Abstract
Background:
Perineural dexamethasone has been shown to improve analgesia in single injection supraclavicular block. Systemic mechanism of action of dexamethasone along with safety concerns of perineural route of administration has prompted the investigation of intravenous route as an alternative.
Aims:
We aim to compare the effects of dexamethasone as an additive to local anesthetic when used via perineural and intravenous route in terms of duration of analgesia and onset of motor and sensory block.
Settings and Design:
The study was done as a prospective comparative observational study conducted in a tertiary care hospital in India among 50 patients during a period of 1 year.
Materials and Methods:
Twenty-five patients aged 18–60 years, belonging to the American Society of Anesthesiologists physical status Classes I and II, receiving supraclavicular block with 0.5% bupivacaine and perineural dexamethasone were compared with similar number of patients receiving the block along with intravenous dexamethasone. Duration of analgesia, onset of sensory block, and onset of motor block were studied.
Statistical Analysis:
The results were analyzed using Chi-square test for qualitative variables and unpaired t-test for quantitative variables.
Results:
The duration of analgesia in the group receiving perineural dexamethasone (Group DP) 817.2 ± 88.011 min was comparable to the group receiving intravenous dexamethasone (Group DI) 858.00 ± 86.168, with a P = 0.104. Time to onset of sensory block in Group DP (10.20 ± 1.443 min) was significantly faster than that of Group DI (11.60 ± 1.443) with a P = 0.001. Time to onset of motor block in Group DP (13.92 ± 1.754 min) was significantly earlier than that of Group DI (14.96 ± 1.274 min) with a P = 0.02.
Conclusion:
It is concluded from this study that intravenous and perineural dexamethasone equally prolongs the duration of analgesia in supraclavicular block. However, perineural dexamethasone resulted in a faster onset of motor and sensory blockade.
Keywords: Brachial plexus block, bupivacaine, dexamethasone, intravenous, perineural
INTRODUCTION
Acute postoperative pain can be effectively controlled with the use of peripheral nerve blocks. Use of additives further prolongs the duration of analgesia.[1] Supraclavicular approach to brachial plexus block is useful for procedures done at or below the level of elbow. This technique involves the deposition of local anesthetic near the brachial plexus approached from immediately above the clavicle. Brachial plexus is formed by ventral rami of C5, C6, C7, C8, and T1 which forms the roots. These then continue distally to form trunks, divisions, cords, and branches. Supraclavicular approach blocks the brachial plexus at the level of distal trunks. Compact arrangement of structures at this site results in rapid onset of dense and reliable blockade of the brachial plexus.[2]
Dexamethasone a fluorinated derivative of prednisolone has anti-inflammatory properties.[3] The use of dexamethasone perineurally along with local anesthetic has been shown to improve the duration of analgesia.[4] Intravenous dexamethasone is also useful in attenuating the postoperative need for analgesics in different clinical settings even in the absence of any nerve blocks.[5] Hence, it is logical to compare the duration of analgesia with the use of dexamethasone in the setting of supraclavicular brachial plexus block, dexamethasone given either perineurally or intravenously. This assumes importance in view of safety concerns when dexamethasone is deposited near the nerves mixed with local anesthetic agent. Various studies done on this subject give conflicting results; hence, we intend to fill in the knowledge gap in this matter.
MATERIALS AND METHODS
A prospective, comparative observational study was conducted in a tertiary care teaching hospital during a period of 1 year from March 2016 to February 2017. After obtaining institutional ethics committee approval and written informed consent, 50 patients aged between 18 and 60 years belonging to the American Society of Anesthesiologists physical status Classes I and II of either sex undergoing elective surgical procedures of elbow, forearm, or hand were included in the study. The exclusion criteria included pregnancy, diabetes mellitus, coagulopathy, local skin infection, surgeries with duration more than 180 min, and patients with allergy to local anesthetics or dexamethasone. The sample size was calculated based on a study by Kumar et al. using ropivacaine and dexamethasone,[6] in which the mean duration of analgesia was 1179 ± 108.6 min. Considering this and to detect an effect size of 100 min with power of 80% and α error of 5%, the sample size calculated is 18.28 per group and we included 25 patients per group. Twenty-five consecutive cases receiving supraclavicular block with 25 ml 0.5% bupivacaine and 8 mg perineural dexamethasone (Group DP) were compared with the similar number of patients receiving the block with 25 ml 0.5% bupivacaine perineurally and 8 mg dexamethasone intravenously (Group DI). Intravenous dexamethasone was administered just before injecting the local anesthetic solution. Preoperatively, all patients were instructed regarding how to read the Numerical Rating Scale (NRS). Characteristics of the block were evaluated with respect to duration of analgesia and onset of sensory and motor block. Duration of analgesia was taken as the time between onset of sensory block and reappearance of pain and request for pain relief by the patient or NRS more than or equal to 4. Onset of sensory block was considered as the time between injection of local anesthetic and complete abolition of pinprick response. Onset of motor block was considered as the time between injection of local anesthetic and decreased muscle strength with ability to move only fingers (Modified Bromage Scale Grade I). Postoperative analgesia was assessed by NRS. Statistical analysis was done using Chi-square test for qualitative variables and unpaired t-test for quantitative variables using computer software Statistical Package for the Social Sciences (Version 18.0. Chicago SPSS Inc. - 2009, IBM Corporation). P < 0.05 was considered statistically significant.
RESULTS
Twenty-five patients each in Group DP and DI were analyzed. Demographic data were comparable between the groups, and there was no statistically significant difference [Table 1].
Table 1.
Demographic data*
| Variable | Group DP | Group DI |
|---|---|---|
| Age | 37.44±8.520 | 34.72±8.116 |
| Weight | 57.96±3.434 | 57.36±4.672 |
| Sex | 17:8 | 15:10 |
*Data are expressed in mean±SD (age, weight) and frequency (sex). SD=Standard deviation, DP=Perineural dexamethasone, DI=Intravenous dexamethasone
Time to onset of sensory block in the group receiving perineural dexamethasone (Group DP) was 10.2 ± 1.443 min, which was significantly faster than that of the group receiving intravenous dexamethasone (Group DI) 11.60 ± 1.443 min with a P = 0.001 and degree of freedom (dof) 48 [Figure 1].
Figure 1.
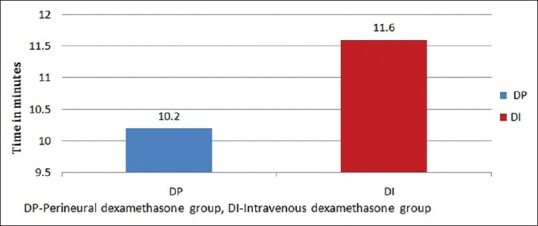
Comparison of onset of sensory block
Time to onset of motor block in Group DP was 13.92 ± 1.754 min which was significantly earlier than Group DI 14.96 ± 1.274 min with a P = 0.02 and dof 48 [Figure 2].
Figure 2.
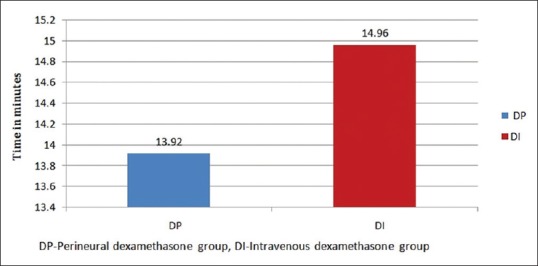
Comparison of onset of motor block
The duration of analgesia in the group receiving perineural dexamethasone (Group DP) 817.2 ± 88.01 min was comparable to the group receiving intravenous dexamethasone (Group DI) 858.00 ± 86.16 with a P = 0.104 and dof 48 [Figure 3].
Figure 3.
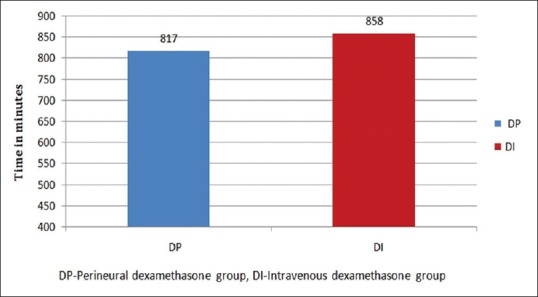
Comparison of duration of analgesia
There were no major side effects in any of the groups. Vitals were stable throughout the surgery. Two patients in the Group DP had emesis in the postoperative period. Symptoms of both the patients were relieved on giving injection ondansetron 4 mg intravenously. Statistical analysis of outcomes are summarised in Table 2.
Table 2.
Statistical analysis of outcomes
| Group DP | Group DI | P | dof | |
|---|---|---|---|---|
| Duration of analgesia | 817.2±88.01 | 858.00±86.16 | 0.104 | 48 |
| Onset of sensory block | 10.2±1.443 | 11.60±1.443 | 0.001 | 48 |
| Onset of motor block | 13.92±1.754 | 14.96±1.274 | 0.02 | 48 |
DP=Perineural dexamethasone, DI=Intravenous dexamethasone, dof=Degree of freedom
DISCUSSION
Acute postoperative pain is an undesirable outcome in any surgical procedure and can delay the functional recovery of the patient.[7] Although general anesthesia continues to be the choice of anesthesia for most of the surgical procedures, regional anesthesia has been increasing in popularity in recent years. This is mainly because the regional anesthesia techniques can be utilized for analgesia not only during the operative period, but during the postoperative period as well. Other advantages are that it avoids the complications of general anesthesia and results in reduced opioid consumption, decreased hospital cost, and increased patient satisfaction.[8] Painful procedures previously requiring inpatient hospital admission for pain control are now commonly performed as ambulatory procedures facilitated by regional anesthesia. This is very important in our setting where postoperative pain is often reported to be inadequately managed.
Brachial plexus block is widely used in our practice for forearm and hand surgeries. It provides good intraoperative and postoperative analgesia. The brachial plexus block consists of injecting local anesthetic drugs in the fascial spaces surrounding the nerve plexus, thereby blocking the autonomic, sensory, and motor fibers supplying the upper extremity. It is a simple, safe, and effective technique of anesthesia having distinct advantages over general and intravenous regional anesthesia. A regional technique should always be considered whenever general condition of the patient is poor, or the patient is not adequately prepared or in the presence of associated conditions such as uncontrolled diabetes, cardiovascular, or respiratory diseases.
Supraclavicular approach to the brachial plexus block provides analgesia suitable for most surgical procedures of elbow, forearm, and hand including fracture manipulations. Due to the versatility of this approach, supraclavicular block has been called the spinal of the upper extremity. A common limitation of single injection peripheral nerve block is its brief duration of action. To circumvent this limitation, one can place a perineural catheter. However, it may be accompanied by problems such as catheter migration, anesthetic leakage, or pump malfunction requiring complex logistic organization. Another common option is the use of adjuvants to improve block duration. Dexamethasone is one such adjuvant.[8]
Dexamethasone is a synthetic glucocorticoid that has anti-inflammatory and immunosuppressant properties.[9] Dexamethasone sodium phosphate is water soluble, rendering it appropriate for parenteral use. Although analgesic mechanism of dexamethasone is still unclear, it seems that a decrease in cyclooxygenase and lipoxygenase production, via inhibition of peripheral phospholipase, plays a main role.[10] This is supported by the finding that the degree of block prolongation had the same rank order as the relative anti-inflammatory potencies of glucocorticoids and is completely reversed by administration of specific glucocorticoid receptor antagonist, In addition, dexamethasone reduces bradykinin which reinforces pain in the inflamed tissues and operated area. The decreased concentration of nerve proteins secreted from the peripheral nerve system also help in the analgesic effect. Local effects include blocking transmission of nociceptive unmyelinated C-fibers and suppressing ectopic neuronal discharge.[11] They might bring about this effect by altering the function of potassium channels in the excitable cells.
Several studies have shown that addition of 4–8 mg of dexamethasone to local anesthetics effectively and significantly prolongs the duration of analgesia.[12,13,14] Similarly, there are studies which show that intravenous dexamethasone given preoperatively effectively controls postoperative pain.[15]
In a study by Desmet et al.,[16] the authors conducted a prospective double-blind, randomized, placebo-controlled study to test the hypothesis that perineural and intravenous dexamethasone would have an equivalent effect on prolonging analgesic duration of interscalene block. They concluded that the route of administration did not have an impact on duration of analgesia for interscalene block with ropivacaine.
In another study by Rahangdale et al.,[17] the authors compared effects of perineural and intravenous dexamethasone on sciatic nerve block with bupivacaine. The primary outcome evaluated was the global score in quality of recovery (QoR-40). The secondary outcomes included analgesia duration, opioid consumption, patient satisfaction, numeric pain rating scores, and postoperative neurologic symptoms. They concluded that preoperative administration of intravenous and perineural dexamethasone compared with saline did not improve overall QoR-40 or decrease opioid consumption, but did prolong analgesic duration in patients undergoing elective foot and ankle surgery and receiving sciatic nerve block. They also opined that due to the lack of clinical benefit and concern of dexamethasone neurotoxicity[18,19] as demonstrated in animal studies, the practice of perineural dexamethasone administration needs to be further evaluated.
In a study by Abdallah et al.,[20] they tested the hypothesis that intravenous and perineural dexamethasone similarly prolongs the duration of analgesia after supraclavicular brachial plexus block with 0.5% bupivacaine and 8 mg dexamethasone. In this study, duration of analgesia was designated as the primary outcome. They also analyzed motor block duration, pain scores, and opioid consumption. From this study, the authors concluded that the effectiveness of intravenous and perineural dexamethasone in prolonging the duration of analgesia seems similar.
In our study, we tested the hypothesis that perineural and intravenous dexamethasone will equally prolong the duration of analgesia in supraclavicular brachial plexus block with 0.5% bupivacaine and 8 mg dexamethasone administered either via perineural or intravenous route. Duration of analgesia produced by both routes was taken as the primary outcome. We also studied the time to onset of sensory and motor blockade as the secondary outcomes, which were not evaluated in any of the above-mentioned studies. Our study demonstrates that the duration of analgesia is comparable whether dexamethasone is given perineurally or intravenously (P = 0.104). However, time to onset of both sensory and motor blockade has a significant difference, perineural administration of dexamethasone resulting in a faster onset of blockade than intravenous route.
From these data and from review of available literature, we could prefer an intravenous route of administration of dexamethasone as an additive in brachial plexus block. This is due to better understanding of potential side effects of the drug when administered intravenously. It will also reduce the potential for neurotoxicity, contamination, and other hazards. Limitations of our study include the sample size and observational nature of the study. We also could not do a long term follow up of patients given perineural dexamethasone for any delayed neurological complications. Perhaps a much larger experimental study, with preservative-free dexamethasone would help to formulate a more definitive conclusion.
CONCLUSION
It is concluded from this study that both intravenous and perineural routes of administration of dexamethasone equally prolong the duration of analgesia in supraclavicular brachial plexus block. However, perineural dexamethasone results in a faster onset of motor and sensory blockade.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Brummett CM, Williams BA. Additives to local anesthetics for peripheral nerve blockade. Int Anesthesiol Clin. 2011;49:104–16. doi: 10.1097/AIA.0b013e31820e4a49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fisher L, Gordon M. Green's Operative Hand Surgery. 6th ed. Vol. 1. Philadelphia, PA 19103-2899: Elsevier Churchill Livingstone; 2011. Anaesthesia for hand surgery; pp. 25–40. [Google Scholar]
- 3.Hargreaves KM, Costello A. Glucocorticoids suppress levels of immunoreactive bradykinin in inflamed tissue as evaluated by microdialysis probes. Clin Pharmacol Ther. 1990;48:168–78. doi: 10.1038/clpt.1990.132. [DOI] [PubMed] [Google Scholar]
- 4.Movafegh A, Razazian M, Hajimaohamadi F, Meysamie A. Dexamethasone added to lidocaine prolongs axillary brachial plexus blockade. Anesth Analg. 2006;102:263–7. doi: 10.1213/01.ane.0000189055.06729.0a. [DOI] [PubMed] [Google Scholar]
- 5.De Oliveira GS, Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: A meta-analysis of randomized controlled trials. Anesthesiology. 2011;115:575–88. doi: 10.1097/ALN.0b013e31822a24c2. [DOI] [PubMed] [Google Scholar]
- 6.Kumar S, Palaria U, Sinha AK, Punera DC, Pandey V. Comparative evaluation of ropivacaine and ropivacaine with dexamethasone in supraclavicular brachial plexus block for postoperative analgesia. Anesth Essays Res. 2014;8:202–8. doi: 10.4103/0259-1162.134506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gan TJ. Poorly controlled postoperative pain: Prevalence, consequences, and prevention. J Pain Res. 2017;10:2287–98. doi: 10.2147/JPR.S144066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shrestha BR, Maharjan SK, Tabedar S. Supraclavicular brachial plexus block with and without dexamethasone – A comparative study. Kathmandu Univ Med J (KUMJ) 2003;1:158–60. [PubMed] [Google Scholar]
- 9.Barnes PJ. Anti-inflammatory actions of glucocorticoids: Molecular mechanisms. Clin Sci (Lond) 1998;94:557–72. doi: 10.1042/cs0940557. [DOI] [PubMed] [Google Scholar]
- 10.Vyvey M. Steroids as pain relief adjuvants. Can Fam Physician. 2010;56:1295–7, e415. [PMC free article] [PubMed] [Google Scholar]
- 11.Johansson A, Hao J, Sjölund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990;34:335–8. doi: 10.1111/j.1399-6576.1990.tb03097.x. [DOI] [PubMed] [Google Scholar]
- 12.Choi S, Rodseth R, McCartney CJ. Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: A systematic review and meta-analysis of randomized trials. Br J Anaesth. 2014;112:427–39. doi: 10.1093/bja/aet417. [DOI] [PubMed] [Google Scholar]
- 13.Cummings KC, 3rd, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, et al. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine. Br J Anaesth. 2011;107:446–53. doi: 10.1093/bja/aer159. [DOI] [PubMed] [Google Scholar]
- 14.Shrestha BR, Maharjan SK, Shrestha S, Gautam B, Thapa C, Thapa PB, et al. Comparative study between tramadol and dexamethasone as an admixture to bupivacaine in supraclavicular brachial plexus block. JNMA J Nepal Med Assoc. 2007;46:158–64. [PubMed] [Google Scholar]
- 15.Dhanger S, Vaidyanathan B, Rajesh IJ, Vinayagam S, Bahurupi Y, Vimalraj D. Efficacy of low dose intravenous dexamethasone for prolongation of analgesia in supraclavicular block: Randomized controlled trial. Indian J Pain. 2016;30:194. [Google Scholar]
- 16.Desmet M, Braems H, Reynvoet M, Plasschaert S, Van Cauwelaert J, Pottel H, et al. IV and perineural dexamethasone are equivalent in increasing the analgesic duration of a single-shot interscalene block with ropivacaine for shoulder surgery: A prospective, randomized, placebo-controlled study. Br J Anaesth. 2013;111:445–52. doi: 10.1093/bja/aet109. [DOI] [PubMed] [Google Scholar]
- 17.Rahangdale R, Kendall MC, McCarthy RJ, Tureanu L, Doty R, Jr, Weingart A. The effects of perineural versus intravenous dexamethasone on sciatic nerve blockade outcomes: A randomized, double-blind, placebo-controlled study. Anesth Analg. 2014;118:1113–9. doi: 10.1213/ANE.0000000000000137. [DOI] [PubMed] [Google Scholar]
- 18.Williams BA, Hough KA, Tsui BY, Ibinson JW, Gold MS, Gebhart GF, et al. Neurotoxicity of adjuvants used in perineural anesthesia and analgesia in comparison with ropivacaine. Reg Anesth Pain Med. 2011;36:225–30. doi: 10.1097/AAP.0b013e3182176f70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shishido H, Kikuchi S, Heckman H, Myers RR. Dexamethasone decreases blood flow in normal nerves and dorsal root ganglia. Spine (Phila Pa 1976) 2002;27:581–6. doi: 10.1097/00007632-200203150-00005. [DOI] [PubMed] [Google Scholar]
- 20.Abdallah FW, Johnson J, Chan V, Murgatroyd H, Ghafari M, Ami N, et al. Intravenous dexamethasone and perineural dexamethasone similarly prolong the duration of analgesia after supraclavicular brachial plexus block: A randomized, triple-arm, double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2015;40:125–32. doi: 10.1097/AAP.0000000000000210. [DOI] [PubMed] [Google Scholar]


