Abstract
Smoking in the United States follows a clear socioeconomic gradient: low-income Americans smoke more and quit less than those with more education and income. Evidence-based interventions like tobacco quitlines are designed to make effective cessation services available on a population basis to all smokers. However, these interventions do not address many of the unique challenges faced by low-income smokers, including unmet basic needs like food, housing, personal safety and money for necessities that often supersede health needs. Research is needed to maximize the use and effectiveness of tobacco quitlines in low-income populations. This paper details the rationale, design and methods for a 2×2 randomized controlled trial currently underway comparing the effects of Standard and Specialized Tobacco Quitlines with and without Basic Needs Navigation on intervention engagement and smoking cessation among low-income smokers. Smokers are recruited from United Way 2-1-1 in Missouri and all participants receive tobacco quitline services from Optum. Quitline and navigation services are provided for 3 months. Participants complete telephone surveys at baseline, 3- and 6-month follow up. The primary study outcome is self-reported 7-day point prevalence abstinence at 6-month follow up. Embedding the study in practice agencies will accelerate dissemination and scalability should our findings demonstrate intervention effectiveness.
Keywords: smoking cessation, health disparities, minority health, behavioral intervention, behavior change, clinical protocols
Introduction
There is a greater burden of smoking and smoking-related cancers in low-income populations. In the US, those with lower incomes are more likely to smoke (26%), have greater nicotine dependence, lower readiness to change, lower self-efficacy for quitting, and are less likely to quit.1–8
Effective cessation programs and resources are available but underutilized by low-income smokers.2,9,10 Telephone counseling for smoking cessation is an evidence-based intervention11–13 that is recommended in both clinical and community practice guidelines.11,14,15 Because tobacco quitlines offer population-wide free access to smoking cessation support, they have the potential to reach a diverse population of smokers. Scant evidence exists for the success of quitlines across levels of socioeconomic status,12 although several recent studies have shown promising effects with low-income samples.16–19
Traditionally, health promotion and disease prevention programs targeting low-income individuals have focused on adopting or changing health behaviors without addressing unmet basic needs such as food, shelter, safety, and money for necessities that may impede participants’ ability to engage in the programs and make and sustain behavior changes. Thus, traditional interventions alone may fail to yield desired results in very low-income populations. Adapted from our prior work,20,21 Figure 1 illustrates the bi-directional process in the conceptual model guiding this study. Scarcity diminishes one’s cognitive capacity to focus on goals beyond meeting basic needs22 by attenuating attention, planning, follow-through and other self-care actions, which in turn affect motivation and ability to perform health behaviors like quitting smoking.22–26 Support for this model is provided by reported associations27–33 and interventions – focused on coping, support, and problem resolution – showing beneficial effects on healt behaviors, psychological distress, and mental health outcomes.34–36,37–42
Figure 1.
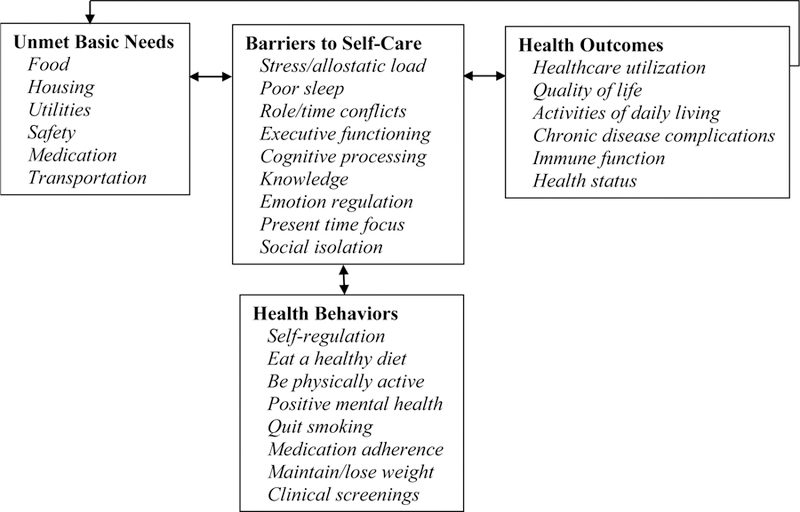
Conceptual Model of How Unmet Basic Needs Indirectly Impact Health Outcomes
Providing coaching or navigation services to address basic needs among low-income smokers is a promising approach to improving cessation. In a previous study, navigators helped participants follow-up on referrals they had received to agencies and organizations that provide needed health services. Smokers paired with a health service navigator were twice as likely to call the quitline,43 although calling the quitline did not translate into increased cessation. The current study seeks to extend previous research to improve cessation outcomes by 1) using navigators to specifically assist with unmet basic needs and 2) adapting the standard quitline program for low-income smokers.
Study Objectives
The primary aims of this statewide field trial are to compare the relative and combined effects of two interventions on use of the tobacco quitline and abstinence among low-income smokers. We hypothesize that participants who are exposed to the specialized quitline and who receive basic needs navigation will be more likely to engage in and complete the quitline program and quit smoking, as measured by 7-day point-prevalence abstinence at 6-month follow up. We also will examine secondary outcomes including 30-day abstinence, 24 hour quit attempts, and reduction in the number of cigarettes smoked per day.
Materials and Methods
Study Design
Our interventions are tested using a 2 (type of quitline service: standard vs. specialized) x 2 (help with basic needs: no navigator vs. navigator) factorial design. Telephone surveys will be administered at baseline, 3- and 6-month follow up. All materials and procedures were approved by the Washington University Institutional Review Board.
Study Population, Eligibility Criteria, Recruitment and Retention
Each incoming call to the 2-1-1 helpline in Missouri is distributed to whichever information specialist has been idle the longest or is first to become available if all specialists are currently taking calls. Among all information specialists in the call center, a subset of specially trained staff identify potential participants for the study. After providing standard 2-1-1 service, they ask callers if they would be willing to answer a few health questions. Callers eligible to receive the invitation to screen for study eligibility are: adult (age 18+) Missouri residents, English-speaking, and not in acute crisis or with obvious cognitive limitations. Callers who agree to answer the questions are asked, “Do you currently smoke cigarettes every day, some days, or not at all?” This item is used in the Behavioral Risk Factor Surveillance System,44 is recommended by the North American Quitline Consortium,45 and has high test-retest reliability in multi-ethnic populations in the U.S. and Missouri.46–49 Daily smokers are further screened for eligibility by asking if they are thinking about quitting in the next 30 days. Study eligibility is not dependent on the number of cigarettes smoked per day, because historically this criterion has excluded African Americans from cessation trials.50 Daily smokers interested in quitting are asked if they are willing to share their contact information with a research team conducting a study to help smokers quit. 2-1-1 information specialists record all recruitment screening data in a secure electronic database that is shared with University research staff.
Research staff attempt to reach interested smokers by phone by the next business day to confirm their interest and eligibility, obtain verbal informed consent, administer the baseline survey, and obtain detailed contact information and preferred dates and times for follow-up. Additional eligibility criteria applied during the baseline call include willingness to receive calls from others to help them quit smoking (i.e., from quit coaches) and address unmet basic needs (i.e., from navigators). Smokers who report being pregnant or breastfeeding are ineligible for the study, as are those with health insurance through their employer, because they may be eligible for different services through the quitline.
Research staff assign participants who complete the baseline survey to one of the four study conditions using a computer generated list of random numbers in batches of 500 numbers to ensure equal proportions in the four groups over time. By the end of each business day, research staff share enrolled participants’ contact information and study group assignment with the quitline and, when applicable, the basic needs navigator. Research staff also inform the quitline of participants who opt-in to the quitline’s Text2Quit and/or Internet programs that supplement telephone coaching by providing a mobile phone number and/or email address.
In all study conditions, participants are proactively called by the intervention messenger (a quit coach and/or navigator). Quitline coaches attempt to reach smokers within 3 business days of receiving their contact information, while navigators attempt to reach smokers within two weeks after randomization. This 2-week lag allows participants to contact the referrals they received from 2-1-1 and engage with the quitline prior to receiving additional assistance from the navigator.
Maintaining contact with participants during study follow up is a challenge, especially in low-income populations. To maximize retention we: (1) clearly inform participants at consent about follow ups and timing; (2) provide financial incentives for completing each follow-up survey ($10 at 3- and 6-month follow up); (3) collect up to three different contact numbers and mailing addresses from each participant; (4) obtain from participants a “best time to call”; (5) make at least two attempts per week to reach each participant at each follow up across different days of the week and times of the day over the span of 3 months; (6) use multiple channels (e.g., mail, email, text, voice message) to contact participants for 3- and 6-month follow-up surveys; and (7) send signed thank-you notes with incentive payments after each survey is completed.
Interventions
Standard Tobacco Quitline Intervention.
Missouri Tobacco Quitline services are provided by Optum, which also provides these services for many other states and many large corporations and health systems. Optum’s Quit For Life® is the nation’s leading tobacco cessation program, using a combination of physical, psychological, and behavioral strategies to help smokers quit. Optum’s quit coaches are trained in the science of behavior change and motivational interviewing.
Quit for Life helps smokers set a quit date within 30 days of enrollment and provides scheduled coaching calls to assist smokers in quitting. Calls are scheduled at the smoker’s convenience, usually last 10–15 minutes, can be spread over 1–3 months around the quit date, and are adjusted based on each individual’s quitting success or needs. Smokers can also contact the quitline on their own as desired, outside of scheduled counseling sessions. Quit coaches try to reach a smoker up to three times for each counseling session. The counseling goal is to increase a smoker’s readiness to quit and develop an individually tailored quit plan.
At the start of study recruitment in June 2017, the Missouri Tobacco Quitline provided: (1) up to four scheduled coaching calls; (2) unlimited calls to a toll-free phone number by the smoker; (3) access to Optum’s Internet and Text2Quit programs; (4) printed self-help materials (i.e., “Quit Guide”); and (5) up to 2 weeks of free NRT (patch or gum) mailed to smokers if they are ready to quit in the next 30 days, have no contraindications to NRT, and do not have Medicaid insurance. Because participants with Medicaid insurance have more pharmacological options and coverage available, they are referred to their doctor and health plan to obtain cessation aids.
Specialized Tobacco Quitline Intervention.
The standard Quit for Life program was modified in content, personnel and protocol to better fit the needs of low-income smokers. All aspects of cessation counseling were reviewed and adapted as necessary to suit the life context of low-income smokers. For example, resource constraints prevent many low-income smokers from buying cessation aids routinely recommended by quit coaches; low-income smokers are often renters and low-wage workers who have less control over tobacco exposure at home and work, respectively; and distal potential benefits of quitting may be less salient to low-income smokers than immediate, tangible ones. The training program for coaches was adapted to recognize and address these differences.
As an alternative to the 50-page Quit Guide sent by Optum to participants in the standard quitline condition, a brief 13-page version was developed and tailored to low-income smokers. The specialized guide used more graphics, first-person narratives and plain language: it was written at a 5th grade reading level compared to 7th grade for the 50-page Quit Guide. Unique topics covered in the quit guide included low-cost and free cessation aids and ways to ask for help. It also provided scripts for talking to family and friends about quitting and simple worksheets for planning to quit.
A subset of quit coaches who are experienced with both standard and specialized programs deliver the unique counseling protocols using custom software. Intervention-specific training included four interactive modules (see Appendix) focused on understanding the daily lives of low-income smokers (e.g., resource constraints, time orientation), unique aspects of their smoking behavior (e.g., acquiring and using tobacco, brand preferences), their information processing and communication styles (e.g. concrete vs. abstract language, health literacy), and attributes of trusted information sources (e.g., lived experience, expertise). Specialized quitline calls are longer – 25–30 minutes -- allowing more time for rapport-building and support.
Compared to standard quitline services, the specialized intervention obtains and uses more contact numbers for each smoker and collateral contacts for family members or close friends who could reach a smoker if their phone number was disconnected or changed. The number of call attempts to reach smokers in was increased from three in the standard quitline program to five in the specialized quitline.
Basic Needs Navigation Intervention.
The navigation intervention centers around five main objectives (Table 1): (1) establish trust and rapport; (2) identify unmet basic needs; (3) help participants prioritize among needs; (4) jointly generate solutions; and (5) create actionable steps to reach solutions.
Table 1.
Navigation Objectives
| Establish trust and rapport |
| Introduce participants to the navigation program and the navigator’s role |
| Re-introduce or remind participants about the navigation program and the navigator on each call |
| Differentiate navigation calls from other program calls (cessation coaching, survey administration) |
| Explain the benefits (kinds of assistance and support) the navigator will provide to resolve needs |
| Use participants’ names correctly and use a sympathetic tone of voice and attitude |
| Express empathy and reassurance that solutions to participants’ problems exist |
| Establish frequency and timing of interactions – (dates, times, duration, goals) |
| Follow up on notes from previous calls to maintain continuity and build rapport |
| Identify smoker’s unmet needs |
| Review information sent by 2-1-1 about participant’s needs during initial call for assistance |
| Assess participant’s unmet needs through systematic and open-ended questions |
| Confirm if previously reported needs remain unmet and document any new unmet needs |
| Discuss current unmet needs in detail – (what are the barriers, why is it a need?) |
| Help participants prioritize among multiple needs |
| Separate the unmet need(s) into specific categories, e.g., housing, financial, food, health |
| Probe participants with questions: “What is most important to you right now?”, What do you want to work on first?” |
| Encourage participants to prioritize serious needs or those with immediate solutions |
| Jointly generate solutions |
| Use participants’ zip code to identify relevant local resources/organizations |
| Determine participants’ eligibility for services, contacting resource/organization to inquire if needed |
| Discuss resources participant has used in the past to address needs |
| Identify additional resources through participants’ social network – (case worker, church, etc.) |
| Provide participants with information on resources – (address, distance, requirements, etc.) |
| Create actionable steps to reach solutions |
| Prepare participants to interact with service agencies and/or act as an advocate on their behalf |
| Call the resource/organization before referring the participant to determine their ability to assist |
| Provide instrumental support such as arranging transportation to and from service agencies |
| Follow up on problem solving actions and remind participants to follow through |
| Review progress made towards resolving unmet basic needs and adapt solutions |
Basic needs navigation is provided by a research team member employed by Washington University who helps smokers address unmet basic needs by connecting them to resources in their community. Within two weeks of a participant completing the baseline survey, the navigator calls the participant. In the initial call, the navigator describes her role as a personal resource specialist to the participant as someone that focuses on finding resources in their area to resolve at least some of their needs, and distinguishes her role from others in the research project who will talk to participants by phone to help them to quit smoking or complete research surveys. The navigator reviews the unmet needs participants reported on the baseline survey and elicits any new unmet needs. This process of reviewing changes in previously reported and newly emerging needs is part of each navigation call. The navigator identifies potential resources for each participant using professional contacts and accessing the 2-1-1 resource database available through the study’s partnership with United Way 2-1-1 of Missouri. The navigator refers participants to resources, coaches them on how to contact organizations, and, when needed, acts as an advocate by proactively contacting organizations on the participant’s behalf to see if the organization has available resources or to verify the participant’s eligibility to receive assistance. The navigator and participant work together to determine which needs to address first, based on severity of need and availability of community resources. The navigator does not introduce the subject of smoking cessation nor provide direct assistance or advice for quitting. If the topic of cessation is raised by a participant, the navigator offers encouragement for quitting and contacting the quitline.
The frequency of navigator follow-up calls depends on the number and severity of participants’ needs. For example, those with immediate or pressing needs may receive weekly calls, while those with no new needs receive a call every other week. Participants are encouraged to initiate calls to the navigator as needed. Navigation services are provided for three months post-baseline.
The study’s basic needs navigator has 12 years of experience in social services and case management working with racially and ethnically diverse low-income individuals and families, as well as those with special health conditions or basic needs. In addition, the navigator received extensive project-specific training in basic needs problem-solving techniques, resource mapping and documentation, cultural competency, basic counseling concepts and approaches, and research ethics.
Navigator training involves three modules focused on tasks, techniques, and processes for communication, problem solving, and empowerment. The first module introduces techniques for effective communication with participants. The second establishes guidelines for problem solving and empowerment, including making effective referrals and helping participants access resources. The final module consists of mastering protocols and scripts for calling, recording participant notes, and crisis intervention resources. Prior to launching the navigation intervention, the navigator practiced by completing mock calls using the telephone script and electronic data collection system. Throughout the study, the navigator also receives individualized supervision and feedback, critiques of recorded calls, and bi-weekly sessions discussing challenging cases with the full research team.
Intervention Fidelity Monitoring.
Audio-recordings of Standard Quitline calls, Specialized Quitline calls, and Basic Needs Navigation calls are collected throughout the study. For each of the four study groups in the trial, a 10% random sample of participants and all their calls are analyzed to assess fidelity to study protocols.
To evaluate the fidelity of the quitline intervention, research staff listen to audio-recorded calls and rate the presence or absence of eight key components: (1) describing their expertise as coaches during the introduction; (2) asking questions that would elicit details about the caller’s life context; (3) providing context-relevant insights about the caller’s situation and connecting it back to smoking and/or cessation; (4) providing directive planning through context-relevant tips and confirming their appropriateness with the caller; (5) promoting the use of quit-smoking medication using a metaphor to explain NRT and assisting with medication-related challenges as needed; (6) stating the importance of taking the next coaching call and explaining that the next coach may be a different person and that it will benefit the caller to hear a new perspective from the next coach; (7) using plain language to explain concepts; and (8) responding to the caller with empathy.
At the end of each fidelity assessment form, coders indicate whether they believe the recording was from a standard or specialized quitline call. Coders then meet to reconcile the scoring and reach a consensus on how to categorize the call. For example, calls that do not adhere to most of the required components of the specialized quitline program are coded as standard quitline. Final analyses will address differences between the randomly assigned intervention group and raters’ evaluation of the content of the intervention received. Specialized coaches are aware of the fidelity assessment criteria and will receive feedback and follow-up training when their calls do not meet the criteria. Examples of follow-up training include “cheat sheets” provided to coaches with examples of plain language substitutes for jargon or examples of how to elicit stories and express empathy to participants with challenging life contexts.
To evaluate fidelity of the navigation intervention, research staff listen to audio-recorded calls and rate whether or not the navigator sufficiently: (1) explained the purpose of navigation in this study, and built rapport by assessing strengths, ability to cope with life challenges, and goals for personal growth during each call; (2) identified and prioritized participant needs, and took a history of past resources a participant has utilized; (3) identified community resources, made referrals, and jointly created actionable steps toward problem resolution for both the participant and the navigator; (4) redirected participants to the quitline if they wanted to discuss cessation; and (5) closed each call by scheduling call-backs, confirming contact information and asking if the participant had questions. The navigator is aware of the fidelity assessment criteria and receives performance feedback and follow-up training as applicable.
Data Collection from Multiple Sources
2-1-1 Data Shared with the Research Team.
Contact information including name, address, and telephone number is shared with the research team along with the reason(s) for each participant’s call to 2-1-1 so the research team can track problem resolution.
Telephone Surveys Administered by the Research Team.
Baseline.
Standard measures from the North American Quitline Consortium Minimal Dataset for Quitlines45 are used. Socio-demographics (age, sex, race/ethnicity, sexual orientation, education, income, employment), health and healthcare access (health insurance status and type, regular doctor, history of 13 chronic conditions), smoking history (age at smoking initiation, current use of other tobacco products), nicotine dependence measured by the Heaviness of Smoking Index51 (cigarettes per day; time elapsed between waking and smoking), cessation history (last quit attempt and length of quit, prior use of pharmacologic cessation aids, self-help, and counseling services to quit), environment (living with a smoker, smoke-free home rules, workplace smoking rules, and coworkers who smoke), and intention to quit are assessed (Table 2). Items developed for this study assess how participants obtain cigarettes, money spent on cigarettes, and preferred brand of cigarettes.
Table 2.
Survey Measures
| Measures | Baseline | 3-Month | 6-Month |
|---|---|---|---|
| Socio-demographics | x | ||
| Health and healthcare access | x | ||
| Smoking history | x | ||
| Nicotine dependence | x | x | x |
| Cessation history | x | ||
| Smoke free home rules | x | x | |
| Workplace smoking | x | ||
| Intention to quit (if not quit at follow up) | x1 | x | x |
| Unmet basic needs | x | x | x |
| Perceived Stress Scale (Cohen 4-item) | x | x | x |
| Sleep quality (Pittsburgh Sleep Quality Index) | x | x | x |
| Social support (PROMIS) | x | x | |
| Depression (PHQ-2) | x | x | x |
| Self-rated health (poor-excellent) | x | ||
| Cessation, aids & quit attempts | x | x | |
| Confidence in staying quit (if applicable) | x | x | |
| Basic needs problem resolution | x | x | |
| Evaluation of intervention components | x | ||
| Evaluation of print materials | x | ||
| Life Satisfaction (BRFSS) | x | ||
| Purpose (Steger’s Meaning in Life) | x |
All participants must report an interest in quitting smoking in the next 30 days to be enrolled in a quitline program
Measures specific to our conceptual model and used in previous studies include: (1) Unmet basic needs: 10 items assess the likelihood that the smoker’s safety, housing, food, employment, and different financial needs (bills, necessities, unexpected expenses, childcare) will be met in the next month;52 (2) Cohen’s Perceived Stress Scale (4 items);53 (3) two items adapted from the Pittsburgh Sleep Quality Index54 rate sleep quality overall in the past month on a 4-point response scale from very bad to very good, and how often they have trouble sleeping (never, <1/week, 1–2 times/week, 3 or more times/week); (4) three social support items from the PROMIS Emotional Support item bank55 assess whether participants have someone who understands their problems, someone who will listen when they need to talk, and someone to turn to for suggestions about how to deal with a problem, and an additional item created by the study team assesses whether they have someone who will help them if they decide to quit smoking, all on 5-point response scales from never to always; (5) the PHQ-2 depression screener;56 and (6) self-rated health (excellent-poor).
Follow-up Surveys at 3 & 6 Months.
Measures repeated from baseline are reported in Table 2. The primary study outcomes are cessation-related. Participants are asked if they smoked at all in the past 7 days57 and past 30 days to assess point prevalence abstinence.58 Those who report any smoking in the past 7 days are asked if they quit for at least 24 hours since the previous survey. All participants report use of any pharmacologic cessation aids (i.e., NRT, bupropion, Chantix), self-help, or counseling resources since the prior survey or intend to use any in the next 3 months. We also ask participants how they obtained NRT, such as from a doctor, quitline, retail store, friend or family member. Successful quitters (≥ 7 days) report their confidence in staying quit and all others report their current intention to quit.59
Follow-up surveys also assess changes in unmet basic needs and problem resolution for each reason they called 2-1-1 at enrollment. Life satisfaction (1 item60) and life purpose (2 items adapted from Steger’s Meaning in Life Questionnaire61) are assessed with 4-point response scales: very dissatisfied to very satisfied and strongly disagree to strongly agree, respectively. Evaluations of the quitline and navigation staff assess user experience (easy to talk to, cared about me as a person, expert at helping me solve problems, and understood my life situation) on 4-point response scales from strongly disagree to strongly agree.43,62,63 Evaluations of the program and print materials include whether participants remembered them, used them and would recommend them to a friend.
Biochemical Validation of Self-Reported Smoking Cessation Collected by the Research Team.
All participants who complete the 6-month follow-up survey and report ≥ 7-day smoking abstinence are invited to participate in a biochemical validation sub-study and receive an additional $25–$35. Those who accept are administered a breath test using the coVita Micro+ Smokerlyzer developed by Bedfont Scientific. This device instantly measures the amount of CO on a smoker’s breath and has been used to biochemically assess individual’s smoking status and validate abstinence.64,65 The device captures results in ppm (CO) in lungs, collects a range of 0–500ppm, and has built-in technology to ensure infection control. The results are added to the participant’s study record. For analysis, we will use the recommended 8ppm cut-point as identifying a participant as a smoker, based on prior research.66
In addition to the smokerlyzer, participants are also offered a urine cotinine test to validate self-reported abstinence. This option was added to address those with transportation barriers and those who reside outside of the St. Louis area. Using the NicAlert™ test in their homes, participants dip a test strip into their urine sample at a depth of 1/2 inch for 20 seconds then lay it flat for 10–15 minutes. The result appears as a red band within one of six “levels” on the test strip. Participants send a digital photo of the test strip to the study team by text or email. The result is added to the participant’s study record. We provide visual step-by-step instructions for test use, review those instructions with participants prior to mailing the test, and are available by phone to answer questions. For analysis, we will use a 50ng/ml cut-point to identify someone as a smoker (Level 3 on the test strip) as recommended in prior research.66
Data Collected by the Basic Needs Navigator.
We developed a computer database to track the number, dates, duration, and content of navigator calls. Most qualitative content is recorded as notes in free text boxes. During the introductory call, the navigator records qualitative information on participants’ strengths, goals, and coping strategies, and prioritizes up to three needs to address first. During each navigation call thereafter, the navigator records progress made on previously identified unmet basic needs and notes any new needs that the participant may have. Additional questions may be asked for each need reported. For example, the basic needs navigator may ask participants reporting certain housing needs how many others live with them, whether they have enough furniture, whether they have ever applied for Section 8 housing, and/or their history of eviction and homelessness.
The navigator also records the types of resources participants have used in the past including supplemental income, food assistance programs, case management, and ongoing support from a community organization. At the end of the introductory call, the navigator also may record whether the participant has the documents such as a driver’s license, birth certificate (for self and/or child), proof of income, or Medicaid card needed to establish identity and/or eligibility for certain resources.
Data Collected by Optum and Shared with the Research Team.
Optum records the number and dates of calls attempts and completed, as well as the type of calls completed (e.g., enrollment, proactive counseling, ad hoc calls) and whether the calls were inbound to the quitline or outbound from the quitline. These provide objective process measures for each participant enrolled in the trial. Further, Optum records who participates in their Text2Quit and Internet programs.
Planned Data Analyses.
Sample Size and Power Considerations.
To be consistent with national reporting guidelines and evidence reviews, the primary cessation outcome is 7-day point prevalence abstinence measured at 6 months post-baseline following an intent-to-treat analysis approach. Estimated quit rates were based on the range of 6-month cessation rates from previous Optum clients which was consistent with intervention effects in a previous review of telephone cessation trials12 (Table 3). The sample size estimation is based on our plans to conduct intent-to-treat analyses. Thus, all participants who completed a baseline assessment, were randomized, and were not reported to have died during the study period will be included in the analysis. It will be assumed that those lost to follow up, refusing interviews, or otherwise unreachable are still smokers. We established 5% as the smallest meaningful difference between study groups.
Table 3.
Sample Size Estimation
| Quit rate: total study sample | Comparing quit rates by group | Odds ratio | Total sample size needed† |
|---|---|---|---|
| 8% | 5% vs. 10% | 2.10 | 870 |
| 10% | 7% vs. 12% | 1.80 | 1078 |
| 12% | 9% vs. 14% | 1.60 | 1276 |
| 14% | 11% vs. 16% | 1.50 | 1466 |
Total N assumes equal group sizes; Power=.80; Alpha=.05
G*Power was used to conduct power calculations for proportions.68 We project a 5% rate of 7-day abstinence among smokers in the standard quitline only group at 6-month follow-up. To identify 7-day abstinence rates that are 5% in the standard quitline only condition and 10% or higher in any other intervention group (our primary hypothesis), 435 smokers are needed in each of the two groups (N=870 total) for a Z-test to detect the difference at a 5% level of significance and 80% power.67 Comparable effects measured as odds ratios that would be statistically significant for each sample size estimate are shown in Table 3. If the quit rate in the standard quitline only group is higher than projected, larger sample sizes are needed to find a 5% difference between groups. Thus, with our baseline sample of 2,000 smokers (500 per group), we will have sufficient power for testing our primary hypothesis of a 5% difference between groups for a range of quit rates.
Feasibility.
Missouri 2-1-1 received 204,432 calls for assistance in 2017,69 and previous surveys of 2-1-1 callers have found high smoking rates (>30%).43,70 We estimate that to enroll 2000 participants, 2-1-1 would need to invite over 15,000 callers to be screened for eligibility for our study over the 3.5-year recruitment period and provide contact information of interested participants for approximately 13 smokers to the research team each week, assuming we could enroll 70–75% of those, similar to previous recruitment rates from 2-1-1.43 Our period of planned recruitment runs from June 2017 to June 2020 with follow-up data collection ending in December 2020 and data analysis continuing through the end of the study in June 2021. We may extend data collection timelines if needed to reach recruitment goals or allow for more time to complete the final 6 month survey and biochemical validation before classifying a participant as a non-respondent.
Primary Data Analyses.
Group-level prevalence of abstinence at 6-month follow up will be calculated by dividing the number of participants in each group who meet the binary 7-day abstinence criterion by the number of participants randomized to that group at baseline. In preliminary analyses, we will use t-test and chi-square tests to assess group differences for continuous and categorical sociodemographic and other baseline variables, respectively. We will explore group differences for the first seven categories of variables measured at baseline shown in Table 2. We expect that the four intervention groups will not differ on baseline sample characteristics due to random assignment and a large sample size. Our primary analysis will follow intent-to-treat principles; we will use logistic regression to examine whether smoking abstinence is higher in the combined intervention groups compared to the standard quitline only group using three dummy variables with the standard quitline only group as the referent. Odds ratios and 95% confidence intervals for group differences in abstinence rates will be used to quantify the association. We will not include covariates in the logistic model testing the primary hypothesis unless we find variables that are significantly different among intervention groups at baseline.
Additional Data Analyses.
Sensitivity analyses will be conducted to report the range of abstinence under different conditions. Similar power estimates will apply when analyses involve the full sample. For example, we will compare the abstinence rates between (1) all self-reported quitters vs. non quitters and lost to follow up, (2) self-reported quitters who agreed to participate in the biochemical verification test vs. non quitters, lost to follow up, and those who refused the biochemical verification test, (3) self-reported quitters who completed the biochemical verification test vs. non quitters, lost to follow up, and those who refused or did not complete the biochemical verification test, and (4) self-reported quitters whose non-smoking status was verified by the biochemical verification test vs. non quitters, lost to follow up, and those without biochemical verification.
All analyses will be repeated to test intervention effects on secondary trial outcomes including 30-day point prevalence abstinence and 24-hour quit attempts measured at 3- and 6-month follow up, as well as several measures of intervention dose. For example, we will examine both the total number and types of quitline services used (coaching calls, Text2Quit, Internet program, NRT), the number of navigation and/or cessation counseling calls completed and completion of the quitline cessation program coded as a binary variable (4 vs. <4 calls). We will also explore differences by intervention fidelity (e.g., program content delivered as intended vs. not).
Statistical tests will be chosen based on each outcome. For example, differences in the type of quitline services used by the intervention groups will be compared using multinomial logistic regression. Differences in the number of calls completed by intervention group members (a count variable) will be compared using Poisson regression. Binary logistic regression will be used to examine the association between completion of the quitline telephone coaching program (4+ calls) and intervention group.
Discussion
Low-income populations bear a greater burden of smoking and smoking-related disease than other populations, and standard smoking cessation programs may not adequately address the unmet basic needs and unique life context that can make quitting more difficult. This study integrates health and social service interventions in a real-world field trial involving the nation’s largest information and referral network for low-income Americans (2-1-1) and the largest tobacco quitline provider (Optum). Specialized Quitline services designed for low-income smokers and Basic Needs Navigation to assist them in resolving unmet needs are expected to improve cessation rates in this vulnerable population.
The intervention strategies we will test involve established approaches with proven effectiveness, but combined in a novel way. Finding efficient and sustainable ways to enhance and deliver proven cessation science to low-income populations is essential to eliminating smoking-related cancer disparities. Working with practice organizations in real-world conditions creates challenges for randomization and attrition, but our design will increase confidence in the reproducibility of effects and the potential for spread and sustainability of positive study results.
Acknowledgements
This research is supported by funding from the National Cancer Institute (R01CA201429; PI: Kreuter), but NCI was not involved in the design or implementation of the study. We thank all the participants for their time. We thank 2-1-1 of Missouri and Illinois for their support and recruitment efforts (Regina Greer, Kristin Womack, 2-1-1 information specialists), the Missouri Tobacco Quitline for its support and partnership (Valerie Howard), Optum quitline coaches and staff who have contributed to the final study design and implementation (Alula Torres, Kristina Muramoto, Erica Salmon, and Ryan Hedrix), and Washington University Health Communication Research Laboratory members who contributed to the conduct of the study (Dominique Brown, Balaji Golla, Courtney Guntly, Erika Halsey, Eliot Jost, Alina Luke, Jordan Richardson, Mikayla Branz, Shannon Davis, Abbie Tolon, Merriah Croston, Eileen Michael, Bill Michalski, and Timothy Poor).
Appendix. Specialized Quit Coach Training Materials
| Training Component | Description |
|---|---|
| Training Workbook | • Designed to supplement the first three training modules • The workbook adds: ◦ Readings and activities such as brainstorming exercises and quizzes ◦ Strategies to engage, respond and deliver content to low income smokers ◦ Six first-person personas, or fictionalized descriptions of lowincome smokers created by the research team based on literature and prior experience used to convey social context of smoking in low-income groups and increase coaches’ understanding and empathy ◦ A plain language dictionary and “cheat sheet” that translate common smoking cessation and quitline jargon |
| Module 1: What are the Basic Needs and How are They Resolved | • Defines basic needs such as lack of food, housing, safety, money for necessities, transportation, employment, child care, and social support • Outlines common strategies for addressing basic needs among lowincome populations • Explains the project’s theory of behavior change |
| Module 2: Smoking Behaviors and Patterns in LowIncome Smokers | • Describes smoking behaviors and patterns in low-income smokers • Explains the difference between chronic and acute stressors and how stress affects quitting smoking • Illustrates how the social environment of low-income smokers may influence the type of social support they receive when quitting smoking |
| Module 3: Tactics to Help Engage, Respond, and Deliver Content to LowIncome Smokers |
• Teaches coaches how to deliver the specialized intervention • Coaches practice introducing their expertise, using plain language, asking probing questions, responding empathetically, and framing the strengths and challenges faced by low-income smokers • Coaches listen to sample standard vs. specialized coaching calls to reflect on differences |
| Module 4: Basic Needs Protocol | • Introduces study contacts and components • Describes study procedures and protocols ◦ More, varied call attempts • Training on the specialized coaching intervention content and the computerized coach support tools |
Footnotes
Conflicts of interest
Dr. Terry Bush is employed by Optum, a leading provider of state-supported tobacco quitlines in the U.S. All other authors have no conflicts of interest to report.
References
- 1.Centers for Disease Control and Prevention. Current Cigarette Smoking Among Adults-United States, 2005–2012. Morbidity and Mortality Weekly Report 2014;63(02):29–34. [PMC free article] [PubMed] [Google Scholar]
- 2.Siahpush M, McNeill A, Borland R, Fong G. Socioeconomic variations in nicotine dependence, self efficacy, and intention to quit across four countries: findings from the International Tobacco Control (ITC) Four Country Survey. Tobacco Control 2006;15(Supplement III):iii71–iii75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barbeau E, Krieger N, Soobader M. Working class matters: Socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. American Journal of Public Health 2004;94(2):269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flint A, Novotny T. Poverty status and cigarette smoking prevalence and cessation in the United States, 1983–1993: the independent risk of being poor. Tobacco Control 1997;6(1):14–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Businelle M, Kendzor D, Reitzel L, et al. Mechanisms linking socioeconomic status to smoking cessation: A structural equation modeling approach. Health Psychology 2010;29(3):262–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reid J, Hammond D, Boudreau C, Fong GT, Siahpush M, Collaboration I. Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: Findings from the International Tobacco Control Four Country Survey. Nicotine & Tobacco Research 2010;12:S20–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smit E, Fidler J, West R. The role of desire, duty, and intention in predicting attempts to quit smoking. Addiction 2011;106:844–851. [DOI] [PubMed] [Google Scholar]
- 8.Jamal A, King B, Neff L, Whitmill J, Babb S, Graffunder C. Current cigarette smoking among adults - United States, 2005–2015. Morbidity and Mortality Weekly Report 2016;65(44):1205–1211. [DOI] [PubMed] [Google Scholar]
- 9.Carpenter MJ, Ford ME, Cartmell K, Alberg AJ. Misperceptions of nicotine replacement therapy within racially and ethnically diverse smokers. Journal of the National Medical Association 2011;103(9–10):885–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Missouri Department of Health and Senior Services. County-level study – Tobacco use 2007; http://www.dhss.mo.gov/CommunityDataProfiles/ Accessed 2008.
- 11.Lichtenstein E, Glasgow R, Lando H, al e. Telephone counseling for smoking cessation: rationales and meta-analytic review of evidence. Health Education Research 1996;11(2):243–257. [DOI] [PubMed] [Google Scholar]
- 12.Stead L, Perera R, Lancaster T. Telephone counseling for smoking cessation (review). The Cochrane Database of Systematic Reviews 2006. 2009(3). [DOI] [PubMed] [Google Scholar]
- 13.McAfee T. Quitlines: A tool for research and dissemination of evidence-based cessation practices. American Journal of Preventive Medicine 2007;33(6):S357–367. [DOI] [PubMed] [Google Scholar]
- 14.Fiore M. US Public Health Service clinical practice guideline: Treating tobacco use and dependence. Respiratory Care 2000;45(10):1200–1260. [PubMed] [Google Scholar]
- 15.Zaza S, Briss PA, Harris KW. The guide to community preventive services: What works to promote health? New York, NY: Oxford University Press; 2005. [Google Scholar]
- 16.Bernstein SL, Weiss JM, Toll B, Zbikowski SM. Association between utilization of quitline services and probability of tobacco abstinence in low-income smokers. Journal of Substance Abuse Treatment 2016;71:58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fraser DL, Fiore MC, Kobinsky K, et al. A randomized trial of incentives for smoking treatment in Medicaid members. American Journal of Preventive Medicine 2017;53(6):754–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Slater JS, Nelson CL, Parks ML, Ebbert JO. Connecting low-income smokers to tobacco treatment services. Addictive Behaviors 2016;52:108–114. [DOI] [PubMed] [Google Scholar]
- 19.Vidrine JI, Shete S, Cao Y, et al. Ask-Advise-Connect. JAMA Intern Med 2013;173(6):458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thompson T, Kreuter MW, Boyum S. Promoting health by addressing basic needs: Effect of problem resolution on contacting health referrals. Health Education and Behavior 2016;43(2):201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thompson T, McQueen A, Croston M, et al. Social needs and health-related outcomes among Medicaid beneficiaries Under review. [DOI] [PubMed]
- 22.Mullainathan S, Shafir E. Scarcity: Why having too little means so much New York: Times Books; 2013. [Google Scholar]
- 23.Senn T, Walsh J, Carey M. The mediating roles of perceived stress and health behaviors in the relation between objective, subjective, and neighborhood socioeconomic status and perceived health. Annals of Behavioral Medicine 2014;48:215–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kissane R. What’s need got to do with it? Barriers to use of nonprofit social services. Journal of Sociology and Social Welfare 2003;30(2):127–148. [Google Scholar]
- 25.Remler D, Glied S. What other programs can teach us: Increasing participation in health insurance programs. American Journal of Public Health 2003;93(1):67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu C-F, Eamon M. Need for and barriers to accessing public benefits among lowin-come families with children. Children and Youth Services Review 2010;32:58–66. [Google Scholar]
- 27.Melchior M, Caspi A, Howard L, et al. Mental health context of food insecurity: a representative cohort of families with young children. Pediatrics 2009;124(4):e564–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ng W, Diener E, Arora R, Harter J. Affluence, feelings of stress, and well-being. Social Indicators Research 2009;94:257–271. [Google Scholar]
- 29.Blazer D, Sachs-Ericsson N, Hybels C. Perception of unmet basic needs as a predictor of depressive symptoms among community-dwelling older adults. Journal of Gerontology: Medical Sciences 2007;62(2):191–195. [DOI] [PubMed] [Google Scholar]
- 30.Sachs-Ericsson N, Schatschneider C, Blazer D. Perception of unmet basic needs as a predictor of physical functioning among community-dwelling older adults. Journal of Aging and Health 2006;18(6):852–868. [DOI] [PubMed] [Google Scholar]
- 31.Blazer D, Sachs-Ericsson N, Hybels C. Perception of unmet basic needs as a predictor of mortality among community-dwelling older adults. American Journal of Public Health 2005;95(2):299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Taylor S, Repetti R. Health Psychology: What is an Unhealthy Environment and How Does it Get Under the Skin? Annual Review of Psychology 1997;48:411–447. [DOI] [PubMed] [Google Scholar]
- 33.Lynch J, Kaplan G, Shema S. Cumulative Impact of Sustained Economic Hardship on Physical, Cognitive, Psychological, and Social Functioning. New England Journal of Medicine 1997;337:1889–1895. [DOI] [PubMed] [Google Scholar]
- 34.Kushel M, Gupta R, Gee L, Haas J. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med 2006;21(1):71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Timmerman G, Acton G. The relationship between basic need satisfaction and emotional eating. Issues in Mental Health Nursing 2001;22(7):691–701. [DOI] [PubMed] [Google Scholar]
- 36.Acton G, Malathum P. Basic need status and health-promoting self-care behavior in adults. Western Journal of Nursing Research 2000;22(7):796–811. [DOI] [PubMed] [Google Scholar]
- 37.Fitzpatrick-Lewis D, Ganann R, Krishnaratne S, Ciliska D, Kouyoumdjian F, Hwang S. Effectiveness of interventions to improve the health and housing status of homeless people: a rapid systematic review. BMC Public Health 2011;11:638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wolitski R, Kidder D, Pals S, et al. Randomized Trial of the Effects of Housing Assistance on the Health and Risk Behaviors of Homeless and Unstably Housed People Living with HIV. AIDS Behav 2010;14(3):493–503. [DOI] [PubMed] [Google Scholar]
- 39.Thomson H, Thomas S, Sellstrom E, Petticrew M. The Health Impacts of Housing Improvement: A Systematic Review of Intervention Studies from 1887 to 2007. American Journal of Public Health 2009;99(3):681–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leventhal T, Brooks-Gunn J. Moving to Opportunity: an Experimental Study of Neighborhood Effects on Mental Health. American Journal of Public Health 2003;93(9):1576–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ludwig J, Duncan G, Gennetian L, et al. Long-term neighborhood effects on low-income families: Evidence from moving to opportunity. Amercan Economic Review: Papers and Proceedings 2013;103(3):226–231. [Google Scholar]
- 42.Williams D, Costa M, Odunlami A, Mohammed S. Moving upstream: How interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract 2008;14(Suppl):S8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kreuter MW, Eddens KS, Alcaraz KI, et al. Use of cancer control referrals by 2-1-1 callers: A randomized trial. American Journal of Preventive Medicine 2012;43(6S5):S425–S434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire Atlanta, GA: Department of Health and Human Services; 2007. [Google Scholar]
- 45.Campbell H, Ossip-Klein D, Bailey L, Saul J, Research and Evaluation Working Group. Minimal dataset for quitlines: a best practice. Tobacco Control 2007;16:i16–i20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shea S, Stein A, Lantigua R, Basch C. Reliability of the behavioral risk factor survey in a triethnic population. American Journal of Epidemiology 1991;133(5):489–500. [DOI] [PubMed] [Google Scholar]
- 47.Brownson R, Eyler A, King A, Shyu Y, Brown D, Homan S. Reliability of information on physical activity and other chronic disease risk factors among US women aged 40 years or older. American Journal of Epidemiology 1999;149(4):379–391. [DOI] [PubMed] [Google Scholar]
- 48.Brownson R, Jackson-Thompson J, Wilkerson J, Kiani F. Reliability of information on chronic disease risk factors collected in the Missouri Behavioral Risk Factor Surveillance System. Epidemiology 1994;5(5):545–549. [PubMed] [Google Scholar]
- 49.Nelson D, Holtzman D, Bolen J, Stanwyck C, Mack K. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS). Social and Preventive Medicine 2001;46 Suppl 1:S3–S42. [PubMed] [Google Scholar]
- 50.King A, Cao D, Southard C, Matthews A. Racial differences in eligibility and enrollment in a smoking cessation clinical trial. Health Psychology 2011;30(1):40–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. British Journal of Addiction 1989;84(7):791–800. [DOI] [PubMed] [Google Scholar]
- 52.Kreuter MW, McQueen A, Boyum S, Fu Q. Unmet basic needs and health intervention effectiveness in low-income populations. Preventive Medicine 2016;91:70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cohen S, Kamarck T, Mermelstein RJ. A global measure of perceived stress. Journal of Health and Social Behavior 1983;24:385–396. [PubMed] [Google Scholar]
- 54.Buysse D, Reynolds C, Monk T, Berman S, Kupfer D. The Pittsburgh Sleep Quality Index (PSQI): A new instrument for psychiatric research and practice. Psychiatry Research 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 55.PROMIS. NIH Toolbox item bank v2.0 Emotional support (Ages 18+) - Fixed form Accessed July 2018 online at http://www.healthmeasures.net/administrator/components/com_instruments/uploads/TOOLBOX%20FF%20v2.0%20-%20Emotional%20Support%2018%20plus_11-172016.pdf.
- 56.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care 2002;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 57.Velicer WF, Prochaska JO. A comparison of four self-report smoking cessation outcome measures. Addictive Behaviors 2004;29:51–60. [DOI] [PubMed] [Google Scholar]
- 58.Velicer W, Prochaska J, Rossi J, Snow M. Assessing outcome in smoking cessation studies. Psychological Bulletin 1992;111(1):23–41. [DOI] [PubMed] [Google Scholar]
- 59.Lipkus I, Lyna P, Rimer B. Using tailored interventions to enhance smoking cessation among African-American smokers at a community health center. Nicotine & Tobacco Research 1999;1:77–85. [DOI] [PubMed] [Google Scholar]
- 60.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System (BRFSS) survey questionnaire U.S. Department of Health and Human Services; Atlanta, GA: Available at https://www.cdc.gov/brfss/questionnaires/pdfques/2017_BRFSS_Pub_Ques_508_tagged.pdf. 2017. [Google Scholar]
- 61.Steger MF, Frazier P, Oishi S, Kaler M. The Meaning in Life Questionnaire: Assessing the presence of and search for meaning in life. Journal of Counseling Psychology 2006;53(1):80–93. [Google Scholar]
- 62.McQueen A, Kreuter MW. Women’s cognitive and affective reactions to breast cancer survivor stories: A structural equation analysis. Patient Education and Counseling 2010;81(Suppl. 1):15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McQueen A, Kreuter MW, Kalesan B, Alcaraz K. Understanding narrative effects: The impact of breast cancer survivor stories on message processing: Attitudes and beliefs in African American women. Health Psychology 2011;30(6):674–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bedfont Scientific Ltd. Smokerlyzer Range User Manual Available online at https://www.bedfont.com/file/2494-LAB679%20Smokerlyzer%20Manual%20Issue%203.pdf.
- 65.Vasthare R, Kumar S, Arron LY. Carbon monoxide breath analyzers and its role in tobacco cessation: A narrative review of literature. Journal of International Oral Health 2018;10:71–76. [Google Scholar]
- 66.Benowitz N, Ahijevych K, Hall S, et al. Biochemical verification of tobacco use and cessation. Nicotine & Tobacco Research 2002;4(2):149–159. [DOI] [PubMed] [Google Scholar]
- 67.D’Agostino RB, Chase W, Belanger A. The Appropriateness of Some Common Procedures for Testing the Equality of Two Independent Binomial Populations. The American Statistician 1988;42(3):198–202. [Google Scholar]
- 68.Faul P, Erdfelder E, Lang A, Buchner A. G*Power: A flexible statistical power analysis for the social, behavioral, and biomedical sciences Behavior Research Methods 2007;39(2):175–191. [DOI] [PubMed] [Google Scholar]
- 69.Health Communication Research Laboratory, Health Communication Impact. Top service requests for MO 2-1-1 in 2017 Accessed at http://211mo.211counts.org/.
- 70.Eddens K, Kreuter MW, Archer K. Proactive screening for health needs in United Way’s 2-1-1 information and referral service. Journal of Social Service Research 2011;37(2):113–123 [DOI] [PMC free article] [PubMed] [Google Scholar]


