Abstract
Voluntary hyperventilation triggers seizures in the vast majority of people with absence epilepsy. The mechanisms that underlie this phenomenon remain unknown. Herein, we review observations – many made long ago – that provide insight into the relationship between breathing and absence seizures.
Keywords: Epilepsy, Respiration, Seizure, Circuit, Thalamus, pH
1. Clinical considerations
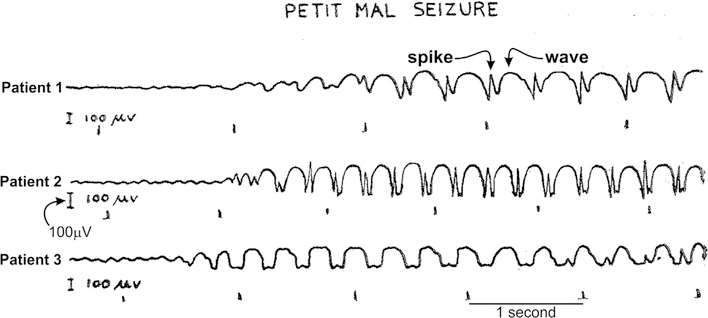
In 1770, a Swiss physician named Samuel Tissot reported his observations of a young girl who lost consciousness multiple times a day (Tissot, 1770). Although impairment of consciousness was already a known symptom of epilepsy, the lack of any concomitant convulsions led Tissot to conclude that the girl’s epilepsy was distinct (Tissot, 1770). Tissot’s instincts were correct and he is credited with the coining these events as petit mal seizures (Tissot, 1770). But only much later, in 1935, did we learn about the dramatic, highly-stereotyped, electrical activity patterns that likely pulsed within the girl’s brain during her brief episodes of unconsciousness. It was Gibbs et al. (1935) who used newly developed electroencephalogram (EEG) recording techniques to provide the first description of the characteristic 3-Hz, spike-and-wave electrical discharge (SWD) now synonymous with absence epilepsy (Fig. 1). Over 80 years later, clinicians still use the electrographic signature of the SWD, accompanied by a loss of consciousness, as diagnostic criteria for absence epilepsy.
Fig. 1.
Early electroencephalogram (EEG) recordings of absence seizures. A single electrode was placed on the vertex of the skull. A second, reference electrode was placed into the lobe of the ear. Hypodermic needles were used as electrodes. Absence seizure recordings from three different patients are shown. The seizure is associated with periodic, three-per-second events that are composed of a relatively slow, rounded component (i.e. the wave) that is punctuated by a sharp, rapidly evolving upward component (i.e. the spike). Note the abrupt onset of the seizure. Modified from Gibbs et al. (1935).
In 1989, the International League Against Epilepsy (ILAE) partitioned absence epilepsy into two distinct epilepsy syndromes: Childhood Absence Epilepsy (CAE) and Juvenile Absence Epilepsy (JAE) (ILAE, 1989). While seizures associated with CAE and JAE are both characterized by impaired consciousness and accompanying 3–4 Hz SWDs, differences between the two syndromes exist. In 2004, Trinka et al. retrospectively examined 163 patients to identify pyknoleptic absences and non-pyknoleptic absences (Trinka, 2004). While such terminology has generally fallen out of favor, pyknoleptic absences refer to seizures that occur in clusters, often hundreds per day, while non-pyknoleptic absences occur less frequently (i.e. < 1 per day). Pyknoleptic absences are also associated with an abrupt and severe state of unconsciousness, while the state of unconsciousness associated with non-pyknoleptic absences is often less pronounced.
When the operational distinction between pyknoleptic and non-pyknoleptic absences is applied to patients, absence epilepsy appears to subdivide into two syndromes with differing onset ages (Trinka, 2004). CAE, with a peak onset between 5 and 7 years of age (Matricardi et al., 2014), is primarily associated with frequent, abrupt absences (i.e. pyknoleptic). In contrast, patients with JAE (mean age of onset: 15 years) typically present with infrequent absences (i.e. non-pyknoleptic). Also, relative to CAE, patients with JAE are more likely to present with additional, different seizure types at the time of diagnosis. Specifically, Trinka et al. reported that nearly 95% of JAE patients eventually develop generalized tonic clonic seizures (GTCS), compared to 69% of CAE patients; other reports suggest that GTCS prevalence in the CAE population may be much lower (Shinnar, 2015).
In aggregate, the data indicate that two distinct absence epilepsy syndromes exist. In CAE, relatively young patients present with frequent, abrupt seizures of a singular form that generally subside with age. In JAE, generally older patients present with fewer, less pronounced absence seizures, but also present with other seizure subtypes that, collectively, are less likely to remit. Despite these differences, much overlap between CAE and JAE exists, leading some to argue that absence epilepsy represents a continuum of syndromes primarily characterized by SWDs (Reutens and Berkovic, 1995; Guilhoto, 2017). Moreover, absence seizures are not unique to children and juveniles. Absence seizures occur in adults (Gastaut, 1981), more often in women (Gastaut, 1981; Panayiotopoulos, 1992). Sometimes these seizures recur in patients who had absence seizures in their youth (Michelucci, 1996; Berkovic and Bladin, 1983). Usually, these absence episodes arise in conjunction with other idiopathic generalized epilepsies (IGE) (Marini et al., 2003) or psychoses (Iivanainen et al., 1984). Thus, while CAE represents the prototypical form of the epileptic disorder, absence seizures consisting of SWDs with concomitant impaired consciousness are observed in wide-ranging clinical contexts. Finally, electrographic SWDs and unconsciousness are not the only feature of absence epilepsy; associated comorbidities include attentional problems, depression, anxiety and memory impairments (Tenney and Glauser, 2013).
2. Etiology
The causes of absence epilepsy are complex and varied, but primarily involve genetic mutations. While many rodent studies highlight potential mechanisms underlying absence epilepsy (Depaulis and Charpier, 2017; Depaulis et al., 2016; Felix, 2002; Cortez et al., 2016; Coenen and Van Luijtelaar, 2003), herein we primarily focus on human genetic mutations associated with the disorder. To date, identified human mutations include genes encoding for specific subunits of (1) the primary ionotropic receptor for γ-aminobutyric acid (GABA), the main inhibitory neurotransmitter in the brain, and (2) the low threshold, T-type calcium channel. The primary ionotropic receptor for GABA, also called the A-type GABA (GABAA) receptor, is a pentameric structure, wherein each of the 5 subunits corresponds to one of four subunit subtypes: α, β, δ, γ (Jones-Davis and Macdonald, 2003; Macdonald et al., 2010; Rudolph et al., 2001). Identified, CAE-associated mutations have been localized to the γ2 (Tan, 2007); α1 (Cossette, 2002; Lachance-Touchette, 2011; Maljevic, 2006) and β3 (Huntsman et al., 1999; Roden et al., 2010; Holopainen, 2001) subunits of the GABAA receptor.
While more studies are required, the aforementioned GABAA receptor subunit mutations generally appear to reduce the capacity of the receptor to traffic to the plasma membrane of neurons (Berkovic and Bladin, 1983). For example, mice heterozygous for the R43Q point mutation in the γ2 subunit produce SWDs (Berkovic and Bladin, 1983). Cortical neurons in these mice receive reduced GABAergic inhibition, an effect attributed to reduced surface expression of the receptor; GABAergic inhibition was largely spared in other brain structures involved in SWD generation. Similar to the R43Q mutation in the γ2 subunit, α1 subunit mutations are also associated with both increased SWDs (Cossette, 2002; Maljevic, 2006) and reduced GABAA receptor expression at the cell membrane (Lachance-Touchette, 2011; Maljevic, 2006). Finally, mutations in the β3 subunit of the GABAA receptor are also associated with SWDs. And again, the emerging picture indicates that β3 subunit mutations reduce the number of functional GABAA receptors and, generally, reduce inhibition (Jones-Davis and Macdonald, 2003; Huntsman et al., 1999; Roden et al., 2010).
In contrast to the aforementioned, loss-of-function mutations in the GABAA receptor, T-Type Ca2+ channel mutations associated with absence epilepsy lead to a gain of function. Chen et al. originally identified missense mutations in CACNA1H, the gene encoding the α1H subunit of the T-type channel complex, in a Han Chinese cohort (Chen, 2003). Subsequent studies on other, non-Chinese populations confirm that CACNA1H mutations are associated with CAE (Heron, 2007). Consistent with these observations, several studies have demonstrated that CAE-associated CACNA1H mutations generally lead to greater calcium influx through the channel following activation (Khosravani, 2004; Vitko, 2005; Peloquin, 2006). Greater Ca2+ influx, in turn, is thought to support robust low-threshold Ca2+ spikes that sustain SWDs (see below). The induction of absence seizure-like SWDs in otherwise normal rats by the introduction of the human-associated, C456S, gain-of-function CACNA1H mutation (Wang, 2015) supports this hypothesis. However, this conclusion warrants a word of caution. Epilepsy-associated variants in CACNA1H are also observed in unaffected individuals (Heron, 2007), suggesting that T-Type Ca2+ channel mutations appear to increase CAE susceptibility, but alone do not cause CAE. Indeed, the emerging paradigm is that most epilepsies are complex disorders that do not arise from a single, clear biological origin (Heron, 2007; Staley, 2015). Instead, most epilepsies are multifactorial disorders that likely involve mutations in several proteins (i.e. polygenic), and are disorders often influenced by the environment, a recurring theme within this Special Issue.
3. Outcome & treatment
As remission often occurs by early adulthood, absence epilepsy is frequently described as a benign disorder. Such a designation requires reconsideration (Tenney and Glauser, 2013). First, reported remission rates are variable and generally not as high as commonly perceived. Several studies report that approximately 60% of subjects remit by 20 years of age (Trinka, 2004; Loiseau et al., 1983; Wirrell et al., 1996), although the number of seizurefree subjects no longer requiring medication is likely lower (Sillanpää et al., 1998). Second, prior to possible remission, a cocktail of anti-seizure drugs (ASDs) – ethosuximide, valproic acid and lamotrigine – is sometimes recommended to manage seizures (Glauser, 2013). While ASD cocktails are at times effective, the treatment strategy also often contributes to additive and intolerable side-effects (Matricardi et al., 2014). Moreover, little is known regarding the effects of such a blunt pharmacological strategy on the developing brain. Third, long-term cognitive and psychosocial problems are prominent in absence patients. Comorbidities include social anxiety disorder, depression, attention deficit disorder and behavioral/linguistic problems (Tenney and Glauser, 2013; Wirrell, 1997; Caplan, 2008; Caplan, 2015). Considering remission rates, available treatment methods and comorbidities, labeling absence seizures as benign appears ill-suited.
4. Hyperventilation triggers absence seizures
SWDs are triggered by voluntary hyperventilation in over 90% of patients with absence epilepsy (Glauser, 2013; Wirrell, 1997; Caplan, 2008, 2015; Panayiotopoulos, 1999), a phenomenon initially documented in the early 20th century (Watemberg, 2015; Giannakodimos et al., 1995). The use of hyperventilation to unequivocally and quickly diagnose patients with absence epilepsy is now commonplace, and largely obviates the need for a protracted EEG recording procedure to capture spontaneous seizures (Adams and Leuders, 1981). The effectiveness of this diagnostic tool even provides fodder for Holowach and O’Leary’s suggestion that a diagnosis of absence epilepsy “should be seriously questioned [if one] does not have an attack on hyperventilation.” (Holowach et al., 1962).
Hyperventilation elicits high-amplitude, slow and rhythmic brain activity even in nonepileptic individuals (Nims et al., 1940; Lum et al., 2002). This phenomenon, known as Hyperventilation-Induced, High-Amplitude Rhythmic Slowing (HIHARS), is often confused with SWD activity in the EEG. HIHARS and SWDs are both observed on most cortical recording electrodes, reflecting a generalized EEG pattern. HIHARS also evokes many of the automatisms – staring, eye opening/eyelid fluttering, yawning – observed during absence seizures (Lum et al., 2002). Electrographically, however, HIHARS and seizure-associated SWDs are distinct EEG events. HIHARS consists of slow (2–5 Hz), high-amplitude (>100 mV) electrical activity reminiscent of delta waves observed during slow-wave sleep (Khosravani, 2004). In contrast, spontaneous and hyperventilation-triggered SWDs observed in absence patients consist of the canonical 3 Hz, high-amplitude, nearly sinusoidal EEG wave that is punctuated by an abrupt and rapid spike during each cycle of the oscillation (see Fig. 1). Thus, while hyperventilation can clearly alter brain activity in healthy individuals, it is also clear that such rapid breathing evokes distinct electrical activity patterns in absence patients.
5. Physiological response to hyperventilation
To understand how hyperventilation alters EEG patterns, it is important to understand the relationship between breathing and blood pH, a relationship that is critically dependent on carbon dioxide (CO2) in the blood. Indeed, in 1942, Gibbs et al. admonished brain researchers by suggesting that “students of cerebral function have, in general, paid too little attention to carbon dioxide.” (Gibbs et al., 1942) In that spirit, we begin by directing our attention to CO2.
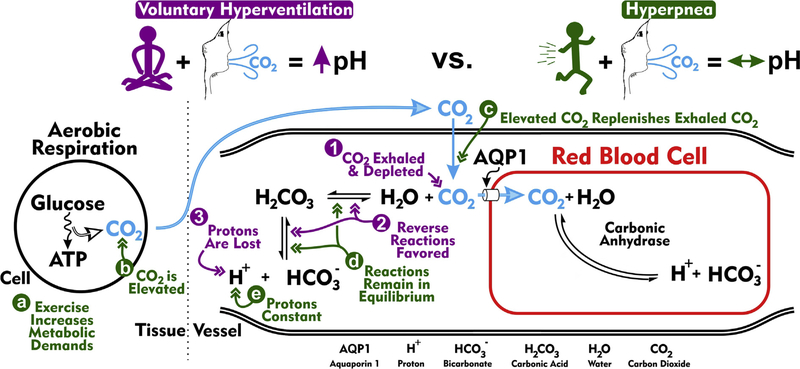
CO2 is a waste product of aerobic respiration, the series of biochemical events utilized by cells to convert glucose metabolites into energy (Fig. 2). Once produced, CO2 diffuses out of the tissue and into the blood plasma. Most plasma CO2 enters red blood cells, where it associates with water to produce bicarbonate and a hydrogen ion, a reaction catalyzed by carbonic anhydrase. Plasma CO2 that does not enter red blood cells is converted into carbonic acid (H2CO3), an uncatalyzed reaction. Carbonic acid, in turn, dissociates into bicarbonate and hydrogen ions. The concentration of the free hydrogen ions ([H+]), in turn, determines blood plasma pH. Naturally, this reaction can proceed in the reverse direction such that bicarbonate and a hydrogen ion associate to form carbonic acid. When this reverse reaction is favored, [H+] drops and the blood becomes more alkaline. The reverse reaction is favored when the partial pressure of CO2 (pCO2) drops.
Fig. 2.
Acid-base blood physiology during rapid breathing. The schematic depicts biochemical reactions largely responsible for establishing blood pH. On the left is shown a cell situated in the tissue undergoing aerobic respiration, the process of converting glucose into ATP. Carbon dioxide (CO2) is produced during this conversion process. CO2 then diffuses into capillary plasma, after which the bulk is primarily transported into erythrocytes (red blood cells) via aquaporin 1 (AQP1) channels (Endeward, 2006). Within the red blood cell, CO2 associates with H2O (water) to produce H+ (proton) and (bicarbonate), a reaction catalyzed by carbonic anhydrase. Carbonic anhydrase is found in abundance in red blood cells, but not in the plasma. The dissociated proton acidifies the red blood cell and, in doing so, promotes the dissociation of hemoglobin and oxygen. A small portion of CO2 entering the capillary remains in the plasma. As in the red blood cell, plasma CO2 is also converted into H+ and , but this reaction is primarily not catalyzed by carbonic anhydrase [i.e. an uncatalyzed reaction (however, some carbonic anhydrase isoforms are localized to the extracellular surface of many cells (Boron, 2010; Svichar and Chesler, 2003), including red blood cells, and contribute to the catalyzed production of H+ and from CO2 and H2O (Svichar and Chesler, 2003)]. The uncatalyzed reaction reversibly proceeds through H2CO3 (carbonic acid) and occurs at low basal rates. Purple (1–3). Acid-base physiology during voluntary hyperventilation. Voluntary hyperventilation is defined by excessive breathing (high rate and quantity) leading to the pronounced ventilation of CO2 and ensuing respiratory alkalosis, a phenomenon in which blood plasma becomes alkaline. (1) Excessive ventilation reduces plasma concentrations of CO2. (2) CO2 depletion promotes the association of plasma H+ and to replenish, via H2CO3, CO2. (3) Favoring the reverse reactions reduces the concentration of plasma H+, thereby making the blood more alkaline. Green (a–e). Acid-base physiology during exercise-related hyperventilation (i.e. hyperpnea). (a) Unlike during voluntary hyperventilation, hyperpnea occurs during times of heightened metabolic demand. (b) Aerobic respiration associated with high metabolic demands produces high levels of CO2. (c) Increased CO2 production and subsequent diffusion into capillaries balances the increased CO2 exhalation. (d) The equilibria underlying CO2-H2O biochemical reactions remain unperturbed. (e) As these biochemical reactions remain in equilibrium, plasma protons are not lost and plasma pH is stable. Importantly, absence seizures are triggered by voluntary hyperventilation, but not hyperpnea.
Taking into account the aforementioned bicarbonate buffering system present in the blood plasma, we can begin to understand how hyperventilation alters blood pH (Fig. 2). Rapid breathing causes CO2 levels in the plasma to drop; in short, the individual blows off CO2. The drop in free CO2 in the blood plasma is called hypocapnia and promotes the reverse reaction in which carbonic acid dissociates into CO2 and water. The resultant drop in carbonic acid, in turn, promotes the association of bicarbonate and H+ ions to replenish depleted carbonic acid, a reaction that removes free H+ ions. In toto, as CO2 drops, the [H+] in the blood also drops, causing the blood to become more alkaline. This process during which rapid breathing alkalizes the blood is called respiratory alkalosis.
An important consideration regarding respiratory alkalosis is that rapid breathing occurs when metabolic activity is low. Accordingly, the CO2-producing, biochemical process of cellular aerobic respiration occurs at low rates. Under conditions of low CO2 production and high respiratory CO2 elimination, the pCO2 of blood drops and the blood alkalizes, as described above (see Fig. 2, purple). In contrast, elevated breathing during exercise, a phenomenon known as hyperpnea, is associated with increased metabolic demands. Under such conditions, high CO2 elimination is matched by high CO2 production (Fig. 2, green). As the pCO2 of blood is relatively stable during hyperpnea, the pH of blood does not change. The distinction between hyperventilation and hyperpnea is relevant, as the latter does not trigger seizures in absence patients (Esquivel et al., 1991), suggesting that absence seizures are specifically sensitive to blood pH.
Homeostatic mechanisms are in place to compensate for changes in blood pH. Namely, the vasculature responds when blood pH changes. Vessels normally dilate when blood acidifies, and constrict when blood alkalizes. The mechanisms by which vascular tone (i.e. dilation versus constriction) is modulated by blood pH are well-documented; as such, we direct the interested reader towards excellent reviews on the subject (Kontos et al., 1977; Cipolla, 2009; Boron and Boulpaep, 2009). Suffice to say, vascular tone is a highly regulated process that involves complex interactions between the endothelial cells that line the inner walls of blood vessels and the smooth muscle cells that contract or relax to change vessel diameter. The canonical vasodilatory effect of nitric oxide (NO) underscores the intimate interaction between endothelial cells and muscle cells: sheer stress sensed by transient receptor potential (TRP) channels on endothelial cells triggers the production of endothelial nitric oxide synthase (eNOS) to catalyze the production of NO, a diffusible molecule that relaxes nearby muscle cells (Boron and Boulpaep, 2009). Vascular tone is also directly regulated by pH, a process that involves internal calcium stores, calcium-activated potassium (BK) channels (Koide et al., 2012) and, possibly, TRP channels (Sonkusare, 2012).
Regardless of the specific mechanism, it is clear that vascular tone responds to blood CO2 and pH in healthy individuals. Interestingly, Nims et al (Gibbs et al., 1940) showed that inherent differences in this response likely exist between individuals with absence epilepsy and those without absence epilepsy. Specifically, the authors measured the CO2 content and pH of the carotid artery and jugular vein blood supplies, thereby enabling them to compare the physiochemical properties of blood entering and exiting the brain, respectively. The authors observed a standard response to hyperventilation in both epileptic and non-epileptic cohorts insofar that arterial blood CO2 dropped to comparable levels. However, following hyperventilation, the drop in CO2 content and concurrent alkalization of the jugular blood in absence epileptic individuals was consistently larger and persisted longer than that of healthy individuals. Taken together, the data indicate that (1) the blood supplying the brain is normal in absence patients, (2) the blood returning from the brain is different in absence patients, and (3) hyperventilation unmasks this difference. Thus, not only does voluntary hyperventilation trigger seizures in absence patients, but the brain’s response to hypocapnic episodes is also different. Although Nims et al. published their findings more than 75 years ago, it remains unclear if the two phenomena are related. The observation that CO2 inhalation can temporarily abolish absence seizures (Cossette, 2002; Lennox, 1928; Yang, 2014) suggests interdependence.
At present, no consensus exists regarding whether the observed EEG changes in response to hyperventilation result from hypocapnia, the concomitant change in brain pH, or a combination of the two. An explanation will likely require a better understanding of pH-sensitivity among specific elements within the neural circuits that generate absence seizures. Below, we begin by describing results that highlight how crosstalk between structures in the cortex and in the thalamus, a subcortical structure, may precipitate seizures in response to hyperventilation. Then, we detail the neural circuits involved in absence epilepsy. Finally, we summarize evidence supporting the hypothesis that specific nodes within thalamic circuits are pH-sensitive.
6. Absence seizures: crosstalk between the thalamus and cortex
Decades of research highlight how reciprocal interactions between cortical and thalamic circuits act as critical architects of absence seizure generation (Avoli, 2012). As early as 1935 clinicians noted that highly synchronized seizure activity could be simultaneously recorded from EEG electrodes placed throughout the cortex, leading to the prescient postulation that subcortical structures with widespread cortical connectivity are likely involved (Jasper and Kershman, 1941; Penfield and Erickson, 1941). The structure receiving early attention was the thalamus.
Besides serving as a relay station for vision, proprioception and hearing (Jones, 2007), the thalamus houses critical neural circuity responsible for electrical oscillations observed during sleep (Steriade and Llinás, 1988; McCormick and Bal, 1997) and seizures. Morison and Dempsey (Dempsey and Morison, 1942a,b; Morison and Dempsey, 1942), as well as Jasper and colleagues (Jasper and Kershman, 1941; Jasper and Droogleever-Fortuyn, 1947; Hunter and Jasper, 1949; Hanbery and Jasper, 1953), provided several key lines of evidence in support of the hypothesis that thalamic circuits play an important role in SWD generation. First, recordings from depth electrodes placed in the thalamus of cats reveal that thalamic circuits are highly oscillatory (Dempsey and Morison, 1942b; Morison and Dempsey, 1942). Second, electrical stimulation of the cat thalamus evokes generalized, cortical SWDs (Jasper and Droogleever-Fortuyn, 1947; Hunter and Jasper, 1949). Third, severing thalamus-cortex connections mitigates the capacity of thalamic stimulation to evoke SWDs (Hanbery and Jasper, 1953). Following these insightful studies, Fisher and Prince (Fisher, 1977), as well as Avoli and colleagues (Avoli and Gloor, 1982a,b; Avoli et al., 1983), used the feline generalized penicillin model of epilepsy (FGPE) to assess, on a more granular level, thalamic contribution to SWDs. The FGPE is an experimental epilepsy model in which a large, intramuscular injection of penicillin reliably evokes SWDs (Prince and Fischer, 1969). By closely examining temporal relationships of neuronal activity throughout the brain in the FGPE, it was possible to determine that excessive, hypersynchronous cortical activity likely initiates the SWD (Avoli and Gloor, 1982b; Avoli et al., 1983). A similar conclusion was later derived in an inbred rat model of absence epilepsy (van Heukelum et al., 2016; van Luijtelaar and Coenen, 1986). Thus, decades of work underscore the notion that a “close coupling” of activity produced by the thalamus and cortex contributes to the onset and maintenance of the SWD (Avoli and Gloor, 1982b).
7. The riddle in the middle: midline structures of the thalamus
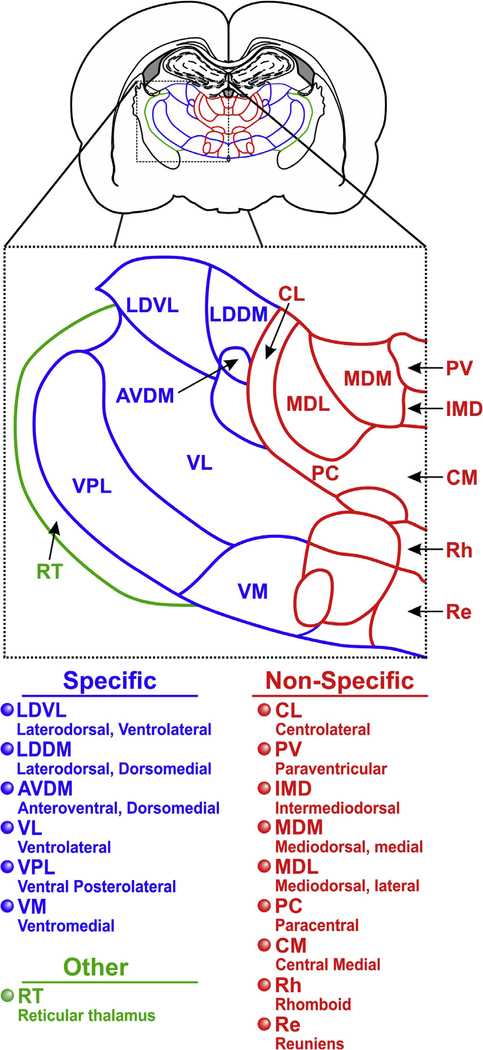
The pioneering studies of Rose and Woolsey prompted an era dedicated to organizing the thalamic nuclei based upon structure and function (Jones, 2007). Using anatomical and electrophysiological methods, their work revealed that the cortex receives inputs from specific subdivisions of the dorsal thalamus (Jones, 2007). Rose and Woolsey divided the dorsal thalamus into two distinct divisions: extrinsic and intrinsic. The extrinsic nuclei included the anterior and ventral thalamic groups as well as the geniculate bodies. They proposed that these extrinsic structures projected to specific cortical areas, including motor, sensory and limbic areas. The intrinsic nuclei, consisting of the midline, intralaminar and posterior thalamic groups, were thought to receive only intrathalamic projections. However, the distinction between extrinsic and intrinsic was highly speculative and subsequent studies failed to demonstrate the existence of purely intrathalamic connectivity among thalamic nuclei.
Later, Morison and Dempsey proposed a second classification scheme to distinguish the dorsal thalamic nuclei. They used the term specific to describe dorsal thalamic nuclei with distinct, topographically-mapped connections to the cortex. In contrast, the term non-specific (Dempsey and Morison, 1942a,b) was used to describe those nuclei, primarily the midline and intralaminar nuclei, with diffuse projections throughout the cortex. These non-specific nuclei are collectively called the non-specific thalamic projecting system (NSTPS) and include the mediodorsal nucleus, central medial (CM) nucleus, as well as other nuclei of the intralaminar complex (Jones, 2007). We illustrate the organization of the specific and non-specific thalamic nuclei in Fig. 3. Special attention will be given to the NSTPS, as this system appears to play a critical role in hyperventilation-induced changes in EEG patterns.
Fig. 3.
Specific and non-specific nuclei of the thalamus. On top is shown a coronal section of a rat brain (Paxinos and Watson, 2007). An expanded view of nuclei from the thalamus on one side is shown directly below the full coronal section. Nuclei abbreviations are found below the expanded view. Structures outlined in blue represent the specific thalamic nuclei, whereas the structures outlined in red represent the non-specific nuclei. Collectively, specific and non-specific nuclei comprise the dorsal thalamus. The reticular nucleus (green), a member of the ventral thalamus, forms a thin, shell-like structure that surrounds the dorsal thalamus. Nuclei along the midline are considered members of the Non-Specific Thalamic Projection System (NSTPS). The following structures are not labeled: submedius thalamic nucleus (dorsal and ventral), anteromedial thalamic nucleus, ventral reuniens, mammillothalamic tract.
Morison and Dempsey first demonstrated that electrical stimulation of specific and non-specific thalamic nuclei in the anesthetized cat evoked divergent cortical responses. Stimulation of the specific nuclei evoked a localized, multiphasic response consisting of an early primary response and a later augmenting response. The latter response was so-called because it became larger after repetitive stimulation (Fig. 4A). In contrast, stimulation of the NSTPS evoked widespread responses in the cortex (Dempsey and Morison, 1942a,b; Morison and Dempsey, 1942), consistent with the diffuse nature of NSTPS projections. Interestingly, successive NSTPS stimuli delivered at 6–12 Hz often produced robust, high amplitude cortical responses that grew during the repetitive stimulus train (Fig. 4B). This latter feature led Morison and Dempsey to introduce the term recruiting response. There are several important characteristics that distinguish the recruiting response from the augmenting response (see Fig. 4: (1) the latency from stimulus to event onset is much longer for the recruiting response; (2) the recruiting response waxes and wanes with repetitive stimulation; (3) the recruiting response spreads throughout the cortex, while the augmenting response is highly localized; (4) the recruiting response is not preceded by the primary response. The phenomenon of the NSTPS-evoked recruiting response was subsequently confirmed in great detail by Jasper and colleagues (Jasper and Kershman, 1941; Jasper and Droogleever-Fortuyn, 1947; Hunter and Jasper, 1949; Hanbery and Jasper, 1953). Moreover, Jasper and colleagues demonstrated that even brief stimulation of the NSTPS in lightly anesthetized (Jasper and DroogleeverFortuyn, 1947) or unanesthetized (Hunter and Jasper, 1949) cats can evoke behavioral arrest and synchronized SWDs throughout the cortex that long outlasts the stimulus. The capacity for NSTPS stimulation to evoke either the recruiting response or prolonged SWDs accompanied with behavioral arrest likely depends on the state of anesthesia: recruiting responses are observed in anesthetized animals, while seizures are observed in unanesthetized animals. This observation firmly placed the NSTPS at the forefront of possible structures that drive absence seizures, even prompting Jasper to conclude that this collection of nuclei serves as the “diencephalic basis for [absence epilepsy], or a diencephalic pacemaker for its characteristic cortical discharge.” (Hunter and Jasper, 1949).
Fig. 4.
Electrophysiological cortical response to electrical stimulation of specific versus non-specific thalamic nuclei. (A) Schematic representing experiment. Field responses are recorded in the cortex (e.g. anterior sigmoid gyrus, visual cortex). Electrical stimuli are delivered to either the lateral thalamic nuclei (blue), or the midline thalamic nuclei (red). (B) A single electrical stimulation of the lateral thalamic nuclei evokes events known as the primary and augmenting responses (top, blue). The primary response is collectively composed of two positive deflections (1 & 2), followed by a larger negative component. Repetitive lateral nuclei stimulation produces a secondary component known as the augmenting response. In contrast to lateral nuclei stimulation, a single electrical stimulation of the midline thalamic nuclei evokes a single, small, negative component (bottom, red). Successive midline stimuli yield a progressively larger event known as the recruiting response. Schematized responses are based on those described in The Thalamus (Jones, 2007).
Following these seminal findings, Dominick Purpura set out to determine how the NSTPS drives widespread cortical activity. He focused much of his efforts on intrinsic thalamic connectivity (Jones, 2007). By performing intracellular recordings of neurons in the specific and non-specific thalamic nuclei of anesthetized cats, Purpura and colleagues revealed complex, bidirectional interactions between the NSTPS and the specific thalamic nuclei (Desiraju and Purpura, 1970; Purpura and Cohen, 1962). Their findings also provided a glimpse into how these interactions may contribute to the aforementioned recruiting response. Many of their studies focused on the CM nucleus, a member of the NSTPS.
Purpura and colleagues showed that CM stimulation in the cat evokes post-synaptic potentials (PSPs) in neurons localized to several specific thalamic nuclei, including the ventral group of the dorsal thalamus and the reticular nucleus (Fig. 5). The evoked PSPs follow a complex pattern (Purpura and Cohen, 1962). CM stimulation evokes putative short-latency excitatory post-synaptic potentials (EPSPs) in neurons of the ventral group (i.e. ventromedial thalamus), followed by long-duration, inhibitory post-synaptic potentials (IPSPs) (Fig. 5). The short latency of the putative EPSPs led Purpura to posit that CM provided direct excitation to the ventral group.
Fig. 5.
The central medial (i.e. non-specific) nucleus of the thalamus is functionally connected to specific and reticular thalamic nuclei. Shown are experimental results from Purpura and Cohen (Purpura and Cohen, 1962). (A) Experimental preparation. In vivo experiments were performed in the cat. The central medial (CM) nucleus was stimulated with an extracellular stimulating electrode. Responses to such stimulation were recorded in neurons of the ventromedial (VM) using intracellular recording pipettes. Thalamic structures that are likely involved in the VM neuron responses are filled in with red, blue or green. (B) An example, intracellular recording of a VM neuron. Each red arrowhead represents a single electrical stimulus delivered to CM. Prior to CM stimulation, action potentials are spontaneously generated by the VM neuron. The first electrical stimulus elicits a putative excitatory postsynaptic potential (EPSP, blue) with a short latency in the recorded neuron. The putative EPSP is followed by a longer latency inhibitory postsynaptic potential (IPSP, green). Purpura and Cohen speculated that rapid EPSP occurred as a result of direct, monosynaptic connectivity between CM and VM nuclei. The IPSP, in contrast, likely resulted from an indirect, disynaptic connection that initially involved excitation of GABAergic neurons of the reticular thalamic (RT) nucleus, followed by RT-mediated inhibition of VM neurons. This EPSP-IPSP combination is observed to differing extents with subsequent CM stimulation. Following CM stimulation (i.e. stim. end) results in a phase of slow VM neuron depolarization. Resumption of CM stimulation again evokes the EPSP-IPSP combination.
The origin of CM-evoked IPSPs was more puzzling. When Purpura and Cohen recorded neurons of the reticular thalamus (RT), an inhibitory structure, the picture became clearer: CM stimulation activated RT neurons. As RT neurons inhibit many thalamic structures (Fuentealba and Steriade, 2005), a likely origin of the CM-evoked IPSPs observed in neurons of the ventral group was from the RT nucleus. Thus, it was proposed that CM provides direct excitation, as well as indirect, disynaptic inhibition, to neurons of the ventral group. The observed inhibition of ventral group neurons was quite robust and included a strong, long-lasting component indicative of activation of metabotropic, B-type, GABA (GABAB) receptors. GABAB receptor antagonists effectively inhibit experimentally-induced absence seizures (Vergnes et al., 1997).
Purpura and Cohen ultimately attempted to relate the progression of CM-evoked EPSPs-IPSPs observed in ventral group neurons to the CM-evoked recruiting response. They proposed that the initial, large component of the recruiting response associates with ventral group EPSPs, while the ensuing, secondary component of the response associates with ventral group IPSPs. Moreover, special attention was paid to the potential synchronizing effect neurons of the RT nucleus had on thalamic activity. In sum, these experiments provided an unprecedented, macroscopic understanding of the structures involved in generating absence seizures. Left unaddressed was whether the NSTPS was involved in hyperventilation-triggered absence seizures.
8. A basic modulation of the thalamus
Despite the long-established documentation of hyperventilation-induced (i.e. respiratory alkalosis-induced) absence seizures, few studies have attempted to experimentally recapitulate this phenomenon. Experiments performed by Ira Sherwin in the 1960s represent some of the few attempts to do so. Sherwin posed two key questions in his experiments: (1) what brain structures are recruited by hyperventilation to increase the occurrence of SWDs (Sherwin, 1965, 1967), and (2) do these structures possess a specific, element that is responsive to respiratory-induced changes in pH?
In the first study we discuss (Sherwin, 1965), Sherwin demonstrated that hyperventilating a cat elicits high amplitude, rhythmic slowing in the cortical EEG comparable to activity observed during HIHARS (Fig. 6). Stimulating the cortex during HIHARS further transformed the activity to include generalized cortical seizures similar to SWDs. To determine how the coupling of HIHARS and cortical stimulation evokes seizures, Sherwin used a common procedure at the time to assess cortical excitability: the direct cortical response (DCR, see Fig. 6A). Briefly, local electrical field potentials are evoked and recorded in one area of the cortex by stimulating another area of the cortex. The activation of excitatory synapses formed between thalamocortical and cortical neurons is thought to contribute to the DCR. Using this assay of cortical excitability, Sherwin showed that the DCR was enhanced during hyperventilation. Severing connections between the cortex and subcortical structures (i.e. isolating the cortex) abolished this hyperventilation-induced DCR enhancement. These findings prompted Sherwin to conclude that some subcortical structure capable of enhancing cortical excitability was recruited during hyperventilation. A few years later, Sherwin performed experiments designed to identify this structure.
Fig. 6.
Hyperventilation-induced, high-amplitude slowing of cortical activity depends on non-specific thalamic nuclei. Panels A and B represent experimental observations from two in vivo cat studies performed by Sherwin (1965, 1967). (A) In the first study, electrophysiological recordings were obtained from the cortex (1). Electrocorticogram (ECoG) recordings, similar to EEG recordings, were used to measure large-scale cortical activity in the mid-suprasylvian gyrus (MSS) and the coronal gyrus (COR). Local field recordings recorded in the MSS reveal the direct cortical response (DCR) evoked by a nearby electrical stimulating electrode. Importantly, the DCR is hypothesized to arise from direct activation of afferents that originate from the thalamus (Adrian, 1939; Chang, 1951; Burns, 1950). The experiment compared ECoG and DCR responses during hyperventilation before and after subcortical connections to the MSS were selectively severed. Cortical responses recorded before (2) and after (3) severing connections between the cortex and thalamus. With intact thalamus-cortex connectivity, normal respiration was associated with low-amplitude ECoG activity, as well as an evoked DCR of moderate amplitude. Hyperventilation produced high-amplitude, slow ECoG activity in both the MSS and COR. Also, the evoked DCR was larger. After severing thalamus-MSS connections, hyperventilation did not alter ECoG activity recorded in the MSS. Importantly, after severing connections, hyperventilation also did not augment the DCR. (B) In the second study, the effects of CL lesion on hyperventilation-induced, high amplitude ECoG signals were assessed (1). As in panel A, hyperventilation elicits ECoG signals that consist of high amplitude events in the intact sigmoid gyrus (SIG) and MSS. (2). After CL lesion, these hyperventilation-induced events are not observed (3).
In 1967, Sherwin presented a study that demonstrated a critical role for the NSTPS in modulating cortical excitability (Sherwin, 1967). Sherwin specifically examined the contribution of the central lateral (CL) nucleus, a member of the NSTPS, to hyperventilation-induced changes in cortical excitability and HIHARS. Sherwin demonstrated that HIHARS was abolished after lesioning the CL (Fig. 6B), thereby presenting the strongest available data that provide an explanation for how hyperventilation alters cortical EEG patterns. At the time he could only postulate that the observed changes in cortical activity resulted from an element, likely in the thalamus, that is both chemoreceptive (Sherwin, 1967) and capable of enhancing cortical activity. The conclusions drawn by Sherwin were never pursued further in the context of absence epilepsy. Nonetheless, the few-yet-critical results documented by Sherwin uncovered the interesting possibility that the thalamus acts as a potential pH-sensor (or contains pH sensing pathways to the cortex). It remains uncertain how the NSTPS engages with other rhythmic microcircuits in the thalamus during hyperventilation-induced SWDs.
9. Rhythmic microcircuits in the thalamus
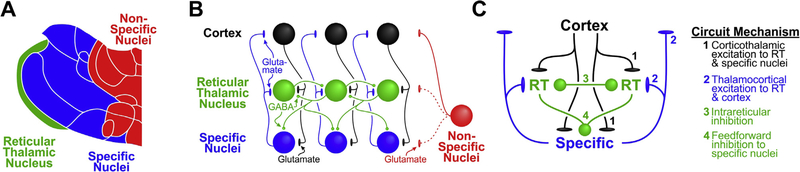
The decades leading up to the 1980s provided invaluable insights into the key brain structures associated with absence epilepsy. The decades that followed this era provided a much deeper, mesoscopic understanding of thalamocortical circuit dynamics that produce the SWD. A number of studies from the 1980 to 90s (McCormick and Bal, 1997; Jahnsen and Llinás, 1984a; Llinás and Jahnsen, 1982; Steriade et al., 1993; Contreras et al., 1996; Destexhe et al., 1998; Sherman and Guillery, 1996; Bal et al., 1995; Huguenard and McCormick, 1992; McCormick and Huguenard, 1992) support the hypothesis that thalamic circuits underlie the rhythmic nature of the SWD. Three neuronal populations are likely critical for orchestrating thalamocortical rhythms: glutamatergic thalamocortical relay (TC) neurons, glutamatergic corticothalamic (CT) neurons, and GABAergic neurons of the reticular thalamus (RT). The interactions among these three neuron subpopulations have been extensively described in several excellent review articles (Beenhakker and Huguenard, 2009; Huguenard and McCormick, 2007; McCormick and Contreras, 2001; Fogerson and Huguenard, 2016); therefore, we only briefly highlight salient aspects of the circuitry.
As we illustrate in Fig. 7, CT neurons send excitatory projections to both RT neurons and TC neurons. RT neurons provide feedforward inhibition to TC neurons. TC neurons, in turn, provide recurrent excitation back to RT neurons. The populations of reciprocally connected RT and TC neurons constitute a critical circuit for generating rhythmic activity patterns in the thalamus. As TC neurons project to the cortex, such rhythmicity is imposed on cortical neurons. Circuit rhythmicity is primarily observed during sleep and seizure states. In contrast, during wakefulness, most thalamic neurons fire action potentials in tonic mode, a firing property in which a neuron produces action potentials at a relatively low and arrhythmic rate. More detail on the firing properties of thalamic neurons and thalamocortical circuit connectivity can be found elsewhere (McCormick and Bal, 1997; Destexhe et al., 1998; McCormick and Huguenard, 1992; Fogerson and Huguenard, 2016; Guillery and Harting, 2003; Blumenfeld and McCormick, 2000; Llinás et al., 1998; Steriade and Contreras, 1995).
Fig. 7.
Rhythm generating circuits of the thalamus. (A) Schematic representation of thalamic nuclei likely involved in electrical oscillations produced by the thalamus. Several hypotheses propose that circuit rhythmicity can be achieved through interactions between the reticular thalamic (RT, green) nucleus and specific thalamic nuclei (blue). (B) Circuit diagram representing connections among cortical and RT neurons, as well as neurons of the lateral specific nuclei. Cortical neurons (black) provide direct, glutamatergic excitation to both RT neurons (green) and specific thalamic neurons (blue). Specific thalamic neurons provide direct, glutamatergic excitation to both RT and cortical neurons. RT neurons provide GABAergic inhibition to other RT neurons and neurons of the specific nuclei. Based on the conclusions of Purpura and Cohen (1962), neurons of the non-specific nuclei (red) putatively excite neurons of the specific nuclei and the cortex. As there is little anatomical evidence for this conclusion, we represent such connectivity with a red dashed line. There is limited evidence demonstrating that the non-specific nuclei project to the RT (red dash line). (C) Simplified representation of circuit dynamics shown in (B) to highlight nodes proposed to regulate SWD generation. Studies that have discovered these nodes have primarily focused on the specific nuclei. Therefore, the non-specific connections were omitted for simplicity. Elements highlighted in 1 & 2 represent excitatory, glutamatergic nodes. Intrareticular inhibition node (node 3) represents inhibition among RT neurons proposed to desynchronize thalamic circuit activity and limit seizure activity (Sohal et al., 2000). RT-mediated, feedforward inhibition (node 4) is proposed to promote burst firing and seizure-related activity patterns (Kim et al., 1997; Sanchez-Vives and McCormick, 1997).
Several hypotheses attempt to account for the abrupt onset of highly rhythmic circuit activity observed during a SWD. Many of these hypotheses ultimately depend on the activation of robust burst firing in RT and TC neurons. In contrast to the aforementioned tonic firing mode, burst firing mode in thalamic neurons, first described by Jahnsen and Llinas (Jahnsen and Llinás, 1984a,b; Llinás and Jahnsen, 1982)**, is a firing property in which a neuron produces a brief, high-frequency burst of action potentials. Thalamic burst firing depends on low threshold, T-type calcium (Ca2+) channels, and is proposed to play a critical role in sustaining thalamic circuit rhythmicity during SWDs (Chen et al., 2014; Cheong and Shin, 2014; Choi et al., 2015). Indeed, as described above, gain-of-function mutations in this channel are associated with absence epilepsy and ethosuximide, a T-type Ca2+ blocker, is used clinically to treat absence epilepsy.
As enhanced T-type Ca2+ channel activity represents a common thread in most hypotheses regarding SWD generation, many studies have focused on mechanisms that promote thalamic burst firing. We briefly highlight two. First, strengthened feedforward, RT neuron-mediated inhibition of TC neurons (see Fig. 7C) is known to promote robust burst firing in TC neurons. The T-type Ca2+ channel-mediated mechanism known as post-inhibitory rebound bursting drives this TC neuron behavior. Proposed mechanisms that account for augmented feedforward, RT-mediated inhibition include a breakdown of processes that normally dampen RT neuron activity (Huntsman et al., 1999; Destexhe et al., 1998; Castro-Alamancos, 1999) (see Fig. 7C). Second, diminished glutamatergic excitation of RT neurons is proposed to promote SWD generation (Menuz and Nicoll, 2008; Paz, 2011) and can lead to enhanced T-type Ca2+ channel-mediated bursting (Paz, 2011). Thus, perturbations in several nodes of the thalamocortical circuit likely contribute to SWD generation.
We have described only a small subset of the rich dataset, accumulated over many decades, that highlights the critical role that thalamocortical circuits play in the generation of absence seizures. But what of pH sensitivity in these circuits? For the remainder of this review, we attempt to describe more specifically how pH alters thalamocortical circuits to possibly trigger absence seizures.
10. pH sensitivity in the thalamus
Despite a considerable void in literature detailing pH sensitive mechanisms in the NSTPS, evidence demonstrates that certain neurons of the specific thalamic nuclei possess pH-sensitive ion channels that contribute to the resting membrane potential of thalamic neurons. We focus on two such channels: the HCN channel responsible for the so-called h-current (Ih) (Soltesz, 1991), and TASK 1/3 channels responsible for a resting potassium current (ITASK) (Meuth, 2006).
Meuth et al. revealed a complex, pH-sensitive interaction between Ih and ITASK in thalamocortical (TC) neurons of the dorsal lateral geniculate nucleus, a “specific” thalamic nucleus that receives visual information from the retina (Meuth, 2006). The authors demonstrate that Ih and ITASK exert opposing effects on TC neuron resting membrane potential. Ih is a mixed cationic (Na+ and K+) current that is activated at relatively hyperpolarized membrane potentials (Biel et al., 2009). The reversal potential of Ih is around −20 mV, meaning that when Ih is active, a neuron will typically depolarize towards −20 mV. Because the resting membrane potential of TC neurons is relatively hyperpolarized (~−70 mV), partial activation of Ih is observed at rest and contributes to TC neuron resting membrane potential. Evidence for this last point comes from the more hyperpolarized resting membrane potential observed in TC neurons when Ih is pharmacologically or genetically removed: the resting membrane potential shifts towards −80 mV (Meuth, 2006). ITASK, in contrast, is a K+ current and, as such, has a reversal potential of around −90 mV, meaning that when ITASK is active, a neuron will typically hyperpolarize towards −90 mV. ITASK is often described as a background current because it is usually active at rest and contributes significantly to the resting membrane potential of neurons.
Ih and ITASK are both pH-sensitive in TC neurons (Meuth, 2006). Extracellular acidification blocks both currents. Because these two currents have functionally opposing actions – Ih depolarizes cells while ITASK hyperpolarizes cells – the net result of extracellular acidification is minimal; the resting membrane potential of TC neurons does not change much during extracellular acidification. The action potential firing properties of TC neurons are also unchanged during extracellular acidification. The results of Meuth et al. suggest that, functionally, TASK 1/3 and HCN expression levels are commensurate in TC neurons. If such expression levels were mismatched in a sub-population of TC neurons, then changes in pH would likely significantly impact TC neuron activity. Also, it remains formally possible that extracellular alkalization, as might occur during hyperventilation, might preferentially modulate one current (e.g. Ih) over another (e.g. ITASK), thereby significantly changing TC neuron firing behavior. To date, this possibility remains purely speculative. It remains entirely unclear to what extent pH sensitivity in the so-called “specific” nuclei contributes to hyperventilation-induced absence seizures. After all, much of the aforementioned work suggests that the NSTPS plays a major role in absence seizures triggered by respiratory alkalosis.
11. Conclusion
Herein, we highlight the potential link among thalamocortical networks, hyperventilation, and absence epilepsy. Specifically, we focus on studies indicating that the NSTPS of the thalamus may be capable of evoking hyperventilation-induced absence seizures. This conclusion is derived from demonstrations that the NSTPS appears critically involved in both SWDs and hyperventilationtriggered cortical activity patterns. Moreover, some thalamocortical circuit elements appear to be endowed with pH-sensitive proteins. What remains unclear is whether these observations point to a common mechanism accounting for hyperventilationtriggered absence seizures, a striking phenomenon shared by over 90% of absence patients. Perhaps the next few decades of thalamic research will shed light on this possibility.
Acknowledgements
We thank Peter Klein for helpful comments on early versions of this manuscript. We also thank Dr. Mitchell Chesler for helpful comments regarding acid-base physiology. We also thank Annika Klara Beenhakker for Fig. 2 illustrations. This review was supported by R01NS099586.
Footnotes
Conflict of interest
The authors declare no competing financial interests.
References
- Tissot SAD, 1770. Traité de l’epilepsie: faisant le tome troisieme du Traite des nerfs et de leurs maladies.
- Gibbs F, Davis H, Lennox W, 1935. The electroencephalogram in epilepsy and in conditions of impaired consciousness. Arch. Neurol. Psychiatry Clin. Neurosci 34, 13. [Google Scholar]
- ILAE, 1989. Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia 30, 389–399. [DOI] [PubMed] [Google Scholar]
- Trinka E et al. , 2004. Long-term prognosis for childhood and juvenile absence epilepsy. J. Neurol 251, 1235–1241. 10.1007/s00415-004-05211. [DOI] [PubMed] [Google Scholar]
- Matricardi S, Verrotti A, Chiarelli F, Cerminara C, Curatolo P, 2014. Current advances in childhood absence epilepsy. Pediatr. Neurol 50, 205–212. 10.1016/j.pediatrneurol.2013.10.009. [DOI] [PubMed] [Google Scholar]
- Shinnar S et al. , 2015. Long-term outcomes of generalized tonic-clonic seizures in a childhood absence epilepsy trial. Neurology 85, 1108–1114. 10.1212/wnl.0000000000001971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reutens DC, Berkovic SF, 1995. Idiopathic generealized epilepsy of adolescence: are the syndromes clinically distinct? Neurology 45, 1469–1476. [DOI] [PubMed] [Google Scholar]
- Guilhoto LM, 2017. Absence epilepsy: continuum of clinical presentation and epigenetics? Seizure 44, 53–57. 10.1016/j.seizure.2016.11.031. [DOI] [PubMed] [Google Scholar]
- Gastaut H, 1981. Individualization of so-called benign and functional epilepsy at different ages. Appraisal of variations corresponding the predisposition for epilepsy at these ages. Rev. Electroencephalogr. Neurophysiol. Clin 11, 346–366. [DOI] [PubMed] [Google Scholar]
- Panayiotopoulos CP et al. , 1992. Typical absence seizures in adults: clinical, EEG, video-EEG findings and diagnostic/syndromic considerations. J. Neurol. Neurosurg. Psychiatry 55, 1002–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michelucci R et al. , 1996. Electroclinical features of idiopathic generalised epilepsy with persisting absences in adult life. J. Neurol. Neurosurg. Psychiatry 61, 471–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkovic SF, Bladin PF, 1983. Absence status in adults. Clin. Exp. Neurol 19, 198–207. [PubMed] [Google Scholar]
- Marini C, King MA, Archer JS, Newton MR, Berkovic SF, 2003. Idiopathic generalised epilepsy of adult onset: clinical syndromes and genetics. J. Neurol. Neurosurg. Psychiatry 74, 192–196. 10.1136/jnnp.74.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iivanainen M, Bergström L, Nuutila A, Viukari M, 1984. Psychosis-like absence status of elderly patients: successful treatment with sodium valproate. J. Neurol. Neurosurg. Psychiatry 47, 965–969. 10.1136/jnnp.47.9.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenney JR, Glauser TA, 2013. The current state of absence epilepsy: can we have your attention? Epilepsy Curr. 13, 135–140. 10.5698/15357511-13.3.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depaulis A, Charpier S, 2017. Pathophysiology of absence epilepsy: insights from genetic models. Neurosci. Lett 10.1016/j.neulet.2017.02.035. [DOI] [PubMed] [Google Scholar]
- Depaulis A, David O, Charpier S, 2016. The genetic absence epilepsy rat from Strasbourg as a model to decipher the neuronal and network mechanisms of generalized idiopathic epilepsies. J. Neurosci. Methods 260, 159–174. 10.1016/j.jneumeth.2015.05.022. [DOI] [PubMed] [Google Scholar]
- Felix R, 2002. Insights from mouse models of absence epilepsy into Ca2+ channel physiology and disease etiology. Cell Mol. Neurosci 22, 103–120. [DOI] [PubMed] [Google Scholar]
- Cortez MA, Kostopoulos GK, Snead OC, 2016. Acute and chronic pharmacological models of generalized absence seizures. J. Neurosci. Methods 260, 175–184. 10.1016/j.jneumeth.2015.08.034. [DOI] [PubMed] [Google Scholar]
- Coenen A, Van Luijtelaar EL, 2003. Genetic animal models for absence epilepsy: a review of the WAG/Rij strain of rats. Behav. Genet 33, 635–655. [DOI] [PubMed] [Google Scholar]
- Jones-Davis DM, Macdonald RL, 2003. GABAA receptor function and pharmacology in epilepsy and status epilepticus. Curr. Opin. Pharmacol 3, 12–18. 10.1016/S1471-4892(02)00015-2. [DOI] [PubMed] [Google Scholar]
- Macdonald RL, Kang J-Q, Gallagher MJ, 2010. Mutations in GABAA receptor subunits associated with genetic epilepsies. J. Physiol 588, 1861–1869. 10.1113/jphysiol.2010.186999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph U, Crestani F, Möhler H, 2001. GABAA receptor subtypes: dissecting their pharmacological functions. Trends Pharmacol. Sci 22, 188–194. 10.1016/S0165-6147(00)01646-1. [DOI] [PubMed] [Google Scholar]
- Tan HO et al. , 2007. Reduced cortical inhibition in a mouse model of familial childhood absence epilepsy. Proc. Natl. Acad. Sci 104, 17536–17541. 10.1073/pnas.0708440104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cossette P et al. , 2002. Mutation of GABRA1 in an autosomal dominant form of juvenile myoclonic epilepsy. Nat. Genet 31, 184–189. [DOI] [PubMed] [Google Scholar]
- Lachance-Touchette P et al. , 2011. Novel a1 and c2 GABAA receptor subunit mutations in families with idiopathic generalized epilepsy. Eur. J. Neurosci 34, 237–249. 10.1111/j.1460-9568.2011.07767.x. [DOI] [PubMed] [Google Scholar]
- Maljevic S et al. , 2006. A mutation in the GABAA receptor a1-subunit is associated with absence epilepsy. Ann. Neurol 59, 983–987. 10.1002/ana.20874. [DOI] [PubMed] [Google Scholar]
- Huntsman MM, Porcello DM, Homanics GE, DeLorey TM, Huguenard JR, 1999. Reciprocal inhibitory connections and network synchrony in the mammalian thalamus. Science 283, 541–543. [DOI] [PubMed] [Google Scholar]
- Roden WH, Peugh LD, Jansen LA, 2010. Altered GABAA receptor subunit expression and pharmacology in human Angelman syndrome cortex. Neurosci. Lett 483, 167–172. 10.1016/j.neulet.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holopainen IE et al. , 2001. Decreased binding of [11C]flumazenil in Angelman syndrome patients with GABAA receptor b3 subunit deletions. Ann. Neurol 49, 110–113. . [DOI] [PubMed] [Google Scholar]
- Chen Y et al. , 2003. Association between genetic variation of CACNA1H and childhood absence epilepsy. Ann. Neurol. 54, 239–243. 10.1002/ana.10607. [DOI] [PubMed] [Google Scholar]
- Heron SE et al. , 2007. Extended spectrum of idiopathic generalized epilepsies associated with CACNA1H functional variants. Ann. Neurol. 62, 560–568. 10.1002/ana.21169. [DOI] [PubMed] [Google Scholar]
- Khosravani H et al. , 2004. Gating effects of mutations in the Cav3.2 T-type calcium channel associated with childhood absence epilepsy. J. Biol. Chem 279, 9681–9684. 10.1074/jbc.C400006200. [DOI] [PubMed] [Google Scholar]
- Vitko I et al. , 2005. Functional characterization and neuronal modeling of the effects of childhood absence epilepsy variants of CACNA1H, a T-type calcium channel. J. Neurosci 25, 4844–4855. 10.1523/jneurosci.084705.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peloquin JB et al. , 2006. Functional analysis of Cav3.2 T-type calcium channel mutations linked to childhood absence epilepsy. Epilepsia 47, 655–658. 10.1111/j.1528-1167.2006.00482.x. [DOI] [PubMed] [Google Scholar]
- Wang G et al. , 2015. CaV3.2 calcium channels control NMDA receptor-mediated transmission: a new mechanism for absence epilepsy. Genes Dev. 29, 1535–1551. 10.1101/gad.260869.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staley K, 2015. Molecular mechanisms of epilepsy. Nat. Neurosci 18, 367–372. 10.1038/nn.3947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loiseau P, Pestre M, Dartiques JF, Commenges D, Barberger-Gateau C, Cohadon S, 1983. Long-term prognosis in two forms of childhood epilepsy: typical absence seizures and epilepsy with rolandic (centrotemporal) EEG foci. Ann. Neurol 13, 642–648. [DOI] [PubMed] [Google Scholar]
- Wirrell EC, Camfield P, Camfield CS, Gordon KE, Dooley JM, 1996. Long-term prognosis of typical childhood absence epilepsy: remission or progression to juvenile myoclonic epilepsy. Neurology 47, 912–918. [DOI] [PubMed] [Google Scholar]
- Sillanpää M, Jalava M, Kaleva O, Shinnar S, 1998. Long-term prognosis of seizures with onset in childhood. New Engl. J. Med. 338, 1715–1722. 10.1056/nejm199806113382402. [DOI] [PubMed] [Google Scholar]
- Glauser TA et al. , 2013. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy: initial monotherapy outcomes at 12 months. Epilepsia 54, 141–155. 10.1111/epi.12028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirrell EC et al. , 1997. Long-term psychosocial outcome in typical absence epilepsy: sometimes a wolf in sheeps clothing. Arch. Pediatr. Adolesc. Med 151, 152–158. 10.1001/archpedi.1997.02170390042008. [DOI] [PubMed] [Google Scholar]
- Caplan R et al. , 2008. Childhood absence epilepsy: behavioral, cognitive, and linguistic comorbidities. Epilepsia 49, 1838–1846. 10.1111/j.1528-1167.2008.01680.x. [DOI] [PubMed] [Google Scholar]
- Caplan R, 2015. A call to arms against “the phantom of epilepsy”. Epilepsia 56, 1710–1711. 10.1111/epi.13197. [DOI] [PubMed] [Google Scholar]
- Panayiotopoulos CP, 1999. Typical absence seizures and their treatment. Arch. Dis. Child 81, 351–355. 10.1136/adc.81.4.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watemberg N et al. , 2015. Hyperventilation during routine electroencephalography: are three minutes really necessary? Pediatr. Neurol. 52, 410–413. 10.1016/j.pediatrneurol.2014.12.003. [DOI] [PubMed] [Google Scholar]
- Giannakodimos S, Ferrie C, Panayiotopoulos CP, 1995. Qualitative and quantitative abnormalities of breath counting during brief generalized 3 Hz spike and slow wave ‘subclinical’ discharges. Clin. Electroencephalogr 26, 200–203. [DOI] [PubMed] [Google Scholar]
- Adams DJ, Leuders H, 1981. Hyperventilation and 6-hour EEG recording in evaluation of absence seizures. Neurology 31, 1175–1177. [DOI] [PubMed] [Google Scholar]
- Holowach J, Thurston D, O’Leary JL, 1962. Petit mal epilepsy. Pediatrics 30, 893–901. [PubMed] [Google Scholar]
- Nims L, Gibbs EL, Lennox WG, Gibbs FA, Williams D, 1940. Adjustment of acid-base balance of patients with petit mal epilepsy to overventilation. Arch. Neurol. Psychiatry 43, 262–269. [Google Scholar]
- Lum LM, Connolly MB, Farrell K, Wong PKH, 2002. Hyperventilation-induced high-amplitude rhythmic slowing with altered awareness: a video-EEG comparison with absence seizures. Epilepsia (Series 4) 43, 1372–1378. 10.1046/j.1528-1157.2002.35101.x. [DOI] [PubMed] [Google Scholar]
- Gibbs EL, Gibbs F, Lennox WG, Nims LF, 1942. Regulation of cerebral carbon dioxide. Arch. Neurol. Psychiatry 47, 879–889. [Google Scholar]
- Esquivel E, Chaussain M, Plouin P, Ponsot G, Arthuis M, 1991. Physical exercise and voluntary hyperventilation in childhood absence epilepsy. Electroencephalogr. Clin. Neurophysiol 79, 127–132. 10.1016/0013-4694(91)90050-E. [DOI] [PubMed] [Google Scholar]
- Kontos HA, Raper AJ, Patterson JL, 1977. Analysis of vasoactivity of local pH, PCO2 and bicarbonate on pial vessels. Stroke 8, 358–360. 10.1161/01.str.8.3.358. [DOI] [PubMed] [Google Scholar]
- Cipolla MJ, 2009. In: The Cerebral Circulation. San Rafael (Ch. 5).
- Boron W, Boulpaep EL, 2009. Medical Physiology. Saunders. [Google Scholar]
- Koide M, Bonev AD, Nelson MT, Wellman GC, 2012. Inversion of neurovascular coupling by subarachnoid blood depends on large-conductance Ca2+-activated K+ (BK) channels. Proc. Natl. Acad. Sci 109, E1387–E1395. 10.1073/pnas.1121359109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonkusare SK et al. , 2012. Elementary Ca2+ signals through endothelial TRPV4 channels regulate vascular function. Science 336, 597–601. 10.1126/science.1216283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs EL, Lennox WG, Gibbs FA, 1940. Variations in the cabon dioxide content of the blood in epilepsy. Arch. Neurol. Psychiatry 43, 223–239. [Google Scholar]
- Lennox W, 1928. The effect on epileptic seizures of varying composition of respired air. J. Clin. Invest 6, 6–23. [Google Scholar]
- Yang X-F et al. , 2014. 5% CO2 inhalation suppresses hyperventilation-induced absence seizures in children. Epilepsy Res. 108, 345–348. 10.1016/j.eplepsyres.2013.11.012. [DOI] [PubMed] [Google Scholar]
- Avoli M, 2012. A brief history on the oscillating roles of thalamus and cortex in absence seizures. Epilepsia 53, 779–789. 10.1111/j.15281167.2012.03421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasper H, Kershman J, 1941. Electroencephalographic classification of the epilepsies. Arch. Neurol. Psychiatry 45, 903–943. [Google Scholar]
- Penfield W, Erickson T, 1941. Epilepsy and Cerebral Localization.
- Jones EG, 2007. The Thalamus, Vol. 1 Cambridge University Press. [Google Scholar]
- Steriade M, Llinás RR, 1988. The functional states of the thalamus and the associated neuronal interplay. Physiol. Rev 68, 649–742. [DOI] [PubMed] [Google Scholar]
- McCormick DA, Bal T, 1997. SLEEP AND AROUSAL: thalamocortical mechanisms. Annu. Rev. Neurosci 20, 185–215. 10.1146/annurev.neuro.20.1.185. [DOI] [PubMed] [Google Scholar]
- Dempsey E, Morison RS, 1942a. The interaction of certain spontaneous and induced cortical potentials. Am. J. Physiol 135, 301–308. [Google Scholar]
- Dempsey E, Morison RS, 1942b. The production of rhythmically recurrent cortical potentials after localized thalamic stimulation. Am. J. Physiol 135, 293–300. [Google Scholar]
- Morison R, Dempsey EW, 1942. Mechanism of thalamocortical augmentation and repetition. Am. J. Physiol [Google Scholar]
- Jasper HH, Droogleever-Fortuyn J, 1947. Experimental studies of the functional anatomy of petit mal epilepsy. Res. Publ. Assoc. Res. Nerve Ment. Dis 26, 272–298. [Google Scholar]
- Hunter J, Jasper HH, 1949. Effects of thalamic stimulation in unanaesthetised animals: the arrest reaction and petit Mal-like seizures, activation patterns and generalized convulsions. Electroencephalogr. Clin. Neurophysiol. 1, 305–324. 10.1016/0013-4694(49)90196-0. [DOI] [PubMed] [Google Scholar]
- Hanbery J, Jasper HH, 1953. Independence of diffuse thalamocortical projection system shown by specific nuclear destructions. J. Neurophysiol 252–271. [DOI] [PubMed] [Google Scholar]
- Fisher RAPD, 1977. Spike-wave rhythms in cat cortex induced by parenteral penicillin I. Electroencephalographic features. Electroencephalogr. Clin. Neurophysiol. 42, 608–624. [DOI] [PubMed] [Google Scholar]
- Avoli M, Gloor P, 1982a. Role of the thalamus in generalized penicillin epilepsy: observations on decorticated cats. Exp. Neurol 77, 386–402. 10.1016/0014-4886(82)90252-7. [DOI] [PubMed] [Google Scholar]
- Avoli M, Gloor P, 1982b. Interaction of cortex and thalamus in spike and wave discharges of feline generalized penicillin epilepsy. Exp. Neurol 76, 196–217. 10.1016/0014-4886(82)90112-1. [DOI] [PubMed] [Google Scholar]
- Avoli M, Gloor P, Kostopoulos G, Gotman J, 1983. An analysis of penicillin-induced generalized spike and wave discharges using simultaneous recordings of cortical and thalamic single neurons. J. Neurophysiol 50, 819–837. [DOI] [PubMed] [Google Scholar]
- Prince DA, Fischer D, 1969. “Centrencephalic” spike wave discharges following parenteral penicillin injection in the cat. Neurology 19, 309–310. [Google Scholar]
- van Heukelum S, Kelderhuis J, Janssen P, van Luijtelaar G, Lüttjohann A, 2016. Timing of high-frequency cortical stimulation in a genetic absence model. Neuroscience 324, 191–201. 10.1016/j.neuroscience.2016.02.070. [DOI] [PubMed] [Google Scholar]
- van Luijtelaar EL, Coenen AM, 1986. Two types of electrocortical paroxysms in an inbred strain of rats. Neurosci. Lett 70, 393–397. [DOI] [PubMed] [Google Scholar]
- Desiraju T, Purpura DP, 1970. Organization of specific-nonspecific thalamic internuclear synaptic pathways. Brain Res. 21, 169–181. 10.1016/0006-8993(70)90361-6. [DOI] [PubMed] [Google Scholar]
- Purpura DP, Cohen B, 1962. Intracellular recording from thalamic neurons during recruiting responses. J. Neurophysiol 25, 621–635. [DOI] [PubMed] [Google Scholar]
- Fuentealba P, Steriade M, 2005. The reticular nucleus revisited: Intrinsic and network properties of a thalamic pacemaker. Prog. Neurobiol 75, 125–141. 10.1016/j.pneurobio.2005.01.002. [DOI] [PubMed] [Google Scholar]
- Vergnes M, Boehrer A, Simler S, Bernasconi R, Marescaux C, 1997. Opposite effects of GABAB receptor antagonists on absences and convulsive seizures. Eur. J. Pharmacol 332, 245–255. 10.1016/S0014-2999(97)01085-6. [DOI] [PubMed] [Google Scholar]
- Sherwin I, 1965. Differentional effects of hyperventilation on the excitability of intact and isolated cortex. Electroencephalogr. Clin. Neurophysiol 18, 599–607. [DOI] [PubMed] [Google Scholar]
- Sherwin I, 1967. Alterations in the non-specific cortical afference during hypervenitlation. Electroencephalogr. Clin. Neurophysiol 23, 532–538. [DOI] [PubMed] [Google Scholar]
- Jahnsen H, Llinás R, 1984a. Electrophysiological properties of guinea-pig thalamic neurones: an in vitro study. J. Physiol 349, 205–226. 10.1113/jphysiol.1984.sp015153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llinás R, Jahnsen H, 1982. Electrophysiology of mammalian thalamic neurones in vitro. Nature 297, 406–408. [DOI] [PubMed] [Google Scholar]
- Steriade M, McCormick D, Sejnowski T, 1993. Thalamocortical oscillations in the sleeping and aroused brain. Science 262, 679–685. 10.1126/science.8235588. [DOI] [PubMed] [Google Scholar]
- Contreras D, Destexhe A, Sejnowski TJ, Steriade M, 1996. Control of spatiotemporal coherence of a thalamic oscillation by corticothalamic feedback. Science 274, 771–774. 10.1126/science.274.5288.771. [DOI] [PubMed] [Google Scholar]
- Destexhe A, Contreras D, Steriade M, 1998. Mechanisms underlying the synchronizing action of corticothalamic feedback through inhibition of thalamic relay cells. J. Neurophysiol 79, 999–1016. [DOI] [PubMed] [Google Scholar]
- Sherman SM, Guillery RW, 1996. Functional organization of thalamocortical relays. J. Neurophysiol 76, 1367–1395. [DOI] [PubMed] [Google Scholar]
- Bal T, Von Krosigk M, McCormick DA, 1995. Role of the ferret perigeniculate nucleus in the generation of synchronized oscillations in vitro. J. Physiol. (Lond.) 483, 665–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huguenard JR, McCormick DA, 1992. Simulation of the currents involved in rhythmic oscillations in thalamic relay neurons. J. Neurophysiol 68, 1373–1383. [DOI] [PubMed] [Google Scholar]
- McCormick DA, Huguenard JR, 1992. A model of the electrophysiological properties of thalamocortical relay neurons. J. Neurophysiol 68, 1384–1400. [DOI] [PubMed] [Google Scholar]
- Beenhakker MP, Huguenard JR, 2009. Neurons that fire together also conspire together: is normal sleep circuitry hijacked to generate epilepsy? Neuron 62, 612–632. 10.1016/j.neuron.2009.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huguenard JR, McCormick DA, 2007. Thalamic synchrony and dynamic regulation of global forebrain oscillations. Trends Neurosci. 30, 350–356. 10.1016/j.tins.2007.05.007. [DOI] [PubMed] [Google Scholar]
- McCormick DA, Contreras D, 2001. On the cellular and network bases of epileptic seizures. Annu. Rev. Physiol 63, 815–846. 10.1146/annurev.physiol.63.1.815. [DOI] [PubMed] [Google Scholar]
- Fogerson PM, Huguenard John R., 2016. Tapping the brakes: cellular and synaptic mechanisms that regulate thalamic oscillations. Neuron 92, 687–704. 10.1016/j.neuron.2016.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillery RW, Harting JK, 2003. Structure and connections of the thalamic reticular nucleus: advancing views over half a century. J. Comp. Neurol 463, 360–371. 10.1002/cne.10738. [DOI] [PubMed] [Google Scholar]
- Blumenfeld H, McCormick DA, 2000. Corticothalamic inputs control the pattern of activity generated in thalamocortical networks. J. Neurosci 20, 5153–5162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llinás R, Ribary U, Contreras D, Pedroarena C, 1998. The Neuronal Basis for Consciousness. vol. 353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steriade M, Contreras D, 1995. Relations between cortical and thalamic cellular events during transition from sleep patterns to paroxysmal activity. J. Neurosci 15, 623–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahnsen H, Llinás R, 1984b. Ionic basis for the electro-responsiveness and oscillatory properties of guinea-pig thalamic neurones in vitro. J. Physiol 349, 227–247. 10.1113/jphysiol.1984.sp015154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Parker WD, Wang K, 2014. The tole of T-type calcium channel genes in absence seizures. Front. Neurol 5 10.3389/fneur.2014.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheong E, Shin H-S, 2014. T-type Ca2+ channels in absence epilepsy. Pflugers Arch. – Eur. J. Physiol 466, 719–734. 10.1007/s00424-0141461-y. [DOI] [PubMed] [Google Scholar]
- Choi S, Yu E, Lee S, Llinás RR, 2015. Altered thalamocortical rhythmicity and connectivity in mice lacking CaV3.1 T-type Ca2+ channels in unconsciousness. Proc. Natl. Acad. Sci 112, 7839–7844. 10.1073/pnas.1420983112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro-Alamancos MA, 1999. Neocortical synchronized oscillations induced by thalamic disinhibition in vivo. J. Neurosci 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menuz K, Nicoll RA, 2008. Loss of inhibitory neuron AMPA receptors contributes to ataxia and epilepsy in Stargazer mice. J. Neurosci 28, 10599–10603. 10.1523/jneurosci.2732-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paz JT et al. , 2011. A new mode of corticothalamic transmission revealed in the Gria4/model of absence epilepsy. Nat. Neurosci 14, 1167–1173. http://www.nature.com/neuro/journal/v14/n9/abs/nn.2896.html#supplementaryinformation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soltesz I et al. , 1991. Two inward currents and the transformation of low-frequency oscillations of rat and cat thalamocortical cells. J. Physiol 441, 175–197. 10.1113/jphysiol.1991.sp018745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuth SG et al. , 2006. Membrane Resting Potential of Thalamocortical Relay Neurons Is Shaped by the Interaction Among TASK3 and HCN2 Channels Vol. 96. [DOI] [PubMed] [Google Scholar]
- Biel M, Wahl-Schott C, Michalakis S, Zong X, 2009. Hyperpolarization-activated cation channels: from genes to function. Physiol. Rev 89, 847–885. 10.1152/physrev.00029.2008. [DOI] [PubMed] [Google Scholar]
- Endeward V et al. , 2006. Evidence that aquaporin 1 is a major pathway for CO2 transport across the human erythrocyte membrane. FASEB J. 20, 1974–1981. 10.1096/fj.04-3300com. [DOI] [PubMed] [Google Scholar]
- Boron W, 2010. Evaluating the role of carbonic anhydrases in the transport of HCO3-related species. Biochim. Biophys. Acta (BBA) 1804, 410–421. 10.1016/j.bbapap.2009.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svichar N, Chesler M, 2003. Surface carbonic anhydrase activity on astrocytes and neurons facilitates lactate transport. Glia 41, 415–419. 10.1002/glia.10187. [DOI] [PubMed] [Google Scholar]
- Paxinos GA, Watson C, 2007. The Rat Brain in Stereotaxic Coordinates. Academic Press. [DOI] [PubMed] [Google Scholar]
- Adrian E, 1939. The spread of activity in the cerebral cortex. J. Physiol 88, 127–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang H, 1951. Dendritic potential of cortical neurons produced by direct electrical stimulation of the cerebral cortex. J. Neurophysiol 14, 1–21. [DOI] [PubMed] [Google Scholar]
- Burns B, 1950. Some properties of the cat’s isolated cortex. J. Physiol 111, 50–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohal VS, Huntsman MM, Huguenard JR, 2000. Reciprocal inhibitory connections regulate the spatiotemporal properties of intrathalamic oscillations. J. Neurosci 20, 1735–1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim U, Sanchez-Vives MV, McCormick DA, 1997. Functional dynamics of GABAergic inhibition in the thalamus. Science 278, 130–134. 10.1126/science.278.5335.130. [DOI] [PubMed] [Google Scholar]
- Sanchez-Vives MV, McCormick DA, 1997. Functional properties of perigeniculate inhibition of dorsal lateral geniculate nucleus thalamocortical neurons in vitro. J. Neurosci 17, 8880–8893. [DOI] [PMC free article] [PubMed] [Google Scholar]