Abstract
Background:
Since the late 1990s, health departments and sexually transmitted disease (STD) programs throughout the United States have used technologies, such as the Internet and mobile phones, to provide services to persons with a sexually transmitted infection, including human immunodeficiency virus (HIV), and their sex partners, also known as partner services. This study reviewed the published literature to assess and compare partner services outcomes as a result of using technology and to calculate cost savings through cases averted.
Methods:
We conducted a structured literature review of all US studies that examined the use of technology to notify persons exposed to an STD (syphilis, chlamydia, gonorrhea), including HIV, by health care professionals in the United States from 2000 to 2017. Outcome measures, including the number of partners notified, screened or tested; and new positives identified, were captured and cost savings were calculated, when data were available.
Results:
Seven studies were identified. Methods used for partner services differed across studies, although email was the primary mode in 6 (83%) of the 7 studies. Only 2 of the 7 studies compared use of technology for partner services to traditional partner services. Between 10% and 97% of partners were successfully notified of their exposure through the use of technology and between 34% and 81% were screened or tested. Five studies reported on new infections identified, which ranged from 3 to 19. Use of technology for partner serves saved programs between US $22,795 and US $45,362 in direct and indirect medical costs.
Conclusions:
Use of technology for partner services increased the number of partners notified, screened or tested, and new infections found. Importantly, the use of technology allowed programs to reach partners who otherwise would not have been notified of their exposure to an STD or HIV. Improved response times and time to treatment were also seen as was re-engagement into care for previous HIV positive patients. Data and outcome measures across the studies were not standardized, making it difficult to generalize conclusions. Although not a replacement for traditional partner services, the use of technology enhances partner service outcomes.
Partner services, and specifically partner notification, whereby partners of patients with a diagnosed sexually transmitted disease (STD) or human immunodeficiency virus (HIV) infection are informed of their exposure, has long been a staple in public health efforts to control STD and HIV transmission.1 According to the Centers for Disease Control and Prevention (CDC), the goal of partner services is to maximize the number of partners who are notified of their exposure to an STD or HIV, treated, and linked to services.2 Notification can be undertaken in 3 ways—by the patient themselves, known as self- or patient-referral; by a health department staff member, often referred to as a disease intervention specialist (DIS), known as provider referral; or via third-party referral, where a professional other than health department staff member carries out the notification. Disease intervention specialist–led, partner notification investigations include interviewing patients who have tested positive for an STD, typically syphilis or HIV, eliciting sex partners within a prescribed time frame, locating and notifying those partners of their potential exposure, and referring those partners for STD screening, treatment, and care. Disease intervention specialists also link patients and partners to other services, such as HIV care, alcohol and drug programs, and mental health services.
For decades, DIS-led partner notification efforts involved notifying partners of their exposure by mailing letters or locating them “in the field” at their homes, places of work, or other venues.3 However, with the advent of the Internet, and later mobile phones, DIS began using technology-driven strategies to locate and notify partners.3–5 With the rising popularity of the Internet in the late 1990s, STD patients increasingly reported meeting sex partners online in chat rooms and later on websites specifically designed to facilitate sexual encounters. As the use of technology-based social venues increased, many patients could not provide traditional locating information about their partners, such as a real name, physical address, or telephone number. Rather, profile names and, in some cases, email addresses were often the only information known. To reach partners online, DIS began sending messages via email or joining websites to provide partner services through the venue’s internal messaging platforms. This became known as Internet-based partner services. Over time, the Internet became a recognized information source, allowing DIS to find traditional locating information of partners. Internet access also provided other invaluable pieces of information about partners, such as work affiliations, pictures, and social contacts that could be used to verify that the correct person was being reached. More recently, social networking sites and mobile applications have become popular venues for meeting sex partners.3,6–8
The purpose of this review was to assess and compare the outcomes of studies that examined the use of technology for STD and HIV partner services in the United States. Specifically, we sought to determine if the use of email, texting, social or sexual networking sites, or mobile phones increased the number of partners notified, screened, or tested; and new positives identified. Where applicable, we calculated the potential direct medical costs and indirect costs saved by technology-based partner service activities using the CDC’s Sexually Transmitted Infection Costs (STIC) calculator, a tool designed to help estimate the economic benefits of STD prevention programs such as partner services.9
METHODS
Our search included peer-reviewed studies that examined the use of technology to notify persons exposed to an STD (syphilis, chlamydia, gonorrhea), including HIV, by public health professionals in the United States from 2000 to August 31, 2017. We excluded studies that were conducted prior to 2000, outside the United Stated, not published in English, or did not report outcome measures. Systematic reviews, dissertations, editorials/opinion pieces, or studies in the grey literature, such as conference proceedings, technical reports, and white papers, were also excluded.
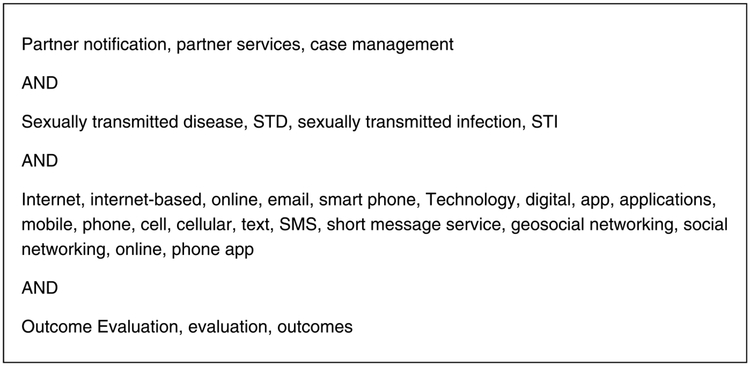
Search terms (Fig. 1) were entered into the following databases: PubMed, MEDLINE, PsycINFO, ProQuest, Embase, Google Scholar, and Scopus. The search identified 185 articles. The articles were compiled in EndNote and an initial review of the title and abstracts was conducted by 2 researchers. After a full review of the 185 articles, 178 were excluded for failing to meet the inclusion criteria, resulting in a final data set of 7 articles. One hundred forty-five articles were not about technology-based partner services, 18 did not report outcome data, 8 were grey literature/commentary/editorial, and 7 were not conducted in the U.S. References from the final data set of 7 articles were reviewed for additional relevant studies. No additional articles were identified.
Figure 1.
List of search terms. Partner notification, partner services, case management AND Sexually transmitted disease, STD, sexually transmitted infection, STI AND Internet, Internet-based, online, email, smart phone, Technology, digital, app, applications, mobile, phone, cell, cellular, text, SMS, short message service, geosocial networking, social networking, online, phone app AND Outcome Evaluation, evaluation, outcomes.
The STIC FIGURE (STIC) calculator allows programs to estimate the direct medical costs and indirect costs averted as a result of prevention program activities such as sequelae costs prevented due to treatment, prevention of congenital syphilis or STI-attributable HIV infections, or interruption of STI transmission within a population.8 To calculate direct medical costs and indirect costs saved, we reviewed the 7 identified articles for data variables required to generate an estimate, specifically the number of infections treated and the number of presumptive or preventive treatment instances. Three studies provided enough information to allow for a STIC calculation given the following assumptions—all partners were male, all syphilis cases were either primary or secondary, and where not reported, infected cases were treated.10–12 Timeframes for cost savings calculations were based on reported study dates and therefore vary by study.
RESULTS
Between 2000 and 2015, 7 studies3,10–15 reported outcome data (Table 1) on the use of technology for reaching partners including online chat rooms, email, social or sexual networking sites, mobile phone applications, and text messages. Due to the ever-changing communication landscape, the methods used for partner services differed across studies; however, there were overlaps. Only 2 of the 7 studies compared technology-based with traditional partner services.10,14 Below we report results by outcome measure (notification, screening and testing, and new positives) and by type of technology used (email, text, social/sexual websites, etc.)
TABLE 1.
Study Descriptions and Reported Outcomes Related to Use of Technology for STD-related Partner Services
| Author/Year of Publication | Study Location and Year of Data Collection | Population | Disease Type | Means of Contact Exposure or Intervention | No. Index Cases | No. Partners Notified | No. Partners Evaluated/Screened/Tested | No. New Infections |
|---|---|---|---|---|---|---|---|---|
| (1) Klausner et al., 20003 | San Francisco, June to August 1999 | MSM syphilis cases | Syphilis | Online chat room | 2 | NR | 20* | 4* |
| (2) Pioquinto et al., 200713 | Los Angeles, case 1 in December 2002; case 2 in January 2003 | MSM syphilis cases | Syphilis | Email messages | 2 | Case 1:29 (26%) of 111 partners notified Case 2: 13 of 16 partners (81%) |
Case 1: NR Case 2: 7 (54%) of 13 |
NR |
| (3) Vest et al., 200710 | Austin or Travis Co, TX; January 1, 2004 to June 30, 2006 | Cases: 53 partners of HIV and/or syphilis index patients for whom only email addresses were
known Controls: 265 partners of HIV and/or early syphilis index patients for whom traditional contact information was known |
HIV or early syphilis | Cases: Email sent to partners. Controls: Traditional contact (letter, face to face, telephone) |
Cases: 53 Controls: (traditional): 265 |
Cases: 88 (49.7%) of 177 Controls: 372 (69.7%) of 534 |
Cases: 71 (80.7%) of 88 Controls: 355 (95.4%) of 372 |
Cases: 19 (26.8%) Controls: 106 (29.9%) |
| (4) Ehlman et al., 200812 | Washington, DC, January 2007 to June 2008 | Patients with early syphilis infections (primary, secondary, and early latent) | Early syphilis | Emails to named partners | 27 | 291 (76%) of 381 | 101 (35%) of 291 | 7 (7%) |
| (5) Hightow-Wiedman etal.,201411 | State of North Carolina IPN data from July 1,2011 to June 30, 2012; Traditional PN from January
1 to December 31, 2010 Evaluation of pilot TxtPN program, November 21, 2011 to June 30, 2012 |
Clients diagnosed with HIV or syphilis | HIV and syphilis | Emails, social or sexual networking sites, mobile phone text messages | Internet: 362 Text: 29 |
Internet: 230 (63.5%) of 362 Text: 14† (48.3%) of 29 |
Internet: NR Text: NR |
Internet: 7 HIV (3.0%‡) 11
(4.8%‡) syphilis Text: 2 (14%) syphilis 1 (7%) HIV |
| (6) Udeagu et al., 201414 | New York City, NY January 2011 to October 2012 | HIV-diagnosed patients and their named partners | HIV | Emails, messages sent to social and dating/hook-up websites, mobile phone text messages | Traditional PS: 2604 Internet: 275 Text: 368 |
Traditional: 1803 (69%) contacted 1770 (98%) notified Internet: 112 (41%) contacted§ 100 (89%) notified¶ Text: 285 (77%) contacted§ 276 (97%) notified¶ |
Traditional: 805 (69%) Internet: 31 (34%) Text: 105 (45%) |
Traditional: 106(13%) Internet: 3 (10%) Text: 5 (5%) |
| (7) Pennise et al, 201515 | Monroe Co, Rochester, New York, February to May 2013. | Large case investigation stemming from a GC diagnosis in a previously known HIV-positive male. | HIV, gonorrhea, syphilis, chlamydia | Messages sent via unnamed website | Index cases: 14 2 (7 new infections; 7 Previously known HIV positive cases) Cluster cases: 2 (uninfected partners of index cases) |
2 | 31 (32%)∥ | 7 new infections total:∥
|
Klausner et al. did not specifically note, of the partners screened/tested and new infections identified, which were a direct result of using technology-based partner services.
Twenty nine contacts were texted of which 14 responded. Hightow-Weidman et al. do not indicate whether all 29 contacts were considered notified or only the 14 who responded.
Percentages were calculated by authors of this review who assumed that all patients who presented for testing were tested for both HIV and syphilis.
Udeagu et al. defined contact rates as the number of partners reached by any means divided by the number of partners for whom contact was attempted.
Udeagu et al. defined notification rates as the proportion of partners contacted who accepted HIV exposure notification.
Pennise et al. did not indicate, of the partners screened/tested and new infections identified, which were a direct result of technology-based partner services.
NR, not reported; GC, gonorrhea/gonococcal; PKP, previously known positive.
NOTIFICATION
E-mail was the type of technology used in 6 (83%) of the 7 studies.3,10–14 It should be noted that definitions of notification varied slightly across programs. For most studies, notification included a direct response from a contacted partner or presentation at a clinic. Two studies included the return of email read receipt messages.11,12 Udeagu et al14 defined notification as those partners who responded to DIS and who accepted information about an HIV exposure. In the earliest study, Klausner et al3 sent email messages to identified partners’ screen names, informing them of their exposure. However, Klausner et al3 did not report the number of partners notified specifically through the use of a communication technology, nor did they provide data comparing outcomes of partner services as a result of technology vs traditional means. Similarly, 3 studies also did not compare the use of technology to traditional partner services, but they all provided data regarding successful email notifications.11–13 Accordingly, between 26% and 89% of partners were successfully notified of their exposure through e-mail notification across the 5 studies providing such data.10–14
Vest et al10 and Udeagu et al14 were the only studies that compared technology-based partner services to traditional partner services. As mentioned earlier, their definitions of notification varied slightly. Vest et al10 defined notification as any elicited partner contacted by DIS staff, regardless of a response from the partner. They found that traditional partner services yielded a higher percentage of successful partner notifications than by email (69.7% vs 49.7%). Udeagu and colleagues,14 on the other hand, made clear distinctions in how they defined contact versus notification rates. The contact rate was defined as the proportion of partners from whom DIS received a response. The contact rate was inclusive of partners who refused notification—partners who did not want to know the purpose of the DIS email. Of the partners who were contacted and responsive to DIS, those who were then given information about their exposure to HIV were considered notified. That is, the notification rate consisted of the proportion of partners who responded to DIS and accepted HIV exposure information. Those notified included partners confirmed to be previously HIV diagnosed or who reported an unknown or HIV-negative serostatus. Udeagu et al14 found that the contact rate for traditional partner notification (69%) was higher in comparison to email notification (41%). However, the use of technology resulted in a higher likelihood of notifying partners of their exposure than traditional notification (odds ratio [OR], 2.1; 95% confidence interval [95% CI], 1.2–3.4).
Texting
Two studies assessed text messaging for partner notification.11,14 Hightow-Weidman et al11 sent text messages to 29 identified partners who did not respond to traditional or email-based partner notification. Fourteen (48%) of the partners responded and were notified of their exposure. The study, however, did not compare outcomes between text messages, traditional, and email-based partner notification. Similarly, Udeagu and colleagues14 sent texts to 368 partners whose only viable contact information was a cellphone number. They compared partner notification outcomes by mode of contact and found that texting resulted in a higher contact rate (77%) than traditional (69%) or technology-based methods (41%; P <0.0001). However, no significant differences were found in notification rates between texting vs technology-based partner services, though both had a higher likelihood of notifying a contacted partner when compared to traditional partner services (OR, 2.4; 95% CI, 1.7–3.2 and OR, 2.1; 95% CI, 1.2–3.4; P=0.0001 respectively). Both studies found that partners responded quickly to texts with a median response time of 57.5 minutes and 1 day, respectively.
Mobile Applications and Social Media Websites
Only 1 study, Pennise et al15 reported on the use of mobile applications (“apps”) and social media websites. The apps and social media websites were used to gather demographic and geographic information about the sexual partners named in 16 DIS interviews. Six (29%) partners were located using information gathered from apps and websites and 2 (10%) were notified of their exposure via an unnamed website. The authors noted that mobile apps were not used for notification.
SCREENING AND TESTING
Five (71%) of the 7 studies provided sufficient data on the number of partners screened or tested as a result of the use of technology.3,10,12–14 Of the 2 studies reporting on texting,11,14 only one provided information on screening/testing outcomes.14 Accordingly, the percentage of partners tested or screened due to technology use ranged from 34% to 80.7% across the 5 studies. Vest et al10 reported the highest percentage of technology-initiated testing and screening (80.7%) in their case-comparison study among HIVor syphilis-infected persons with pseudonymous e-mail sexual partners and unmatched controls. Yet, traditional partner notification generated an even higher percentage of partners tested and screened (95.4%; P < 0.001). Pioquinto et al13 also reported a high percentage of testing and screening (54%) as a result of technology use in their case study of a 31-year-old man infected with syphilis who reported 16 Internet sex partners.
In contrast, Ehlman et al12 and Udeagu et al14 reported the lowest percentage of successful technology-initiated testing and screening among the 5 studies. Udeagu et al14 found that 34% (n = 31) of partners notified through email and 45% (n = 105) notified through text were tested for HIV compared to partners notified through traditional means (69%, P ≤ 0.0001). Ehlman et al12 found that 35% of email-notified partners presented for syphilis testing. Specifically, 53 (52%) partners who provided DIS with traditional contact information were screened for syphilis, whereas 48 (48%) partners who did not provide traditional contact information to DIS reported they were evaluated and treated if necessary.
NEW INFECTIONS
Five (71%) studies reported the number of new infections found through technology10,14,15 and as a result of texting, specifically, in 2 studies.11,14 Technology use resulted in identification of new infections ranging from 3 to 19 with Vest and colleagues10 reporting the highest number and percentage (26.8%) of new HIV and/or syphilis infections identified among 71 Internet partners tested. This was a slightly lower percentage, but not statistically significant (P = 0.601), when compared with traditional partner notification, which yielded 106 new infections or 29.9% of the 355 partners screened and tested.
The remaining studies reported lower numbers3,11,12,14,15 and percentages (7%–10%) of new HIVand/or syphilis infections among Internet-notified partners. Klausner et al3 identified 4 new cases of syphilis (20%) and 1 previous positive. Ehlman et al12 found 7 (7%) new syphilis cases of the 101 partners evaluated. Hightow-Weidman et al11 found 7 new HIV infections and 11 new syphilis infections among 230 email-notified partners. They texted 29 contacts who did not respond to traditional or email-based partner services and identified 1 (7%) new HIV infection and 2 (14%) new syphilis infections among the 14 partners who responded. Udeagu et al14 also found new infections among partners notified through email or text message. Three (10%) new HIV infections were discovered among 31 partners notified through email, and 5 (5%) new HIV infections were identified among 105 text-notified partners.
Finally, only 1 study, Pennise et al,15 reported new infections of gonorrhea and chlamydia in addition to new HIV and syphilis infections. The researchers identified 2 new HIV infections, 1 new HIV-gonorrhea coinfection, 1 syphilis-chlamydia coinfection, 1 new chlamydia infection, and 2 new gonorrhea infections, one of which was in a previously diagnosed HIV positive partner. Pennise et al15 did not specify which new infections were found as a result of the use of technology.
COST SAVINGS
Of the 3 studies for which we were able to estimate direct medical and indirect costs (Table 2), we found that technology-based partner service efforts saved programs between US $22,795 and US $45,362 (in 2016 dollars) due to interrupted transmission of syphilis and future cases averted.10–12
TABLE 2.
Potential DirectMedical Costs and Indirect Costs Saved by Technology-based Partner Service Activities Using the CDC’s STIC Calculator
| Study | STD Cases Prevented | Direct Medical Costs Saved* | Indirect Costs (Lost Productivity†) | Total Costs Saved | Period |
|---|---|---|---|---|---|
| Vest et al, 200710 | 28.5 | US $26,620 | US $18,742 | US $45,362 | January 01, 2004, to June 30, 2006 |
| Hightow-Wiedman et al, 201411 | 26.40 | US $23,968 | US $14,862 | US $38,830 | July 01, 2011 to June 30, 2012 |
| Ehlman et al, 200812 | 16.50 | US $14,661 | US $8,134 | US $22,795 | January 2007 to June 2008 |
Dollar amounts reported in 2016 dollars
Indirect costs refer to loss of productivity in diagnosed patients as a result of illness, disability, and premature death. For more information, see Chesson et al.9
DISCUSSION
Overall, we found the use of technology resulted in additional partners being notified, screened or tested, and identified as new positives. Importantly, DIS reached partners who otherwise would not have been notified of their STD/HIV exposure and, in some instances, reached HIV positive individuals who had fallen out of care.11 We estimate that the use of technology for partner services saved programs between US $22,795 and US $45,362 in direct medical costs and indirect costs. Although notification alone does not guarantee that partners will seek screening and treatment, it does provide them with information from which they can make informed decisions about medical care and future partners.
Most studies encouraged the integration of technology into existing partner service programs, when possible. All concluded that technology offered worthwhile advantages including increased operational efficiency10,11,14; improved outcomes in both traditional and technology-based partner service cases12; and rapid, efficient, and reliable means of finding and notifying partners.3,10–12,14 Though not identified as a benefit in the studies, technology helps to fulfill the ethical duty or privilege to warn. As outlined in the CDC’s Recommendations for Partner Services Programs, health care providers, either directly or with help from public health authorities, bear the responsibility of, at a minimum, doing their due diligence to let a person know of an exposure whenever possible.2 In one study, researchers found that partners were appreciative of partner service messages and found them helpful and appropriate.3 Another study suggested that patient involvement in partner notification and use of instant messaging improved response rates.13
Texting offered unique advantages. Often, it was the only mode of communication that yielded a reply and had vastly quicker response times than traditional or email-based partner services.11,14 Data security and confidentiality concerns exist, however, as telecommunication providers are not required to protect the content of text messages,11 prompting fear that messages could be turned over to external parties, such as the police.
The importance of DIS who are technologically savvy and abreast of the ever-changing privacy rules of social and sexual networking venues was also noted.11,12,14 Disease intervention specialist also benefited from real-time access to websites and mobile apps, which allowed index patients to access their social networking accounts to gather partner location information, verify screen names, and identify other social network contacts.15 Programs noted that resources, buy-in, and training are needed when integrating technology into a partner services program; however, once in place, use of technology did not result in additional field work or extended work hours. Instead, the reach and effectiveness of partner services was expanded.10,14 One study compared outcomes before and after centralizing technology-based activities with a single field coordinator. Centralization increased the number of partner’s notified, screened, and new positives identified and treated.11 It is unknown if other factors may have contributed to the success of centralization—for example, morbidity levels, coordinator skill and experience with communication technology, and comprehensive policies. More studies comparing centralization and decentralization of technology-based partner services could help answer these questions.
This review had limitations. First, a review of the grey literature was not conducted. It is possible technology-based partner service studies were highlighted in conference proceedings, technical reports, and white papers. Second, differences in program goals and objectives, data collection techniques, and variations in the definitions of contact and notification prevented us from comparing partner service efforts across studies and as such, we are unable to speak to the reasons for program successes and failures beyond noting that technology use resulted in additional partners notified, screened, and new infections identified. These variations occur for a variety of reasons which include: (1) functions of a program’s data management system, which dictates what information is available to be evaluated; (2) a program’s approaches to conducting PS, which can affect evaluation efforts; and (3) integral factors, such as the reputation of the health department, interviewing skills of DIS, and the (in)ability to collect identifying information from websites and apps. More research and evaluation of existing partner service programs would be useful. Future evaluations could compare partner service outcomes by mode of notification (eg, telephone vs email vs texting) when possible. These evaluations can elucidate which methods result in more notifications, new infections, faster response times, or quicker time to treatment. They could also provide useful information to programs about changes in communication use and preferences of patients and partners over time. Future studies could also compare outcome measures before and after the implementation of technology to determine if new notification modes improve the number of partners notified, screened, and treated.
Finally, generalizability is limited given that most of the study participants were men, a large proportion of which were men who have sex with men. Thus, it is not clear if technology use would enhance partner services for other populations.
Although not a replacement for traditional PS, technology enhances partner service outcomes. We would like to be able to point to a specific program and declare it to be the most effective, unfortunately, given the limitations stated above, we are unable to do that. Rather, programs will need to determine their level of technology use for partner services—from accessing the Internet to search for traditional information to being able to log into sex seeking websites or apps to directly notify a partner—based on their program goals, infrastructure, epidemiology, and available resources. The CDC’s Division of STD Prevention has supported the adaption and integration of technology into partner service activities and offers a toolkit to help health departments incorporate the use of technology into their efforts.16–18 Given the ubiquity and near total integration of technology into all aspects of American lives, at a minimum, the ability to gather information about partners from the Internet and other social networking venues seems essential for partner services.
Footnotes
Conflicts of interest and Sources of Funding: None declared.
REFERENCES
- 1.Parran T Shadow on the Land: Syphilis. Reynal & Hitchcock: New York, NY, 1937. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. Morb Mortal Wkly Rep 2008; 57(RR-9):1–63. [PubMed] [Google Scholar]
- 3.Klausner JD, Wolf W, Fischer-Ponce L, et al. Tracing a syphilis outbreak through cyberspace. JAMA 2000; 284:447–449. [DOI] [PubMed] [Google Scholar]
- 4.McFarlane M, Kachur R, Klausner JD, et al. Internet-based health promotion and disease control in the 8 cities: Successes, barriers, and future plans. Sex Transm Dis 2005; 32:s60–s4. [DOI] [PubMed] [Google Scholar]
- 5.Wohlfeiler D, Potterat JJ. Using gay men’s sexual networks to reduce sexually transmitted disease (STD)/human immunodeficiency virus (HIV) transmission. Sex Transm Dis 2005; 32(10 Suppl):S48–S52. [DOI] [PubMed] [Google Scholar]
- 6.Young SD, Szekeres G, Coates T. The relationship between online social networking and sexual risk behaviors among men who have sex with men (MSM). PLoS One 2013; 8:e62271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beymer MR, Weiss RE, Bolan RK, et al. Sex on demand: Geosocial networking phone apps and risk of sexually transmitted infections among a cross-sectional sample of men who have sex with men in Los Angeles County. Sex Transm Infect 2014; 90:567–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zou H, Fan S. Characteristics of men who have sex with men who use smartphone geosocial networking applications and implications for HIV interventions: A systematic review and meta-analysis. Arch Sex Behav 2017;46:885–894. [DOI] [PubMed] [Google Scholar]
- 9.Chesson HW, Collins D, Koski K. Formulas for estimating the costs averted by sexually transmitted infection (STI) prevention programs in the United States. Cost Eff Resour Alloc 2008; 6:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vest JR, Valadez AM, Hanner A, et al. Using e-mail to notify pseudonymous e-mail sexual partners. Sex Transm Dis 2007; 34:840–845. [DOI] [PubMed] [Google Scholar]
- 11.Hightow-Weidman L, Beagle S, Pike E, et al. “No one’s at home and they won’t pick up the phone”: using the Internet and text messaging to enhance partner services in North Carolina. Sex Transm Dis 2014; 41:143–148. [DOI] [PubMed] [Google Scholar]
- 12.Ehlman DC, Jackson M, Saenz G, et al. Evaluation of an innovative internet-based partner notification program for early syphilis case management, Washington, DC, January 2007-June 2008. Sex Transm Dis 2010; 37:478–485. [DOI] [PubMed] [Google Scholar]
- 13.Pioquinto RM, Tupas EA, Kerndt PR, et al. Using the Internet for partner notification of sexually transmitted diseases – Los Angeles County, California, 2003. MMWR Morb Mortal Wkly Rep 2004; 53:129–131. [PMC free article] [PubMed] [Google Scholar]
- 14.Udeagu CC, Bocour A, Shah S, et al. Bringing HIV partner services into the age of social media and mobile connectivity. Sex Transm Dis 2014;41:631–636. [DOI] [PubMed] [Google Scholar]
- 15.Pennise M, Inscho R, Herpin K, et al. Using smartphone apps in STD interviews to find sexual partners. Public Health Rep 2015; 130:245–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kachur R, Strona FV, Kinsey J, et al. Introducing technology into partner services: A toolkit for programs. Centers for Disease Control and Prevention: Atlanta, GA, 2015. [Google Scholar]
- 17.Douglas JM, Janssen R. Dear colleague letter. Centers for Disease Control and Prevention: Atlanta, GA, 2005. [Google Scholar]
- 18.Walsh C Dear colleague letter. Centers for Disease Control and Prevention: Atlanta, GA, 2010. [Google Scholar]