Abstract
Background:
Some athletes demonstrate excellent dynamic stability after anterior cruciate ligament (ACL) rupture and return to sport without ACL reconstruction (copers). Others demonstrate persistent instability despite rehabilitation (non-copers) and require surgical stabilization. Testing to determine coper classification can identify potential copers early after rupture. It is unclear how coper classification changes after a brief intervention, and how early classification relates to long-term outcomes.
Hypothesis/Purpose:
(1) To evaluate the consistency of early coper classification (potential coper vs. non-coper) before and after progressive neuromuscular and strength training (NMST) in athletes early after acute ACL rupture and (2) to evaluate the association of early coper classification with two-year success after ACL rupture.
Study Design:
Prospective cohort study
Methods:
This was a prospective analysis from the Delaware-Oslo ACL cohort study, a cohort of athletes consecutively enrolled early after ACL rupture. Participants (n=271) were tested and classified as potential copers or non-copers using established criteria before and after a 10-session NMST program. Success two years after ACL reconstruction (ACLR) or non-operative rehabilitation (Non-Op) was defined as meeting/exceeding sex- and age-matched norms for knee function, no ACL graft rupture, and ≤1 episode of giving way within the previous year. McNemar’s test evaluated changes in coper classification pre- to post-training. Logistic regression adjusted for baseline characteristics was used to evaluate the association of early coper classification and surgical status with two-year success.
Results:
Of 300 athletes enrolled, 271 (90%) completed the post-training data collection and 219 (73%) returned for the two-year follow-up. The coper classifications were different between timepoints; nearly half of those classified initially as non-copers became potential copers (p<0.001). At the two-year follow-up, 64% of the ACLR group and 74% of the Non-Op group were successful. Athletes who were potential copers post-training and chose ACLR or Non-Op rehabilitation had 2.7(95%CI 1.3–5.6) and 2.9(95%CI 1.2–7.2) times the odds of success, respectively, compared to non-copers who chose ACLR.
Conclusion:
Coper classification improved after NMST; more athletes became potential copers. Athletes who were potential copers following NMST were more likely to succeed two years later regardless of whether they had surgery, strongly supporting the addition of NMST prior to ACLR. Persistent non-copers fared poorly, indicating more intensive rehabilitation may be needed.
Keywords: ACL injury, coper classification, prehabilitation, neuromuscular training
INTRODUCTION.
Individuals respond differently to acute, complete anterior cruciate ligament (ACL) rupture. Nearly 20 years ago, we coined the terms copers (athletes who resume prior levels of activity without dynamic instability following ACL rupture) and persistent non-copers (athletes who continue to have episodes of dynamic instability despite progressive rehabilitation).7 In early work by our group, Fitzgerald et al. developed a functional screening test battery to identify those we called “potential copers” early after ACL rupture who could delay operative treatment.11 This screening test battery uses functional tests and patient-reported outcome measures to classify athletes as potential copers (i.e., those who demonstrate dynamic stability and good self-reported and performance-based knee function), or non-copers (i.e. those with instability and/or poor self-reported or performance-based knee function). Potential copers generally demonstrate better clinical presentation7, 8, balance25, movement patterns2, 4, 5, 23, 24, and muscle activation16, 23 compared to non-copers. The extent to which these classifications change with early rehabilitation and how they relate to long-term outcomes, however, is unclear.
Dynamic knee stability can improve with rehabilitation after ACL rupture.9, 20 When treated with rehabilitation alone, 70% of those who were classified as non-copers early after injury became true copers after 1 year.20 These findings indicated that early coper classification is not static, and is mutable with intervention. It is unclear, however, if a brief period of prehabilitation (i.e. rehabilitation prior to definitive intervention of ACL reconstruction [ACLR] or non-operative rehabilitation [Non-Op]) is sufficient to change an athlete from a non-coper to a potential coper. Clinically, it would be most useful to recognize early how an athlete will fare long-term after an ACLR or Non-Op intervention and, potentially, who needs surgery.
Prior work by our group indicates that a 10-session prehabilitation program improves long-term outcomes after ACLR. Failla et al.10 and Grindem et al.15 compared the two-year outcomes of the US and Norwegian participants in the Delaware-Oslo ACL Cohort to participants in the MOON cohort and the Norwegian National Knee Ligament Registry (NKLR), respectively.10, 15 All three cohorts used a criterion-based rehabilitation program following ACLR. The Delaware-Oslo ACL Cohort uniquely received prehabilitation via a 5-week9 (10 sessions) progressive neuromuscular training and strength training (NMST) program prior to surgery (Figure 1). Two years after ACLR, superior patient-reported knee function and rates of return to preinjury sports were observed in the Delaware-Oslo ACL Cohort compared to the MOON cohort10 and NKLR15.
Figure 1.
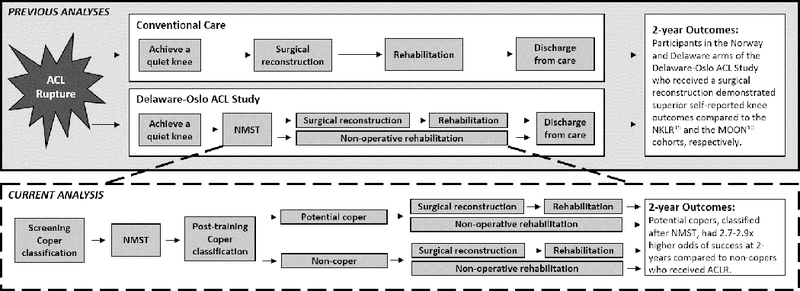
This figure presents the findings of the current study in the context of previous analyses in this cohort.
While we know that NMST results in improved outcomes before and after ACLR, it remains unclear if NMST affects coper classification prior to ACLR or continued Non-Op management. Potential copers and non-copers demonstrate different functional outcomes7, 8 and movement patterns2, 4, 5, 23, 24, but it is unclear how coper classifications relate to outcomes two years later. The purpose of this study was two-fold: (1) To evaluate the consistency of early coper classification (potential coper vs. non-coper) before and after 10 sessions of progressive NMST in athletes early after acute ACL rupture and (2) to evaluate the association of early coper classification with two-year outcomes. We hypothesized that (1) non-copers could become potential copers after NMST and (2) potential copers would have greater odds of two-year success than those who continued to be classified as non-copers after NMST.
MATERIALS AND METHODS.
Design.
This study was the primary analysis from the Delaware-Oslo ACL cohort, a prospective study evaluating athletes after ACL rupture. Participants in the Delaware-Oslo ACL cohort study underwent clinical testing at the time of enrollment (‘screening’), after a 10-session NMST program (‘post-training’), and six months, one year and two years after self-selecting ACLR or Non-Op rehabilitation. Data from screening, post-training, and two-year follow-up were used in this analysis. This study was approved by the Institutional Review Board at the University of Delaware and the Regional committee for Medical and Health Research Ethics South East Norway.
Participants.
The Delaware-Oslo ACL cohort study includes athletes consecutively enrolled at the University of Delaware (n=150) and at the Norwegian Sports Medicine Clinic (n=150) from 2007–2012. Athletes were included if they sustained a unilateral ACL rupture confirmed by MRI within seven months of enrollment and regularly (>50 hours per year) participated in level I/II sports prior to injury.6 Exclusion criteria were previous injury or surgery on the contralateral knee or significant concomitant injuries (full-thickness cartilage defect >1cm2, symptomatic or repairable meniscal tear, or other grade 3 ligamentous injury). Eligible participants were enrolled in the study following the resolution of initial injury impairments (i.e. full knee range of motion, minimal effusion, minimal pain, quadriceps strength limb symmetry index ≥70%).
Neuromuscular training and strength training (NMST).
All athletes completed a 10-session NMST program over approximately 5 weeks. The training program was previously described in detail9, and consisted of progressive strengthening, plyometric, and neuromuscular exercises with the goal of restoring muscle strength and neuromuscular control.
Coper classification.
Participants completed clinical testing before and after NMST (Table 1) and were classified as potential copers or non-copers based on our previously established screening criteria.11 Briefly, potential copers were identified as those with Knee Outcome Survey-Activities of Daily Living Scale (KOS-ADLS) score ≥80%, global rating score ≥60%, ≥80% symmetry on the timed hop (uninvolved/involved*100), and ≤1 recent episodes of giving way during activities of daily living. Non-copers failed to meet at least one of these criteria.
Table 1.
Screening examination and coper classification
| Screening test | Coper classification threshold* |
|---|---|
| Timed 6 meter hop | ≥ 80% |
| Knee Outcome Survey – Activities of Daily Living Score | ≥ 80% |
| Global Rating Score | ≥ 60% |
| Number of giveway episodes | ≤1 |
Potential Coper: Meets threshold on all 4 tests; Non-coper: Fails any of the 4 tests.
Surgical decision-making.
Patients decided over the course of the pre-operative rehabilitation whether to proceed with ACLR or continue with rehabilitation management.14 This decision was the self-selected, and was not dictated by the study.
Success at two year follow-up.
Success two years after ACLR or Non-Op rehabilitation was defined as meeting or exceeding sex- and age-matched norms (15th percentile) on the International Knee Documentation Committee Subjective Knee Form (IKDC)3, no ACL graft rupture, and ≤1 episode of giving way within the last year. Failure two years after ACLR or Non-Op rehabilitation was defined as meeting one of the following criteria: falling below IKDC sex- and age-matched norms, sustaining an ACL graft rupture, or multiple episodes of giving way in the last year.
Statistical analyses.
Descriptive statistics were performed on all variables. McNemar’s test was performed to evaluate changes in coper classification from screening to post-training (hypothesis 1). Four exposure groups were created by combining coper classification (potential coper vs. non-coper) and the definitive intervention (Non-Op vs. ACLR): Non-Op potential copers, ACLR potential copers, Non-Op non-copers, ACLR non-copers. These four groups were created using both the screening and post-training coper classifications. Logistic regression was performed to evaluate the association of the exposure with two-year success using odds ratios (OR) and 95% confidence intervals (95%CI), adjusting for sex, baseline age, and baseline body mass index (hypothesis 2). We adjusted for age and sex since ACL graft rupture rates are affected by these variables.18, 26 The odds ratios were calculated with the ACLR non-copers as the reference group. As a sensitivity analysis, we used patient acceptable symptom state21 for the IKDC threshold for failure instead of the age-matched normative data. Analyses were conducted in SAS 9.4 and hypotheses were tested at alpha=0.05.
RESULTS.
Of 300 athletes who enrolled in the study (Table 2), 271 (90%) completed the post-training data collection. Time from screening to post-training testing was 5.2±2.4 weeks on average. Of the 271 athletes who participated in the post-training testing, 219 (81%) returned for the two-year follow-up (73% of those enrolled). Participants who returned for the two-year follow-up included 93 ACLR potential copers (43%), 61 ACLR non-copers (28%), 51 Non-Op potential copers (23%), and 14 Non-Op non-copers (6%) (Table 5b).
Table 2.
Baseline participant characteristics (n=300)
| Mean ± SD (Range) or %(n) | |
|---|---|
| Sex, female | 45.7 (137) |
| Age at baseline, years | 26.5 ± 9.7 (13 – 55) |
| Body mass index at baseline, kg/m2 | 24.7 ± 4.0 (18.3 – 40.3) |
| Level of sport prior to injury
Level I Level II |
69.3 (208) 30.7 (92) |
| Time from injury to enrollment (days) | 58 ± 35 (1 – 272) |
| ACL status at two-yearsλ ACLR Non-Op |
70.8 (211) 29.1 (87) |
| Knee Outcome Survey – Activities of
Daily Living Score at baseline* |
84.7 ± 10.5 (50–100) |
| Global Rating Score at baseline† | 78.0 ± 14.7 (10–100) |
| No giveway (≤1 episodes) at baseline* | 79.8 (237) |
Missing data for 2 participants
Missing data for 3 participants
Missing data for 1 participant
Abbreviations: SD, Standard deviation; ACL, Anterior cruciate ligament; ACLR, ACL reconstruction; Non-Op, Continued non-operative rehabilitation
Table 5.
Unadjusted and adjusted odds ratios and 95% confidence intervals (OR (95% CI)) of success two years following ACL injury and/or reconstruction based on (A) screening coper classification and surgical status, and (B) post-training coper classification and surgical status.
| A. Using coper classification at screening (N=232) | |||||
| Coper classification | Surgical status | Percent of analytic sample* (n) | Success rate† (n) | Unadjusted OR (95% CI) |
Adjusted‡ OR (95% CI) |
| Potential coper | Non-Op | 15% (35) | 77% (27) | 2.5 (1.0 – 6.2) | 2.0 (0.79 – 5.3) |
| ACLR | 40% (93) | 73% (68) | 2.0 (1.1 – 3.9) | 2.4 (1.2 – 4.8) | |
| Non-coper | Non-Op | 13% (31) | 71% (22) | 1.8 (0.73 – 4.5) | 1.4 (0.54 – 3.6) |
| ACLR | 32% (73) | 58% (42) | REF | REF | |
| B. Using coper classification at post-training (N=219) | |||||
| Coper classification | Surgical status | Percent of analytic sample* (n) | Success rate‡ (n) | Unadjusted OR (95% CI) |
Adjusted‡ OR (95% CI) |
| Potential coper | Non-Op | 23% (51) | 82% (42) | 3.7 (1.5 – 8.9) | 2.9 (1.2 – 7.2) |
| ACLR | 43% (93) | 75% (70) | 2.4 (1.2 – 4.8) | 2.7 (1.3 – 5.6) | |
| Non-coper | Non-Op | 6% (14) | 43% (6) | 0.60 (0.18 – 1.9) | 0.51 (0.15 – 1.7) |
| ACLR | 28% (61) | 56% (34) | REF | REF | |
Abbreviations: OR, Odds ratio; CI, Confidence interval; ACL, Anterior cruciate ligament; ACLR, ACL Reconstruction; Non-Op, Continued non-operative rehabilitation; REF, Reference group
This column contains the percent (and count) of the analytic sample that were classified as each respective unique combination of coper classification and surgical status 2-years later (e.g. potential coper who had non-operative rehabilitation).
This column contains the percent (and count) of each unique group that were classified as successful at the two-year follow up.
Adjusted for age, sex, body mass index
Consistency in coper classification at screening and post-training.
The potential coper and non-coper classifications were different between time points (p<0.0001, Table 3). 55% were potential copers at screening and 68% were potential copers post-training (Table 3). Almost half (45%) of initial potential non-copers became potential copers post-training, while only 13% of initial potential copers became non-copers after NMST. About a quarter of the athletes were non-copers at screening, and remained non-copers post-training. Characteristics of athletes classified as potential copers and non-copers post-training are presented in Table 4.
Table 3.
Contingency table of coper classification before (screening) and after (post) the neuromuscular and strength training (NMST) program
| Post-training Coper classification | ||||
|---|---|---|---|---|
| Potential Coper | Non-coper | Total | ||
|
Screening
Coper classification |
Potential Coper | 131 | 19 | 150 |
| Non-coper | 54 | 67 | 121 | |
| Total | 185 | 86 | 271 | |
| McNemar’s Test: p<0.001 | ||||
Table 4.
Summary statistics of baseline demographics and two-year outcomes by post-training coper classification
| Mean ± SD (Range) or % (n) | ||
|---|---|---|
| Potential Coper | Non-coper | |
| n | 185 | 86 |
| Sex, female | 49.2% (91) | 43.0% (37) |
| Age at baseline, years | 26.1 ± 9.9 (13 – 54) | 27.5 ± 9.8 (15 – 55) |
| Body mass index at baseline, kg/m2 | 24.2 ± 3.5 (18.3 – 39.8) | 25.6 ± 4.7 (18.6 – 40.3) |
| Level of sport prior to
injury Level I Level II |
69.1% (128) 30.8% (57) |
69.8% (60) 30.2% (26) |
| Time from injury to enrollment, days | 57 ± 30 (1 – 272) | 64 ± 43 (8 – 270) |
| ACL status at two
years ACLR Non-Op |
64.9% (120) 35.1% (65) |
82.6% (71) 17.4% (15) |
| IKDC at two years | 91.9 ± 9.7 (50.0 – 100) | 88.2 ± 12.9 (37.9 – 100) |
| ≤1 episodes of giveway at two years | 96.4% (133, missing 47) | 81.4% (57, missing 16) |
| ACL graft rupture by two years | 6.0% (11) | 10.5% (9) |
Abbreviations: SD, Standard deviation; ACL, Anterior cruciate ligament; IKDC, International Knee Documentation Subjective Knee Form
Association of coper classification with two-year success.
At the follow-up, 64% of the ACLR group and 74% of the Non-Op group were successful (per strict study criteria defined in the methods). Using coper classification at screening, ACLR potential copers had 2.3 (95%CI 1.2–4.7) times the odds of success compared to ACLR non-copers; Non-Op potential copers and non-copers did not significantly differ from ACLR non-copers (Table 5a). Using coper classification post-training, ACLR and Non-Op potential copers had 2.7 (1.3–5.6) and 2.9 (1.2–7.2) times the odds of success compared with ACLR non-copers, respectively (Table 5b). The Non-Op non-copers had 0.51 (0.15–1.7) times the odds of success compared to ACLR non-copers, however it was not statistically significant, potentially due to the exceedingly small number of non-copers who elected non-operative management after NMST. In the sensitivity analysis, using patient acceptable symptom state in lieu of IKDC norms did not change the overall outcome (Supplemental Table 1).
DISCUSSION.
This study evaluated the consistency of coper classification in response to rehabilitation and the implications of early coper classification on long-term outcomes. The findings upheld our hypotheses. Nearly half (45%) of non-copers became potential copers following NMST, while conversion from potential coper to non-coper was uncommon (13%). Further, athletes who were potential copers post-training were more likely to have a successful two-year outcome regardless of operative management compared to the non-copers who received ACLR. The odds ratios also indicated that non-copers with Non-Op may have lower odds for success compared to ACLR, however these results were not conclusive due to the small number of non-copers who elected Non-Op management.
Coper classification can change after NMST.
There are varying degrees of dynamic stability after ACL rupture, however we observed that many athletes improved coper classification after NMST early after injury. Nearly half of the initial non-copers became potential copers after NMST, indicating improved dynamic stability. We are unable to solely attribute the change in coper classification to the NMST program, as there was no control group. It is unclear to what extent natural recovery over the ~5 week NMST contributes to changing coper classification. Since a “quiet knee” was required for study enrollment, we are confident that participants were at a similar criterion stage of recovery. Interestingly, 55% of the current sample were classified as potential copers at the screening, which is greater than the 42% previously reported by Hurd et al.17 While the inclusion criteria in both samples were similar, the current sample was tested an average 2 weeks later after injury (8 weeks17 vs. 6 weeks), which may contribute to the discrepancy and indicated that time also plays a role in the development of dynamic stability after ACL rupture.
Coper classification after a challenge (NMST) to the neuromuscular system improves insight into two-year outcomes.
Our data indicate that completing progressive NMST early after injury and then evaluating dynamic stability is a critical component to providing early insight into long-term prognosis for young athletes with ACL rupture. A primary goal of progressive NMST is to restore adequate neuromuscular responses, in addition to recovering muscular strength.9 NMST included exercises designed to progressively challenge the neuromuscular system. The response to this brief NMST intervention was significant. Nearly half (45%) of the athletes who were non-copers prior to NMST responded positively, that is they became potential copers following the intervention. The other half (55%) of non-copers did not respond to the intervention, and continued to demonstrate instability. Most (87%) of the athletes who were initial potential copers demonstrated dynamic stability throughout the progressive intervention. A small percentage (7 %) of athletes who initially were classified as potential copers became non-copers. Potential copers classified after NMST, regardless of intervention with ACLR or Non-Op rehabilitation, had 2.7–2.9 times the odds to succeed two years later compared to non-copers who received ACLR.
Brief prehabilitation (via NMST) improves long-term success.
Early progressive rehabilitation (i.e. 10-session NMST program) after the athlete achieves a quiet knee, is a hallmark of the Delaware-Oslo ACL study, and provides a model of care that improves upon current standard care following ACL rupture in athletes.10, 15 The two-year functional outcomes of participants in the Delaware-Oslo ACL cohort were superior to comparable samples from the US (MOON cohort) and Norway (National Knee Ligament Registry) who received standard care, that is ACLR and post-operative rehabilitation with criterion-based progression (Figure 1).10, 15 The current results extend these findings, adding that, within a sample of athletes who outperform those treated with standard care10, 15, athletes who demonstrate dynamic stability after NMST have 2.7 times the odds of success two-years after ACLR compared to non-copers. Taken together, these studies strongly support the addition of early progressive NMST prior to ACLR to standard care to improve the long-term success of our patients after ACL rupture.
Dynamic stability (i.e. being a potential coper) may be more important than mechanical stability (i.e. receiving an ACLR) for two-year success.
The rationale for ACLR after ACL rupture is to restore mechanical stability to the joint. Yet, the results of this study suggest that dynamic stability (potential coper vs. non-coper) was more important than mechanical stability (ACLR vs. Non-Op) for functional success two years later. Athletes who demonstrated good dynamic stability without mechanical stability had greater odds of long-term success compared to those had mechanical stability but poor dynamic stability. That is, athletes who were potential copers and chose Non-Op rehabilitation in lieu of ACLR had 2.9 times the odds of success compared to non-copers who received an ACLR. Within potential copers, we did not observe differences in outcomes between those who chose ACLR or Non-Op rehabilitation. These findings indicate that potential copers who choose non-operative management after NMST (i.e. prehabilitation) may succeed without an ACLR. The odds ratio for ACLR non-copers was 0.51, favoring ACLR, but the exceedingly small sample of non-copers who chose non-operative management leaves us unable to confidently make recommendations. This is consistent with other studies that similarly reported little difference in long-term outcomes between those who received ACLR and Non-Op rehabilitation.1, 6, 12–14, 19, 22 In this study, it is important to note that ACLR or Non-Op was not prescribed, rather the decision for surgical intervention was made by the athlete.
Alternative strategies are needed for persistent non-copers.
While about half of non-copers become potential copers following NMST, those who were non-copers after NMST had worse prognosis for success two years later. Further, despite early NMST and extensive Non-Op rehabilitation or ACLR with post-operative rehabilitation, 25% of the non-copers at baseline remained persistent non-copers at six-month follow-up (analysis not shown). Perhaps these athletes would respond to more intense rehabilitation or, alternate approaches need to be developed to improve stability, function, and long-term outcomes in this unresponsive subgroup.
Strengths and limitations.
A strength of this study is the long-term follow-up for this prospective, longitudinal observational cohort. However, we were limited by missing data and loss to follow-up at post-training (<10% missing) and two-year follow-up (<30% missing). This study also had other limitations. Success and failure were operationally defined. Failure at the two-year follow-up for this study was defined as not meeting the same level of knee function and symptoms (IKDC) relative to age-matched norms, an ACL graft rupture, or recurrent instability (≤ 1 episode of giving way). As a sensitivity analysis, we used patient acceptable symptom state21 for the IKDC threshold for failure instead of the age-matched norms, however the results were the same (Supplemental Table 1). The operational definitions of success and failure in this study were intended to reflect the general recovery of knee function to support activities of daily life. However, we recognize that this definition did not consider the patient’s perspective of success or failure, joint health, or level of return to sport. We did not conduct magnetic resonance images (MRIs) at the two-year follow-up, and thus were not able to identify new cartilage or meniscus damage. As reported in our previous work14, athletes who chose ACLR were more likely to return to level I sports and less likely to return to level II sports compared to those who chose Non-Op (Supplemental Table 2). When adjusting the analyses for activity level pre-injury or at two-year follow-up, the interpretation of the results did not change (Supplemental Table 3). Other patient specific factors, such as lifestyle choices, occupation, and psychological factors, likely play a role in these considerations, and were beyond the intended scope of this analysis.
CONCLUSION.
Coper classification can be changed with a 10-session NMST program early after ACL rupture, and robustly predicts the long-term outcome of the athlete. Specifically, athletes who demonstrate dynamic stability after NMST have the highest odds of success over two years later, regardless of their surgical status. For athletes who present initially as non-copers, a NMST program is warranted, as nearly half may become potential copers and thus have higher odds of long term success. Athletes who demonstrate persistent dynamic instability despite rehabilitation may require more intense rehabilitation in addition to ACLR, however further work is needed to determine the best course of action for persistent non-copers.
Supplementary Material
What is known about the subject:
Athletes who demonstrate dynamic stability and are classified as potential copers have better short-term outcomes after ACL rupture
Dynamic stability, defined with a coper classification, can change over one year after rehabilitation in athletes who are ACL deficient
What this study adds to existing knowledge:
Dynamic stability improves after a 10-session neuromuscular and strength training program early after ACL rupture
Potential copers after NMST are more likely to succeed than non-copers two years after ACL reconstruction or non-operative rehabilitation
Persistent non-copers, who continue to demonstrate instability despite surgery and rehabilitation, may need more intense intervention
REFERENCES
- 1.Ageberg E, Thomee R, Neeter C, Silbernagel KG, Roos EM. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two to five-year followup. Arthritis Rheum. 2008;59(12):1773–1779. [DOI] [PubMed] [Google Scholar]
- 2.Alkjær T, Henriksen M, Simonsen EB. Different knee joint loading patterns in ACL deficient copers and non-copers during walking. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):615–621. [DOI] [PubMed] [Google Scholar]
- 3.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34(1):128–135. [DOI] [PubMed] [Google Scholar]
- 4.Button K, van Deursen R, Price P. Recovery in functional non-copers following anterior cruciate ligament rupture as detected by gait kinematics. Phys Ther Sport. 2008;9(2):97–104. [DOI] [PubMed] [Google Scholar]
- 5.Chmielewski TL, Rudolph KS, Fitzgerald GK, Axe MJ, Snyder-Mackler L. Biomechanical evidence supporting a differential response to acute ACL injury. Clin Biomech (Bristol, Avon). 2001;16(7):586–591. [DOI] [PubMed] [Google Scholar]
- 6.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22(5):632–644. [DOI] [PubMed] [Google Scholar]
- 7.Eastlack ME, Axe MJ, Snyder-Mackler L. Laxity, instability, and functional outcome after ACL injury: copers versus noncopers. Med Sci Sports Exerc. 1999;31(2):210–215. [DOI] [PubMed] [Google Scholar]
- 8.Eitzen I, Eitzen TJ, Holm I, Snyder-Mackler L, Risberg MA. Anterior Cruciate Ligament—Deficient Potential Copers and Noncopers Reveal Different Isokinetic Quadriceps Strength Profiles in the Early Stage After Injury. Am J Sports Med. 2010;38(3):586–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2010;40(11):705–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Failla MJ, Logerstedt DS, Grindem H, et al. Does Extended Preoperative Rehabilitation Influence Outcomes 2 Years After ACL Reconstruction? Am J Sports Med. 2016;44(10):2608–2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2000;8(2):76–82. [DOI] [PubMed] [Google Scholar]
- 12.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A Randomized Trial of Treatment for Acute Anterior Cruciate Ligament Tears. N Engl J Med. 2010;363(4):331–342. [DOI] [PubMed] [Google Scholar]
- 13.Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ. 2013;346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grindem H, Eitzen I, Engebretsen L, Snyder-Mackler L, Risberg MA. Nonsurgical or Surgical Treatment of ACL Injuries: Knee Function, Sports Participation, and Knee Reinjury: The Delaware-Oslo ACL Cohort Study. J Bone Joint Surg Am. 2014;96(15):1233–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grindem H, Granan LP, Risberg MA, Engebretsen L, Snyder-Mackler L, Eitzen I. How does a combined preoperative and postoperative rehabilitation programme influence the outcome of ACL reconstruction 2 years after surgery? A comparison between patients in the Delaware-Oslo ACL Cohort and the Norwegian National Knee Ligament Registry. Br J Sports Med. 2015;49(6):385–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Houck JR, Wilding GE, Gupta R, De Haven KE, Maloney M. Analysis of EMG patterns of control subjects and subjects with ACL deficiency during an unanticipated walking cut task. Gait Posture. 2007;25(4):628–638. [DOI] [PubMed] [Google Scholar]
- 17.Hurd WJ, Axe MJ, Snyder-Mackler L. A 10-Year Prospective Trial of a Patient Management Algorithm and Screening Examination for Highly Active Individuals with ACL Injury. Part I: Outcomes. Am J Sports Med. 2008;36(1):40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Consortium M, Spindler KP. Risk Factors and Predictors of Subsequent ACL Injury in Either Knee After ACL Reconstruction:Prospective Analysis of 2488 Primary ACL Reconstructions From the MOON Cohort. Am J Sports Med. 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meuffels DE, Favejee MM, Vissers MM, Heijboer MP, Reijman M, Verhaar JA. Ten year follow-up study comparing conservative versus operative treatment of anterior cruciate ligament ruptures. A matched-pair analysis of high level athletes. Br J Sports Med. 2009;43(5):347–351. [DOI] [PubMed] [Google Scholar]
- 20.Moksnes H, Snyder-Mackler L, Risberg MA. Individuals With an Anterior Cruciate Ligament-Deficient Knee Classified as Noncopers May Be Candidates for Nonsurgical Rehabilitation. J Orthop Sports Phys Ther. 2008;38(10):586–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muller B, Yabroudi MA, Lynch A, et al. Defining Thresholds for the Patient Acceptable Symptom State for the IKDC Subjective Knee Form and KOOS for Patients Who Underwent ACL Reconstruction. Am J Sports Med. 2016;44(11):2820–2826. [DOI] [PubMed] [Google Scholar]
- 22.Myklebust G, Holm I, Mæhlum S, Engebretsen L, Bahr R. Clinical, Functional, and Radiologic Outcome in Team Handball Players 6 to 11 Years after Anterior Cruciate Ligament Injury. Am J Sports Med. 2003;31(6):981–989. [DOI] [PubMed] [Google Scholar]
- 23.Rudolph KS, Axe MJ, Buchanan TS, Scholz JP, Snyder-Mackler L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9(2):62–71. [DOI] [PubMed] [Google Scholar]
- 24.Rudolph KS, Eastlack ME, Axe MJ, Snyder-Mackler L. 1998 Basmajian Student Award Paper: Movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;8(6):349–362. [DOI] [PubMed] [Google Scholar]
- 25.Soltani N, Rahimi A, Naimi SS, Khademi K, Saeedi H. Studying the Balance of the Coper and Non-Coper ACL-Deficient Knee Subjects. Asian J Sports Med. 2014;5(2):91–98. [PMC free article] [PubMed] [Google Scholar]
- 26.Webster KE, Feller JA. Exploring the High Reinjury Rate in Younger Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44(11):2827–2832. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


