Abstract
Purpose
As many as 3 million US residents are injured in traffic-related incidents every year leaving many victims with disabling conditions. To date, limited numbers of studies have examined the effects of traffic-related injuries on self-reported health. This study aims to examine the association between health-related quality of life (HRQOL) and traffic-related injuries longitudinally in a nationally representative sample of US adult population.
Methods/approach
This is a longitudinal study of adult participants (age≥C18) from seven panels (2000–2007) of the Medical Expenditure Panel Survey. The dependent variables included the physical and mental components of the SF-12, a measure of self-reported health. The outcome was assessed twice during the follow-up period: round 2 (~4–5 months into the study) and round 4 (~18 months into the study) for 62,298 individuals. Two methods estimate the association between traffic-related injuries and HRQOL: a within person change using paired tests and a between person change using multivariable regression adjusting for age, sex, income and educational level. Results Nine hundred and ninety-three participants reported traffic-related injuries during the follow-up period. Compared to their pre-crash HRQOL, these participants lost 2.7 of the physical component score while their mental component did not change. Adjusted results showed significant deficits in the physical component (−2.84, p value = <.001) but not the mental component (−0.07, p value = .83) of HRQOL after controlling for potential confounders.
Conclusion
Traffic injuries were significantly associated with the physical component of HRQOL. These findings highlight the individual and societal burden associated with motor vehicle crash-related disability in the United States.
Keywords: Motor vehicle crashes, SF-12, Health-related quality of life, Injuries
Introduction
Motor vehicle injuries are among the leading causes of morbidity and mortality worldwide. According to the World Health Organization, as many as 50 million individuals are injured in motor vehicle crashes across the world every year, and this number is expected to increase into the foreseeable future due to the expansion of motor vehicle transportation globally [1]. A recent report of the Global Burden of Disease 2010 indicates that traffic injuries ranked 10th as a cause of disability adjusted life years globally compared to 12th in 1990 [2]. While many lives are saved due to advances in trauma prevention, emergency medical services, and medical care, those who survive motor vehicle injuries often experience long-term disability. The National Highway Traffic Administration estimates that about 3 million US residents are injured in traffic-related incidents every year [3]. In 1995, researchers from the CDC estimated that over 1.2 million adults were living with long-term disabilities due to traffic crashes [5]. Health-related quality of life (HRQOL) is a measure of health status that incorporates self-reported functioning and perception of health [4]. Individuals surviving serious trauma are likely to have significant decrements in their HRQOL [6–10], perhaps comparable to the decrements associated with diseases such as diabetes and stroke.
Despite the importance of motor vehicle-related injuries as a public-health problem, most focus on mortality rates or years of life lost, and relatively, few studies have examined their effects on HRQOL [12]. In contrast, there is an extensive literature on the effects on HRQOL of other chronic and acute health conditions [5, 13, 14, 30–32, 36–38, 40]. While a number of studies have looked at HRQOL following injuries, these studies lack methodological rigor and few focus specifically on automobile-related injuries [6, 15–20, 32–34].
The objectives of the present study are to investigate in a nationally representative sample of the US civilian, non-institutionalized, adult population: (1) HRQOL after traffic injuries among injured persons relative to their pre-crash HRQOL; and (2) changes over time in both physical and mental HRQOL in persons reporting health conditions due to motor vehicles injuries compared to such changes in a control population not reporting motor vehicle injury-related health conditions. For the second objective, it is important to adjust for factors that may confound the association between motor vehicle injuries and changes in HRQOL, such as age, gender, income and education.
Methods
Dataset
The Medical Expenditure Panel Survey (MEPS) is a nationally representative, longitudinal survey of health care use, expenditures, sources of payment, and insurance coverage of the US civilian non-institutionalized population [22]. For the present study, we used panels 5–11 of the MEPS from years 2000 to 2007. Every year, the MEPS selects a new probability sample of approximately 15,000 households, representing one panel, which is then followed longitudinally. Each longitudinal survey includes five rounds of interviews spaced 4–5 months apart during two full calendar years. The MEPS comprises several data files covering areas such as expenditures, demographics, health status, and medical conditions.
For the purpose of this analysis, we combined two data files: the medical conditions file and the individual characteristics file. The medical conditions file lists health conditions reported by respondents during each round of the study, and using this file we created an indicator variable for motor vehicle-related injuries. The individual characteristics file includes demographics and the measures of HRQOL, which are obtained twice during follow-up.
Exposure measure
Injury definition
In the MEPS dataset, injury is defined as a “physical problem that arose from some sort of external trauma to the body such as a fall.” According to this definition, physical damage is necessary for a health condition to qualify as an injury, and other important consequences of traumatic events, such as enduring psychological effects (including post-traumatic stress disorder), are distinct from the physical injuries. At the same time, physical injuries, as defined above, may affect both the physical and mental dimensions of HRQOL.
Motor vehicle-related injuries in the MEPS
Within the field of injury prevention and control, the causes of injury are classified by the mechanism leading to energy exchange resulting in tissue damage, and motor vehicle crashes are among the most common mechanisms of severe injury [47, 49]. A health condition in the MEPS can be identified from the reason reported by the respondent for a particular medical event (hospital stay, outpatient visit, emergency room visit, home health episode, prescribed medication purchase, or medical provider visit). In addition, the condition may be reported as the reason for one or more episodes of disability days or even as a condition “bothering” the person during the reference period. We are unable to examine conditions by the reason they were reported (i.e., hospital stay vs. just bothering the respondent).
Respondents reporting a medical condition are asked whether the condition was due to an injury. For those reporting injuries, a further question asked whether the injury involved a motor vehicle. Some of the other mechanisms of injury reported in the MEPS are falls, weapons, poisoning, and sport injuries. In 2008, the MEPS survey did not ask whether the injury involved motor vehicles or other mechanisms; therefore, 2007 is the latest year included in the present study.
Outcomes of interest
The outcomes of interest are obtained from the Short Form 12 (SF-12) instrument [22, 23]. The SF-12 encompasses eight domains: physical functioning, role limitation due to physical problems, bodily pain, vitality, general health, social functioning, role limitation due to mental problems, and mental health. The specific outcomes of interest include the Physical Components Score (PCS) and the Mental Component Score (MCS). Values for these two summary scores can each range from 0 to 100 with lower scores indicating poorer HRQOL. The PCS and MCS are standardized to have a mean 50 and standard deviation 10. The SF-12 has been used extensively for measuring the association between health conditions and HRQOL, and evidence of its validity and reliability has been reported in previous studies [23–26, 39].
Participant selection
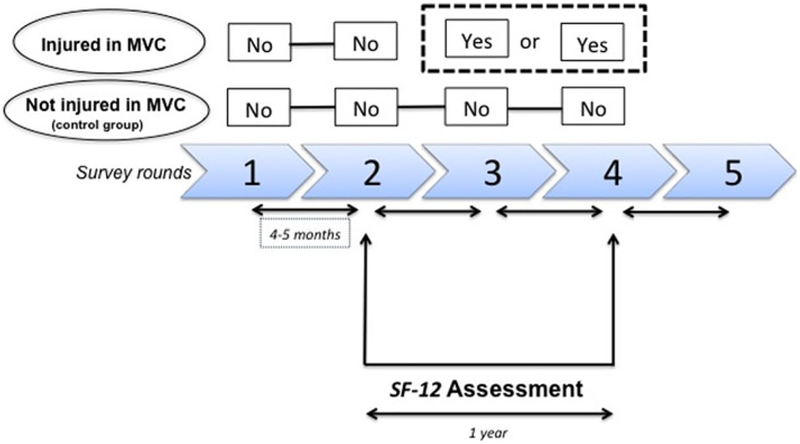
The study was limited to those who are age 18 and older, as quality of life measures are not collected by MEPS for younger ages. In order to maximize our sample, we pooled all years for which quality of life measures were available (2000–2007). Within this pooled dataset, each subject is surveyed five times during the follow-up period and asked about health conditions, expenditures, and utilization (Fig. 1). At each round, respondents are asked whether they had any health condition since the last time they were surveyed [22].
Fig. 1.
Classification of the comparison groups: MVC-injured and control group
The quality of life instruments were administered twice during the follow-up study (rounds 2 and 4) using Self-Administered Questionnaires (SAQ) of the MEPS (Fig. 1). Therefore, for those reporting injuries in round 3 and/or 4, baseline health status at round 2 is available as a measure of health before injury occurrence to be compared to a health measure after potentially reporting an injury (at round 4). Time lag from the injury to the administration of round 4 cannot be more than approximately 9 months (i.e., if an injury was sustained immediately after answering the round 2 questionnaire, the maximum time to round 4 administration would be about 9 months). We excluded participants reporting a motor vehicle injury on round 1 or 2 because measures of their HRQOL prior to their motor vehicle injuries are not available. Individuals not reporting health problems due to a traffic injury were assumed not to have sustained a traffic injury. As a result, there were no missing data with respect to the independent variable.
Among the 63,950 respondents, 1,652 (2.5 %) individuals had missing values on the PCS or MCS in either round 2 or 4. Those with missing dependent variable data were similar to those with complete information in terms of the frequency of traffic injury and gender. Given this similarity and the relatively low frequency of missing values, we chose to exclude those with missing dependent variable values. We used the longitudinal survey weights provided from the survey developers to account losses to follow-up.
Analytic approach
All analyses were conducted using STATA 12. Analyses of MEPS data must account for survey weights, strata, and clustering of individuals due to the complex survey design. Due to the longitudinal nature of the analysis, a longitudinal weight that adjusts for attrition in the survey rounds was also incorporated for all analyses (provided by the survey developers). Accordingly, all variance calculations were adjusted incorporating the Taylor series method [27, 37].
Descriptive statistics at baseline of the characteristics of those reporting a motor vehicle injury on rounds 3 or 4 and respondents not reporting a motor vehicle injury (the control group) were obtained. Differences with respect to continuous variables were assessed using the Student’s t test accounting for the complex design of the survey [37]. Even though the physical and mental component scores were not normally distributed, student’s t test is robust to the normality assumption and considered a good approximation for hypothesis tests [46]. For categorical variables, chi-square tests were used to compare proportions [27].
The impact of motor vehicle injuries on HRQOL was examined in two ways: a within-group analysis of change in HRQOL and a between-groups analysis comparing changes between groups unadjusted and adjusted for covariates.
Within-group analysis
The mean differences (i.e., changes over time) in HRQOL scores were obtained separately for those with and without a history of motor vehicle-related injuries and tested for statistical significance using paired t tests. Ninety-five percent confidence intervals for the mean scores were also obtained.
Between-groups analysis
Two between-group analyses were performed. First, PCS and MCS values were compared at round 2 (baseline) between respondents who reported motor vehicle-related injury and those who did not.
Second, changes over time in PCS and MCS (from round 2 to 4) were modeled as continuous outcomes with the main predictor of interest being the reporting of a motor vehicle-related injury. Covariates were selected based on associations with both motor vehicle injuries and HRQOL [18–20] and include gender, age (5-years intervals), highest educational degree obtained (no degree, high school, bachelors, and beyond bachelors degree as the reference group), and income, as a percentage of poverty level [poor as the reference group (<100 %), near poor (100–<125 %), low income (125–<200 %), middle (200–<400 %), and high income (≥400 %)]. Interaction effects were also examined to determine whether the association of motor vehicle-related injuries with change in quality of life differed by gender, as reported in previous studies [29]. Statistical significance was defined as p < 0.05 unless specified otherwise. Consistent with previous studies, differences greater than 2.0 points on QOL life scales were considered clinically meaningful differences on SF-12 subscales [19, 38].
The study was granted an exemption status by the University of Wisconsin–Madison Institutional Review Board since it only used the Household component of the MEPS.
Results
Respondent characteristics
During the study period, 993 respondents, 1.5 % of those surveyed, reported new-health conditions that were associated with motor vehicle injuries during round 3 or 4 of the survey. After accounting for sampling weights, these data suggest that approximately 3 million adults in the US sustain traffic-related injuries each year. Those who reported a motor vehicle injury were more likely to be young adults (between the ages 18 and 45) than the control group. In addition, those with motor vehicle-related injuries were less likely than the control group to report high income. The proportions of males, and individuals with stroke, coronary heart disease or high blood pressure were not significantly different between the two groups. Diabetes, on the other hand, was significantly more frequent among those reporting motor vehicle injuries than in the control group (Table 1).
Table 1.
Descriptive characteristics at baseline by later motor vehicle-related injury involvement
| Variable | Reporting MVC injury weighted | Not reporting MVC injury weighted | Total weighted | p value |
|---|---|---|---|---|
| N (unweighted) | 993 | 61,305 | 62,298 | |
| Age category (%) | ||||
| 18–24 | 21.6 | 11.8 | 11.9 | <.0001 |
| 25–45 | 45.5 | 38.8 | 39.0 | |
| 46–64 | 23.9 | 32.7 | 32.6 | |
| 65≥ | 8.7 | 16.5 | 16.4 | |
| Male (%)b | 46.1 | 47.2 | 47.20 | .56 |
| Income (%)a,b | ||||
| Poor (<100 %) | 12.0 | 10.7 | 10.7 | .021 |
| Near poor (100–<125 %) | 4.0 | 4.0 | 4.0 | |
| Low (125–<200 %) | 17.0 | 13.6 | 13.6 | |
| Middle (200–<400 %) | 31.0 | 31.6 | 31.6 | |
| High (≥400 %) | 36.4 | 40.0 | 39.9 | |
| Highest degree (%)b | ||||
| No degree | .33 | .39 | .38 | .049 |
| High school | 21.8 | 18.1 | 18.2 | |
| Some college | 30.2 | 32.7 | 32.7 | |
| Bachelor | 23.6 | 22.9 | 23.0 | |
| Beyond | 23.9 | 25.8 | 25.7 | |
| Diabetes (%)b | 9.6 | 6.7 | 6.8 | .002 |
| High Blood Pressure (%)b | 25.7 | 24.7 | 24.7 | .36 |
| Coronary Heart Disease (%)b | 2.7 | 3.0 | 3.0 | .95 |
| Stroke (%)b | 2.7 | 2.3 | 2.3 | .14 |
MVC motor vehicle crash
Percentage of poverty line
Age-adjusted (2000 US population)
Change in HRQOL
The average of both the physical and mental component scores of the SF-12 and 95 % CI is shown in Table 2 by injury status for both periods (round 2 and round 4), together with their changes. The baseline physical component score was similar in participants reporting motor vehicle-related injury and controls (50.17 vs. 49.52, p = .08). The baseline mental component, however, was slightly lower among those reporting a motor vehicle related injury than among controls (49.22 vs. 50.90, p = <.001).
Table 2.
Physical and MCS at baseline and follow-up
| SF-12 | N | Round 2 mean (95 % CI) | Round 4 mean (95 % CI) | Δ | p |
|---|---|---|---|---|---|
| Reported motor vehicle-related injury | |||||
| Physical score | 2,157 | 50.17 (49.44, 50.89) | 47.45 (46.71, 48.20) | −2.72 | <.001 |
| Mental score | 2,157 | 49.22 (48.46, 49.98) | 49.38 (48.60, 50.15) | 0.16 | .68 |
| No reported motor vehicle-related injury | |||||
| Physical score | 132,687 | 49.52 (49.37, 49.68) | 49.72 (49.56, 49.88) | 0.20 | <.001 |
| Mental score | 132,747 | 50.90 (50.77, 51.02) | 51.24 (51.11, 51.36) | 0.34 | <.001 |
The results also indicate a decline in the physical component score at round 4 from pre-injury scores, measured on round 2, among respondents reporting a motor vehicle-related injury. The decrement is about 2.7, reaching both statistical and clinical significance (Table 2). The MCS, however, did not change between the pre-and post-injury periods. Respondents who did not experience a vehicle-related injury during the study period did not have a clinically meaningful change in either their mental or physical scores.
Results adjusted for differences in baseline characteristics
Results from the multivariable regressions show that, on average, the decline in the physical component score of HRQOL (round 4–round 2) was significantly sharper (2.84) among those reporting a motor vehicle-related injury than among controls, after adjusting for age and sex. When income and education were added to the model, the coefficient for motor vehicle injury did not change and it retained statistical significance.
Similarly, controlling for age and sex had little effect on the difference between persons reporting injuries and controls, with both groups showing negligible changes over time in the mental component of HRQOL, in both the univariate (Table 2) and multivariable analyses (coefficient −.090, p value 0.79, Table 3). When we added income and education to the model, the coefficient remained close to zero (−.070, Table 3). While diabetes was associated with both traffic-related injuries and HRQOL, it was not significant in the multivariable analysis, and its inclusion did not affect the coefficient for motor vehicle injury; thus, diabetes was not included in the final model. The interaction of vehicle-related injury and sex was not significant for either the physical and mental components and was not included in the final models.
Table 3.
Adjusted differences between those reporting motor vehicle injuries and controls in changes over time in HRQOL
| Model adjustment | N | Vehicle-related injury coefficient | 95 % CI |
|---|---|---|---|
| Physical component | |||
| Age, sexa | 62,702 | −2.84 (<.001) | −3.53, −2.16 |
| Age, sex, income, educationa | 62,298 | −2.84 (<.001) | −3.54, −2.15 |
| Mental component | |||
| Age, sexa | 62,755 | −0.09 (.79) | −.83, .64 |
| Age, sex, income, educationa | 62,350 | −0.07 (.84) | −.82, .66 |
For those injured, the changes over time in HRQOL were between pre-and post-motor vehicle-related injury p values are in parenthesis
Weighted regression models
Discussion
Using a large nationally representative population-based survey, we show that adults reporting health conditions due to motor vehicle injuries experience a significant decrease in physical but not mental HRQOL compared to those not reporting motor vehicle injuries. The negative effects we observed on the physical component of HRQOL are both statistically and clinically significant. We are not aware of other studies that examined motor vehicle injuries and HRQOL using a large nationally representative sample and including baseline health measures before the occurrence of the vehicle-related injury. While we cannot directly compare our study to previous studies, our finding is consistent with other studies that have found negative effects of motor vehicle injuries on HRQOL.
HRQOL is an important outcome in population health and considered to be one of the fundamental objectives of Healthy People 2020 initiative [21]. Nevertheless, it has not been a major focus within the trauma research literature, especially in studies based on representative samples and including injury-free comparison groups and multiple measures of health status [35, 41]. The majority of the existing literature has examined HRQOL using samples of injured individuals as a result of any type of injury without recognizing that the long-term consequences of injury on HRQOL might vary by injury mechanism [6–11, 16, 28, 29]. Mortality and other indicators of severity of health outcomes following injury have been found to differ by injury mechanism [48]. Future studies are necessary to examine whether the effects of injury on HRQOL differ for other mechanisms of injury than what we have observed in this study for motor vehicle injuries, and whether they differ within the mechanism of motor vehicle injuries depending on whether the person injured was a motor vehicle occupant versus a pedestrian or bicyclist.
A study by Ameratunga et al. [19] among drivers in New Zealand examined the association of experiencing a motor vehicle crash on HRQOL. The authors asked respondents after a crash to recall their quality of life prior to injury and found motor vehicle injuries to be associated with a decrease in HRQOL. However, due to the method of assessing pre-crash health, the observed association could be due to recall bias if those injured in traffic crashes were more likely to overestimate the level of their pre-crash health [17, 19].
Another study by Villanueva et al. [18] examined HRQOL before and after traffic-related injuries among university graduates in Spain. They found that injured respondents exhibited a decline in the physical component of HRQOL compared to their baseline status and that their mental component did not change over time, which consistent with findings from our study. However, unlike the Villanueva et al. study, we did not find those with motor vehicle-related injuries to have worse baseline physical health than the uninjured group. In addition, despite finding a slight difference in baseline mental health, a difference that was statistically significant due to the large number of respondents surveyed, this difference was not clinically meaningful.
Our findings indicate a meaningful impact of motor vehicle-related injuries on the physical component of HRQOL. Our estimate of decrease in the physical component was more pronounced than reported in the study by Villanueva et al. Perhaps this was because the Villanueva et al. studied university graduates who might have been more likely than the general population to adopt effective coping mechanism and able to seek care. In addition, the time lag after the injuries in the Villaneueva et al. study was up to 4 years, which could have resulted in patients regaining some of the lost HRQOL after the injury [18, 34]. In our data, those injured in the earlier round (3) did exhibit less magnitude in HRQOL deficit than those injured at round 4, supporting the fact that injured individuals regain some lost quality of life.
One of the major advantages of health measurement tools is the ability to compare the decrease in health across conditions. To put our findings in context, the 2.8-point decline in the physical component we found is comparable to a difference between those diagnosed with debilitating chronic diseases, such as diabetes, and those who were not. Two studies that examined the effects of diabetes on the SF-12 found that those with diabetes had physical HRQOL scores that were 2.8–3.3-points lower than controls [5, 36].
Contrary to what we expected, our study did not find any impact of motor vehicle injuries on the mental component of quality of life. Although a negative association was present in the adjusted analysis, its magnitude was minimal, and the results were not statistically significant. Other studies suggest that motor vehicle injuries can have lasting negative effects on mental wellbeing [18–20, 42]. Our failure to find such effects could be due to a number of factors. First, our population-based sample likely included persons experiencing varying levels of injury severity, though we have no measures of severity. It is possible that adverse effects on the mental component of HRQOL are associated with more severe injuries but could not be detected in our sample if the majority sustained relatively mild injuries.
Another potential explanation has to do with the instrument used for evaluating the mental component of quality of life. Kiely et al. evaluated the SF-12 correlation to the SF-36 in a population of trauma population and found the MCS, in contrast to the physical component score, to be not responsive to change. They concluded that other methods may be necessary to fully evaluate the mental component of HRQOL in injured populations [43]. Other studies, however, have found the SF-12 to be a valid instrument for measuring both the physical and mental components of HRQOL [23–26]. Future studies incorporating other measures of the mental component of HRQOL, in addition to the SF-12, should be done to see whether these identify deficits in the mental component of HRQOL in response to injuries or other illnesses.
The effects of motor vehicle injuries on HRQOL could extend to uninjured family members or others who are affected by the injury either because of the loss in the case of a fatal injury, the demands of caregiving, or financial distress. It is unlikely that the MEPS questions, aimed to identify health conditions associated with hospital stay, outpatient visit, emergency room visit, home health episode, prescribed medication purchase, medical provider visit, or conditions bothering the respondents, will identify these effects, as they tend to imply specific injuries that affected the respondents, not others. Lastly, those who experienced a tragic motor vehicle crash could have adopted a positive attitude toward their conditions by becoming more appreciative of life or through social support. This, as a result, may facilitate regaining mental health after injury. All of those factors may have contributed to our failure to identify an impact of motor vehicle-related injuries on the mental component of HRQOL in our population.
Our study found the prevalence of self-reported motor vehicle-related health problems to be similar in men and women. In contrast, previous epidemiological studies based on objective measures of injury occurrence consistently find that motor vehicle injuries are more common among men [19, 42, 43]. A previous study based on MEPS data also found no association between gender and frequency of vehicle-related injury [20]. In addition, population-level estimates of long-term disability due to traffic injuries indicate higher prevalence among females than males in the US [4]. It is important to note that the self-reported nature of the motor vehicle-related health conditions in the MEPS does not necessarily reflect the frequency of motor vehicle-related crashes or injuries to MEPS participants.
Unlike previous studies [17–20, 44], our study did control for baseline health status by analyzing the difference, as recommended in the methodological literature [45, 46]. Furthermore, the employment of a comparison group allowed us to avoid spurious finding due to regression to the mean or aging.
The present study is limited by the fact that the MEPS dataset does not have detailed information on the circumstances of the motor vehicle injuries and whether it involved other family members or close friends, which can affect reported quality of life. If someone lost a loved one in a motor vehicle crash, his or her quality of life will more likely be affected. Clearly, future research is warranted in order to fully understand the effects traffic-related injuries both on injured individuals and their family members. In addition, those who did not report a medical condition due to a motor vehicle injuries will not appear in our injured group. Therefore, the true impact of vehicle-related crashes on HRQOL might be underestimated. However, we believe our analysis will be generalizable to those who had injuries severe enough to be reported during the study period.
Despite the limitations, this study is the first large representative sample of the US population evaluating HRQOL and motor vehicle injuries using the SF-12. This instrument is a generic measure of both components of health status: physical and mental health, and is easy to communicate to the public, clinicians as well as to policy makers. An important strength of this study is the longitudinal design using two measurements of the quality of life instruments at two points during follow-up, which permits tracking the change in reported health among those injured in motor vehicle crashes. This unique design makes the MEPS an ideal sources to examine HRQOL among injured individuals and provide advantage over other existing datasets.
Conclusion
This study demonstrates that non-fatal motor vehicle injuries have enduring impacts on HRQOL that extend beyond the well-documented and acute effects of trauma and premature mortality. Specifically, we found that a population-based sample of adults who survived motor vehicle-related injuries reported clinically significant decrements in the physical health up to 9 months after the injury. These effects persisted after controlling for potential confounders and are comparable in magnitude to other debilitating conditions such as diabetes.
References
- 1.Road Safety Status; World Health Organization website. Accessed November 5 http://www.who.int/violence_injury_prevention/road_safety_status/2009/en/index.html.
- 2.Murray CJ, Vos T, & Lozano RNM (2013). Global burden of disease. (Seatle, 2013) at http://www.healthmetricsandevaluation.org/gbd/visualizations/gbd-2010-change-leadingcauses-and-risks-between-1990-and-2010?cr=risk&metric=DALY. [Google Scholar]
- 3.National Highway Traffic Safety Administration [NHTSA]. (2003). Motor vehicle traffic crash injury and fatality estimates: 2002 early assessment. (Report No. DOT HS 809 586). Washington, DC: U.S. Department of Transportation. [Google Scholar]
- 4.Shults RA, Jones BH, Kresnow MJ, Langlois JA, & Guerrero JL (2004). Disability among adults injured in motor vehicle crashes in the United States. Journal of Safety Research, 35(4), 447–452. [DOI] [PubMed] [Google Scholar]
- 5.Fu AZ, Qiu Y, Radican L, & Luo N (2011). Marginal differences in health-related quality of life of diabetic patients with and without macrovascular comorbid conditions in the United States. Quality of Life Research, 20(6), 825–832. [DOI] [PubMed] [Google Scholar]
- 6.Ringdal M, Plos K, Lundberg D, Johansson L, & Bergbom I (2009). Outcome after injury: Memories, health-related quality of life, anxiety, and symptoms of depression after intensive care. Journal of Trauma, 66, 1226–1233. [DOI] [PubMed] [Google Scholar]
- 7.Holbrook TL, Anderson JP, Sieber WJ, Browner D, & Hoyt DB (1999). Outcome after major trauma: 12-month and 18-month follow-up results from the Trauma Recovery Project. Journal of Trauma, 46, 765–771. [DOI] [PubMed] [Google Scholar]
- 8.Michaels AJ, Michaels CE, Smith JS, Moon CH, Peterson C, & Long WB (2000). Outcome from injury: General health, work status, and satisfaction 12 months after trauma. Journal of Trauma, 48, 841–848. [DOI] [PubMed] [Google Scholar]
- 9.Holtslag HR, Van Beeck EF, Lindeman E, & Leenen LP (2007). Determinants of long-term functional consequences after major trauma. Journal of Trauma, 62, 919–927. [DOI] [PubMed] [Google Scholar]
- 10.Aitken LM, Davey TM, Ambrose J, Connelly LB, Swanson C, & Bellamy N (2007). Health outcomes of adults 3 months after injury. Injury, 38, 19–26. [DOI] [PubMed] [Google Scholar]
- 11.Christensen MC, Banner C, Lefering R, Vallejo-Torres L, & Morris S (2011). Quality of life after severe trauma: Results from the global trauma trial with recombinant factor VII. Journal of Trauma, 70, 1524–1531. [DOI] [PubMed] [Google Scholar]
- 12.Black JA, Herbison GP, Lyons RA, Polinder S, & Derrett S (2011). Recovery after injury: An individual patient data meta-analysis of general health status using the EQ-5D. Journal of Trauma, 71, 1003–1010. [DOI] [PubMed] [Google Scholar]
- 13.Alonso J, Ferrer M, Gandek B, Ware JE Jr, Aaronson NK, Mosconi P, et al. (2004). Health-related quality of life associated with chronic conditions in eight countries: Results from the International Quality of Life Assessment (IQOLA) project. Quality of Life Research, 13(2), 283–298. [DOI] [PubMed] [Google Scholar]
- 14.Haley WE, Roth DL, Kissela B, Perkins M, & Howard G (2011). Quality of life after stroke: A prospective longitudinal study. Quality of Life Research, 20(6), 799–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Read KM, Kufera JA, Dischinger PC, Kerns TJ, Ho SM, Burgess AR, et al. (2004). Life-altering outcomes after lower extremity injury sustained in motor vehicle crashes. Journal of Trauma, 57(4), 815–823. [DOI] [PubMed] [Google Scholar]
- 16.Brasel KJ, Deroon-Cassini T, & Bradley CT (2010). Injury severity and quality of life: Whose perspective is important? Journal of Trauma, 68(2), 263–268. [DOI] [PubMed] [Google Scholar]
- 17.Andersen D, Ryb G, Dischinger P, Kufera J, & Read K (2010). Self-reported health indicators in the year following a motor vehicle crash: A comparison of younger versus older subjects. Annals of Advances in Automotive Medicine, 54, 359–367. [PMC free article] [PubMed] [Google Scholar]
- 18.Pons-Villanueva J, Rodríguez de Armenta MJ, Martínez González MA, & Seguí-Gómez MD (2011). Longitudinal assessment of quality of life and its change in relation to motor vehicle crashes: The SUN (Seguimiento Universidad de Navarra) Cohort. Journal of Trauma, 70(5), 1072–1077. [DOI] [PubMed] [Google Scholar]
- 19.Ameratunga SN, Norton RN, Connor JL, Robinson E, Civil I, Coverdale J, Bennett D, & Jackson RT (2006). A population-based cohort study of longer-term changes in health of car drivers involved in serious crashes. Annals of Emergency Medicine, 48(6), 729–36. Epub 2006 Sep 25. [DOI] [PubMed] [Google Scholar]
- 20.Nyman JA, Barleen NA, & Kirdruang P (2008). Quality adjusted life years lost from nonfatal motor vehicle accident injuries. Medical Decision Making, 28(6), 819–828. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Department of Health and Human Services. (2012). Healthy People 2020; Accessed May 31, 12: http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx.
- 22.Agency for Healthcare Research and Quality web site. Medical Expenditure Panel Survey. Available from: http://www.meps.ahrq.gov/mepsweb/. Accessed October 15, 2011. [PubMed]
- 23.Ware J, et al. (1996). How to score the SF-12 physical and mental health summary scales, 2nd ed Lincoln RI: Quality Metric, Inc., and the Health Assessment Lab. [Google Scholar]
- 24.Ware J, Kosinski M, Turner-Bowker D, & Gandek B (2002). SF12v2: How to score version 2 of the SF-12 health survey. Lincoln, RI: QualiyMetric Incorporated. [Google Scholar]
- 25.The EuroQol Group. Available at: http://www.euroqol.org/download/ref.pdf. Accessed November 11, 2011.
- 26.McDowell I, & Newell C (1996). Measuring health: A guide to Rating Scales and Questionnaires (2nd ed.). New York: Oxford University Press. [Google Scholar]
- 27.Thomas DR, & Rao JNK (1987). Small sample comparison of level and power for simple goodness-of-fit statistics under cluster sampling. Journal of American Statistical Association, 82, 630–636. [Google Scholar]
- 28.Holbrook TL, Hoyt DB, Coimbra R, Potenza B, Sise MJ, Sack DI, et al. (2007). Trauma in adolescents causes long-term marked deficits in quality of life: Adolescent children do not recover preinjury quality of life or function up to two years postinjury compared to national norms. Journal of Trauma, 62(3), 577–583. [DOI] [PubMed] [Google Scholar]
- 29.Holbrook TL, & Hoyt DB (2004). The impact of major trauma: Quality-of-life outcomes are worse in women than in men, independent of mechanism and injury severity. Journal of Trauma, 56(2), 284–290. [DOI] [PubMed] [Google Scholar]
- 30.Ellis JJ, Eagle KA, Kline-Rogers EM, & Erickson SR (2005). Validation of the EQ-5D in patients with a history of acute coronary syndrome. Current Medical Research and Opinion [0300–7995] Ellis 21(8), 1209–1216. [DOI] [PubMed] [Google Scholar]
- 31.Sullivan PW, & Ghushchyan V (2006). Preference-based EQ-5D index scores for chronic conditions in the United States. Medical Decision Making, 26(4), 410–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ponsford J, Hill B, Karamitsios M, & Bahar-Fuchs A (2008). Factors influencing outcome after orthopedic trauma. Journal of Trauma, 64(4), 1001–1009. [DOI] [PubMed] [Google Scholar]
- 33.Yang Z, Lowe AJ, de la Harpe DE, & Richardson MD (2010). Factors that predict poor outcomes in patients with traumatic vertebral body fractures. Injury, 41(2), 226–230. Epub 2009 Nov 3. [DOI] [PubMed] [Google Scholar]
- 34.Hu X-B,Feng Z, Fan Y-C, Xiong Z-Y, & Huang Q-W (2012). Health-related quality-of-life after traumatic brain injury: A 2-year follow-up study in Wuhan, China. Brain Injury, 26(2), 183–187. [DOI] [PubMed] [Google Scholar]
- 35.Sampalis S, Liberman M, Davis L, Angelopoulos J, Longo N, Sampalis F, et al. (2006). Functional status and quality of life in survivors of injury treated at tertiary trauma centers: What are we neglecting? Journal of Trauma, 60(4), 806–813. [DOI] [PubMed] [Google Scholar]
- 36.Jia H, & Lubetkin EI (2005). The impact of obesity on health related quality-of-life in the general adult US population. Journal of Public Health (Oxford), 27(2), 156–164. Epub 2005 Apr 8. [DOI] [PubMed] [Google Scholar]
- 37.Heeringa S, West B, & Berglund P (2010). Applied survey data analysis (pp. 140–144). Boca Raton: Chapman & Hall/CRC, Taylor & Francis Group. [Google Scholar]
- 38.Edelman D, Olsen MK, Dudley TK, et al. (2002). Impact of diabetes screening on quality of life. Diabetes Care, 25, 1022–1026. [DOI] [PubMed] [Google Scholar]
- 39.Cheak-Zamora NC, Wyrwich KW, & McBride TD (2009). Reliability and validity of the SF-12v2 in the Medical Expenditure Panel Survey. Quality Life Research, 18, 727–735. [DOI] [PubMed] [Google Scholar]
- 40.Khanna D, Maranian P, Palta M, Kaplan RM, Hays RD, Cherepanov D, et al. (2011). Health-related quality of life in adults reporting arthritis: Analysis from the National Health Measurement Study. Quality of Life Research, 20(7), 1131–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.MacKenzie EJ, McCarthy ML, Ditunno JF, Forrester-Staz C, Gruen GS, Marion DW, et al. (2002). Pennsylvania Study Group on Functional Outcomes Following Trauma. Using the SF-36 for characterizing outcome after multiple trauma involving head injury. Journal of Trauma, 52(3), 527–534. [DOI] [PubMed] [Google Scholar]
- 42.Tøien K, Bredal IS, Skogstad L, Myhren H, & Ekeberg O (2011). Health related quality of life in trauma patients. Data from a one-year follow up study compared with the general population. Scand Journal of Trauma Resuscitation Emergency Medicine, 19, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kiely JM, Brasel KJ, Guse CE, & Weigelt JA (2006). Correlation of SF-12 and SF-36 in a trauma population. Journal of Surgical Research, 132(2), 214–218. [DOI] [PubMed] [Google Scholar]
- 44.Langley J, Derrett S, Davie G, Ameratunga S, & Wyeth E (2011). A cohort study of short-term functional outcomes following injury: The role of pre-injury socio-demographic and health characteristics, injury and injury-related healthcare. Health Qual Life Outcomes, 9, 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Glymour MM, Weuve J, Berkman LF, Kawachi I, & Robins JM (2005). When is baseline adjustment useful in analyses of change? An example with education and cognitive change. American Journal of Epidemiology, 162(3), 267–278. [DOI] [PubMed] [Google Scholar]
- 46.Vittinghoff E, Glidden DV, Shiboski SC, & Charles E (2005). McCulloch regression methods in biostatistics: Linear, logistic, survival, and repeated measures models (pp. 33, 263–266). New York: Springer Science ? Business Media Inc. [Google Scholar]
- 47.Holder Y, Peden M, Krug EG, et al. (2004). Injury surveillance guidelines. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 48.Haider AH, Chang DC, Haut ER, Cornwell EE I. I. I., & Efron DT (2009). Mechanism of injury predicts patient mortality and impairment after blunt trauma. Journal of Surgical Research, 153, 138–142. [DOI] [PubMed] [Google Scholar]
- 49.Robertson L (2007). Injury epidemiology, (3rd ed., p. 14). New York: Oxford University Press. [Google Scholar]
- 50.Overgaard M, Høyer CB, & Christensen EF (2011). Long-term survival and health-related quality of life 6 to 9 years after trauma. Journal of Trauma, 71(2), 435–441. [DOI] [PubMed] [Google Scholar]