Abstract
Falls remain a major geriatric problem, and the search for new solutions continues. We investigated how existing fall prevention technology was experienced within nursing home nurses’ environment and workflow. Our NIH-funded study in an American nursing home was followed by a cultural learning exchange with a Dutch nursing home. We constructed two case reports from interview and observational data and compared the magnitude of falls, safety cultures, and technology characteristics and effectiveness. Falls were a high-magnitude problem at the US site, with a collectively vigilant safety culture attending to non-directional audible alarms; falls were a low-magnitude problem at the NL site which employed customizable, infrared sensors that directed text alerts to assigned staff members’ mobile devices in patient-centered care culture. Across cases, 1) a coordinated communication system was essential in facilitating effective fall prevention alert response, and 2) nursing home safety culture is tightly associated with the chosen technological system.
Keywords: Fall prevention, Long-term care, Monitoring technology, Position monitors, Bed exit alarms, Pressure sensor mats, Alarm fatigue
Introduction
Falls and related injuries are a global public health issue that is expected to worsen with increasing population aging. In developed countries up to half of all nursing home residents fall each year. Falls incur both direct costs to the healthcare system (nurse evaluation, hospitalization, emergency room visits, pain management, and rehabilitation) and indirect costs (informal caregiving and lost social participation from fear of falling).1 Although much is known about their multifactorial nature, falls remain a problem and the search for additional potential solutions continues, increasing in urgency as more medically complex older adults enter long-term care amid industry nursing shortages.2,3
As one compelling potential solution, fall prevention technology has yet to be examined within nursing home nurses’ environment and workflow. This is true despite the fact that technology is increasingly used in hospitals4 and long-term-care settings to monitor movement to prevent falls. Common devices in the US include inexpensive tab alarms (corded alarms that are clipped onto a resident’s clothing and sound when detached as a result of resident movement) and pressure sensitive mats (weight-sensitive sensor pads on beds or chairs that alarm when resident gets up; also called position monitors or bed monitors).5 Common devices in the Netherlands (NL) are infrared sensors in the resident’s room to alert caregivers of movement.6 Tab alarms, pressure sensitive mats, and infrared sensors are all static non-obtrusive approaches to alert caregivers of resident movement in what Hamm et al (2016)7 call pre-falls prevention intervention systems, in contrast to other technologies that provide cognitive or physical training for residents to remedy functional deficits or other technologies that alert staff when residents are on the ground. Unfortunately, research has not substantiated that these movement monitors reduce falls 8–10 or injury associated with falls.11,12 Nor have alternative technologies been recommended for effective use in fall prevention. Many of these potential fall prevention technologies are deemed “fall detection devices” because they typically notify staff of falls with too short notice for staff to arrive to prevent a fall.13
Our US research team sought to develop technology to predict bed exits based on physiological patterns. After receiving funding, we recognized that even dramatically improved technologies would necessitate understanding the nursing context in which they would be implemented. We therefore conducted a qualitative study focusing on existing technologies within nurses’ fall prevention practices at the study site where the prediction technology was being tested. A subsequent cultural learning exchange with the NL long-term care system Stichting Zorgcombinatorie Marga Klompe (SZMK) in Eastern Netherlands, provided an opportunity to replicate the investigation at a NL nursing home. The objective of this study was to examine how existing fall prevention technology was experienced within nursing home nurses’ environment and workflow. Doing so at two very different nursing home sites in the United States (US) and the Netherlands (NL) was designed to maximize differences to potentially introduce new ways of framing care problems and new ways of solving them.
Methods
We used a case study approach with a multiple-case (holistic) research design, following Yin (1984),14 in order to examine nurses’ experience of technology in fall prevention within two distinct and bounded systems (i.e., cases).15 We used a convenience sample of two nursing homes. The study protocols were approved by the Emory University Institutional Review Board. The lead author researcher was present at both case study sites.
Sample
Case 1 (US site)
An initial study at a 168-bed nonprofit academic teaching nursing home in Atlanta, Georgia, United States, was conducted in May 2013. The home had a superlative rating from US Nursing Home Compare.16 Study participants included site administrators (the administrator and assistant administrator), nurse managers (unit managers, licensed practical nurses (LPNs)) and registered nurses (RNs)), and direct care nurses (certified nursing assistants (CNAs)).
Case 2 (NL site)
A replication of the study at a 152-bed nursing home in Win-terswijk, Netherlands occurred in May 2014. The home had a superlative rating from the NL Ministry of Health, Welfare and Sport.17 Finding equivalent focus group populations was challenging because of differing nurse educational systems in the two nations. There was no Dutch equivalent to a CNA, an entry level nursing position that requires no more than a high school diploma and 8 weeks of training but whose role is to assist residents with their activities of daily living, take vital signs and inform the licensed nurse of any changes in resident health or function. The Dutch nursing system has five levels, or niveaux, and it was determined through discussions with administrators and staff that the niveau 3 mid-level nurse had the most overlap with the American CNAs, although they receive a full three years of training. The niveau 4 and 5 nurses that we included in our nurse manager group had supervisory roles and were therefore considered equivalent to the US unit managers.
Focus group participants were selected by the site administrator depending on employee availability. Each potential participant was presented a consent form emphasizing that participation was voluntary and was then offered the opportunity to sign and participate. Consistent with local customs, monetary incentives (US $15) and lunch were offered at the US site only.
Data collection
Data included staff interview data, observations, and facility records. At each site we first conducted two 90 minute in-depth interviews with administrators to obtain an overview of policies, procedures, and personnel in place to deal with falls, as well as to ask permission and help in recruiting nurse participants for focus groups. We then conducted two 90 min focus groups with nurses of different levels, using a common interview guide; questions and sample probes are displayed in Table 1. All interviews were conducted in native languages except in the case of the first Dutch administrator interview which was conducted by the lead author in English. All focus group participants completed brief questionnaires identifying background characteristics. Finally, the lead author wrote field notes on several site visits.
Table 1.
Focus group guide.
| Question | Sample probes |
|---|---|
| 1. What experiences have each of you had here with resident falls? | Particular falls? Warning signs? Frequency of falls? Impact of falls? |
| 2. As a staff person working here, what responsibilities do you have with regard to falls? | Monitoring of residents? Reporting falls? Fall prevention? |
| 3. How big a task is preventing falls in terms of your other work duties? | Effort involved? Priorities in terms of rest of work? Effect on workflow? |
| 4. What tools a do you use that give you information about residents? | Types of systems? Kind of information received? Problems with the tools? |
| 5. What tools do you use to deal with falls? | For prevention? Advantages of these tools? Problem with these tools? |
| 6. Can you imagine technology would be useful to help you prevent a fall? | Type? Modality? Location? |
From technology to low-tech tools.
Analysis
Cases were analyzed separately to understand how each bounded system functioned on its own terms but in relation to the same interview questions. Extensive discussion and debriefing occurred following each focus group with research teams in US and NL. Individual and group interviews were recorded and transcribed verbatim. Two authors (VO and BV), working with another (AV), translated the Dutch transcripts into English.
Magnitude of the problem of falling, safety cultures, technological systems, and technological effectiveness were characterized in descriptive case reports, triangulating across multiple information sources within cases (administrator interviews, direct care staff focus groups, nurse manager focus groups, and observations) to establish themes. Case reports were then compared to establish cross-case patterns. In addition to deep engagement with the transcripts, the first two researchers met biweekly to discuss findings, challenging and informing the ongoing analysis and increasing credibility of the results. Finally, we re-visited each site to observe or discuss technology with staff following focus group sessions to confirm our understanding.
Results
The two cases differed in terms of environment – configuration, patient mix, and staffing ratios – but both similarly faced market pressures. The US facility had six care units in a seven-story high-rise, with 37% of its residents in long-term care (including those with dementia) and 63% in shorter-term care in the form of sub-acute rehabilitation, reimbursable by Medicare. The US administrator reported market pressures to increase the share of sub-acute care delivered.
In contrast, the NL site combined an old-style two-story ward (recently divided into smaller 10-room units with their own living rooms within each floor) with a cluster of ten small-scale houses for dementia residents (six in each) around an adjacent garden. There were three care units: psychogeriatric long-term care (47% of the patient mix), somatic long-term care (32%), and rehabilitation shorter-term care (21%). The NL nursing homecare was reimbursed in all cases by the Exceptional Medication Expenses Act or the Health Insurance Act. However, the NL administrator reported market pressures from competition with other health care systems for dwindling numbers of patients in a system increasingly moving towards home health delivery.
The two cases were of roughly equivalent sizes in terms of overall nursing staff and high proportion of female workers. Site 1 had 147 full-time equivalencies (FTEs), compared with 151 FTEs at site 2. The sites reflected regional differences, with a part-time female work culture at the NL site and an underrepresented minority nursing home work culture at the US site, in addition to differences in nursing levels and training already described. Staffing ratios were lower at the US site than the NL site during the day but higher at night. For example, during the day at the US 1 CNA cared for about 10 dementia residents, compared, at the NL site, to 1 niveau 3 nurse caring for six dementia residents. However, at night 1 US CNA cared for about 15 residents, compared, at the NL site, to one niveau 3 nurse caring for 36 dementia residents spread across 6 small buildings.
Study participant characteristics are detailed in Table 2. The focus group samples differed by race, by age (with a younger NL sample), by shift (with more US site staff assigned to the day shift), and by years in position (more years management but fewer years in direct care in the NL sample).
Table 2.
Participant characteristics.
| US administrators (n = 2) |
US focus group 1 (nurse managers) (n = 5) |
US focus group 2 (direct care) (n = 6) |
NL administrators (n = 2) |
NL focus group 1 (nurse managers) (n = 6) |
NL focus group 2 (direct care) (n = 6) |
|
|---|---|---|---|---|---|---|
| Gender | 1 female | 4 female | 6 female | 1 female | 2 female | 6 female |
| Race | 2 white | 5 black | 6 black | 2 white | 6 white | 6 white |
| Age | 1 > 50 | 4 age 30–49 1 > 50 |
3 age 30–49 3 > 50 |
1 > 50 | 1 < 30 3 age 30–49 2 age 50+ |
2 < 30 4 age 30–49 |
| Job title | 1 administrator; 1 assistant administrator |
2 RNsa 3 LPNsb |
6 CNAsc | 1 sector chief; 1 care development manager |
3 niveau 4 3 niveau 5 |
6 niveau 3 |
| Employment status | 2 full time | 100% full time | 100% full time | 2 full time | 67% full time 33% part time |
17% full time 83% part time |
| Shift | 2 day | 100% – day | 83% – dayd | 2 day | 33% – day 67% – all (day, evening, night) |
100% – all (day, evening, night) |
| Years in position (mean) | 5 | 9 | 13 | 10.5 | 12 | 10 |
| Years in long-term care (mean) | 21 | 22 | 21 | 12 | 18 | 14 |
Note: All categories but race were self-reported by focus group participants. Race was assessed visually by researcher.
Registered nurses.
Licensed practical nurses.
Certified nursing assistants.
One respondent did not answer the question.
Table 3 details fall prevention strategies and tools reported by participants. Strategies used by both sites were low beds and mats beside beds (physical environment strategies); rounding, supporting residents in walking, and using restraints as necessary and legal (care process strategies); and the call bell system (technology strategies). Contextualized strategies are described for each site below.
Table 3.
Fall prevention strategies and tools.a
| Description | Within US site |
Within NL site |
|---|---|---|
| Physical environment | ||
| Low beds and mats beside beds | Yes | Yes |
| Small unit building design | No | Yes |
| Relocating residents close to nurses’station in large wards | Yes | No |
| Clear and dry physical environment | No | Yes |
| Visual indicators of high fall risk (signage) | Yes | No |
| Care processes | ||
| Monitor rooms in person (rounding) | Yes | Yes |
| Support residents in walking to avoid environmental hazards | Yes | Yes |
| Use restraints as necessary and legal | Yes | Yes |
| Use equipment properly (e.g., lifts) | No | Yes |
| Technology | ||
| Call bell system | Yes | Yes |
| Position and clip-on monitors | Yes | No |
| Mobile infrared sensors (Wakend Oog) | No | Yes |
| Beepers, pagers, DECT phone | No | Yes |
| Cameras in common areas | No | Yes |
Reported by at least two of three response groups.
US site: “Everybody’s supposed to be listening”
Both US administrators used the term “huge” to describe the issue of falls. The assistant administrator noted an inability to change fall rates and, despite a low injury rate, the ever-present potential for a complaint survey or litigation with any injury. Licensed nursing staff perceived falls to be common. Direct care staff were emotionally shaken by their experiences with falling residents, often describing witnessed falls or resident fall-related injuries in graphic terms; four out of six of CNAs described these experiences as “frightening.”
Three types of residents were identified as high fall risk: residents with dementia, residents under the influence of anesthesia, and rehabilitation residents who misjudge their capabilities. Among all strategies mentioned to prevent falls in these high-risk residents (see Table 3), four were mentioned by all groups: removing a motivation for movement through pre-emptive toileting; preventing the possibility of falling from a height by using low beds; alerting staff to resident movement with position monitors; and increasing visibility of residents by relocating them close to the nursing station. An approach mentioned by two groups was communicating high fall risk with bright yellow visual indicators, such as a falling star on resident doors, “grippy socks” on resident feet, and blankets on resident beds or laps.
Nursing staff described a safety culture of constant and communal vigilance towards residents who were at high risk for falling. All groups mentioned relocating these residents closer to the nurses’ station, where all staff share the task of observing them. As one CNA stated, “It takes everyone to watch that person.” A nurse manager reported that “if we have someone on the unit who’s fallen frequently I’ll call it on the floor, ‘All hands on deck.’” A CNA put it in terms of shared responsibility: “It’s everybody’s responsibility. So that’s why we all try to make sure we monitor and make sure we don’t have any falls because it’s a reflection on us, you know, as if we’re not really doing our job.” In addition to watching residents in person, CNAs acknowledged that they are constantly listening for position monitors to sound as required (one nurse manager stated, “Everybody’s supposed to be listening”).
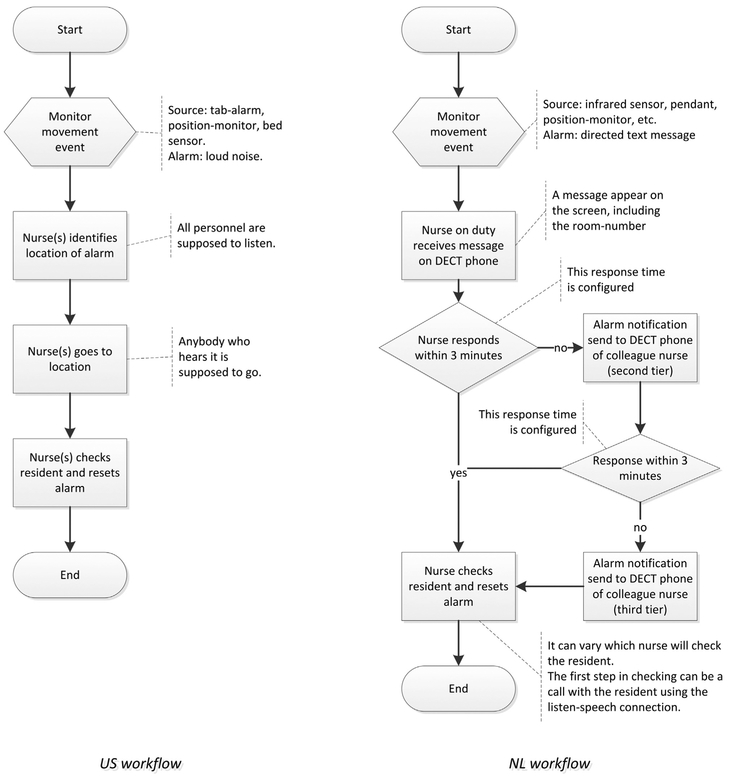
The key resident monitoring technology, position monitors, were described as stand-alone devices emitting “penetrating” alarms that sound at the site of the body, without connecting to any other communication system. As a result, staff rely on their senses and judgment and cannot coordinate care. Two LPNs depicted a moment of hesitation after the sounding of an alarm, one stating: “A lot of times you’re standing in the middle of the hall trying to figure out where it’s coming from.” An alarm can provoke chaos among the staff. As one CNA said, “Everybody’s heading in the same direction, coming from different directions,” leaving other residents unattended. There was general consensus that staff cannot tell who was taking care of the problem until arriving on the scene (see Figs. 1 and 2, left panels). An LPN explained that some staff use the call bell system as a paging system to locate and summon help. The assistant administrator summed up workflow problems as serious; a fall results in “huge down time, … whether it’s major or minor.” In addition to not allowing care delegation or coordination, stand-alone position monitors had other problems and were faulted for breaking easily, being easy to dismantle by residents, providing a signal that was too late to prevent falls, and emitting a piercing noise that inhibited movement or caused agitation in residents and haunted staff after they went home. In response to workflow problems, focus group members discussed a need for more staffing and were generally suspicious of potential technological solutions such as cameras that they felt could be used to blame staff for wrong-doing.
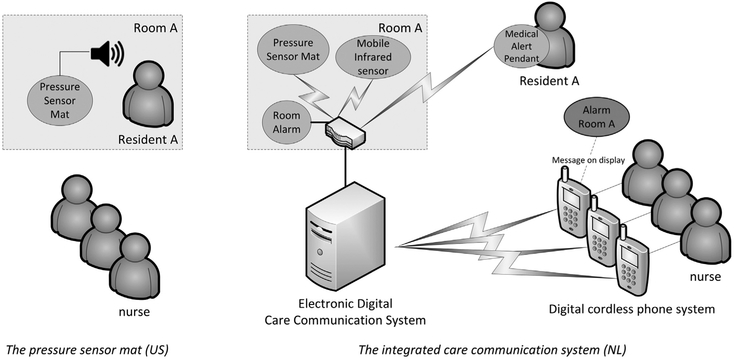
Fig. 1.
Resident monitoring technology at US and Netherlands (NL) sites. At the US site (left), the main fall prevention instrument used is the pressure sensor mat, which is positioned on the chair or bed of high fall risk residents. The sensor is activated when a resident tries to get up. The alarm is a loud sound that is heard by the nurses (and residents). At the NL site (right), each resident room is equipped with a communication module mounted on the wall; this module is part of a monitoring and communication system and has a wired connection to an electronic digital care system. The communication module is equipped with listen-speech functionality and, depending on needs and desires, additional systems can be connected wirelessly to this communication module. An example is a mobile infrared sensor (wakend oog or “watching eye”) used to detect when residents try to get out of bed. Other types of systems that can be connected wirelessly are a wearable emergency alert pendant and a sound sensor that can be used at night to send alarms when it detects unusual sound levels. The monitoring system is installed in a way that suits the monitoring needs of a particular resident. The wakend oog, for instance, can be placed at virtually any desirable place in the room, and the device settings can be varied for different conditions, making the system highly personalized. Once the monitoring system generates an alarm (silent), the event is communicated via the electronic digital care system to a designated DECT telephone (a European-standard digital cordless phone system). A nurse carries the phone and receives alarm text messages that display the room number of the associated alarm. From here three different reactions follow: 1. The nurse presses a button on the phone and goes to the indicated room to give assistance. 2. The nurse calls the room (via a speech-listen connection) to talk to the resident (e.g., explaining that assistance is on its way). 3. The nurse does not react to the alarm. In the third case, the electronic care system detects a non-response and after 3 min reroutes the alarm to a second unit of staff; if a second non-response is detected, additional units of staff area alerted.
Fig. 2.
Nursing workflow in response to resident movement notification.
NL site: “I just feel normal, during the night shift too.”
In contrast to the US staff, 4 of 6 direct care workers and 2 of 6 nursing managers at the NL site said that they had rarely encountered falls. This view was not expressed by any US site participant. In addition there was a more relaxed attitude towards falling from the management. The administrator stated that the problem of falling was “less important than medication failures” and “less important than taking people’s freedom away.” One niveau 3 nurse stated that when residents fell “nine times out of ten they were in really good shape too … And those people almost considered it normal to happen, so yeah, it did not really have a big impact.”
Similar to the US staff, NL staff described people at risk for falls as those with dementia, residents under the influence of anesthesia, and rehabilitation residents who misjudge their capabilities. Among fall prevention strategies mentioned (see Table 3), four reported by all three response groups were getting to know residents to intervene individually to prevent falling; making agreements with residents to determine preference for freedom versus protection and developing a care plan accordingly; preventing the possibility of falling from a height by using low beds; and using an integrated care communication system to gain information that is useful in preventing resident falling.
Nursing staff described a safety culture of individualized care with delegated and coordinated responsibilities enabled by their technology and care unit configuration. It begins with making agreements with residents about the tradeoff between safety and freedom. Residents and their families who want more freedom agree to accept risk; residents and families who want more safety agree to accept more limitations on privacy and freedom of movement. These agreements are recorded in the resident care plan. Examples given were expressing the wish to walk independently without help or to lock bedroom doors at night rather than have staff check on them. Non-injurious falls of those who had accepted risk are not recorded as fall incidents because they were expected. Beyond making agreements with residents, nurses are connected to the various alarm systems of assigned residents through a mobile device. These alarm systems can be customized in various ways by nurses based on their knowledge of resident behavior. Participants in both focus groups also mentioned a move towards small-unit building design (units for 6–10 people) in the early 2000s as facilitating better fall management; with small-scale living, one nurse manager said, “you know people very well” and the administrator said, “it’s quiet, it’s easy to see what’s happening, and people are familiar to each other, so there’s more peace.”
In terms of technology, the NL site had eliminated position monitors (belmatje) (which they never used as audible, non-directional alarms) because of too many false alarms and device failures. Instead, NL staff use an approximately 6″ high mobile infrared sensor called the wakend oog (“watching eye”) to detect movement. The sensor can be positioned differently depending on the resident’s fall risk and movement speed: on a bed’s headboard (aimed at the rising torso), on the side of the bed (aimed at the limbs extending over the edge of the bed), on the floor (showing feet touching ground), or at the door (indicating exit from the room). Alarms generated are directed silently to the assigned nurses’ mobile phone device. Other room alarms such as medical alert consoles by the door are directed in a similar silent fashion to nurse mobile phones. If unit staff do not respond to alarms, nursing staff of the second closest unit are alerted, and if these do not respond, nursing staff at multiple other units are alerted (see Figs. 1 and 2, right panels). In addition, nurses in psychogeriatric units can see the common areas of ten small homes displayed at the same time at night when all the cameras are on. These technologies extend the nurses’ field of information without requiring travel through the environment.
The NL integrated technology supports delegation and coordination of care and was generally well accepted by the nurses. One nurse manager from the rehabilitation unit stated that the mobile device made it so that “I am always reachable. I just feel normal, during the night shift too. It’s safe if you have it with you. You know … you have it always in your pocket wherever you go. So it’s more security, familiarity.” Staff in both focus groups who were working outside of psychogeriatrics wished for cameras for their units, and some psychogeriatrics staff wished for an expansion of cameras from public to private areas.
Discussion
Our work examined the magnitude of the problem of falling, safety cultures, technological systems, and technological effectiveness at two nursing homes in the US and the NL, revealing starkly different institutional experiences. Participants at the US site experienced falls as a high-magnitude problem, safety culture as requiring constant and collective vigilance, and stand-alone fall prevention technologies as producing noise, resident agitation, and workflow chaos. Participants at the NL site, in contrast, experienced falls as a low-magnitude problem, safety culture as built around individual person-centered care, technology as customizable to the individual resident and caregiver, providing controlled and organized response.
Two cross-case patterns emerged. First, a coordinated communication system was essential in facilitating effective fall prevention alert response. At the US site where alarms were not directed to particular nurses, nurses were diverted rather than enabled by their technology to care for residents. They expressed creative work arounds for communicating with each other, such as using the call bell system to page staff and indicate their location and marking or flagging high fall risk residents visually with yellow indicators or positioning them for high visibility within the physical environment. Although nursing staff sought solutions through increased staffing and were suspicious of technology, these same needs could be met through the integrated care communication system described by the NL nurses, which effectively coordinated care.
Second, nursing home safety culture is tightly associated with the chosen technological system. Because the US site’s system was built around uncoordinated alarms, staff had developed a culture of constant, collective vigilance in listening for alarms, and they simultaneously rushed towards potential crises and away from patients being tended, disrupting workflow. Despite the fact that US staff cared passionately about knowing their patients and addressing individualized needs, they felt responsible and worried about receiving blame for lack of attention to the alarm. In contrast, use of the customizable wakend oog at the NL site dovetailed policies of individualized care. NL staff described technology as enabling them to do their work in caring for residents in a calm and peaceful way. Decision makers calling for patient-centered care 18 need to consider the role of technology in delivering or impeding that care.
The study points to the value of case studies in health services research. Unexamined environments tend to be taken for granted, and getting outside one’s environment is not usually a readily available option. A cross-cultural two-case study presents an especially useful method through which to examine ingrained and potentially detrimental care assumptions. Not only can environments be changed but environmental change is particularly powerful in having the potential to impact an entire resident population. It is clear that audible undirected position monitor alarms were taken for granted at the US site environment, despite the fact that research has not substantiated that these monitors reduce falls 5,8,10 or injury associated with falls 11,12 and despite longtime practitioner calls for their elimination.19–21 In addition, the nursing station remains a fixture of coordination, a site to place high-risk residents for high visibility despite its trafficked, noisy, and public nature. In an environment without position monitors or nursing stations, equipped instead with wakend oog sensors connected to assigned staff beepers, and cameras in common areas for dementia care, NL nursing staff had enhanced monitoring capabilities for distant residents while retaining focus on residents at hand.
A real strength of this study was that the interviews, initial coding, and analysis were conducted by native speakers working with informants in their native languages, where regional nuances could be captured and analyzed. Deeper exploration of structural differences, including financial, cultural, and legal factors, is important for understanding barriers to suggested solutions. As costs mount under the Dutch system of national insurance for long term care and high labor costs (considerably higher than in the US, given training levels involved), there has been strong motivation to develop cost savings strategies to care such as labor-saving technology.2 Silent infrared sensors such as the wakend oog, along with cameras in psychogeriatric units, appear common, in part to handle low staffing at night.6 Sensor implementation also fits well with a policy emphasis on reducing restraint use and promoting freedom of movement in long-term care.22 In the United States, infrared sensors have been in existence since at least the 1980s with some evidence that they reduce falls.23 At present, all existing nursing home fall prevention technology remains reactive to rather than predictive of falls. The findings of this exploratory study point the way to additional research to quantify the prevalence of alarm types in each country, along with associated fall rates at a representative sample of nursing homes.
Conclusions
Our comparative cross-cultural case study of one US and one NL nursing home revealed two distinct safety cultures, with differing degrees of workflow ease in preventing and managing resident falls associated with different technologies. While the US site, employing a system of monitors positioned under and emitting alarms within the vicinity of the resident’s body, had developed a listen-and-scramble strategy within a large physical environment, the NL site, equipped with an integrated and customizable care system that detected movement and notified delegated care staff wherever they were through individual beepers, facilitated concentrated care for residents and help with dangerous situations as needed. Beyond such findings, the study points to the value of comparative cross-cultural case studies in challenging assumptions about care environments.
Acknowledgment
This project is an outgrowth of a project originally intended to develop a nonintrusive bed exit technology for nursing homes. In the process we recognized that any new technologies would work better if sensitivity to nurses and their long-term-care work were understood. Our sponsors did not contribute to study design, collection, analysis, interpretation of data, writing of the report, or the decision to submit our manuscript for publication. However, we would like to acknowledge Thomas Whalen, Murray Cohen, Zobair Nagamia, and Manuel Eskildsen for their contributions in providing the impetus for this project. We would also like to acknowledge Molly Perkins for her guidance and the Marga Klompe Healthcare Foundation for their generous support and participation in this investigation. Funding: This work was supported by the National Institute on Aging (SBIR 1 R43 AG042237-01 to T.W. of CDIC, Inc.).
Footnotes
Conflicts of interest: None.
References
- 1.World Health Organization. WHO Global Report on Falls Prevention in Older Age: Epidemiology of Falls. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 2.Smits CH, Van den Beld HK, Aartsen MJ, Schroots JF. Aging in The Netherlands: state of the art and science. Gerontologist. 2013;54:335–343. 10.1093/geront/gnt096. [DOI] [PubMed] [Google Scholar]
- 3.Tak SH, Benefield L, Mahoney DF. Technology for long-term care. Res Gerontol Nurs. 2010;3(10):61–72. 10.3928/19404921-20091103-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shrever LL, Titler MG, Mackin ML, Kueny A. Fall prevention practices in adult medical-surgical nursing units described by nurse managers. West J Nurs Res. 2011;33:385–397. 10.1177/0193945910379217. [DOI] [PubMed] [Google Scholar]
- 5.Rubenstein LZ, Josephson KR, Osterweil D. Falls and fall prevention in the nursing home. Clin Geriatr Med. 1996;12:881–902. [PubMed] [Google Scholar]
- 6.Schikhof Y, Mulder I, Choenni S. Who will watch (over) me? Humane monitoring in dementia care. Int J Hum Comput Stud. 2010;68:410–422. 10.1016/j.ijhcs.2010.02.002. [DOI] [Google Scholar]
- 7.Hamm J, Money AG, Atwal A, Paraskevopoulos I. Fall prevention intervention technologies: a conceptual framework and survey of the state of the art. J Biomed Inform. 2016;59:319–345. 10.1016/j.jbi.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Choi Y-S, Lawler E, Boenecke CA, Ponatoski ER, Zimring CM. Developing a multi-systemic fall prevention model, incorporating the physical environment, the care process and technology: a systematic review. J Adv Nurs. 2011;67: 2501–2524. 10.1111/j.1365-2648.2011.05672.x. [DOI] [PubMed] [Google Scholar]
- 9.Kosse NM, Brands K, Bauer JM, Hortobagyi T, Lamoth CJC. Sensor technologies aiming at fall prevention in institutionalized old adults: a synthesis of current knowledge. Int J Med Inf. 2013;82:743–752. 10.1016/j.ijmedinf.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Shorr RL, Chandler AM, Mlon LC, et al. Effects of an intervention to increase bed alarm use to prevent falls in hospitalized patients. Ann Intern Med. 2012;157: 692–699. 10.7326/0003-4819-157-10-201211200-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson O, Boshier PR, Hanna GB. Interventions designed to prevent healthcare bed-related injuries in patients. Cochrane Databaase Syst Rev; 2012;CD008931 10.1002/14651858.CD008931.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Capezuti E, Brush BL, Lane S, Rabinowitz HR, Secic M. Bed-exit alarm effectiveness. Arch Gerontol Geriatr. 2009;49:27–31. 10.1016/j.archger.2008.04.007. Epub 2008 Jun 3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaudhuri S, Thompson H, Demiris G. Fall detection devices and their use with older adults: a systematic review. J GeriatrPhys Ther. 2014;37:178–196. 10.1519/JPT.0b013e3182abe779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yin RK. Case Study Research: Design and Methods. Beverly Hills, CA: Sage Publications Inc.; 1984. [Google Scholar]
- 15.Stake R The Art of Case Study Research. Thousand Oaks, CA: Sage Publications Inc.; 1998. [Google Scholar]
- 16.Centers for Medicare and Medicaid. Nursing Home Compare, https://www.medicare.gov/nursinghomecompare/search.html; 2013. Accessed 13 June 2013.
- 17.Inspectie voor de Gezondheidszorg, Ministerie van Volksgezondheid, Welzijn en Sport. Kwaliteitsdocument2013 Verpleging. Verzorgin en ZorgThuis, http://www.igz.nl/Images/Kwaliteitsdocument-VVT-2013_tcm294-329148.pdf; 2013. Accessed 07 February 2016. [Google Scholar]
- 18.Weil AR. The patient engagement imperative. Health Aff. 2016;35(4):563 10.1377/hlthaff.2016.0337. [DOI] [PubMed] [Google Scholar]
- 19.Masspro, Quality Improvement Organization for Massachusetts. Nursing Home Alarm Elimination Program: It’s Possible to Reduce Falls by Eliminating Resident Alarms, https://www.pioneernetwork.net/Data/Documents/Alarm%20Elim%20C%2020Sep%202006.pdf; 2006. Accessed 07 June 2016.
- 20.Rader J, Frank B, Brady C. Rethinking the Use of Position Change Alarms, http://www.healthandwelfare.idaho.gov/LinkClick.aspx?fileticket=Dbip2Pr9SdI%3D&tabid=281&mid=2432; 2007. Accessed 07 June 2016.
- 21.Bressler K, Redbern RE, Brown M. Elimination of position-change alarms in an Alzheimer’s and dementia long-term care facility. Am J Alzheimers Dis. 2011;26: 599–605. 10.1177/1533317511432730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The NetherlandsOrganisation for Economic Cooperation and Development, http://www.oecd.org/els/health-systems/Netherlands-OECD-EC-Good-Time-in-Old-Age.pdf; 2013. Accessed 25 February 2016.
- 23.Dubner NP, Creech R. Using infrared scanning to decrease nighttime falls on a psychogeriatric unit. Hosp Community Psychiatry. 1988;39:79–81. [DOI] [PubMed] [Google Scholar]