drugs that affect libido through means other than via testosterone suppression include antipsychotics and serotonergic antidepressants (SSRI) (Baldwin 2003). Selective serotonin reuptake inhibitors (SSRIs) have been associated with reduced libido and delayed orgasm in 60% to 70% of people taking them (Montejo 2001).
Exact information on rates of administering medication to sexual offenders in practice are limited, as are precise data on the acceptability of treatments. Some data suggest that psychological treatment is considered acceptable by two‐thirds of offenders, but pharmacological treatment only by one‐third (Nagayama‐Hall 1995). Researchers in Germany, concerned at the absence of data for drug use in a clinical context, recently conducted a survey of German forensic‐psychiatric hospitals and outpatient clinics and found that of 611 sex offenders, "almost all were treated psychotherapeutically and 37% were receiving an additional pharmacological treatment" (Turner 2013, p 570). Of the latter, 15.7% were treated with testosterone‐lowering medications (10.6% with a GnRH agonist and 5.1% with CPA); 11.5% with SSRIs, and 9.8% with antipsychotic medications.
How the intervention might work
1.1 Testosterone‐suppressing drugs
Testosterone production in men is controlled by the hypothalamus, anterior pituitary, and the gonads. Gonadotrophin‐releasing hormone (GnRH) is released from the hypothalamus in a pulsatile manner, which stimulates the secretion of the gonadotrophins (luteinising hormone (LH) and follicle‐stimulating hormone (FSH)), from the anterior pituitary. LH acts on Leydig cells in the testes resulting in the production and secretion of testosterone, which, in turn, has a negative feedback effect on the anterior pituitary and hypothalamus.
Testosterone has been linked to sexual development and drive in men (Grubin 2008). Testosterone has both organisational and activational effects on the nervous system. The former is associated with the structural development of the brain and the latter with the effect of testosterone on the organised brain (Sisk 2006). The effect of testosterone on sexual interest and arousal appears to be one of maintaining a level of spontaneous functionality as opposed to being stimulus bound (Bancroft 1989). These effects are not immediate and take several weeks to occur after a change in plasma testosterone levels (Bancroft 2005).
The direct relationship between testosterone and sexual behaviour, however, is confounded by the link between testosterone and aggressive behaviour (Book 2001). In addition, there is evidence that behaviour may itself result in changes in plasma testosterone levels and that testosterone levels may be more closely associated with dominance (Mazur 1980).
GnRH analogues appear to be more effective than CPA and MPA in producing long‐term castration levels of testosterone (McEvoy 1999). However, few studies address the issue of reversibility after long‐term use of greater than two years, bar one small cohort study (Rösler 1998). GnRH analogues and MPA have been shown to produce histological changes, such as reduced Leydig cell numbers, in the testes of animals (Avari 1992; Rao 1998; McEvoy 1999).
All three agents are associated with potential adverse effects (Reilly 2000), such as precipitation or aggravation of cardiac conditions (De Voogt 1986; Pierce 1995), gynaecomastia, weight gain, hot flushes, or depression (Grubin 2008). CPA has been associated with fatal liver toxicity (Parys 1991; Roila 1993). An established consequence of low testosterone is osteoporosis (Stĕpán 1989; Schot 1990), a potentially serious and difficult to manage side effect of testosterone suppression, which is more likely to occur with long‐term use of GnRH agonists.
1.2 Drugs that decrease libido via mechanisms unrelated to testosterone suppression
Although the exact mechanisms are unclear, animal studies suggest that mesolimbic dopamine has an activating effect on sexual arousal and that serotonin has the opposite effect (Hull 2004). In addition, dopamine antagonism may result in prolactin elevation, which may have an effect on libido (Bancroft 2005); such drugs may also positively impact on mental disorders prevalent in this population (e.g., depression, substance misuse, and personality disorder) (Fazal 2006).
Both classes of medication in this category, although widely used, have potentially troublesome side effects. The adverse effects of antipsychotics include tardive dyskinesia (Kane 2006), weight gain (Allison 1997), and impaired glucose tolerance (Haddad 2004).
Selective serotonin reuptake inhibitors (SSRIs) are generally considered to have a more benign side effect profile than other antilibidinal interventions. However, SSRIs are associated with restlessness, agitation, and suicidality, particularly in the under 30 age group (CSM Working Group 2004), and they are also associated with an increased risk of bleeding (Paton 2005).
Why it is important to do this review
Both the prevalence of sexual offending and the association between victimisation and subsequent mental health problems mean that these offences make a significant contribution to mental health morbidity and societal concern more generally. Therefore, there is strong social and political pressure to address this problem, not just in terms of helping the victims but in preventing sexual recidivism (Hanson 2000).
Furby et al, in one of the first major reviews of sex offender recividism, concluded that there was little evidence for any intervention for sex offenders (Furby 1989). This report was criticised by Marshall and Pithers (Marshall 1994), as it contained several flaws, including potential biases against treatment effects, duplication of data, and reliance on outdated programmes. Nagayama‐Hall and colleagues subsequently published a meta‐analysis of 12 of the most recent treatment studies of sexual offenders and found a modest treatment effect for both cognitive behavioural and hormonal treatment, which were both significantly more effective than behavioural therapy but not significantly different from one another (Nagayama‐Hall 1995).
An early Cochrane review looked at all types of interventions for sexual offending (White 1998); it was partially updated in 2003 in a review that considered only psychological interventions (Kenworthy 2003, later updated as Dennis 2012). The older review identified only one small trial (n = 21) that compared antiandrogen medication (MPA) plus a psychological intervention versus the same psychological intervention and identified no significant difference between the two groups (McConaghy 1988). The review authors concluded that there were too few data to come to any conclusion about the effectiveness of MPA.
Adi 2002 reviewed the clinical effectiveness and cost‐consequences of SSRIs in the treatment of sex offenders but identified no RCTs and only nine case series studies with a total of 225 participants. The authors concluded that there were insufficient data of high enough quality to come to any conclusion.
Subsequently, a systematic review by Lösel and Schmucker was produced which, like that by White et al, considered all treatment options for sex offenders but included studies of a larger range of designs (Lösel 2005). They reported a treatment effect size of 3.08 (95% confidence interval (CI) 1.40 to 6.79, P value < 0.01) for antilibidinal medication based on six identified studies. However, the review does not report sample sizes or study designs for pharmacological interventions and the methodologies of the included studies were unclear. Briken and Kafka conducted a literature review of the area, which concluded that medication interventions "show definite promise" (p 609), but deplored the absence of randomised controlled trials and recommended pharmacological treatment be combined with other treatments, including cognitive behavioural therapy and community supervision (Briken 2007).
There is, therefore, an urgent need for an up‐to‐date systematic review.
Objectives
To evaluate the effects of pharmacological interventions on target sexual behaviour for people who have been convicted or are at risk of sexual offending.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials, with or without blinding. We excluded quasi‐randomised trials such as those where allocation was undertaken on surname.
Types of participants
Adults aged 18 years old and over, treated in institutional (prison or psychiatric facility) or community settings for sexual behaviours that have resulted in conviction or caution for sexual offences, offences with a sexual element, or violent behaviours with a sexual element (for example, sexual offences where murder is the index offence), or seeking treatment on a voluntary basis for behaviours that would be classified as illegal.
Defining what constitutes a sexual offence in the context of the international literature can be problematic as definitions of criminally sexual behaviour differ between jurisdiction, cultures, and over time. We decided to include trials of interventions where the participants had committed a sexual offence that would be accepted by most jurisdictions as crimes, viz. penetrative or non‐penetrative sexual acts carried out by adults on non‐consenting adult victims, and penetrative or non‐penetrative sexual acts carried out by adults on consenting or non‐consenting children or adults unable to give informed consent due to their physical or mental disability, or both.
Excluded: Studies of interventions for sex offenders where there was no clear international consensus as to whether the sexual behaviour was a crime or not (although it is possible that in two studies a minority of participants may no longer meet the criteria for being 'at risk' of a crime of a sexual nature (Cooper 1981; McConaghy 1988)). General examples of exclusions include consenting same‐sex acts between adults, consenting sadomasochistic acts, and transvestitism. We also excluded interventions for sex offenders with learning disabilities as this is the subject of a separate Cochrane review (Ashman 2008).
In addition, we excluded studies concerning abnormal sexual behaviour/sexual disinhibition arising from dementia, as this is covered within the scope of the Cochrane Dementia and Cognitive Improvement Group.
Types of interventions
Pharmacological interventions versus placebo or standard care (which might include psychological interventions or no treatment). Where psychological therapy was also a part of treatment, we only analysed comparable therapies within the same comparison.
Types of outcome measures
Primary outcomes
Sexual recidivism as measured by reconviction, self report, or caution (a legal construct valid in the UK and Hong Kong in which an official warning is given by police to someone who has committed a minor offence but has not been charged, to the effect that further action will be taken if they commit another such offence) or by self report.
Secondary outcomes
* Physiological capacity for sexual arousal as measured by phallometric measures (for example, penile plethysmography or PPG); number of reported spontaneous erections; achieved orgasms; circulating levels of hormones, including plasma testosterone).
* Sexually anomalous urges or sexual obsessions ('sexually anomalous' behaviours was a term coined by the late Dr Neil McConaghy to cover "the broad range of sexual paraphilic behaviours including those that attracted criminal penalties...". The term was used to avoid pejorative connotations associated with terms such as 'deviant', 'aberrant' etc.) (Blaszczynski 2011). This measure aims to capture thoughts and behaviours that participants experience as negative, but which do not always result in a formal charge, or urges likely to lead to recidivism. Such urges may be assessed (for example) by diaries or scales of intrusive deviant fantasies.
* Anxiety as measured (for example) by the State‐Trait Anxiety Inventory (STAI) (Spielberger 1983).
* Anger or aggression as measured (for example) by the State‐Trait Anger Expression Inventory‐2 (STAXI‐II) (Spielberger 1999).
Dropping out of treatment.
Adverse events, including suicide or suicide attempts, and sudden or unexpected death, from any cause.
We divided outcomes into immediate (post‐treatment to within six months), short‐term (six months to 24 months), medium‐term (24 months to five years), and long‐term (beyond five years) during the period at risk, for example, post release from prison or discharge from hospital facility. If the participants were receiving treatment in the community then we considered the period at risk as including the period during treatment and also at maximum follow‐up.
* Starred outcomes were added post‐protocol and are justified as follows:
As investigators comment, in some studies, "the population studied is one compulsorily detained" and "although this provides certain advantages, it does mean that there will be no opportunities for the deviant behavior which brought the subjects into hospital" and "therefore, other variables relevant to sexual behavior need to be measured" (p 263) (Tennent 1974).
The rationale for adding the outcomes asterisked above was based on research concerning dynamic risk factors in sex offending. They have also been added to the companion review to this one, which assesses psychological outcomes for sex offenders (Dennis 2012). These changes may be important for sex offenders yet to be released who have little opportunity to reoffend and so should also be reported on (especially those like anxiety and anger, which may particularly be affected by pharmacological action that suppresses testosterone).
In contrast to the review on psychological interventions, we did not include the outcome of 'cognitive distortions' (a dynamic risk factor according to Hanson 2000), as these are not generally targets of pharmacological therapy except when the latter is used to create a 'window' in which psychological therapies may be used within the context of combined modality therapy.
We did add the outcome of "physiological capacity for sexual arousal", as this is an important target of pharmacological rather than psychological treatments (particularly for those with diagnoses of paraphilias).
Appreciating that different investigators were interested in different aspects of physiological arousal in accordance with the hypothesised mechanism of the drug under investigation, we were careful to record intended action as well as results. As one set of investigators note, "Castration itself is not necessarily followed by loss of libido" (Bancroft 1974, p 262), so it may be important to assess physiological arousal (for example, via PPG) in concert with psychological arousal (for example, urges or obsessions).
Search methods for identification of studies
Electronic searches
We ran the first set of searches in July 2008. We updated them in 2010, again in 2013, and most recently in July 2014. We searched the following databases:
Cochrane Central Register of Controlled Trials (CENTRAL 2014, Issue 7), 8 July 2014.
Ovid MEDLINE, 1950 to 8 July 2014.
EMBASE (Ovid), 1980 to 8 July 2014.
AMED ‐ Allied and Complementary Medicine, 1985 to 8 July 2014.
ASSIA ‐ Applied Social Sciences Index and Abstracts (CSA), 1987 to 8 July 2014.
Biosis Previews, 1985 to 9 July 2014.
CINAHL (EBSCO host), 1982 to 9 July 2014.
Copac Academic and National Library Catalogue, last searched January 2008.
IBSS ‐ International Bibliography of the Social Sciences, 1951 to 8 July 2014.
ISI Proceedings, 1990 to 9 July 2014.
ISI‐SCI ‐ Science Citation Index Expanded, 1970 to 9 July 2014.
ISI‐SSCI ‐ Social Sciences Citation Index, 1970 to 9 July 2014.
National Criminal Justice Reference Service Abstracts Database, last searched 10 July 2014.
OpenSIGLE, last searched July 2008.
ProQuest Dissertations and Theses, last searched 8 July 2014.
PsycINFO (Ovid), 1806 to 9 July 2014.
Social Care Online, last searched 9 July 2014.
Sociological Abstracts, 1952 to 9 July 2014.
ZETOC, last searched September 2010.
The OpenSIGLE website was being redesigned at the time of searching in 2010 and the export function was not available; test searches of OpenGrey in 2013 were unproductive and we decided not to run further searches in this database. We searched ZETOC up until 2010, but not for later updates because of the large volume of irrelevant records. Any relevant records were also found in other databases.
In addition, we added searches of two clinical trials registers for this update:
International Clinical Trials Registry Platform (ICTRP; www.who.int/ictrp/en/) (8 July 2014);
Clinicaltrials.gov (http://clinicaltrials.gov/) (8 July 2014).
We used randomised controlled trial filters as appropriate. We applied no restrictions based on language, date, or publication status. See Appendix 1 for the full list of databases and search terms used.
We constructed the electronic searches taking into account the changing terminology and perception of sex offences. We recognise that several of these terms would now be regarded as unacceptable or misleading, or both, as terms signifying sexual offending.
Searching other resources
Handsearching
We searched reference lists of included studies for additional relevant trials along with the reference lists of reviews.
Requests for additional data
We attempted to contact investigators from each included study and we contacted known experts in the field for information regarding unpublished data or ongoing studies, or both. These included Paul Federoff (Canada), Don Grubin (UK), Markus Kruesi (USA), Stephen Hucker (Canada), and Martin Kafka (USA).
Data collection and analysis
Except where indicated in Differences between protocol and review, we followed the methods outlined in the protocol for this review (Khan 2009).
Selection of studies
A minimum of two review authors working in pairs (NH, MF, OK, JD, and MP) independently read and assessed the titles and abstracts of studies identified through searches of electronic databases. Two review authors (NH, MF or JD) then independently assessed full copies of those papers that appeared to meet the inclusion criteria. We resolved uncertainties concerning the appropriateness of studies for inclusion in the review through consultation with a third review author (OK). Review authors were not blinded to the name(s) of the study author(s), their institution(s), or publication sources at any stage of the review.
Data extraction and management
Two authors (MF, NH and/or JD) extracted data independently using a piloted data extraction form. We extracted information on study design and implementation, setting, sample characteristics, intervention characteristics, and outcomes from all included studies. NH, JD, and/or OK entered data into Review Manager 5 (RevMan) software (Review Manager 2014). Where data were not available in the published trial reports, we contacted the authors and asked them to supply the missing information.
Assessment of risk of bias in included studies
For each included study, two review authors (MF, NH, and/or JD) independently completed The Cochrane Collaboration's tool for assessing risk of bias (Higgins 2011a). This required authors to assess the degree to which:
the allocation sequence was adequately generated ('sequence generation');
the allocation was adequately concealed ('allocation concealment');
knowledge of the allocated interventions was adequately prevented during the study ('blinding');
incomplete outcome data were adequately addressed;
reports of the study were free of suggestion of selective outcome reporting.
We made assessments for each domain as 'low', 'unclear', or 'high' risk of bias.
Sequence generation
We determined whether studies used computer‐generated random numbers, table of random numbers, drawing lots or envelopes, coin tossing, shuffling cards, or throwing dice.
Low risk: the study authors explicitly stated that they used one of the above methods.
High risk: the authors did not use any of the above methods.
Unclear: there is no information on the randomisation method or it is not clearly presented.
Allocation concealment
We evaluated whether investigators and participants could foresee assignments before screening was complete and consent was given.
Low risk: researchers and participants were unaware of future allocation to treatment conditions.
High risk: allocation was either not used or was not concealed from researchers before eligibility was determined or from participants before consent was given.
Unclear: information regarding allocation concealment is not known or not clearly presented.
Blinding of participants and personnel
Low risk: participants and personnel were blinded to the treatment conditions.
High risk: there is doubt about the placebo control via differences in appearance, mode of administration etc.
Unclear: information on the blinding of participants is unclear or unavailable from study authors.
Blinding of outcome assessment
Low risk: assessors were blinded to the treatment conditions.
High risk: assessors were not blinded to the treatment conditions.
Unclear: information on the blinding of assessors is unclear or unavailable from study authors.
Incomplete outcome data
Low risk: no participants dropped out or were excluded from treatment; there are some missing data but the reasons for missing data are unlikely to be related to the true outcome; or missing data are balanced in proportion across intervention groups, with similar reasons for missing data across groups.
High risk: there is differential attrition across groups; reasons for dropping out of treatment are different across groups; there was inappropriate application of simple imputation.
Unclear: the attrition rate is unclear or the authors state that intention‐to‐treat (ITT) analysis was used but provide no details.
Selective reporting bias
To assess outcome reporting bias, we attempted to collect all study reports (and protocols, where possible) and tracked the collection and reporting of outcome measures across all available reports within each included study.
Low risk: a protocol is available and all outcome measures and follow‐ups are reported; or, a study protocol is not available but it seems clear that the published report included all expected outcomes, including those that were pre‐specified.
High risk: data from some outcome measures are reported partially (e.g., means but no standard deviations (SD)) or without numerical data and only as 'ns' (non‐significant) or not at all.
Unclear risk: it is not clear whether all data collected by study authors were reported.
Other sources of bias
To assess other sources of bias not detailed above, we scanned all reports of included studies to attempt to ascertain whether other factors (either within or outside the control of investigators) might have introduced bias. These might have included (for example) the nature of recruitment procedures, the source of funding for the trial, changes to definitions of offending over time, etc. We supplied ratings as follows for each study:
Low risk: no issues likely to bias the results of the trial (apart from those elsewhere dealt with within the 'Risk of bias' tool) were identified;
High risk: issues likely to bias the results of the trial identified and judged serious; and
Unclear risk: it is not clear whether relevant issues identified as being likely to bias the trial did in fact do so (or if so, in what direction the bias was likely to be directed).
Measures of treatment effect
All primary outcomes and (originally) all secondary outcomes were dichotomous and we planned to use the risk ratio (RR) with a 95% confidence interval (CI) to summarise results within each study. Some secondary outcomes introduced post‐protocol have been reported as continuous outcomes. Whilst no meta‐analysis has been possible in this review, we plan at update to report these as mean differences with a 95% CI. Where different scales measure the same outcome, we will calculate standardised mean differences (SMDs).
We planned comparisons for specific follow‐up periods:
within the first six months;
between six and 24 months;
between 24 months and five years;
beyond five years.
Unit of analysis issues
Cross‐over trials
The method planned at protocol stage was to use data from any cross‐over trials as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), using approximated paired analysis by imputing missing standard deviations and with due attention to other recommendations in section 16.4 (Higgins 2011b).
Multiple treatment arms
In the protocol originally produced for this review we neglected to state our plans for handling studies in which more than one eligible treatment was compared with control. Whilst this does not affect the current results, for future updates we plan to treat such studies as follows:
a) in the event that two or more intervention arms test treatments that would (if employed against similar controls in separate trials) be amenable to combining in a meta‐analysis within our review, then we will pool data from both eligible arms against control. An example of such a study might be one in which different dosages of a drug were compared against placebo;
b) if, in contrast, trials compare two eligible interventions with an eligible control but the former are not sufficiently similar that they merit pooling (for example, should a SSRI be trialled alongside a GnRH agonist against a shared control), we will treat the study as two studies and divide the data from the control group in half (so as to avoid double counting of control group participant data).
We will transparently document all decisions made in regard to such studies.
Dealing with missing data
We assessed missing data and the number of participants that dropped out of treatment for each included study and reported the number of participants who were included in the final analysis as a proportion of all randomised participants in each study. We provided reasons, where known, for missing data in the narrative summary, as well as details of the investigators' use of intention‐to‐treat (ITT) analysis (where applicable).
Assessment of heterogeneity
We did not undertake a meta‐analysis because of the heterogeneity of interventions and outcome measures used, and because of concerns regarding carry‐over effects from some cross‐over studies, especially Bradford 1993.
Plans for assessing statistical consistency of results of any meta‐analysis in future updates can be found in Appendix 2; clinical heterogeneity within the present review is described in detail in the following sections: Description of studies, Effects of interventions, and in the Discussion.
Assessment of reporting biases
We identified insufficient comparable trials for funnel plots to be feasible for this version of the review. See Appendix 2.
Data synthesis
We originally planned to synthesise data using both a fixed‐effect and a random‐effects model. In the event, no meta‐analysis was possible and all results are reported narratively below.
See Appendix 2 for plans for data synthesis for future versions of the review.
Subgroup analysis and investigation of heterogeneity
We identified insufficient comparable trials for subgroup analysis to be possible for this version of the review. See Appendix 2.
Sensitivity analysis
We identified insufficient comparable trials for sensitivity analysis to be possible for this version of the review. See Appendix 2.
Results
Description of studies
See also Characteristics of included studies.
Results of the search
We performed electronic searches over four consecutive time periods (2008, 2010, 2013, and July 2014). Searches were not restricted to pharmacological interventions, but included terms relevant to the companion review on psychological interventions for the same population (Dennis 2012). Due to the degree of overlap between these searches, and the fact that fewer studies related to pharmacological treatment than to psychological treatment, we judge it uninformative to produce a flowchart of selection, but report data narratively.
Searches to 2008 yielded 26,197 records (of which we examined 343 in full text).
Searches from September 2008 to October 2010 produced 10,507 records, of which we examined 53 in full text.
Searches run in June 2013, covering the period of 2010 to June 2013, resulted in 6228 records, of which we assessed nine in full text. From these 405 records, we extracted data on eight studies; we excluded one study following clarification from the author regarding lack of a placebo control (Kruesi 1992).
Searches run in July 2014, covering the period of June 2013 to 8‐9 July 2014, resulted in 4242 records, of which we assessed 10 in full text. No new studies were included but we added three new excluded studies (Excluded studies).
As far back as 2012, investigators indicated to us that they had heard that a plan for a randomised controlled trial of a newer medication (triptorelin), a GnRH agonist, was being proposed by Peer Briken and colleagues, but our investigations of the same bore no fruit. Early in 2014 we identified a study protocol for this trial (Briken 2012), whilst the reference remained 'in process' within MEDLINE. We anticipate incorporating its results into the first update of this review.
Included studies
Design
All seven included studies were published between 1974 and 1993.
All studies are described as randomised controlled trials. Four out of seven employed a cross‐over design (Bancroft 1974; Tennent 1974; Cooper 1981; Bradford 1993); three studies used a parallel design with no cross‐over (Langevin 1979; Hucker 1988; McConaghy 1988). Two early studies conducted in the same setting used 'Williams squares' or 'Latin squares' as part of their design (Bancroft 1974; Tennent 1974).
Four trials used a single comparison (Langevin 1979; Cooper 1981; Hucker 1988; Bradford 1993), whilst the other three trials each involved three conditions or 'arms' (Bancroft 1974; Tennent 1974; McConaghy 1988).
No study used clustering or reported stratification or matching of participants by type of offence, age, or any other participant characteristic.
Sample sizes
The total number of participants randomised in the seven included studies was 138. The number randomised to eligible arms within the studies was 123. The difference between the two figures can be accounted for by the subtraction of participants from one ineligible active treatment arm from each of two three‐armed trials, McConaghy 1988 (n = 10) and Langevin 1979 (n = 5) (see also Characteristics of included studies).
Overall sample sizes were small, varying from nine (Cooper 1981) to 37 (Langevin 1979). No study included a reference to any power calculation for change within this population.
Setting and recruitment
Location
All studies were conducted in high‐income countries, largely English speaking, whether in the UK (Bancroft 1974; Tennent 1974), Canada (Langevin 1979; Cooper 1981; Hucker 1988; Bradford 1993), or Australia (McConaghy 1988). We identified no study conducted in the USA. This is in contrast to Dennis 2012 (a companion review with data from over 1000 participants in trials assessing the effects of psychological interventions on sex offenders) where five of the 10 included studies were conducted in the USA.
Two studies, conducted in England by the same team of researchers (Bancroft 1974; Tennent 1974), recruited from within a high security psychiatric hospital. Investigators in all other studies recruited male sex offenders or those with paraphilias who were receiving outpatient treatment, the majority of whom had already committed offences or had reported 'anomalous urges' likely to result in contact with law enforcement agencies, or both.
Participants in some studies volunteered themselves for treatment after serving time in prison for offences. Other studies, for example, Cooper 1981, included a mix of referrals, including court referrals of participants awaiting trial but not yet convicted of offences; here, those who were offered treatment were told that "compliance in no way implied a more lenient judicial outcome" (p 460). Participants who were already incarcerated were told that their participation would not influence their release from hospital, although if the drug were to be found effective, it might be helpful for them on their release (Bancroft 1974; Tennent 1974). Hucker and colleagues recruited participants with a history of sex crimes against children, all of whom had been instructed to engage in some form of treatment as a condition of their probation (Hucker 1988); these investigators made particular efforts to record baseline data on those offered treatment within their trial (n = 48) who declined to participate as well as data for those who consented.
Participants
Gender, age, and ethnicity
Whilst the capacity of women to commit sexual offences is recognised, the majority of sex offenders are male and all participants in the included studies were male.
Participant age ranged from 16 to 68 years. Mean age varied from 26.08 (standard deviation (SD) = 3.87) (Bancroft 1974) to 43.11 (SD = 12.14) (Cooper 1981). The largest study in the review (Langevin 1979, N = 37) included no data on age.
Ethnicity of participants was not reported in any study.
Baseline characteristics of participants
Participant characteristics in the seven included studies were heterogeneous, but were clearly reported in terms of offences committed, type of paraphilia (where relevant), and other details of the presenting clinical problem.
Authors of the two British studies provided clear details of the time participants had spent in a secure hospital, their most recent offences (for example, from indecent exposure to rape to 'manslaughter with a sexual element') and the overall number of offences (Bancroft 1974; Tennent 1974). Unsurprisingly, given their setting, these two trials included uniformly 'severe' offenders.
Hucker 1988 included only those with a primary attraction to, and a history of offences against, children. Bradford 1993 included a 'mixed' group and reported on the nature of sexual deviation (for example, paedophilia and whether homosexual or heterosexual, and number of convictions).
Investigators involved in the Langevin 1979 study included, by comparison, less severe offenders (exhibitionists in the main, with some presenting with prominent voyeurism). The small study (n = 9) undertaken by Cooper et al provided sufficient details to make it clear that investigators had recruited two participants who would not meet the inclusion criteria for this review (hypersexuality and homosexuality but with no reported paedophilic interest) (Cooper 1981). McConaghy et al described the offending behaviour and Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM‐III) (APA 1980) paraphilia status of participants in their study (McConaghy 1988), some of whom also might not meet contemporary criteria for offending.
Other demographic information is reported well in only two studies. Data on IQ scores, education, alcohol, and drug use were reported in Hucker 1988; data on marital status, literacy, IQ scores, brain damage, and mental illness (schizophrenia) were reported in McConaghy 1988.
Overall (perhaps not surprisingly given the nature of the intervention), participants in studies included within this review were more likely to be in psychiatric care (within or outside the penal system) and more likely to have a diagnosis of a paraphilia than those in the companion review on psychological treatments for this population (Dennis 2012).
Exclusion criteria
Four of the included trials did not report exclusion criteria. Exclusion criteria listed by Hucker 1988, McConaghy 1988, and Bradford 1993 included having any medical conditions that would contraindicate participation, active psychosis, and an extensive list of medical and psychiatric conditions (from heart disease, cancer and sickle cell anaemia to severe depression), respectively.
Characteristics of interventions
Most interventions studied fell into the category of testosterone‐suppressing drugs involving progestogens or antiandrogens; only one small study assessed antipsychotics (Tennent 1974).
Testosterone‐suppressing drugs
Bancroft 1974 compared ethinyl oestradiol (EO) with cyproterone acetate (CPA) (both testosterone‐suppressing drugs) versus placebo; Bradford 1993 and Cooper 1981 compared cyproterone acetate (CPA) with placebo; Hucker 1988 compared medroxyprogesterone acetate (MPA, delivered orally) with placebo; McConaghy 1988 compared medroxyprogesterone (MPA, intramuscular) with imaginal desensitisation versus imaginal desensitisation alone. Langevin 1979 compared assertiveness training with MPA (orally) versus assertiveness training alone.
We identified no study assessing the effects of serotonergic antidepressants (SSRIs) or gonadotropin‐releasing hormone (GnRH) analogues.
Trials of antilibidinal medications ('other')
Tennent 1974 compared benperidol with chlorpromazine (both antipsychotics) and placebo.
Outcomes
Sexual recidivism Only two studies formally measured recividism by reports of being charged for sexual offences (Langevin 1979; McConaghy 1988).
Two studies were both conducted in a high security facility from which participants were not due to be released for some years, if ever (Bancroft 1974; Tennent 1974). Recividism data therefore could not be collected. Recividism data were also not reported in Hucker 1988, where all participants undertook treatment as a condition of probation.
In two studies, it was unclear whether "sexual activity" or "abnormal sexual activity" was of a criminal nature and therefore recividism cannot be said to be formally assessed (Cooper 1981; Bradford 1993).
Physiological capacity for sexual arousal
Capacity for sexual arousal was assessed by phallometric measures (for example, penile plethysmography or PPG); number of reported spontaneous erections; achieved orgasms; and circulating levels of hormones, including plasma testosterone.
Bancroft 1974 and Tennent 1974 both used an overall "sexual activity score" derived from self reported data on the number of times that masturbation or "any overt sexual acts" led to orgasm; penile erection whilst watching erotic stimuli (film clips) was also measured in mm by means of a "mercury‐in‐rubber gauge" (Bancroft 1966; Bancroft 1971); the latter measure was also used by Bradford 1993 when assessing arousal in participants exposed to erotic stimuli during the course of a slideshow.
Participants involved in three studies were asked to provide data on numbers of spontaneous erections, sexual outlets, and activity during the course of the trials (Cooper 1981; Hucker 1988; Bradford 1993).
Physical capacity per se was not formally assessed in either Langevin 1979 or McConaghy 1988.
Sexually anomalous urges or sexual obsessions
These were measured variously as follows:
The "sexual attitude score" (a "semantic differential technique" (Marks 1967)) uses four seven‐point scales. Here, a low number indicates positive interest and a high number indicates that the participant finds the stimulus "repulsive". This scale was the most common, used by investigators involved in two studies (Bancroft 1974; Tennent 1974).
Cooper 1981 reported self report scores of sexual interest; whilst, in another trial, frequency of sexual fantasies were subdivided into those about adults and those about children (Hucker 1988).
Data were collected on "sexually anomalous urges" as defined above by McConaghy 1988.
Sexual arousal, as recorded by self report and rating scales in response to exposure to erotic stimuli via a slideshow, were recorded in one trial (Bradford 1993).
Anxiety
Anxiety was measured formally (Spielberger 1983) in just one study (McConaghy 1988). "Feelings of anxiety" were measured (in an unvalidated way) in one study (Bradford 1993). The 'calming' effects of interventions were reported anecdotally in two studies (Cooper 1981; Hucker 1988).
Anger or aggression
Anger was measured formally in only one included study (Bradford 1993), using the Buss‐Durkee Hostility Inventory (BDHI) (Buss 1957). As above, the 'calming' effects of interventions were reported anecdotally in two studies (Cooper 1981; Hucker 1988).
Dropping out of treatment
All included studies reported data on dropping out of treatment; all investigators reported reasons for the same.
Adverse events
All included studies sought reports of adverse events.
Excluded studies
We formally excluded 50 studies from this review (reasons are given in the Characteristics of excluded studies table). Two relevant RCTs (one planned in Norway, the other in France) appear to have been terminated within the last decade (NCT00379626 and NCT00601276, respectively).
Risk of bias in included studies
See also Characteristics of included studies and Figure 2.
2.
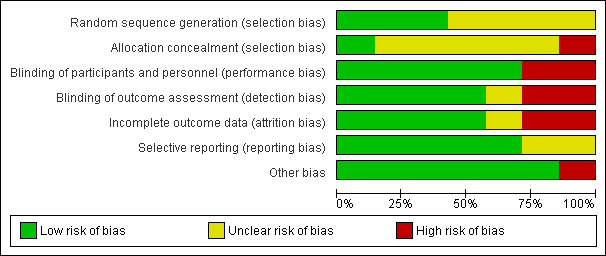
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
Sequence generation
With the exception of Bancroft 1974 and Tennent 1974, who used Williams square designs, no study authors described their methods of randomisation; however, personal communication with an author from McConaghy 1988 provided information that clarified the method of randomisation (Blaszczynski 2011), and in these three cases, we have assessed the risk of bias for this criterion to be low. In the four remaining cases, we judged the adequacy of sequence generation in the review to be unclear (even after communication with one author, Hucker 1988).
Allocation concealment
The method of allocation concealment was not reported in any study included within this review; however personal communications with one author, Hucker 1988, caused us to reassess the risk of bias as low (as the investigator recalled remote assignment made by the pharmacist involved). In contrast, personal communication with an author involved in McConaghy 1988 led to an assessment of 'high' risk of bias for one study, as it was confirmed that no method of concealment was employed. We assessed the remaining five studies as unclear.
Blinding
Participants and personnel
Care in blinding treating staff and participants by means of an off‐site pharmacist using coded bottles of identical intervention and placebo pills was clearly reported in the two oldest studies in the review (Bancroft 1974; Tennent 1974); we therefore assessed these and Bradford 1993 (wherein staff are described as "blinded to allocation") as at low risk of bias. Cooper 1981 reported using a placebo pill (described as "identical" to the active intervention), which would guarantee blinding of participants; we assessed the risk of bias of this study and of Hucker 1988 within the context of this review as 'low'.
We assessed McConaghy 1988 as being at high risk of bias as the conduct of one component of the intervention (imaginal desensitisation) could not be 'blinded' to anyone involved in the study. We assessed Langevin 1979 as being at high risk of bias for the same reason (the intervention common to both arms of the trial was assertiveness training).
Outcome assessors
We assessed three studies as having an overall low risk of bias given the measures taken to blind staff or assessors to group allocation (Bancroft 1974; Tennent 1974; Hucker 1988).
We assessed two studies as having an unclear risk due to lack of information (Langevin 1979), or changes to study protocol based on participants being allowed to change treatment phase (Bradford 1993).
We rated the sixth study as having a high risk of bias as the measures of interest to this review were collected by self report only (Cooper 1981). We also assessed the remaining study, McConaghy 1988, as having a high risk of bias (in contrast to previous work by the same authors, McConaghy 1985) because no attempt was made to blind outcome assessors.
Incomplete outcome data
Incomplete outcome data are a limitation in this review. In one study, Bancroft 1974 (n = 12), no data appeared to be missing (perhaps not surprising in a study of only 12 participants in a secure setting); however, it transpired that one that dropped out during the CPA phase was "replaced" by another participant. Within a similar study conducted in the same setting (Tennent 1974), it is unclear which phases of the study saw the loss of three participants who withdrew or were withdrawn early in the study (for depression or other reasons). New participants were brought in to replace those that dropped out so that outcome data appear for 12 participants, but not those who were recruited. In Bradford 1993, we assessed the risk of bias as 'low' as reasons were supplied for the two participants who left (as well as details of their further conduct).
Attempts to compensate for missing data appear to have been made in two studies, but with varying levels of clarity. In Cooper 1981, the authors reported that to compensate for missing data, appropriate corrections were made, and analysis of variance carried out. For McConaghy 1988, a study in which a high level of dropout in the two drug intervention arms is reported (25% ‐ five of 20 ‐ did not complete their course of medication), the method of dealing with incomplete data is not given for all outcomes although results for all participants appear to be reported.
We have assessed two studies as at 'high' risk of bias for this criterion (Langevin 1979; Hucker 1988), given that the former featured a dropout rate of 67% in the combined treatment arm and 29% in that involving a psychological treatment alone. The study conducted by Hucker et al excluded data from one participant who had a 'medical condition' then lost a further four (almost 25% of the full sample) "of their own accord"; it transpired that these men had "higher frequency of fantasies about children" (p 234); the investigators themselves were unsure whether this might represent "selection bias" of a higher risk group unwilling or unable to give up fantasies about children (Hucker 1988), thus leaving the remaining data at risk of bias.
Selective reporting
Whilst we do not have access to any of the trial protocols for studies included within this review (which were largely conducted and reported in the 1970s and 1980s), we have identified no internal evidence of selective reporting in any paper, nor are any obvious outcomes missing. Testosterone data are missing from one study (Langevin 1979), but this may have been an artefact of measurement issues (data were described as "erratic"). Standard deviations are missing from some measures from another paper (McConaghy 1988), but there is no reason to suspect these were suppressed; data appear to have been lost (Blaszczynski 2011).
Other potential sources of bias
Two potential sources of bias other than those recorded above have been identified. The first was beyond the control of all researchers conducting trials where treatments are not mandated, and that is the phenomenon of those unwilling to participate in treatment at all. Hucker et al remarked that "a key question that is seldom addressed by researchers administering sex drive reducing drugs to sex offenders is the extent to which these drugs are accepted by patients" (Hucker 1988, p 229). As "those participating in a treatment trial are already a select group....", Hucker et al emphasised the need for trialists to consider "a count of all cases approached" [emphasis added]. Such information was not always clear in the studies included within this review. In their own trial, Hucker et al noted that of 100 consecutively referred cases, only 48 were "prepared to complete a comprehensive assessment, consider treatment, or even admit they might have a problem of sexual attraction toward children.... Of these 48, only 18 were willing to participate in a three month double blind trial of MPA versus placebo" (p 231).
In the trial conducted by Bradford and colleagues, authors admit in the discussion that "the placebo phase in this study is not a truly inactive phase nor pharmacologically comparable to the baseline phase" (p 396).
Effects of interventions
We did not undertake meta‐analysis for reasons of heterogeneity of different types, which we summarise briefly here.
Heterogeneity of interventions (results from different drug classes e.g., antilibidinals and antipsychotics must not be combined, as they have entirely different mechanisms of action, side effect profiles, etc.). Results of particular drugs within classes are not always comparable, e.g., ethinyl oestradiol (EO), cyproterone acetate (CPA), and medroxyprogesterone acetate (MPA) due to differing side effect profiles and other issues (the use of MPA is now virtually abandoned in many areas except as a female contraceptive).
Even when interventions were identical, we had concerns regarding differing length of treatment regimes and carry‐over effects from cross‐over studies, especially between Cooper 1981 (where CPA was administered in a 20‐week cross‐over trial with four‐week periods of prescription or four weeks' placebo) and Bradford 1993, where treatment lasted more than a year and was delivered in blocks of 12‐week prescription or 12‐week placebo, compromised (as the investigator admits) by participants being likely to have even more extended periods on the drug if they complained about intrusive thoughts) to the extent that the "placebo phase was not a true placebo phase" (Bradford 1993).
Difference in outcome measures or dropout rates or adequacy of data to calculate effect sizes. Whilst some trials are superficially similar (Langevin 1979 and McConaghy 1988 feature MPA plus psychological treatment versus psychological treatment alone), the former trial reports few real data for analysis due to catastrophic dropout (100% of the MPA arm of the trial, 29% of the psychological treatment arm, and 67% of the combined treatment arm left the study). Finally, one might hope data from the latter trial, McConaghy 1988, might be comparable to data within the trial conducted by Hucker (Hucker 1988), but the former provided no standard deviations (SDs) for any of the means provided for continuous data (and data have since been destroyed). These trials moreover have no dichotomous data (e.g., recividism) in common.
Results are therefore reported narratively; first for antilibidinal medications involving testosterone‐suppressing drugs, then for 'other' antilibidinal medications.
1. Trials of antilibidinal medications involving antiandrogens (testosterone‐suppressing drugs) (six studies)
Six studies assessed the impact of testosterone‐suppressing drugs (Bancroft 1974; Langevin 1979; Cooper 1981; Hucker 1988; McConaghy 1988; Bradford 1993).
a) Ethinyl oestradiol to cyproterone acetate (both testosterone‐suppressing drugs) versus no treatment (one study)
Bancroft 1974 reported on 12 patients within a high security institutional setting using a cross‐over design involving six‐week periods of no treatment, ethinyl oestradiol 0.01 mg (twice daily), and cyproterone acetate (CPA) 50 mg (twice daily). Investigators claim no carry‐over effects were evident in their analysis of residual effects, and concluded that "there were no significant differences between the two drugs on any measure" (p 312).
For some outcomes, treatment was not superior to no treatment. Whilst "sexual attitudes" (deviant urges) appeared unaffected by treatment, physiological capacity could be affected.
Primary outcome
Sexual recidivism as measured by reconviction, self report, or caution
Not reported within this study.
Secondary outcomes
Physiological capacity for sexual arousal
A "sexual activity score" was derived from data given by each participant on the number of times that masturbation or "any overt sexual acts" led to orgasm (p 310); penile erection whilst watching erotic stimuli (film clips) was also measured in millimetres by means of a "mercury‐in‐rubber gauge". For "sexual interest", means for all participants (n = 12) during the ethinyl oestradiol phase were 1.58 (SD = 0.84), compared with a mean of 1.67 (SD = 0.61) in the CPA phase, and a mean of 2.9 (SD = 0.89) in the no treatment phase (trial investigators' analysis: F = 9.44; df = 2.22; P value < 0.001). Both drugs were reported to decrease sexual activity significantly in comparison with placebo. However, phallometric data (erectile responses to fantasy, slides, and film) did not demonstrate a statistically significant effect between treatments, with CPA only mildly superior to no treatment and ethinyl oestradiol not significantly different from no treatment.
Sexually anomalous urges or sexual obsessions
The trial investigators report that "When compared with no treatment... sexual attitudes were not significantly altered" (p 312). During the ethinyl oestradiol phase, mean 'sexual attitude' scores were 9.68 (SD = 4.25), compared with a mean of 10.28 (SD = 5.25) in the CPA phase and 7.24 (SD = 3.49) in the no treatment phase (investigators' analysis: F = 1.91; df = 2.22; P value = not significant (NS)).
Anxiety; anger or aggression
No data were reported for these outcomes.
Dropping out of treatment
One participant was removed before completion of the study because of depression whilst in the CPA treatment phase. Trial investigators reported that his depression was unlikely to have been due to the treatment and that "another patient . . . replaced" him (p 313).
Adverse events, including suicide or suicide attempts, and sudden or unexpected death, from any cause
No side effects attributable to the drugs were reported by the investigators. One participant was withdrawn three days after starting CPA having become depressed (see above) but this was not considered to be related to the intervention.
b) Cyproterone acetate with placebo (two studies)
Bradford 1993 recruited 19 outpatients (volunteers) who fulfilled the Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM‐III‐R) criteria for paraphilia for at least 12 months, and had been charged with a related criminal offence (APA 1987). The study used a cross‐over design with a one‐month baseline phase, followed by four three‐month periods of alternating cyproterone acetate (50 mg to 200 mg per day) or placebo for a total of 13 months. Investigators concluded that CPA was "an effective agent when compared to placebo in controlling important aspects of sexual activity" (Bradford 1993, p 400), albeit with caveats concerning aspects of the cross‐over design employed. These included concerns about a potential "rebound effect" following the placebo phase of treatment, and the fact that some participants were moved on to the active phase of treatment if they experienced concerns about their own sexual impulses.
Cooper 1981, in a community study, recruited nine participants. Seven of these men were described as presenting with severe sexual acting out resulting in social and legal implications, some of whom were facing trial. There is some concern that the remaining two participants might not meet the criteria for this review, as one was included on the basis of "excessive demands on his wife" (p 459) and the other was recruited due to homosexuality, without paedophilic interest. Participants were randomised in a cross‐over design as follows: no treatment, placebo, or cyproterone acetate 50 mg, twice daily; or no treatment, placebo, and then CPA, in four‐week phases. The trial investigators concluded that CPA was effective in reducing libido and associated sexual behaviour to "acceptable levels" (p 463).
We judged meta‐analysis to be inappropriate because of differences in treatment length (treatment phases varied between four and 12 weeks), and inclusion criteria (Cooper's sample being demonstrably less 'severe' than Bradford's). A further limitation, acknowledged by the latter trial investigators, was that "the placebo phase in this study is not a truly inactive phase nor pharmacologically comparable to the baseline phase" (Bradford 1993, p 396). This was related to the fact that inequalities in treatment dosage and duration will have been introduced in the Bradford study, as "if the patient complained that sexual fantasies were returning or they were concerned they might reoffend they were moved ahead to the start of the next three month phase as it was possible that their complaints were due to placebo".
Primary outcome
Sexual recidivism as measured by reconviction, self report, or caution
In the study conducted by Bradford et al, recividism data are not reported specifically, although reference is made to two study participants who had apparently "showed and reported excellent treatment responses to CPA" (p 399) but dropped out because they felt they no longer required treatment. Within six months, one participant committed a "minor homosexual pedophilic act" for which he was charged (Bradford 1993). One may infer no other charges took place during the course of the study, but this outcome does not appear to have been systematically assessed.
Cooper et al do not describe asking about recidivism via self report when assessing sexual activity (recorded as a simple count of episodes rather than subdivided by type or character); therefore it is assumed no data are available for this outcome from this study (Cooper 1981).
Secondary outcomes
Physiological capacity for sexual arousal
Clinical measures for this outcome included monthly assessments of sex hormone profiles, penile tumescence (whilst watching erotic stimuli or contemplating a particular fantasy), sexual activity scores, counts of spontaneous daytime erections, and data from episodes of programmed masturbation.
In terms of hormone profiles, measurement anomalies meant half of the prolactin data were unavailable for one study (Bradford 1993). Luteinising hormone (LH) was not significantly affected across placebo and treatment phases but testosterone and follicle‐stimulating hormones (FSH) both changed significantly in the desired directions. Results of the other objective measure for arousal (millimetres of circumference change of the penis) were analysed as well as assessments by the subjective measure for this outcome (self report). Whilst arousal thus measured was significantly decreased between the baseline and active treatment stage, there were no statistically significant differences between placebo and treatment phases (all relevant data are reported as per the published paper, in Table 1).
1. Bradford 1993 data (Table III, pp 390‐1).
| Measures or variable | Baseline x (SD) | Placebo x (SD) | Active x (SD) | Wilks's F (df) | Phase | t |
| ENDOCRINE | ||||||
| Testosterone | 24.81 (7.93) | 23.52 (6.44) | 12.37 (6.9) | 21.46 d (2, 16) | B ‐ A
P ‐ A B ‐ P |
6.52 d 5.82 d 0.70 |
| Luteinising hormone | 12.24 (4.81) | 12.18 (5.15) | 10.78 (5.22) | 0.854 (2, 14) | ||
| Follicle‐stimulating hormone | 10.78 (6.25) | 11.42 (7.17) | 7.83 (5.37) | 7.37 b (2, 14) | B ‐ A
P ‐ A B ‐ P |
3.71 c 3.77 c ‐78 |
| SEXUAL AROUSAL | ||||||
| Slide (mm circ change) | 11.01 (8.77) | 11.07 (9.71) | 7.33 (9.54) | 2.33 (2, 16) | ‐ | ‐ |
| Fantasy (mm circ change) | 6.66 (7.23) | 11.25 (8.67) | 5.21 (7.87) | 2.75 (2, 16) | ‐ | ‐ |
| Slide self report (mm circ change) | 3.29 (1.36) | 2.53 (1.81) | 2.35 (1.62) | 3.68 a (2, 15) | ‐ | ‐ |
| Fantasy self report sexual arousal | 2.65 (1.47) | 2.41 (1.42) | 2.09 (1.68) | 0.79 (2, 15) | ‐ | ‐ |
| PSYCHOPATHOLOGY | ||||||
| BPRS (total score) | 11.44 (5.24) | 7.33 (5.91) | 5.22 (4.59) | 16.48 d (2, 16) | B ‐ A
P ‐ A B ‐ P |
5.96 d 2.17 a 3.21 c |
| Buss‐Durkee Hostility Inventory | 35.67 (10.43) | 37.50 (9.98) | 35.39 (9.11) | ‐ | ‐ | ‐ |
| SEXUAL BEHAVIOUR | ||||||
| Sexual interest | 3.50 (1.09) | 2.94 (1.11) | 2.78 (1.17) | 2.35 (2, 16) | ‐ | ‐ |
| Sexual activity | 5.65 (4.69) | 6.58 (8.25) | 3.59 (4.19) | 11.91 d (2, 15) | B ‐ A
P ‐ A B ‐ P |
2.56 a 2.39 a ‐0.49 |
B ‐ baseline A ‐ active P ‐ placebo BPRS ‐ Brief Psychiatric Rating Scale df ‐ degrees of freedom mm circ ‐ millimetres of circumference SD ‐ standard deviation aP value < 0.005 bP value < 0.01 cP value < 0.005 dP value < 0.001
A statistically significant effect favouring treatment was found for the 'Sexual Activity Score' (calculated as the total number of orgasms reported for the week) (Bradford 1993). This is correlated with data in another table provided by the investigators in which frequency of masturbation is significantly reduced by active treatment, but other forms of sexual activity (e.g., coitus and homosexual activity) show no difference. Sexual activity data are reproduced in Table 2.
2. Bradford 1993 (Table VII, Sexual activity, p 397).
| Effect | Phase | Chi rank | Cases (n) | Friedmann 2‐way ANOVA Chi2 |
| Nocturnal emissions | B A P | 2.30 1.77 1.93 |
15 | 2.2333 (df = 2) |
| Spontaneous morning erections | B A P | 2.38 1.66 1.97 |
16 | 4.1563 (df = 2) |
| Spontaneous ejaculation | B A P | 2.03 1.88 2.09 |
16 | 0.4063 (df = 2) |
| Masturbation | B A P | 2.47 1.44 2.09 |
16 | 8.7188 (df = 2, P value < 0.05) |
| Coitus | B A P | 1.94 2.09 1.97 |
16 | 0.2188 (df = 2) |
| Homosexual activity | B A P | 1.91 2.03 2.06 |
16 | 0.2188 (df = 2) |
| Homosexual change of partner | B A P | 1.91 2.03 2.06 |
16 | 0.2188 (df = 2) |
| Abnormal sexual activity | B A P | 2.09 2.03 1.88 |
16 | 0.4063 (df = 2) |
B ‐ baseline A ‐ active P ‐ placebo df ‐ degrees of freedom n ‐ number of participants
Non‐significant effects except otherwise indicated.
Cooper 1981 assessed spontaneous daytime erections and sexual outlets as well as arousal or pleasure during (programmed) masturbation. Results for CPA when compared with either no treatment or placebo were significant for both comparisons, even when strict significance levels were applied (P value < 0.001). Here, the advantage for CPA over the other groups was 0.32, 0.17, and 13.2 respectively (Cooper 1981). Investigators also sought confirmation that CPA was at a "therapeutically adequate level" by measuring testosterone plasma levels, commenting that their parallel reduction "in the order of 30%" (alongside those of troublesome sexual symptoms) was, although statistically highly significant, "less important functionally", being"secondary to suppression of hypothalamic releasing factors and pituitary gonadotrophins" (p 463). The investigator also noted that oligospermia (reduction in volume of ejaculate) was remarked upon by all participants during the CPA phase (p 463).
Sexually anomalous urges or sexual obsessions
"Sexual fantasies" were measured in Bradford 1993, where a statistically significant difference was found between baseline and both active and placebo phases, with fewer fantasies during the active phase; however, differences were not significant between active and placebo phases (Table 1).
Cooper 1981 assessed sexual interest, defined as the level of intensity of thoughts and fantasies (i.e., whether "mildly disturbing" or "highly disturbing") reported by participants on a scale from 0 to 100. CPA is significantly superior to no treatment for this outcome.
Anxiety
Anxiety data were not specifically collected and reported in Cooper 1981, but investigators note a "dramatic anti aggressive effect" (Cooper 1981, p 463) similar to that reported in the literature, so providing evidence of "the tranquillising actions" of CPA (Cooper 1981, p 463).
Anger or aggression
Bradford 1993 assessed the effects of CPA on hostility as measured by the Buss‐Durkee Hostility Inventory (BDHI) and found "no differences" across any phase (run‐up or during either cross‐over period); however, the investigator noted that no participant met the clinical cut‐off point (38) at any phase.
Cooper 1981 did not measure anger formally, but reported that"the majority of patients noted that they were less irritable, more tolerant, and more relaxed physically and mentally" during administration of CPA (p 463).
Dropping out of treatment
Two participants (of 19) dropped out of Bradford 1993, including one man described as a homosexual paedophile and one sexually aggressive man with fantasies and urges to rape, both of whom were described as having"reported excellent treatment responses to CPA" (p 399) and left the study early as they felt they no longer needed treatment. The first participant was charged with a "minor" homosexual paedophilic act (fondling) three to six months afterwards and the second reported a return of fantasies six months later but he felt these could be controlled if his drinking was controlled too.
No participants appeared to have left the study conducted by Cooper et al (Cooper 1981).
Adverse events, including suicide or suicide attempts, and sudden or unexpected death, from any cause
No statistically significant differences are reported in Bradford 1993 concerning general condition (physical, affective, concentration, social adjustment), mood measures (restlessness, anxiety, mood swings, loss of drive, suicide, euphoria) or somatic conditions (appetite, sleep, micturition, defecation, hair on head or body, flushes, sweating, headaches, nausea or vomiting, lumbago, gynaecomastia) between the various conditions for the duration of the study. Weight gain, however, was assessed as important with participants gaining an average of 3.1 kg throughout the duration of the trial.
In contrast, Cooper 1981, in a trial of shorter duration, reported that four of nine participants experienced "some loss of energy" (p 463).
c) Medroxyprogesterone plus imaginal desensitisation versus imaginal desensitisation alone (one study)
One small study randomised 30 sex offenders to one of three treatments: medroxyprogesterone (via intramuscular injection, 150 mg, at fortnightly intervals for four injections, followed by four further injections at monthly intervals) versus imaginal desensitisation delivered over five days whilst admitted to a psychiatric hospital) versus combination medroxyprogesterone with imaginal desensitisation (McConaghy 1988). The trial investigators concluded that there were no significant differences in response to the three treatments.
The investigators were principally interested in anxiety as an outcome (measured by the State‐Trait Anxiety Inventory (Spielberger 1983)), as the hypothesis being tested in the trial was that "compulsive sexual behaviours ... are driven by a sense of tension and excitement that becomes aversive if the patient doesn't complete the behaviour in situations where he feels the impulse to do so" (p 200). Testosterone levels were also measured to check the effectiveness of medroxyprogesterone and the one‐month percentage of pre‐treatment levels shown to correlate with self‐ and assessor‐reported reductions in anomalous urges ‐ which was apparently also the case for levels of dihydrotestosterone, luteinising hormone, follicle‐stimulating hormone, and prolactin. Results of the two arms (n = 20) comparing medroxyprogesterone (MPA) with imaginal desensitisation, were as follows:
Primary outcome
Sexual recidivism as measured by reconviction, self report, or caution
Recidivism data are reported using information obtained from solicitors or third party requests to clinicians on participants who had been formally charged for "sexually anomalous behaviour". At two‐year follow‐up, investigators found that no participant who had received both imaginal desensitisation and medroxyprogesterone had received a charge for sexually anomalous behaviour, whereas one who was treated with imaginal desensitisation alone relapsed.
Secondary outcomes
Physiological capacity for sexual arousal
A number of hormone levels were checked in participants taking MPA within this trial, but only those for testosterone are reported.
Testosterone levels were reported for both the combined treatment (MPA plus imaginal desensitisation) arm of this trial and for the MPA‐only condition (not reported on in this review). Of the 20 participants in these groups, testosterone was reduced from 6% to 63% of baseline levels (mean change 31%; range 0.92 to 15.1 nmol/l) (pp 201‐2). Correlations between all participants' testosterone levels at one‐month follow‐up and their anxiety levels as measured by the State‐Trait Anxiety Inventory (Spielberger 1983) are also provided and effects are significant at a level of P value < 0.01 at one month and one year for self assessed "anomalous urges". These results are, however, less robust when assessed by clinicians, particularly when "urge" is contrasted with "behaviour".
Investigators also reported that "most treated with [the drug]maintained heterosexual intercourse at pretreatment frequency" (p 199).
Sexually anomalous urges or sexual obsessions
Investigators summarised data on participant reports' of percentage reductions in "anomalous urges". Percentages are given without standard deviations and are reported narratively here. There was an average decrease in self reported anomalous urges of 70% at one month for the combined treatment group (medication plus imaginal desensitisation, n = 10), which improved further at one‐year follow‐up (75%). Decrease in self reported anomalous urges for the imaginal desensitisation‐only group (n = 10) was initially reduced at 52%, but approached levels reported by the combined‐group at one year, with the imaginal desensitisation‐only group reporting a 72% reduction in urges.
The authors reported that of those who described complete control following treatment were discharged at one year. Of the 24 patients that met this criteria, three "relapsed" with anomalous behaviour; two of these had been treated with MPA alone and one with imaginal desensitisation alone. However, the authors reported that all three 'responded' to institution of MPA.
Anxiety
Correlations between anxiety and testosterone are reported above (and these are the only data given by the treatment group).
Investigators collected data for anxiety using the State‐Trait Anxiety Inventory (Spielberger 1983) (both measures). Means were not provided by the treatment group and were further reported without either standard deviations (SDs) or precise P values. Personal contact with investigators revealed such data have not been preserved (Blaszczynski 2011). Investigators did report that "Patients STAI state and anxiety scores were significantly lower following than preceding all 3 treatments" (McConaghy 1988, p 202) and data in one table show group improvements between P value < 0.001 for state anxiety at one year and P value < 0.05 for trait anxiety at one year for all treated groups.
Anger or aggression
No data are reported for this outcome.
Dropping out of treatment
One participant allocated to combined treatment was "concerned about his low level of normal sexual interest [and] decided not to have [drug] treatment when informed his plasma testosterone was low. He was treated with ID alone and excluded from the study" (p 200).
Adverse events, including suicide or suicide attempts, and sudden or unexpected death, from any cause
No adverse events were reported in the imaginal desensitisation alone group. Adverse events of the drug treatment (medroxyprogesterone) were reported in both the other treatment arms. Four participants ceased injections after three to five episodes due to side effects, though none were reported as having relapsed and they also "reported persistence of the therapeutic effect" (McConaghy 1988, p 201). One patient left the study (from the arm not included in this review) after five injections and did not maintain contact.
d) Medroxyprogesterone acetate (MPA) versus placebo (one study)
One small study randomised 18 sex offenders with a primary attraction to children to either medroxyprogesterone acetate (orally) 200 mg daily or an identical placebo (Hucker 1988). Investigators concluded that MPA was a "useful sex drive reducing medication with few side effects" (p 228) but that compliance was a major obstacle in this population.
Primary outcomes
Sexual recidivism as measured by reconviction, self report, or caution
No formal data are reported for this outcome.
Secondary outcomes
Physiological capacity for sexual arousal
Participants were asked to keep records of episodes of masturbation, intercourse, and total orgasms, as well as any change in frequency of orgasm, level or number of erections, and ejaculate volume on an "urges questionnaire". Investigators supplied only means (without SDs) and there appeared to be a substantial difference at baseline between the two small groups (placebo n = 6; treatment = 5). Whilst all urges appeared to decrease over the period of the study, there were no significant differences on the items listed above between groups. The trial investigators suggested that the overall decrease may have been a "placebo effect of therapy itself or a systematic reduction in sexual activity of these individuals, perhaps due to incarceration" (all participants were on probation) "or some other non‐specific factors" (p 235). Data are reproduced in Table 3.
3. Hucker 1988 data (Table 3, p 235).
| Placebo (n = 6) | Placebo (n = 6) | MPA (n = 5) | MPA (n = 5) | |
| FREQUENCY OF: | Pre | Post | Pre | Post |
| Sexual fantasies | 28.0 | 11.6 | 5.8 | |
| Masturbation | 13.3 | 6.5 | 4.8 | 3.9 |
| Intercourse | 0.9 | 1.4 | 1.7 | 1.0 |
| Total orgasms | 13.3 | 6.5 | 4.8 | 3.9 |
| CHANGES IN: | ||||
| Frequency of orgasm | 2.2 | 1.8 | 1.8 | 1.5 |
| Level of erection | 2.2 | 1.7 | 2.0 | 1.4 |
| Number of erections | 2.2 | 1.6 | 1.8 | 1.4 |
| Ejaculate volume | 2.2 | 1.9 | 2.0 | 1.5 |
MPA ‐ medroxyprogesterone acetate
The effect of MPA on sex hormones, metabolites, and liver enzymes was also reported within this trial. As with the data described above, there would seem to be substantial imbalances at baseline. Investigators reported significance levels for luteinising hormone (LH), follicle‐stimulating hormone (FSH), and testosterone, and reported that for "FSH there is a main effect of drug condition but no interaction with time, F = 7.18, df = 1.14, P < 0.05 as well as for LH, F = 6.60, df =1.14, P < 0.05" (Hucker 1988, p 238). For testosterone, the drug effect was reported as "F = 27.08, df = 1.14, P < 0.01, and drug by time interaction F = 9.43, df = 1.53, P < 0.01" (p 238).
Sexually anomalous urges or sexual obsessions
Investigators reported data on frequency of sexual thoughts and fantasies as part of the "urges questionnaire" mentioned above and these were the only results showing a significant time effect of MPA (SDs not given). The mean number of fantasies was 5.8 (n = 5) for the MPA group and 8.7 (n = 6) for the control group.
Anxiety; anger or aggression
Data were not systematically reported but the investigators commented (p 240) that levels of anxiety and depression seemed high in the study, possibly due to participants' low mood as their court appearance approached, as well as due to other issues common amongst paedophiles, including alcohol and drug abuse.
Dropping out of treatment
One participant allocated to treatment dropped out of the placebo phase due to the discovery of a thyroid tumour (unconnected to this study). A further four dropped out "of their own accord" (p 240). These men appeared to have had "higher frequency of fantasies about children" (p 234); the trial investigators themselves were unsure whether this might represent selection bias of a higher‐risk group unwilling or unable to give up fantasies about children.
Adverse events, including suicide or suicide attempts, and sudden or unexpected death, from any cause
Two of 27 potential side effects were found to be statistically significant (depression and excess salivation). Participants in the placebo group complained of many symptoms and investigators suggested the likelihood of "a complex interaction of awaiting trial, life circumstances and the MPA" (p 235). Overall, investigators viewed "compliance in taking the drug as a major obstacle in its use with pedophiles" (p 228, Hucker 1988).
e) Assertiveness training with medroxyprogesterone acetate (MPA) versus assertiveness training alone (one study)
The largest study in this review randomised 37 men charged with exposure to either medroxyprogesterone acetate (MPA, aka Provera®) almost certainly delivered orally (100 to 150 mg daily) with assertiveness training involving 15 x one‐hour sessions of communication‐based training and with a third treatment group involving both MPA and assertiveness training (Langevin 1979). The latter therapy focused on communication with females but also addressed interpersonal difficulties and was tailored to individuals' own problems. All participants in the first group (MPA) discontinued almost immediately and analysis was confined to the two remaining groups, which also suffered substantial dropout (67% of the combined group and 29% of the assertiveness training group). Investigators concluded that MPA was associated with increased dropout and that side effects were substantial; participants were also more likely to leave assertiveness training if led by a female therapist. Recidivism data were compromised by the high rate of discontinuation.
Primary outcome
Sexual recidivism as measured by reconviction, self report, or caution
We judged the results for this outcome to be at high risk of bias given the significant dropout rate (see below). By the end of the study, half (6/12) of the participants remaining in the assertiveness‐only treatment group and 20% (1/5) of participants remaining in the combined assertiveness training and MPA group recidivated. Participants who dropped out did so even though treatment had been mandated by the court.
Secondary outcomes
Physiological capacity for sexual arousal
No data were reported for this outcome.
Sexually anomalous urges or sexual obsessions
The investigators reported that by the end of treatment only three participants, or 9% of the total sample, experienced decreased urges to expose, but it is unclear how this was measured, and these results apply only to the subset of participants remaining in the study.
Anxiety; anger or aggression
No data were reported for these outcomes.
Dropping out of treatment
The entire medication‐only group (n = 5) discontinued treatment soon after the study commenced. Of the remaining 32 participants (17 in the combined group and 15 in the assertiveness training group), 47% dropped out of treatment before the full course was completed, leaving 12 in the assertiveness training group and five in the combined assertiveness training/MPA group.
Adverse events, including suicide or suicide attempts, and sudden or unexpected death, from any cause
The investigators noted that "Only two patients reported any side effects" (p 279); these were weight gain and nausea (with the latter resolved by taking the medication with milk). Several participants reported feeling psychologically "demasculated" and this (the investigators suggest) "may have been important in their dropping out of treatment". (p 279).
2. Trials of antilibidinal medications ('other')
Antipsychotics (benperidol and chlorpromazine) versus placebo (one study)
One small study (n = 12) compared two antipsychotics (benperidol and chlorpromazine) against placebo over 18 weeks (three six‐week periods) within a highly secure institutional setting (Tennent 1974). Carry‐over effects were not investigated directly, although an unplanned, no treatment phase (which occurred when the active interventions were changed from syrup to tablet forms) allowed additional data to be collected. Based on these data, the investigators claimed that a placebo effect in this study was unlikely; they concluded that chlorpromazine was not effective whereas benperidol"does have a libido reducing effect" but this "is weak and has only been convincingly demonstrated in terms of the reported frequency of sexual thoughts" (p 270).
Primary outcome
Sexual recidivism as measured by reconviction, self report, or caution
Not reported within this study.
Secondary outcomes
Physiological capacity for sexual arousal
The mean "sexual activity" score during the chlorpromazine phase was 3.17, compared with 1.33 in the benperidol phase, and 2.33 in the placebo phase (no SDs available; F = 2.5; df = 2.22; P value = non significant; investigators' analysis). Erections when viewing erotic slides or films were counted and there were no significant differences between conditions ((F < 1.0) in both cases; investigators' analyses).
Sexually anomalous urges or sexual obsessions
The mean score during the chlorpromazine phase for 'sexual attitude' (Marks 1967) was 7.09, compared with 9.99 in the benperidol phase, and 8.76 in the placebo phase (no SDs available; F = 5.1; df = 2.22; P value = 0.025; investigators' analysis). This represents a statistically significant difference between treatments in favour of benperidol over chlorpromazine, although neither was significantly better than placebo.
Anxiety; anger or aggression
No data were reported for these outcomes.
Dropping out of treatment
Three participants left the study early (two within the first week, of their own volition; a third was withdrawn due to severe depression). These three participants were replaced by three other volunteers. Subsequently, all participants appear to have remained in the study for its 18‐week duration.
Adverse events, including suicide or suicide attempts, and sudden or unexpected death, from any cause
Data on side effects were measured throughout the study and whilst investigators noted that "severity of side effects was not systematically assessed... patients' reports were recorded" (p 270, Tennent 1974), they also observed that, in some cases, side effects were of a severity "either to present a transient marked disturbance or, if prolonged, to require increase in orphenadrine" (to counteract extra‐pyramidal side effects). Results appear to indicate that benperidol was associated with considerably more dyskinetic extra‐pyramidal side effects than chlorpromazine, but that chlorpromazine was slightly superior in terms of drowsiness. Blurred vision, photosensitivity, dry mouth, and impaired exercise tolerance were also reported for both drugs.
Discussion
Summary of main results
We identified seven studies that met our criteria for inclusion. No meta‐analysis was possible and all results were reported narratively. Five different drugs were used, two of which were in 'head‐to‐head' (active treatment comparison) trials (Bancroft 1974; Tennent 1974); three against placebo alone (Cooper 1981; Hucker 1988; Bradford 1993); and two where the drug was augmented with a psychological intervention and compared against the psychological intervention on its own (Langevin 1979; McConaghy 1988). Three of the drugs were progestogens or antiandrogens; two were antipsychotics. There were no data on the use of serotonergic antidepressants (SSRIs) or gonadotropin‐releasing hormone (GnRH) analogues.
The overall number (N) of participants for whom data were available in this review is 123. For any one outcome, data are available for a maximum of 100 participants. Given this fact (and the issues of consent and compliance mentioned elsewhere in this review) all results must be interpreted with caution.
Primary outcome ‐ sexual recividism as measured by reconviction, self report, or caution
Results for CPA were moderately encouraging, with reductions in some targets (e.g., physiological arousal) but recividism data do not appear to have been formally collected (Cooper 1981; Bradford 1993); follow‐up ran for up to 13 months. Medroxyprogesterone acetate MPA (intramuscular) appeared effective in the one trial assessing it (McConaghy 1988), with no reports of recividism at two‐year follow‐up. Another small trial of MPA delivered orally did not report on recividism formally, but it may be inferred that no charges were made during the course of the trial (Hucker 1988). In contrast, results for one trial of oral MPA in combination with psychological treatment were discouraging ‐ all participants in the arm of the trial assessing drug treatment alone dropped out immediately and of those few remaining in a combined drug and psychological treatment condition, 20% recidivated. Participants who dropped out did so even though treatment had been mandated by the court (Langevin 1979).
Two studies included within this review took place in one highly secure psychiatric facility where participants' chance of release into the community was low, so collection of recividism data was impossible (Bancroft 1974; Tennent 1974).
Secondary outcomes
Physiological capacity for sexual arousal
In one small study comparing ethinyl oestradiol (EO) to cyproterone acetate (CPA), both drugs were assessed as significantly decreasing sexual activity compared to placebo, but these self report data were not confirmed by phallometric data (Bancroft 1974).
CPA was assessed as effective in decreasing capacity for arousal, number of orgasms, and hormone levels (testosterone, luteinising hormone (LH), follicle‐stimulating hormone (FSH)), compared to placebo in two studies (Cooper 1981; Bradford 1993). MPA was also reported to reduce circulating testosterone significantly in one trial in which the drug was administered intramuscularly (McConaghy 1988). These encouraging results were not replicated in a trial assessing MPA by oral administration (Hucker 1988), either in terms of sex hormones or in counts of sexual activity (e.g., numbers of erections and orgasms), where treatment and control results did not differ significantly and investigators postulated a "placebo effect of therapy itself" (Hucker 1988, p 235). In the one small study assessing antipsychotics within this review (Tennent 1974), chlorpromazine was superior to benperidol in reducing "sexual activity"; but in terms of measures of participants' arousal during erotic stimuli, no significant differences between drugs (or placebo) could be detected.
Sexually anomalous urges or obsessions
"Sexual attitudes" were not significantly altered by either drug (EO or CPA) investigated in one small included trial (Bancroft 1974). CPA was assessed as effective in decreasing sexual interest and the "disturbing" intensity of fantasies in one study (Cooper 1981), but in the larger study assessing CPA findings were less encouraging (Bradford 1993), as a significant improvement for this outcome was recorded from baseline to end‐point for both active and placebo conditions, but not between active and placebo conditions. "Anomalous urges" were reduced by the administration of MPA intramuscularly in one study (McConaghy 1988), with an average decrease of 70% at one month, which was strengthened to 75% at one year; these encouraging results were replicated in a trial assessing MPA by oral administration (Hucker 1988), where MPA intervention delivered its sole significant treatment effect (on frequency of sexual thoughts and fantasies). Results from another trial, which assessed the effects of a combination of orally administered MPA and psychological treatment (Langevin 1979), indicated that few participants experienced a decrease in urges to expose themselves, but it is unclear how this was measured.
The effects of antipsychotics were assessed in one study on only 12 participants (Tennent 1974). Results indicated that chlorpromazine was ineffective and that benperidol had (at best) a weak libido‐reducing effect.
Anxiety
Anxiety was formally measured in only one trial (McConaghy 1988), where treatment (MPA) significantly reduced anxiety levels, and was formally correlated with a decrease in testosterone levels as well. Other investigators, e.g., Cooper 1981, commented extensively on the "calming" nature of antiandrogen treatments in general (particularly, CPA).
Anger or aggression
Only one study formally measured anger and found no significant differences in a comparison between CPA and placebo (Bradford 1993); other investigators, e.g., Cooper 1981, commented on the known "anti‐aggressive" effects of CPA.
Dropping out of treatment
Participants left studies early in five of the seven studies, and effects on overall participant numbers ranged from 3% to 54%.
In the study comparing EO with CPA, one individual (non‐treatment related) from a total of 12 participants droppped out (Bancroft 1974). One participant left the MPA‐only condition of the trial conducted by McConaghy et al (n = 31), due to concerns about his low sexual interest (McConaghy 1988). In the trial conducted by Hucker et al, four participants (all of whom had a high frequency of fantasies about children) left the study. Investigators commented that it was possible that this represented selection bias of a higher‐risk group unwilling to surrender fantasies of children (Hucker 1988). One quarter (3/12) of the participants of the one trial assessing the effects of antipsychotics left the study, two of their own volition and one because of depression (Tennent 1974). The most severe dropout took place in the three‐armed study conducted by Langevin et al (n = 37) in which MPA, assertiveness training, and MPA combined with assertiveness training, were compared. All participants in the first group dropped out immediately, five left the assertiveness training condition and 10 left the combined treatment condition (Langevin 1979).
Adverse events, including suicide or suicide attempts, and sudden or unexpected death, from any cause
Six studies provided information on adverse events (Bancroft 1974; Tennent 1974; Langevin 1979; Hucker 1988; McConaghy 1988; Bradford 1993). No study tested the effects of testosterone‐suppressing drugs beyond six to eight months and the cross‐over design of some studies leads to further uncertainty (given the 'rebound effect' of some hormonal treatments). Considerable weight gain was reported in two trials of oral MPA and CPA. Side effects of intramuscular MPA led to discontinuation in some participants after three to five injections (the nature of these side effects was not described). Notable increases in depression and excess salivation were reported in one trial of oral MPA. The most severe side effects (extra‐pyramidal movement disorders and drowsiness) were reported in a trial of antipsychotic medication (Bancroft 1974). No deaths and no suicide attempts were reported in any of the studies. The latter is important given the association between antilibidinal hormonal medication and mood changes (Thibaut 2010; Gooren 2011), and there has been at least one case report of treatment failure and attempted suicide associated with GnRH use (Briken 2004). Where reported, no significant effect of medication on dropout was noted.
In summary, there were few trials of a limited number of drugs and limited duration, the effect of which on our primary outcome of recidivism reduction was not compelling, particularly given a) acceptance of treatment; b) adherence to treatment; and c) the possibility of adverse events.
Overall completeness and applicability of evidence
The evidence that addressed our review question was very weak. Only seven studies met our entry criteria and most of these were small, with an average of fewer than 20 individuals at randomisation.
An additional and surprising limitation was the absence of any contemporary studies; the most recent that met our inclusion criteria was published two decades ago (Bradford 1993). As a consequence, several new promising drugs (e.g., SSRIs and GnRH analogues) have no good quality trial evidence to support their use. This neglect of an important area of clinical practice requires urgent attention.
There are other limitations too. As expected, all studies were on male participants. The fact that there were no intervention studies on females represents additional evidence of the historical limitation of our inquiry as it does not address recent attention to female sexual offending (Gannon 2010). Of note, progestogens (Cooper 1981), SSRIs, and antipsychotics have similar effects in reducing libido in both sexes.
In as much as current practice recommends that complementary psychological interventions be employed alongside pharmacological agents (Lösel 2005; Briken 2007), another limitation is that this type of combined treatment was only examined in two studies (McConaghy 1988; Bradford 1993).
Two important limitations arise from the seriousness of the offending history and the setting in which the interventions took place. Profiles for recividism for categories of sex offenders vary, for example, those guilty of intrafamilial sex abuse have the lowest rate and exhibitionists have the highest rate of recividism (Seto 1999), and most included studies recruited a variety of offender types and levels of severity within those types. The two trials that recruited serious sexual offenders were both in high security hospitals in the UK. Inevitably, investigators could not report recidivism data, as the individuals treated were not released because of the serious nature of their offences together with the location of their detention. Conversely, the trials in non‐institutional settings suffered from the opposite limitation – namely, that many of those recruited exhibited sexual behaviour that was not sufficiently serious enough to warrant a custodial sentence. For instance, the largest study included within this review included only sexual exhibitionists (Langevin 1979). Similarly, the nature of the sexual offending in other studies was such that there was only "… a possibility of imprisonment" (Cooper 1981, p 459) suggesting that the behaviours may not have been extreme.
Currently, the majority of those convicted of serious sexual offences are detained in prison; yet none of the trials reported here took place in a prison setting. While prison samples contain individuals with sexual behaviour of sufficient seriousness to merit a custodial sentence, as their numbers are very much greater than those in secure hospital, they offer the opportunity of intervening close to the offender's release date thereby allowing for the collection of recidivism data.
As current criminological thinking suggests that sexual offenders have versatile criminal careers so that their sexual offending is part of their general offending behaviour, there is an argument for including general recidivism as a secondary outcome. Indeed, Lösel and Schmucker found in their 2005 review of the literature that interventions for sexual offending had an equivalent effect in reducing non‐sexual offending (Lösel 2005). This, however, introduces a further caveat in interpreting the evidence of efficacy as some programmes designed to reduce sexual offending may reduce further violent behaviour but not further reduce sexual offending. For instance, whilst the psychologically based prison sex offender treatment programme (SOTP) in the UK was shown to reduce future violent and sex offending when analysed in combination, it failed to demonstrate a statistically significant reduction in sex offending alone (Friendship 2003).
This is an important distinction as follow‐up studies show that while sexual offenders continue to commit a range of offences (including sexual offences), violent non‐sexual offenders rarely commit further sexual offences (Bonta 1995; Duggan 2013). This suggests that sexual offenders require specific interventions to reduce their propensity to reoffend sexually and that generic violence reduction programmes are insufficient.
This absence of good quality evidence places the practitioner in an unenviable position. One the one hand, clinical practice necessitates that decisions have to be made here and now with whatever evidence is available. As Lösel and Schmucker point out: "... policymaking and practice cannot wait until an unrealistic goal standard evaluation study but must be informed about the results of sub‐optimal, quasi‐experimental studies" ((emphasis added) Lösel 2003, p 3). In the absence of good quality evidence from appropriate trials, clinicians have to resort to guidelines drawn from expert opinion such as those of Thibaut et al (2010) on the role of pharmacological agents for paraphilias (Thibaut 2010). In so doing, it is surely important that quasi‐judicial hearings (e.g., the parole board) determining the release or further incarceration of a sexual offender, on the basis of whether he has engaged successfully with sex offending treatment, are properly informed as regards uncertainties about the evidence base for such treatment.
In summary, while there are a number of serious ethical challenges in conducting trials in this area that we will consider further below, the fact remains that the evidence in support of any pharmacological intervention for those who sexually offend is very limited.
Quality of the evidence
Our review retrieved seven small studies with a total of 138 participants, for whom data were available for only 123. No study was preceded by a defined pre‐published protocol and each contained several methodological flaws. No study described attempts to conceal allocation, few could be considered to have adequate sequence generation (Bancroft 1974; Tennent 1974), and blinding of outcome assessors was an issue in several. These limitations do not allow robust conclusions to be drawn.
A significant issue was the cross‐over design used in most included studies, particularly as rebound hypersexuality may occur in placebo phases due to receptor hypersensitivity, and may take a month to normalise (Bradford 1993). Given that medication treatment phases ranged from three to six months, the possibility of carry‐over effects should also be considered.
Despite this, most studies consistently showed reductions in sexual interest and arousal with medication intervention, with three studies being able to correlate this to reduced plasma levels of testosterone (Cooper 1981; McConaghy 1988; Bradford 1993).
Potential biases in the review process
Meta‐analysis does suggest that deviant sexual interests and sexual preoccupation are significant predictors of sexual recidivism (Hanson 2005). This is relevant as, except for the Tennent study (Tennent 1974), which used typical neuroleptics, the other studies employing testosterone‐lowering interventions or oestrogens all showed a positive effect in reducing various components of the sexual process. Whether this translates in turn to a reduction of sexual reoffending has not been answered.
Treatment for sexual offending may have positive consequences other than a reduction of further sexual offending, including non‐sexual offending and improved psychological health (Hansen 1997), but these outcomes are not discussed in this review. These are important limitations as current criminological thinking suggests that sexual offenders have versatile criminal careers such that their sexual offending is part of their general offending behaviour (Simon 2000; Hanson 2010), creating an argument for including general recidivism as a secondary outcome. Indeed, Lösel and Schmucker found in their 2005 review of the literature that interventions for sexual offending had an equivalent effect in reducing non‐sexual offending (Lösel 2005). Our failure to consider this issue therefore can be seen as a limitation; however, had we so done we would have been obliged to report that none of our included studies reported on non‐sexual offending.
An additional limitation was our restriction to studies with a randomised design, which explains why our conclusions are discrepant with those of other reviews (e.g., Lösel 2005), which included evidence from non‐randomised trials. We recognise the importance of such trials; however, as they produce suggestive evidence of effectiveness that then needs to be trialled in rigorous randomised trials later, we effectively excluded other studies that might otherwise provide useful data. The current situation is therefore one in which some non‐randomised trials of poor quality can show a significant effect for medication while randomised trials that are of superior quality can only report weak evidence.
One additional important bias that arises when one restricts the review to randomised controlled trials (RCTs) is that, as the process of recruitment requires informed consent, it is likely to result in only the most compliant being included, particularly for this type of treatment. Nagayama‐Hall 1995 pointed out that psychological treatment was considered acceptable by two‐thirds of offenders, but pharmacological treatment only by one‐third). Thus, failing to consider that only a minority of offenders will consent to treatment might inflate the effect of those trials of medication that show benefit. Consequently, it is difficult to generalise the findings from such trials to other sex offenders who might require (and possibly benefit from) such intervention, but who refuse to accept or comply with it.
Agreements and disagreements with other studies or reviews
This report was preceded by several major reviews into the treatment of sexual offending. These have arrived at mixed conclusions; some claiming that interventions are effective in reducing recidivism and others the reverse.
Furby, Weinrott, and Blackshaw concluded that treatment did not reduce recidivism rates in sex offenders (Furby 1989). Nagayama‐Hall updated the Furby et al review by conducting a meta‐analysis of 12 new studies that contradicted its predecessor by finding equivalent positive effects for hormonal treatment and cognitive behavioural therapy (CBT), both of which were assessed as superior to behavioural interventions (Nagayama‐Hall 1995). Overall, treatment was found to be modest in its effect, reducing recidivism by 8%. Castrated patients had the lowest recidivism rate (0.3) and the largest effect sizes (r = 0.53). An early Cochrane review by White et al identified only a single drug trial (i.e., MPA reviewed in this report) and found it to be ineffective (White 1998).
Lösel and Schmucker conducted a thorough systematic review of controlled outcome studies of all relevant interventions, which included 80 comparisons involving data from 22,181 participants (Lösel 2005). This review included data from both published and unpublished studies reported up to June 2003. Main results featured a large effect size for surgical castration (odds ratio (OR) 15.34; 95% confidence interval (CI) 7.34 to 32.05; eight studies), and a reasonably large effect size for hormonal treatment (OR 3.08; 95% CI 1.40 to 6.79; six studies). This compared to a moderate effect size for CBT (OR 1.45; 95% CI 1.12 to 1.86; 35 studies). Overall, 11.1% of the treated offenders and 17.5% of the controls showed sexual recidivism (a 37% difference) when both pharmacological and psychological treatments were considered. The authors also noted that the interventions were effective in reducing reoffending in general.
More recently, two relevant literature reviews have appeared focusing on drug treatments for both paraphilic and non‐paraphilic sexual disorders (Guay 2009) and for paraphilic disorders alone (Garcia 2011). Neither restricted itself to trials of any particular study design; neither searched more than two databases; both indicated that treatment looked promising but that the state of the intervention literature was poor. Subsequently, Langstrom and colleagues conducted a review of the effectiveness of treatments for offenders against children (Langstrom 2013). These authors did not restrict their review by type of treatment, by age of offender, or to randomised controlled trials. Their review included eight studies and the authors did not find meta‐analysis feasible. Conclusions were that scientific evidence is weak and that there is an urgent need for better quality studies.
One explanation for these discrepant findings is that the quality of the evidence required to arrive at a conclusion differed. This variability arises from differences in the types of study design. Indeed, a similar point was made by Rice and Harris (Rice 2003), when commenting on the previous review by Hanson and colleagues (Hanson 2002). Rice and Harris observed that not only were many methodologically flawed studies included, but that the 'best' studies showed no effect. Similarly, the review by Lösel and Schmucker cast its net very widely, with 60% of the studies considered to be of non‐equivalent design (only six were RCTs) (Lösel 2005). Mindful of Sackett et al's 1996 warning that "…we should avoid non‐experimental approaches … since these routinely lead to false positive conclusions about efficacy…" (Sackett 1996, p 71), this raises concerns regarding the positive conclusions in relation to the efficacy of current interventions. Moreover, only two of the seven trials described in this report were considered in their meta‐analysis (Langevin 1979; McConaghy 1988), because their inclusion criteria specified recividism as a prospective outcome. To be fair to the authors, they do acknowledge that "we need more high‐quality outcome studies that address specific subgroups of sex offenders as well as more detailed process evaluations on various treatment characteristics and components." (Lösel 2005, p 138). Briken and Kafka concluded that, even after decades of experimentation, pharmacological treatments showed "definite promise" but further research was required and pharmacological treatment should not be seen as a "standalone" treatment (Briken 2007); Eher likewise deplored the quality of the existing evidence base (Eher 2010). The present review concurs in finding, as yet, no compelling evidence in favour of medication.
Authors' conclusions
Implications for practice.
As the victim of a sexual offence is likely to suffer considerable harm, an individual convicted of a sexual offence can expect a lengthy custodial sentence. In addition, some states in the USA have now introduced preventative detention for sex offenders who are thought to be at high risk of sexual reoffending in the future. Similarly, amendments to the UK Mental Health Act 1983 have meant that paraphilias are now mental disorders within the meaning of the Act, thereby allowing for their involuntary treatment subject to certain conditions being satisfied. When such 'civil commitment' was challenged in the USA, the Supreme Court made it clear that this can only be legitimate if meaningful treatment is provided (Justia US Supreme Court 1997).
In the light of these significant infringements of civil liberty, it is imperative that good quality trial evidence is available if an individual's likelihood of release is to be determined by engaging in an intervention that is deemed to be effective.
This review does not provide sufficient evidence for a reduction of sexual recidivism in offenders following pharmacological treatment. While it does identify trends for a reduction of proxy measures of sexual offending with some antiandrogens, these are associated with considerable bias and – because the trials are dated – they inevitably have a focus on medications which may have been superseded in modern practice, and for which adverse events remain of concern.
Here, we recognise the frustration of many practising clinicians when faced with treating sexual offenders in their daily practice and expecting that the research community will provide him or her, with some practical and research‐based guidance. Here, the algorithmic treatment regimens of Grubin 2008 and Thibaut 2010 no doubt have their value, but, from the perspective of evidence‐based practice, these recommendations – however sensible – remain at the lowest level of the evidence hierarchy when not supported by properly conducted randomised controlled trials.
Implications for research.
The difficulties in carrying out medication trials for sexual offenders was aptly summarised by a quotation from the oldest trial included in this review (Bancroft 1974) "Not only is it conceivable that a transient placebo effect may follow the use of any preparation, but also one is dealing with sexual offenders in many of whom the main motivation for accepting treatment is their wish to avoid further penalties and in whom the desire to lose the deviant sexual interest is difficult to assess" (p 310). Other investigators identified both acceptance of and compliance with treatment as major obstacles (Hucker 1988; Nagayama‐Hall 1995), together with censure of investigators if a sexual offender in the control group commits a further sexual offence (Marshall 2007).
While all of these are reasonable concerns, they are not unique to the treatment of sexual offenders and other areas of health care facing similar challenges in treatment (e.g., cancer, psychosis) have managed to overcome them. The evidence from this review (and from its companion review into psychological treatments for sexual offenders, Dennis 2012) suggests that, whatever advances in treatment are likely to occur, they will be at the margins – i.e., equipoise remains. Consequently, it remains essential to conduct properly designed, large‐scale trials of medications in this area. Given the biological underpinning of sexual activity, one might anticipate that trials of antilibidinal medication would be commonplace; in fact, the reality is the reverse. In this review, for instance, we could only find seven trials of antilibidinal medication that satisfied the Cochrane criteria for acceptability. Given the prevalence of sexual offending, together with its consequences for both the victim and the offender, a failure to provide evidence of an effective intervention is worrying and requires some further analyses.
We have reviewed some of the problems in conducting randomised controlled trials for sex offenders in general (Duggan 2014), and here discuss these in relation to medication. The very point of conducting a randomised trial is to determine (a) if the intervention is effective and (b) that it does no harm. There is the mistaken belief, however, that those randomised to the control condition (particularly if it is a placebo) are likely to be disadvantaged so that were they to reoffend after the study, then the investigator might expect to be criticised; this again can be answered with a challenge to consider ethical equipoise. This may explain why there are (a) so few drug trials in what would otherwise be a profitable area to exploit because of its chronicity and (b) the apparent absence of any trial activity within the past two decades, prior to one ongoing trial in Germany (Briken 2012).
Second, drug trials are generally of short duration and, since we know that sexual recidivism may occur after several years of follow‐up, does this mean that the treatment needs to be life‐long to maintain a reduction in sexual offending? Currently, given the extant knowledge, the answer to this question can only be gleaned from expert opinion (Thibaut 2010). Although the studies reviewed show a mixed response as regards the side effects associated with the medication, all of these were of relatively short duration so that the response to their chronic usage may have more serious consequences. Berlin suggests that the risks of androgen deprivation treatment, in association with a proper protocol for prostate cancer patients, are broadly similar to other commonly prescribed psychotropics (Berlin 2009), and investigators must remain alert to minimising these risks where possible (Ahmadi 2013). Investigators must also remain alert to the possibility of a treatment effect being undermined by exercise or by other medications used to undermine the effect of antilibidinals (Cormie 2013; Lee 2013), as well as being mindful of the 'rebound effect' in testosterone levels and fantasising following cessation of some types of treatment (Bradford 1993; Koo 2013; Koo 2014).
Third, trials hitherto may have lacked a specific rationale for their intervention. However, recent advances may have changed this thinking. The use of serotonergic antidepressants (SSRIs), for instance, to target the obsessional preoccupation of sexual offenders would require that they be prescribed at a high dose for a sufficient period. Similarly, the use of gonadotropin‐releasing hormone (GnRH) drugs (used in the treatment of prostate carcinoma) has been reported to be effective in case series of those who are at high risk of sexual offending (Rösler 1998).
Lastly, the difficulty in attracting a sufficient number of participants into trials is well recognised (Hucker 1988), and has recently been reported as the reason for the termination of a trial in Norway (NCT00379626). This may be due to a number of factors involving typical characteristics of sex offenders, including denial, cognitive distortion, and antisocial attitudes (Hanson 2005), as well as the intrinsic consequences of the use of antilibidinal medication, such as stigma, and psychological effects such as perceived demasculinisation (Langevin 1979). Small numbers in trials is a common theme and inevitably affects the power and duration of studies, the homogeneity of participants, the scope for logistical regression, and ultimately, the quality of evidence available.
Given that a significant proportion of those detained in prisons in the UK and elsewhere have been convicted of a sexual offence, there is no excuse that this is not a legitimate area in which to conduct a randomised controlled trial using medication. This ought to include a homogeneous population (i.e., rapists or paedophiles) with a clear rationale for its use together with an appropriate follow‐up period (minimally five years). Initially, these active treatments ought to be trialled against whatever treatment is currently being offered before proceeding to more complex 'head to head' trials, should the evidence warrant it. Attention should also be paid to comorbidities (generally mood disorders, anxiety disorders, psychoactive substance abuse disorders, attention deficit hyperactivity disorder (ADHD), and neuropsychological conditions), which appear to occur more frequently than expected in sexually impulsive men (Briken 2007).
Although these recommendations appear to set the bar at a high level, the failure to do so in the past has meant that uncertainty continues with detrimental effects for both perpetrator and victim.
Acknowledgements
We would like to thank the authors of both the original reviews by White et al and Kenworthy et al for establishing the methodology on which this review is principally based. We would like to thank Mark Fenton for devising the initial search strategy and Lynn Turner, Jo Abbott, and Margaret Anderson of the Cochrane Developmental, Psychosocial and Learning Problems Group, for running the searches. We also thank Dr R Stocking Korzen for his help in assessing French language papers and Professor Birgit Völlm for assessing German language papers. We would also like to thank Professor Don Grubin and Associate Professor Richard Kreuger for advice on the biological effects of testosterone and testosterone‐suppressing medications.
Appendices
Appendix 1. Search strategies
Filters designed to capture RCTs were used where appropriate. No language or date restrictions were applied. The electronic searches were constructed taking into account changing terminology and perception of sex offences. We recognise that several of the terms above would now be regarded as unacceptable or misleading, or both, as terms signifying sexual offending. These searches were also run for a related review (Dennis 2012).
Searches were run in October 2010, June 2013, and July 2014, except where noted.
1. AMED (Allied and Complementary Medicine) (via OVID)
1 (sex$ adj2 devia$).tw.)
2 (public adj2 masturbat$).tw.
3 (child$ adj2 molest$).tw.
4 (child$ adj2 (sex$ or abuse$)).tw.
5 (sex$ adj2 (murder$ or tortur$ or abus$ or fondl$)).tw.
6 (indecen$ adj2 behav$).tw.
7 (child$ adj2 porn$).tw.
8 (lewd$ adj2 (behav$ or act)).tw.
9 bondag$.tw.
10 frotteur$.tw.
11 necrophi$.tw.
12 bugger$.tw.
13 molest$.tw.
14 pederast$.tw.
15 paedoph$.tw.
16 pedoph$.tw.
17 scatologia.tw.
18 necrophilia.tw.
19 zoophilia.tw.
20 coprophilia.tw.
21 urophilia.tw.
22 partialism.tw.
23 klismaphilia.tw.
24 bestiality.tw.
25 sodom$.tw.
26 molest$.tw.
27 paraphil$.tw.
28 voyeur$.tw.
29 exp Sex offenses/
30 exp Paraphilias/
31 exp Sex behavior/
32 exp Child abuse sexual/
33 or/1‐32
34 random$.ab,ti.
35 (double adj2 blind).ab,ti.
36 (triple adj2 blind).ab,ti.
37 (single adj2 blind).ab,ti.
38 (treble adj2 blind).ab,ti.
39 (random adj2 (allocat$ or assign$)).ab,ti.
40 exp clinical trials/
41 exp Double blind method/
42 exp Random allocation/
43 or/34‐42
44 33 and 43
2. ASSIA (via ProQuest)
Query: ((DE=("rape" or "acquaintance rape" or "date rape" or "drug rape"
or "gang rape" or "male rape" or "marital rape" or "serial rape")) or
(DE=("incest" or "father daughter incest" or "mother son incest")) or
(DE="exhibitionism") or (DE="sex offending") or (DE=("sexual deviance" or
"erotomania" or "frotteurism" or "gender dysphoria" or "necrophilia" or
"paedophilia" or "paedophiliacs" or "paraphilia" or "fetishism" or
"klismaphilia" or "paraphiliacs" or "sadism" or "sadomasochism" or
"masochism" or "sodomy" or "transsexuals" or "transvestism" or
"transvestites" or "zoophilia" or "zoophiliacs")) or (sex* within 2
devia*) or (public* within 2 masturbat*) or (child* within 2 (sex* or
abuse*)) or (child* within 2 porn*) or (child* within 2 molest*) or
(lewd* within 2 (behav* or act)) or (indecen* within 2 behav*) or (sex*
within 2 (murder* or tortur* or abus* or fondl*)) or (partialism or
klismaphilia or bestiality* or sodom* or molest* or paraphil* or voyeur*)
or (bondag* or frotteur* or necrophi* or bugger* or molest* or pederast*
or paedoph* or pedoph* or scatalogia or necrophilia or zoophilia or
coprophilia or urophilia)) and ((DE=(double blind studies) or (single*
near blind*)) or (TI=(double* blind*) or AB=(double* blind*)) or
(DE=(randomi?ed controlled trials)) or (TI=random* or AB=random*))
2013 (DE("rape" or "acquaintance rape" or "date rape" or "drug rape" or "gang rape" or "male rape" or "marital rape" or "serial rape") or DE("incest" or "father daughter incest" or "mother son incest") or DE("exhibitionism") or DE("sex offending") OR DE("sexual deviance" or "erotomania" or "frotteurism" or "gender dysphoria" or "necrophilia" or "paedophilia" or "paedophiliacs" or "paraphilia" or "fetishism" or "klismaphilia" or "paraphiliacs" or "sadism" or "sadomasochism" or "masochism" or "sodomy" or "transsexuals" or "transvestism" or "transvestites" or "zoophilia" or "zoophiliacs") or (sex* within 2 devia*) or (public* within 2 masturbat*) or (child* within 2 (sex* or abuse*)) or (child* within 2 porn*) or (child* within 2 molest*) or (lewd* within 2 (behav* or act)) or (indecen* within 2 behav*) or (sex* within 2 (murder* or tortur* or abus* or fondl*)) or (partialism or klismaphilia or bestiality* or sodom* or molest* or paraphil* or voyeur*) or (bondag* or frotteur* or necrophi* or bugger* or molest* or pederast* or paedoph* or pedoph* or scatalogia or necrophilia or zoophilia or coprophilia or urophilia)) and (DE(double blind studies) or (single* near blind*) or TI(double* blind*) or AB(double* blind*) or DE(randomi?ed controlled trials) or TI(random*) or AB(random*))
3. BIOSIS (via Web of Science)I took two words our
# 12 #11 AND #10
# 11 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1
# 10 #9 OR #8
# 9 TS=((singl* OR doubl* OR tripl* OR trebl*) SAME (mask* OR blind*))
# 8 TS=(random* OR crossover)
# 7 TS=(urophilia OR partialism OR klismaphilia OR bestiality OR sodom*)
# 6 TS=(molest* OR paraphil* OR voyeur* OR bondag* OR frotteur* OR necrophi* OR bugger* OR pederast* OR paedoph* OR pedoph* OR scatalogia)
# 5 TS=(zoophilia OR coprophilia OR fetishi* OR exhibitionism OR voyeuris* OR sadis* OR masochis* OR incest* OR rapist* OR rape*)
# 4 TS=(sex* SAME (murder* OR tortur* OR abus* OR fondl*))
# 3 TS=(sex* SAME devia*) OR TS=(public SAME masturbat*) OR TS=(child* SAME molest*) OR TS=(child* SAME sex*)
# 2 TS=(indecen* SAME behav*) OR TS=(child* SAME porn*) OR TS=(lewd* SAME behav*) OR TS=(lewd* SAME act*)
# 1 TS=((sex* SAME offen*))
4. Cochrane Central Register of Controlled Trials (CENTRAL)
#1 MeSH descriptor Child Abuse, Sexual explode all trees
#2 MeSH descriptor Sexual and Gender Disorders explode all trees
#3 MeSH descriptor Sexual Dysfunctions, Psychological explode all trees
#4 MeSH descriptor Sex Offenses, this term only
#5 MeSH descriptor Incest explode all trees
#6 MeSH descriptor Rape explode all trees
#7 sex* near/2 devia*
#8 public* near/2 masturbat*
#9 child* near/2 sex*
#10 child* near/2 abuse*
#11 child* near/2 porn*
#12 child* near/2 molest*
#13 sex* near/2 murder*
#14 sex* near/2 tortur*
#15 sex* near/2 abus*
#16 sex* near/2 fondl*
#17 indecen* near/2 behav*
#18 lewd* near/2 behav*
#19 lewd* near/2 act
#20 bondag*
#21 frotteur*
#22 necrophi*
#23 bugger*
#24 molest*
#25 pederast*
#26 paedoph*
#27 pedoph*
#28 scatologia
#29 zoophilia
#30 coprophilia
#31 urophilia
#32 partialism
#33 klismaphilia
#34 bestiality
#35 sodom*
#36 paraphil*
#37 voyeur*
#38 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30)
#39 (#31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37)
#40 (#38 OR #39)
5. CINAHL (platforms prior to 2010 unknown, OVID in 2010)
1 (sex$ adj2 devia$).tw.
2 (public adj2 masturbat$).tw.
3 (child$ adj2 molest$).tw.
4 (child$ adj2 (sex$ or abuse$)).tw.
5 (sex$ adj2 (murder$ or tortur$ or abus$ or fondl$)).tw.
6 (indecen$ adj2 behav$).tw.
7 (child$ adj2 porn$).tw.
8 (lewd$ adj2 (behav$ or act)).tw.
9 bondag$.tw.
10 frotteur$.tw.
11 necrophi$.tw.
12 bugger$.tw.
13 molest$.tw.
14 pederast$.tw.
15 paedoph$.tw.
16 pedoph$.tw.
17 scatologia.tw.
18 necrophilia.tw.
19 zoophilia.tw.
20 coprophilia.tw.
21 urophilia.tw.
22 partialism.tw.
23 klismaphilia.tw.
24 bestiality.tw.
25 sodom$.tw.
26 molest$.tw.
27 paraphil$.tw.
28 voyeur$.tw.
29 exp PARAPHILIAS/
30 exp Sexuality/
31 exp Child Abuse, Sexual/
32 exp INCEST/
33 exp RAPE/
34 or/1‐33
35 randomi$.mp.
36 clin$.mp.
37 trial$.mp.
38 (clin$ adj3 trial$).mp.
39 singl$.mp.
40 doubl$.mp.
41 tripl$.mp.
42 trebl$.mp.
43 mask$.mp.
44 blind$.mp.
45 (39 or 40 or 41 or 42) and (43 or 44)
46 crossover.mp.
47 random$.mp.
48 allocate$.mp.
49 assign$.mp.
50 (random$ adj3 (allocate$ or assign$)).mp.
51 Random Assignment/
52 exp Clinical Trials/
53 exp Meta Analysis/
54 50 or 46 or 45 or 38 or 35 or 51 or 52 or 53
55 34 and 54
2013 and 2014 ‐ spelling error concerning BESTIALITY corrected. Platform now EBSCOhost
6. Dissertation Abstracts International (via ProQuest) (July 2008 by Jo Abbott; October 2010 by Nick Huband)
((randomi* w/8 control*) or (triple w/10 blind*) or (double w/10 blind*) or (treble w/10 blind*) or (single w/10 blind*) or (treble w/10 blind*) or ab(double blind*) or ab(randomi*) or (controlled clinical trial)) and (rape or (date and rape) or (male and rape) or (sexual and fetishism) or (child* and sexual and abuse) or (sexual and violence) or (sex and identity) or (sex and offender) or (sex and offence) or (sex* and devia*) or (public and masturbate*) or (child and molest*) or (sex* and (murder or tortur* or abus* or fondl*)) or (indecent* and behav*) or (child* and porn*) or (lewd and (behave* or act*)) or (gender and dysphoria) or bestiality or bondag* or bugger* or coprophilia or erotomania or exhibitionism or fetishism or frotteur* or incest or klismaphilia or masochism or molest* or necrophi* or necrophilia or paedoph* or pedoph* or paedophilia or paedophiliacs or paraphil* or paraphilia or paraphiliacs or partialism or pederast* or pedoph* or rape or sadism or sadomasochism or scatalogia or sodom* or sodomy or transsexuals or transvestism or transvestites or urophilia or voyeur* or zoophilia or zoophilia or zoophiliac)
7. EMBASE (Ovid)
1 exp Sex Offenses/
2 exp Paraphilias/
3 exp Sexual Behavior/
4 exp Child Abuse, Sexual/
5 exp "Fetishism (Psychiatric)"/
6 exp Exhibitionism/
7 exp Voyeurism/
8 exp Pedophilia/
9 exp Sadism/
10 exp Masochism/
11 exp Incest/
12 exp Rape/
13 (sex$ adj2 devia$).tw.
14 (public adj2 masturbat$).tw.
15 (child$ adj2 molest$).tw.
16 (child$ adj2 (sex$ or abuse$)).tw.
17 (sex$ adj2 (murder$ or tortur$ or abus$ or fondl$)).tw.
18 (indecen$ adj2 behav$).tw.
19 (child$ adj2 porn$).tw.
20 (lewd$ adj2 (behav$ or act)).tw.
21 bondag$.tw.
22 frotteur$.tw.
23 necrophi$.tw.
24 bugger$.tw.
25 molest$.tw.
26 pederast$.tw.
27 paedoph$.tw.
28 pedoph$.tw.
29 scatologia.tw.
30 necrophilia.tw.
31 zoophilia.tw.
32 coprophilia.tw.
33 urophilia.tw.
34 partialism.tw.
35 klismaphilia.tw.
36 bestiality.tw.
37 sodom$.tw.
38 molest$.tw.
39 paraphil$.tw.
40 voyeur$.tw.
41 or/1‐40
42 clin$.tw.
43 trial$.tw.
44 (clin$ adj3 trial$).tw.
45 singl$.tw.
46 doubl$.tw.
47 trebl$.tw.
48 tripl$.tw.
49 blind$.tw.
50 mask$.tw.
51 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
52 randomi$.tw.
53 random$.tw.
54 allocat$.tw.
55 assign$.tw.
56 (random$ adj3 (allocat$ or assign$)).tw.
57 crossover.tw.
58 57 or 56 or 52 or 51 or 44
59 exp Randomized Controlled Trial/
60 exp Double Blind Procedure/
61 exp Crossover Procedure/
62 exp Single Blind Procedure/
63 exp RANDOMIZATION/
64 59 or 60 or 61 or 62 or 63 or 58
65 41 and 64
8. International Bibliography of Social Sciences (ProQuest)
Query: (((sex* within 2 devia*) or (public* within 2 masturbat*) or
(child* within 2 (sex* or abuse*)) or (child* within 2 porn*) or (child*
within 2 molest*) or (lewd* within 2 (behav* or act)) or (indecen* within
2 behav*) or (sex* within 2 (murder* or tortur* or abus* or fondl*)) or
(partialism or klismaphilia or bestiality* or sodom* or molest* or
paraphil* or voyeur*) or (bondag* or frotteur* or necrophi* or bugger* or
molest* or pederast* or paedoph* or pedoph* or scatalogia or necrophilia
or zoophilia or coprophilia or urophilia)) or(DE=("incest" or "rape")))
and(((single within 3 blind*) or (triple within 3 blind*) or (treble
within 3 blind*)) or(TI=random* or AB=random*) or(TI=trial* or
AB=trial*))
2013 (DE("rape" or "acquaintance rape" or "date rape" or "drug rape" or "gang rape" or "male rape" or "marital rape" or "serial rape") or DE("incest" or "father daughter incest" or "mother son incest") or DE("exhibitionism") or DE("sex offending") OR DE("sexual deviance" or "erotomania" or "frotteurism" or "gender dysphoria" or "necrophilia" or "paedophilia" or "paedophiliacs" or "paraphilia" or "fetishism" or "klismaphilia" or "paraphiliacs" or "sadism" or "sadomasochism" or "masochism" or "sodomy" or "transsexuals" or "transvestism" or "transvestites" or "zoophilia" or "zoophiliacs") or (sex* within 2 devia*) or (public* within 2 masturbat*) or (child* within 2 (sex* or abuse*)) or (child* within 2 porn*) or (child* within 2 molest*) or (lewd* within 2 (behav* or act)) or (indecen* within 2 behav*) or (sex* within 2 (murder* or tortur* or abus* or fondl*)) or (partialism or klismaphilia or bestiality* or sodom* or molest* or paraphil* or voyeur*) or (bondag* or frotteur* or necrophi* or bugger* or molest* or pederast* or paedoph* or pedoph* or scatalogia or necrophilia or zoophilia or coprophilia or urophilia)) and (DE(double blind studies) or (single* near blind*) or TI(double* blind*) or AB(double* blind*) or DE(randomi?ed controlled trials) or TI(random*) or AB(random*))
2014 (DE("rape" or "acquaintance rape" or "date rape" or "drug rape" or "gang rape" or "male rape" or "marital rape" or "serial rape") or DE("incest" or "father daughter incest" or "mother son incest") or DE("exhibitionism") or DE("sex offending") OR DE("sexual deviance" or "erotomania" or "frotteurism" or "gender dysphoria" or "necrophilia" or "paedophilia" or "paedophiliacs" or "paraphilia" or "fetishism" or "klismaphilia" or "paraphiliacs" or "sadism" or "sadomasochism" or "masochism" or "sodomy" or "transsexuals" or "transvestism" or "transvestites" or "zoophilia" or "zoophiliacs") or (sex* within 2 devia*) or (public* within 2 masturbat*) or (child* within 2 (sex* or abuse*)) or (child* within 2 porn*) or (child* within 2 molest*) or (lewd* within 2 (behav* or act)) or (indecen* within 2 behav*) or (sex* within 2 (murder* or tortur* or abus* or fondl*)) or (partialism or klismaphilia or bestiality* or sodom* or molest* or paraphil* or voyeur*) or (bondag* or frotteur* or necrophi* or bugger* or molest* or pederast* or paedoph* or pedoph* or scatalogia or necrophilia or zoophilia or coprophilia or urophilia)) and (DE(double blind studies) or (single* near blind*) or TI(double* blind*) or AB(double* blind*) or DE(randomi?ed controlled trials) or TI(random*) or AB(random*))
9. ISI Proceedings (Web of Science)
# 12 #11 AND #10
# 11 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1
# 10 #9 OR #8
# 9 TS=((singl* OR doubl* OR tripl* OR trebl*) SAME (mask* OR blind*))
# 8 TS=(random* OR crossover)
# 7 TS=(urophilia OR partialism OR klismaphilia OR bestiality OR sodom*)
# 6 TS=(molest* OR paraphil* OR voyeur* OR bondag* OR frotteur* OR necrophi* OR bugger* OR pederast* OR paedoph* OR pedoph* OR scatalogia)
# 5 TS=(zoophilia OR coprophilia OR fetishi* OR exhibitionism OR voyeuris* OR sadis* OR masochis* OR incest* OR rapist* OR rape*)
# 4 TS=(sex* SAME (murder* OR tortur* OR abus* OR fondl*))
# 3 TS=(sex* SAME devia*) OR TS=(public SAME masturbat*) OR TS=(child* SAME molest*) OR TS=(child* SAME sex*)
# 2 TS=(indecen* SAME behav*) OR TS=(child* SAME porn*) OR TS=(lewd* SAME behav*) OR TS=(lewd* SAME act*)
# 1 Topic=((sex* SAME offen*))
10. Science Citation Index (Web of Science)
# 12 #11 AND #10
# 11 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1
# 10 #9 OR #8
# 9 TS=((singl* OR doubl* OR tripl* OR trebl*) SAME (mask* OR blind*))
# 8 TS=(random* OR crossover)
# 7 TS=(urophilia OR partialism OR klismaphilia OR bestiality OR sodom*)
# 6 TS=(molest* OR paraphil* OR voyeur* OR bondag* OR frotteur* OR necrophi* OR bugger* OR pederast* OR paedoph* OR pedoph* OR scatalogia)
# 5 TS=(zoophilia OR coprophilia OR fetishi* OR exhibitionism OR voyeuris* OR sadis* OR masochis* OR incest* OR rapist* OR rape*)
# 4 TS=(sex* SAME (murder* OR tortur* OR abus* OR fondl*))
# 3 TS=(sex* SAME devia*) OR TS=(public SAME masturbat*) OR TS=(child* SAME molest*) OR TS=(child* SAME sex*)
# 2 TS=(indecen* SAME behav*) OR TS=(child* SAME porn*) OR TS=(lewd* SAME behav*) OR TS=(lewd* SAME act*)
# 1 Topic=((sex* SAME offen*))
11. Social Science Citation Index (Web of Science)
# 12 #11 AND #10
# 11 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1
# 10 #9 OR #8
# 9 TS=((singl* OR doubl* OR tripl* OR trebl*) SAME (mask* OR blind*))
# 8 TS=(random* OR crossover)
# 7 TS=(urophilia OR partialism OR klismaphilia OR bestiality OR sodom*)
# 6 TS=(molest* OR paraphil* OR voyeur* OR bondag* OR frotteur* OR necrophi* OR bugger* OR pederast* OR paedoph* OR pedoph* OR scatalogia)
# 5 TS=(zoophilia OR coprophilia OR fetishi* OR exhibitionism OR voyeuris* OR sadis* OR masochis* OR incest* OR rapist* OR rape*)
# 4 TS=(sex* SAME (murder* OR tortur* OR abus* OR fondl*))
# 3 TS=(sex* SAME devia*) OR TS=(public SAME masturbat*) OR TS=(child* SAME molest*) OR TS=(child* SAME sex*)
# 2 TS=(indecen* SAME behav*) OR TS=(child* SAME porn*) OR TS=(lewd* SAME behav*) OR TS=(lewd* SAME act*)
# 1 TS=((sex* SAME offen*))
12. Ovid MEDLINE
1 exp Sex Offenses/
2 exp Paraphilias/
3 exp Sexual Behavior/
4 exp Child Abuse, Sexual/
5 exp "Fetishism (Psychiatric)"/
6 exp Exhibitionism/
7 exp Voyeurism/
8 exp Pedophilia/ (570)
9 exp Sadism/ (461)
10 exp Masochism/
11 exp Incest/
12 exp Rape/
13 (sex$ adj2 devia$).tw.
14 (public adj2 masturbat$).tw.
15 (child$ adj2 molest$).tw.
16 (child$ adj2 (sex$ or abuse$)).tw.
17 (sex$ adj2 (murder$ or tortur$ or abus$ or fondl$)).tw.
18 (indecen$ adj2 behav$).tw.
19 (child$ adj2 porn$).tw.
20 (lewd$ adj2 (behav$ or act)).tw.
21 bondag$.tw.
22 frotteur$.tw.
23 necrophi$.tw.
24 bugger$.tw.
25 molest$.tw.
26 pederast$.tw.
27 paedoph$.tw.
28 pedoph$.tw.
29 scatologia.tw.
30 necrophilia.tw.
31 zoophilia.tw.
32 coprophilia.tw.
33 urophilia.tw.
34 partialism.tw.
35 klismaphilia.tw.
36 bestiality.tw.
37 sodom$.tw.
38 molest$.tw.
39 paraphil$.tw.
40 voyeur$.tw.
41 or/1‐40
42 randomized controlled trial.pt.
43 controlled clinical trial.pt.
44 randomized controlled trials.sh.
45 random allocation.sh.
46 double blind method.sh.
47 single blind method.sh.
48 or/42‐47
49 (animals not humans).sh.
50 48 not 49
51 clinical trial.pt.
52 exp Clinical Trials/
53 (clin$ adj25 trial$).ti,ab.
54 ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab.
55 placebos.sh.
56 placebo$.ti,ab.
57 random$.ti,ab.
58 research design.sh.
59 or/51‐58
60 59 not 49
61 60 not 50
62 comparative study.sh.
63 exp Evaluation Studies/
64 follow up studies.sh.
65 prospective studies.sh.
66 (control$ or prospectiv$ or volunteer$).ti,ab.
67 or/62‐66
68 67 not 49
69 68 not (50 or 61)
70 50 or 61 or 69
71 41 and 70
13 National Criminal Justice Reference Service Abstracts (ncjrs.gov/app/abstractdb/abstractdbsearch.aspx)
Search terms:
sex* offend*
sex* offend* random*
sex* offend* control*
sex* offend* blind*
sex* abus
Sex* violence
14 OpenSIGLE (last searched July 2008; NOT searched for 2011 [unreliable access to interface or records not downloadable]) OpenSIGLE has since been succeeded by OpenGrey (opengrey.eu/)
random* OR "double blind" AND bestiality
random* OR "double blind" AND bondag*
random* OR "double blind" AND bugger*
random* OR "double blind" AND coprophilia*
random* OR "double blind" AND erotomania*
random* OR "double blind" AND exhibition*
random* OR "double blind" AND fetishism
random* OR "double blind" AND frotteur*
random* OR "double blind" AND incest
random* OR "double blind" AND klismaphilia*
random* OR "double blind" AND masochism
random* OR "double blind" AND molest*
random* OR "double blind" AND necrophi*
random* OR "double blind" AND paedoph*
random* OR "double blind" AND paraphil*
random* OR "double blind" AND partialism
random* OR "double blind" AND pederast*
random* OR "double blind" AND pedoph*
random* OR "double blind" AND rape
random* OR "double blind" AND sadism
random* OR "double blind" AND sadomasochism
random* OR "double blind" AND scatalogia
random* OR "double blind" AND sodom*
random* OR "double blind" AND urophilia*
random* OR "double blind" AND voyeur*
random* OR "double blind" AND zoophilia*
random* OR "double blind" AND "sex offen*"
random* OR "double blind" AND "sexual deviance"
random* OR "double blind" AND "public masturbation"
random* OR "double blind" AND "child molestation"
random* OR "double blind" AND "child sexual abuse"
random* OR "double blind" AND "child abuse"
random* OR "double blind" AND murder*
random* OR "double blind" AND tortur*
random* OR "double blind" AND "sexual abuse"
random* OR "double blind" AND fondl*
random* OR "double blind" AND "child porn*"
random* OR "double blind" AND "lewd behav*"
random* OR "double blind" AND "lewd act"
15 PsycINFO (Ovid)
1 exp Sex Offenses/
2 exp PARAPHILIAS/
3 exp Psychosexual Behavior/
4 Child Abuse/
5 exp SADISM/
6 MASOCHISM/
7 Acquaintance Rape/
8 exp Sexual Orientation/
9 Sexual Attitudes/
10 Sexual Risk Taking/
11 Sexual Development/
12 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11
13 ((sex* adj2 devia*) or public masturbat* or child* molest*).mp.
14 (child sex or child abuse or (sex* adj2 murder*)).mp.
15 ((sex* adj2 tortut*) or (sex* adj2 abus*) or (sex* adj2 fondl*)).mp.
16 (indecen* behav* or child* porn* or (lewd* behav* or lewd* act*)).mp.
17 (sex* offen* or (bondag* or frotteur* or necrophi* or bugger* or molest* or pederast*)).mp.
18 (paedoph* or pedoph* or scatalogia or necrophilia or zoophilia or coprophilia or urophilia or partialism or klismaphilia or bestiality or sodom* or molest* or paraphil* or voyeur*).mp.
19 randomi$.tw.
20 singl$.tw.
21 doubl$.tw.
22 trebl$.tw.
23 tripl$.tw.
24 blind$.tw.
25 mask$.tw.
26 (or/20‐23) adj3 (or/24‐25)
27 clin$.tw.
28 trial$.tw.
29 (clin$ adj3 trial$).tw.
30 placebo$.tw.
31 exp PLACEBO/
32 crossover.tw.
33 exp Treatment Effectiveness Evaluation/
34 exp Mental Health Program Evaluation/
35 random$.tw.
36 assign$.tw.
37 allocate$.tw.
38 (random$ adj3 (assign$ or allocate$)).tw.
39 38 or 34 or 33 or 32 or 31 or 30 or 29 or 26 or 19
40 12 or 13 or 14 or 15 or 16 or 17 or 18
41 39 and 40
16 Social Care Onlinescie‐socialcareonline.org.uk/
Searched using the term "SEXUAL OFFENCES"
17 Sociological Abstracts (ProQuest)
Query: ((DE="incest") or (DE="rape") or (DE=("sexual deviation" or
"sodomy")) or ((sex* within 2 devia*) or (public* within 2 masturbat*) or
(child* within 2 (sex* or abuse*)) or (child* within 2 porn*) or (child*
within 2 molest*) or (lewd* within 2 (behav* or act)) or (indecen* within
2 behav*) or (sex* within 2 (murder* or tortur* or abus* or fondl*)) or
(partialism or klismaphilia or bestiality* or sodom* or molest* or
paraphil* or voyeur*) or (bondag* or frotteur* or necrophi* or bugger* or
molest* or pederast* or paedoph* or pedoph* or scatalogia or necrophilia
or zoophilia or coprophilia or urophilia))) and (((single within 3
blind*) or (triple within 3 blind*) or (treble within 3 blind*)) or
(AB=random* or TI=random* or DE=(randomi?ed controlled trial*)))
2013 (DE("rape" or "acquaintance rape" or "date rape" or "drug rape" or "gang rape" or "male rape" or "marital rape" or "serial rape") or DE("incest" or "father daughter incest" or "mother son incest") or DE("exhibitionism") or DE("sex offending") OR DE("sexual deviance" or "erotomania" or "frotteurism" or "gender dysphoria" or "necrophilia" or "paedophilia" or "paedophiliacs" or "paraphilia" or "fetishism" or "klismaphilia" or "paraphiliacs" or "sadism" or "sadomasochism" or "masochism" or "sodomy" or "transsexuals" or "transvestism" or "transvestites" or "zoophilia" or "zoophiliacs") or (sex* within 2 devia*) or (public* within 2 masturbat*) or (child* within 2 (sex* or abuse*)) or (child* within 2 porn*) or (child* within 2 molest*) or (lewd* within 2 (behav* or act)) or (indecen* within 2 behav*) or (sex* within 2 (murder* or tortur* or abus* or fondl*)) or (partialism or klismaphilia or bestiality* or sodom* or molest* or paraphil* or voyeur*) or (bondag* or frotteur* or necrophi* or bugger* or molest* or pederast* or paedoph* or pedoph* or scatalogia or necrophilia or zoophilia or coprophilia or urophilia)) and (DE(double blind studies) or (single* near blind*) or TI(double* blind*) or AB(double* blind*) or DE(randomi?ed controlled trials) or TI(random*) or AB(random*))
18 ZETOCzetoc.mimas.ac.uk/(not searched after 2010)
45 general: zoophil
44 general: voyeur*
43 general: transvestite
42 general: transvestism
41 general: torture
40 general: sodom*
39 general: sadism
38 general: rapist
37 general: rape
36 general: pederast*
35 general: paedoph*
34 general: pedoph*
33 general: partialism
32 general: paraphil*
31 general: necrophi*
30 general: murder*
29 general: molest*
28 general: masochism
27 general: klismaphilia
26 general: frotteur*
25 general: frotter*
24 general: fetish
23 general: exhibitionism
22 general: eroticism
21 general: erotisicm
20 general: erotica
19 general: bugger*
18 general: bondage
17 general: bestiality
16 general: sexual* and devia*
15 general: sex* and violence
14 general: sex* and offending
13 general: sex* and offender*
12 general: sex* and offence*
11 general: child and porn*
10 general: child and porn*
9 general: public and masturb*
8 general: gender and dysphoria
7 general: lewd and behav*
6 general: child and molest
5 general: child and sex and abuse
4 general: indecent and behavior
3 lewd and act
2 general: indecent and behaviour
1 general: sex and abuse
19. clinicaltrials.gov
sex offenders OR paraphilia OR pedophilia OR paedophilia OR rape OR rapist inCONDITION
20 WHO HEALTH ORGANIZATION'S INTERNATIONAL CLINICAL TRIALS REGISTRY PLATFORM (ICTRP)
BASIC SEARCH
Term: “sex offen*”
plus
ADVANCED SEARCH
sex offen* OR paedop* OR pedop* OR paraphilia* OR rapist* IN TITLE
sex offen* OR paedop* OR pedop* OR paraphilia* OR rapist* IN CONDITION
Appendix 2. Methods archived for future updates
Dealing with missing data
In the event of missing data we will make efforts to contact investigators; however, if the data are still unforthcoming and the investigators have not reported conducting their analysis on an intention‐to‐treat basis, then we will consider recommendations from the Cochrane Handbook for Systematic Reviews of Interventions for methods for dealing with missing data (Higgins 2011).
Where the missing data can be assumed to be missing at random (for example, if there is reason to suppose from included studies that participants left the study because they moved from the area or through other evidence that the effects of the intervention were not related to 'dropping out of treatment') we will analyse the available data as presented.
Where it cannot be assumed that the data are missing at random we may attempt to impute the missing data with replacement values, whether by 'last observation carried forward' (if the assessment points are not far apart in time) or by using other methods to impute the missing data accounting for the fact that these were imputed with uncertainty and using statistical models to allow for missing data. We will seek the advice of a statistician on which methods of dealing with missing data are appropriate on a case by case basis.
Assessment of heterogeneity
We will assess the extent of between‐trial differences and the consistency of results of any meta‐analysis in three ways:
by visual inspection of the forest plots;
by performing the Chi2 test of heterogeneity (where a significance level less than 0.10 will be interpreted as evidence of heterogeneity);
by examining the I2 statistic (Higgins 2011; section 9.5.2).
The I2 statistic describes approximately the proportion of variation in point estimates due to heterogeneity rather than sampling error. Heterogeneity may well prove to be a significant problem, therefore we will carry out each analysis twice using a fixed‐effect and a random‐effects model.
Assessment of reporting biases
We will draw funnel plots (effect size versus standard error) if sufficient studies are found. We recognise that symmetry of the plots may indicate publication bias, although it may also represent a true relationship between trial size and effect size. If such a relationship is identified, we will examine the clinical diversity of the studies as a possible explanation (Egger 1997).
Data synthesis
We will synthesise data using both a fixed‐effect and a random‐effects model.
We will perform meta‐analysis where studies are considered to have sufficiently similar participants, interventions, comparators, and outcome measures. We will carry out separate meta‐analyses for separate classes of pharmacological interventions and where there are different comparators, for example, placebo, standard care, or psychological interventions. In carrying out a meta‐analysis, the weight given to each study will be the inverse of the variance so that the more precise estimates (from larger studies with more events) are given more weight.
Subgroup analysis and investigation of heterogeneity
If sufficient studies are found, we will undertake a subgroup analysis by type of offending, severity of offending, conviction versus self report, and by individual 'family' of medication within class of drug (for example, GnRH analogues within the larger class of hormone modulators).
Sensitivity analysis
We will use a sensitivity analysis to assess the impact of study quality if there are sufficient data identified, particularly to consider the potential impact of outcome assessors being blinded, or other factors identified in the risk of bias analysis.
We will also undertake a sensitivity analysis to investigate the robustness of the overall findings where there has been uncertainty or disagreement regarding, for example, the inclusion of studies, data extraction or missing data, or in the event of one or more large studies dominating the results.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bancroft 1974.
| Methods | Design: RCT (cross‐over, Williams Square design; see note 1) | |
| Participants |
Participants: prisoners detained in a high security hospital after having committed sex offences Sex: all male Age: mean = 26.08 years (SD = 3.87, range = 19 to 34 years) Unit of allocation: individual Number randomised: 12 (see note 2) Number completing: 12 Setting: Broadmoor Hospital, Berkshire, England Inclusion criteria: "For inclusion in the study, scope for change in the physiological measurement and one of the other two measurements was required. Arbitrary levels of sexual behaviour ratings (for sexual intercourse a mean score of 3, for sexual activity a means score of 3), of sexual activity (a mean score of 3), of sexual attitude (a mean score of 12 or less), and of erectile response to erotic stimuli ... were used as criteria for inclusion" (p 266, Tennent 1974, in an earlier report of this study) Exclusion criteria: none reported Baseline characteristics: all 12 participants in this study were convicted sex offenders and a number were exceptionally violent. Baseline characteristics of "most recent offence" included: 1 participant with a conviction for manslaughter (with sexual element); 1 guilty of wounding with intent in addition to rape; 1 who had committed indecent assault with an attempt to choke, 1 of assault with a weapon causing actual bodily harm, 1 found guilty of 15 accounts of indecent assault, another of 24 offences of rape or indecent assault, or both, etc. The mean number of previous sexual offences per participant was 5.6; age of victims of assaults ranged from 6 to 50 and were (in the vast majority of cases) female (p 312). Ethnicity and other demographics not reported |
|
| Interventions | Three conditions:
Duration of intervention: 12 weeks Length of follow‐up: none past end of study |
|
| Outcomes |
Primary outcome Recidivism as measured by reconviction, caution or self report: not reported (and not feasible as participants were long‐term patients in a high security setting) Secondary outcomes Capacity for physiological arousal: a sexual activity score was derived from participants' reports on the number of times that masturbation or "any overt sexual acts" led to orgasm (p 310); penile erection whilst watching erotic stimuli (film clips) was also measured in mm by means of a mercury‐in‐rubber gauge (Bancroft 1966; Bancroft 1971) Anomalous urges: measured by the"sexual attitude score" (a semantic differential technique (Marks 1967) using four seven‐point scales where low scores indicate positive interest and high scores that the participant found the stimulus repulsive Dropping out of treatment Adverse events Other outcomes Sexual interest where participants reported the frequency of sexual thoughts in the preceding 7 days on a continuous scale from 0 to 5). We judged this not to be a specific measure of anomalous urges, unlike the 'sexual attitudes score' described above |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Implicit in the Williams square design |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment not reported; attempts to locate investigators were unsuccessful |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Treatment conditions were concealed to participants and staff by using sealed and coded containers prepared by a pharmacist (p 312) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Staff carrying out the testing would not know whether a drug or no treatment was being administered" (p 312) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One participant was removed from the study early on because of depression whilst in the CPA treatment phase. Trial investigators reported that his depression was unlikely to have been due to the treatment and that "another patient . . . replaced" him |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but it seems clear that the published report included all expected outcomes, including those that were pre‐specified |
| Other bias | Low risk | No other obvious sources of bias |
Bradford 1993.
| Methods | Design: RCT (cross‐over) | |
| Participants |
Participants: paraphilic men "who had also recidivated in a variety of sexual crimes" (p 383) Sex: all male Age: mean = 30.5 years (SD = 8.55, range = 19 to 45) Unit of allocation: individual Number randomised: 19 Number completing: 17 Setting: outpatient setting, Ottawa, Canada Inclusion criteria: participants had to be between 18 and 60 years of age and male Exclusion criteria: history of malignancy, cardiovascular disease, deep vein thrombosis and embolism, chronic liver disease, diabetes mellitus, chronic alcoholism, active psychosis, severe chronic depression, sickle cell anaemia or organic brain disease. Participants on any form of medication were excluded Baseline characteristics: all fulfilled the diagnostic criteria for a psychosexual disorder, paraphilia, as outlined in DSM‐III‐R (APA 1987) with, in addition, "a persistence of their condition, that is, it had affected their functioning to the extent that they had been charged with a criminal offense. The paraphilia had to be present for at least 12 months prior to their initial presentation" (p 387). Baseline data on sex hormone profiles, sexual preferences (focusing on rape and paedophilia) were assessed by interview and penile tumescence measurements. Between the 19 participants recruited, 5 were described (under "sexual deviation") as chiefly interested in homosexual paedophilia, 3 in heterosexual paedophilia, 4 reported both homosexual and heterosexual paedophilia; 2 had committed incest; 2 were rapists; 1 was guilty of frotteurism; 1 was reported to be a fetishist, and the last, an exhibitionist. 7 participants had never been convicted of an offence; the mean number of previous convictions was 2.7 per participant (range 0 to 12). Ethnicity and other demographics were not reported |
|
| Interventions | Two conditions:
Duration of intervention: trial lasted 13 months in total and was comprised of a 1‐month baseline (no treatment) period and 4 alternating 3‐month periods of either placebo or CPA Length of follow‐up: none past end of study |
|
| Outcomes |
Primary outcome Recidivism as measured by reconviction, caution or self report: see note 1 Secondary outcomes Capacity for physiological arousal: numbers of orgasms for previous week; responses to erotic stimuli (2‐minute exposure to a slide); arousal measured by penile erection using a mercury‐in‐rubber gauge Anomalous urges: arousal to slide as above, measured by self report and rating scales Anxiety: self reported feelings of anxiety Anger: Buss‐Durkee Hostility Inventory (BDHI) (Buss 1957) Dropping out of treatment Adverse events: (see note 2) Other outcomes Hormone profiles: plasma testosterone, luteinising hormone; follicle‐stimulating hormone Brief Psychiatric Rating Scale (BPRS) ‐ inventory of aggression (a self report measure) (Overall 1962) Sexual interest: score where participants reported the frequency of sexual thoughts in the preceding 7 days on a continuous scale from 0 to 5. We judged this not to be a specific measure of anomalous urges, unlike the 'sexual attitudes score', as in Bancroft 1974 Mood: in addition to anxiety, other 'mood' characteristics, such as 'loss of drive' and 'increased drive', not specified in our protocol were reported |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to allow a judgement to be made |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to allow a judgement to be made |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The treating psychiatrist, nursing, and other medical staff, and the participants were all blind to allocation. However, the trialists admit that if a participant felt fantasies were returning, or were concerned that they might reoffend, they were moved ahead to the next treatment phase. This would cause concern with regard to blinding had participants remained in analysis but it appears they were removed at this point |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Main outcomes measured by self report were generally backed up by physiological measures; however, there is some concern that due to participants' being "moved ahead" to treatment in some cases, staff would have had to be aware of treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 2 participants dropped out (a homosexual paedophile and a "sexually aggressive" man who had reported urges to rape). Both were described by the trial investigators as showing "excellent responses" and judged by them to have dropped out because they felt they no longer required treatment. The latter was rearrested; the former felt "in control" as long as he did not drink |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but it seems clear that the published report included all expected outcomes, including those that were pre‐specified |
| Other bias | High risk | The authors admit in the discussion that "the placebo phase in this study is not a truly inactive phase nor pharmacologically comparable to the baseline phase" (p 396). "Months completed in the study may be fewer than 13 months because if the patient complained that sexual fantasies were returning or they were concerned they might reoffend they were moved ahead to the start of the next three month phase as it was possible that their complaints were due to placebo." |
Cooper 1981.
| Methods | Design: RCT (cross‐over) | |
| Participants |
Participants: men who, with the exception of 1 who had marital problems, demonstrated severe sexual acting‐out with social and legal implications, including, in some cases, the possibility of imprisonment Sex: all male Age: mean = 43.11 years (SD = 12.14, range 30 to 68) Unit of allocation: individual Number randomised: 9 Number completing: 9 Setting: outpatients in a psychiatric hospital, Sarnia, Ontario, Canada Inclusion criteria: unclear (see baseline characteristics) Exclusion criteria: none reported Baseline characteristics: detailed individual characteristics are provided. Only 2 referrals came from courts (for participants charged with homosexuality with juveniles and also incest and/or homosexuality, fetishism, and 'excessive demands on wife'); 3 referrals came from family physicians (regarding 3 men who committed acts of indecent exposure or voyeurism, or both; hypersexuality or homosexuality, or both); 2 jointly from wife and participant due to hypersexuality; 2 by participant himself (homosexuality alone and homosexuality with juveniles). 2 participants would not meet current inclusion criteria (hypersexuality and homosexuality but with no reported paedophilic interest) (p 459). Ethnicity and other demographics not reported Trial investigators note that "in those cases awaiting trial, it was stressed that compliance in no way implied a more lenient judicial outcome" and that "in no case was psychotherapy given" (p 460) |
|
| Interventions | Two conditions:
Duration of trial: 20 weeks in total (a 4‐week 'run in' period before the study began, a 4‐week washout period between drug or placebo phases; and a 4‐week observation period) Length of follow‐up: none past end of study |
|
| Outcomes |
Primary outcome Recidivism as measured by reconviction, caution or self report: unclear but unlikely. It is unclear whether the 'sexual activity' reported is of a criminal nature or not (see note 1) Secondary outcomes Capacity for physiological arousal: spontaneous daytime erections, spontaneous 'sexual outlets to orgasm and ejaculation', ability to orgasm through masturbation Anomalous or deviant urges or desires: sexual interest scores were measured on a scale of 0 to 100, the scale is described as assessing whether such fantasies are 'mildly' or 'intensely' disturbing Anxiety or anger: not systematically collected or reported (see note 2) Adverse events: side effects of medroxyprogesterone Other outcomes Hormone profiles: plasma testosterone |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were described as "allocated randomly" (p 460) to order of treatment (p 460); method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo in identical tablet form to CPA |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All measures were by self report only; it is unclear whether 'sexual interest' required 'confession' of the nature of the interest |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The authors report that to compensate for missing data, appropriate corrections were made, and an analysis of variance was carried out (p 461) |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but it seems clear that the published report included all expected outcomes, including those that were pre‐specified |
| Other bias | Low risk | No obvious indications of other bias |
Hucker 1988.
| Methods | Design: parallel RCT | |
| Participants |
Participants: paedophiles currently charged with a sexual offence against children or convicted of such an offence in the past and instructed to take treatment as a condition of probation Sex: male Age: mean = 40.5 years. No SD or range given Unit of allocation: individual Number randomised: 18 Number completing: 11 Setting: the Forensic Service of the Clarke Institute (Toronto, Canada) Inclusion criteria: primary attraction to children Exclusion criteria: suffering from any medical condition that would "contraindicate participation" (p 230) Baseline characteristics: data provided on IQ scores (mean = 106.7; education (mean years completed = 12.2), and number of previous sex offences (mean = 1.7). 2 neuropsychological tests and a phallometric test to confirm sexual preference for children were also administered. Alcohol and drug use data were collected and reported (p 230, p 233) |
|
| Interventions | 2 conditions:
Both interventions administered orally Duration of trial: 3 months Length of follow‐up: none past end of study |
|
| Outcomes |
Primary outcome Recidivism as measured by reconviction, caution or self report: no data reported Secondary outcomes Capacity for physiological arousal: number of erections, sexual activity (masturbation or intercourse) Anomalous or deviant urges or desires: frequency of sexual fantasies (participants in this trial were all paedophiles. Fantasies were subdivided into those about adults and those about children) Anxiety or mood: anecdotally reported; potentially artefacts of distress whilst awaiting trial Dropping out of treatment: (see note 1) Adverse events: side effects of medroxyprogesterone Other outcomes Hormone profiles: plasma testosterone levels; metabolites; liver enzymes |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was done at a pharmacy; method of sequence generation unknown (Hucker 2012) |
| Allocation concealment (selection bias) | Low risk | Investigator clarified that the preparation of both treatment and placebo was done remotely and in batches by the pharmacy involved. Treating staff were unaware of allocation (Hucker 2012) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Neither participants nor their treating physicians were aware of assignment throughout the study (Hucker 2012) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Neither participants nor their treating physicians were aware of assignment throughout the study at outcome assessment (Hucker 2012) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 1 participant was excluded from the study due to a medical condition (parathyroid tumour). A second was excluded from analysis as hormone analysis showed he was not taking the MPA. 5 participants left of their own accord; these men appeared to have had "higher frequency of fantasies about children" (p 234); investigators themselves were unsure whether this might represent selection bias of a higher risk group unwilling or unable to give up fantasies about children |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but it seems clear that the published report included all expected outcomes, including those that were pre‐specified |
| Other bias | Low risk | The study appeared free of other sources of bias. The investigators made strenuous efforts to assess potential baseline differences between those choosing to participate in the study and those who did not and found, for example, those accepting had generally higher IQ scores. They also compared baseline data for those who dropped out and those who completed the study, and found no significant differences except on fantasies |
Langevin 1979.
| Methods | Design: parallel RCT (see note 1) | |
| Participants |
Participants: men who had exposed themselves on at least 2 occasions
Sex: all male Age: not reported Unit of allocation: individual Number randomised: 37 (prior to 1 of 3 arms of the trial being discontinued) Number completing: 17 Setting: outpatient clinic, Toronto, Ontario, Canada Inclusion criteria: participants had exposed themselves on at least 2 occasions Exclusion criteria: not reported Baseline characteristics: as above. Many of the participants were also voyeurs |
|
| Interventions | Originally, 3 conditions:
Assertion sex offender treatment programme: Assertiveness training involved 15 x 1‐hour sessions of communication‐based training. This focused on communication with females but included attention to other interpersonal problems and was tailored to individuals' own problems, not 'generalised' as per a diagnostic group. Modelling and coaching, video tapes, and readings were used. Therapy was delivered by 2 male and 2 female graduate students (of psychology or sociology) who had been given specialised training. Therapy incorporated principles including appropriate behaviours (Eisler 1973); discriminations of unassertive, assertive, and aggressive behaviours; developing a belief system of personal rights and those of others (Lazarus 1975); and giving and receiving compliments (Lazarus 1973). Other texts were made available (e.g., Alberti 1970) Duration of intervention: 15 weeks Length of follow‐up: "up to two years" (p 278) |
|
| Outcomes |
Primary outcome Recidivism as measured by reconviction, caution, or self report Secondary outcomes Dropping out of treatment Adverse events Other outcomes not used in this review Post‐treatment questionnaires assessing whether participants liked their therapist and whether they felt their treatment was beneficial |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Investigators reported that they "attempted to randomise" (p 277) between male and female therapists for the psychological component of this combined‐intervention trial, but provided no further details. Clarification was requested from the trial investigators, but no further information was available at the time this review was prepared |
| Allocation concealment (selection bias) | Unclear risk | No information reported. Clarification was requested from the trial investigators, but no further information was available at the time this review was prepared |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | It is not possible that participants or staff could be blinded to the psychological portion of this review. No mention of placebo was made |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Recividism was apparently determined from state records; dropping out of treatment were verifiable; the only 'unblindable' outcome (questionnaires) is not reported in this review; the risk of bias for this criterion is therefore assessed as 'low' |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Due to participants discontinuing treatment, the entire first arm of the trial (Provera® only) was dropped by the investigators. 29% (5 participants) dropped out of the assertiveness training part of the trial; 67% dropped out of the combined treatment arm of the study. No indication of intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Trial investigators stated that data from testosterone levels were collected but were 'erratic' and so not reported |
| Other bias | Low risk | The study appeared free of other sources of bias |
McConaghy 1988.
| Methods | Design: parallel RCT | |
| Participants |
Participants: men seeking treatment for anomalous urges and behaviours they felt unable to control Sex: all male Age: mean = 30 years (SD = see note 2, range 16 to 50) Unit of allocation: individual participant Number randomised: 31 (n = 10 M; n = 10 ID; n = 11 M + ID) Number completing: 30 (n = 10 M; n = 10 ID; n = 10 M + ID) Setting: inpatient for duration of ID treatment only; single site; Sydney, Australia Inclusion criteria: male; seeking treatment for anomalous urges and behaviours they felt unable to control Exclusion criteria: active psychosis Baseline characteristics: at recruitment, 17 participants were single, 9 married, 3 separated, and 1 divorced. 22 of the 30 participants met DSM‐III criteria for 1 paraphilia and 8 participants for 2 or more paraphilias. 19 had been convicted for sexual offences; 8 of the remaining 11 who had carried out sexual offences and had not been charged, were paedophiles. 2 participants were of low intelligence and functionally illiterate and a third participant had brain damage as a result of a motor vehicle accident. Another had a chromosomal anomaly and, while rated as normal in terms of IQ score on the WAIS measure (Wechsler 1981), had a lower than normal score on the Wechsler Memory Scale (Wechsler 1945). A 5th participant had schizophrenia in remission and was being treated with fluphenazine decanoate. Ethnicity of participants not reported |
|
| Interventions | Three conditions:
Medroxyprogesterone (M): 150 mg by IM injection; total of 8 injections; 4 injections at 2‐week intervals followed by 4 injections at monthly intervals Imaginal desensitisation (ID): based on hypothesis that anomalous behaviours are driven by a sense of tension and excitement that becomes aversive if behaviour not completed; each participant initially trained to relax; then to visualise situation where they have carried out anomalous behaviour in the past but visualise not completing the behaviour while remaining relaxed; 14 sessions: 2 sessions on day 1, 3 sessions on subsequent 4 days; delivered during a 5‐day admission to a psychiatric ward Duration of intervention: ID = 5 days, M = 6 months Duration of trial: 2 years Length of follow‐up: 1 month and 1 year following treatment |
|
| Outcomes |
Primary outcome Recidivism as measured by reconviction or caution: reports of being charged for sexually anomalous behaviour Secondary outcomes Anomalous urge: participants' report of % reduction in their anomalous urge in response to treatment; independent assessment of change in anomalous desire following treatment; independent assessment of change in anomalous behaviour following treatment Anxiety State: mean scores on State‐Trait Anxiety Inventory (STAI) (Spielberger 1983) Dropping out of treatment Adverse events: side effects of medroxyprogesterone Other outcomes General tension: participants' report of % reduction in their general tension in response to treatment Hormone profiles: plasma testosterone, dihydrotestosterone, LH, FSH, and prolactin |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Insufficient information appeared in the published paper to allow a judgement to be made. Clarification about method of sequence generation was requested from 1 trial investigator, who reported that a random numbers table was used (Blaszczynski 2011) |
| Allocation concealment (selection bias) | High risk | Insufficient information appeared in the published papers to allow a judgement to be made. Clarification about method of allocation concealment was requested from 1 trial investigator, who reported that the first author made no attempts to conceal allocation (Blaszczynski 2011) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The relevant comparison for this review is between a combined pharmacological plus psychological intervention and a psychological intervention. A placebo was not used for the control condition and it was not possible to blind to allocation |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The outcome assessor was not blinded and thus there is a risk of detection bias. This is despite the investigator's observation: "The significant correlations in this study between the assessor's and patients'measures of response and those between both these measures and the patients’ STAI and tension scores further support the validity of the measures of response . . . this suggests that the fact that the assessor in the present study was not blind to the different treatments did not significantly bias his assessments" (p 205, col 1) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At 1 month, 0/10 missing from ID condition; 0/10 missing from M condition; 1/10 (10%) missing* from ID + M condition At 12 months, 0/10 missing from ID condition; 0/10 missing from M condition; 1/10 (10%) missing* from ID + M condition (*1 participant changed his mind after random allocation and withdrew from M treatment) Numbers of missing data are small, and reasons for missing outcome data are likely to be related to true outcome. Investigators emphasise, as in their previous (1985) study, their certainty that solicitors acting for any of their clients would have informed them of any post‐treatment arrests or convictions (p 200) |
| Selective reporting (reporting bias) | Unclear risk | Study protocol is not available but it seems clear that the published report included all expected outcomes, including those that were pre‐specified. However, neither means nor standard deviations were reported for anxiety (only correlations between participants' and assessors' views). These data have been requested from one trial investigator but do not appear to have survived (Blaszczynski 2011) (see note 2 above) |
| Other bias | Low risk | No other obvious source of bias |
Tennent 1974.
| Methods | Design: cross‐over RCT (Williams square design, see note 1) | |
| Participants |
Participants: prisoners detained in a high security hospital after having committed sex offences against children Sex: all male Age: mean = 33.33 years (SD = 10.81, range = 21 to 56) Unit of allocation: individual Number randomised: of 15 volunteers, 13 met the inclusion criteria (see below); of these 12 "with the highest responses" were chosen (p 266). Later 1 of those initially rejected was re‐recruited to replace someone who dropped out as were 2 new volunteers Number completing: 12 Setting: Broadmoor Hospital, Berkshire, England Inclusion criteria: "Arbitrary levels of sexual behaviour ratings (for sexual intercourse a mean score of 3, for sexual activity a means score of 3), of sexual activity (a mean score of 3), of sexual attitude (a mean score of 12 or less), and of erectile response to erotic stimuli ... were used as criteria for inclusion" (p 266) Exclusion criteria: none reported Baseline characteristics: all 12 participants had been convicted sex offenders against children. Baseline characteristics of the most recent offence included 5 participants convicted of completed or attempted acts of anal intercourse with boys between 7 and 16 years of age; 4 participants with convictions for indecent assault against children as young as 6 years of age; 2 convicted of rape against girls between the ages of 4 and 13 years. The mean number of previous sexual offences per participant was 3.1; age of victims of assaults ranged from 4 to 16 years (p 266). Ethnicity and other demographics of participants, e.g., education, marital status, not reported |
|
| Interventions | Three conditions:
The initial route was by oral syrup but due to intolerance and difficulty in controlling dosage this was changed to tablets after the first 6‐week period Duration: each phase lasted 6 weeks; total duration of the study was 36 weeks Length of follow‐up: none beyond study end‐point |
|
| Outcomes |
Primary outcome Not reported (and not feasible as participants were long‐term patients in a high security setting) Secondary outcomes Capacity for physiological arousal: a sexual activity score was derived from data the participant gave on number of times that masturbation or "any overt sexual acts" led to orgasm (p 264); penile erection whilst watching erotic stimuli (film clips) was also measured in mm by means of a mercury‐in‐rubber gauge Anomalous urges: measured by the "sexual attitude score" meant to assess strength of deviant urges (a semantic differential technique) (Marks 1967) using 4 x 7‐point scales where a low number indicated positive interest and a high number that the participant found the stimulus "repulsive" Dropping out of treatment Adverse events Other outcomes Sexual interest: measured by self report where the participant was asked to report the frequency of his sexual thoughts in the preceding 7 days on a continuous scale from 0 to 5. We judged that this was not a measure of "deviant" urges unlike the "sexual attitudes" score reported above |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation of the order of treatments is implicit in the Williams square design |
| Allocation concealment (selection bias) | Unclear risk | Method not reported. Insufficient information to allow a judgement to be made. Efforts to contact investigators were unsuccessful |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Drugs were prepared and labelled by the drug company and the allocation code was kept sealed by the pharmacy. Doctors, nurses, and participants unaware of the code (pp 266‐7). Change in administration of the drugs (syrup to tablet) appears to have been accompanied by a change in the appearance of the placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Investigators stress that the participants did not know the allocation code and that the trial was double‐blind (p 267) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2 patients withdrew in the first week and a third was withdrawn because of depression. Not reported which arm of the trial they were in. New participants were brought in to replace those who dropped out |
| Selective reporting (reporting bias) | Low risk | The trial protocol remains unavailable; however, review authors judge that the published report includes all expected outcomes, including those that were pre‐specified |
| Other bias | Low risk | No other source of bias apparent. Trial investigators report investigators were satisfied that "within the limits of this design... no evidence of placebo effect has been demonstrated" (p 269) |
BDHI ‐ Buss‐Durkee Hostility Inventory BP ‐ benperidol BPRS ‐ Brief Psychiatric Rating Scale CPA ‐ cyproterone acetate CPZ ‐ chlorpromazine DSM‐III‐R ‐ Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised EO ‐ ethinyl oestradiol FSH ‐ follicle‐stimulating hormones ID ‐ imaginal desensitisation IM ‐ intramuscular IQ ‐ intelligence quotient LH ‐ luteinising hormones M ‐ medroxyprogesterone mg ‐ milligrams MPA ‐ medroxyprogesterone acetate N ‐ number P ‐ placebo RCT ‐ randomised controlled trial SD ‐ standard deviation STAI ‐ State‐Trait Anxiety Inventory WAIS ‐ Wechsler Adult Intelligence Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Amelung 2012 | Retrospective observational study of treatment‐seeking paedophiles. No control group |
| Anonymous 1999 | Political commentary |
| Appelt 1974 | Study of patients with oligophrenia, schizophrenia, or abnormal personality treated with CPA. No control group |
| Balon 2000 | Review of the literature on lithium for paraphilias |
| Baron 1977 | Case series of 10 patients treated with CPA for sexual deviancy |
| Belaisch 1997 | Review article |
| Berner 1983 | Study of CPA for sex offenders but no comparable control group |
| Bradford 1995 | Open pilot study of sertraline for paedophilia. No control group |
| Briken 2000 | Case report of a paedophile treated with depot leuprolide acetate who subsequently reoffended and attempted suicide |
| Briken 2001 | Case series of 11 patients with no control group |
| Briken 2002 | Review article |
| Briken 2004 | Case report of 1 paedophilic patient treated with luteinising hormone‐releasing hormone |
| Bártová 1978 | Comparison of participants with paraphilias treated either with lithium or fluphenazine decanoate. Allocation was not random |
| Bártová 1979 | Sample of 40 patients with sexual deviances treated with lithium and diethylstilbestrol. 'Head to head' study with no random allocation |
| Bártová 1986 | Oxyprothepine decanoate, lithium, and CPA ‐ allocation was not random |
| Cooper 1992a | Double‐blind, 2‐dose comparison of MPA and CPA in 10 patients with paraphilias. The authors described the drug order as quasi‐randomised |
| Cooper 1992b | Case report of a paedophile |
| Cooper 1994 | Case report comparing CPA and LA with a paedophile |
| Czeizel 1996 | Single case report of a homosexual paedophile treated with CPA |
| Fedoroff 1995 | Review of treatment choice and compliance of a 100 men with paraphilias. No control group |
| Gagné 1981 | Report of 48 male patients with paraphilias treated with MPA. No control group |
| García‐Fernández 2002 | Case report of patient with De Clérambault's syndrome treated with olanzapine and risperidone |
| Glander 1981 | Summary of the results of treatment of 63 sex offenders or sexual deviants treated with antiandrogen therapy. No control group |
| Gottesman 1993 | Report of 7 patients with paraphilias treated with low‐dose MPA. No control group and no comparator intervention |
| ISRCTN09267489 | Excluded because this trial was never conducted (i.e., stopped before recruitment). Its goal was to administer SSRI or placebo "to determine whether either the healthy sexual functioning (HSF) module of the sex offenders treatment programme or selective serotonin reuptake inhibitor (SSRI) medication have a positive impact on relevant psychological mechanisms associated with sexual offending". The primary outcome of this review (recividism) was not planned as an outcome but sexual obsessions, penile plethysmograph, and impulsivity would have been assessed |
| Kafka 1994 | Cohort study of participants with paraphilias treated with sertraline. No control group |
| Kiersch 1990 | Case series of 8 patients with participants receiving MPA for 16 weeks followed by saline injections (placebo) for 16 weeks. No randomisation of phases and outcome measures were testosterone levels, deviant fantasies, and PPG |
| Klotz 1977 | Review and case series |
| Koo 2013 | Not a RCT. Single group (treatment outcomes of 'chemical castration' on 38 Korean sex offenders |
| Koo 2014 | 2‐group comparison of differing lengths of androgen deprivation therapy conducted in the interest of prostate cancer research, but all participants were male sex offenders who "voluntarily received leuprolide acetate in order to alleviate sexual aberrance". Not randomised |
| Kraus 2007 | SSRIs for paraphilias but no control group |
| Kravitz 1995 | Report of a cohort of 29 men receiving MPA. No control group |
| Krueger 2001 | Case series of 12 participants with paraphilias treated with depot LA. No control group |
| Kruesi 1992 | RCT. This was a 2‐armed cross‐over trial comparing 2 antidepressants, desipramine and clomipramine. A placebo phase was conducted first, to eliminate placebo responders, but there was no placebo phase during the main trial |
| Lehne 2000 | 40‐year follow‐up of the first case of paraphilia treated with MPA |
| Leo 1995 | Case reports of 2 elderly male patients with dementia and problematic sexual behaviour, including exhibitionism, treated with clomipramine |
| McLaughlin 2013 | Case report of ropinirole |
| Meyer 1992 | The comparison was between MPA plus psychotherapy versus psychotherapy but the comparator group were participants who refused drug treatment |
| Mothes 1976 | Letter |
| Moulier 2012 | Single case study measuring changes in brain activation patterns in a paedophile'; control was an age‐matched "healthy control" |
| NCT00379626 | Planned "Cognitive Group and Hormonal Treatment of Sex Offenders" (hormonal treatment not specified) at the Norwegian University of Science and Technology. The objective was to reduce the relapse rate of sex offenders. The primary outcome was cognitive distortions. The study was terminated as "too few patients participated" |
| NCT00601276 | Planned "Comparative Controlled Clinical Trial of Two Pharmacological Treatments of Pedophilia" at the Institut National de la Santé Et de la Recherche Médicale, France. The objective was to compare the therapeutic efficacy of cyproterone acetate (CPA) and leuprolide, with the hypothesis that leuprolide would be more effective. The study was terminated; no reason supplied |
| Polak 2005 | Uncontrolled study of 4 inpatients in a forensic psychiatric hospital |
| Rich 1994 | Case study of a male patient with Huntington's disease who exposed himself, treated with LA |
| Rösler 1998 | Report of a cohort of 28 males with intractable paraphilias treated with the GnRH analogue triptorelin. No control group |
| Schober 2005a | The study compares 5 male paedophiles receiving LA for 12 months followed by saline solution (placebo) for 12 months but with no randomisation of order |
| Schober 2005b | Design of the study was LA plus CBT in phase 1 followed by placebo plus CBT in phase 2 for all participants with no randomisation to different order groups |
| Thibaut 1998 | Review of the literature on antilibidinal medication and surgical castration for sex offenders |
| Zohar 1994 | Case study of fluvoxamine |
| Žourková 2000 | Not a RCT |
CBT ‐ cognitive behavioural therapy CPA ‐ cyproterone acetate GnRH ‐ gonadotropin‐releasing hormone HSF ‐ healthy sexual functioning LA ‐ leuprolide acetate for depot suspension MPA ‐ medroxyprogesterone acetate PPG ‐ penile plethysmography RCT ‐ randomised controlled trial SSRIs ‐ selective serotonin reuptake inhibitors
Characteristics of ongoing studies [ordered by study ID]
Briken 2012.
| Trial name or title | Double‐blind, controlled, clinical trial, planned in Germany to investigate the efficacy of psychotherapy combined with triptorelin in adult male patients with severe pedophilic disorders |
| Methods | RCT (double‐blinded) |
| Participants | Adult men (> 18 years of age) with severe paedophilia within forensic psychiatric hospitals in multiple sites (n = unknown) |
| Interventions | Cognitive behavioural psychotherapy together with intramuscular 3‐monthly injections of triptorelin versus cognitive behavioural treatment together with a placebo |
| Outcomes | 1. Changes in psychosexual characteristics using the Multiphasic Sex Inventory (scale: sexual abuse of children) 2. Changes in the risk of violent sexual behaviour using the Sexual Violence Risk‐20 total score 3. Changes in serum testosterone concentration. Treatment effects will be assessed by comparing baseline values with those at the final examination (month 12) 4. Tolerability |
| Starting date | Unclear |
| Contact information | Prof. Dr. med. Peer Briken, Institute for Sex Research and Forensic Psychiatry, Interdisciplinary Competence Centre for Sexual Health, University Medical Centre Hamburg‐Eppendorf, House W38, Martinistrasse 52, D – 20246, Hamburg, Germany briken@uke.uni‐hamburg.de |
| Notes | "Limitations: The absence of real‐life stimulants to test for actual recidivism limits possible findings. The study will be conducted in agreement with the European GCP‐guideline, all relevant legal requirements, and the legal framework for voluntary treatment of convicted sexual offenders in Germany" (from the abstract) "The study was planned by the principle investigator (first author) and the advisory board ... together with Dr R Phleger GmbH. The study is sponsored by Dr. R. Pfleger GmbH, Germany, with financial and pharmaceutical contributions from Beaufour Ipsen Pharma, France" |
n ‐ number of participants
Differences between protocol and review
A post hoc subgroup analysis by individual 'family' of medication within class of drug (for example, GnRH analogues within the larger class of hormone modulators).
The author byline has changed (addition of Melanie Powney and Jane Dennis, withdrawal of Nadja Smailagic).
The review includes five additional 'proxy' outcomes not specified in the original protocol. This was done because it was decided these admittedly proxy outcomes best assessed inappropriate arousal and stress and had a sound evidence base in terms of being 'dynamic risk factors' for recidivism.
More authors contributed to the scanning and selection of studies than initially described in the protocol.
Plans for assessing the risk of bias to included studies now include 'Other sources of bias'.
Contributions of authors
OK was responsible for the clinical background to the protocol and MF was responsible for the methodology section of the protocol. Lynn Turner and Jo Abbott conducted initial searches in 2007 and 2008 as well as the updated searches in 2010. JD conducted searches in 2013 and 2014. Various review authors (NH, MF, MP, and JD) inspected the identified citations for inclusion and exclusion with a third author adjudicating where there was disagreement (OK). Full papers of the included citation were obtained and reviewed by two authors (MF, NH and/or JD) with a third review author adjudicating (OK) where there was disagreement. Data extraction was carried out by two review authors (MF and JD) with a third adjudicating (NH). 'Risk of bias' tables were completed by two review authors (JD, NH) with a third author adjudicating (OK). Data entry was completed by JD and checked by MF and NH. CD, OK, and JD were responsible for writing the discussion and conclusions.
Sources of support
Internal sources
-
Nottinghamshire Healthcare NHS Trust, UK.
The Trust provided salary support for several authors engaged with the review
External sources
-
NHS Cochrane Collaboration Programme Grant Scheme, UK.
The Grant Scheme paid for some CDPLPG editorial base support (largely for searches, acquisition of papers, and some staff time)
Declarations of interest
Omer Khan ‐ receives payment for providing independent expert psychiatric testimonies for mental health tribunals and other court cases. Omer receives a salary for a substantive post as a Consultant Forensic Psychiatrist, from Priory Secure Services. Michael Ferriter ‐ the Institute of Mental Health at the University of Nottingham (who were at the time 0.5 FTE employer) received a grant from the National Institute for Health Research for the completion of this review (amongst others). Nick Huband ‐ held the post of Clinical Research Fellow with Nottinghamshire Healthcare NHS Trust and the Institute of Mental Health, Nottingham and was employed in that role during the production of this review. Melanie J Powney ‐ at the time of the review, was affiliated with the Forensic Division of Nottinghamshire Healthcare NHS Trust. Jane A Dennis ‐ received payment from the Institute of Mental Health at the University of Nottingham, which had received a grant from the National Institute for Health Research for the completion of this review (amongst others). Jane A Dennis is the Managing Editor of the Social Welfare Group in the Campbell Collaboration. Conor Duggan ‐ whilst employed at the Institute of Mental Health at the University of Nottingham (until 2011) Conor Duggan's institute received money from the Department of Health, who commissioned this work. In October 2011, he began a part‐time appointment as Head of Research and Development for Partnerships in Care, an independent secure hospital provider. In addition, Conor Duggan has recently (January 2015) been invited to participate in a UK Ministry of Justice advisory group, titled "Expert Advisory Group for Evaluation of Sex Offender Treatment Programme", due to begin its work later in the year.
New
References
References to studies included in this review
Bancroft 1974 {published data only}
- Bancroft J, Tennett G, Loucas K, Cass J. The control of deviant sexual behaviour by drugs. 1. Behavioural changes following oestrogens and anti‐androgens. British Journal of Psychiatry 1974;125(1):310‐5. [DOI] [PubMed] [Google Scholar]
Bradford 1993 {published data only}
- Bradford JMW, Pawlak A. Effects of cyproterone acetate on sexual arousal patterns of pedophiles. Archives of Sexual Behavior 1993;22(6):629‐41. [DOI] [PubMed] [Google Scholar]
Cooper 1981 {published data only}
- Cooper AJ. A placebo‐controlled trial of the antiandrogen cyproterone acetate in deviant hypersexuality. Comprehensive Psychiatry 1981;22(5):458‐65. [DOI] [PubMed] [Google Scholar]
Hucker 1988 {published data only}
- Hucker S [pers comm]. Requesting clarification on matters regarding your 1979 and 1988 trial publications [personal communication]. Email to: J Dennis 28 March 2012.
- Hucker S, Langevin R, Bain J. A double blind trial of sex drive reducing medication in pedophiles. Sexual Abuse: A Journal of Research and Treatment 1988;1(2):227‐42. [Google Scholar]
Langevin 1979 {published data only}
- Langevin R, Paitich D, Hucker S, Newman S, Ramsay G, Pope S, et al. The effect of assertiveness training, Provera and sex of therapist in the treatment of genital exhibitionism. Journal of Behavior Therapy and Experimental Psychiatry 1979;10(4):275‐82. [Google Scholar]
McConaghy 1988 {published data only}
- McConaghy NBA, Blaszczynski A, Kidson W. Treatment of sex offenders with imaginal desensitization and/or medroxyprogesterone. Acta Psychiatrica Scandinavica 1988;77(2):199‐206. [DOI] [PubMed] [Google Scholar]
Tennent 1974 {published data only}
- Tennent G, Bancroft J, Cass J. The control of deviant sexual behavior by drugs: a double‐blind controlled study of benperidol, chlorpromazine, and placebo. Archives of Sexual Behaviour 1974;3(3):261‐71. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Amelung 2012 {published data only}
- Amelung T, Kuhle LF, Konrad A, Pauls A, Beier KM. Androgen deprivation therapy of self‐identifying, help‐seeking pedophiles in the Dunkelfeld. International Journal of Law and Psychiatry 2012;35(3):176‐84. [DOI] [PubMed] [Google Scholar]
Anonymous 1999 {published data only}
- Anonymous. The chemical castration of peodophiles [La castration chimique des pédophiles divise la classe politique autrichienne]. Medecine et Hygiene 1999;27(2268):1697. [0025‐6749] [Google Scholar]
Appelt 1974 {published data only}
- Appelt M, Floru L. The effect on sexuality of cyproterone acetate. International Pharmacopsychiatry 1974;9(2):61‐76. [PubMed] [Google Scholar]
Balon 2000 {published data only}
- Balon R. Lithium for paraphilias? Probably not. Journal of Sex & Marital Therapy 2000;26(4):361‐3. [DOI] [PubMed] [Google Scholar]
Baron 1977 {published data only}
- Baron DP, Unger HR. A clinical trial of cyproterone acetate for sexual deviancy. New Zealand Medical Journal 1977;85(587):366‐9. [PubMed] [Google Scholar]
Bártová 1978 {published data only}
- Bártová D, Náhunek K, Švestka J. Pharmacological treatment of deviant sexual behaviour. Activitas Nervosa Superior 1978;20(1):72‐4. [PubMed] [Google Scholar]
Bártová 1979 {published data only}
- Bártová D, Náhunek J, Švestka J, Hajnová R. Comparative study of prophylactic lithium and diethylstilbestrol in sexual deviants. Activitas Nervosa Superior 1979;21(3):163‐4. [PubMed] [Google Scholar]
Bártová 1986 {published data only}
- Bártová D, Burešová A, Hajnová J, Švestaka J, Tich P. The effect of oxyprothepine decanoate, lithium and cyproterone acetate on deviant sexual behavior [Účinek oxyprothepin dekanoátu lithia a cyproteron acetátu na deviantní sexuální chování]. Ceskoslovenska Psychiatrie 1986;82(6):355‐60. [PubMed] [Google Scholar]
Belaisch 1997 {published data only}
- Belaisch J, Kervasdoué A. Sexual violence; the hormonal treatment [Violences sexuelles: ie traitement hormonal]. Contraception Fertilité Sexualité 1997;25(9):694‐9. [PubMed] [Google Scholar]
Berner 1983 {published data only}
- Berner W, Brownstone G, Sluga W. The cyproteronacetate treatment of sexual offenders. Neuroscience & Biobehavioral Reviews 1983;7(3):441‐3. [DOI] [PubMed] [Google Scholar]
Bradford 1995 {published data only}
- Bradford JMW. An open pilot study of sertraline in the treatment of outpatients with pedophilia. Annual Meeting of the American Psychiatric Association. 1995; Vol. 148.
Briken 2000 {published data only}
- Briken P, Berner W, Noldus J, Nika E, Michl U. Treatment of paraphilia and sexually aggressive impulsive behavior with the LHRH‐agonist leuprolide acetate [Therapie mit dem LHRH‐agonisten leuprorelinacetat bei paraphilien und sexuell aggressiven Impulshandlungen]. Der Nervenarzt 2000;71(5):380‐5. [DOI] [PubMed] [Google Scholar]
Briken 2001 {published data only}
- Briken P, Nika E, Berner W. Treatment of paraphilia with luteinizing hormone‐releasing hormone agonists. Journal of Sex & Marital Therapy 2001;27(1):45‐55. [DOI] [PubMed] [Google Scholar]
Briken 2002 {published data only}
- Briken P. Pharmacotherapy of paraphilias with luteinizing hormone‐releasing hormone agonists. Archives of General Psychiatry 2002;59(5):469‐70. [DOI] [PubMed] [Google Scholar]
Briken 2004 {published data only}
- Briken P, Hill A, Berner W. A relapse in pedophilic sex offending and subsequent suicide attempt during luteinizing hormone‐releasing hormone treatment. Journal of Clinical Psychiatry 2004;65(10):1429. [DOI] [PubMed] [Google Scholar]
Cooper 1992a {published data only}
- Cooper AJ, Sandhu S, Losztyn S, Cernovsky Z. A double‐blind placebo controlled trial of medroxyprogesterone acetate and cyproterone acetate with seven pedophiles. Canadian Journal of Psychiatry 1992;37(10):687‐93. [DOI] [PubMed] [Google Scholar]
Cooper 1992b {published data only}
- Cooper AJ, Cernovsky Z, Magnus RV. The long‐term use of cyproterone acetate in pedophilia: a case study. Journal of Sex & Marital Therapy 1992;18(4):292‐302. [DOI] [PubMed] [Google Scholar]
Cooper 1994 {published data only}
- Cooper AJ, Cernovsky ZZ. Comparison of cyproterone acetate (CPA) and leuprolide acetate (LHRH agonist) in a chronic pedophile: a clinical case study. Biological Psychiatry 1994;36(4):269‐71. [DOI] [PubMed] [Google Scholar]
Czeizel 1996 {published data only}
- Czeizel E. Chemical castration in homosexual pedophilia. Orvosi Hetilap 1996;137(1):23‐5. [PubMed] [Google Scholar]
Fedoroff 1995 {published data only}
- Fedoroff JP. Antiandrogens vs. serotonergic medications in the treatment of sex offenders: a preliminary compliance study. Canadian Journal of Human Sexuality 1995;4(2):111‐22. [Google Scholar]
Gagné 1981 {published data only}
- Gagné P. Treatment of sex offenders with medroxyprogesterone acetate. American Journal of Psychiatry 1981;138(5):644‐6. [DOI] [PubMed] [Google Scholar]
García‐Fernández 2002 {published data only}
- García‐Fernández L, Alcántara Lapaz AG, Martinez Herrera MJA. Paranoia erotica (Clerambault syndrome) successfully treated with risperidone. Annals of Pharmacotherapy 2002;36(12):1972‐3. [DOI] [PubMed] [Google Scholar]
Glander 1981 {published data only}
- Glander HJ. Anti‐androgenic treatment of sexual deviations from an andrological point of view. Deutsche Gesundheitswesen 1981;36(44):1873‐8. [Google Scholar]
Gottesman 1993 {published data only}
- Gottesman HG, Schubert DS. Low‐dose oral medroxyprogesterone acetate in the management of the paraphilias. Journal of Clinical Psychiatry 1993;54(5):183‐8. [PubMed] [Google Scholar]
ISRCTN09267489 {unpublished data only}
- Grubin D. A randomised controlled trial to investigate the effectiveness of the healthy sexual functioning module and selective serotonin reuptake inhibitor medication to treat deviant sexual arousal as part of the HM prison sex offender treatment programme. http://bit.ly/1yLMQ7E (accessed April 2014).
Kafka 1994 {published data only}
- Kafka MP. Sertraline pharmacotherapy for paraphilias and paraphilia‐related disorders: an open trial. Annals of Clinical Psychiatry 1994;6(3):189‐95. [DOI] [PubMed] [Google Scholar]
Kiersch 1990 {published data only}
- Kiersch TA. Treatment of sex offenders with Depo‐Provera. Bulletin of the American Academy of Psychiatry and the Law 1990;18(2):179‐87. [PubMed] [Google Scholar]
Klotz 1977 {published data only}
- Klotz HP. Effects of an antitestosterone agent (cyproterone acetate) on sex behavior in man [Les effets d'un anti‐testostérone (acétate de cyprotérone) sur le comportement sexuel de l'homme]. Problèmes Actuels d Endocrinologie et de Nutrition 1977;21:87‐105. [PubMed] [Google Scholar]
Koo 2013 {published data only}
- Koo KC, Shim GS, Park HH, Rha KH, Choi YD, Chung BH, et al. Treatment outcomes of chemical castration on Korean sex offenders. Journal of Forensic and Legal Medicine 2013;20(6):563‐6. [DOI] [PubMed] [Google Scholar]
Koo 2014 {published data only}
- Koo KC, Lee DH, Kim KH, Lee SH, Hong CH, Hong SJ, et al. Unrecognized kinetics of serum testosterone: impact on short‐term androgen deprivation therapy for prostate cancer. Yonsei Medical Journal 2014;55(3):570‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kraus 2007 {published data only}
- Kraus C, Strohm K, Hill A, Habermann N, Berner W, Briken P. Selective serotonine reuptake inhibitors (SSRI) in the treatment of paraphilia. Fortschritte der Neurologie‐Psychiatrie 2007;75(6):351‐6. [DOI] [PubMed] [Google Scholar]
Kravitz 1995 {published data only}
- Kravitz HM, Haywood TW, Kelly J, Wahlstrom C, Liles S, Cavanaugh JL Jr. Medroxyprogesterone treatment for paraphiliacs. Bulletin of the American Academy of Psychiatry and the Law 1995;23(1):19‐33. [PubMed] [Google Scholar]
Krueger 2001 {published data only}
- Krueger RB, Kaplan MS. Depot‐leuprolide acetate for treatment of paraphilias: a report of twelve cases. Archives of Sexual Behavior 2001;30(4):409‐22. [DOI] [PubMed] [Google Scholar]
Kruesi 1992 {published data only}
- Kruesi MJP [pers comm]. Clarification sought on methods [personal communication]. Email and telephone conversation with: J Dennis 27‐28 March 2012.
- Kruesi MJP, Fine S, Valladares L, Phillips RA, Rapoport JL. Paraphilias: a double‐blind crossover comparison of clomipramine versus desipramine. Archives of Sexual Behavior 1992;21(6):587‐93. [DOI] [PubMed] [Google Scholar]
Lehne 2000 {published data only}
- Lehne GK, Money J. The first case of paraphilia treated with depo‐provera: 40‐year outcome. Journal of Sex Education and Therapy 2000;25(4):213‐20. [Google Scholar]
Leo 1995 {published data only}
- Leo RJ, Kim KY. Clomipramine treatment of paraphilias in elderly demented patients. Journal of Geriatric Psychiatry and Neurology 1995;8(2):123‐4. [DOI] [PubMed] [Google Scholar]
McLaughlin 2013 {published data only}
- McLaughlin T, Oscar‐Berman M, Simpatico T, Giordano J, Jones S, Barh D, et al. Hypothesizing repetitive paraphilia behavior of a medication refractive Tourette's syndrome patient having rapid clinical attenuation with KB220Z‐Nutrigenomic Amino‐Acid Therapy (NAAT). Journal of Behavioral Addictions 2013;2(2):117‐24. [DOI] [PubMed] [Google Scholar]
Meyer 1992 {published data only}
- Meyer III WJ, Cole C, Emory E. Depo Provera treatment for sexual offending behavior: an evaluation of outcome. Bulletin of the American Academy of Psychiatry and Law 1992;20(3):249‐59. [PubMed] [Google Scholar]
Mothes 1976 {published data only}
- Mothes C. Cyproterone acetate. Lancet 1976;308(7993):1020. [DOI] [PubMed] [Google Scholar]
Moulier 2012 {published data only}
- Moulier V, Fonteille V, Pelegrini‐Issac M, Cordier B, Baron‐Laforet S, Boriasse E, et al. A pilot study of the effects of gonadotropin‐releasing hormone agonist therapy on brain activation pattern in a man with pedophilia. International Journal of Offender Therapy and Comparative Criminology 2012;56(1):50‐60. [DOI] [PubMed] [Google Scholar]
NCT00379626 {unpublished data only}
- Nøttestad JA. Cognitive and hormonal treatment of sex offenders. www.clinicaltrials.gov/show/NCT00379626 (accessed 7 June 2014).
NCT00601276 {unpublished data only}
- Stolerau I. Comparison of two pharmacological treatments of pedophilia (PCNET). www.clinicaltrials.gov/show/NCT00601276 (accessed 7 June 2014).
Polak 2005 {published data only}
- Polak MA, Nijman H. Pharmacological treatment of sexually aggressive forensic patients. Psychology, Crime & Law 2005;11(4):457‐65. [Google Scholar]
Rich 1994 {published data only}
- Rich SS, Ovsiew F. Leuprolide acetate for exhibitionism in Huntington's disease. Movement Disorders 1994;9(3):353‐7. [DOI] [PubMed] [Google Scholar]
Rösler 1998 {published data only}
- Rösler A, Witztum E. Treatment of men with paraphilia with a long‐acting analogue of gonadotropin‐releasing hormone. New England Journal of Medicine 1998;338(7):416‐22. [DOI] [PubMed] [Google Scholar]
Schober 2005a {published data only}
- Schober JM, Kuhn PJ, Kovacs PG, Earle JH, Byrne PM, Fries RA. Leuprolide acetate suppresses pedophilic urges and arousability. Archives of Sexual Behavior 2005;34(6):691‐705. [DOI] [PubMed] [Google Scholar]
Schober 2005b {published data only}
- Schober JM, Kuhn PF, Kovacs PG, Earle JH, Byrne PM, Fries RA. Leuprolide acetate suppresses pedophilic urges and arousability. Archives of Sexual Behavior 2005;34(6):691‐705. [DOI] [PubMed] [Google Scholar]
Thibaut 1998 {published data only}
- Thibaut F, Kuhn JM, Cordier B, Petit M. Hormonal treatment of sex offenders [Les traitments hormonaux de las délinquance sexuelle]. L'Encéphale 1998;24(2):132‐7. [PubMed] [Google Scholar]
Zohar 1994 {published data only}
- Zohar J, Kaplan Z, Benjamin J. Compulsive exhibitionism successfully treated with fluvoxamine: a controlled case study. Journal of Clinical Psychiatry 1994;55(3):86‐8. [PubMed] [Google Scholar]
Žourková 2000 {published data only}
- Žourková A, Bártová D, Hajnová R. Alternatives of antiandrogenic therapy in the treatment of paraphiliac behaviour [Alternativy antiandrogenní léčby v ovlivňování prafilního chování]. Česká a Slovenská Psychiatrie 2000;96(7):369‐71. [Google Scholar]
References to ongoing studies
Briken 2012 {published data only}
- Briken P, Berner W. Double‐blind, controlled, clinical trial planned in Germany to investigate the efficacy of psychotherapy combined with triptorelin in adult male patients with severe pedophilic disorders: presentation of the study protocol. Israel Journal of Psychiatry and Related Sciences 2012;49(4):306‐13. [PubMed] [Google Scholar]
Additional references
Abel 2000
- Abel GG, Candice CA. The paraphilias. In: Gelder MG, Lopez‐Ibor Jr JJ, Andreasen NC editor(s). New Oxford Textbook of Psychiatry. Vol. 1, Oxford: Oxford University Press, 2000. [Google Scholar]
Abrahams 2014
- Abrahams N, Devries K, Watts C, Pallitto C, Petzold M, Shamu S, et al. Worldwide prevalence of non‐partner sexual violence: a systematic review. Lancet 2014;383(9929):1648‐54. [DOI] [PubMed] [Google Scholar]
Adi 2002
- Adi Y, Ashcroft D, Browne K, Beech A, Fry‐Smith A, Hyde C. Clinical effectiveness and cost‐consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders. Health Technology Assessment 2002;6(28):1‐66. [PubMed] [Google Scholar]
Ahmadi 2013
- Ahmadi H, Daneshmand S. Androgen deprivation therapy: evidence‐based management of side effects. British Journal of Urology International 2013;111(4):543‐8. [DOI] [PubMed] [Google Scholar]
Alberti 1970
- Alberti R, Emmons ML. Your Perfect Right: A Guide to Assertion Behavior. San Luis Obispo, CA: Impact Press, 1970. [Google Scholar]
Allison 1997
- Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante CM, et al. Antipsychotic‐induced weight gain: a comprehensive research synthesis. American Journal of Psychiatry 1997;156(11):1686‐96. [DOI] [PubMed] [Google Scholar]
AML 2007
- About Megan's Law. Megan's Law. www.about‐megans‐law.com/ (accessed August 2008).
APA 1980
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐III). 3rd Edition. Washington, DC: American Psychiatric Association, 1980. [Google Scholar]
APA 1987
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐III‐R). 3rd Edition. Washington, DC: American Psychiatric Association, 1987. [Google Scholar]
APA 1994
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV). Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
Ashman 2008
- Ashman L, Duggan L. Interventions for learning disabled sex offenders. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD003682.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Avari 1992
- Avari KM, Bhiwgade DA. Effect of depot medroxyprogesterone acetate and testosterone anathate on the testis of albino rats: ultrastructural and biochemical studies. Indian Journal of Experimental Biology 1992;30(12):1118‐27. [PubMed] [Google Scholar]
Baldwin 2003
- Baldwin D, Mayers A. Sexual side effects of antipsychotic and antidepressant drugs. Advances in Psychiatric Treatment 2003;9:202‐10. [Google Scholar]
Bancroft 1966
- Bancroft JHJ, Jones HG, Pullen BR. A simple transducer for measuring penile erection, with comments on its use in the treatment of sexual disorders. Behaviour Research and Therapy 1966;4(3):239‐41. [DOI] [PubMed] [Google Scholar]
Bancroft 1971
- Bancroft JHJ. The application of psychophysiological measures to the assessment and modification of sexual behaviour. Behaviour Research and Therapy 1971;9(2):119‐30. [DOI] [PubMed] [Google Scholar]
Bancroft 1989
- Bancroft J. Human Sexuality and its Problems. Edinburgh: Churchill Livingstone, 1989. [Google Scholar]
Bancroft 2005
- Bancroft J. The endocrinology of sexual arousal. Journal of Endocrinology 2005;186(3):411‐27. [DOI] [PubMed] [Google Scholar]
Barth 2013
- Barth J, Bermetz L, Heim E, Trelle S, Tonia T. The current prevalence of child sexual abuse worldwide: a systematic review and meta‐analysis. International Journal of Public Health 2013;58(3):469‐83. [DOI] [PubMed] [Google Scholar]
Berlin 2009
- Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. Journal of the American Academy of Psychiatry and the Law 2009;37(1):59‐62. [PubMed] [Google Scholar]
Blaszczynski 2011
- Blaszczynski A [pers comm]. Clarification of methods used in McConaghy 1983 and 1985 and confirmation that no data (means, standard deviations) remains on file. Reported that he knew of no other RCTs in the area [personal communication]. Email to: J Dennis 30‐31 August 2011.
Bonta 1995
- Bonta J, Hanson RK. Violent recidivism of men released from prison. Paper Presented at the 103rd Annual Convention of the American Psychological Association; New York; USA. Washington, DC: American Psychological Association, 1995.
Book 2001
- Book AS, Starzyk KB, Quinsey VL. The relationship between testosterone and sexual aggression: a meta‐analysis. Aggression and Violent Behaviour 2001;6(6):579‐99. [Google Scholar]
Briken 2007
- Briken P, Kafka MP. Pharmacological treatment for paraphilic patients and sexual offenders. Current Opinion in Psychiatry 2007;20(6):609‐13. [DOI] [PubMed] [Google Scholar]
Buss 1957
- Buss AH, Durkee A. An inventory for assessing different kinds of hostility. Journal of Consulting and Clinical Psychology 1957;21(4):343‐9. [DOI] [PubMed] [Google Scholar]
Chapman 2004
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders 2004;82(2):217‐25. [DOI] [PubMed] [Google Scholar]
Cormie 2013
- Cormie P, Newton RU, Taaffe DR, Spry N, Joseph, D, Akhlil H, et al. Exercise maintains sexual activity in men undergoing androgen suppression for prostate cancer: a randomized controlled trial. Prostate Cancer and Prostatic Diseases 2013;16(2):170‐5. [DOI] [PubMed] [Google Scholar]
CSM Working Group 2004
- Committee on Safety of Medicines (CSM). Safety of selective serotonin reuptake inhibitor antidepressants. http://goo.gl/okEvdJ (accessed May 2009).
Davies 1974
- Davies TS. Cyproterone acetate for male hypersexuality. Journal of International Medical Research 1974;2(2):159‐63. [DOI] [PubMed] [Google Scholar]
De Voogt 1986
- Voogt HJ, Smith PH, Pavone‐Macaluso M, Pauw M, Suciu S. Cardiovascular side effects of diethylstilbestrol, cyproterone acetate, medroxyprogesterone acetate and estramustine phosphate used for the treatment of advanced prostatic cancer: results from European Organization for Research on Treatment of Cancer trials 30761 and 30762. Journal of Urology 1986;135(2):303‐7. [DOI] [PubMed] [Google Scholar]
Dennis 2012
- Dennis J, Huband N, Khan O, Ferriter M, Jones H, Powney M, et al. Psychological interventions for adults who have sexually offended or are at risk of offending. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD007507.pub2] [DOI] [PubMed] [Google Scholar]
DOH 2008
- Department of Health. Code of Practice: Mental Health Act 1983 (Published pursuant to section 118 of the Act). London: The Stationery Office, 2008. [Google Scholar]
Duggan 2013
- Duggan CF, Hollin CR, Huband N, Clarke M, McCarthy L, Davies S. A comparison of mentally disordered male offenders with and without a sexual offence: their characteristics and outcome. Sex Offender Treatment 2013;8(1):1‐8. [Google Scholar]
Duggan 2014
Eastman 2012
- Eastman N, Adshead G, Fox S, Latham R, Whyte S. Forensic Psychiatry (Oxford Specialist Handbooks in Psychiatry). Oxford: Oxford University Press (OSH Psychiatry), 2012. [Google Scholar]
Edwards 2003
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. The relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experience study. American Journal of Psychiatry 2003;160(8):1453‐9. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey‐Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eher 2010
- Eher R. Antiandrogen treatment of sexual offenders: empirical evidence and criminological facts [Die antiandrogene behandlung von sexualstraftatern vor dem hintergrund der aktuellen wirksamkeitsforschung und der kriminologischen realitat]. Forensische Psychiatrie, Psychologie, Kriminologie 2010;4(1):S27‐32. [DOI: 10.1007/s11757-010-0055-6] [DOI] [Google Scholar]
Eisler 1973
- Eisler RM, Miller PM, Hersen M. Components of assertive behavior. Journal of Clinical Psychology 1973;29(3):295‐9. [DOI] [PubMed] [Google Scholar]
Farrow 2012
- Farrow S [pers comm]. Permission to use a figure from K Gelb's 2007 'Recividism of Sex Offenders Research Paper' [personal communication]. Email to: J Dennis and colleagues 1 October 2012.
Fazal 2006
- Fazal S, Grann M. The population impact of severe mental illness on violent crime. American Journal of Psychiatry 2006;163:1397‐403. [DOI] [PubMed] [Google Scholar]
Firestone 2000
- Firestone P, Bradford JM, Greenberg DM, Serran GA. The relationship of deviant sexual arousal and psychopathy in incest offenders, extrafamilial child molesters, and rapists. Journal of the American Academy of Psychiatry and Law 2000;28(3):303‐8. [PubMed] [Google Scholar]
Friendship 2003
- Friendship C, Mann RE, Beech AR. Evaluation of a national prison‐based treatment program for sex offenders in England and Wales. Journal of Interpersonal Violence 2003;18(7):744‐59. [DOI] [PubMed] [Google Scholar]
Furby 1989
- Furby L, Weinrott MR, Blackshaw L. Sex offender recidivism: a review. Psychological Bulletin 1989;105(1):3‐30. [DOI] [PubMed] [Google Scholar]
Gannon 2010
- Gannon RA, Cortoni F (editors). Female Sexual Offenders: Theory, Assessment and Treatment. Chichester: John Wiley & Sons, 2010. [Google Scholar]
Garcia 2011
- Garcia FD, Thibaut F. Current concepts in the pharmacotherapy of paraphilias. Drugs 2011;71(6):771‐90. [DOI] [PubMed] [Google Scholar]
Gelb 2007
- Gelb K. Recividism of sex offenders research paper. http://goo.gl/uGmOrg (accessed 13 February 2014).
Gooren 2011
- Gooren LJ. Ethical and medical considerations of androgen deprivation treatment of sex offenders. Journal of Clinical Endocrinology and Metabolism 2011;96(12):3628‐37. [DOI] [PubMed] [Google Scholar]
Great Britain 2003
- Great Britain. Chapter 42. Sexual Offences Act 2003 Elizabeth II. London: The Stationery Office, 2003. [ISBN 9 780 105442035] [Google Scholar]
Greenfeld 1997
- Greenfeld LA. Sex offences and offenders: an analysis of data on rape and sexual assault. www.mincava.umn.edu/documents/sexoff/sexoff.html (accessed 1 August 2012).
Grubin 2008
- Grubin D. Medical models and interventions in sexual deviance. In: Laws DR, O'Donohue W editor(s). Sexual Deviancy: Theory, Assessment and Treatment. 2nd Edition. New York: The Guildford Press, 2008. [Google Scholar]
Guay 2009
- Guay DR. Drug treatment of paraphiliac and nonparaphiliac sexual disorders. Clinical Therapeutics 2009;31(1):1‐31. [DOI] [PubMed] [Google Scholar]
Haddad 2004
- Haddad PM. Antipsychotics and diabetes: review of non‐prospective data. British Journal of Psychiatry 2004;184(47):S80‐6. [DOI] [PubMed] [Google Scholar]
Hansen 1997
- Hansen H, Lykke‐Olesen L. Treatment of dangerous sexual offenders in Denmark. Journal of Forensic Psychiatry 1997;8(1):195‐9. [Google Scholar]
Hanson 1998
- Hanson RK, Bussiere MT. Predicting relapse: a meta‐analysis of sexual offender recidivism studies. Journal of Consulting and Clinical Psychology 1998;66(2):348‐62. [DOI] [PubMed] [Google Scholar]
Hanson 2000
- Hanson RK, Harris AJR. Where should we intervene? Dynamic predictors of sexual offense recidivism. Criminal Justice and Behavior 2000;27(1):6‐35. [Google Scholar]
Hanson 2002
- Hanson RK, Gordon A, Harris AJ, Marques JK, Murphy W, Quinsey VL, et al. First report of the collaborative outcome data project on the effectiveness of psychological treatment for sex offenders. Sex Abuse 2002;14(2):169‐94. [DOI] [PubMed] [Google Scholar]
Hanson 2005
- Hanson RK, Morton‐Bourgon KE. The characteristics of persistent sexual offenders: a meta‐analysis of recidivism studies. Journal of Consulting and Clinical Psychology 2005;73(6):1154‐63. [DOI] [PubMed] [Google Scholar]
Hanson 2010
- Hanson RK. Meta‐analysis of treatment outcome in sexual offenders. Oral Presentation of Paper at 11th Conference of the International Association for the Treatment of Sex Offenders in Oslo. 2010.
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG. Chapter 16. Special topics in statistics. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hildebrand 2004
- Hildebrand M, Ruiter C, Vogel C. Psychopathy and sexual deviancy in treated rapists: association with sexual and nonsexual recidivism. Sexual Abuse: A Journal of Research and Treatment 2004;16(1):1‐24. [DOI] [PubMed] [Google Scholar]
Hill 2000
- Hill J, Davis R, Byatt M, Burnside E, Rollinson L, Fear S. Childhood sexual abuse and affective symptoms in women: a general population study. Psychological Medicine 2000;30(6):1283‐91. [DOI] [PubMed] [Google Scholar]
Hood 2002
- Hood R, Shute S, Feilzer M, Wilcox A. Sex offenders emerging from long‐term imprisonment. A study of their long‐term reconviction rates and of parole board members' judgements of their risk. British Journal of Criminology 2002;42(2):371‐94. [Google Scholar]
Hucker 2012
- Hucker S [pers comm]. Requesting clarification on matters regarding your 1979 and 1988 trial publications [personal communication]. Email to: J Dennis 28 March 2012.
Hull 2004
- Hull EM, Muschamp JW, Sato S. Dopamine and serotonin: influences on male sexual behaviour. Physiology and Behaviour 2004;83(2):291‐307. [DOI] [PubMed] [Google Scholar]
Justia US Supreme Court 1997
- Justia US Supreme Court. United States Supreme Court Case: Kansas v. Hendricks ‐ 521 U.S. 346 (1996). http://supreme.justia.com/cases/federal/us/521/346/case.html (accessed 1 September 2012).
Kane 2006
- Kane JM. Tardive dyskinesia circa 2006. American Journal of Psychiatry 2006;163(8):1316‐8. [DOI] [PubMed] [Google Scholar]
Kenworthy 2003
- Kenworthy T, Adams CE, Bilby C, Brooks‐Gordon B, Fenton M. Psychological interventions for those who have sexually offended or are at risk of offending. Cochrane Database of Systematic Reviews 2003, Issue 4. [DOI: 10.1002/14651858.CD004858] [DOI] [PubMed] [Google Scholar]
Langstrom 2013
- Langstrom N, Enebrink P, Lauren E‐M, Lindblom J, Werko S, Hanson RK. Preventing sexual abusers of children from reoffending: systematic review of medical and psychological interventions. BMJ 2013 August 9 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
Lazarus 1973
- Lazarus AA. On assertive behavior: a brief note. Behavior Therapy 1973;4(5):697‐9. [Google Scholar]
Lazarus 1975
- Lazarus AA, Fay A. I Can if I Want To. New York: William Morrow, 1975. [Google Scholar]
Lee 2013
- Lee S, Kang S, Ji D, Baeck S, Lee S, Oh SM, et al. Quantitative LC‐MS/MS method in urine for the detection of drugs used to reverse the effects of chemical castration. Analytical and Bioanalytical Chemistry 2013;405(10):3185‐94. [DOI] [PubMed] [Google Scholar]
Lipscombe 2012
- Lipscombe S. Sarah’s law: the child sex offender disclosure scheme. www.parliament.uk/briefing‐papers/SN01692 (accessed April 2013).
Lösel 2003
- Lösel F, Schmucker M. Protocol for a systematic review of the effects of sexual offender treatment. www.campbellcollaboration.org/lib/project/53/ (accessed September 2014).
Lösel 2005
- Lösel F, Schmucker M. The effectiveness of treatment for sexual offenders: a comprehensive meta‐analysis. Journal of Experimental Criminology 2005;1(1):117‐46. [Google Scholar]
Marks 1967
- Marks IM, Sartorius NH. A contribution to the measurement of sexual attitudes: the semantic differential as a measure of sexual attitude in sexual deviations. Journal of Nervous and Mental Diseases 1967;145(6):441‐51. [DOI] [PubMed] [Google Scholar]
Marshall 1994
- Marshall WL, Pithers WD. A reconsideration of treatment outcome with sex offenders. Criminal Justice and Behavior 1994;21(1):10‐27. [Google Scholar]
Marshall 2007
- Marshall WL, Marshall LE. The utility of the random controlled trial for evaluating sexual offender treatment: the gold standard or an appropriate strategy?. Sexual Abuse: A Journal of Research and Treatment 2007;19(2):175‐91. [DOI] [PubMed] [Google Scholar]
Mazur 1980
- Mazur A, Lamb T. Testosterone and dominance in men. Behavioural and Brain Sciences 1980;21(3):353‐63. [PubMed] [Google Scholar]
McCauley 1997
- McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, et al. Clinical characteristics of women with a history of childhood abuse. JAMA 1997; Vol. 277, issue 17:1362‐8. [PubMed]
McConaghy 1985
- McConaghy N, Armstrong MS, Blaszczynski A. Expectancy, covert sensitization and imaginal desensitization in compulsive sexuality. Acta Psychiatrica Scandinavica 1985;72(2):176‐87. [DOI] [PubMed] [Google Scholar]
McEvoy 1999
- McEvoy G (editor). AHFS Drug Information. Bethesda, Maryland: American Society of Health System Pharmacists, 1999. [Google Scholar]
Mchichi 2004
Molnar 2001
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. American Journal of Public Health 2001;91(5):753‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Montejo 2001
- Montejo AL, Llorca G, Izquierdo JA, Rico‐Villademoros F. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Journal of Clinical Psychiatry 2001;62 Suppl 3:10‐21. [PubMed] [Google Scholar]
Nagayama‐Hall 1995
- Nagayama‐Hall GC. Sexual offender recidivism revisited: a meta‐analysis of recent treatment studies. Journal of Consulting and Clinical Psychology 1995;63(5):802‐9. [DOI] [PubMed] [Google Scholar]
Overall 1962
- Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychological Reports 1962;10:799‐812. [Google Scholar]
Parys 1991
- Parys BT, Hamid S, Thomson RG. Severe hepatocellular dysfunction following cyproterone acetate therapy. British Journal Urology 1991;67(3):312‐30. [DOI] [PubMed] [Google Scholar]
Paton 2005
- Paton C, Ferrier IN. SSRIs and gastrointestinal bleeding. BMJ 2005;331:529‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pierce 1995
- Pierce EJ. Angina pectoris and myocardial infarction with the use of leuprolide acetate. American Journal of Obstetrics and Gynecology 1995;172(4 Pt 1):1323. [DOI] [PubMed] [Google Scholar]
Prentky 1997
- Prentky RA, Lee AFS, Knight RA, Cerce D. Recidivism rates among child molesters and rapists: a methodological analysis. Law and Human Behavior 1997;21(6):635‐59. [DOI] [PubMed] [Google Scholar]
Rao 1998
- Rao MV, Roy GK, Prasannalata SN. Effect of medroxyprogesterone acetate and testosterone enanthate on vas deferens of rats. Indian Journal of Experimental Biology 1998;36(2):157‐61. [PubMed] [Google Scholar]
Reilly 2000
- Reilly DR, Delva NJ, Hudson RW. Protocols for the use of cyproterone, medroxyprogesterone, and leuprolide in the treatment of paraphilia. Canadian Journal of Psychiatry 2000;45(6):559‐63. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rice 2003
- Rice ME, Harris GT. The size and sign of treatment effects in sex offender therapy. Annals of the New York Academy of Sciences 2003;989:428‐40; discussion 441‐5. [DOI] [PubMed] [Google Scholar]
Roila 1993
- Roila F, Crino L, Carloni G, Natalini G. Cyproterone acetate: hepatotoxicity and prostate cancer treatment. Annals of Oncology 1993;4:701. [DOI] [PubMed] [Google Scholar]
Sackett 1996
- Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ 1996;312:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schot 1990
- Schot LPC, Schuurs AHWM. Pathophysiology of bone loss in castrated animals. Journal of Steroid Biochemistry and Molecular Biology 1990;37(3):461‐5. [DOI] [PubMed] [Google Scholar]
Seto 1999
- Seto M, Barbaree H. Psychopathy, treatment behavior, and sex offender recidivism. Journal of Interpersonal Violence 1999;14(12):1235‐48. [DOI] [PubMed] [Google Scholar]
Simon 2000
- Simon LMJ, Felthous AR. Sex offenders: part two/three. Public policy. Behavioral Sciences & the Law 2000;18(2‐3):131‐4. [DOI] [PubMed] [Google Scholar]
Sisk 2006
- Sisk CL. New insights into the neurobiology of sexual maturation. Sexual and Relationship Therapy 2006;21(1):5‐14. [Google Scholar]
Soothill 2000
- Soothill K, Francis B, Sanderson B, Ackerley E. Sex offenders: specialists, generalists or both? A 32‐year criminological study. British Journal of Criminology 2000;40(1):56‐67. [Google Scholar]
Spielberger 1983
- Spielberger CD. Manual for the State‐Trait Anxiety Inventory (STAI). Palo Alto, CA: Consulting Psychologists Press, 1983. [Google Scholar]
Spielberger 1999
- Spielberger CD. STAXI‐2: State‐Trait Anger Expression Inventory‐2. Odessa, FL: Psychological Assessment Resources, Inc, 1999. [Google Scholar]
Stĕpán 1989
- Stĕpán JJ, Lachman M, Zvĕrina J, Pacovský V, Baylink DJ. Castrated men exhibit bone loss: effect of calcitonin treatment on biochemical indices of bone remodelling. Journal of Clinical Endocrinology and Metabolism 1989;69(3):523‐7. [DOI] [PubMed] [Google Scholar]
Swanston 2003
Taylor 1998
- Taylor PJ, Leese M, Williams D, Butwell M, Daly R, Larkin E. Mental disorder and violence. A special (high security) hospital study. British Journal of Psychiatry 1998;172(3):218‐26. [DOI] [PubMed] [Google Scholar]
Thibaut 2010
- Thibaut F, Barra F, Gordon H, Cosyns P, Bradford JM, WFSBP Task Force on Sexual Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of paraphilias. World Journal of Biological Psychiatry 2010;11(4):604‐55. [DOI] [PubMed] [Google Scholar]
Turner 2013
- Turner D, Basdekis‐Jozsa R, Briken P. Prescription of testosterone‐lowering medications for sex offender treatment in German forensic‐psychiatric institutions. Journal of Sexual Medicine 2013;10(2):570‐8. [DOI] [PubMed] [Google Scholar]
Wechsler 1945
- Wechsler D. A standardised memory scale for clinical use. Journal of Psychology 1945;20(1):87‐95. [Google Scholar]
Wechsler 1981
- Wechsler D. Manual for the Wechsler Adult Intelligence Scale. New York: The Psychological Corporation, 1981. [Google Scholar]
White 1998
- White P, Bradley C, Ferriter M, Hatzipetrou L. Managements for people with disorders of sexual preference and for convicted sexual offenders. Cochrane Database of Systematic Reviews 1998, Issue 4. [DOI: 10.1002/14651858.CD000251] [DOI] [PubMed] [Google Scholar]
WHO 1992
- World Health Organization. The ICD‐10 Classification of Mental and Behavioural Disorders. Geneva: World Health Organization, 1992. [Google Scholar]
References to other published versions of this review
Khan 2009
- Khan O, Ferriter M, Huband N, Smailagic N. Pharmacological interventions for those who have sexually offended or are at risk of offending. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007989] [DOI] [PMC free article] [PubMed] [Google Scholar]


