Abstract
Context:
Adjuvants to bupivacaine for single shot caudal block in children.
Aims:
This study entitled was conducted to compare the effects of addition of tramadol to bupivacaine over addition of clonidine to bupivacaine as a single shot caudal block in children.
Settings and Design:
Sixty children of ASA grade I and II in the age group of 2-12 years coming for various infra-umbilical surgeries were included.
Materials and Methods:
They were divided into two groups of 30 each. Group BC received caudal bupivacaine 0.25% 0.5ml/kg with clonidine 2 mcg/kg Group BT received caudal bupivacaine 0.25% 0.5 ml/kg with tramadol 2 mg/kg. The main parameters studied were hemodynamic changes, duration of post-operative analgesia and incidence of adverse effects.
Statistical Analysis Used:
The results of continuous variables are given as mean ± SD and proportion as percentage. The difference between the two groups was assessed by student's – t test and chi-square test
Results:
The mean duration of post-operative analgesia in group BT was statistically significant (P <0.001), reducing the requirement of analgesics in group BT. There was no difference in sedation score, nausea, vomiting, urinary retention.
Conclusions:
The present study demonstrated that caudal administration of bupivacaine 0.25% 0.5 ml/kg with tramadol 2 mg/kg resulted in superior analgesia with longer duration of action and reduced requirement of analgesics in first 24 hours postoperatively when compared with 0.25% bupivacaine 0.5 ml/kg with clonidine 2 mcg/kg.
Keywords: Adjuvants, caudal space, epidural space, post operative analgesia, sedation
INTRODUCTION
Pain results in immediate physiological, humoral, immunological, and behavioral responses in a child, which are associated with increase in circulating catecholamines, cortisol, aldosterone, glucagon, and other steroid hormones leading to harmful effects.[1] Caudal epidural block has gained popularity, especially for procedures below the umbilicus, since it is a simple, safe, and reliable technique.[2,3]
The main disadvantage of this single-shot caudal block is its shorter duration of action even with the use of long-acting local anesthetic agents such as bupivacaine.[2] To prolong the duration and improve the quality of intraoperative and postoperative analgesia of local anesthetics, various drugs such as opioids,[4,5,6] epinephrine, midazolam,[7] ketamine,[8] neostigmine,[9] and clonidine[2,10,11] have been used as adjuvants with various advantages, disadvantages, and adverse effects.
Clonidine is used as an adjuvant in caudal block to improve the intraoperative and post operative analgesia and to reduce the dose of local anesthetic.[12]
MATERIALS AND METHODS
This prospective study was conducted in a 750-bedded hospital between December 2012 and July 2014.
Approval from the Ethics and Standards Committee of this institution was obtained. Informed consent was obtained from the parent before including the children in the study.
The study included 60 children, of either sex, divided into two groups of 30 patients each randomly.
Inclusion criteria
Patients in the age group of 2–12 years
Patients with American Society of Anesthesiologists (ASA) Physical Status Classes I and II
Patients coming for elective lower abdominal and lower limb surgeries.
Exclusion criteria
Patients with ASA Physical Status Classes III and IV
Patients with infection at the site of injection
Patients on coagulopathy or on anticoagulation
Patients with congenital abnormalities of lower spine and meninges
Patients with active disease of the central nervous system
Patients with a history of allergy to local anesthetics, clonidine, and tramadol
Parents’ refusal
Patient posted for emergency surgery.
Methods
Preanesthetic assessment was done, and baseline investigations were sent
Preoperative fasting was followed based on pediatric fasting guidelines.
Premedication
All patients were premedicated with syrup promethazine 1 mg/kg, once on the night before the surgery and on the day 2 h before the surgery, after securing an intravenous (IV) access injection atropine 0.02 mg/kg IV was given.
Procedure
Depending on the weight of the patient, isolyte-P or normal saline IV fluids were started. All patients were preoxygenated with 100% oxygen for 3 min using Jackson–Rees circuit.
Patients were induced using injection thiopentone 5 mg/kg IV until eyelash reflex is lost. Injection succinylcholine 2 mg/kg was given, and the patients were intubated using appropriate-sized endotracheal tubes.
Caudal block was performed in the right lateral position
Group BC – received inj bupivacaine 0.25%, 0.5 ml/kg with inj Clonidine 2 mcg/kg.
Group BT – received inj bupivacaine 0.25%, 0.5 ml/kg with inj Tramadol 2 mg/kg.
After procedure, the child was placed in supine and head up position. No analgesia was given by any route preoperatively or intraoperatively. Anesthesia was maintained with O2:N2O = 33%:66%, halothane 0.5%–0.75%, and muscle relaxation with NDMR-non depolarising muscle relaxant (NDMR) injection vecuronium according to the body weight.
At the end of the surgery, the patients were reversed and extubated and shifted to the recovery room.
The child was monitored for another 1 h with SpO2, respiratory rate, noninvasive blood pressure (NIBP), and heart rate every 15 min. After that, the child was shifted to the ward and monitored thereafter.
Monitoring
Intraoperative monitoring included precordial stethoscope, pulse oximetry, NIBP, respiratory rate, and electrocardiogram. The time of caudal block and duration of surgery were noted.
Parameters studied
Hemodynamic parameters
Patient's heart rate, respiration rate, and blood pressure were monitored after the administration of caudal block at 0, 5, 10, 15, 20, 40, and 60 min.
Rescue analgesia
It is the time interval between the administration of caudal block and the first requirement of supplementary analgesia for the patient.
Post-operative analgesia is assessed by Paediatric Objective Pain Scale [Table 1]. The assessment was done for 24 h after caudal block. If the pain score was ≥6 for two consecutive intervals of 10 min, then supplementary analgesia with suppository paracetamol (20 mg/kg) was given. These assessments were made at 1, 2, 3, 4, 8, 12, and 24 h after caudal block.
Table 1.
Pediatric objective pain scale
| Observations | Criteria | Points |
|---|---|---|
| BP | ±10% preoperative value | 0 |
| >20% preoperative value | 1 | |
| >30% preoperative value | 2 | |
| Crying | Not crying | 0 |
| Crying but responds to tender loving care | 1 | |
| Crying with no response to tender loving care | 2 | |
| Movement | None | 0 |
| Restlessness | 1 | |
| Thrashing | 2 | |
| Agitation | Asleep | 0 |
| Mild | 1 | |
| Hysterical | 2 | |
| Posture | No special posture | 0 |
| Flexing legs and thighs | 1 | |
| Holding penis or groin | 2 |
BP=Blood pressure
Side effects were monitored
Nausea and vomiting, bradycardia, hypotension, and respiratory depression, sedation score [Table 2] were noted.
Table 2.
Sedation: A five point sedation score
| Score | Degree of sedation |
|---|---|
| 1 | Fully awake and oriented |
| 2 | Drowsy |
| 3 | Eyes closed but arousable to command |
| 4 | Eyes closed but arousable to mild physical stimulation |
| 5 | Eyes closed but unarousable to mild physical stimulation |
Statistical analysis
Analysis of the present study was made using the following parameters.
Percentages
The arithmetic mean (m or x)
The standard deviation (SD) (S)
Student's t-test
Proportion test.
The results of continuous variables are presented as mean ± SD and proportion as percentage. The difference between the two groups was assessed by Student's t-test and Chi-square test. For all the tests, a P ≤ 0.05 was considered statistically significant.
RESULTS
A total number of 60 children in the age group of 2–12 years were enrolled.
Age distribution of patients
Graph 1 shows the age distribution of the patients studied.
Graph 1.
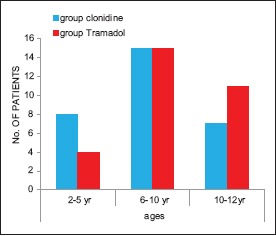
Age distribution
Mean age distribution
The mean age in Group BC was 8.26 ± 2.98 years whereas in Group BT was 9.03 ± 2.94 years (P = 0.320).
Mean weight of the patients
The mean weight was 22.16 ± 7.78 in group bupivacaine + clonidine and 26.76 ± 6.74 in group bupivacaine + tramadol, with P = 0.018 [Graph 2].
Graph 2.
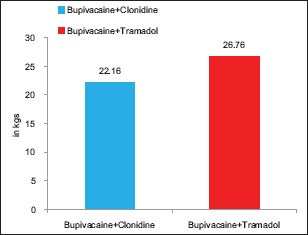
Mean weight
Mean height of the patients
The mean height in group bupivacaine + clonidine was 120.03 ± 14.95 and mean height in group bupivacaine + tramadol was 125.67 ± 7.72, with P = 0.072 [Graph 3].
Graph 3.
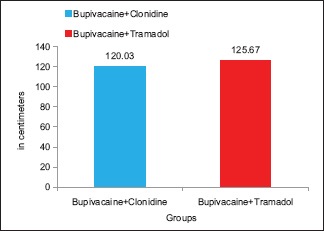
Mean height
Sex distribution
Group BC has 26 (86.7%) males and 4 (13.3%) females, while Group BT has 27 (90.0%) males and 3 (10.0%) females [Graph 4].
Graph 4.
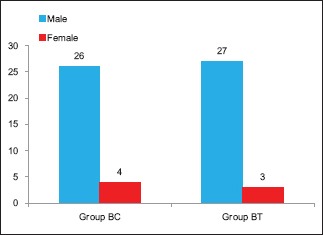
Sex distribution
Changes in mean arterial pressure
The baseline mean arterial pressure (MAP) was 87.66 ± 7.013 mmHg in group bupivacaine + clonidine. The MAP was 85.16 ± 8.11 mmHg at 15 min and then gradually decreased to 67.5 ± 3.26 mmHg at 60 min. In group bupivacaine + tramadol, the baseline MAP was 84.46 ± 7.71 mmHg, which increased to 86.73 ± 6.09 mmHg at 15 min and then gradually decreased to 76.6 ± 4.81 mmHg at 60 min. Moreover, P value was statistically significant at 10th, 20th, 40th, and 60th min [Table 3].
Table 3.
Changes in mean arterial pressure
| Bupivacaine + clonidine | Bupivacaine + tramadol | Mean difference | P | |
|---|---|---|---|---|
| Basal BP | 87.66±7.013 | 84.46±7.71 | 3.20000 | 0.098 |
| 5 min | 76.4±6.61 | 76.83±9.59 | −0.43333 | 0.839 |
| 10 min | 85.16±7.90 | 91.8±8.20 | −6.63333 | 0.002 |
| 15 min | 85.16±8.11 | 86.73±6.09 | −1.56667 | 0.401 |
| 20 min | 76.43±5.69 | 81.73±4.68 | −5.30000 | 0.001 |
| 40 min | 71.13±4.36 | 78.5±5.17 | −7.36667 | 0.001 |
| 60 min | 67.5±3.26 | 76.6±4.81 | −9.10000 | 0.001 |
BP=Blood pressure
Changes in heart rate
In group bupivacaine + clonidine, the mean baseline heart rate was 110.43 ± 13.45 beats/min. Heart rate gradually decreased to 80.66 ± 5.52 beats/min at 60 min. The mean baseline heart rate in group bupivacaine + tramadol was 109.3 ± 11.82 beats/min, which then gradually decreased to 84.56 ± 4.59 beats/min at the end of 60 min. Moreover, P value was statistically significant at 15th and 60th min [Table 4].
Table 4.
Changes in heart rate
| Bupivacaine + clonidine | Bupivacaine + tramadol | Mean difference | P | |
|---|---|---|---|---|
| Basal HR | 110.43±13.45 | 109.3±11.82 | 1.13333 | 0.730 |
| 5 min | 117.13±13.02 | 100.86±19.52 | 16.26667 | 0.000 |
| 10 min | 123.67±13.36 | 119.43±13.72 | 4.23333 | 0.231 |
| 15 min | 124.7±11.82 | 108.53±10.01 | 16.16667 | 0.001 |
| 20 min | 102.4±10.91 | 98.43±8.18 | 3.96667 | 0.117 |
| 40 min | 85.5±7.81 | 90.43±7.784 | −4.93333 | 0.017 |
| 60 min | 80.66±5.52 | 84.56±4.59 | −3.90000 | 0.004 |
HR=Heart rate
Mean duration of surgery
There was not much difference in two groups. It was shown by P = 0.550 [Graph 5].
Graph 5.
Mean duration of surgery
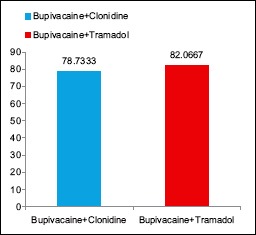
Incidence of complications
Four patients in group bupivacaine + clonidine and seven patients in group bupivacaine + tramadol had an incidence of nausea and vomiting, with P = 0.317. Moreover, two and three patients in bupivacaine + clonidine and bupivacaine + tramadol group, respectively, had a incidence of urinary retention, with P = 0.640 [Graph 6].
Graph 6.
Incidence of complications
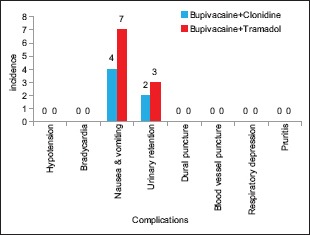
Sedation score at various time intervals
The mean sedation score was 1 in both the groups at all the time intervals [Graph 7].
Graph 7.
Sedation scoring
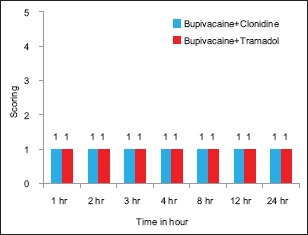
Mean duration of postoperative analgesia
The mean duration of analgesia provided by group bupivacaine + clonidine and group bupivacaine + tramadol was 412 ± 42.68 and 851.93 ± 66.69, respectively, with P = 0.001 [Graph 8].
Graph 8.
Mean duration of postoperative analgesia
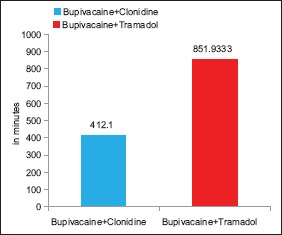
Number of times analgesics given in first 24 h
Twenty-four patients in Group BT required analgesics only twice in the first 24 h and remaining six patients in Group BT required analgesics three times in the first 24 h postoperatively. However, 25 patients in Group BC required analgesics three times in the first 24 h postoperatively and remaining five patients needed it four times. P = 0.001 is considered statistically significant [Graph 9].
Graph 9.
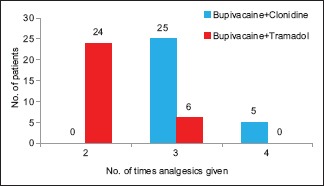
Number of times analgesics given in first 24 h
DISCUSSION
The major disadvantage of single-shot caudal anesthesia is the short duration of action. To overcome this problem, additives were used.
Drug concentration and volume
In 1989, Dalens and Hasnaoui[13] compared the efficacy of different local anesthetics and concluded that bupivacaine provides a long duration of analgesia.
Different volumes of bupivacaine were used by different studies. Cook et al.[14] in 1995 had used 1 ml/kg, and Klimscha et al.[15] in 1998 had used 0.75 ml/kg.
Concentration of bupivacaine used in different studies is also different. In 1989, Coad and Hain[16] studied 40 children posted for inguinal surgery using 0.25% and 0.5% bupivacaine. They concluded that the preferred regimen for caudal anesthesia would be 0.25% bupivacaine.
In both the groups, males were more (>85%). This could be due to inclusion of surgeries such as herniotomy, hypospadias repair, orchidopexy, and circumcision in our study.
Primary outcome
Mean duration of postoperative analgesia
If the pain score was more or equal to 6 at two consecutive intervals of 10 min, supplementary analgesic with paracetamol suppository (20 mg/kg) was given.
Constant et al.[11] in 1998 observed the duration of analgesia as 265 min in those who received clonidine 1.5 μg/kg and 287 min in those who received caudal clonidine 0.75 μg/kg with fentanyl 0.5 μg/kg as adjuvants to 0.25% bupivacaine 1 mg/kg.
In 2007, Khalid et al. studied 60 children aged from 1 to 12 years undergoing unioscrotal surgeries and they were randomly divided into two groups. Group BT was given 0.25% of 0.8 ml/kg bupivacaine and tramadol 2 mg/kg, while the other Group B was given 0.25% of 0.8 ml/kg bupivacaine through caudal route.
Addition of tramadol with bupivacaine resulted in increased postoperative analgesic period (16.06 ± 4.04 h). It was concluded that use of tramadol as an additive can prolong the postoperative analgesic period when administered caudally.[17]
Taheri et al.[18] in 2010 evaluated 60 children undergoing inguinal herniorrhaphy. They were either given 0.25% bupivacaine 1 ml/kg with neostigmine 2 μg/kg (Group BN) or tramadol 1 mg/kg (Group BT). Duration of analgesia was longer in Group BT (17.30± 8.24 h) compared with Group BN (13.98 ± 10.03 h) (P = 0.03).
However, in 2000, De Mey et al.[19] concluded that addition of clonidine to caudal bupivacaine does not offer any additional benefit over bupivacaine; in our study, the mean duration postoperative analgesia seen in Group BT was 851.9333 ± 66.69 min, which correlates with these studies.
Secondary outcome
Changes in hemodynamic parameters
Prakash et al.,[20] in their study, on addition of tramadol to bupivacaine have reported no significant changes in hemodynamic parameters between the two groups.
Initially, there was an increase in MAP in both groups, i.e., 85.16 ± 8.11 mmHg in Group BC and 86.73 ± 6.09 mmHg in Group BT at 15 min, which could be due to the use of injection atropine as a premedicant or due to surgical stimulus itself.
However, once after the commencement of action of caudal block, gradual decline in MAP was noticed, which was more pronounced in Group BC 67.5 ± 3.26 mmHg at 60 min compared to 76.6 ± 4.81 mmHg in Group BT at 60 min, which was statistically significant (P < 0.001).
Similarly, the mean baseline heart rates in two groups were 110.43 ± 13.45 beats/minute in Group BC and 109.3 ± 11.82 beats/minute in Group BT, which initially increased to 123.67 ± 13.36 beats/minute in Group BC and 119.43 ± 13.72 beats/minute in Group BT that could be due to injection atropine or because of surgical stimulus; however, later once caudal block started acting, there was gradual decline in mean heart rates. It reached to 80.66 ± 5.52 beats/ minute in Group BC and 84.56 ± 4.59 beats/minute in Group BT at 60 min. Decrease in the mean heart rate was more pronounced in Group BC which was statistically significant P = 0.004 at the end of 60 min.
Complications
In our study, 4 (13.3%) of the children in Group BC and 7 (23.3%) of them in Group BT had an episode of vomiting which was treated with injection metoclopramide (0.1–0.2 mg/kg) IV and the incidence of vomiting was comparable in both the groups.
Sabbar et al.[21] and Prakash et al.[20] have reported that addition of tramadol did not result in any significant increase in incidence of vomiting, which correlates well with our study.
In our study, we observed 2 (6.7%) cases of urinary retention in Group BC and 3 (10.0%) cases of urinary retention in Group BT, and the incidence was comparable in both the groups.
Sedation scores
The mean sedation score was 1 at all the time intervals in both the groups. Somasundran and Garasia[22] and Sabbar et al.[21] found no significant difference in sedation scores.
Strengths
The study population was uniform with respect to age, weight, height, and type of surgical procedure, i.e., infraumbilical.
Limitation
Assessment of pain is complex in children, based only on physiological, behavioral parameters
More studies are needed in this area to keep children comfortable in the postoperative period.
CONCLUSION
The present study demonstrated that caudal administration of bupivacaine 0.25% 0.5 ml/kg with tramadol 2 mg/kg resulted in superior analgesia with longer duration of action and reduced requirement of analgesics in first 24 h postoperatively when compared with 0.25% bupivacaine 0.5 ml/kg with clonidine 2 μg/kg. As compared to tramadol with bupivacaine, clonidine with bupivacaine produced significant decrease in mean heart rate and MAP without any significant increase in the incidence of side effects.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Maunuksela EL, Olkkola KT. Pediatric pain management. Int Anaesthesiol Clin. 1991;29:37–56. doi: 10.1097/00004311-199102910-00006. [DOI] [PubMed] [Google Scholar]
- 2.Walker SM. Acute pain management in pediatric patients. Int Anaesthesiol Clin. 1997;35:105–30. doi: 10.1097/00004311-199703520-00008. [DOI] [PubMed] [Google Scholar]
- 3.Hansen TG, Henneberg SW, Larsen SW, Lund J, Hansen M. Caudal bupivacaine supplemented with caudal or intravenous Clonidine in children undergoing hypospadias repair: A double blind study. Br J Anaesth. 2004;92:223–7. doi: 10.1093/bja/aeh028. [DOI] [PubMed] [Google Scholar]
- 4.Sanders JC. Paediatric regional anaesthesia, a survey of practice in the United Kingdom. Br J Anaesth. 2002;89:707–10. [PubMed] [Google Scholar]
- 5.Kundra P, Deepalakshmi K, Ravishankar M. Preemptive caudal bupivacaine and morphine for postoperative analgesia in children. Anaesth Analg. 1998;87:52–6. doi: 10.1097/00000539-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Choudhuri AH, Dharmani P, Kumarl N, Prakash A. Comparison of caudal epidural bupivacaine with bupivacaine plus tramadol and bupivacaine plus ketamine for postoperative analgesia in children. Anaesth Intensive Care. 2008;36:174–9. doi: 10.1177/0310057X0803600206. [DOI] [PubMed] [Google Scholar]
- 7.Doda M, Mukherjee S. Postoperative analgesia in children- comparative study between caudal bupivacaine and bupivacaine plus tramadol. Indian J Anaesth. 2009;53:463–6. [PMC free article] [PubMed] [Google Scholar]
- 8.Naguib M, El Gammal M, Elhattab YS, Seraj M. Midazolam for caudal analgesia in children: Comparison with caudal bupivacaine. Can J Anaesth. 1995;42:758–64. doi: 10.1007/BF03011172. [DOI] [PubMed] [Google Scholar]
- 9.Naguib M, Sharif AM, Seraj M, el Gammal M, Dawlatly AA. Ketamine for caudal analgesia in children: Comparison with caudal bupivacaine. Br J Anaesth. 1991;67:559–64. doi: 10.1093/bja/67.5.559. [DOI] [PubMed] [Google Scholar]
- 10.Abdulatif M, El-Sanabary M. Caudal neostigmine, bupivacaine, and their combination for postoperative pain management after hypospadias surgery in children. Anesth Analg. 2002;95:1215–8. doi: 10.1097/00000539-200211000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Constant I, Gall O, Gouyet L, Chauvin M, Murat I. Addition of clonidine or fentanyl to local anaesthetics prolongs the duration of surgical analgesia after single shot caudal block in children. Br J Anaesth. 1998;80:294–8. doi: 10.1093/bja/80.3.294. [DOI] [PubMed] [Google Scholar]
- 12.Yildiz TS, Korkmaz F, Solak M, Toker K. Clonidine addition prolongs the duration of caudal analgesia. Acta Anaesthesiol Scand. 2006;50:501–4. doi: 10.1111/j.1399-6576.2005.00941.x. [DOI] [PubMed] [Google Scholar]
- 13.Dalens B, Hasnaoui A. Caudal anesthesia in pediatric surgery: Success rate and adverse effects in 750 consecutive patients. Anesth Analg. 1989;68:83–9. [PubMed] [Google Scholar]
- 14.Cook B, Grubb DJ, Aldridge LA, Doyle E. Comparison of the effects of adrenaline, clonidine and ketamine on the duration of caudal analgesia produced by bupivacaine in children. Br J Anaesth. 1995;75:698–701. doi: 10.1093/bja/75.6.698. [DOI] [PubMed] [Google Scholar]
- 15.Klimscha W, Chiari A, Michalek-Sauberer A, Wildling E, Lerche A, Lorber C, et al. The efficacy and safety of a clonidine/bupivacaine combination in caudal blockade for pediatric hernia repair. Anesth Analg. 1998;86:54–61. doi: 10.1097/00000539-199801000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Coad NR, Hain WR. Caudal anaesthesia for postoperative pain relief in children: A comparative trial of different regimens using plain bupivacaine. Ann R Coll Surg Engl. 1989;71:245–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Khalid A, Siddiqui SZ, Haider S, Aftab S. Single dose caudal tramadol with bupivacaine and bupivacaine alone in pediartic inguinoscrotal surgeries. J Coll Physicians Surg Pak. 2007;17:519–22. [PubMed] [Google Scholar]
- 18.Taheri R, Shayeghi S, Razavi SS, Sadeghi A, Ghabili K, Ghojazadeh M, et al. Efficacy of bupivacaine-neostigmine and bupivacaine-tramadol in caudal block in pediatric inguinal herniorrhaphy. Paediatr Anaesth. 2010;20:866–72. doi: 10.1111/j.1460-9592.2010.03374.x. [DOI] [PubMed] [Google Scholar]
- 19.De Mey JC, Strobbet J, Poelaert J, Hoebeke P, Mortier E. The influence of sufentanil and/or clonidine on the duration of analgesia after a caudal block for hypospadias repair surgery in children. Eur J Anaesthesiol. 2000;17:379–82. doi: 10.1046/j.1365-2346.2000.00690.x. [DOI] [PubMed] [Google Scholar]
- 20.Prakash S, Tyagi R, Gogia AR, Singh R, Prakash S. Efficacy of three doses of tramadol with bupivacaine for caudal analgesia in paediatric inguinal herniotomy. Br J Anaesth. 2006;97:385–8. doi: 10.1093/bja/ael155. [DOI] [PubMed] [Google Scholar]
- 21.Sabbar S, Khan RA, Siddiqui MA, Khan FA. Comparison of caudal bupivacaine with and without tramadol for postoperative analgesia in paediatric inguinoscrotal surgeries. Pak J Surg. 2010;26:155–9. [Google Scholar]
- 22.Somasundran S, Garasia M. A comparative study of ketamine and tramadol as additives to plain bupivacaine in caudal anaesthesia in children. Internet J Anaesthesiol. 2008;17:2. [Google Scholar]


