Abstract
Objective:
To evaluate a novel educational intervention for physician trainees to improve sexual healthcare provision, including condom distribution, in the pediatric emergency department.
Methods:
Resident physicians and medical students in an urban pediatric emergency department viewed an evidence-based educational video on sexual healthcare provision. It featured role-plays and a description of the condom distribution process, and targeted trainees who provide healthcare to patients aged ≥14 years with potential genitourinary (GU) complaints. Trainees completed pre- and post-intervention surveys to assess attitudes, motivation and confidence for four recommended practices (Likert scale, 1=not at all to 4=extremely). We used Wilcoxon signed rank tests to assess differences in paired responses to motivation and confidence statements. A subset of 33 trainees completed a brief survey to assess condom distribution during emergency department clinical encounters.
Results:
51/56 (91%) trainees participated: 53% female, 58% from pediatrics. At baseline, participants reported high levels of confidence and motivation to provide sexual healthcare. Post-intervention, there were significant increases in the proportion of participants who reported greater motivation and confidence to: 1) ask a parent to step out of the room, 2) obtain sexual history, 3) discuss condom use, and 4) offer condoms (all p<0.05). Post-intervention, fewer participants “agreed/strongly agreed” that there is inadequate time to obtain sexual histories (22% vs. 45%, p<0.05). Most (60%) sexually active patients accepted condoms during clinical care.
Conclusion:
In this pediatric emergency department, a low-cost intervention showed promise to improve trainee attitudes, motivation, and confidence towards adolescent sexual healthcare provision. This data may inform strategies to improve access to care for this population.
Keywords: Adolescent sexual health, condom distribution, educational intervention
Introduction
Adolescents in the U.S. are disproportionately affected by sexually transmitted infections (STIs) and unintended pregnancies. While these outcomes are preventable, adolescents face significant barriers to sexual healthcare, including lack of access to knowledgeable healthcare providers (HCPs) and concerns about privacy and costs.1,2,3 Reduced access to care contributes to STIs, unintended pregnancies, and adolescent health disparities.4 As such, there is growing support for the use of non-traditional settings, including the emergency department (ED), to improve adolescent sexual health services; specifically the provision of contraception (including condoms), behavioral counseling, and linkage to primary care.5,6
Adolescents make approximately 19 million ED visits annually and often do not receive regular primary care.7,8 These youth frequently report high-risk sexual behaviors,9 and have rates of Chlamydia trachomatis and Neisseria gonorrhea infection up to 7 times higher than the general population.10 Though adolescents often present to EDs with complaints possibly indicating STIs11, HCPs frequently fail to inquire about sexual health behaviors and risks.12,13,14,15,16 Provider-level barriers include lack of knowledge and communication skills regarding adolescent sexual health.2
The ED represents an important, but underutilized location for reaching large numbers of at-risk adolescents. However, few proven interventions are available for ED providers to improve sexual health care provision.17,18 The primary objective of this study was to develop a novel educational intervention for trainees to improve attitudes, confidence and motivation regarding adolescent sexual healthcare, including provision of condoms. We also describe a new process to make condoms available for adolescents within our pediatric ED.
Materials and Methods
Study Design
We conducted pre-intervention (Time 1) and immediate post-intervention (Time 2) surveys to assess attitudes, motivation, and confidence to obtain sexual history and discuss condom use (see pre-intervention and post-intervention surveys, Supplemental Digital Content 1 and 2) among n= 51 medical trainees exposed to our intervention. A subset was surveyed during clinical care to assess condom distribution to eligible adolescent patients. This study was conducted from January 1, 2013 to March 31, 2013 within the ED at a Midwestern urban pediatric hospital. This study was approved by the hospital institutional review board.
Sample
Trainees (medical students and resident physicians) were eligible for participation if they were completing a one-month rotation in the pediatric ED. Trainees working in the ED for sporadic shifts were excluded.
The patient population is primarily non-White (68%) with public or no insurance (71%). The ED is staffed by pediatric emergency medicine (PEM) and emergency medicine trained physicians who provide supervision and clinical training for trainees with varied clinical experience. Nurse practitioners and general pediatricians provide care independently.
Intervention for Adolescent Sexual Health
Intervention Development:
We involved key stakeholders (i.e., ED administration, physicians and nurses) when designing the video intervention and the process for condom distribution. Stakeholder feedback informed our focus on physician trainees as study participants and our decision to limit condoms to a specific subset of ED patients (i.e., youth old enough to provide legal consent for sexual intercourse who have GU complaints). We educated all ED staff to prepare for intervention implementation.
Educational Intervention:
Participants viewed a novel, ten minute web-based video we created (see video, Supplemental Digital Content 3) based on national guidelines for providing sexual health care.19,20,21,22,23 Based on state law, as well as our previous research with PEM providers,1,2 we tailored our project specifically for adolescents aged ≥ 14 years seeking care in the ED with potential genitourinary (GU) complaints. The video provided epidemiologic information regarding the significance of STIs and unintended pregnancy, and barriers to care. We also described a new condom distribution process (detailed below). We featured role-play scenarios to highlight four recommended practices: 1) ask a parent/guardian to step out of the room to establish privacy, 2) obtain a thorough sexual history, 3) discuss condoms, and 4) offer condoms to sexually active adolescents.
Condom distribution process:
Initially, condoms were only available in limited practice settings at our institution. Therefore, we developed and piloted a new process for condom distribution in the ED. Study authors (DJ, MKM) met with key stakeholders (e.g., ED nurses and physicians, ED administrators) to discuss integration of condoms into clinical care. We partnered with our local health department, which provided individual packages containing 2–3 condoms, lubricant, and condom use instructions (in Spanish and English). Stakeholders were supportive and agreed on the following process: 1) condom packages would be stored in the main physician charting room, 2) while conducting the private sexual health interview, trainees would distribute condoms confidentially to interested patients, and 3) trainees would inform the supervising physician when condoms were distributed. This new process was described to study participants and all ED staff via the intervention video, e-mail, and signs posted in ED staff areas.
Study Procedures
Recruitment
Educational Intervention:
We recruited participants via an e-mail with corresponding hyper-links to the web-based surveys (Survey Monkey) and online educational intervention. Participants were required to complete the pre-intervention survey in order to access the video. The post-intervention survey immediately followed the end of the video. E-mails were sent to all trainees several days prior to the start of their ED rotation. In addition, one team member (DJ) reminded trainees in person of the recruitment email. To protect participant anonymity and confidentiality, participants created unique numeric identifier codes, to be used for paired analyses before and after exposure to the intervention.
Condom Distribution Process:
Following completion of the intervention, a convenience subset of participants providing care to adolescents in the ED completed a written survey regarding clinical care and the condom distribution process (See condom distribution survey, Supplemental Digital Content 4). Trained research assistants (RAs) used a computerized tracking board in the ED to identify eligible participants (i.e., trainees who had completed the video intervention and were providing care for an adolescent ≥ 14 years with a GU complaint). Recruitment during this phase was based on RA availability, which varied across days of the week and time of day. Following their initial patient evaluation, RAs asked participants to complete a brief survey. Each participant could complete this assessment a maximum of two times.
Measures
The survey was developed by the authors, guided by variables deemed relevant in adolescent medicine and behavior change literature.24,25 Demographic data included age, gender, level of training, training specialty, and completion of a previous ED or adolescent medicine rotation. To assess practice patterns, we assessed frequency (1=not at all to 4=always) of sexual health history inquiry (e.g., previous sexual intercourse, number of lifetime partners) with female and male adolescent ED patients. To assess attitudes and beliefs, participants were asked to indicate their level of agreement (1=strongly disagree to 4=strongly agree) with several statements, e.g., “I am uncomfortable discussing sex with adolescent patients.” Guided by literature on Motivational Interviewing,26,27 we used a Likert scale (1=not at all to 4=extremely), to determine participants’ motivation and confidence to perform four recommended practices (e.g., ask a parent to step out of the room).
Completion of all three components (pre-intervention survey, intervention, and post-intervention survey), took approximately 20 minutes. We piloted the survey with nine PEM fellows and four faculty members for comprehension and clarity, which resulted in minimal revisions.
Condom Distribution Survey
The condom distribution process was assessed by six closed-ended questions to determine who was present with the patient and whether the recommended practices were performed. Participants were asked to provide reasons when practices were not completed. Two open-ended questions elicited feedback on the condom distribution process.
Statistical Analysis
Video Intervention:
Demographic characteristics and baseline health assessment practices were summarized by standard descriptive measures. We used Wilcoxon signed rank tests to assess differences in paired responses to motivation and confidence statements. Responses to frequency, attitudes, and beliefs were dichotomized (e.g., “strongly agree/agree” vs. “strongly disagree/disagree”). Comparisons between subgroups (e.g. gender, level of training) were analyzed using chi-square tests for categorical data. We used McNemar’s test to analyze differences in paired proportions. The sample size of n=51 paired proportions provided 90% power to detect a difference in proportions of 20% with an expected discordant pair proportion of 25% and a two-sided alpha of 0.05. Analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC).
Condom Distribution:
Sexual health practices and condom distribution during clinical care were summarized by standard descriptive measures. Responses to the two condom distribution process questions i.e., “how is the current condom distribution process working,” “any suggestions to improve distribution process”) were coded by two authors (DJ, MKM) with any disagreements resolved by consensus from a third author (SFK).
Results
Educational Intervention:
Among the 56 trainees recruited, n=51 (91%) participated. Most participants were female (53%), pediatric resident physicians (58%), and had not completed a rotation in adolescent health (59%), Table 1.
Table 1.
Characteristics of participants (N=51).
| Characteristics | N (%) |
|---|---|
| Gender | |
| Female | 27 (52.9) |
| Male | 24 (47.1) |
| Age (in years) | |
| 20–29 | 36 (70.6) |
| 30–39 | 13 (25.5) |
| 40–49 | 2 (3.9) |
| Level of Training | |
| Medical student | 2 (3.9) |
| PGY 1 | 18 (35.3) |
| PGY 2 | 13 (25.5) |
| PGY 3 | 18 (35.3) |
| Training Specialty | |
| Pediatrics | 26 (58.3) |
| Emergency medicine | 14 (29.2) |
| Family medicine | 6 (12.5) |
| Not applicable (medical students) | 2 (3.9) |
| Completed previous ED Rotation | |
| Yes | 32 (62.7) |
| No | 19 (37.3) |
| Completed previous adolescent medicine Rotation | |
| Yes | 21 (41.2) |
| No | 30 (58.8) |
Sexual Health Assessment Practices
Overall, at pre-intervention, participants infrequently performed complete sexual health assessments. Compared to female patients, participants more frequently asked male patients about previous intercourse, though this was not statistically significant (Table 2). Neither participant gender nor level of medical training was associated with any differences in pre-intervention assessment practices.
Table 2.
Baseline (pre-intervention) sexual health assessment practices for adolescent patients with genito-urinary complaints in the ED (participants responding “always”)
| Assessment practice | Female patients N (%) |
Male patients N (%) |
P value |
|---|---|---|---|
| Previous sexual intercourse | 18 (36.7) | 25 (51.0) | .092 |
| Last sexual intercourse | 6 (12.5) | 10 (20.8) | .125 |
| Number of lifetime partners | 3 (6.1) | 5 (10.2) | .625 |
| Gender of partners (male, female or both) | 5 (10.2) | 7 (14.3) | .625 |
| Previous STIsa | 17 (34.7) | 22 (44.9) | .180 |
| Condom use | 24 (49.0) | 22 (44.9) | .754 |
| Last menstrual period | 29 (58.0) | N/A | |
| Previous anal intercourse | 3 (6.1) |
= Sexually Transmitted Infections
Impact of Educational Intervention
Motivation and Confidence to provide sexual health care
At pre-intervention, participants reported high levels of confidence and motivation to provide sexual health care (Table 3). Post-intervention, for male and female patients, there were significant increases in the number of participants who reported greater motivation and confidence to: 1) ask a parent to step out of the room, 2) obtain sexual history, 3) discuss condom use, and 4) offer condoms (Table 3). When examined separately by gender, female participants reported an increase in confidence to obtain a sexual history (median difference 0, IQR=1, p=0.02) while male participants did not (median difference 0, IQR=0, p=0.25). No other pre- to post-intervention changes were found.
Table 3.
Motivation and confidence in sexual health assessment practices pre- and post-intervention (Median score and range)
| Pre-intervention Median (Range) |
Post-intervention Median (Range) |
P | |
|---|---|---|---|
| Female Patient | |||
| Motivation | |||
| Ask parent to step out | 3.5 (2–4) | 4.0 (3–4) | <0.001 |
| Obtain sexual history | 4.0 (2–4) | 4.0 (3–4) | <0.001 |
| Discuss condoms | 3.0 (2–4) | 4.0 (2–4) | <0.001 |
| Offer condoms | 3.0 (1–4) | 4.0 (1–4) | <0.001 |
| Confidence | |||
| Ask parent to step out | 4.0 (2–4) | 4.0 (3–4) | 0.002 |
| Obtain sexual history | 4.0 (2–4) | 4.0 (3–4) | 0.003 |
| Discuss condoms | 4.0 (2–4) | 4.0 (3–4) | <0.001 |
| Offer condoms | 3.0 (1–4) | 4.0 (1–4) | <0.001 |
| Male Patient | |||
| Motivation | |||
| Ask parent to step out | 4.0 (2–4) | 4.0 (3–4) | <0.001 |
| Obtain sexual history | 4.0 (2–4) | 4.0 (2–4) | 0.033 |
| Discuss condoms | 3.0 (2–4) | 4.0 (3–4) | <0.001 |
| Offer condoms | 3.0 (1–4) | 4.0 (1–4) | <0.001 |
| Confidence | |||
| Ask parent to step out | 4.0 (2–4) | 4.0 (3–4) | 0.004 |
| Obtain sexual history | 4.0 (2–4) | 4.0 (3–4) | 0.011 |
| Discuss condoms | 4.0 (2–4) | 4.0 (3–4) | <0.001 |
| Offer condoms | 3.0 (1–4) | 4.0 (1–4) | <0.001 |
Attitudes towards providing sexual health care
Discomfort discussing sexual health and time constraints were the two most common barriers reported before the intervention (Table 4). Post-intervention, significantly fewer participants agreed that “there is inadequate time in an ED visit to obtain sexual histories” (22% vs. 45%, p< 0.05).
Table 4.
Perceived barriers to sexual health assessments before and after intervention (participants responding “agree or strongly agree”).
| Pre N (%) |
Post N (%) |
P value |
|
|---|---|---|---|
| Attitudes and Beliefs | |||
| Because of my religious/cultural beliefs, I am uncomfortable discussing sex with adolescent patients | 2 (3.9) | 0 (0) | -- |
| Because of my religious/cultural beliefs, I am uncomfortable offering condoms to adolescent patients | 7 (13.7) | 5 (9.8) | .500 |
| Providing condoms promotes promiscuity among adolescents | 3 (5.9) | 3 (5.9) | -- |
| I am more comfortable discussing sex w/ older adolescents | 35 (68.6) | 32 (62.7) | .250 |
| Training | |||
| I lack sufficient training in obtaining sexual histories from adolescents | 4(7.8) | 1(2.0) | .250 |
| Time | |||
| I am concerned that there is not enough time in an ED visit to appropriately discuss sexual health issues | 23 (45.1) | 11 (21.6) | <.001b |
= significant
Condom Distribution Process
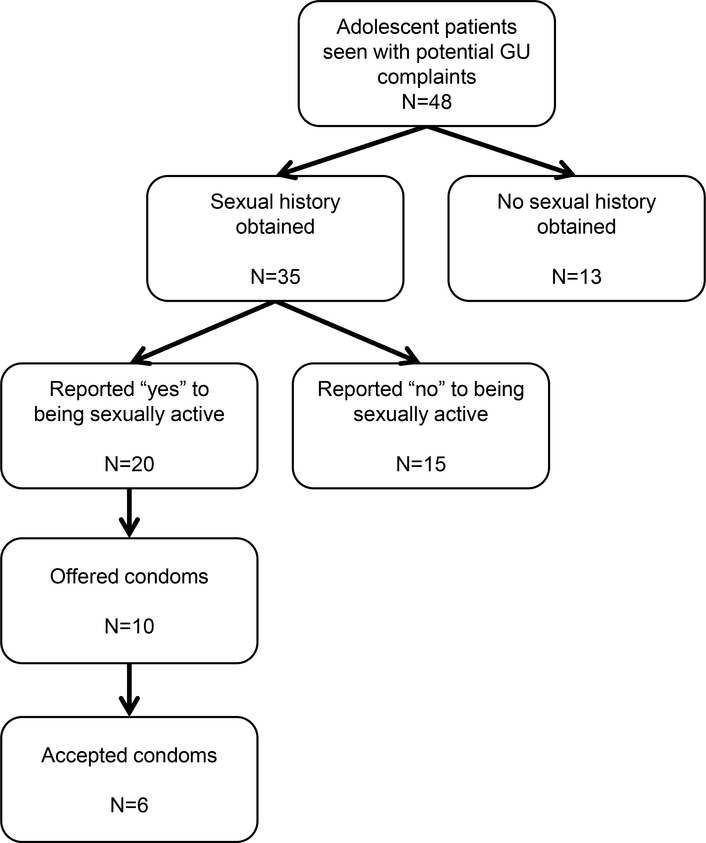
During 48 clinical care encounters, trainee participants (n=33) reported sexual history assessment in 73% of encounters with adolescents ≥ 14 years with a GU complaint. Most adolescents (60%), who reported previous sexual activity during sexual history assessment, accepted condoms when offered (Figure 1).
Figure 1:
Sexual health assessment practices and condom distribution during clinical care.
Reasons for not offering condoms were: patient not currently sexually active (n=3), patient already using condoms (n=2), patient sexual orientation (i.e., lesbian; n=1), trainee participant believed visit was not related to sexual health (n=3), or no answer provided (n=1). For 31 encounters, participants provided responses to the open-ended questions and all felt condoms should continue to be available in the ED and were satisfied with the current distribution process.
A small number of ED nurses and staff physicians questioned if this type of care was appropriate in the pediatric, acute care setting; citing concerns of parents and community disapproval of providing condoms. We resolved these issues by holding informal forums for staff to voice concerns, providing additional staff education, removing flavored condoms, and clarifying that staff physicians would be notified when condoms were distributed by trainees under their direct supervision. Notably, study participants responsible for distributing the condoms were invariably positive regarding the program.
Discussion
This study demonstrates the impact of a brief, web-based educational intervention that significantly improved provider motivation and confidence to perform recommended sexual healthcare practices among physician trainees in a pediatric ED. Participants demonstrated an increase in confidence to obtain sexual histories for male and female patients with changes in confidence most notable among female trainees. The perception of inadequate time as a barrier to care provision was significantly reduced, which may be important in influencing practice change.
Interventions to change provider behavior around sexual health practices in the pediatric ED have been mixed.18,28 From our previous work2 as well as the literature,29 we anticipated provider- and system-level barriers to bringing condoms to our ED. While the majority of trainees supported the newly implemented program, some ED staff expressed concerns during the study. Providing an opportunity to air concerns and being willing to make modifications to the initial process were key to garnering support for condom distribution in the ED.
Given the high demands on provider time, we designed a brief online intervention accessible at their convenience. A minimal investment of time and financial resources were required to develop and implement this educational intervention; making replication in the ED or other clinical settings feasible. A few studies describe video interventions for providers, most commonly focusing on improved communication with patients and attitudes towards patients with sickle cell disease.30,31 Our work highlights a video intervention to improve provider communication and best practices for sexual health among adolescents; recognizing these skills are often underdeveloped in traditional medical training, and contribute to missed prevention opportunities among youth.32 Future studies to assess the intermediate and long term impact of this intervention on provider practice are warranted.
Limitations:
Several limitations should be considered. While this study had a small sample size and lacked a control group, the literature demonstrates that similar sample sizes and design have been used for initial intervention evaluation.33,34,35 Data was collected from a single, Midwestern urban pediatric ED, thus findings may not be generalizable to trainees in varied geographic locations. Due to the rotating nature of trainees in the ED, we only obtained immediate post-intervention assessments and do not know if changes will be sustained over time.
It was surprising that many of our participants reported such high levels of confidence at baseline in providing sexual healthcare, given multiple reports of HCP deficits in this area.14–16 This may reflect improved training in this area, or a degree of self-reporting bias as participants may have felt an expectation to be well versed in sexual health or had concerns regarding confidentiality. Despite higher than anticipated reporting at baseline, significant improvements in provider confidence were observed.
Conclusion:
This educational intervention shows promise to improve the quality of adolescent sexual healthcare provided by physician trainees in a busy pediatric ED, which may improve access to care for adolescents. Future studies should focus on the evaluation of sustained changes in trainee attitudes, motivation, and confidence over time and the potential use of this intervention in other clinical settings.
Supplementary Material
Pre-intervention survey
Post-intervention survey
educational intervention video
Condom distribution survey
Acknowledgements:
We gratefully acknowledge this individual who contributed significantly to the work presented in this article: Sharon Humiston for her assistance in preparing and editing the surveys and abstract.
The authors report no external funding source for this study.
Abbreviations:
- STIs
sexually transmitted infections
- HCPs
healthcare providers
- ED
emergency department
- PEM
pediatric emergency medicine
- GU
genitourinary
- RAs
research assistants
Footnotes
The authors declare no conflict of interest.
The abstract of this manuscript was displayed in the exhibition hall at the Pediatric Academic Societies annual meeting in Vancouver in May 2014.
References
- 1.Miller MK, Plantz DM, Dowd MD, et al. Pediatric emergency medicine health care providers’ knowledge, attitudes and experiences regarding emergency contraception. Acad Emer Med. 2011; 18: 605–612. [DOI] [PubMed] [Google Scholar]
- 2.Miller MK, Hornberger L, Sherman AK, et al. (2013). Acceptability of Sexual Health Discussion and Testing in the Pediatric Acute Care Setting. Pediatric emergency care. 2013; 29(5): 592–597. [DOI] [PubMed] [Google Scholar]
- 3.Cohen D, Scribner R, Bedimo R, et al. Cost as a barrier to condom use: the evidence for condom subsidies in the United States. Am J Public Health. 1999; 89(4): 567–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rizkalla C, Bauman LJ, Avner JR. Structural impediments to condom access in a High HIV/STI-risk area. Journal of environmental and public health. Volume 2010: Article ID 630762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ford CA, Bearman PS, Moody J. Foregone health care among adolescents. JAMA 1999; 282(23): 2227–2234. [DOI] [PubMed] [Google Scholar]
- 6.Hock-Long L, Herceg-Baron R, Cassidy AM, et al. Access to adolescent reproductive health services: financial and structural barriers to care. Perspectives on sexual and reproductive health.2003–05; 35: 144–147. [PubMed] [Google Scholar]
- 7.O’Brien Rebecca F Condom Use by Adolescents. Pediatr.2013; 132: 973–981. DOI: 10.1542/peds.2013-2821 [DOI] [PubMed] [Google Scholar]
- 8.Ziv A, Boutlet JR, Slap GB. Emergency department utilization by adolescents in the US. Pediatr 1998; 101: 987–994. [DOI] [PubMed] [Google Scholar]
- 9.Park MJ, Mulye TP, Adams SH, et al. The health status of young adults in the United States. Journal of adolescent health.2006; 39: 305–317. [DOI] [PubMed] [Google Scholar]
- 10.Scott ME, Wildsmith E, Welti K, et al. Risky Adolescent Sexual Behaviors and Reproductive Health in Young Adulthood. Perspectives on Sexual and Reproductive Health. 2011; 43(2): 110–118, doi: 10.1363/4311011 [DOI] [PubMed] [Google Scholar]
- 11.Biro FM, Rosenthal SL, Kiniyalocts M. Gonoccocal and chlamydial genitourinary infections in symptomatic and asymptomatic adolescent women. Clin Pediat (Phila). 1995; 34(8): 419–423. [DOI] [PubMed] [Google Scholar]
- 12.Wimberly YH, Hogben M, Moore-Ruffin J, et al. Sexual history-taking among primary care physicians. J Natl Med Assoc, 2006; 98(12): 1924–1929. [PMC free article] [PubMed] [Google Scholar]
- 13.Torkko KC, Gershman K, Crane LA, et al. Testing for Chlamydia and sexual history taking in adolescent females: results from a statewide survey of Colorado primary care providers. Pediatrics. 2000; 106(3): E32 doi: 10.1542/peds.106.3.e32 [DOI] [PubMed] [Google Scholar]
- 14.Goyal M, McCutcheon M, Hayes K, et al. Sexual history documentation in adolescent emergency department patients. Pediatrics. 2011; 128 (1). [DOI] [PubMed] [Google Scholar]
- 15.Banas DA,Cromer BA,Santana M, et al. Comparison of clinical evaluation of genitourinary symptoms in female adolescents among primary care versus emergency department physicians. J Pediatr Adolesc Gynecol. 2010;23(2):71–76 [DOI] [PubMed] [Google Scholar]
- 16.Musacchio NS, Gehani S, Garofalo R. Emergency department management of adolescents with urinary complaints: missed opportunities. J Adolesc Health. 2009; 44(1):81–83 [DOI] [PubMed] [Google Scholar]
- 17.Chernick L, Westhoff CL, Ray M, et al. An enhanced referral process of sexually active adolescent females from the emergency department to family planning clinic: can we improve follow up? Abstract presented at The American Academy of Pediatrics NCE October 25, 2013. [Google Scholar]
- 18.Pitts SA, Corliss HL, Kharasch SJ, et al. Advance provision of emergency contraception in an urban pediatric emergency department. J Pediatr Adolesc Gynecol. 2011; 24(6): 392–396. [DOI] [PubMed] [Google Scholar]
- 19.Hagan JF, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 20.Copperman S GAPS (AMA Guidelines for Adolescent Preventive Services). Arch Pediatr Adolesc Med. 1997; 151(9): 957–958. doi: 10.1001/archpedi.1997.02170460095019 [DOI] [PubMed] [Google Scholar]
- 21.World Wide Web. U.S Preventive Services Task Force. Available at:http://www.uspreventiveservicestaskforce.org/uspstf13/sti12/sties.pdf. Accessed August 13, 2012.
- 22.World Wide Web Physicians for Reproductive Health. Standardized case videos: Adolescent reproductive and sexual health/. Available at: http://prh.org/resources/standardized-case-videos-adolescent-reproductive-and-sexual-health. Accessed September 5, 2012.
- 23.World Wide Web Physicians for Reproductive Health. Adolescent reproductive and sexual health education program (ARSHEP). Available at: http://prh.org/teen-reproductive-health/arshep-explained/ Accessed September 5, 2012.
- 24.Morand A, McLeod S, Lim R. Barriers to sexual history taking in adolescent girls with abdominal pain in the pediatric emergency department. Pediatr Emerg Care.2009; 25(10): 629–632. [DOI] [PubMed] [Google Scholar]
- 25.Rollnick S, Mason P, Butler C. Health Behavior Change: A Guide for Practitioners. London, UK: Churchill Livingstone; 1999. [Google Scholar]
- 26.Miller WR, Rollnick S. Motivational Interviewing: Preparing People For Change. 2nd ed. New York, NY: The Guilford Press; 2002. [Google Scholar]
- 27.Borrelli B, Riekert K, Weinstein A, et al. Brief motivational interviewing as a clinical strategy to promote asthma medication adherence. J Allergy Clin Immunol. 2007; 120(5); 1023–1030. [DOI] [PubMed] [Google Scholar]
- 28.Mollen C, Lavelle J, Hawkins L, et al. Description of a novel pediatric emergency department-based HIV screening program for adolescents. AIDS Patient Care STDS. 2008; 22(6): 505–512. doi: 10.1089/apc.2007.0098 [DOI] [PubMed] [Google Scholar]
- 29.Goyal M, Zhao H, Mollen C. Exploring emergency contraception knowledge, prescription practices, and barriers to prescription for adolescents in the emergency department. Pediatrics. 2009; 123(3); 765–770. doi: 10.1542/peds.2008-0193 [DOI] [PubMed] [Google Scholar]
- 30.Haywood C Jr, Lanzkron S, Hughes MT, et al. A video-intervention to improve clinician attitudes toward patients with sickle cell disease: The results of a randomized experiment. Journal of general internal medicine. 2011; 26(5); 518–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anderson LA, Sharpe PA. Improving patient and provider communication: a synthesis and review of communication interventions. Patient Education and Counseling. 1991; 17(2), 99–134. [Google Scholar]
- 32.Tao GG. American journal of preventive medicine: Missed opportunities to assess sexually transmitted diseases in U.S. adults during routine medical checkups. Elsevier; 02/2000;18:109. [DOI] [PubMed] [Google Scholar]
- 33.Long T, Chaiyachati KH, Khan A, et al. Expanding health policy and advocacy education for graduate trainees. J Grad Med Educ. 2014; 6(3): 547–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Madsen TE, Riese A, Choo EK, et al. Effects of a web-based educational module on pediatric emergency medicine physicians’ knowledge, attitudes, and behaviors regarding youth violence. West J Emerg Med. 2014; 15(5): 615–622. doi: 10.5811/westjem.2014.4.21365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nollen NL, Hutcheson T, Carlson S, et al. Development and functionality of a handheld computer program to improve fruit and vegetable intake among low income youth. HealthEduc Res. 2013; 28(2): 249–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Pre-intervention survey
Post-intervention survey
educational intervention video
Condom distribution survey