Abstract
Background:
Modified radical mastectomy (MRM) is the most common surgery for cancer breast that is associated with marked postoperative pain. Effective control of this pain suppresses the surgical stress response and decreases the opioids and general anesthetics’ needs. This study compared the erector spinae plane (ESP) block and the pectoral plane (PECS) block effects on the opioid consumption postoperatively, stress response, fentanyl needs intraoperatively, pain scores, and incidence of complications in female patients subjected to MRM surgery.
Patients and Methods:
Fifty patients were allocated randomly and divided into two groups. Forty-seven patients were included in the final analysis after exclusion. ESP block group (E group, n = 24) received 20 mL of 0.25% levobupivacaine plus 0.5 μ/kg dexmedetomidine that was injected in-between erector spinae muscle and transverse process. PECS block group (P group, n = 23) received 30 mL of 0.25% levobupivacaine plus 0.5 μg/kg dexmedetomidine divided into 10 mL that was injected between the two pectoralis muscles in the interfascial plane and the other was 20 mL injected between the serratus anterior and the pectoralis minor.
Results:
Postoperative morphine consumption and stress hormone level in P group were significantly lower than E group. The pain scores and number of patients requested analgesic postoperatively showed significantly higher values in E group. Hemodynamic parameters, fentanyl needed intraoperatively and the incidence of postoperative complications recorded no significant difference between the two groups.
Conclusion:
The current study demonstrated that PECS block provides better quality of analgesia than ESP block in patients subjected to MRM operations.
Keywords: Cancer breast, erector spinae plane block, pectoral nerve block, stress response
INTRODUCTION
Female cancer breast statistics shows that in every eight women, there is one develops cancer breast during their lifetime.[1] The most common surgical procedure for cancer breast is modified radical mastectomy (MRM), which removes entire breast with axillary evacuation and a generous amount of skin.[2] Patients undergoing breast surgery experience marked acute pain postoperatively (about 60%). The axillary component of the surgery is responsible of the majority of this pain.[3] When the postoperative pain is not controlled well, this leads to both psychological and physiological negative consequences. While effective control of the acute pain suppresses the surgical stress response and decreases the opioids and general anesthetics needs, that leads to preservation of the immune response.[4] In addition, regional anesthesia can reduce the stress response caused by surgical trauma.[5]
Hence, various analgesic techniques can attenuate postoperative acute pain as, for example, local anesthetic (LA) infiltration, thoracic epidural anesthesia, intercostal, paravertebral, and pectoral plane block (PECS).[6]
Blanco et al. described an interfascial block technique and considered it as a simple alternative to the paravertebral and neuroaxial blocks during breast surgery which is the modified pectoral nerve block. This block acts as a second version of the PECS block as the pectoral nerves, intercostobrachial, intercostals, and long thoracic nerve are blocked.[7] Previous studies reported that it had a considerable analgesic effect with mastectomy surgeries.[8,9]
Forero et al. described ultrasound-guided erector spinae plane (US-ESP) block as a novel analgesic technique in which LA injection is done beneath the erector spinae muscle.[10] Previous studies[11,12,13,14] reported effective postoperative pain reduction with ESP block after radical mastectomy surgery. Nevertheless, few studies have compared the efficacy of ESP block with another block technique. A recent study by Altiparmak et al. showed that US-guided modified PECS block reduced postoperative tramadol consumption and pain scores more effectively than ESP block in the first 24 h after elective unilateral radical mastectomy surgery. However, they reported that the optimum dose and concentration of LA agent is still unclear for ESP block.[15] Hence, this study aimed to compare the influences of US-ESP block and PECS block on the quality of analgesia postoperatively and stress response in patients subjected to MRM surgeries.
PATIENTS AND METHODS
This randomized, prospective, controlled study was carried out after obtaining approval of the Institutional Research Board (R.1901404). All patients participated in the study wrote an informed consent. Patients undergoing unilateral MRM surgeries including axillary lymph node dissection, aged 18–65 years, and with American Society of Anesthesiologists physical status Classes I and II were included in the study. Any patient with known allergy to the study drugs, coagulation disorders, obesity (body mass index [BMI] >35 kg/m2), the injection site infection, or opioid abuse was excluded from the study. Patients were assigned randomly by a computer-generated assignment according to the block used into two groups, ESP block group (E group, n = 24) and PECS block group (P group, n = 23).
The patients were trained to evaluate their pain intensity using the visual analog scale (VAS) using a ruler graded from 0 to 100 mm, where 0 = no pain and 100 = the worst imaginable pain.
General anesthesia
In the operating room, monitoring included electrocardiogram, noninvasive arterial blood pressure, pulse oximeter, capnography, and bi-spectral index monitoring (BIS, Philips Healthcare, Andover, MA). An intravenous line (22 guage) was inserted; then, a 2 mL blood sample was withdrawn in a plasma tube for determination of the baseline level of stress hormones (cortisol and prolactin). After that, isotonic saline infusion was started intravenously with a rate of 15 mL/kg/h. After preoxygenation with 100% oxygen, anesthesia was inducted by 2 μg/kg fentanyl and 2–3 mg/kg propofol; endotracheal tube intubation was facilitated by 0.5 mg/kg atracurium. All patients received intravenous ondansetron 4 mg and dexamethasone 8 mg for nausea and vomiting postoperatively. Maintenance of anesthesia was achieved by isoflurane in a 50% oxygen/air mixture with minimum alveolar concentration that kept a BIS value between 40 and 60 and ventilation parameters to maintain end-tidal CO2 of approximately 35–45 mmHg. Intravenous fentanyl was given in a dose of 0.5 μg/kg as the heart rate (HR) or the blood pressure of any patient increased more than 20% of the basal measurements, and its total amount was recorded. Hemodynamic parameters were recorded before induction and every 15 min till the end of the operation. When the skin closure ended, isoflurane was stopped and neuromuscular reversal was achieved with 0.05 mg/kg neostigmine and 0.02 mg/kg atropine, intravenously. After successful extubation, patients were transported to the postanesthetic care unit (PACU).
Technique of block
The studied block in either group was performed under complete aseptic conditions after induction of anesthesia directly and 15 min before the skin incision with 100 mm 21G needle under the guidance of a linear US probe with a frequency range of 6–13 MHz (Siemens, CA 94043, USA). In the first group (E), ESP block was performed unilaterally while the patients were in a lateral decubitus position, as showed by Chin et al.[11] The block was done at T4 level of the spine with the probe placed 2–3 cm lateral to the spine with a sagittal approach. The needle was inserted into the muscle deeply as the transverse processes and the erector spinae muscle were identified. The needle was directed craniocaudally, and 20 mL of the study solution (0.25% levobupivacaine plus 0.5 μ/kg dexmedetomidine) was administered between erector spinae muscle and transverse process for block performance and LA distributed cranially and caudally.
In the second group (P), PECS block was performed unilaterally. Patients were placed in supine position with their ipsilateral upper limbs abducted 90° below the lateral third of the clavicle. After identification of the axillary vessels, the US-probe was turned inferolaterally till the serratus anterior and the two pectoralis muscles (major and minor) were detected in one plane. The needle was inserted in the interfascial plane between the two pectoralis muscles; 10 mL of the same study solution was injected. After that, the probe was turned toward the axilla, and as the serratus anterior muscle was recognized above the third and fourth ribs, 20 mL of that study solution was injected above this muscle.
Postoperative assessment
As the patients were transported to PACU, where they were followed up and hemodynamic parameters were recorded every 15 min for 1 h. Patients were assessed at 0 (immediately after arrival to PACU) for pain intensity by VAS. On the ward, all patients were evaluated at 2, 4, 6, 12, and 24 h postoperatively for hemodynamics and pain intensity by VAS score. When VAS score was ≥30, intravenous ketorolac 30 mg was given. If VAS was still ≥30, morphine 0.05 mg/kg/dose was given till VAS <30. Number of patients requested analgesic, total morphine consumption in the 24 h were recorded. Side effects such as vascular injury, pneumothorax, hypotension, bradycardia, or arrhythmia were treated and recorded.
Two blood samples were withdrawn at 1 and 24 h postoperatively to assess stress hormone levels (cortisol and prolactin). The blood samples which collected in serum tubes were centrifuged and stored at −20°C till assayed. Serum levels of these hormones were measured by chemiluminescence immunoassay on an Immulite R 1000 automated analyzer (Siemens Healthineers, Erlangen, Germany). The primary outcome measures of this study were total morphine consumption in the first 24 h postoperatively and the levels of stress hormones whereas the secondary outcome measures were the VAS score, number of patients requested analgesic, intraoperative fentanyl needed, and postoperative complications.
Statistical analysis
A preliminary study on ten patients on each group showed a 25% difference in postoperative morphine consumption in the first 24 h between ESP block group and PECS block group (15.8 ± 5.8 mg compared to 11.9 ± 4.5 mg). For 80% power and Type I error of 0.05, Type II error of 0.2 the sample size necessary to detect a 25% difference in the morphine requirements at 24 h postoperatively was calculated as 22 subjects for each group. This study included 25 patients in each group for securing patient dropouts. All data were collected by an Excel program (Microsoft Corporation, Redmond, WA, USA) and were then analyzed with SPSS Version 20.0 (IBM Corporation, Armonk, NY, USA). Kolmogorov–Smirnov test was used to detect normality of data distribution. Quantitative data were described using mean and standard deviation whereas qualitative data were described by numbers and percentages. A Chi-square test was used to examine the relationship between qualitative variables and independent samples, and a t-test was used to compare between 2 groups of quantitative data. P value was considered significant when < 0.05.
RESULTS
Fifty-eight women were screened for the present study. One patient had coagulation disorders, one patient had infection at the site of injection, another one was found to have opioid abuse, and five of the patients declined block procedures, all of them were removed from the study. The remaining 50 patients were allocated into the groups of this study. One patient in E group was lost during follow-up due to hematoma formation that operated again and two patients in P group were also lost during follow-up, one patient failed to rate her pain using VAS, and the other one developed pulmonary embolism.
Hence, the results of 24 patients in the E group and 23 patients in P group were analyzed [Figure 1]. There were no significant difference among the two groups regarding demographic data (age, weight, BMI, and height) and the operative duration [Table 1]. Neither HR nor mean arterial pressure showed any significant difference between both groups intraoperatively, and in PACU, however, they were lower in P group at 2, 4, 6, 12, and 24 h postoperatively at the ward.
Figure 1.
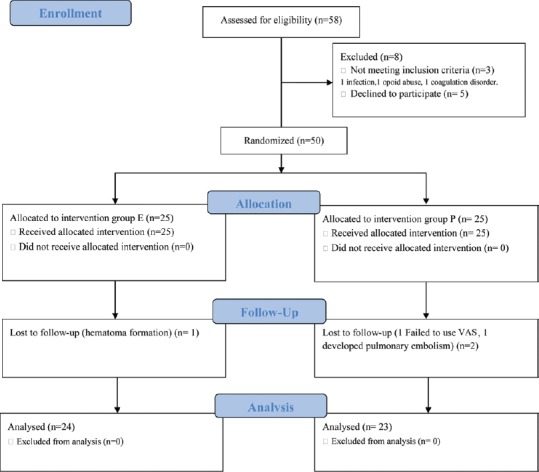
The flow diagram of patient progress through the randomized trial
Table 1.
The demographic data and the operative duration of the studied groups (mean±standard deviation)
| Group E (n=24) | Group P (n=23) | P | |
|---|---|---|---|
| Age (year) | 48.61±10.87 | 49.6±10.51 | 0.75 |
| Weight (kg) | 73.49±11.48 | 73.27±10.57 | 0.95 |
| Height (cm) | 161±40 | 162±37 | 0.93 |
| BMI (kg/m2) | 26.97±5.65 | 27.19±5.46 | 0.89 |
| Operative duration (min) | 90.4±22.82 | 89±21.13 | 0.83 |
Data are in mean±SD. E=ESP. P=PECS. P<0.05 is statistically significant. n=Number of patients, BMI=Body mass index, SD=Standard deviation, ESP=Erector spinae plane, PECS=Pectoral plane block
Total morphine consumption in the first 24 h postoperatively recorded a significant higher value in E group compared with P group (P = 0.001). Moreover, number of patients requested analgesic was significantly higher value in E group (P = 0.016). However, there was no significant difference between the two studied groups regarding the fentanyl needs intraoperatively (P = 0.601) [Table 2].
Table 2.
The analgesic requirements intraoperatively and postoperatively in the studied groups
| Group E (n=24) | Group P (n=23) | P | |
|---|---|---|---|
| Intraoperative fentanyl needs | 116.2±15.6 | 114±12.9 | 0.601 |
| Postoperative morphine consumption | 16.7±7.21 | 10.7±3.12* | 0.001 |
| Number of patients requested analgesic (%) | 19 (79) | 12 (52)* | 0.016 |
*Significant for P compared to E. Data are in mean±SD. Number of patients requested analgesic is expressed as n (%). E=ESP. P=PECS. P<0.05 is significant. n=Number of patients, SD=Standard deviation, ESP=Erector spinae plane, PECS=Pectoral plane block
Although there were no significant differences between the two groups as regards the cortisol and prolactin levels at the basal values (P > 0.05), there were significant decreases in their levels at 1 and 24 h postoperatively in P group compared to E group. In addition, these hormones levels showed a significant decrease in each group at 1 and 24 h postoperatively compared with its basal values (P < 0.05) [Figures 2 and 3].
Figure 2.
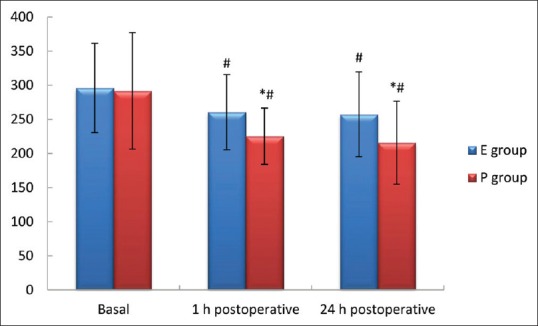
The cortisol levels of the studied groups (μg/dL). Data are in mean ± standard deviation. E = ESP. P = PECS. P<0.05 is significant. *Significant for P in comparison to E, #Significant at 1 h, 24 h postoperative in comparison with basal in the same group. ESP = Erector spinae plane, PECS=Pectoral plane block
Figure 3.
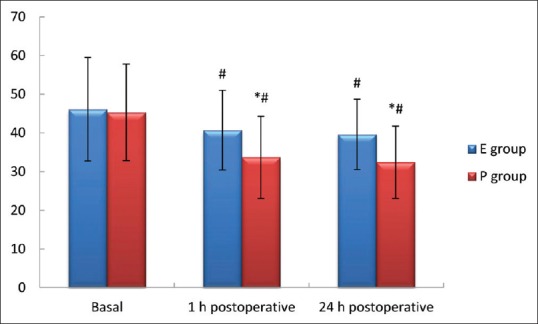
The prolactin levels of the studied groups (ng/mL) data are in mean ± standard deviation. E = ESP, P = PECS. P<0.05 is significant. *Significant for P in comparison to E, #Significant at 1 h, 24 h postoperative in comparison with basal in same group. ESP = Erector spinae plane, PECS=Pectoral plane block
VAS score showed no significant difference between the two studied groups at the postoperative 0 value; however, E group recorded significantly higher values at all other time points compared with P group [Table 3]. There were no significant differences in the incidences of the postoperative complications between both groups.
Table 3.
Postoperative visual analog scale of the studied groups (median and range)
| Group E (n=24) | Group P (n=23) | P | |
|---|---|---|---|
| 0 | 10 (0-20) | 10 (0-20) | 0.298 |
| 2 h | 10 (10-20) | 10 (10-30)* | 0.025 |
| 4 h | 20 (10-30) | 10 (10-30)* | 0.018 |
| 6 h | 20 (10-40) | 20 (10-30)* | 0.021 |
| 12 h | 30 (10-40) | 20 (0-40)* | 0.019 |
| 24 h | 10 (0-30) | 10 (0-30)* | 0.011 |
*Significant for P in comparison with E group. Data are in median and range. E=ESP. P=PECS. P<0.05 is significant. n=Number of patients, ESP=Erector spinae plane, PECS=Pectoral plane block
DISCUSSION
The present study findings showed that P group recorded lower postoperative opioid consumption and stress hormone level than E group. In addition, the pain scores and number of patients requested analgesic were significantly lower in P group. However, hemodynamic parameters and fentanyl needs intraoperatively did not differ between the studied groups. The incidence of postoperative complications in both groups was insignificantly different.
ESP block is a safe alternative to paravertebral block (PVB) due to the usage of the transverse process as a barrier so avoiding injury to the pleura by the needle.[13] US-ESP provides analgesia for either abdominal or thoracic segmental innervation depending on the injection site level.[11] LA spreads craniocaudally through multiple levels after administered beyond the transverse process of T4 level. LA spreads to the thoracic paravertebral space through the costotransverse foramina. Hence, ESP can block dorsal and ventral rami of spinal nerves and their communicants.[16] When thoracic PVB is done in the sitting position, LA spreads almost under the site of injection.[17] Hence, ESP block could be considered as an alternative to PVB with a better cranial and caudal spread. On the other hand, a recent study comparing modified PECS block with thoracic PVB in patients undergoing radical mastectomy surgeries showed that modified PECS block provided a lower opioid consumption and more pain relief, postoperatively than PVB.[18]
Adhikary et al. stated that spread of the radiocontrast dye after ESP block to the intercostal spaces, epidural and neural foraminal in a cadaveric study.[19] Accordingly, ESP block is covering a large surgical area with a wider spread of LA. However, another cadaveric study by Ivanusic et al. reported that the dye was stained the dorsal rami posterior to the costotransverse foramen, and it did not spread anteriorly to involve origins of the ventral and dorsal branches of the thoracic spinal nerves in paravertebral space.[20] Hence, ESP block mechanism is not yet clear, and its action could be affected by various concentrations or volumes of LA. While the modified PECS block affects long thoracic nerves, thoracic intercostal nerves, intercostobrachial nerve, and lateral and medial pectoral nerves. Magnetic resonance imaging studies recorded that LA could spread to the thoracodorsal nerve distribution in PECS block, that leads to regional anesthesia for the chest wall as well as axillary areas.[7]
In the current study, both blocks were achieved after induction of general anesthesia (GA). The spread of LA is affected by various body positions. PECS block is done while the patient is laying supine which gives the advantage of easy positioning under GA. Previous studies performed PECS blocks with the patient laying supine and the LA spread gone cranially and caudally to the injection site in-between T2 and T6.[21,22,23] However, in spite of the US-ESP block is a simple technique, it is almost done while the patients are sitting and awake that may put them in a stress. ESP block was done under GA eliminating this stress effect in the present study. ESP block was achieved while the patient in the lateral decubitus position and after the block procedure was completed the patient was turned to lay supine, rapidly. Therefore, the positional effect on LA spread was eliminated. However, the ESP block is believed as a safer method in comparison with the PVB;[10] Ueshima recorded development of pneumothorax as a complication of ESP block.[24] Accordingly, achieving ESP block while the patient is supine could be safer to face this side effect.
In a previous study, it was preferred to achieve ESP block using 25 mL of 0.25% bupivacaine at the level of T5.[12] The present study performed ESP block at the level of T4 with 20 mL of 0.25% levobupivacaine plus 0.5 μ/kg dexmedetomidine to include the axillary area. Gürkan et al. performed ESP block using 20 mL of 0.25% bupivacaine comparing it with a control group without intervention; they reported that this block decreased morphine consumption significantly in the first 24 h postoperatively.[14]
Stress responses to postoperative pain and surgical trauma lead to various changes in hormones secretion such as cortisol, prolactin, and adrenocorticotrophic hormone and may have deleterious metabolic and cardiovascular effects. Hence, postoperative analgesia has a very important role in the stress response attenuation.[25] The dexmedetomidine attenuation effect of stress in regional technique was in accordance to Nasr and Abdelhamid, who found that caudal dexmedetomidine provided better postoperative analgesic effect and reducing stress response to surgical trauma.[26] Dexmedetomidine lowering the level of cortisol could be explained as it is considered an imidazole that inhibits the synthesis of cortisol when administered by all routes.[27] In the present study, however, the two blocks decreased stress hormone levels compared by basal values, these hormone levels and VAS in addition to the morphine consumption postoperatively, all were recorded significant lower values in the PECS group. Bashandy and Abbas agreed with the present study as they reported that PECS block reduced pain scores during the first 24 h postoperatively in a more effective manner.[6]
The first limitation of this study was that the patients were under GA; that made the sensory area could not be evaluated after block procedures. Hence, it was difficult to know if there was any block failure. Another limitation was that it was not clear whether the total analgesic consumption was related to the block itself or the systemic effects of LA. A third limitation was that the postoperative nausea and vomiting incidence could not be assessed because ondansetron and dexamethasone were routinely applied intraoperatively as a preventive strategy regarding nausea and vomiting in the postoperative period in this study.
CONCLUSION
The modified PECS block lowered postoperative morphine consumption, stress hormone level, and pain scores more effectively than ESP block in the first 24 h after unilateral radical mastectomy surgery. However, further more studies are required to establish the optimum position, dose, and concentration of LA agent for ESP block as these still are unclear.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer J Clin. 2014;64:52–62. doi: 10.3322/caac.21203. [DOI] [PubMed] [Google Scholar]
- 2.Bland KI, Vezedis MP, Copeland EM., 3rd . Breast. In: Schwartz SI, editor. Principles of Surgery. 7th ed. New York: McGraw-Hill; 1999. pp. 576–9. [Google Scholar]
- 3.Fecho K, Miller NR, Merritt SA, Klauber-Demore N, Hultman CS, Blau WS. Acute and persistent postoperative pain after breast surgery. Pain Med. 2009;10:708–15. doi: 10.1111/j.1526-4637.2009.00611.x. [DOI] [PubMed] [Google Scholar]
- 4.Gärtner R, Jensen MB, Nielsen J, Ewertz M, Kroman N, Kehlet H. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302:1985–92. doi: 10.1001/jama.2009.1568. [DOI] [PubMed] [Google Scholar]
- 5.Bozkurt P, Kaya G, Yeker Y, Altintaş F, Bakan M, Hacibekiroglu M, et al. Effectiveness of morphine via thoracic epidural vs. intravenous infusion on postthoracotomy pain and stress response in children. Paediatr Anaesth. 2004;14:748–54. doi: 10.1111/j.1460-9592.2004.01278.x. [DOI] [PubMed] [Google Scholar]
- 6.Bashandy GM, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: A randomized clinical trial. Reg Anesth Pain Med. 2015;40:68–74. doi: 10.1097/AAP.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 7.Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of pecs II (modified pecs I): A novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470–5. doi: 10.1016/j.redar.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Blanco R. The ‘pecs block’: A novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66:847–8. doi: 10.1111/j.1365-2044.2011.06838.x. [DOI] [PubMed] [Google Scholar]
- 9.Blanco R, Garrido Garcia M, Diéguez P, Nebril BA, Lopez alvarez S, Pensado Castineiras A. Analgesic efficacy of blockage of the pectoral nerves in surgery. Cir May Amb. 2011;16:89–93. [Google Scholar]
- 10.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: A novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 11.Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72:452–60. doi: 10.1111/anae.13814. [DOI] [PubMed] [Google Scholar]
- 12.Singh S, Chowdhary NK. Erector spinae plane block an effective block for post-operative analgesia in modified radical mastectomy. Indian J Anaesth. 2018;62:148–50. doi: 10.4103/ija.IJA_726_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Veiga M, Costa D, Brazão I. Erector spinae plane block for radical mastectomy: A new indication.? Rev Esp Anestesiol Reanim (English Edition) 2018;65:112–5. doi: 10.1016/j.redar.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 14.Gürkan Y, Aksu C, Kuş A, Yörükoǧlu UH, Kılıç CT. Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: A randomized controlled study. J Clin Anesth. 2018;50:65–8. doi: 10.1016/j.jclinane.2018.06.033. [DOI] [PubMed] [Google Scholar]
- 15.Altıparmak B, Korkmaz Toker M, Uysal Aİ, Turan M, Gümüş Demirbilek S. Comparison of the effects of modified pectoral nerve block and erector spinae plane block on postoperative opioid consumption and pain scores of patients after radical mastectomy surgery: A prospective, randomized, controlled trial. J Clin Anesth. 2019;54:61–5. doi: 10.1016/j.jclinane.2018.10.040. [DOI] [PubMed] [Google Scholar]
- 16.El-Boghdadly K, Pawa A. The erector spinae plane block: Plane and simple. Anaesthesia. 2017;72:434–8. doi: 10.1111/anae.13830. [DOI] [PubMed] [Google Scholar]
- 17.Naja Z, Lönnqvist PA. Somatic paravertebral nerve blockade. Incidence of failed block and complications. Anaesthesia. 2001;56:1184–8. doi: 10.1046/j.1365-2044.2001.02084-2.x. [DOI] [PubMed] [Google Scholar]
- 18.Kulhari S, Bharti N, Bala I, Arora S, Singh G. Efficacy of pectoral nerve block versus thoracic paravertebral block for postoperative analgesia after radical mastectomy: A randomized controlled trial. Br J Anaesth. 2016;117:382–6. doi: 10.1093/bja/aew223. [DOI] [PubMed] [Google Scholar]
- 19.Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector spinae plane block versus retrolaminar block: A Magnetic resonance imaging and anatomical study. Reg Anesth Pain Med. 2018;43:756–62. doi: 10.1097/AAP.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 20.Ivanusic J, Konishi Y, Barrington MJ. A cadaveric study investigating the mechanism of action of erector spinae blockade. Reg Anesth Pain Med. 2018;43:567–71. doi: 10.1097/AAP.0000000000000789. [DOI] [PubMed] [Google Scholar]
- 21.Wahba SS, Kamal SM. Thoracic paravertebral block versus pectoral nerve block for analgesia after breast surgery. Egypt J Anaesth. 2014;30:129–2. [Google Scholar]
- 22.Versyck B, van Geffen GJ, Van Houwe P. Prospective double blind randomized placebo-controlled clinical trial of the pectoral nerves (Pecs) block type II. J Clin Anesth. 2017;40:46–50. doi: 10.1016/j.jclinane.2017.03.054. [DOI] [PubMed] [Google Scholar]
- 23.Morioka H, Kamiya Y, Yoshida T, Baba H. Pectoral nerve block combined with general anesthesia for breast cancer surgery: A retrospective comparison. JA Clin Rep. 2015;1:15. doi: 10.1186/s40981-015-0018-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ueshima H. Pneumothorax after the erector spinae plane block. J Clin Anesth. 2018;48:12. doi: 10.1016/j.jclinane.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 25.Solak M, Ulusoy H, Sarihan H. Effects of caudal block on cortisol and prolactin responses to postoperative pain in children. Eur J Pediatr Surg. 2000;10:219–23. doi: 10.1055/s-2008-1072362. [DOI] [PubMed] [Google Scholar]
- 26.Nasr DA, Abdelhamid HM. The efficacy of caudal dexmedetomidine on stress response and postoperative pain in pediatric cardiac surgery. Ann Card Anaesth. 2013;16:109–14. doi: 10.4103/0971-9784.109744. [DOI] [PubMed] [Google Scholar]
- 27.Maze M, Virtanen R, Daunt D, Banks SJ, Stover EP, Feldman D. Effects of dexmedetomidine, a novel imidazole sedative-anesthetic agent, on adrenal steroidogenesis: In vivo and in vitro studies. Anesth Analg. 1991;73:204–8. doi: 10.1213/00000539-199108000-00015. [DOI] [PubMed] [Google Scholar]


