Abstract
Objectives
Seizure burden is typically measured by seizure frequency yet it entails more than seizure counts, especially for people with severe epilepsies and their caregivers. We aimed to characterize the multi‐faceted nature of seizure burden in young people and their parents who are living with severe early‐life epilepsies.
Methods
A one‐day workshop and a series of teleconferences were held with parents of children with severe, refractory epilepsy of early‐life origin and providers for children with epilepsy. The workshop sessions were structured as focus groups and aimed to identify components of seizure burden and their impact from the perspective of parents and providers. Data were gathered, organized, and refined during the workshop using an iterative 4‐step process that drew upon grounded theory.
Results
Three primary components of seizure burden were identified: frequency, severity, and unpredictability, which was as important if not more important at times than frequency and severity. Caregivers noted that the impacts of seizures were experienced as acute‐immediate consequences, longer‐term consequences, and as chronic effects that develop and evolve over time. The severity of the child's neurological and medical status as well as where in the disease journey a family was represented additional contextual factors that influenced the experience of seizure burden.
Significance
Patient‐reported and patient‐centered outcomes are increasingly incorporated into the evaluation of treatment effectiveness. Without understanding how the disease creates burden for the patient (or family), it is difficult to know how to assess the impact of treatment. Our preliminary findings indicate seizure burden is a complex construct and unpredictability can be as important as frequency and severity.
Keywords: caregiver, family impact, social isolation, stress
Key Points.
Beyond seizure frequency and severity, unpredictability is an equally important contributor to seizure burden
Unpredictability creates a 24‐7‐52 constant state of impending or actual crisis
The severity of the child's neurological and medical status influences perceptions of seizure burden
Stage in the disease course, from initial shock to desolation over the lifelong severe condition, influences perception of seizure burden
Parents perceive the long‐term effects as a type of chronic traumatic stress disorder
1. INTRODUCTION
Epilepsy is a large group of disorders characterized by “an enduring predisposition of the brain to generate seizures and by the neurobiological, cognitive, social, and other consequences of the disorder.1” Seizure frequency, the most commonly monitored aspect of disease state by physicians, is an often used marker of epilepsy (disease) severity and treatment success. In fact, it is the basis of the popular Engel classification of seizure outcomes used for surgery and the derivative ILAE seizure outcome classification.2 Seizures are the target of epilepsy therapies, and for most purposes, seizure frequency appears to be an adequate outcome measure. In severe early‐life developmental epilepsies, however, many if not most patients fall in the most severe end of any globally utilized measure of seizure outcome. Thus, current measures cannot reflect the inherent variability that exists within this most severe range. Yet, variations within this severe range could have profound impacts on the quality of life of the patient and the family. With the increased focus on drug development for these rare early‐life disorders, it is all the more imperative to understand the natural history and outcomes of a disease.3 Identifying the domains that may become the primary or secondary targets of therapeutic interventions and developing outcome measures for these domains that are responsive to meaningful change is essential for the new wave of therapies being developed for these serious and rare neurodevelopmental disorders.
A model of those aspects of seizure burden that affect children with epilepsy and their parents, particularly those with severe epilepsies, could provide insights into (a) means of alleviating those burdens and (b) ways to measure treatment effects beyond “simple” seizure frequency. To gain insight into this extreme end of the seizure spectrum, we gathered input from parents of children who have severe early‐life epilepsies (ELE) and pediatric epileptologists about seizure burden.
2. METHODS
The project goal was to identify the qualities of seizures that create burdens and the ways in which they do so. Qualitative data were gathered during a one‐day workshop held June 20, 2018 and followed by a series of telephone group discussions. To ensure at least 8‐10 parent participated, we invited 20 parents, representing different types of ELE, known to us either through parent voluntary organizations or as parents of patients at our hospital. We specifically invited parents whose children had poorly controlled seizures. The workshop was moderated by a pediatric epilepsy researcher with over 30 years of experience and assisted by a co‐moderator/note taker. Additionally, an experienced qualitative methodologist attended and assisted with oversite of the group discussion. The workshop was structured like a focus group,4 beginning with introductions, an icebreaker activity, and moving into a full group discussion led by the moderator about the different concepts associated with the term “seizure burden.” The discussion was opened with the question “What is seizure burden?” Participants were encouraged to consider all aspects that came to mind. Our data analysis approach drew upon grounded theory in that data collection and analysis were simultaneous and concepts were derived from the data without relying on preexisting frameworks.5 We identified key themes through an iterative four‐step process. First, during the discussion, all concepts were recorded on a large whiteboard and organized by preliminary themes (similar to open coding in grounded theory). Next, participants reviewed the results, added further comments, and reorganized the notes to reflect their views of how the concepts grouped into themes. Third, breakout group sessions addressed individual themes identified during the previous stage and expanded upon them. Fourth, the group used input from the breakout sessions to further refine and organize the concepts. In this way, the workshop participants provided data and assisted with interpretation and organization of the data, and provided additional data to refine findings. This process is akin to a grounded theory approach to data collection and analysis with an emphasis on the co‐construction of data and findings by the study participants and the research team.6, 7
Following the meeting, the study team developed a model of seizure burden based on the themes and the discussions that occurred at the meeting. All workshop participants were sent the results. Three conference calls were held at different times to accommodate participants who wished to discuss the findings. Revisions were made based on discussions that occurred during calls and written comments made to drafts of the manuscript that was circulated. These revisions were sent out again for further comments and clarifications. Thus, the postworkshop telephone calls and emails served as “member checks,” which allowed participants to comment on the validity of our findings.8
3. RESULTS
Ten parents of children with ELE and three pediatric epileptologists participated in the workshop. Six parents and two pediatric epileptologists participated in the phone calls after. The results of the discussion are summarized under the following headings: (a) the domains of seizure burden; (b) the ways in which seizures create burdens; and (c) modulating and contextual factors. The participating physicians primarily facilitated conversations by asking more detailed questions and providing information to help parents elaborate on and articulate difficult concepts. Consequently, this summary focuses on the parents’ comments.
3.1. “Domains of Seizure Burden”
The “burden” created by seizures fell into three distinct domains: frequency, severity, and unpredictability.
3.1.1. Frequency
Participants generally agreed that any reduction in seizure number is a positive outcome. The degree of burden created by frequent seizures, however, is very dependent on seizure severity with less severe but frequent seizures often causing less burden than relatively infrequent but very severe seizures. One parent said that her child could have dozens of very brief tonic seizures and she could deal with that, but it was the big convulsive seizures and risk of arrested breathing that had a much greater impact on everyone. At the same time, parents discussed how frequent absence or myoclonic seizures (less severe) are important and referred to them as “little seizures with big consequences,” particularly for cognitive function. Thus, seizure frequency needs to be considered in the context of a child who has multiple seizures types and related to the consequences of each type. While therapies that reduce seizure frequency are desirable, participants identified factors that offset benefits of reduction or elimination of seizures. These included potential side effects and interactions with other therapies. The costs, additional and hassles in obtaining or administering a medication were other considerations. Somewhat paradoxically, a few parents mentioned that periods of best seizure control may also be when behavioral problems seem worse.
3.1.2. Severity
Participants identified several key aspects of severity, including motor manifestations (ie, convulsive), duration, respiratory/cardiac compromise during or after a seizure (and risk of SUDEP), and postictal impairment and sleepiness. Injuries due to a seizure were also incorporated into the concept of seizure severity. These could be injuries to the child or to the parent. The effects of rescue medications in response to a seizure, however, were also incorporated into the concept of severity. It was often difficult to separate the two.
3.1.3. Unpredictability
Seizures were described as random events. This results in parents spending large amounts of time and energy in‐between seizures anticipating when a seizure might happen and taking steps to avoid the consequences of seizures. As a result, their world consists of a “24‐7‐52” pending crisis. Plans change at a second's notice or plans are not made in the first place in anticipation of an inevitable crisis. “You think you are making it out the door to school and then, bam! You're in the emergency department.” As a case in point, one parent emailed after missing a call to discuss this manuscript to explain that she and her child had been in the emergency department all night and things had not yet settled down.
Parents suggested that one measure of the impact of unpredictability would be to ask, “How much you have your cancelled reservations (trips, etc.) cost you in the past year?” Many of the other topics discussed by the group were directly or indirectly due to the unpredictability.
3.2. Types of burdens created by seizures
Distinct although inter‐related seizure burdens emerged from the discussions (Table 1, Figure 1).
Table 1.
Themes and specific examples of the burdens created by seizures
| General theme | Examples |
|---|---|
| Immediate consequences of a seizure | Death/SUDEP Need for rescue medications; Trips to the emergency department; Hospital admission; Injuries to the child |
| Effects on the child of seizures and seizure medications | Developmental and intellectual delays; Regression in skills following a seizure; Small seizures can have a big impact; Medication side effects on appetite; Sleepiness from seizures and seizure medications; Illness susceptibility after seizures (pneumonia); Effects of seizures and of treatment on behavior; Effects of comorbidities difficult to sort out from effects of behavior |
| Educating others to provide appropriate care for child | Always quarterbacking; Hard to leave child with others who cannot provide adequate care; Trusting other you don't know; Educating providers, EMT, ED, others |
| Time to manage medical care and related tasks | Cleaning up after a seizure; Managing all the prescriptions, memorizing the medication schedules; Making appointments, calling pharmacies; Taking child to multiple appointments; Time at doctors’ offices and laboratories; Keeping track of everything (seizure counts…); Struggling with insurance companies and advocating for what child needs |
| Medical decisions that parents need to make. | What are the next steps? Making the best decision with limited or no information; Making a tough decision when risks are associated with any choice; Having to make tough decisions about surgery; Diet, and alternative therapies; Balancing quality of life versus seizure control; Chronic negotiations concerning challenging parenting decisions |
| Impact on the child's quality of life | How much does the child understand? Mental health of the affected child Inability to partake in age‐appropriate activities; Missing activities and school because of seizures or appointments; Isolation of the child from typical peers |
| Impact on siblings | Social reaction of others to seizures rubs off on other siblings; Child's seizures and other needs take away from time spent with other children in the family; Abandonment; Emotional support; Mental health depression; Sibs take on responsibility, grow up too fast. |
| Impact on family | Missing out on family functions (weddings, etc.); Adverse effects on immediate and extended family dynamics; Isolation from others emotionally and socially; Having extra people in the house to help with child (eg, nurses) alters family life |
| Impact on caregiver | Injuries to caregiver as a result of seizures, lifting, or aggressive behaviors; Guilt because of sacrifices other family members have to make, for not preventing more seizures, for never doing enough, for having missed something; Fear that child would die and fear that child would outlive parent; Grieving for what might have been; Health of the caregiver, no time for self‐care; No outlets; Emotional/psychological stress, PTSD; Caregiver isolation, loneliness, decreased sociability; Not free to do as pleases (constrained); Sleep deprivation, brain fog; Stress on marriage, high divorce rate; Lack of support from others and isolation from (family, friends) |
| 24‐7‐52 | Constant fear and anxiety waiting for the next seizure; Fear of SUDEP; Constantly on high alert, can never be off duty; Tracking child nonstop; Nonstop care needed everyday; Always having to be prepared, multiple contingency plans; Tracking seizures and identifying seizure patterns; Exhaustion; Hard to plan life |
| Future | Identifying educational expectations; Fear of the unknown; Transition and guardianship; Legal concerns with financial planning; What happens when I'm gone? DNR (Do Not Recussitate) decisions |
| Financial | Financial strain due to high cost of care, including hospitalizations; Lack of resources for immediate care during challenging times; Missed work due to child's seizures; Missed career opportunities |
| Social reactions of others | Reactions of others to child having seizures or child's behavior; School‐aged peers’ ability to cope with watching a friend have seizures; Fear of child by others; Social impact of having a seizure around friends or strangers; Neighbors woken up in night by ambulance |
Figure 1.
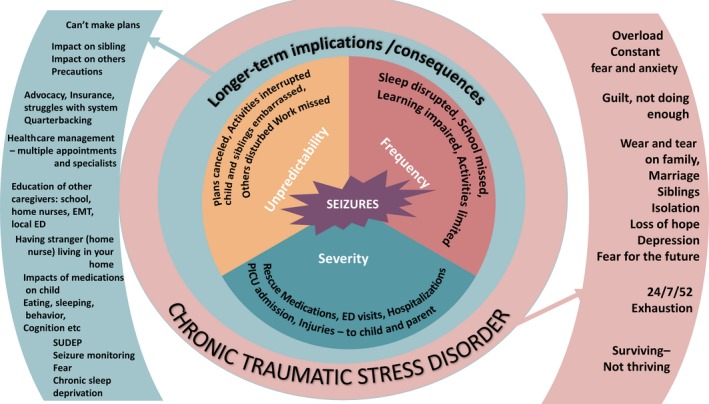
The concept of seizure burden ranges from the initial seizure to the eventual impact on caregivers and family for whom the fabric of their lives and their well‐being is altered
Immediate effects on the child, the parents, and other family members included the seizure itself, the rescue treatments, injuries, emergency services, the interruption of activities as well as the immediate aftermath such as the postictal and medication effects, cleaning up, apologizing to others, and the feeling of being traumatized.
Beyond the immediate, parents discussed burdens associated with management of medical (including home) care, the many medical and therapy appointments, and educating others who might provide care for the child such as home and school nurses, emergency medical personnel and emergency department staff, and navigating the insurance system. Seizures and medications were noted to have cumulative negative effects on the child, interrupted sleep for child and caregivers, and interrupted plans for everyone in the family. Fear of SUDEP (sudden unexpected death in epilepsy) was an ever‐present concern.
On a more pervasive level, because of seizures and their unpredictability, parent said they function in crisis mode throughout every day, 24‐7‐52. Over time, this leads to burnout from the physical and emotional burdens as well as sheer exhaustion when parents attempt to obtain what their children need with state agencies, insurance companies, hospitals, physicians, schools, and others. Parents referred to feelings of demoralization and hopelessness. As one parent notes, “What do you do when your soul is so broken?” The term “chronic traumatic stress disorders” was considered.
This chronic fatigue may present as anger or indifference and influences how parents are perceived by others, although parents often seemed past the point of caring what others thought. Reactions of others to the child having a seizure or having an age‐inappropriate outburst in public were discussed but were not of central importance.
To compound matters, a consequence of the frequent and unpredictable seizures is a withdrawal from family and social life. Parents must cancel plans or never make them as it becomes increasingly difficult to make plans or travel with the frequent, severe seizures and necessary medical and other appointments for the child. This leads to growing isolation and limited emotional outlets and support. The emotional toll extended to the health of marriages; parents pointed to high divorce rates. The impact also extended to siblings who “grew up too fast” were “shipped off to a friend's house during hospitalizations” and had to accept a certain level of “abandonment” as the parents’ attention and energies were focused on the ill sibling. Many parents also talked about the impact their children's condition had on the parents’ ability to take care of their own physical and mental health.
Financial consequences were also extremely important. Parents described having to stop work, reducing to part‐time work, or missing career opportunities to take care of their child. The severity of the seizures and underlying conditions also place constraints on where families can live (near a medical center), the types of homes they can have (stairs are a problem), and the type of cars they can have (vans suitable for wheelchair transport are needed for some).
3.3. Modulating and contextual factors
Other considerations modified the ways in which seizures affected an individual and the relative importance of these different aspects of burden.
3.3.1. The seizure rhythm
On a day‐to‐day basis, parents described a pattern that oscillates between acute crises when seizures occur, an aftermath, and the interseizure time. During the interseizure period, the rest of life has to go on but may be abruptly interrupted with no warning by the next seizure (Figure 2). Given the unpredictability of seizures, the interseizure time is hard to plan. This consideration was particularly salient for parents of children with severe seizures. Frequent severe seizures are overwhelming; but even infrequent severe seizures can create perpetual stress as there is constant dread of the next seizure; precautions are always in place for when the reprieve ends, which it inevitably does.
Figure 2.

The seizure rhythm may oscillate within a day, a week, or over the course of longer periods of time. Activities of life are interrupted by the seizure and cannot return to “normal” until the aftermath has passed
3.3.2. Severity of the child's condition
Those affected by severe early‐life epilepsy have a range of functional abilities and include children who are delayed but are still independently mobile, able to communicate to some degree, and able to use their hands for adaptive purposes. At the other end of the spectrum are children who are unable to move about independently, have little or no functional communication, and may not even be able to recognize their parents. “It really sucks that my child doesn't know who I am.” Medical fragility is a component of the severity of the child's condition. The concerns surrounding survival of the child beyond the parents’ life, the decisions surrounding DNR (Do Not Recussitate) orders, and the weighing of seizure control at all costs over quality of life were important considerations for individual parents based on their children's situation. One parent expressed, “We prioritize quality of life over quantity of life… some outcomes are worse than death.”
For some parents, their children's ability to participate in simple activities with other typical peers was important (eg, eating birthday cake, having sleepovers), whereas other parents, whose children were severely disabled, did not feel this was a priority for them. One parent expressed frustration that the occupational therapist was still trying to teach the child sign language even though the child is profoundly impaired and does not recognize the parents. This was a highly personal perspective, and generalizations would obscure the myriad considerations influencing how these factors might be prioritized.
3.3.3. Stage in the disease journey
Reactions and priorities varied according to where a family was in the disease journey which, for early‐life epilepsies, closely corresponds to the age of the child.9 As one parent expressed, there are four stages: initial shock of diagnosis, treatment odyssey where families try one therapy after another, desperation because “we're running out of options,” and then desolation and questioning “how long can we keep doing this?” In addition, the realization settles in, as a child grows older, that the hoped‐for improvements may never occur. Concerns about the future, especially financial security and plans beyond the parents’ lifetime, begin to take precedence. Parents discussed how “We're afraid our child will die before we do, and we're also afraid we'll die before our child does.” The sense of loss for what might have been also deepens.
4. DISCUSSION
Seizure frequency and severity are common measures of seizure burden.10, 11, 12, 13, 14 From a treatment perspective, these are relatively clear and measurable outcomes. Our qualitative data from a sample of parents of children with severe epilepsies indicate that unpredictability is an equally important aspect of seizure burden. While seemingly intuitive, unpredictability is not a feature of seizures commonly captured in current measurement scales, research studies, or in clinical practice.
The notion that seizures have consequences that extend to all aspects of life is not a new concept and is routinely reflected in quality of life measure such as the QOLIE‐89 (Quality of Life in Epilepsy‐89) which has separate physical and mental health, cognitive distress, and epilepsy‐targeted domains. Linking disease severity of burden to these domains largely emphasizes the importance of complete seizure freedom,11, 15 the primary goal of seizure therapy for all patients.16
The feature of unpredictability, however, adds another dimension and creates the need to be prepared and ready for the next seizure at any moment. This engenders another set of burdens that infiltrate and alter many if not most aspects of family life.
Caregiver burden has been extensively studied for many disease areas, for example, oncology.17 In pediatric epilepsy, the literature highlights that seizures create stress above and beyond other associated conditions.18, 19 Buelow conducted qualitative interviews with parents of children with both epilepsy and mild to moderate intellectual disability (IQ 55‐75) and identified five contributors to stress: concerns about the child, communication with physicians and other providers, effects on family relationships, school, and community sources of support.20 One survey of parents of children with Lennox‐Gastaut syndrome found about a third of parents reporting constant stress and worry as one effect of the disease.21 About 15%‐25% reported interrupting activities, no time for other children and financial stress. Bringing spouses closer together was also reported by about a third in Gibson's survey, and several comments about realization of strengths were also reported by workshop participants.21 Another survey of 24 parents of children with Dravet syndrome identified themes similar to those in our workshop such as development, behavior, sleep, and impact on children.22 Communicating with healthcare providers was another point raised in both groups.
Many studies have emphasized the depression associated with being a caregiver of a chronically ill family member (child or adult) and the consequences of depression and time constraints on caring for oneself, emotionally and medically.23, 24, 25, 26 These issues may not be specific to early‐life epilepsy. The time horizon and the impact on young parents and younger family members are very different, however, than what is typically the case in caregivers of people with, for example, Alzheimer disease or diseases in children that do not entail intellectual disability and guardianship. For children with ELE, parents must plan well beyond their own lifetimes, whereas for caregivers of older relatives with Alzheimer or similar diseases and conditions, that is usually not the case. The unpredictable nature of seizures stood out as a distinct element, however, from other diseases and represents a dimension that needs further study and means of quantifying.
4.1. Modulating factors
Where a family is in the treatment odyssey, the child's age and duration of the disorder influenced what is important for the parent and adds depth and complexity to the concept of seizure burden. While others have noted that the level of stress for parents did not vary by age of the child,19 our discussions suggested that the factors creating burden and causing stress changed over time, so stress may always be there but for different reasons. For example, aggressive behavior in a developmentally impaired two‐year‐old child was usually manageable, but the same behavior in a developmentally impaired, adult‐sized child posed risks for the parents or others and was described as more difficult to accommodate. Further, delineating distinct burdens caused directly or indirectly by seizures versus the burdens created by the child's level of disability, behavior, and medical fragility was not always possible.
The continued journey through the treatment odyssey from shock to desolation has not, to our knowledge, been well‐described, and there is clearly much to be understood in this regard. Nolan distinguished four phases in Dravet syndrome representing the different impacts of seizures versus behavioral morbidities over time but begin with the shock of diagnosis and uncertainty.9 Our participants highlighted the disease path as having a thread that went from hope that things would get better to dashed hopes of finding a solution and realization that the situation was never going to improve.
There are limitations to our workshop and report. The parents were mostly individuals known to the investigators, and many parents already knew each other. This, however, seemed to facilitate open conversation and a sense of common understanding. Although typical qualitative approaches utilize multiple focus groups to gather the breadth and depth of perspectives, we held a single day‐long workshop. This allowed us to gather significant quantities of information from participants and work with them to organize that information in a way that is consistent with their experiences. Additionally, we provided opportunities for further discussions and comments via teleconferences. Nonetheless, additional workshops or focus groups with a more varied sample could provide further insights. The discussions and this summary are only intended to reflect the most severe end of the spectrum of early‐life epilepsies and may not be applicable to individuals with better controlled or less severe seizures or who are not as severely disabled as the participants’ children. While children of participants ranged in age from infancy to adulthood, further exploration into age‐specific concerns is needed. Although not specifically “seizure burden,” medical and behavioral concerns surrounding puberty and healthcare, educational systems, and legal matters surrounding the transition to adult care were areas that require dedicated attention.
For many individuals affected by ELE, the goal of complete seizure freedom is currently not attainable. Even if it were, it is unclear that it would resolve all of the burdens associated with ELE. Seizure therapies, however, are specifically directed at seizures. A better understanding of how seizures—and their treatment—create their burden and what might constitute a meaningful improvement requires a balance—often delicate—between changes in seizure frequency and severity versus the additional burdens created by side effects from therapies, costs, and the time burden for parents in the context of unpredictability and all that that entails. Priorities will vary according to many factors, including over time.
With increased research focused on precision medicine and mechanism‐targeted therapies, such information is required to develop relevant measures that are responsive to meaningful change in patient outcomes. Our workshop sheds light on some of the complexities of the concept of seizure burden from the parent as well as provider perspective and specifically identifies the importance of unpredictability as a key driver in seizure burden.
DISCLOSURES
None of the authors has any conflict of interest to disclose. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
ACKNOWLEDGMENTS
This work was supported by the Stanley Manne Children's Research Institute and Ann & Robert H. Lurie Children's Hospital of Chicago under the Precision Medicine Strategic Research Initiative. We would like to thank the other parents who participated in this workshop for their time and their insights. We are grateful to Dr. John Millichap kindly agreed to cover for one of the physicians so she could attend this workshop.
Berg AT, Kaiser K, Dixon‐Salazar T, et al. Seizure burden in severe early‐life epilepsy: Perspectives from parents. Epilepsia Open. 2019;4:293–301. 10.1002/epi4.12319
REFERENCES
- 1. Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55:475–82. [DOI] [PubMed] [Google Scholar]
- 2. Durnford AJ, Rodgers W, Kirkham FJ, Mullee MA, Whitney A, Prevett M, et al. Very good inter‐rater reliability of Engel and ILAE epilepsy surgery outcome classifications in a series of 76 patients. Seizure. 2011;20:809–12. [DOI] [PubMed] [Google Scholar]
- 3. Rare diseases: common issues in drug development: guidance for industry. In: U.S. Department of Health and Human Services FaDA; 2015.
- 4. Krueger RA, Casey MA. Focus groups: a practical guide for applied research, 3rd edn Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- 5. Glaser B, Strauss AL. The discovery of grounded theory. Chicago, IL: Aldine; 1967. [Google Scholar]
- 6. Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- 7. Higginbottom G, Liamputtong P. What is participatory research? Why do it? In: Higginbottom G, Liamputtong P, editors. Participatory qualitative research methodologies in health. Los Angeles, CA: Sage, 2015. [Google Scholar]
- 8. Lincoln YS, Guba EG. Naturalistic inquiry. Newbury Park, CA: Sage; 1985. [Google Scholar]
- 9. Nolan KJ, Camfield CS, Camfield PR. Coping with Dravet syndrome: parental experiences with a catastrophic epilepsy. Dev Med Child Neurol. 2006;48:761–5. [DOI] [PubMed] [Google Scholar]
- 10. Lagae L, Brambilla I, Mingorance A, Gibson E, Battersby A. Quality of life and comorbidities associated with Dravet syndrome severity: a multinational cohort survey. Dev Med Child Neurol. 2018;60:63–72. [DOI] [PubMed] [Google Scholar]
- 11. Vickrey BG, Hays RD, Engel J, Spritzer K, Rogers WH, Rausch R, et al. Outcome assessment for epilepsy surgery: the impact of measuring health‐related quality of life. Ann Neurol. 1995;37:158–66. [DOI] [PubMed] [Google Scholar]
- 12. Chan CJ, Zou G, Wiebe S, Speechley KN. Global assessment of the severity of epilepsy (GASE) Scale in children: validity, reliability, responsiveness. Epilepsia. 2015;56:1950–6. [DOI] [PubMed] [Google Scholar]
- 13. Jain P, Subendran J, Smith ML, Widjaja E. Care‐related quality of life in caregivers of children with drug‐resistant epilepsy. J Neurol. 2018;265:2221–30. [DOI] [PubMed] [Google Scholar]
- 14. Camfield C, Breau L, Camfield P. Assessing the impact of pediatric epilepsy and concomitant behavioral, cognitive, and physical/neurologic disability: impact of Childhood Neurologic Disability Scale. Dev Med Child Neurol. 2003;45:152–301. [DOI] [PubMed] [Google Scholar]
- 15. Birbeck GL, Hays RD, Cui X, Vickrey BG. Seizure reduction and quality of life improvements in people with epilepsy. Epilepsia. 2002;43:535–8. [DOI] [PubMed] [Google Scholar]
- 16. Engel J. The goal of epilepsy therapy: no seizures, no side effects, as soon as possible. CNS Spectr. 2004;9:95–7. [DOI] [PubMed] [Google Scholar]
- 17. Streisand R, Braniecki S, Tercyak KP, Kazak AE. Childhood illness‐related parenting stress: the pediatric inventory for parents. J Pediatr Psychol. 2001;26:155–62. [DOI] [PubMed] [Google Scholar]
- 18. Camfield C, Breau L, Camfield P. Impact of pediatric epilepsy on the family: a new scale for clinical and research use. Epilepsia. 2001;42:104–12. [DOI] [PubMed] [Google Scholar]
- 19. Lowes L, Clark TS, Noritz G. Factors associated with caregiver experience in families with a child with cerebral palsy. J Pediatr Rehabil Med. 2016;9:65–72. [DOI] [PubMed] [Google Scholar]
- 20. Buelow JM, McNelis A, Shore CP, Austin JK. Stressors of parents of children with epilepsy and intellectual disability. J Neurosci Nurs. 2006;38:147–54, 176. [DOI] [PubMed] [Google Scholar]
- 21. Gibson PA. Lennox‐Gastaut syndrome: impact on the caregivers and families of patients. J Multidiscip Healthc. 2014;7:441–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Camfield P, Camfield C, Nolan K. Helping families cope with the severe stress of Dravet syndrome. Can J Neurol Sci. 2016;43(suppl 3):S9–s12. [DOI] [PubMed] [Google Scholar]
- 23. Khangura SD, Karaceper MD, Trakadis Y, Mitchell JJ, Chakraborty P, Tingley K, et al. Scoping review of patient‐ and family‐oriented outcomes and measures for chronic pediatric disease. BMC Pediatr. 2015;15:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Myhre J, Bjornstad Tonga J, Ulstein ID, Hoye S, Kvaal K. The coping experiences of spouses of persons with dementia. J Clin Nurs. 2018;27:e495–502. [DOI] [PubMed] [Google Scholar]
- 25. Piersol CV, Canton K, Connor SE, Giller I, Lipman S, Sager S. Effectiveness of interventions for caregivers of people with Alzheimer's disease and related major neurocognitive disorders: a systematic review. Am J Occup Ther. 2017;71:7105180020p7105180021–7105180020p7105180010. [DOI] [PubMed] [Google Scholar]
- 26. Brémault‐Phillips S, Parmar J, Johnson M, Huhn A, Mann A, Tian V, et al. The voices of family caregivers of seniors with chronic conditions: a window into their experience using a qualitative design. Springerplus. 2016;5:620. [DOI] [PMC free article] [PubMed] [Google Scholar]


