Abstract
Background:
Arthroscopic knee surgery is most commonly performed minimally invasive surgical procedure in orthopaedics. Postoperative pain relief is must for early mobilisation that reduces patient's morbidity and improves postoperative recovery.
Aims and Objectives:
We sought to compare analgesic efficacy of intraarticular buprenorphine with dexmedetomidine following arthroscopic surgery of knee.
Settings and Design:
A prospective , randomized controlled double blinded study was conducted involving 60 patients undergoing arthroscopic knee surgery.
Materials and Methods:
Patients were allocated into group B (n = 30) and group D (n = 30) receiving 100 μg of intraarticular buprenorphine and 100 μg of intraarticular dexmedetomidine respectively. Parameters observed were the time to first rescue analgesia , the number of patients requiring rescue analgesia with in next 24 hours, Visual analogue scale (VAS) at rest and on mobilization at 1st, 2nd, 4th, 8th, 12th and 24th hour.
Statistical Analysis:
Quantitative data were analyzed by unpaired student's t test and categorical data by Fisher's exact test. A P < 0.05 was considered to be significant. Statistical analysis was done using Statistical Package for the Social Sciences (SPSS 19.0, SPSS Inc., Chicago, IL, USA).
Results:
Time to first rescue analgesia was significantly longer in patients receiving in group B. VAS scores at rest were comparable between the groups at 1st, 2nd, 4th and 8th hour but significantly low with intraarticular buprenorphine than intraarticular dexmedetomidine at 12th and 24th hour. VAS scores on ambulation were comparable at 1st, 2nd and 4th hour but significantly higher in dexmedetomidine group as compared to buprenorphine at 8th, 12th and 24th hour.
Conclusion:
Intraarticular buprenorphine 100 μg provides longer duration of analgesia with decreased postoperative rescue analgesic requirement as compared to 100 μg intraarticular dexmedetomidine.
Keywords: Buprenorphine, dexmedetomidine, intra-articular, postoperative analgesia
INTRODUCTION
Arthroscopic knee surgery is the most commonly performed minimally invasive surgical procedure in orthopedics. Postoperative pain is due to irritation of free nerve endings of synovial tissue, anterior fat pad, and joint capsule during surgical excision and resection.[1] Postoperative pain relief is a must for early mobilization that reduces patient's morbidity and improves postoperative recovery. Multimodal techniques for postoperative analgesia have been used such as systemic analgesia, neuraxial analgesia, peripheral nerve blocks, and intra-articular (IA) injections in an attempt to attenuate postoperative pain.
Buprenorphine is an agonist–antagonist opioid, about thirty times more potent than morphine. Its high lipid solubility, higher affinity for opioid receptors, and long duration of action make it a better choice as postoperative analgesic.[2] Dexmedetomidine is a highly selective α2 adrenoceptor agonist that binds eight times more avidly to α2 receptors than clonidine having sympatholytic, sedative-hypnotic, anxiolytic, and analgesic property.[3]
In this study, we sought to compare the analgesic efficacy of IA buprenorphine with dexmedetomidine following arthroscopic surgery of the knee.
MATERIALS AND METHODS
This prospective, randomized controlled double-blinded study was carried out after ethical committee clearance and patient's informed written consent. Inclusion criteria were patients aged >18 years, of both the sex, with American Society of Anesthesiologists physical status I–II, and undergoing knee arthroscopy. Patients with a history of sensitivity to local anesthetics or preoperative administration of opioids or any other analgesics in the preceding 48 h were excluded from the study. Surgical interventions were diagnostic arthroscopies, meniscal excision or repair, removal of loose bodies, and arthroscopic debridement. Cases of extensive arthroscopic synovectomy, ligament reconstruction, and articular cartilage procedures were excluded from the study.
Patients were randomized by sealed envelope methods into two groups each of 30 patients. Two standard portals (anteromedial and anterolateral) were used, and the mean duration of the whole procedure was 45 min (range 35–60 min).
Standardized general anesthesia was selected in all the cases. Muscle relaxants and short-acting opioids (fentanyl) were used at the beginning of the operation. No nonsteroidal anti-inflammatory drugs or additional pain medications were administered. The IA injection was done through arthroscopy at the end of the procedure by the operating surgeon (without knowing the content). Group D patients received 0.2% ropivacaine 20 mL with 100 μg dexmedetomidine and Group B patients received 0.2% ropivacaine 20 mL with 100 μg buprenorphine intra-articularly. Study medications were prepared by an anesthesia assistant not involved in the study. The patient, operating surgeon, and anesthesiologist who helped in data collection were all unaware of the patients’ allocation group. The tourniquet was removed after application of a compression bandage.
Parameters observed were the time to first rescue analgesia (defined as the time elapsed from IA injection to time of first analgesic request), the number of patients requiring rescue analgesia within next 24 h, visual analog scale (VAS) at rest, and on mobilization at 1st, 2nd, 4th, 8th, 12th, and 24th h. Injection tramadol hydrochloride 100 mg was given intravenously as rescue analgesia when patients have a complaint of pain. Adverse events including nausea, vomiting, hypotension, bradycardia, depression of respiration, pruritus, and urinary retention were recorded. Local adverse effects such as hematoma were recorded. Nausea and vomiting were treated with ondansetron 4 mg intravenous (i.v.). Hypotension (defined as a decrease in mean arterial pressure >20% of the baseline value) was treated with i.v. fluids and i.v. ephedrine 5 mg boluses as needed. Bradycardia (defined as heart rate <50 beats/min) was treated by atropine 0.01 mg/kg i.v.
Statistical analysis
Sample size calculation was based on the prolongation of time to first rescue analgesia. Based on the results of previous study, 29 patients were needed in each group at α error of 0.05 and study power of 80%.[4] Quantitative data were described as mean ± standard deviation, and unpaired Student's t-test was used for comparison between the two groups. Categorical data were described as number and Fisher's exact test were used. P < 0.05 was considered statistically significant. Statistical analysis was done using Statistical Package for the Social Sciences (SPSS 19.0, SPSS Inc., Chicago, IL, USA).
RESULTS
All sixty patients enrolled were included in the study [Figure 1]. Demographic data including age, gender, weight, and duration of surgery were comparable among the two groups of buprenorphine and dexmedetomidine [Table 1].
Figure 1.
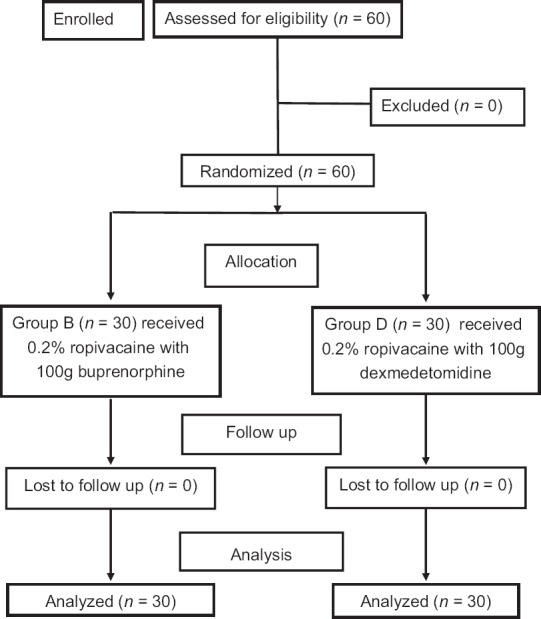
Consort flow
Table 1.
Demographic data and duration of surgery
| Parameters | Group B (n=30) | Group D (n=30) | P |
|---|---|---|---|
| Age (year) | 34.16±9.55 | 35.18±9.2 | 0.67 |
| Gender (male/female) | 26/4 | 25/5 | 0.5 |
| Bodyweight (kg) | 60.27±8.09 | 61.7±7.63 | 0.89 |
| Duration of surgery (min) | 49.2±10.4 | 50.9±10.5 | 0.91 |
Data are expressed as mean standard deviation or patient number. P<0.05 statistical significance. n=Number of patients in each group
Time to first rescue analgesia was significantly longer in patients receiving IA buprenorphine (954.2 ± 96.4 min) than IA dexmedetomidine (628 ± 85.4 min). Only 6 patients in the buprenorphine group and 15 patients in the dexmedetomidine group required rescue analgesia within 24 h (P = 0.03) [Table 2].
Table 2.
Analgesic requirements during next 24 h
| Parameters | Group B (n=30) | Group D (n=30) | P |
|---|---|---|---|
| Time to first rescue analgesia | 954.2±96.4 | 628±85.4 | 0.01 |
| Number of patients requiring rescue analgesia | 6/30 | 15/30 | 0.03 |
Data are expressed as mean standard deviation and patient number. P<0.05 denotes statistical significance
VAS scores at rest were comparable between the groups at 1st, 2nd, 4th, and 8th h, but significantly low with IA buprenorphine than IA dexmedetomidine at 12th and 24th h (P < 0.05) [Table 3]. VAS scores on ambulation were comparable at 1st, 2nd, and 4th h, but significantly higher in the dexmedetomidine group as compared to buprenorphine at 8th, 12th, and 24th h [Table 4].
Table 3.
Visual analog scale at rest
| VAS at rest (h) | Group B | Group D | P |
|---|---|---|---|
| At 1 | 1.0±0.66 | 1.2±0.78 | 0.84 |
| At 2 | 1.1±0.85 | 1.02±0.48 | 0.93 |
| At 4 | 1.77±0.67 | 1.43±0.15 | 0.62 |
| At 8 | 2.35±0.56 | 2.33±0.87 | 0.98 |
| At 12 | 4.56±0.0.70 | 6.33±0.34 | 0.03 |
| At 24 | 3.2±0.25 | 5.3±0.83 | 0.01 |
Data are expressed as mean±SD. P<0.05 denotes statistical significance, n=30 in each group. VAS=Visual analog scale, SD=Standard deviation
Table 4.
Visual analog scale on mobilization
| VAS on mobilization (h) | Group B | Group D | P |
|---|---|---|---|
| At 1 | 1.97±0.47 | 2.00±0.69 | 0.84 |
| At 2 | 2.00±0.32 | 2.07±0.58 | 0.56 |
| At 4 | 2.15±0.73 | 2.33±0.75 | 0.35 |
| At 8 | 2.37±0.65 | 2.65±0.32 | 0.03 |
| At 12 | 4.55±1.03 | 5.97±0.76 | 0.0001 |
| At 24 | 3.54±1.67 | 5.35±1.75 | 0.0001 |
Data are expressed as mean±SD. P<0.05 denotes statistical significance. VAS=Visual analog scale, SD=Standard deviation
None of the patients had any significant adverse effects in either groups [Table 5]. Only two patients in the buprenorphine group had hypotension as compared to one in the dexmedetomidine group, though statistically not significant.
Table 5.
Adverse effects
| Adverse effects | Group B | Group D | P |
|---|---|---|---|
| Bradycardia | 2 | 1 | 1.00 |
| Hypotension | 0 | 0 | 1.00 |
| Nausea | 0 | 0 | 1.00 |
| Vomiting | 0 | 0 | 1.00 |
| Pruritus | 0 | 0 | 1.00 |
| Urinary retention | 0 | 0 | 1.00 |
| Hematoma | 0 | 0 | 1.00 |
Data are expressed as number. P<0.05 denotes statistical significance
DISCUSSION
Various methods of postoperative analgesia have been used for undergoing knee arthroscopy.[5] Side effects of systemic opioids such as nausea and vomiting, respiratory depression, drowsiness, and pruritus lead to an option of providing analgesia locally.[6] IA drug administration is one of the best, simple techniques for pain management after arthroscopic knee surgery, which helps in early ambulation of the patient.[7,8,9]
Ropivacaine is structurally related to bupivacaine, but being less lipid soluble results in less central nervous system and cardiac toxicity.[10] Although i.v. dexmedetomidine produces sedation, analgesia, and sympatholysis, its IA administration along with local anesthetics decreases postoperative pain without significant effects.[4,11] Buprenorphine is a partial agonist with higher receptor affinity than morphine which accounts for intense and prolonged analgesia.
In our study, time to first rescue analgesia was significantly higher in IA buprenorphine than IA dexmedetomidine. Varrassi et al.[12] also concluded that 100 μg buprenorphine provided better postoperative pain and reduced postoperative analgesic requirement. The number of patients requiring rescue analgesia within 24 h was significantly more in the dexmedetomidine group as compared to the buprenorphine group. This is similar to a study where patients receiving IA buprenorphine need less number of rescue analgesia.[13]
We found no significant difference in pain intensity at rest and on ambulation as assessed by VAS at 1, 2, 4, and 8 h between the buprenorphine and dexmedetomidine group. However, at 12th and 24th h, VAS score was significantly high in IA dexmedetomidine group at rest. On ambulation, VAS score was significantly lower with IA buprenorphine at 8th, 12th, and 24th h. Buprenorphine provides longer duration of analgesia with less pain scores. This might be due to its partial agonist action, high receptor affinity, and slow dissociation from local peripheral opioid receptor.[14]
Most of the studies have proved that IA dexmedetomidine has better analgesic efficacy than other drugs.[15,16,17] Till now, no study was published comparing the analgesic efficacy of IA buprenorphine and IA dexmedetomidine following knee arthroscopic surgeries.
None of the patients in the study group had any significant side effects.
CONCLUSION
IA buprenorphine 100 μg provides longer duration of analgesia with decreased postoperative rescue analgesic requirement as compared to 100 μg IA dexmedetomidine.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Dye SF, Vaupel GL, Dye CC. Conscious neurosensory mapping of the internal structures of the human knee without intraarticular anesthesia. Am J Sports Med. 1998;26:773–7. doi: 10.1177/03635465980260060601. [DOI] [PubMed] [Google Scholar]
- 2.Ravindran R, Sajid B, Ramadas KT, Susheela I. Intrathecal hyperbaric bupivacaine with varying doses of buprenorphine for postoperative analgesia after cesarean section: A Comparative study. Anesth Essays Res. 2017;11:952–7. doi: 10.4103/aer.AER_82_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaur M, Singh PM. Current role of dexmedetomidine in clinical anesthesia and intensive care. Anesth Essays Res. 2011;5:128–33. doi: 10.4103/0259-1162.94750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Metwalli RR, Mowafi HA, Ismail SA, Siddiqui AK, Al-Ghamdi AM, Shafi MA, et al. Effect of intra-articular dexmedetomidine on postoperative analgesia after arthroscopic knee surgery. Br J Anaesth. 2008;101:395–9. doi: 10.1093/bja/aen184. [DOI] [PubMed] [Google Scholar]
- 5.Allen GC, St Amand MA, Lui AC, Johnson DH, Lindsay MP. Postarthroscopy analgesia with intraarticular bupivacaine/morphine. A randomized clinical trial. Anesthesiology. 1993;79:475–80. doi: 10.1097/00000542-199309000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Franceschi F, Rizzello G, Cataldo R, Denaro V. Comparison of morphine and ropivacaine following knee arthroscopy. Arthroscopy. 2001;17:477–80. doi: 10.1053/jars.2001.19684. [DOI] [PubMed] [Google Scholar]
- 7.Gupta A, Axelsson K, Allvin R, Liszka-Hackzell J, Rawal N, Althoff B, et al. Postoperative pain following knee arthroscopy: The effects of intra-articular ketorolac and/or morphine. Reg Anesth Pain Med. 1999;24:225–30. doi: 10.1016/s1098-7339(99)90132-3. [DOI] [PubMed] [Google Scholar]
- 8.Reuben SS, Sklar J. Pain management in patients who undergo outpatient arthroscopic surgery of the knee. J Bone Joint Surg Am. 2000;82-A:1754–66. doi: 10.2106/00004623-200012000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Khoury GF, Chen AC, Garland DE, Stein C. Intraarticular morphine, bupivacaine, and morphine/bupivacaine for pain control after knee videoarthroscopy. Anesthesiology. 1992;77:263–6. doi: 10.1097/00000542-199208000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Scott DB, Lee A, Fagan D, Bowler GM, Bloomfield P, Lundh R, et al. Acute toxicity of ropivacaine compared with that of bupivacaine. Anesth Analg. 1989;69:563–9. [PubMed] [Google Scholar]
- 11.Gerlach AT, Murphy CV, Dasta JF. An updated focused review of dexmedetomidine in adults. Ann Pharmacother. 2009;43:2064–74. doi: 10.1345/aph.1M310. [DOI] [PubMed] [Google Scholar]
- 12.Varrassi G, Marinangeli F, Ciccozzi A, Iovinelli G, Facchetti G, Ciccone A, et al. Intra-articular buprenorphine after knee arthroscopy. A randomised, prospective, double-blind study. Acta Anaesthesiol Scand. 1999;43:51–5. doi: 10.1034/j.1399-6576.1999.430112.x. [DOI] [PubMed] [Google Scholar]
- 13.Sugandarajappa SG, Rashmi NR, Sumitha CS, Suresh C. Comparison of analgesic effect of intraarticular buprenorphine and morphine following arthroscopic surgery of knee. J Evol Med Dent Sci. 2016;5:4175–80. [Google Scholar]
- 14.Boas RA, Villiger JW. Clinical actions of fentanyl and buprenorphine. The significance of receptor binding. Br J Anaesth. 1985;57:192–6. doi: 10.1093/bja/57.2.192. [DOI] [PubMed] [Google Scholar]
- 15.Elbadawy A, Salama A, Mohammad M. Comparative study of intraarticular dexmedetomidine versus ketamine as adjuvant analgesics after knee arthroscopy. Egypt J Anaesth. 2015;31:309–14. [Google Scholar]
- 16.Paul S, Bhattacharjee DP, Ghosh S, Dawn S, Chatterjee N. Efficacy of intra-articular dexmedetomidine for postoperative analgesia in arthroscopic knee surgery. Ceylon Med J. 2010;55:111–5. doi: 10.4038/cmj.v55i4.2627. [DOI] [PubMed] [Google Scholar]
- 17.El-Hamamsy M, Dorgham M. Intra-articular adjuvant analgesics following knee arthroscopy: Comparison between dexmedetomidine and fentanyl. Res J Med Med Sci. 2009;4:355–60. [Google Scholar]


