Abstract
Background Ulnar styloid impaction syndrome (USIS) is produced by the tip of an oversized ulnar styloid inappropriately contacting the triquetrum. This condition results in chondromalacia, synovitis, and ulnar-sided wrist pain.
Case Description We report a rare case of bilateral USIS that presented with a prolonged course. The patient's symptoms resolved in both wrists following two separate ulnar styloidectomy procedures.
Literature Review Our case differs from previous reports in that it involves a patient whose own history of USIS led to a timelier diagnosis of the same disease in the contralateral wrist. To the best of our knowledge, there are no prior reports of bilateral USIS.
Clinical Relevance USIS remains an uncommon cause of ulnar-sided wrist pain and a particularly difficult diagnosis to confirm. Here, we illustrate that this syndrome can be confidently approached using a combination of careful attention to patient history, physical examination, and various imaging methods.
Keywords: ulnar styloid, syndrome, impaction, bilateral, ulnar-sided wrist pain
Syndromes causing ulnar-sided wrist pain are historically challenging to diagnose as well as treat. 1 2 3 4 5 6 The highly intricate anatomy of the ulnar wrist coupled with the dynamic nature of its injuries further complicate the pathology of this region. A particularly arduous condition, ulnar styloid impaction syndrome (USIS) involves impaction between the tip of the ulnar styloid process and the triquetrum bone. This syndrome is most commonly seen in patients with excessively long or hypertrophic ulnar styloid processes and is not necessarily associated with positive ulnar variance. 1 The ulnar styloid process index (USPI), calculated as the difference between the ulnar styloid length and the ulnar variance divided by the transverse diameter of the ulnar head, is commonly used to assess the size of the ulnar styloid. 2 An excessively long ulnar styloid has a length greater than 6 mm and/or a USPI more than 0.21. Repetitive friction of the proximal pole of the triquetrum and the ulnar styloid tip leads to chondromalacia, synovitis, and ulnar-sided wrist pain.
USIS has been a known entity for just over two decades. Despite a clear understanding of the mechanical dysfunction causing the syndrome, no consensus has been reached regarding the single best treatment once the diagnosis has been made. 2 3 Furthermore, the recommendations for diagnosing suspected USIS has varied in the literature, contributing to the difficulty in confidently making the diagnosis among hand and wrist specialists. This is a critical step in successful patient management. In general, the diagnostic algorithm should include a thorough history and physical examination, provocative testing, and some combination of imaging. 1 In addition, arthroscopy has been suggested as a useful modality in diagnosing USIS prior to an open approach, allowing direct visualization of impaction and potential chondromalacia of the triquetrum. Multiple authors have reported using this method before proceeding with a definitive styloidectomy, as arthroscopy may either include or exclude other potential causes of ulnar-sided wrist pain. 4
Previous work has demonstrated successful treatment of unilateral USIS with either ulnar styloidectomy or oblique ulnar styloid osteotomy (OUSO); the former has been performed both arthroscopically and with an open approach. We report a case of bilateral USIS that began insidiously on the left wrist and was subsequently discovered on the contralateral side in a patient with excessively long ulnar styloids. Successful diagnosis was made and surgically treated with open ulnar styloidectomy in both wrists.
The purpose of this report is to elaborate on how having high clinical suspicion, derived from patient history along with a physical examination that includes provocative testing and judicious use of radiographic imaging, in the setting of persistent failure of conservative treatments such as steroid injections, can lead to the correct diagnosis of USIS.
Case Report
The patient was a 21-year-old right-hand dominant male with a 7-month history of left-sided wrist pain that failed several conservative treatments, including oral and topical anti-inflammatory agents, occupational therapy, splinting/casting, and multiple intra-articular steroid injections to the ulnocarpal joint. Initially, the clinical presentation mimicked extensor carpi ulnaris (ECU) tendinitis or a ligamentous tear. An ensuing MRI showed no presence of ECU tendinopathy but revealed an increased T2 signal at the ulnar styloid attachment to the triangular fibrocartilage complex (TFCC), suggesting a tear of this structure and warranting further investigation. Exploratory arthroscopy with TFCC debridement gave the patient transient relief, but his pain returned just 1 year later. We ultimately determined that this patient's persistent symptoms were due to an elongated ulnar styloid impinging on the triquetrum. Plain radiographic measurements demonstrated a 9.3-mm ulnar styloid length and a USPI of 0.28, supporting a diagnosis of USIS. An open ulnar styloidectomy was performed on the left wrist, with resolution of the patient's symptoms thereafter.
Just over a year later, the patient presented to the outpatient clinic complaining of contralateral wrist pain for several months, particularly during gripping and loading. The right-sided ulnar wrist pain had no obvious inciting event, and up to that point, he had failed the same myriad of conservative treatments that were employed when he originally presented with left-sided wrist pain (anti-inflammatory drugs, splinting, intra-articular steroids). Acknowledging the prior workup and diagnosis of the left wrist, imaging was promptly obtained. Radiograph measurements revealed a right ulnar styloid length of 7 mm and a USPI of 0.28. MRI also confirmed an enlarged right ulnar styloid ( Fig. 1A , B ).
Fig. 1.
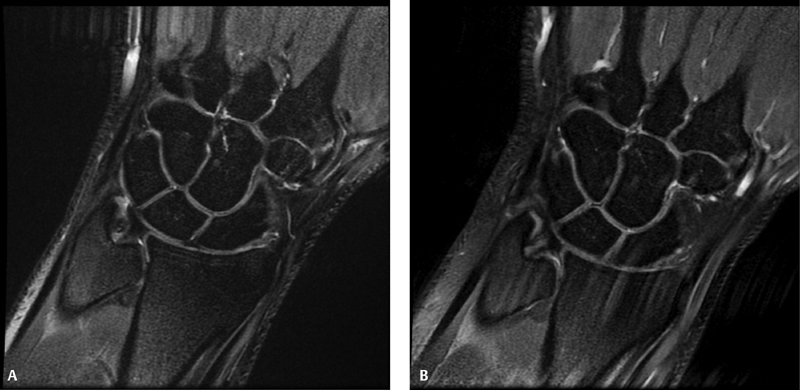
( A ) Preoperative, coronal T2-weighted MRI of the left wrist. ( B ) Preoperative, coronal T2-weighted MRI of the right wrist.
Because of the challenges and lengthy course of management of the patient's left wrist pain, a procedure to remove the distal aspect of the right ulnar styloid was recommended. The patient agreed to proceed with surgery once again. Preoperative X-rays of both wrists are shown in Figs. 2 to 4 .
Fig. 2.

Preoperative posteroanterior X-ray of the left wrist.
Fig. 4.

( A ) Preoperative posteroanterior X-ray of the right wrist. ( B ) Preoperative posteroanterior X-ray of the right wrist in ulnar deviation, demonstrating impaction potential of the ulnar styloid.
Fig. 3.
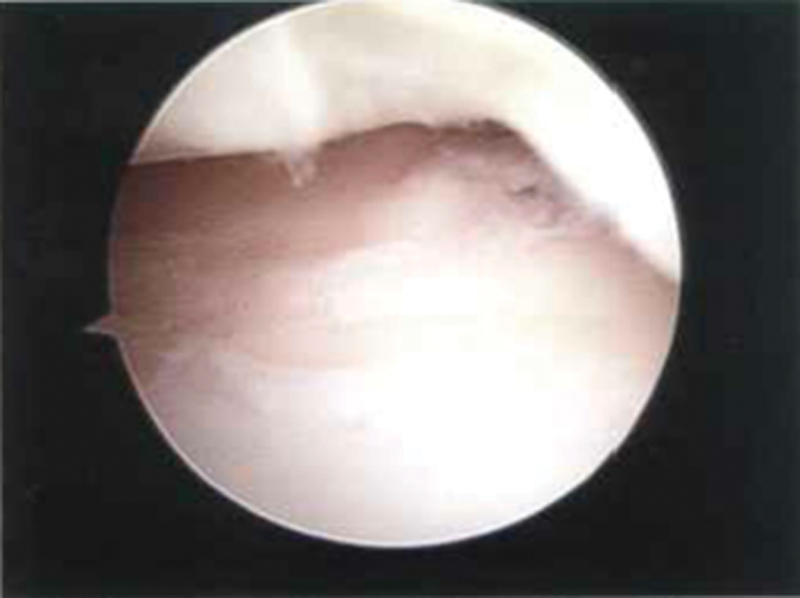
Arthroscopic image of the ulnocarpal joint space after debridement of the left TFCC (performed before the styloidectomy).
Operative Technique
The same general operative procedure was used on both wrists in this patient and is described here. A 2- to 4-cm incision was made in the area of the ulnar styloid prominence, parallel to the ulnar shaft and centered over the ulnocarpal joint. We dissected down to the level of the fascia where the dorsal cutaneous branch of the ulnar nerve was identified and protected. A deep knife was then used at the area of the ulnar collateral ligament for incision to the level of the ulnar styloid, where full-thickness flaps around the styloid tip were created. Once exposed, we used fluoroscopy to verify that we were at the styloid process and distal to the insertion of the superficial and deep radioulnar ligaments. Using a small osteotome and rongeur, the distal aspect of the tip was removed to the level of the fovea base, avoiding disruption of the TFCC insertion.
The wrist was stressed in pronation and supination, and the stability of the distal radioulnar joint was confirmed with direct visualization of the foveal integrity and under fluoroscopy. The wrist was brought through a final range of motion, ensuring that there was no remaining dynamic impingement of the ulnar styloid on the triquetrum with pronation of the forearm, ulnar deviation of the wrist, and loading of the carpus. Postoperative X-rays of both wrists demonstrated sufficient excision of an elongated ulnar styloid ( Figs. 5 and 6 ).
Fig. 5.

Postoperative posteroanterior X-ray of the left wrist demonstrating final styloid resection.
Fig. 6.

Postoperative posteroanterior X-ray of the right wrist demonstrating styloid resection.
Successful rehabilitation was achieved with postoperative splinting for 2 weeks followed by application of a brace and outpatient occupational therapy with transition to a home program. The patient had complete resolution of his pain by 3 months postoperation in the left wrist and 4 months postoperation in the right wrist. Full range of motion and function were also achieved in the respective timeframes.
Discussion
USIS is a relatively uncommon cause of ulnar-sided wrist pain. Our patient experienced several months of chronic, relapsing pain on the left wrist that failed a multitude of conservative treatments. Following our diagnosis of USIS and subsequent styloidectomy, the patient was free of complaints by the 3-month follow-up visit. Coincidentally, the same patient presented with similar symptomatology on the contralateral wrist 1 year later. After an exhaustive course of conservative and surgical treatment for the left wrist, we were consequently more efficient in definitive management of this patient's right wrist pain, as there was now a higher clinical suspicion for USIS along with radiographic demonstration of an enlarged right ulnar styloid. Essentially, we followed the diagnostic algorithm from our initial experience with the left wrist but opted not to use arthroscopic debridement, as it provided only temporary pain relief for the patient's original case.
Without clinical suspicion and adequate workup, USIS can be an elusive condition and challenging to confirm in the presence of persistent ulnar-sided wrist pain. Wrist arthroscopy has been proposed as a useful step in diagnosing USIS, providing direct visualization of impaction and potential chondromalacia of the articular cartilage at the level of the triquetrum. 2 Additionally, it may be used to rule out other conditions that cause ulnar-sided wrist pain, including TFCC disruption, lunotriquetral ligament disruption, and ulnocarpal impaction. However, our case shows that USIS can be effectively diagnosed with thorough clinical assessment and various imaging modalities, both with and without the aid of arthroscopy. We diagnosed left-sided USIS in our patient only after arthroscopic TFCC debridement was deemed unsuccessful. Exploratory or therapeutic arthroscopy was then deferred for the right wrist in the setting of high clinical suspicion based on physical examination and diagnostic radiology. Moreover, our patient was unique in the sense that he presented with a particularly troublesome disease of one wrist that ultimately served to support a higher index of suspicion for the same process occurring in the contralateral extremity. Consideration of these factors ultimately led to a conclusive diagnosis and effective treatment, avoiding the prolonged course typically accompanying USIS. 1
Ulnar styloid impingement has been described previously, first by Topper et al who reported on a group of eight patients in 1997. 1 D'Agostino et al and Tomaino et al also discussed similar studies with a small patient series in 2011 and 2001, respectively. 3 5 All authors reported successful treatment with ulnar styloid osteotomy. More recently, studies by Ahsan et al in 2016 and Bain and Bidwell in 2006 have argued for intervention through an arthroscopic approach. 2 4 While these studies also reported positive outcomes, we elected for an open approach in both of our patient's operations, employing arthroscopy only on his initial presentation, with subsequent recurrence of wrist pain shortly afterward. By the time our patient presented with right-sided wrist pain, his grossly similar symptomatology, physical examination, and radiographic findings afforded us the luxury to forego arthroscopy and to definitively treat him with surgery. Nevertheless, arthroscopy remains useful when considering a diagnosis of USIS since MRI is not entirely specific. It can also give insight regarding other causes of ulnar-sided wrist pain before undergoing styloidectomy.
D'Agostino et al specifically described OUSO as a therapeutic measure. 3 This procedure primarily aims at preventing damage to the ulnolunate, ulnotriquetral, and ulnar collateral ligaments of the TFCC while preserving all ligamentous attachments at the distal pole of the ulnar styloid. While our method does not accomplish the latter, careful soft tissue repair was performed during closure, with careful attention not to violate the more biomechanically important distal radioulnar ligaments. The clinical improvement in our patient with bilateral surgery argues that an open approach without osteotomy does provide sufficient treatment.
Our case differs from previous investigations in that it involves USIS in the left wrist of a patient, which conferred a clinical advantage for discovering the same syndrome on the contralateral side shortly thereafter. Ulnar styloidectomy using an open approach completely resolved the patient's symptoms. Therefore, the diagnosis of USIS should be considered in patients with ulnar-sided pain and oversized ulnar styloids (by length and/or USPI). Furthermore, our patient's symptom course suggests that individuals with unilateral USIS should be counseled on the possibility of developing contralateral symptoms. To the best of our knowledge, there have been no previous reports of bilateral USIS in the orthopaedic literature.
Ultimately, this syndrome continues to be an uncommon occurrence with a lack of prospective evidence for accurate diagnosis and treatment. Without an established standard of care for this pathology, we hope that this case promotes the use of radiographic imaging and provocative physical examination in combination with clinical suspicion to uncover an insidious disease process, which should be treated conservatively before moving forward with surgical intervention. Although the small number of case series and reports, such as our own described here, makes any analysis more challenging, future studies should aim to further describe the most beneficial diagnostic methodologies and corresponding treatment approaches.
Acknowledgments
The authors thank Ms. MaryAnn Gaffuri for her outstanding contributions to this investigation, including patient communication, medical record retrieval, and image gathering.
Conflict of Interest None declared.
Note
This investigation was conducted at the Albany Medical Center and the Capital Region Bone and Joint Center, which are located in Albany, NY.
References
- 1.Topper S M, Wood M B, Ruby L K. Ulnar styloid impaction syndrome. J Hand Surg Am. 1997;22(04):699–704. doi: 10.1016/S0363-5023(97)80131-1. [DOI] [PubMed] [Google Scholar]
- 2.Ahsan Z S, Rivlin M, Jupiter J B. Ulnar-sided wrist pain due to long ulnar styloid: a case report. J Wrist Surg. 2016;5(04):311–314. doi: 10.1055/s-0035-1570743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.D'Agostino P, Townley W A, Le Viet D, Roulot E. Oblique ulnar styloid osteotomy--a treatment for ulnar styloid impaction syndrome. J Hand Surg Am. 2011;36(11):1785–1789. doi: 10.1016/j.jhsa.2011.07.023. [DOI] [PubMed] [Google Scholar]
- 4.Bain G I, Bidwell T A. Arthroscopic excision of ulnar styloid in stylocarpal impaction. Arthroscopy. 2006;22(06):6770–677000. doi: 10.1016/j.arthro.2006.04.083. [DOI] [PubMed] [Google Scholar]
- 5.Tomaino M M, Gainer M, Towers J D. Carpal impaction with the ulnar styloid process: treatment with partial styloid resection. J Hand Surg [Br] 2001;26(03):252–255. doi: 10.1054/jhsb.2001.0591. [DOI] [PubMed] [Google Scholar]
- 6.Sanmartín-Fernández M, Couceiro-Otero J, Costas-Alvarez M, Sotelo-Garcia A. Extensor carpi ulnaris tenosynovitis caused by the tip of an oversized ulnar styloid: a case report. J Wrist Surg. 2015;4(01):65–67. doi: 10.1055/s-0034-1398473. [DOI] [PMC free article] [PubMed] [Google Scholar]


