Short abstract
Preconceptional maternal bile acid species are significantly associated with birth weight of the offspring.
To the Editor:
We read with interest the publication by Hagström et al. reporting on pregnancy outcomes in patients with liver cirrhosis.1 These authors demonstrated in a large general population cohort that maternal liver cirrhosis is associated with an increased risk of (very) low birth weight (BW). This observation might have important implications for offspring health, as low BW is now an established risk factor for metabolic syndrome–related disease later in life.2 Thus, in our view, it would also be relevant and informative to follow up the children born to mothers with liver cirrhosis. The mechanism underlying the observed decreased BW is unclear. However, in patients with liver cirrhosis, circulating bile acids (BA) are commonly elevated. BA are increasingly recognized as endocrine mediators of a diverse range of (patho)physiological functions, including fertility.3
Adding to the observations of Hagström et al., we investigated whether preconceptional alterations in maternal BA are associated with offspring BW. Serum BA were determined at ovum pickup in women undergoing modified natural‐cycle in vitro fertilization, a procedure close to normal physiology using minimal hormone dosages.3 The institutional review board waived approval, as only anonymized material/data were used, and patients did not object to use of waste material for research. The study was conducted in accordance with the 1975 Declaration of Helsinki. Sixty singleton deliveries, without clinical/laboratory indications for pre‐existing or gestational liver dysfunction, were included. Perinatal data have been published.4 A z‐score for BW after correction for gestational age, offspring gender, and parity was calculated (http://www.perinatreg.nl/). Serum levels of the primary BA chenodeoxycholic and cholic acid (Fig. 1) were significantly correlated with BW z‐scores (r = −0.288, P = 0.026 and r = −0.274, P = 0.034, respectively). After additional correction for maternal body mass index and smoking in a multivariate regression analysis, cholic and chenodeoxycholic acid were still significant predictors of BW (β = −477.9, P = 0.016 and β = −159.8, P = 0.009, respectively), while total and secondary BA remained unrelated.
Figure 1.
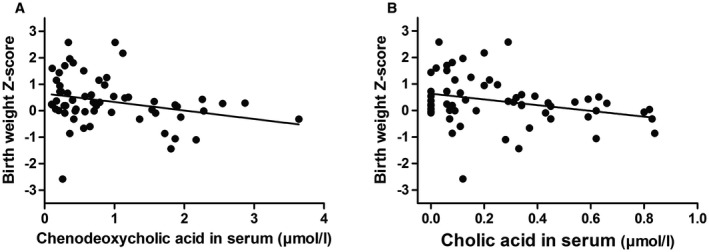
Correlation between maternal serum levels of primary bile acids at the time of conception and birth weight of the neonate. The graphs plot BW z‐score corrected for sex, gestational age at birth, and parity against maternal serum levels of chenodeoxycholic acid (A) or cholic acid (B) at the time of conception.
In summary, the present analysis demonstrates a significant relationship between higher primary BA in maternal serum at the time of conception and low fetal BW. These novel data extend the observations of Hagström et al. and suggest that even in individuals free of liver disease, maternal BA levels are associated with fetal growth.
Acknowledgments
We thank the staff of the Reproductive Medicine Laboratory of the University Medical Center Groningen for collection of patient materials and technical expertise in assisted reproductive medicine and Martijn Koehorst for technical assistance with the bile acid measurements.
Supported by the Netherlands Organization for Scientific Research (VIDI grant 917‐56‐358 to U.J.F.T.).
Potential conflict of interest: Dr. Hoek received grants from Ferring.
References
Author names in bold designate shared co‐first authorship.
- 1. Hagstrom H, Hoijer J, Marschall HU, Williamson C, Heneghan MA, Westbrook RH, et al. Outcomes of pregnancy in mothers with cirrhosis: a national population‐based cohort study of 1.3 million pregnancies. Hepatol Commun 2018;2:1299‐1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barker DJ. The developmental origins of adult disease. J Am Coll Nutr 2004;23(6 Suppl):588S‐595S. [DOI] [PubMed] [Google Scholar]
- 3. Nagy RA, van Montfoort AP, Dikkers A, van Echten‐Arends J, Homminga I, Land JA, et al. Presence of bile acids in human follicular fluid and their relation with embryo development in modified natural cycle IVF. Hum Reprod 2015;30:1102‐1109. [DOI] [PubMed] [Google Scholar]
- 4. Pelinck MJ, Keizer MH, Hoek A, Simons AH, Schelling K, Middelburg K, et al. Perinatal outcome in singletons after modified natural cycle IVF and standard IVF with ovarian stimulation. Eur J Obstet Gynecol Reprod Biol 2010;148:56‐61. [DOI] [PubMed] [Google Scholar]


