Abstract
Although there have been many improvements in prognosis for patients with cancer, anticancer therapies are burdened by the risk of cardiovascular toxicity. Heart failure is one of the most dramatic clinical expressions of cardiotoxicity, and it may occur acutely or appear years after treatment. This article reviews the main mechanisms and clinical presentations of left ventricular dysfunction induced by some old and new cardiotoxic drugs in cancer patients, referring to the most recent advances in the field. The authors describe the mechanisms of cardiotoxicity induced by anthracyclines, which can lead to cardiovascular problems in up to 48% of patients who take them. The authors also describe mechanisms of cardiotoxicity induced by biological drugs that produce left ventricular dysfunction through secondary mechanisms. They outline the recent advances in immunotherapies, which have revolutionised anticancer therapies.
Keywords: Anticancer drugs-induced cardiotoxicity, heart failure, anthracyclines, HER2, VEGF, immunotherapy.
The increasing progress in cancer therapies has reduced mortality rates for many cancers. Unfortunately, many life-saving therapies are burdened by the risk of cardiotoxicity (CTX). The cardiovascular system appears to be particularly susceptible to the action of many anti-neoplastic drugs, which may cause vasospastic or thromboembolic ischaemia, arterial hypertension, dysrhythmia, and left ventricular (LV) dysfunction, leading to heart failure (HF).[1–7] These problems are even more relevant in an ageing population as cancer can occur in patients with pre-existing cardiovascular conditions.[8]
Some of these side-effects may occur or persist once the cancer is eliminated or controlled. Asymptomatic reduction in LV function and HF are the typical complications of cancer therapies in the long term.[9] Many studies have tried to clarify the mechanisms underlying cancer therapy-related HF.[10]
Anthracyclines (ANTs) are the most studied cardiotoxic drugs. The main mechanism hypothesised for their cardiotoxicity is direct damage of cardiomyocytes through the production of reactive oxygen species (ROS) and reactive nitrogen species.[11–15] With the increasing use of new biological drugs, other mechanisms of CTX have been observed, with drugs that affect the heart through secondary mechanisms.[16] Newer intracellular signalling inhibitors block pathways of primary importance for myocardial function, especially under conditions of cardiac stress, such as hypertension or hypertrophy.[17] Furthermore, in recent years, a growing incidence of myocarditis, due to the use of immune checkpoint inhibitors that unleash immune responses, has been recorded.[18–21]
This situation is complicated by the fact that novel biological drugs are sometimes combined (concomitantly or sequentially) with traditional chemotherapies. A typical example is the anti-ErbB2 receptor antibody trastuzumab, which can lead to LV dysfunction on its own and in people without pre-existing cardiovascular disease, but also unmask or worsen LV dysfunction in patients previously treated with ANTs, by interfering with the neuregulin/ErbB2 pathway that seems to modulate the increase in ROS-caused ANTs.[1,2,22,23]
Anthracyclines
ANTs are a typical example of cardiotoxic anticancer drugs, and their effects have been observed and studied since the 1960s.[24] ANT-induced cardiomyopathy is characterised by the occurrence of cardiomyocyte damage that can eventually lead to HF. ANTs are a keystone in the treatment of many cancers, such as lymphomas, leukaemias and sarcomas, but also for early or advanced breast cancer.[17] Their side-effects are usually dose-dependent and more frequently detected in the first year after completing treatment.[25,26] ANT CTX can manifest acutely in up to 30% of patients soon after infusion, requiring either modification or withdrawal of anticancer regimens. Risk factors have been identified for the development of cancer therapy-related HF, pre-existing heart disease and advanced age.[25] Moreover, there seems to be a gender-related predisposition. Although experimental data point towards better resistance from women regarding cardiotoxicity with involvement of mitochondria and less oxidative stress, very few studies have been conducted in humans, although female patients in clinical studies appear to be more susceptible to doxorubicin-induced cardiotoxicity.[2,27,28] This apparent paradox may be explained because both age and menopausal status seem to be the two most important determinants of the sex-specific differences observed in the clinical setting, with higher susceptibility in prepuberal girls and post-menopausal women. Studies in young children receiving anticancer drugs for haematological malignancies suggest that prepuberal girls are more susceptible to develop early or late cardiac toxicity than boys of the same age.[27,29] These data are consistent with the absence of female hormones at this age. Unfortunately, no survey has been conducted to specifically assess sex differences in the occurrence of ANT cardiotoxicity in adults.
Several mechanisms underlying anthracycline CTX have been observed, but the main ones we will focus on are induction of oxidative stress, activation of DNA damage responses and impairment of mitochondrial biogenesis and metabolism. The consequence of these processes is cardiomyocyte death, apoptosis and necrosis, while the surviving cardiomyocytes develop maladaptive changes. This leads to pathological remodelling of the LV, with dilatation and impairment of contractility, until the decline of systolic function and development of clinically manifest HF.[9]
ANTs are characterised by a marked susceptibility to be rapidly reduced to unstable metabolites, such as doxorubicin-semiquinone, which generate hydrogen peroxide and superoxide by reacting with oxygen. ROS are also produced thanks to the ability of these drugs to chelate intracellular free iron, creating iron-doxorubicin complexes that react with oxygen (Figure 1). Furthermore, ANTs can directly interfere with the activity of major iron-transporting and iron-binding proteins, such as ABCB8, a mitochondrial iron exporter, promoting mitochondrial iron accumulation and ROS production. It has also been observed that hearts from patients with doxorubicin-related heart dysfunction have significantly higher mitochondrial iron levels than in patients with other types of cardiomyopathies or normal cardiac function.[30]
Figure 1: The Main Mechanisms of Anthracycline-induced Injury to Cardiac Cells.
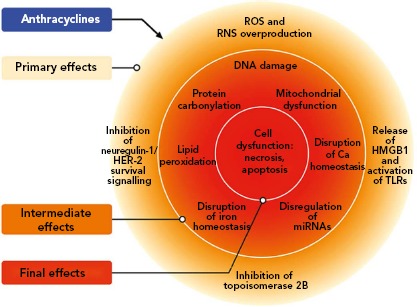
The classic model of anthracycline (ANT) cardiotoxicity involves the generation of reactive oxygen species (ROS) by the quinone moiety common to all anthracyclines. ROS and RNS hyperproduction results in damage to DNA, protein carbonylation and lipid peroxidation, leading to cellular dysfunction and cardiomyocyte death. ANTs can also bind and block the functions of topoisomerases 2A (TOP2A) and 2B (TOP2B). Tumour cells express high levels of TOP2A, whereas TOP2B is ubiquitously expressed. Cardiomyocytes express TOP2B, but not TOP2A. ANTs form a complex with TOP2B inhibiting its enzymatic activity. Without functional TOP2B, DNA breaks accrue, leading to the activation of p53 tumour-suppressor protein, mitochondrial dysfunction and the generation of ROS that result in cardiomyocyte death. Another mechanism underlying doxorubicin-dependent oxidative stress is linked to the ability of the drug to directly interfere with the activity of NADPH oxidase and nitric oxide synthase (NOS). Both NADPH oxidase and NOS can transfer electron from NADPH to doxorubicin, causing the formation of semiquinone doxorubicin (SQ-DOX). SQ-DOX in turn transfers an electron to O2 and generates O2−. In the NOS compartment, O2− can react with NO to form peroxynitrite (ONOO−), a powerful oxidant that can generate free radicals. An alternative mechanism by which ANTs exert their cardiotoxic effects is the inhibition of neuregulin-1-human epidermal growth factor receptor 2 in cardiomyocytes. Doxorubicin also induces necrosis of immune (i.e. macrophages) and cancer cells, releasing high mobility group box 1, which activates Toll-like receptors 2 and 4 in cardiomyocytes and inflammatory cells, inducing the release of proinflammatory cytokines. These primary effects induce a plethora of secondary effects in cardiomyocytes, such as DNA damage, lipid peroxidation, mitochondrial dysfunction, which result in cell dysfunction and death.[9]
HER-2 = human epidermal growth factor receptor 2; HMGB1 = high mobility group box 1 miRNA = micro RNA; RNS = reactive nitrogen species; ROS = reactive oxygen species; TLR = Toll-like receptor. Source: Varricchi et al.[9] Reproduced with permission from Frontiers.
Research led by Edward Yeh has shown that the production of ROS could also be secondary to the interaction of ANTs with the beta isozyme of topoisomerase 2 (Top2), the only isoform expressed by adult mammalian cardiomyocytes.[31] While the interaction of the drug with Top2-alpha – overexpressed in proliferating cancerous cells but not in quiescent tissues – generates a ternary Top2-doxorubicin-DNA cleavage complex that in turn triggers the death of tumour cells, the Top2-beta-doxorubicin-DNA complex induces DNA double strand breaks, ultimately promoting cardiomyocyte death.[31] The ensuing DNA break induces the activation of p53, an enzyme that activates the proteins responsible for the DNA repair process, but can also repress genes involved in mitochondrial biogenesis, such as PPARGC1, oxidative phosphorylation, ultimately leading to defective organelle biogenesis and metabolic failure.[31] An abnormal accumulation of mitochondria damaged by doxorubicin in the myocardium has also been reported, promoting the production of ROS and the death of cardiomyocytes. This accumulation would seem to be caused by the activation of p53, which is able to inhibit the normal recycling of dysfunctional mitochondria via autophagy.[9]
ANTs are also involved in the activation of the mitogen-activated protein kinase (MAPK) cascade through reactive oxygen species and Ca2+. In particular, it is worth mentioning the role of p38 MAPK in the induction of cardiomyocyte death.[32] It has been demonstrated that before any clinical sign of LV dysfunction in ANT cardiotoxicity, there is a reduction in the phosphocreatine:adenosine triphosphate ratio, suggesting the presence of alterations in myocardial energetics.[33] In this study, the authors also demonstrated that ANTs can affect the normal functioning of creatine kinase (CK) by oxidising its sulfhydryl groups. More studies on this pathway are needed to identify novel cardioprotective therapeutic approaches. The possible protective role of CK in heart diseases is supported by improved cardiac function in murine hearts overexpressing myofibrillar CK and subjected to pressure overload, compared with non-transgenic mice.[34] Moreover, CK overexpression seems to improve cardiac function and general myocardial energetics and also the survival of mice affected by CTX induced by ANTs.[35]
Among their other effects on cardiomyocytes energy metabolism, ANTs can alter fatty acid oxidation, due to a reduction of the phosphorylation of the enzyme anti-acetyl-CoA carboxylase and of the intracellular concentration of 5’-activated protein kinase (AMPK). Further studies will be needed to clarify the role of AMPK in ANTs-induced HF.[36,37]
Several approaches have been proposed to reduce ANT CTX. Beside limiting the cumulative anthracycline doses, the interest of the scientific community has also been focusing on antioxidant drugs.[2,3] However, none of these strategies is unanimously recommended, emphasising the need for further studies.[8] The use of dexrazoxane has been clinically evaluated in children treated with doxorubicin for acute lymphoblastic leukaemia, resulting in reduced myocardial injury, as indicated by a decreased level of serum troponin T.[15,38]
Among traditional HF drugs, beta-blockers have been shown to reduce oxidative stress and calcium overload in myocardial cells.[39,40] Carvedilol has been shown to have a preventive role against LV dysfunction in patients treated with ANTs reducing the production of ROS, apoptosis of cardiomyocytes and mitochondrial alterations.[41–43] In some experimental models of ANT-induced cardiotoxicity, nebivolol was also able to improve LV function, increase nitric oxide (NO) levels and reduce oxidative stress.[44,45] Nebivolol, used before ANT-based treatments, also reduced the incidence of LV dysfunction, compared with placebo.[46]
The renin-angiotensin-aldosterone system also plays a key role in ANT-induced CTX.[47] In particular, in patients treated with ANTs, enalapril reduced the incidence of LV dysfunction when compared with placebo.[48] In vitro and in vivo experiments demonstrated the cardioprotective effects of angiotensin receptor blockers – candesartan can reduce in vitro ANT cardiotoxicity, while telmisartan can blunt acute LV dysfunction induced by doxorubicin when administered pre- and post-chemotherapy in rats.[49] Furthermore, telmisartan can inhibit the production of TNF-alpha and interleukin 6 and can affect the availability of NO.[50] It also seems that the co-administration of angiotensin-converting enzyme inhibitors and carvedilol can reduce cardiac damage induced by ANTs.[51]
Biological Drugs
Anti-ErbB2 Drugs
ErbB2 (also known as HER-2/NEU) belongs to the epidermal growth factor receptor (EGFR) family. These receptors can homodimerise or heterodimerise and are phosphorylated upon binding with their ligands, initiating several cellular responses.[52] ErbB2 is overexpressed in 25–30% of breast cancers and this has led to research specifically targeting drugs such as trastuzumab, pertuzumab and lapatinib.[53]
Trastuzumab is the prototypical biological drug. It is a humanised monoclonal antibody that targets ErbB2, binding to its extracellular domain IV, and has revolutionised ErbB2+ breast cancer protocols since its introduction in 1998. It can also cause CTX that spans from asymptomatic decreases in LV ejection fraction (LVEF) to congestive HF.[1,10,54] Most patients with little or no risk factors can tolerate trastuzumab for long periods of time. Given the importance of this drug in ErbB2+ breast cancer, the Cardiac Safety Study in Patients With HER2 + Breast Cancer (SAFE-HEaRt study) has been designed to evaluate whether anti-HER2 therapies can be given to women with mildly reduced heart function and optimised cardiac therapy and monitoring.[55]
The mechanisms of CTX induced by ErbB2 blockers have not been fully elucidated (Figure 2). In the heart, neuregulin, secreted from endothelial cells, upon binding to ErbB4 induces the dimerisation of ErbB4 and ErbB2, thus activating protective trophic and pro-survival pathways in response to stress, such as hypertension, hypertrophy, or exposure to ANTs, and it has also been shown that it can modulate cardiomyocyte proliferation in mammalian hearts.[9,12,56–60] The inhibition of the neuregulin-1/Erbb2 axis weakens the myocardium and makes it vulnerable to myocardial injury. Timolati et al demonstrated a role of neuregulin-1 in the modulation of doxorubicin-induced oxidative damage, with an impact on antioxidant enzymes such as glutathione reductase, suggesting that trastuzumab may act as a modulator of ANT-related toxicity.[23]
Figure 2: Mechanism of Action of Trastuzumab and Pathogenesis of its Cardiotoxicity.
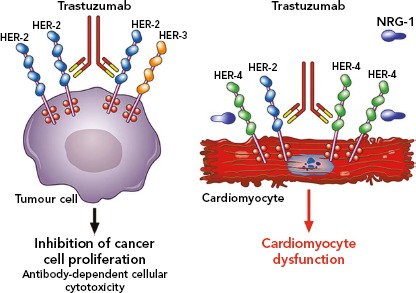
Trastuzumab is a monoclonal antibody that binds the extracellular domain IV of human epidermal growth factor receptor 2 (HER-2). It is used to treat breast cancer patients (~30%) in whom HER-2 is overexpressed and spontaneously homodimerises or forms heterodimers with other HER receptors, especially HER-3. This ligand-independent activation of HER-2 promotes proliferation and survival of tumour cells. Trastuzumab blocks the interaction HER-2/HER-3 and downstream signalling halting the growth of tumour cells. Moreover, trastuzumab induces the antibody-dependent immune cell-mediated cytotoxicity of cancer cells (left side). In the heart, neuregulin-1 (NRG-1) triggers HER-4/HER-4 homodimerisation and HER-4/HER-2 heterodimerisation on cardiomyocytes to induce protective pathways in response to stress. Blockade of cardiac HER-2 by trastuzumab results in the disruption of NRG-1-dependent signaling and consequently in alterations of structure and functions that cause cardiomyocyte death (right side). HER = human epidermal growth factor receptor; NRG = neuregulin. Source: Varricchi et al. 2018[9] Reproduced with permission from Frontiers.
The interactions between ANT and trastuzumab have been extensively studied. The coadministration of trastuzumab with ANTs in people with breast cancer, increased ANT toxicity in early trials and is now avoided.[61–63] In fact, it has now been shown that anti-HER-2 drugs block the protective mechanisms of HER-2, exacerbating the oxidative damage caused by ANTs.[12,64]
ErbB2 knockout mice develop dilated cardiomyopathy and show a higher prevalence of cardiomyocyte death when treated with ANT.[65] On the other hand, Belmonte et al. demonstrated that overexpression of ErbB2 in the heart reduced ROS levels, increasing the activity of glutathione peroxidase 1 and its co-activating factors such as c-Abl and Arg.[66] The same group reported a bidirectional cross-regulation between ErbB2 and beta-adrenergic signalling pathways.[67] Interestingly, patients treated with trastuzumab, ANTs, or both have been shown to be exposed to reduced risk of LV dysfunction when incidentally administered with beta-blockers.[68] Recent data suggest that beta-blockers, such as bisoprolol and metoprolol are not able to fully prevent trastuzumab-induced cardiomyopathy, showing that blockade of beta-1 alone is not sufficient to protect the heart.[69,70] While non-selective beta-blockers did not really prove beneficial in the ANT setting, these clinical and experimental findings support their use in the trastuzumab setting.[67,71]
Anti-vascular Endothelial Growth Factor Drugs
As seen above, ROS play a central role in the mechanisms of CTX induced by ANTs and by ErbB2 blockers. AMPK, which may have a role in ANT-induced cardiotoxicity, seems to be targeted also by the tyrosine kinase inhibitor sunitinib. Indeed, sunitinib is primarily known as a vascular endothelial growth factor (VEGF) inhibitor, but it is also a multiple tyrosine kinase inhibitor. Among many other kinases (>30), it can inhibit ribosomal S6 kinase, activating the intrinsic apoptotic pathway, and AMPK (usually activated by energetic stress), contributing to the reduction of adenosine triphosphate levels.[52,72,73] Our preliminary findings show that CK can also modulate sunitinib actions on the contractile apparatus of cardiomyocytes by regulating oxidative stress.[74,75]
Additionally, it seems that sunitinib can prolong the opening time of the mitochondrial permeability transition pore, with consequent swelling and deformation of the mitochondria in murine cardiomyocytes affected by pressure overload.[76] Conversely, studies have demonstrated that oxidative phosphorylation is not significantly affected by sunitinib and suggest that its CTX is less frequent than predicted.[77]
It has been shown that sunitinib damages pericytes and can affect the microvascular circulation of the heart, rather than impair cardiomyocyte functionality directly, and a recent paper has investigated the connection between afterload and sunitinib-induced CTX.[78,79] Using a preclinical model of engineered cardiomyocytes (first murine and then human), Truitt et al. demonstrated that sunitinib can induce cardiomyocyte death, decrease the contractile force of the heart and generate spontaneous beating at clinical doses. They also found a correlation between an increase in the afterload and the CTX induced by sunitinib. According to these findings, antihypertensive therapies may be used to reduce the effects of sunitinib.[79]
Sorafenib is another tyrosine kinase inhibitor with significant CTX. Most of the information we have on CTX induced by sunitinib and sorafenib comes from two meta-analyses including almost 7,000 patients given sunitinib and 900 patients given sorafenib. These showed that 4.1% of patients treated with sunitinib developed HF, while 1% of patients treated with sorafenib had signs of cardiac dysfunction.[80,81] It is important to highlight that both meta-analyses only included retrospective studies. So far, there are few data derived from prospective studies, although Schmidinger et al. demonstrated that three of 14 patients who had a cardiac event and were administered with sorafenib, developed LV dysfunction assessed by significant reduction of LVEF.[82]
Despite the aforementioned studies, the real incidence of CTX-induced by sorafenib is not yet clear and more studies are needed for this reason. Sorafenib can inhibit at least 15 different kinases, such as VEGFR, PDGFR, Raf-1/B-Raf, FLT3 and c-Kit.[52,83,84] In addition, a 2018 study demonstrated that sorafenib has an intrinsic cardiotoxic effect on cardiomyocytes, impairing calcium homeostasis.[85]
Immunotherapy
Over the past few years, cancer immunotherapies have revolutionised the clinical management of a wide spectrum of solid and haematopoietic malignancies. The forefront of immunotherapy is represented by immune checkpoint inhibitors (ICIs), whose purpose is to inhibit molecules such as cytotoxic-T-lymphocyte-associated antigen 4 (CTLA-4) and of programmed cell death 1 (PD-1) and its ligand PD-L1. CTLA-4, expressed on T cells, competes with CD28 in binding CD80 and/or CD86, expressed on antigen-presenting cells, modulating the amplitude of T-cell activation and showing immunosuppressive activity.[86–88] This results in immunosuppression with downmodulation of T helper cell activity and enhancement of regulatory cells.
PD-1, expressed at low levels on T cells, activated natural killer cells, B cells, monocytes, immature Langerhans’ cells and cardiomyocytes, and its ligand PD-L1, constitutively expressed at low levels on both professional and non-professional antigen-presenting cells as well as on non-haematopoietic cells plays a fundamental role in the maintenance of peripheral tolerance and the prevention of autoimmune diseases.[89] Monoclonal antibodies targeting CTLA-4 (ipilimumab), PD-1 (nivolumab, pembrolizumab), and PD-L1 (atezolizumab, avelumab, durvalumab) block these immune inhibitory checkpoints and restore the antitumour immune response, leading to tumour cell death through the release of cytolytic molecules, such as tumour necrosis factor-alpha, granzyme B and interferon-gamma (Figure 3).[18] However, immune checkpoints play a central role in the maintenance of self-tolerance. Therefore, blocking these pathways can lead to imbalances in immunologic tolerance that results in immune-related adverse events.[90] These side-effects are common, but fortunately in most cases they are reversible and not severe. They include mostly skin manifestations, such as pruritus, rash and vitiligo in 43–45% of patients, but also liver and gastrointestinal events that may occur 6–7 weeks after treatment was initiated. Greater concern is expressed on endocrinopathies, observed in about 6–8% of patients. They are the only immune-related adverse events with a high risk of irreversible toxicity and result from immune infiltration into either the thyroid or pituitary glands, causing thyroiditis or hypophysitis, respectively.[91–93]
Figure 3: Mechanism of Action of Checkpoint Inhibitors.
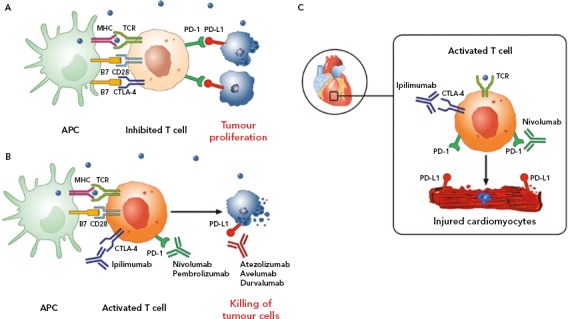
A: Tumour cells escape immune surveillance by promoting checkpoint activation. Tumour cells express the immune checkpoint activator programmed cell death ligand 1 (PD-L1) and produce antigens (blue dots) that are captured by antigen-presenting cells (APCs). These cells present antigens to cytotoxic CD8+ T cells through the interaction of major histocompatibility complex (MHC) molecules and T-cell receptor (TCR). T-cell activation requires costimulatory signals mediated by the interaction between B7 and CD28. Inhibitory signals from cytotoxic T lymphocyte–associated protein 4 (CTLA-4) and programmed cell death protein 1 (PD-1) checkpoints dampen T-cell response and promote tumour proliferation. B: Checkpoint inhibitors stimulate T-cell activation. Monoclonal antibodies targeting CTLA-4 (ipilimumab), PD-1 (nivolumab, pembrolizumab), and PD-L1 (atezolizumab, avelumab, durvalumab) block immune inhibitory checkpoints (CTLA-4, PD-1, and PD-L1, respectively) and restore antitumour immune response, resulting in tumour cell death via release of cytolytic molecules (e.g. tumour necrosis factor-alpha, granzyme B, interferon gamma). C: Hypothetical mechanism by which checkpoint inhibitors can promote autoimmune lymphocytic myocarditis. PD-L1 is expressed in human and murine cardiomyocytes, and its expression can increase during myocardial injury. Combination of checkpoint blockade (ipilimumab plus nivolumab) unleashes immune responses and can cause autoimmune lymphocytic myocarditis. Lymphocytes in myocardium and tumours showed clonality of TCR, suggesting that heart and tumours can share antigens (blue dots) recognised by the same T cell clones. Source: Varricchi et al. 2017[18] Reproduced with permission from Wolters Kluwer Health.
When ICIs were introduced as cancer treatments, little attention was paid to cardiac side-effects. Then, isolated cases of fulminant myocarditis (Figure 3) and other cardiovascular disorders (pericarditis, vasculitis and AV blocks) were reported by several independent groups.[19,94–97] The 2018 study by Mahmood et al. is significantly larger than previous reports.[98] The authors present a retrospective, multicentre review of myocarditis in 35 patients and show that myocarditis presented early, with a median presentation of more than 30 days after starting ICIs, and 81% presenting within 3 months of treatment initiation. This suggests the importance of a surveillance protocol, especially in the initial phases of therapy when it may have the most impact. The same authors showed that serum troponin was abnormal in 94% of the cases, highlighting a possible role in early detection of ICI CTX. Instead, measurement of EF may be less useful for surveillance, because EF with myocarditis was normal in half of the cases. In fact, a preserved EF in not reassuring in ICI myocarditis, unlike other types of myocarditis where a normal EF is traditionally considered relatively benign and self-limiting.[99]
The development of myocarditis in patients treated with ICIs has a solid biological base. In 2001, a seminal paper by Nishimura et al. demonstrated that mice deficient for the CTLA-4 and PD-1 axes presented with autoimmune myocarditis and dilated cardiomyopathy, showing that these molecules can prevent autoimmunity.[100] Furthermore, absence of PD-L1, or its inhibition, can worsen the survival from myocarditis, suggesting a role for PD-1/PD-L1 and CTLA-4 in limitation of T cell–mediated autoimmune myocarditis. Interestingly, PD-1 and PD-L1 were observed to be increased in cardiomyocytes from rat hearts subjected to ischaemia-reperfusion.[100,101]
Future Perspectives
Cardio-oncology is an ever-expanding field of research. In this article we have only discussed the studies conducted on ANTs anti-HER2 drugs and anti-VEGF drugs, but several other drugs (alkylating agents, antimetabolites, proteasome inhibitors, other, tyrosine kinase inhibitors, antimicrotubule agents) can generate LV dysfunction.[17] A tight collaboration among cardiologists and oncologists is building up quickly.[102,103]
Immunotherapies have been introduced more recently, and in view of the fact that autoimmune myocarditis induced by ICIs has fulminant progression, including immunologists in this cardio-oncologic collaboration appears necessary for better management of ICI CTX.[104] At the moment, beyond ICIs, novel monoclonal antibodies targeting several immune checkpoints, and new cancer therapies, such as engineered T cells, cancer vaccines and PI3K inhibitors are being studied and developed.[105–108] A thorough cardio-immuno-oncologic collaboration seems fundamental, to the assessment of potential toxicities of current and novel drugs, in clinical as well as in basic research also considering that these drugs are often combined, thus increasing their cardiotoxic potential.[99,109]
In addition, novel data point to a direct relationship between cancer and the heart. Indeed, cancer and HF share common mechanisms, risk factors and comorbidities, while several studies have suggested that cancer cachexia can trigger cardiac dysfunction, and that cardiovascular health can predict all-cause mortality in cancer patients.[8,110–117] More recently, experimental studies led by Rudolf de Boer have elegantly shown that HF stimulates tumour growth by circulating factors.[118] Investigation of the mechanisms and pathways linking HF to cancer is a novel, but very promising field of research that aims to answer exciting questions of whether HF promotes malignancies.[111]
References
- 1.Suter TM, Ewer MS. Cancer drugs and the heart: importance and management. Eur Heart J. 2013;34:1102–11. doi: 10.1093/eurheartj/ehs181. [DOI] [PubMed] [Google Scholar]
- 2.Zamorano JL, Lancellotti P, Rodriguez Muñoz D et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC. 2016;37:2768–801. doi: 10.1093/eurheartj/ehw211. [DOI] [PubMed] [Google Scholar]
- 3.Armenian SH, Lacchetti C, Barac A et al. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2017;35:893–911. doi: 10.1200/JCO.2016.70.5400. [DOI] [PubMed] [Google Scholar]
- 4.Moslehi JJ. Cardiovascular toxic effects of targeted cancer therapies. N Engl J Med. 2016;375:1457–67. doi: 10.1056/NEJMra1100265. [DOI] [PubMed] [Google Scholar]
- 5.Kenigsberg B, Wellstein A, Barac A. Left ventricular dysfunction in cancer treatment: is it relevant? JACC Heart Fail. 2018;6:87–95. doi: 10.1016/j.jchf.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 6.Guha A, Armanious M, Fradley MG. Update on cardio-oncology: Novel cancer therapeutics and associated cardiotoxicities. Trends Cardiovasc Med. 2018;29:29–39. doi: 10.1016/j.tcm.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Babiker HM, McBride A, Newton M et al. Cardiotoxic effects of chemotherapy: A review of both cytotoxic and molecular targeted oncology therapies and their effect on the cardiovascular system. Crit Rev Oncol Hematol. 2018;126:186–200. doi: 10.1016/j.critrevonc.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Ameri P, Canepa M, Anker MS et al. Cancer diagnosis in patients with heart failure: epidemiology, clinical implications and gaps in knowledge. Eur J Heart Fail. 2018;20:879–87. doi: 10.1002/ejhf.1165. [DOI] [PubMed] [Google Scholar]
- 9.Varricchi G, Ameri P, Cadeddu C et al. Antineoplastic drug-induced cardiotoxicity: a redox perspective. Front Physiol. 2018;9:1–18. doi: 10.3389/fphys.2018.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eschenhagen T, Force T, Ewer MS et al. Cardiovascular side effects of cancer therapies: a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2011;13:1–10. doi: 10.1093/eurjhf/hfq213. [DOI] [PubMed] [Google Scholar]
- 11.Ewer MS, Lenihan DJ. Left ventricular ejection fraction and cardiotoxicity: Is our ear really to the ground? J Clin Oncol. 2008;26:1201–3. doi: 10.1200/JCO.2007.14.8742. [DOI] [PubMed] [Google Scholar]
- 12.Ewer MS, Ewer SM. Troponin I provides insight into cardiotoxicity and the anthracycline-trastuzumab interaction. J Clin Oncol. 2010;28:3901–4. doi: 10.1200/JCO.2010.30.6274. [DOI] [PubMed] [Google Scholar]
- 13.Scott JM, Khakoo A, Mackey JR et al. Modulation of anthracycline-induced cardiotoxicity by aerobic exercise in breast cancer: current evidence and underlying mechanisms. Circulation. 2011;6:2166–71. doi: 10.1161/CIRCULATIONAHA.111.021774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Menna P, Gonzalez Paz O, Chello M et al. Anthracycline cardiotoxicity. Expert Opin Drug Saf. 2012;11:S21–36. doi: 10.1517/14740338.2011.589834. [DOI] [PubMed] [Google Scholar]
- 15.Štĕrba M, Popelová O, Vávrová A et al. Oxidative stress, redox signaling, and metal chelation in anthracycline cardiotoxicity and pharmacological cardioprotection. Antioxid Redox Signal. 2013;18:899–929. doi: 10.1089/ars.2012.4795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mercurio V, Pirozzi F, Lazzarini E et al. Models of heart failure based on the cardiotoxicity of anticancer drugs. J Card Fail. 2016;22:449–58. doi: 10.1016/j.cardfail.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 17.Tocchetti CG, Cadeddu C, Di Lisi D From molecular mechanisms to clinical management of antineoplastic drug-induced cardiovascular toxicity: a translational overview. Antioxid Redox Signal. 2017. epub ahead of press. [DOI] [PMC free article] [PubMed]
- 18.Varricchi G, Galdiero MR, Tocchetti CG. Cardiac toxicity of immune checkpoint inhibitors: cardio-oncology meets immunology. Circulation. 2017;136:1989–92. doi: 10.1161/CIRCULATIONAHA.117.029626. [DOI] [PubMed] [Google Scholar]
- 19.Johnson DB, Balko JM, Compton ML et al. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med. 2016;375:1749–55. doi: 10.1056/NEJMoa1609214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Varricchi G, Marone G, Mercurio V Immune checkpoint inhibitors and cardiac toxicity: an emerging issue. Curr Med Chem. 2017. pp. 1327–39. [DOI] [PubMed]
- 21.Lyon AR, Yousaf N, Battisti NML et al. Immune checkpoint inhibitors and cardiovascular toxicity. Lancet Oncol. 2018;19:e447–58. doi: 10.1016/S1470-2045(18)30457-1. [DOI] [PubMed] [Google Scholar]
- 22.Pentassuglia L, Graf M, Lane H et al. Inhibition of ErbB2 by receptor tyrosine kinase inhibitors causes myofibrillar structural damage without cell death in adult rat cardiomyocytes. Exp Cell Res. 2009;315:1302–12. doi: 10.1016/j.yexcr.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Timolati F, Ott D, Pentassuglia L et al. Neuregulin-1 beta attenuates doxorubicin-induced alterations of excitation-contraction coupling and reduces oxidative stress in adult rat cardiomyocytes. J Mol Cell Cardiol. 2006;41:845–54. doi: 10.1016/j.yexcr.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 24.Ewer MS, Von Hoff DD, Benjamin RS. A historical perspective of anthracycline cardiotoxicity. Heart Fail Clin. 2011;7:363–72. doi: 10.1016/j.hfc.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 25.Rochette L, Guenancia C, Gudjoncik A et al. Anthracyclines/trastuzumab: new aspects of cardiotoxicity and molecular mechanisms. Trends Pharmacol Sci. 2015;36:326–48. doi: 10.1016/j.tips.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 26.Ewer MS, Ewer SM. Cardiotoxicity of anticancer treatments. Nat Rev Cardiol. 2015;12:547–58. doi: 10.1038/nrcardio.2015.65. [DOI] [PubMed] [Google Scholar]
- 27.Lipshultz SE, Lipsitz SR, Mone SM et al. Female sex and higher drug dose as risk factors for late cardiotoxic effects of doxorubicin therapy for childhood cancer. N Engl J Med. 1995;332:1738–44. doi: 10.1056/NEJM199506293322602. [DOI] [PubMed] [Google Scholar]
- 28.Lipshultz PSE, Scully RE, Lipsitz SR et al. Assessment of dexrazoxane as a cardioprotectant in doxorubicin-treated children with high-risk acute lymphoblastic leukaemia: long-term follow-up of a prospective, randomised, multicentre trial. Lancet Oncol. 2010;11:950–61. doi: 10.1016/S1470-2045(10)70204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krischer JP, Epstein S, Cuthbertson DD et al. Clinical cardiotoxicity following anthracycline treatment for childhood cancer: the Pediatric Oncology Group experience. J Clin Oncol. 1997;15:1544–52. doi: 10.1200/JCO.1997.15.4.1544. [DOI] [PubMed] [Google Scholar]
- 30.Ichikawa Y, Ghanefar M, Bayeva M et al. Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation. J Clin Invest. 2014;124:617–30. doi: 10.1172/JCI72931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang S, Liu X, Bawa-Khalfe T et al. Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nat Med. 2012;18:1639–42. doi: 10.1038/nm.2919. [DOI] [PubMed] [Google Scholar]
- 32.Zhu W, Zou Y, Aikawa R et al. MAPK superfamily plays an important role in daunomycin-induced apoptosis of cardiac myocytes. Circulation. 1999;100:2100–7. doi: 10.1161/01.CIR.100.20.2100. [DOI] [PubMed] [Google Scholar]
- 33.Maslov MY, Chacko VP, Hirsch GA et al. Reduced in vivo high-energy phosphates precede adriamycin-induced cardiac dysfunction. Am J Physiol Heart Circ Physiol. 2010;299:H332–7. doi: 10.1152/ajpheart.00727.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gupta A, Akki A, Wang Y et al. Creatine kinase-mediated improvement of function in failing mouse hearts provides causal evidence the failing heart is energy starved. J Clin Invest. 2012;122:291–302. doi: 10.1172/JCI57426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gupta A, Rohlfsen C, Leppo MK et al. Creatine kinase-overexpression improves myocardial energetics, contractile dysfunction and survival in murine doxorubicin cardiotoxicity. PLoS One. 2013;8:1–9. doi: 10.1371/journal.pone.0074675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tokarska-Schlattner M, Zaugg M, da Silva R et al. Acute toxicity of doxorubicin on isolated perfused heart: response of kinases regulating energy supply. Am J Physiol Heart Circ Physiol. 2005;289:H37–47. doi: 10.1152/ajpheart.01057.2004. [DOI] [PubMed] [Google Scholar]
- 37.Cadeddu C, Mercurio V, Spallarossa P et al. Preventing antiblastic drug-related cardiomyopathy. J Cardiovasc Med. 2016;17:e64–75. doi: 10.2459/JCM.0000000000000382. [DOI] [PubMed] [Google Scholar]
- 38.Lipshultz SE, Rifai N, Dalton VM et al. The effect of dexrazoxane on myocardial injury in doxorubicin-treated children with acute lymphoblastic leukemia. N Engl J Med. 2004;351:145–53. doi: 10.1056/NEJMoa035153. [DOI] [PubMed] [Google Scholar]
- 39.Nakamura K, Kusano K, Nakamura Y et al. Carvedilol decreases elevated oxidative stress in human failing myocardium. Circulation. 2002;105:2867–71. doi: 10.1161/01.CIR.0000018605.14470.DD. [DOI] [PubMed] [Google Scholar]
- 40.Asanuma H, Minamino T, Sanada S et al. Beta-adrenoceptor blocker carvedilol provides cardioprotection via an adenosine-dependent mechanism in ischemic canine hearts. Circulation. 2004;109:2773–9. doi: 10.1161/01.CIR.0000130917.12959.04. [DOI] [PubMed] [Google Scholar]
- 41.Matsui H, Morishima I, Numaguchi Y et al. Protective effects of carvedilol against doxorubicin-induced cardiomyopathy in rats. Life Sci. 1999;65:1265–74. doi: 10.1016/S0024-3205(99)00362-8. [DOI] [PubMed] [Google Scholar]
- 42.Spallarossa P, Garibaldi S, Altieri P et al. Carvedilol prevents doxorubicin-induced free radical release and apoptosis in cardiomyocytes in vitro. J Mol Cell Cardiol. 2004;37:837–46. doi: 10.1016/j.yjmcc.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 43.Santos DL, Moreno AJM, Leino RL et al. Carvedilol protects against doxorubicin-induced mitochondrial cardiomyopathy. Toxicol Appl Pharmacol. 2002;185:218–27. doi: 10.1006/taap.2002.9532. [DOI] [PubMed] [Google Scholar]
- 44.de Nigris F, Rienzo M, Schiano C et al. Prominent cardioprotective effects of third generation beta blocker nebivolol against anthracycline-induced cardiotoxicity using the model of isolated perfused rat heart. Eur J Cancer. 2008;44:334–40. doi: 10.1016/j.ejca.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 45.Tocchetti CG, Molinaro M, Angelone T et al. Nitroso-redox balance and modulation of basal myocardial function: an update from the Italian Society of Cardiovascular Research (SIRC) Curr Drug Targets. 2015;16:895–903. doi: 10.2174/1389450116666150304103517. [DOI] [PubMed] [Google Scholar]
- 46.Kaya MG, Ozkan M, Gunebakmaz O et al. Protective effects of nebivolol against anthracycline-induced cardiomyopathy: a randomized control study. Int J Cardiol. 2013;167:2306–10. doi: 10.1016/j.ijcard.2012.06.023. [DOI] [PubMed] [Google Scholar]
- 47.Arnolda L, McGrath B, Cocks M et al. Adriamycin cardiomyopathy in the rabbit: an animal model of low output cardiac failure with activation of vasoconstrictor mechanisms. Cardiovasc Res. 1985;19:378–82. doi: 10.1093/cvr/19.6.378. [DOI] [PubMed] [Google Scholar]
- 48.Cardinale D, Colombo A, Bacchiani G et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131:1981–8. doi: 10.1161/CIRCULATIONAHA.114.013777. [DOI] [PubMed] [Google Scholar]
- 49.Iqbal M, Dubey K, Anwer T et al. Protective effects of telmisartan against acute doxorubicin-induced cardiotoxicity in rats. Pharmacol Rep. 2008;60:382–90. [PubMed] [Google Scholar]
- 50.Yamagishi S, Takeuchi M. Telmisartan is a promising cardiometabolic sartan due to its unique PPAR-gamma-inducing property. Med Hypotheses. 2005;64:476–8. doi: 10.1016/j.mehy.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 51.Bosch X, Rovira M, Sitges M et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (preventiOn of left Ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of Malignant hEmopathies) J Am Coll Cardiol. 2013;61:2355–62. doi: 10.1016/j.jacc.2013.02.072. [DOI] [PubMed] [Google Scholar]
- 52.Force T, Krause DS, Van Etten RA. Molecular mechanisms of cardiotoxicity of tyrosine kinase inhibition. Nat Rev Cancer. 2007;7:332–44. doi: 10.1038/nrc2106. [DOI] [PubMed] [Google Scholar]
- 53.Balduzzi S, Mantarro S, Guarneri V et al. Trastuzumab-containing regimens for metastatic breast cancer. Cochrane Database Syst Rev. 2014;6:CD006242. doi: 10.1002/14651858.CD006242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tocchetti CG, Ragone G, Coppola C et al. Detection, monitoring, and management of trastuzumab-induced left ventricular dysfunction: an actual challenge. Eur J Heart Fail. 2012;14:130–7. doi: 10.1093/eurjhf/hfr165. [DOI] [PubMed] [Google Scholar]
- 55.Lynce F, Barac A, Tan MT et al. SAFE-HEaRt: Rationale and design of a pilot study investigating cardiac safety of HER2 targeted therapy in patients with HER2-positive breast cancer and reduced left ventricular function. Oncologist. 2017;22:518–25. doi: 10.1634/theoncologist.2016-0412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lim SL, Lam CSP, Segers VFM et al. Cardiac endothelium-myocyte interaction: clinical opportunities for new heart failure therapies regardless of ejection fraction. Eur Heart J. 2015;36:205–60. doi: 10.1093/eurheartj/ehv132. [DOI] [PubMed] [Google Scholar]
- 57.Odiete O, Hill MF, Sawyer DB. Neuregulin in cardiovascular development and disease. Circ Res. 2012;111:1376–85. doi: 10.1161/CIRCRESAHA.112.267286.Neuregulin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.de Korte MA, de Vries EGE, Lub-de Hooge MN et al. 111Indium-trastuzumab visualises myocardial human epidermal growth factor receptor 2 expression shortly after anthracycline treatment but not during heart failure: a clue to uncover the mechanisms of trastuzumab-related cardiotoxicity. Eur J Cancer. 2007;43:2046–51. doi: 10.1016/j.ejca.2007.06.024. [DOI] [PubMed] [Google Scholar]
- 59.Gabrielson K, Bedja D, Pin S et al. Heat shock protein 90 and ErbB2 in the cardiac response to doxorubicin injury. Cancer Res. 2007;67:1436–41. doi: 10.1158/0008-5472.CAN-06-3721. [DOI] [PubMed] [Google Scholar]
- 60.D’Uva G, Aharonov A, Lauriola M et al. ERBB2 triggers mammalian heart regeneration by promoting cardiomyocyte dedifferentiation and proliferation. Nat Cell Biol. 2015;17:627–8. doi: 10.1038/ncb3149. [DOI] [PubMed] [Google Scholar]
- 61.Seidman A, Hudis C, Pierri MK et al. Cardiac dysfunction in the trastuzumab clinical trials experience. J Clin Oncol. 2002;20:1215–21. doi: 10.1200/JCO.2002.20.5.1215. [DOI] [PubMed] [Google Scholar]
- 62.Ewer MS, Ewer SM. Cardiotoxicity of anticancer treatments: what the cardiologist needs to know. Nat Rev Cardiol. 2010;7:564–75. doi: 10.1038/nrcardio.2010.121. [DOI] [PubMed] [Google Scholar]
- 63.Suter TM, Procter M, van Veldhuisen DJ et al. Trastuzumab-associated cardiac adverse effects in the herceptin adjuvant trial. J Clin Oncol. 2007;25:3859–65. doi: 10.1200/JCO.2006.09.1611. [DOI] [PubMed] [Google Scholar]
- 64.Sawyer DB, Zuppinger C, Miller TA et al. Modulation of anthracycline-induced myofibrillar disarray in rat ventricular myocytes by neuregulin-1beta and anti-erbB2: potential mechanism for trastuzumab-induced cardiotoxicity. Circulation. 2002;105:1551–4. doi: 10.1161/01.CIR.0000013839.41224.1C. [DOI] [PubMed] [Google Scholar]
- 65.Crone SA, Zhao YY, Fan L et al. ErbB2 is essential in the prevention of dilated cardiomyopathy. Nat Med. 2002;8:459–65. doi: 10.1038/nm0502-459. [DOI] [PubMed] [Google Scholar]
- 66.Belmonte F, Das S, Sysa-Shah P et al. ErbB2 overexpression upregulates antioxidant enzymes, reduces basal levels of reactive oxygen species, and protects against doxorubicin cardiotoxicity. Am J Physiol Heart Circ Physiol. 2015;309:H1271–80. doi: 10.1152/ajpheart.00517.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sysa-Shah P, Tocchetti CG, Gupta M et al. Bidirectional cross-regulation between ErbB2 and β-adrenergic signalling pathways. Cardiovasc Res. 2016;109:358–73. doi: 10.1093/cvr/cvv274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Seicean S, Seicean A, Alan N et al. Cardioprotective effect of β-adrenoceptor blockade in patients with breast cancer undergoing chemotherapy follow-up study of heart failure. Circ Hear Fail. 2013;6:420–6. doi: 10.1161/CIRCHEARTFAILURE.112.000055. [DOI] [PubMed] [Google Scholar]
- 69.Pituskin E, Mackey JR, Koshman S et al. Multidisciplinary approach to novel therapies in cardio-oncology research (MANTICORE 101-Breast): A randomized trial for the prevention of trastuzumab-associated cardiotoxicity. J Clin Oncol. 2017;35:870–7. doi: 10.1200/JCO.2016.68.7830. [DOI] [PubMed] [Google Scholar]
- 70.Gulati G, Heck SL, Ree AH et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 x 2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. Eur Heart J. 2016;37:1671–80. doi: 10.1093/eurheartj/ehw022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Avila MS, Ayub-Ferreira SM, de Barros Wanderley Junior MR et al. Carvedilol for prevention of chemotherapy related cardiotoxicity. J Am Coll Cardiol. 2018;71:2281–90. doi: 10.1016/j.jacc.2018.02.049. [DOI] [PubMed] [Google Scholar]
- 72.Kerkela R, Woulfe KC, Durand JB et al. Sunitinib-induced cardiotoxicity is mediated by off-target inhibition of AMP-activated protein kinase. Clin Transl Sci. 2009;2:15–25. doi: 10.1111/j.1752-8062.2008.00090.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hasinoff BB, Patel D. The lack of target specificity of small molecule anticancer kinase inhibitors is correlated with their ability to damage myocytes in vitro. Toxicol Appl Pharmacol. 2010;249:132–9. doi: 10.1016/j.taap.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 74.Tocchetti CG, Leppo MK, Bedja D et al. Cardiac overexpression of creatine kinase improves cardiomyocytes function in heart failure and during increased redox stress. Circ Res. 2015;117:A338. [Google Scholar]
- 75.Rainer PP, Doleschal B, Kirk JA et al. Sunitinib causes dose-dependent negative functional effects on myocardium and cardiomyocytes. BJU Int. 2012;110:1455–62. doi: 10.1111/j.1464-410X.2012.11134.x. [DOI] [PubMed] [Google Scholar]
- 76.Chu TF, Rupnick MA, Kerkela R et al. Cardiotoxicity associated with the tyrosine kinase inhibitor sunitinib. Lancet. 2007;370:2011–19. doi: 10.1016/S0140-6736(07)61865-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Will Y, Dykens JA, Nadanaciva S et al. Effect of the multitargeted tyrosine kinase inhibitors imatinib, dasatinib, sunitinib, and sorafenib on mitochondrial function in isolated rat heart mitochondria and H9c2 cells. Toxicol Sci. 2008;106:153–61. doi: 10.1093/toxsci/kfn157. [DOI] [PubMed] [Google Scholar]
- 78.Chintalgattu V, Rees ML, Culver JC et al. Coronary microvascular pericytes are the cellular target of sunitinib malate-induced cardiotoxicity. Sci Transl Med. 2013;5:187ra69. doi: 10.1126/scitranslmed.3005066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Truitt R, Mu A, Corbin EA et al. Increased afterload augments sunitinib-induced cardiotoxicity in an engineered cardiac microtissue model. JACC Basic Transl Sci. 2018;3:265–76. doi: 10.1016/j.jacbts.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Richards CJ, Je Y, Schutz FAB et al. Incidence and risk of congestive heart failure in patients with renal and nonrenal cell carcinoma treated with sunitinib. J Clin Oncol. 2011;29:3450–6. doi: 10.1200/JCO.2010.34.4309. [DOI] [PubMed] [Google Scholar]
- 81.Di Lorenzo G, Autorino R, Bruni G et al. Cardiovascular toxicity following sunitinib therapy in metastatic renal cell carcinoma: a multicenter analysis. Ann Oncol. 2009;20:1535–42. doi: 10.1093/annonc/mdp025. [DOI] [PubMed] [Google Scholar]
- 82.Schmidinger M, Zielinski CC, Vogl UM et al. Cardiac toxicity of sunitinib and sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol. 2008;26:5204–12. doi: 10.1200/JCO.2007.15.6331. [DOI] [PubMed] [Google Scholar]
- 83.Cheng H, Force T. Molecular mechanisms of cardiovascular toxicity of targeted cancer therapeutics. Circ Res. 2010;106:21–4. doi: 10.1161/CIRCRESAHA.109.206920. [DOI] [PubMed] [Google Scholar]
- 84.Tocchetti CG, Gallucci G, Coppola C et al. The emerging issue of cardiac dysfunction induced by antineoplastic angiogenesis inhibitors. Eur J Heart Fail. 2013;15:482–9. doi: 10.1093/eurjhf/hft008. [DOI] [PubMed] [Google Scholar]
- 85.Schneider C, Wallner M, Kolesnik E et al. The anti-cancer multikinase inhibitor sorafenib impairs cardiac contractility by reducing phospholamban phosphorylation and sarcoplasmic calcium transients. Sci Rep. 2018;8:1–8. doi: 10.1038/s41598-018-23630-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Freeman GJ, Gribben JG, Boussiotis VA et al. Cloning of B7-2: a CTLA-4 counter-receptor that costimulates human T cell proliferation. Science. 1993;262909 doi: 10.1126/science.7694363. [DOI] [PubMed] [Google Scholar]
- 87.Hathcock KS, Laszlo G, Dickler HB et al. Identification of an alternative CTLA-4 ligand costimulatory for T cell activation. Science. 1993;262:905–7. doi: 10.1126/science.7694361. [DOI] [PubMed] [Google Scholar]
- 88.Linsley PS, Clark EA, Ledbetter JA. T-cell antigen CD28 mediates adhesion with B cells by interacting with activation antigen B7/BB-1. Proc Natl Acad Sci USA. 1990;87:5031–5. doi: 10.1073/pnas.87.13.5031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dong H, Strome SE, Salomao DR et al. Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat Med. 2002;8:793–800. doi: 10.1038/nm730. [DOI] [PubMed] [Google Scholar]
- 90.Boutros C, Tarhini A, Routier E et al. Safety profiles of anti-CTLA-4 and anti-PD-1 antibodies alone and in combination. Nat Rev Clin Oncol. 2016;13:473–86. doi: 10.1038/nrclinonc.2016.58. [DOI] [PubMed] [Google Scholar]
- 91.Corsello SM, Barnabei A, Marchetti P et al. Endocrine side effects induced by immune checkpoint inhibitors. J Clin Endocrinol Metab. 2013;98:1361–75. doi: 10.1210/jc.2012-4075. [DOI] [PubMed] [Google Scholar]
- 92.Lacouture ME, Wolchok JD, Yosipovitch G et al. Ipilimumab in patients with cancer and the management of dermatologic adverse events. J Am Acad Dermatol. 2014;71:161–9. doi: 10.1016/j.jaad.2014.02.035. [DOI] [PubMed] [Google Scholar]
- 93.Weber JS, Kahler KC, Hauschild A. Management of immune-related adverse events and kinetics of response with ipilimumab. J Clin Oncol. 2012;30:2691–7. doi: 10.1200/JCO.2012.41.6750. [DOI] [PubMed] [Google Scholar]
- 94.Menzies AM, Johnson DB, Ramanujam S et al. Anti-PD-1 therapy in patients with advanced melanoma and preexisting autoimmune disorders or major toxicity with ipilimumab. Ann Oncol. 2017;28:368–76. doi: 10.1093/annonc/mdw443. [DOI] [PubMed] [Google Scholar]
- 95.Escudier M, Cautela J, Malissen N et al. Clinical features, management, and outcomes of immune checkpoint inhibitor-related cardiotoxicity. Circulation. 2017;136:2085–7. doi: 10.1161/CIRCULATIONAHA.117.030571. [DOI] [PubMed] [Google Scholar]
- 96.Heinzerling L, Ott PA, Hodi FS et al. Cardiotoxicity associated with CTLA4 and PD1 blocking immunotherapy. J Immunother Cancer. 2016;4:50. doi: 10.1186/s40425-016-0152-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Spallarossa P, Meliota G, Brunelli C et al. Potential cardiac risk of immune-checkpoint blockade as anticancer treatment: what we know, what we do not know, and what we can do to prevent adverse effects. Med Res Rev. 2018;38:1447–68. doi: 10.1002/med.21478. [DOI] [PubMed] [Google Scholar]
- 98.Mahmood S, Fradley MG, Cohen JV et al. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol. 2018;71:A699. doi: 10.1016/S0735-1097(18)31240-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tocchetti CG, Galdiero MR, Varricchi G. Cardiac Toxicity in patients treated with immune checkpoint inhibitors: it is now time for cardio-immuno-oncology. J Am Coll Cardiol. 2018;71:1765–7. doi: 10.1016/j.jacc.2018.02.038. [DOI] [PubMed] [Google Scholar]
- 100.Nishimura H, Okazaki T, Tanaka Y et al. Autoimmune dilated cardiomyopathy in PD-1 receptor-deficient mice. Science. 2001;291:319–22. doi: 10.1126/science.291.5502.319. [DOI] [PubMed] [Google Scholar]
- 101.Love VA, Grabie N, Duramad P et al. CTLA-4 ablation and interleukin-12 driven differentiation synergistically augment cardiac pathogenicity of cytotoxic T lymphocytes. Circ Res. 2007;101:248–57. doi: 10.1161/CIRCRESAHA.106.147124. [DOI] [PubMed] [Google Scholar]
- 102.Pareek N, Cevallos J, Moliner P et al. Activity and outcomes of a cardio-oncology service in the United Kingdom – a five-year experience. Eur J Heart Fail. 2018;20:1721–31. doi: 10.1002/ejhf.1292. [DOI] [PubMed] [Google Scholar]
- 103.Lancellotti P, Suter TM, López-Fernández T Cardio-oncology services: rationale, organization, and implementation. Eur Heart J. 2018. epub ahead of press. [DOI] [PubMed]
- 104.Wang DY, Salem JE, Cohen JV et al. Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol. 2018;4:1721–8. doi: 10.1001/jamaoncol.2018.3923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Brudno JN, Kochenderfer JN. Chimeric antigen receptor T-cell therapies for lymphoma. Nat Rev Clin Oncol. 2018;15:31–46. doi: 10.1182/blood-2017-06-793869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.De Henau O, Rausch M, Winkler D et al. Overcoming resistance to checkpoint blockade therapy by targeting pi3k-γ in myeloid cells. Nature. 2016;539:443–7. doi: 10.1038/nature20554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Li M, Sala V, De Santis MC et al. Phosphoinositide 3-kinase gamma inhibition protects from anthracycline cardiotoxicity and reduces tumor growth. Circulation. 2018;138:696–711. doi: 10.1161/CIRCULATIONAHA.117.030352. [DOI] [PubMed] [Google Scholar]
- 108.Kaneda MM, Messer KS, Ralainirina N et al. PI3Kγ 3 is a molecular switch that controls immune suppression. Nature. 2016;539:437–42. doi: 10.1038/nature19834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sharma A, Burridge PW, McKeithan WL et al. High-throughput screening of tyrosine kinase inhibitor cardiotoxicity with human induced pluripotent stem cells. Sci Transl Med. 2017;9:eaaf2584. doi: 10.1126/scitranslmed.aaf2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Anker MS, von Haehling S, Landmesser U et al. Cancer and heart failure-more than meets the eye: common risk factors and co-morbidities. Eur J Heart Fail. 2018;20:1382–4. doi: 10.1002/ejhf.1252. [DOI] [PubMed] [Google Scholar]
- 111.Bertero E, Canepa M, Maack C, Ameri P. Linking heart failure to cancer. Circulation. 2018;138:735–42. doi: 10.1161/CIRCULATIONAHA.118.033603. [DOI] [PubMed] [Google Scholar]
- 112.Schafer M, Oeing CU, Rohm M et al. Ataxin-10 is part of a cachexokine cocktail triggering cardiac metabolic dysfunction in cancer cachexia. Mol Metab. 2016;5:67–78. doi: 10.1016/j.molmet.2015.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Barkhudaryan A, Scherbakov N, Springer J, Doehner W. Cardiac muscle wasting in individuals with cancer cachexia. ESC Heart Fail. 2017;4:458–67. doi: 10.1002/ehf2.12184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Loncar G, Springer J, Anker M et al. Cardiac cachexia: hic et nunc. J Cachexia Sarcopenia Muscle. 2016;7:246–60. doi: 10.1002/jcsm.12118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Pavo N, Raderer M, Hulsmann M et al. Cardiovascular biomarkers in patients with cancer and their association with all-cause mortality. Heart. 2015;101:1874–80. doi: 10.1136/heartjnl-2015-307848. [DOI] [PubMed] [Google Scholar]
- 116.Anker MS, Ebner N, Hildebrandt B et al. Resting heart rate is an independent predictor of death in patients with colorectal, pancreatic, and non-small cell lung cancer: results of a prospective cardiovascular long-term study. Eur J Heart Fail. 2016;18:1524–34. doi: 10.1002/ejhf.670. [DOI] [PubMed] [Google Scholar]
- 117.Cramer L, Hildebrandt B, Kung T et al. Cardiovascular function and predictors of exercise capacity in patients with colorectal cancer. J Am Coll Cardiol. 2014;64:1310–9. doi: 10.1016/j.jacc.2014.07.948. [DOI] [PubMed] [Google Scholar]
- 118.Meijers WC, Maglione M, Bakker SJ et al. Heart failure stimulates tumor growth by circulating factors. Circulation. 2018;138:678–91. doi: 10.1161/CIRCULATIONAHA.117.030816. [DOI] [PubMed] [Google Scholar]


