Abstract
Background:
Endoscopic retrograde cholangiopancreatography (ERCP) is used to diagnose and treat pancreaticobiliary diseases. It is a potentially uncomfortable procedure that needs to be performed under conscious sedation. Safe and effective sedation protocol is the need of an hour.
Aims:
This study aims to evaluate the requirement of propofol using midazolam and dexmedetomidine as premedication for ERCP. The degree of comfort experienced by endoscopist and the patients was also assessed.
Materials and Methods:
A total of sixty patients were enrolled in a randomized, assessor-blinded study in the age group of 40–80 years, American Society of Anesthesiologists physical class II–III undergoing elective ERCP procedures. They were divided into two groups of 30 each. Group D (n = 30): Dexmedetomidine (100 μg/mL + 18 mL saline) loading dose at 1 μg/kg intravenous (IV) over 10 min followed by 0.5 μg/kg/h infusion, and Group M (n = 30): Midazolam at 0.05 mg/kg IV bolus over 10 min followed by normal saline infusion under hemodynamic monitoring. Satisfaction scores, total propofol requirement, and complications such as gagging, restlessness, agitation, postoperative nausea and vomiting were noted and analyzed statistically.
Statistical Analysis:
Statistical analysis was performed using SSPS 17.0 software (SPSS Inc., 233 South Wacker Drive, Chicago, USA). The Chi-square test was applied for nonparametric data and parametric numerical data, unpaired t-test for intergroup comparison, and repeated measures ANOVA for intragroup comparison. Results were expressed as a mean ± standard deviation. Value of P < 0.05 was considered statistically significant and <0.001 as highly significant.
Results:
Surgeons and patients were more satisfied and comfortable along with less requirement of propofol in the dexmedetomidine group. The incidence of complications was also less in the dexmedetomidine group as compared to that of midazolam group.
Conclusion:
Both dexmedetomidine and midazolam can be safely administered as an anesthetic adjuvant to propofol for short procedures like ERCP's. Dexmedetomidine provided intense and better sedation quality along with lesser requirement of propofol doses. Moreover, it provided stable hemodynamic conditions and good recovery characteristics as compared to midazolam group.
Keywords: Conscious sedation, dexmedetomidine, endoscopic retrograde cholangiopancreatography, midazolam, propofol
INTRODUCTION
The use of endoscopic retrograde cholangiopancreatography (ERCP) to diagnose and treat pancreaticobiliary diseases has increased manifold in recent years. Conscious sedation is administered to the patient to make them comfortable and also to facilitate the work of the gastroenterologist.[1] However, sedation in ERCP can also cause adverse perioperative events.[2,3] The availability of various pharmacological agents such as midazolam, propofol, ketamine, and dexmedetomidine not only allows rapid and smooth induction but also enables quick and uneventful recovery.[4,5]
Propofol is a nonbarbiturate sedative-hypnotic agent with faster onset of action and shorter recovery time. It also has anticonvulsant, amnestic, and anti-emetic properties; hence, it is widely used. However, as a sole agent, large doses may be required which can lead to cardiorespiratory depression.[6] Hence, an adjunct may decrease the dose of propofol and thus, its adverse effects too. Thus, drugs with different pharmacological profiles can be combined for desirable results.
Midazolam has gained popularity in day care procedures because of its rapid onset and shorter duration of action with amnestic and anxiolytic properties. It also has beneficial effect on hemodynamic stability.[7] The repeated doses of midazolam lead to prolonged sedation because of accumulation of its active metabolite. It can produce respiratory depression also, as being a benzodiazepine, it decreases the sensitivity of respiratory center to carbon dioxide.[8]
In the past few years, dexmedetomidine has been widely used as substitute to midazolam for minor procedures needing conscious sedation. It is a selective alpha2(α2)-adrenoceptor agonist and has sympatholytic, amnestic, sedative, and analgesic properties. Dexmedetomidine because of its unique properties such as analgesia and minimal respiratory depression is considered a useful and safe drug for day care procedures.[9] It provides excellent sedation that can be easily titrated, especially in nonintubated patients. Hypotension, hypertension, bradycardia, dry mouth, and nausea are the most commonly seen adverse effects.[10]
The primary aim of this study was to evaluate the requirement of propofol using midazolam or dexmedetomidine as premedicant for ERCP and also to assess the degree of comfort experienced by endoscopist as well as the patients as judged by an anesthesiologist. Secondary outcomes were to evaluate and compare the recovery characteristics.
MATERIALS AND METHODS
This was a prospective, randomized, assessor-blinded study conducted at tertiary care hospital of North India, after approval from the Hospital Ethics Committee. A prior written informed consent was obtained from all the patients. Sixty patients were enrolled in the study from December 2016 to September 2018. Patients between the age group of 40 and 80 years, American Society of Anesthesiologists (ASA) physical classes II and III, undergoing elective ERCP procedures were included in this study. Patients on alpha-adrenergic receptor blockers, with known hypersensitivity to the study drug, compromised cardiac status, psychiatric history, with neurological disease and having motor and sensory deficit were excluded from the study. The sample size was calculated (30 in each group), on the basis of previously published articles, keeping precision of estimates of outcome states as 95% of confidence limits.
Preoperative assessment included history, general physical examination, systemic examination, and routine laboratory investigations. Patients were randomly allocated by computer-generated random numbers to one of two groups of 30 each.
Group D (n = 30): Dexmedetomidine (100 μg/ml + 18 mL saline) loading dose at 1 μg/kg intravenous (IV) over 10 min followed by 0.5 μg/kg/h infusion along with intermittent 10 mg propofol bolus until the Ramsay Sedation Score (RSS) 4.
Group M (n = 30): Midazolam at 0.05 mg/kg IV bolus over 10 min followed by normal saline infusion along with intermittent 10 mg propofol bolus until RSS 4.
Patients were taken to operating room and antecubital venous access secured on nondominant hand by 20G IV cannula, Ringer's Lactate drip started by 8 ml/kg/h, and O2 given by nasal cannula at 4 L/min. Standard monitors such as heart rate (HR), mean arterial blood pressure (MAP), and SpO2 were attached. To reduce the bias, 0.05 mL/kg of normal saline was given as IV bolus in Group D, whereas, in Group M, after giving the study drug, IV infusion of normal saline was started. The study drugs were prepared and given by an assistant who was not involved in the study.
Sedation depth was assessed using the Ramsay Sedation Scale.[11] Scale 1: Patient is anxious and agitated or restless, or both; Scale 2: Patient is cooperative, oriented, and tranquil; Scale 3: Patient responds to commands only; Scale 4: Patient exhibits brisk response to light glabellar tap or loud auditory stimulus; Scale 5: Patient exhibits a sluggish response to light glabellar tap or loud auditory stimulus; and Scale 6: Patient exhibits no response.
Sedation level assessed at 1–3-min interval, and the infusion rate adjusted to achieve RSS of 4. The anesthesiologist who assessed the parameters was blinded to the randomization process and to the study drugs, but he adjusted the infusion rates of both the drugs till achieving RSS of 4. Further, if the RSS of 4 was not achieved on increasing the study drug infusion, then propofol bolus of 10 mg IV was given. Time to achieve RSS of 4 in both groups was recorded. Parameters such as HR, MAP, and SpO2 were recorded following the loading dose for 1 min initially till 10 min and then every 10 min until the completion of the procedure.
The Gloucester Comfort Score[12] was used to evaluate the quality of sedation as observed by gastroenterologist, at the time of insertion of scope, periprocedure, and at the end of procedures.
Comfortable – Talking/comfortable throughout
Minimal – One or two episodes of mild discomfort without distress to patient
Mild – More than two episodes of discomfort without distress
Moderate – Significant discomfort with some distress
Severe – Frequent discomfort with significant distress.
The Numeric Rating Score[13] (0–10) was used by anesthesiologist to assess patient's discomfort every 10-min interval throughout the procedure. Numeric Rating Scale – 0-no discomfort to 10-severe discomfort
During the procedure, any of the following complications such as apnea and oxygen desaturation (SpO2 <94% for >30 s treated with supplemental oxygen), bradycardia (HR <50/min treated with atropine IV bolus of 0.5 mg), tachycardia (>20% of the baseline), hypotension (<20% of the baseline and treated with IV ephedrine bolus dose of 6 mg or mephenteramine 6 mg) coughing or gagging were recorded and managed accordingly. The study drug infusion was discontinued at the end of the procedure. The recovery time was considered from discontinuation of the infusion till achieving Modified Aldrete Score (MAS)[14] of 9–10 [Table 1]. Vitals such as HR, MAP, and SpO2 were recorded every 10-min interval. Postoperative nausea and vomiting (PONV), apnea, pain, and agitation were also managed accordingly. Patient's and endoscopist's satisfaction was assessed at the end of procedure using satisfaction score (4 = excellent, 3 = good, 2 = fair, and 1 = bad).
Table 1.
Modified aldrete’s score
| Parameter | Score | ||
|---|---|---|---|
| 2 | 1 | 0 | |
| Activity | Moves all extremities voluntarily or on command | Moves two extremities voluntarily or on command | Unable to move extremities |
| Respiration | Breathes deeply and coughs freely | Dyspnea, shallow, or limited breathing | Apneic |
| Circulation | BP±20 mm of preanesthetic level | BP±20-50 mm of preanesthetic level | BP±50 mm of preanesthetic level |
| Consciousness | Fully awake | Arousable on calling | Not responding |
| Oxygen saturation | SpO2 >92% on room air | Supplemental O2 required to maintain SpO2 >90% | SpO2 <90% with O2 supplementation |
Total score=10; a score of evelvelor on command to achBP=Blood pressure
On completion of the procedure, further propofol boluses and background infusion of the study drug were stopped. Patient's oropharynx was thoroughly suctioned and they were turned supine with head-up tilt (15°), allowed for complete recovery with end points being eye opening on command, ability to handle secretions, following simple commands, hemodynamic stability, and maintaining saturation >95% on room air.
Patients were kept in propped up position with oxygen supplementation through a face mask (5 L/min) and maintenance of IV fluid (Ringer's Lactate/0.9% saline). Standard monitoring was continued throughout till discharge of the patient at MAS of 9–10.
Statistical analysis
Statistical analysis was done with SSPS 17.0 software (SPSS Inc., 233 South Wacker Drive, 11th floor, Chicago, IL6060660412, USA). The Chi-square test was applied for nonparametric data and parametric numerical data, unpaired t-test for intergroup comparison, and repeated measures ANOVA for intragroup comparison. Results were expressed as a mean ± standard deviation. Value of P < 0.05 was considered statistically significant and <0.001 as highly significant.
RESULTS
A total of 77 patients were chosen, of which 12 patients did not fit into the inclusion criteria and five refused to participate in the study. Finally, 60 patients were included [Figure 1]. There were no statistically significant differences in both the groups in terms of age, sex, type and duration of the procedure, ASA physical status classes, and the baseline vitals [Table 2].
Figure 1.
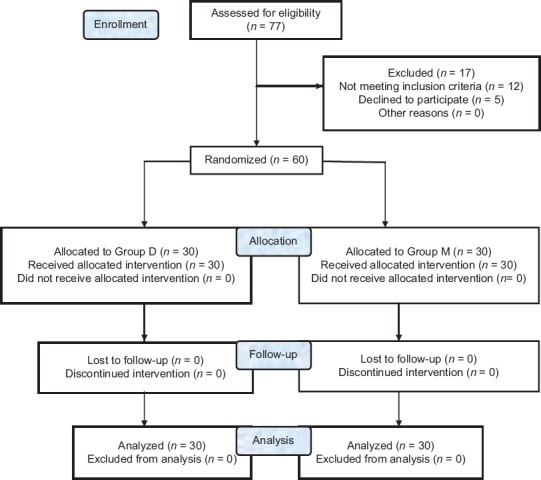
Consort diagram
Table 2.
Demographic data
| Variables | Group D | Group M | P |
|---|---|---|---|
| Age (years) | 45.34±16.4 | 47.21±14.3 | >0.45 |
| Sex (male/female) | 17/13 | 15/15 | >0.39 |
| Duration of procedure (min) | 30.62±10.23 | 32.40±9.45 | >0.42 |
| ASA classes | |||
| II | 13 | 12 | >0.78 |
| III | 17 | 18 | >0.89 |
Data given as mean±SD. SD=Standard deviation, ASA=American Society of Anesthesiologists
The total number of propofol doses in Group M was higher than that in Group D, and this difference was statistically highly significant (P < 0.023) [Table 3 and Figure 2].
Table 3.
Mean number of propofol doses and time to achieve Ramsay Sedation Score 4
| Variables | Group D | Group M | P |
|---|---|---|---|
| Number of propofol doses | 0.70±0.596 | 3.4±0.675 | <0.023 |
| Time to achieve RSS 4 (min) | 3.34±0.96 | 5.96±1.20 | <0.042 |
RSS=Ramsay Sedation Score
Figure 2.
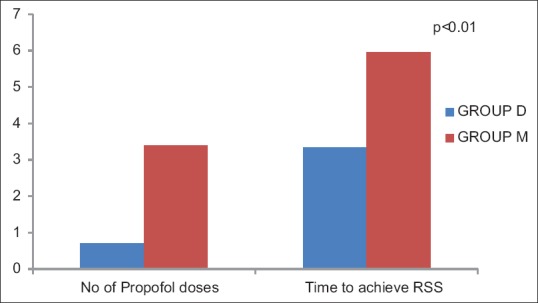
Mean number of propofol doses and time to achieve Ramsay Sedation Score 4
RSS 3–4 was achieved earlier in Group M (P < 0.042). Mean baseline hemodynamic variables were similar in both the groups. Intraoperatively, there was more decrease in HR and MAP in Group D than in Group M at 5, 10, and 20 min which was clinically insignificant [Figure 3].
Figure 3.
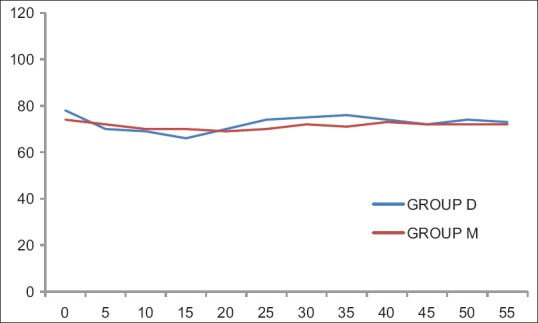
Intraoperative heart rate in both groups
The surgeon and anesthesiologists were more satisfied in Group D as compared to that of Group M (P < 0.031) [Table 4].
Table 4.
Satisfaction scores
| Score | Group D | Group M | P |
|---|---|---|---|
| GCS | 3.6±0.498 | 2.43±0.50 | <0.031 |
| NRS | 6.60±0.49 | 3.33±0.479 | <0.029 |
GCS=Gloucester Comfort Score, NRS=Numeric Rating Score
The complications such as gagging, restlessness, and agitation were higher in the midazolam group as compared to dexmedetomidine group (P < 0.01). In terms of complications in the recovery period, PONV was more in Group D than that in Group M. None of the patients in any group experienced oxygen desaturation and respiratory depression [Table 5].
Table 5.
Perioperative complications
| Variables | Group D (n=30) (%) | Group M (n=30) (%) | P |
|---|---|---|---|
| Gagging | 20 | 87 | <0.01 |
| Restlessness | 8 | 52 | <0.01 |
| Agitation | 3 | 48 | <0.01 |
| Postoperative nausea vomiting | 7 | 2 | <0.05 |
| Desaturation | 0 | 0 | |
| Respiratory depression | 0 | 0 |
Patients in Group D achieved MASs of 9–10 earlier than those in Group M (P < 0.33) [Table 6].
Table 6.
Time to achieve Modified Aldrete Score 9-10
| Variables | Group D | Group M | P |
|---|---|---|---|
| Time to achieve MAS 9-10 (min) | 11.13±2.12 | 15±3.29 | 0.33 |
MAS=Modified Aldrete Score
DISCUSSION
ERCP has evolved from a diagnostic solution to therapeutic procedure. It not only requires expertise in the technique but also adequate sedation and anesthesia with lesser complications, discomfort, and anxiety.
Midazolam, a short-acting benzodiazepine, is commonly used adjunct with propofol for short procedures such as endoscopies. It has faster onset, shorter duration of action, and high amnestic properties. However, when used alone, higher doses are required to maintain the desired depth of sedation which can lead to cardiorespiratory depression and prolonged recovery time.[7]
Dexmedetomidine, an alpha2-adrenergic agonist is recently being used for conscious sedation. It has sedative as well as analgesic properties without appreciable respiratory depression. However, when used as a sole agent for conscious sedation, it was not found to be much effective. Hence, it was used in combination with propofol.[9]
Propofol is a commonly used sedative agent for endoscopies. However, when used alone in higher doses it leads to hemodynamic variations and deep sedation. Hence, by using adjuvants with propofol, these complications can be avoided.[9] Midazolam and low-dose dexmedetomidine were used in our study along with intermittent doses of propofol because of their synergistic effects and favorable outcomes.
Patients in Group M had a rapid onset of sedation (3.34 ± 0.96 min compared to 5.96 ± 1.20 min) but did not achieve the adequate depth of sedation as compared to Group D, probable because of methods of administration IV bolus versus infusion. Similar pattern has been seen in another studies also.[7,15]
A synergistic effect was seen when these sedative drugs were used in combination with propofol. Synergism was more in dexmedetomidine group than midazolam group, which led to decrease propofol requirement in dexmedetomidine group. Similar effect has also been observed in another studies.[16,17,18] As dexmedetomidine is known to suppress neuronal activity and facilitate vagal activity by alpha2 receptor activation in the central nervous system; hence, it has decreased the propofol requirement in Group D.
Statistically significant but clinically insignificant decrease in HR and BP at 5, 10, and 20 min was observed in Group D. Similar observations were reported by Kilic et al., Alhashemi, Dere et al., and Sethi et al.[7,15,19,20] Being an alpha2 agonists agent, dexmedetomidine causes hypotension and bradycardia by activation of alpha2-adrenoreceptor.
Dexmedetomidine group has higher satisfaction scores for both patient and endoscopist, probably due to steady drug levels achieved by infusion form of dexmedetomidine as compared to IV bolus of midazolam. Other authors, also, reported higher satisfaction for dexmedetomidine than midazolam.[7,15]
Although we expected greater incidence of adverse events in Group D than in Group M, but actually there was no significant difference with regard to hypotension, bradycardia, and respiratory depression between the two groups. Similarly, various studies also did not show any significant differences in hemodynamic variables.[21] However, the incidence of complications was higher in midazolam group as compared to that of dexmedetomidine group, that is, gagging (87% vs. 20%), restlessness (52% vs. 8%), and agitation (48% vs. 3%), and the difference was statistically significant. Other complications such as nausea and vomiting were seen in 7% of patients in Group D and 2% in Group M (P > 0.05%). Arain and Ebert[22] and Sethi et al.[7] did not report any intra- and post-operative complications in the dexmedetomidine group.
Time to achieve modified alderete score of 9-10 was more in group M (15±3.24 mins) as compared to group D (11.13±2.12 mins). Similar observations were made by Tomar et al.[23] Midazolam when used with propofol, decreases the propofol requirement but does not produce quality sedation and thus leads to prolonged recovery times. This characteristic arousable sedation action of dexmedetomidine can be explained by its action on α2-adrenoreceptors in locus ceruleus in the brain stem which declines sympathetic but enhances parasympathetic outflow.
The strengths of this study were the absence of selection bias between the groups and also both the groups were comparable in terms of patient characteristics, type and duration of the procedure along with no significant adverse effect with any of the study drugs.
The only limitation of our study was that we did not use bispectral index (BIS) monitoring for assessing the sedation adequacy. Hence, in future, research can be planned with the use of BIS monitor for the depth of sedation.
CONCLUSION
Both dexmedetomidine and midazolam can be safely administered as an anesthetic adjuvant to propofol for short procedures such as ERCPs. Dexmedetomidine provided intense and better sedation quality along with lesser requirement of propofol doses with no significant hemodynamic alterations and good recovery characteristics as compared to midazolam.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chen WX, Lin HJ, Zhang WF, Gu Q, Zhong XQ, Yu CH, et al. Sedation and safety of propofol for therapeutic endoscopic retrograde cholangiopancreatography. Hepatobiliary Pancreat Dis Int. 2005;4:437–40. [PubMed] [Google Scholar]
- 2.Cotton PB. Endoscopic retrograde cholangiopancreatography: Maximizing benefits and minimizing risks. Gastrointest Endosc Clin N Am. 2012;22:587–99. doi: 10.1016/j.giec.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 3.Paspatis GA, Chainaki I, Manolaraki MM, Vardas E, Theodoropoulou A, Tribonias G, et al. Efficacy of bispectral index monitoring as an adjunct to propofol deep sedation for ERCP: A randomized controlled trial. Endoscopy. 2009;41:1046–51. doi: 10.1055/s-0029-1215342. [DOI] [PubMed] [Google Scholar]
- 4.Heidari SM, Loghmani P. Assessment of the effects of ketamine-fentanyl combination versus propofol-remifentanil combination for sedation during endoscopic retrograde cholangiopancreatography. J Res Med Sci. 2014;19:860–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Ramkiran S, Iyer SS, Dharmavaram S, Mohan CV, Balekudru A, Kunnavil R. BIS targeted propofol sparing effects of dexmedetomidine versus ketamine in outpatient ERCP: A prospective randomised controlled trial. J Clin Diagn Res. 2015;9:UC07–12. doi: 10.7860/JCDR/2015/12435.5991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fechner J, Ihmsen H, Hatterscheid D, Jeleazcov C, Schiessl C, Vornov JJ, et al. Comparative pharmacokinetics and pharmacodynamics of the new propofol prodrug GPI 15715 and propofol emulsion. Anesthesiology. 2004;101:626–39. doi: 10.1097/00000542-200409000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Sethi P, Mohammed S, Bhatia PK, Gupta N. Dexmedetomidine versus midazolam for conscious sedation in endoscopic retrograde cholangiopancreatography: An open-label randomised controlled trial. Indian J Anaesth. 2014;58:18–24. doi: 10.4103/0019-5049.126782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gan TJ. Pharmacokinetic and pharmacodynamic characteristics of medications used for moderate sedation. Clin Pharmacokinet. 2006;45:855–69. doi: 10.2165/00003088-200645090-00001. [DOI] [PubMed] [Google Scholar]
- 9.Sakaguchi Y, Takahashi S. Dexmedetomidine. Masui. 2006;55:856–63. [PubMed] [Google Scholar]
- 10.Naaz S, Ozair E. Dexmedetomidine in current anaesthesia practice – A review. J Clin Diagn Res. 2014;8:GE01–4. doi: 10.7860/JCDR/2014/9624.4946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2:656–9. doi: 10.1136/bmj.2.5920.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ball AJ, Rees CJ, Corfe BM, Riley SA. Sedation practice and comfort during colonoscopy: Lessons learnt from a national screening programme. Eur J Gastroenterol Hepatol. 2015;27:741–6. doi: 10.1097/MEG.0000000000000360. [DOI] [PubMed] [Google Scholar]
- 13.Thong IS, Jensen MP, Miró J, Tan G. The validity of pain intensity measures: What do the NRS, VAS, VRS, and FPS-R measure? Scand J Pain. 2018;18:99–107. doi: 10.1515/sjpain-2018-0012. [DOI] [PubMed] [Google Scholar]
- 14.Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970;49:924–34. [PubMed] [Google Scholar]
- 15.Dere K, Sucullu I, Budak ET, Yeyen S, Filiz AI, Ozkan S, et al. A comparison of dexmedetomidine versus midazolam for sedation, pain and hemodynamic control, during colonoscopy under conscious sedation. Eur J Anaesthesiol. 2010;27:648–52. doi: 10.1097/EJA.0b013e3283347bfe. [DOI] [PubMed] [Google Scholar]
- 16.Ong WC, Santosh D, Lakhtakia S, Reddy DN. A randomized controlled trial on use of propofol alone versus propofol with midazolam, ketamine, and pentazocine “sedato-analgesic cocktail” for sedation during ERCP. Endoscopy. 2007;39:807–12. doi: 10.1055/s-2007-966725. [DOI] [PubMed] [Google Scholar]
- 17.Mukhopadhyay S, Niyogi M, Sarkar J, Mukhopadhyay BS, Halder SK. The dexmedetomidine “augmented” sedato analgesic cocktail: An effective approach for sedation in prolonged endoscopic retrograde cholangio-pancreatography. J Anaesthesiol Clin Pharmacol. 2015;31:201–6. doi: 10.4103/0970-9185.155149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghodki PS, Thombre SK, Sardesai SP, Harnagle KD. Dexmedetomidine as an anesthetic adjuvant in laparoscopic surgery: An observational study using entropy monitoring. J Anaesthesiol Clin Pharmacol. 2012;28:334–8. doi: 10.4103/0970-9185.98329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kilic N, Sahin S, Aksu H, Yavascaoglu B, Gurbet A, Turker G, et al. Conscious sedation for endoscopic retrograde cholangiopancreatography: Dexmedetomidine versus midazolam. Eurasian J Med. 2011;43:13–7. doi: 10.5152/eajm.2011.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alhashemi JA. Dexmedetomidine vs. midazolam for monitored anaesthesia care during cataract surgery. Br J Anaesth. 2006;96:722–6. doi: 10.1093/bja/ael080. [DOI] [PubMed] [Google Scholar]
- 21.Riphaus A, Stergiou N, Wehrmann T. Sedation with propofol for routine ERCP in high-risk octogenarians: A randomized, controlled study. Am J Gastroenterol. 2005;100:1957–63. doi: 10.1111/j.1572-0241.2005.41672.x. [DOI] [PubMed] [Google Scholar]
- 22.Arain SR, Ebert TJ. The efficacy, side effects, and recovery characteristics of dexmedetomidine versus propofol when used for intraoperative sedation. Anesth Analg. 2002;95:461–6. doi: 10.1097/00000539-200208000-00042. [DOI] [PubMed] [Google Scholar]
- 23.Tomar GS, Singh F, Ganguly S, Gaur N. Is dexmedetomidine better than propofol and fentanyl combination in minor day care procedures? A prospective randomised double-blind study. Indian J Anaesth. 2015;59:359–64. doi: 10.4103/0019-5049.158740. [DOI] [PMC free article] [PubMed] [Google Scholar]


