Abstract
Background:
In North Karelia, Finland, the regional electronic health records (EHRs) enable flexible data retrieval and area-level analyses. The aim of this study was to assess the early detection of type 2 diabetes (T2D) in the region and to evaluate the performed activities in order to improve the processes between the years 2012 and 2017.
Methods:
Patients with T2D were identified from the EHRs using the ICD-10 codes registered during any visit to either primary or specialized care. The prevalence of T2D was calculated for the years 2012, 2015, and 2017 on the municipality level. The number of people found in the EHRs with diabetes was compared with the number found in the national register of medication reimbursement rights.
Results:
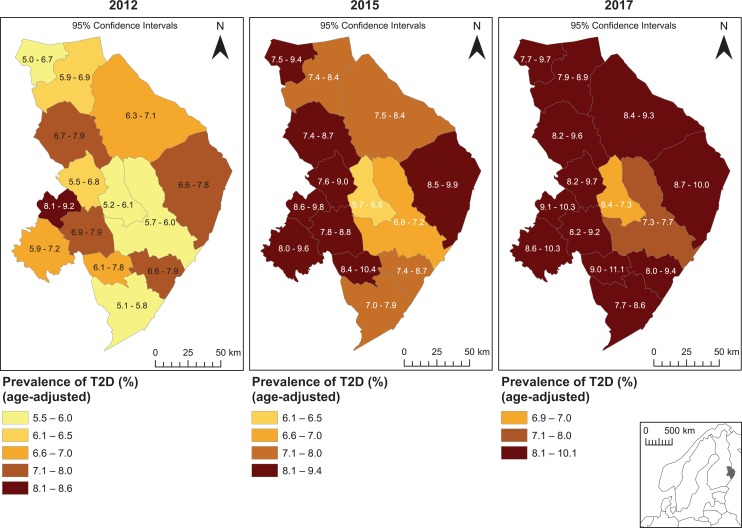
In 2012, the age-adjusted prevalence of T2D in North Karelia varied considerably between municipalities (5.5%-8.6%). These differences indicate variation in the processes of early diagnosis. The findings were discussed in the regional network of health professionals treating patients with T2D, resulting in sharing experiences and best practices. In 2017, the differences had notably diminished, and in most municipalities, the prevalence exceeded 8%. The regional differences in the prevalence and their downward trend were observed both in the EHRs and in the medication reimbursement rights register.
Conclusion:
Clear differences in the prevalence of T2D were detected between municipalities. After visualizing these differences and providing information for the professionals, the early detection of T2D improved and the regional differences decreased. The EHRs are a valuable data source for knowledge-based management and quality improvement.
Keywords: quality improvement, electronic health records, type 2 diabetes, detection, health care, process
Background
The manifestation of type 2 diabetes (T2D) may last several years without noticeable symptoms.1 It has been repeatedly shown that patients with diabetes already have an increased prevalence of complications at the time of diagnosis.2,3 Therefore, more attention needs to be paid to the detection and initiation of care for T2D in order to avoid serious complications.
Electronic health records (EHRs) have great potential for the surveillance of T2D prevalence, as well as for monitoring and improving the processes and quality of diabetes care.4,5 Further, by combining the health records and geographic information, it is possible to map areas where the detection and treatment of diabetes needs to be improved.6-8 The use of EHRs to identify evidence-treatment gaps in the treatment of patients with noncommunicable diseases has been scarce, especially in primary health care.
In the region of the Joint Municipal Authority for North Karelia Social and Health Services (Siun sote) in Finland, the regional EHRs covering both primary and specialized health care enable flexible data retrieval and area-level analyses. In addition, the database of the Finnish Social Insurance Institution contains data on medication reimbursement rights. Using these data sources, the aim of this study was to assess the activities performed in order to improve the detection of T2D in the region between 2012 and 2017 and to evaluate the coverage of T2D diagnoses found in the EHRs.
Methods
The number of patients with T2D in the Siun sote region was identified from the health records. The identification of patients was done using the ICD-10 code E11 that is registered during any visit to either primary or specialized care. The data were collected for the period 2011 to 2017. The age-standardized prevalence of T2D was calculated for the years 2012, 2015, and 2017 on the municipality level in 14 municipalities of the region (Figure 1). Solely patients whose place of domicile was on record and who were alive at the end of 2012, 2015, and 2017 were considered when the prevalence was calculated. The prevalence rates were age-standardized to the population of the study region for each observed year. The rates were mapped using geographic information system software ArcGIS 10.4.1.
Figure 1.
The age-standardized prevalence of T2D in the municipalities of the Joint Municipal Authority for North Karelia Social and Health Services (Siun sote) in 2012, 2015, and 2017.
The statistical database of the Social Insurance Institution of Finland, Kelasto, contains data on medication reimbursement rights. We evaluated the coverage of T2D diagnoses found in the EHRs with the counts received from the medication reimbursement rights database. Eligibility for reimbursement is based upon diagnosis, not the specific medication classes used. However, the registration code for the right to diabetes medication reimbursement in the database includes both type 1 diabetes and T2D and these cannot be separated. For this reason, patients with the diagnosis of type 1 diabetes were also included in the comparison.
Quality improvement activities, such as quarterly workshops for professionals and visits and guidance by diabetologist in charge to improve practices, have been regularly performed inside the regional network of professionals treating diabetes patients in the Siun sote service area since the 1980s. The network has also participated in the development of regional EHR systems and reporting tools since the regional EHR was introduced in 2010. Professionals are able to produce the basic reports themselves from the system. The data from EHRs are also used to identify area-level differences in the detection of T2D and evidence-treatment gaps. The quality-of-care reports have been regularly presented and discussed in the network meetings.
Results
In 2012, the age-adjusted prevalence of T2D according to the EHRs in the Siun sote region varied considerably between municipalities (Figure 1). The highest prevalence of 8.6% in one municipality was significantly higher compared with other municipalities, indicating better detection of the disease. In 2017, the differences between the municipalities had notably diminished, and in most municipalities, the prevalence exceeded 8%. Only in 2 municipalities was the prevalence of diabetes still lower than in other municipalities.
In 2012, 2015, and 2017, the number of patients with diabetes was higher in the data from EHRs than in the medication reimbursement rights data from the Finnish Social Insurance Institution (Table 1), with the exception of 2 municipalities in 2012. The regional differences in the prevalence of T2D and their downward trend from 2012 to 2017 were observed in both data sources.
Table 1.
The Number of Patients with Type 1 Diabetes and T2D According to the EHRs of the Joint Municipal Authority for North Karelia Social and Health Services and the Finnish Register of Medication Reimbursement Rights in 2012, 2015, and 2017, and the Ratio Between Them, Expressed as a Proportion.
| Municipality | 2012 | 2015 | 2017 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| The Health Records of North Karelia | The Register of Medication Reimbursement | The Ratio of Patients With Diabetes in Different Data
Sourcesa
% |
The Health Records of North Karelia | The Register of Medication Reimbursement | The Ratio of Patients With Diabetes in Different Data
Dourcesa
% |
The Health Records of North Karelia | The Register of Medication Reimbursement | The Ratio of Patients With Diabetes in Different Data
Sourcesa
% |
||||
| T1DM (n) | T2DM (n) | Reimbursement Rights (n) | T1DM (n) | T2DM (n) | Reimbursement rights (n) | T1DM (n) | T2DM (n) | Reimbursement Rights (n) | ||||
| Heinävesi | 31 | 323 | 320 | 90.4 | 26 | 427 | 370 | 81.7 | 29 | 437 | 378 | 81.1 |
| Ilomantsi | 32 | 535 | 493 | 86.9 | 37 | 643 | 549 | 80.7 | 31 | 645 | 574 | 84.9 |
| Joensuu | 668 | 3785 | 4001 | 89.8 | 704 | 4560 | 4591 | 87.2 | 676 | 4868 | 4904 | 88.5 |
| Juuka | 36 | 479 | 478 | 92.8 | 36 | 521 | 495 | 88.9 | 39 | 561 | 511 | 85.2 |
| Kitee | 83 | 732 | 803 | 98.5 | 85 | 991 | 977 | 90.8 | 92 | 1075 | 1062 | 91.0 |
| Kontiolahti | 109 | 552 | 594 | 89.9 | 123 | 631 | 682 | 90.5 | 119 | 726 | 756 | 89.5 |
| Lieksa | 100 | 1034 | 896 | 79.0 | 97 | 1187 | 1090 | 84.9 | 93 | 1278 | 1175 | 85.7 |
| Liperi | 90 | 794 | 691 | 78.2 | 94 | 889 | 793 | 80.7 | 90 | 926 | 820 | 80.7 |
| Nurmes | 56 | 640 | 723 | 103.9 | 55 | 771 | 780 | 94.4 | 59 | 803 | 811 | 94.1 |
| Outokumpu | 60 | 703 | 602 | 78.9 | 61 | 721 | 643 | 82.2 | 58 | 747 | 683 | 84.8 |
| Polvijärvi | 47 | 325 | 362 | 97.3 | 45 | 427 | 390 | 82.6 | 43 | 458 | 408 | 81.4 |
| Rääkkylä | 25 | 217 | 189 | 78.1 | 20 | 291 | 242 | 77.8 | 20 | 307 | 261 | 79.8 |
| Tohmajärvi | 23 | 402 | 405 | 95.3 | 29 | 442 | 451 | 95.8 | 32 | 467 | 454 | 91.0 |
| Valtimo | 19 | 178 | 206 | 104.6 | 21 | 251 | 234 | 86.0 | 21 | 247 | 238 | 88.8 |
| Total | 1379 | 10699 | 10443 | 86.5 | 1433 | 12752 | 11917 | 84.0 | 1402 | 13545 | 12657 | 84.7 |
aThe number of people with diabetes in the Finnish Register of Medication Reimbursement Rights divided by the number of people with diabetes in the EHRs of the Joint Municipal Authority for North Karelia Social and Health Services (the ratio is expressed as a proportion).
The ratio between the number of patients in the national medication reimbursement rights register and in the regional EHRs has been very stable during the observed time period (Table 1). However, in some municipalities, the ratio has decreased from the year 2012. This could be partly explained by the improved recording of diagnoses for health care visits in the regional patient register.
Conclusions
Previous studies have shown that it is possible to observe the area-level differences or differences by service provider in processes and quality of care by comparing data from EHRs.9-12 Data are especially useful when explanatory factors other than health care processes (such as demographic determinants) can be taken into account. Further, the possibility to indicate the changes in processes using health record data from different years is valuable.
In this study, quite significant differences were found in the age-adjusted prevalence of T2D between the municipalities in 2012, most likely due to differences in the detection of T2D. These differences considerably diminished from 2012 to 2017, indicating the improvement in the processes resulting from the quality improvement activities which were performed inside the regional network of professionals treating patients with diabetes.
Increasing age is a significant risk factor for T2D. Also, lower socioeconomic status is associated with the higher risk of T2D13-15 and with worse treatment outcomes.16 Apart from age, the population characteristics in this rather remote area are reasonably similar. However, socioeconomic differences could partly explain the lower prevalence of T2D in 2 central municipalities with a younger and more highly educated population.16
The disparities in recording practices could be one reason for the observed differences in the prevalence of T2D between municipalities in the year 2012. However, the data comparisons showed that between the years, the number of patients was very similar in most of the municipalities, both in the EHRs and in the medication reimbursement rights register, and therefore, the differences are not concluded to only be caused by disparities in recording practices. The smaller number of diabetes cases in the medication reimbursement rights register is partly explained by the delay in applying for and granting a special reimbursement right and by the proportion of patients with dietary treatment only. This study shows that the EHRs do not underestimate the number of people with diabetes.
This study confirms that the EHRs are a valuable data source for knowledge-based management and quality improvement. There were real differences in the identification of T2D between the municipalities of North Karelia in 2012, but after visualizing these differences and providing information for the service system and professionals, the detection of T2D improved and the regional differences decreased. The information received from the EHRs needs to be transferred to the field and scaled up to real actions in order to achieve improvements in the processes currently in force. The findings from EHRs in North Karelia have been discussed with the professionals in order to raise awareness of the differences in processes, to find explanations, and to adopt best practices and harmonize them regionally.
Author Biographies
Katja Wikström, PhD, is a research coordinator at the Institute of Public Health and Clinical Nutrition, University of Eastern Finland, and a senior researcher in the Department of Public Health Solutions, National Institute for Health and Welfare.
Maija Toivakka, MSc, is a PhD student in the Department of Geographical and Historical Studies, University of Eastern Finland.
Päivi Rautiainen, MD, PhD, adjunct professor, is an endocrinologist and chief physician in the Joint Municipal Authority for North Karelia Social and Health Services (Siun sote) in Joensuu, Finland.
Hilkka Tirkkonen, MD, is a diabetologist and chief physician in the Joint Municipal Authority for North Karelia Social and Health Services (Siun sote) in Joensuu, Finland.
Teppo Repo, MSc, is a PhD student in the Department of Geographical and Historical Studies, University of Eastern Finland.
Tiina Laatikainen, MD, PhD, a professor of Health Promotion at the Institute of Public Health and Clinical Nutrition, University of Eastern Finland and in the Joint Municipal Authority for North Karelia Social and Health Services (Siun sote), and a research professor in the Department of Public Health Solutions, National Institute for Health and Welfare.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was partly funded by the Strategic Research Council of the Academy of Finland [project IMPRO, 312703, 312704] and the Finnish Diabetes Association.
ORCID iD: Katja Wikström  https://orcid.org/0000-0002-8716-2875
https://orcid.org/0000-0002-8716-2875
References
- 1. Unwin N, Shaw J, Zimmet P, Alberti KGMM. Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med. 2002;19(9):708–723. [DOI] [PubMed] [Google Scholar]
- 2. Harris MI, Klein R, Welborn TA, Knuiman MW. Onset of NIDDM occurs at least 4-7 yr before clinical diagnosis. Diabetes Care. 1992;15(7):815–819. [DOI] [PubMed] [Google Scholar]
- 3. Gedebjerg A, Almdal TP, Berencsi K, et al. Prevalence of micro- and macrovascular diabetes complications at time of type 2 diabetes diagnosis and associated clinical characteristics: a cross-sectional baseline study of 6958 patients in the Danish DD2 cohort. J Diabetes Complications. 2018;32(1):34–40. [DOI] [PubMed] [Google Scholar]
- 4. Klompas M, McVetta J, Lazarus R, et al. Integrating clinical practice and public health surveillance using electronic medical record systems. Am J Prev Med. 2012;102(suppl 3):325–332. [DOI] [PubMed] [Google Scholar]
- 5. Moreno-Iribas C, Sayon-Orea C, Delfrade J, et al. Validity of type 2 diabetes diagnosis in a population-based electronic health record database. BMC Med Inform Decis Mak. 2017;17(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Curtis AJ, Lee WA. Spatial patterns of diabetes related health problems for vulnerable populations in Los Angeles. Int J Health Geogr. 2010;9(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Noble D, Smith D, Mathur R, Robson J, Greenhalgh T. Feasibility study of geospatial mapping of chronic disease risk to inform public health commissioning. BMJ Open. 2012;2(1):e000711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Laranjo L, Rodrigues D, Pereira AM, Ribeiro RT, Boavida JM. Use of electronic health records and geographic information systems in public health surveillance of type 2 diabetes: a feasibility study. JMIR Public Health Surveill. 2016;2(1):e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gill JM, Foy AJ, Jr, Ling Y. Quality of outpatient care for diabetes mellitus in a national electronic health record network. Am J Med Qual. 2006;21(1):13–17. [DOI] [PubMed] [Google Scholar]
- 10. Duftschmid G, Dorda W, Endel G, et al. Fragmentation of diabetes treatment in Austria—an indicator for the need for shared electronic health record systems. Stud Health Technol Inform. 2012;180:667–671. [PubMed] [Google Scholar]
- 11. Guilbert TW, Arndt B, Temte J, et al. The theory and application of UW ehealth-PHINEX, a clinical electronic health record-public health information exchange. WMJ. 2012;111(3):124–133. [PubMed] [Google Scholar]
- 12. Perez-Cuevas R, Doubova SV, Suarez-Ortega M, et al. Evaluating quality of care for patients with type 2 diabetes using electronic health record information in Mexico. BMC Med Inform Decis Mak. 2012;12:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40(3):804–818. [DOI] [PubMed] [Google Scholar]
- 14. Wikström K, Lindström J, Tuomilehto J, et al. Socio-economic differences in dysglycemia and lifestyle-related risk factors in the Finnish middle-aged population. Eur J Public Health. 2011;21(6):768–774. [DOI] [PubMed] [Google Scholar]
- 15. Bijlsma-Rutte A, Rutters F, Elders PJM, Bot SDM, Nijpels G. Socio-economic status and HbA1c in type 2 diabetes: a systematic review and meta-analysis. Diabetes Metab Res Rev. 2018;34(6):e3008. [DOI] [PubMed] [Google Scholar]
- 16. Sikiö M, Tykkyläinen M, Tirkkonen H, Kekäläinen P, Dunbar J, Laatikainen T. Type 2 diabetes care in North Karelia Finland: do area-level socio-economic factors affect processes and outcomes? Diabetes Res Clin Pract. 2014;106(3):496–503. [DOI] [PubMed] [Google Scholar]