Abstract
Children’s perceptions are important to understanding family environment in the bipolar disorder (BD) high-risk context. Our objectives were to empirically derive patterns of offspring- perceived family environment, and to test the association of family environment with maternal or paternal BD accounting for offspring BD and demographic characteristics. Participants aged 12– 21 years (266 offspring of a parent with BD, 175 offspring of a parent with no psychiatric history) were recruited in the US and Australia. We modeled family environment using latent profile analysis based on offspring reports on the Conflict Behavior Questionnaire, Family Adaptability and Cohesion Evaluation Scales, and Home Environment Interview for Children. Parent diagnoses were based on the Diagnostic Interview for Genetic Studies and offspring diagnoses were based on the Schedule for Affective Disorders and Schizophrenia for School- Aged Children. Latent class regression was used to test associations of diagnosis and family environment. Two-thirds of all offspring perceived well-functioning family environment, characterized by nurturance, flexibility, and low conflict. Two ‘conflict classes’ perceived family environments low in flexibility and cohesion, with substantial separation based on high conflict with the father (High Paternal Conflict), or very high conflict and rigidity and low warmth with the mother (High Maternal Conflict). Maternal BD was associated with offspring perceiving High Maternal Conflict (OR 2.8, p=0.025). Clinical care and psychosocial supports for mothers with BD should address family functioning, with attention to offspring perceptions of their wellbeing. More research is needed on the effect of paternal BD on offspring and family dynamics.
MeSH Key Words: Risk Factors, Father-Child Relations, Mother-Child Relations, Mood Disorders, Bipolar Disorder, latent profile analysis
The range of impairments associated with bipolar disorder (BD; American Psychiatric Association, 2013) may include difficulties in parenting and associated challenges to the family environment. Whereas a positive family environment provides for offspring emotional security, physical safety and wellbeing, social integration, and facilitation of self-regulation and independence – families characterized by conflict and aggression, and cold, unsupportive, neglectful relationships are considered especially risky to child and adolescent development (Basic Behavioral Science Task Force, 1996; Bowlby, 1951; Repetti et al., 2002). These characteristics may create or interact with preexisting vulnerabilities in offspring (such as genetic risk associated with offspring of BD parents; Craddock and Jones, 1999) to confer further increased risk for problems with emotional regulation, cognitive development, psychosocial functioning, and biological health (Johnson et al., 2013; Repetti et al., 2002).
Prospective studies of the family environment in families with at least one parent with BD and a comparison group have centered on nurturance, communication, and family system maintenance (e.g., organization, discipline, control, and flexibility). Parents’ perceptions of the family environment are reported much more commonly than children’s. There is a trend in the literature toward lower parent-reported family cohesion among BD parents compared to parents without psychiatric disorders (Ferreira et al., 2013; Park et al., 2015; Romero et al., 2005) and population controls (Chang et al., 2001), with some exceptions (Lau et al., 2018; Vance et al., 2008). While several groups have found BD parents to not differ on conflict or communication compared to parents with other psychiatric disorders (Du Rocher Schudlich et al., 2008; Tarullo et al., 1994; Weintraub, 1987) and no psychiatric disorders (Romero et al., 2005; Vance et al., 2008), others have found worse conflict or communication style reported by BD parents compared to parents with no psychiatric disorders (Barron et al., 2014; Ferreira et al., 2013; Park et al., 2015; Vance et al. 2008). Some BD parents rate their family system maintenance as not significantly different (Du Rocher Schudlich et al., 2008; Park et al., 2015; Petti et al., 2004; Romero et al., 2005; Weintraub, 1987), while others report significant differences in control, structure, or organization (Barron et al., 2014; Chang et al., 2001; Ellenbogen and Hodgins, 2009; Ferreira et al., 2013; Romero et al., 2005). With rare exception (Du Rocher Schudlich et al., 2008; Lau et al., 2018; Weintraub, 1987), these studies had samples involving fewer than 100 families, which may contribute to their contradictory findings; and all used a variable-centered approach.
In several high-risk studies using a case-control design, adolescent offspring of BD parents have reported their family environment as being not significantly different from controls (Doucette et al., 2013; Lau et al., 2018; Petti et al., 2004; Tarullo et al., 1994; Vance et al., 2008). In adolescents, investigators have found that observed levels of offspring engagement, critical/irritable behavior, and comfort/happiness were not associated with maternal diagnosis (Tarullo et al., 1994); offspring-reported expressiveness, conflict, cohesion, and parental negative communication style were not associated with parental BD (Lau et al., 2018; Vance et al., 2008); and offspring-perceived attachment, parental care, and parental overprotection—with father and mother rated separately—were not associated with parental BD (Doucette et al., 2013; Lau et al., 2018). Additionally, although discipline was not significantly associated with parental BD, parents (but not offspring) rated their family discipline levels as significantly higher in those families in which the youth were diagnosed with BD (Petti et al., 2004). In sum, while these findings underscore the importance of measuring multiple constructs of family environment, they do not point to a clear consensus regarding an essential ‘signature’ of the BD-high-risk family, and certainly not a unilaterally negative one, which suggests a need for a different approach in the search for potential modifiable targets of family functioning.
There are several key reasons to focus on offspring reports. Caregiver warmth and discipline influence offspring perceptions of caregiver behavior, and those perceptions, in turn, influence the impact of caregiving (Basic Behavioral Science Task Force, 1996), including psychological wellbeing. Offspring perceptions of the family climate are related to but not necessarily direct reflections of their lived experiences in the family and are largely influenced by the quality of the parent-child relationships, which may provide security for them and buffer them from stress (Cohen and Wills, 1985; Grych and Fincham, 1989). In the BD high-risk literature, offspring reports on the family environment are understudied compared to parent reports. Parents’ reports about their children may reflect their own health status, concerns, and life history, leading to over-endorsement or minimization of problems or disagreement between informants (Chilcoat and Breslau, 1997; Ringoot et al., 2015; Taber, 2010; Weissman et al., 1980). Parent perceptions may be less proximal to their offspring’s experiences than offspring perceptions of their own experiences. Additionally, children as young as 4 years of age can describe the mood and behavior of their parents with BD, with children 7 years of age and older having additional insight into how parents’ symptoms have affected them (Backer et al, 2017). Finally, while we expect that all HR offspring in the current study knew about parental diagnosis because ascertainment was in relation to parental BD, the topic of mental illness may not be actively discussed in all families, reinforcing the importance of understanding offspring perspectives directly. For these reasons, the present study focuses on offspring perceptions of their family environment.
Due to the heterogeneity of findings from case-control studies of the BD high-risk family environment, a relative neglect of offspring perspectives in these contexts, and the importance of addressing the multifaceted nature of family environment and its relation to mental health, we took a person-centered rather than variable-centered approach to modeling offspring-perceived family environment. Families with a parent with BD and families without parental mental illness experience a range of functioning and emotional climate, including both healthy and problematic family environments in each. This makes it important to consider characterizations of family environment that go beyond a case-control approach lumping together children based on their parent’s diagnostic status.
Using a large, international sample of offspring at high familial risk for BD and controls modeled together, we explored whether patterns in offspring-reported family environment would reflect unobserved subpopulations of families using latent profile analysis, enabling hypotheses on specific (and potentially modifiable) family environment impacts to be generated. Because variation in results across studies examining the effect of parental BD on family environment may be due to combining mothers and fathers, we modeled maternal and paternal BD separately. Additionally, because offspring mental health conditions are an important component to understanding family environment (Sameroff and Fiese, 2000; Schermerhorn and Cummings, 2008), we jointly modeled the effect of parental and offspring BD on family environment. Our objectives were to: 1) identify latent profiles of offspring-perceived family environment; and 2) test whether parental BD predicted membership in those family environments, accounting for offspring BD and sociodemographic characteristics.
Methods
Participants and Procedures
The current sample consisted of 441 offspring aged 12–21 years at their recruitment into a prospective study of adolescents at high familial risk for BD and controls (the Bipolar High-Risk Study). The primary study took place from 2006–2013 at urban academic medical centers in the United States (US) and Australia. Institutional Review Boards (US) or Human Research Ethics Committee (Australia) approved the study at all sites. Informed consent (or assent with parent consent for participants under age 18 in the US and 17 in Australia) was obtained from all participants. Participants were compensated for their participation, which was voluntary. Procedures are detailed elsewhere (Nurnberger et al., 2011; Perich et al., 2015).
Offspring at high-risk (HR) for familial BD were identified from probands with BD type I (BD-I), BD type II (BD-II), or schizoaffective disorder bipolar type (SAB) in the NIMH Genetics Initiative bipolar sample and other genetics studies (e.g., Fullerton et al., 2010; McAuley et al., 2009), and from specialty clinics and publicity. Control offspring were recruited via parents from general practitioners, motor vehicle records, and advertising, excluding families with a parent with major mood, psychotic, or substance use disorders; psychiatric hospitalizations; or a first-degree relative with a history of psychosis or hospitalization for a mood disorder. Parent psychiatric diagnoses, or lack thereof, were confirmed using the Diagnostic Interview for Genetic Studies (DIGS; Nurnberger et al., 1994). The current analysis included only offspring (n=441), although the primary study also included siblings and second- degree relatives of BD probands (Nurnberger et al., 2011; Perich et al., 2015). In some families, multiple offspring participated.
Family Environment Measurement Model
Family environment was measured at the first study visit, which took place at the research institutions. Details about identifiability, estimability, and psychometrics of the individual family environment measures are in the Supplement.
Family Adaptability and Cohesion Evaluation Scales (FACES II).
The FACES II is a 30-item self-report questionnaire that measures perceptions of family cohesion and adaptability (Olson et al., 1982). Cohesion refers to family emotional bonding and closeness, supportiveness, and time together (Kouneski, 2000). Adaptability refers to flexibility of the family. Sample items include, “Each family member has input regarding major family decisions” and “Family members are supportive of each other during difficult times.” Higher scores linearly represent healthy family functioning. The FACES II, which was designed for research, does not tap into enmeshed (overly high cohesion) or chaotic (overly high adaptability) extremes of these dimensions. Offspring reported on the family unit; data were complete for 88.4% of offspring.
Conflict Behavior Questionnaire (CBQ).
The CBQ is a 20-item self-report questionnaire that measures perceived parent-adolescent conflict (Robin and Foster, 1989). It captures dissatisfaction with the other family member’s behavior and conflicted interactions between family members (Prinz et al., 1979). Sample items include, “My father screams a lot” and “When I state my own opinion, my mother gets upset.” Higher scores indicate higher conflict. Offspring reported on conflict with their mother (86% complete data) and father (82% complete data) separately.
Home Environment Interview for Children (HEIC).
The HEIC is a semi-structured interview regarding the home and social environment, modeled after Robins’ Home Environment Interview (Reich et al., 1988, Robins et al., 1985) and designed to complement diagnostic interviews for youth (Reich and Earls, 1987). We conducted exploratory factor analysis (EFA) on question stems of substantive importance to parent-child relationships (see Supplement). After identifying a two-factor model based on 16 indicators, we extracted factor scores. Questions and item loadings on each of the two mother-child relationship factors are shown in Table S1. Factor 1, which we labeled “Warm Engagement,” includes items related to cohesion and positivity of maternal temperament. Factor 2, which we have labeled “Permissiveness,” captures elements of a laissez-faire approach to discipline, relatively low on corrections/restriction or critical behavior. Throughout, by “warm engagement” we mean “offspring-perceived maternal warm engagement” and by “permissiveness” we mean “offspring- perceived maternal permissiveness”.
Predictor Variables
Clinical Characteristics.
We tested parental BD, based on DIGS diagnosis, as a key predictor of family environment. Specifically, we looked at the effect of maternal BD and paternal BD separately. High-risk group status (i.e., offspring of BD parent versus control parent) was known for all participants; whether the BD parent was the mother (n=207) or father (n=52) was available for 98.4% of HR offspring.
Extensively trained raters interviewed offspring and parents separately using the Schedule for Affective Disorders and Schizophrenia for School-Aged Children, bipolar disorder version (K-SADS-BP; Nurnberger et al., 2011), which defines specific episodes in time and duration before assessing symptoms, and includes questions targeting each DSM-IV criterion with anchor points. The interview may be obtained from the authors. Lifetime DSM-IV disorders in offspring were confirmed by best estimate consensus of two clinicians using direct interviews of offspring and parents as well as medical history records. Best estimate consensus diagnoses were available for 91% of offspring. Our dichotomous variable for lifetime diagnosis of broad phenotype BD, using all available information, included BD-I, SAB, BD-II with recurrent depression, and BD not otherwise specified (BD-NOS). Inter-rater reliability (Kappa) for diagnosis of a major mood disorder was .82 among the US sites (Nurnberger et al., 2011). There was intensive, on-site training in the K-SADS from the lead US site when the Australian site was initiated, but formal inter-rater reliability studies were not conducted with the Australian site.
Sociodemographic Characteristics.
We adjusted for offspring age at interview, sex (Male or Female), race (binarized into White or non-White), and country of residence (US or Australia). No demographic data were missing. A previous analysis of US sites from this study examined occupation of the head of the household as a proxy for socioeconomic status and did not find a significant difference between HR and control groups (Nurnberger et al., 2011). Offspring reported on whether they lived with their biological mother (91% complete data) and father (78% complete data) at the time of the K-SADS interview, but did not report on custody arrangements (i.e., whether those parents are in the same household).
Statistical Analysis
Latent Class/Profile Analysis.
We used complex mixture modeling in Mplus version 7.4 (Muthén and Muthén, 1998–2012) to identify a person-centered model of offspring-perceived family environment. Specifically, we performed latent profile analysis, i.e., latent class analysis with continuous indicators, which is a special case of mixture modeling useful for measuring patterns in data from multiple observed variables called class indicators. Classes represent unobserved subpopulations of people, called latent because class membership is inferred from the data (Muthén and Muthén, 1998–2012). The classes explain covariance among class indicators while accounting for measurement error in constructs that are difficult to measure. We had 6 class indicators: family adaptability and family cohesion from the FACES II; conflict with Mother and conflict with Father from the CBQ; and factor scores on maternal warm engagement and permissiveness from the HEIC.
Class enumeration.
To determine the number of classes, we examined goodness-of-fit indices for 1–5 classes, including the Bayesian information criterion (BIC), entropy, Vuong-Lo- Mendell-Rubin likelihood ratio test, and Lo-Mendell-Rubin adjusted likelihood ratio test (LMR). We accounted for clustering of siblings within families, which corrected standard errors and the chi-square test of model fit. Latent models were estimated using full information maximum likelihood (FIML), which makes use of all available data to adjust parameter estimates in the presence of missing data using a likelihood function (Schafer and Graham, 2002). Thus, the family environment measurement model was estimated with the full sample of 441 offspring, without dropping cases due to missingness.
Latent Class Regression with Covariates.
We tested the association of observed covariates (maternal or paternal BD, offspring BD, and sociodemographic characteristics) in the structural model with the categorical latent classes in the measurement model to identify predictors of class membership (Muthén and Muthén, 1998–2012). The term predictor is not meant to infer causality. Maximum likelihood estimation was used, and modeling accounted for clustering of siblings within families. Fully adjusted models, run as multivariable regressions in which the association of each observed covariate with the latent classes was adjusted for the effect of all other covariates in the model, were based on a sample of 303 due to missingness on predictor covariates.
Sample statistics were calculated using Stata Version 14 (StataCorp, 2015), based on unadjusted chi-square tests and univariate regressions.
Results
Sample Characteristics
The sample consisted of 441 offspring: 266 HR and 175 controls (see Table 1 for sample characteristics). Although HR and control offspring did not differ significantly on age (mean 16.7, median 17, inter-quartile range 14–19 years), sex (51.5% male), or race (89% White), significantly more HR (34 of 266) than control (1 of 175) offspring themselves received a diagnosis of BD. A slightly higher proportion of HR offspring than controls reported their father as being part of their home environment; the proportions reporting living with their mother was not different by HR-status. Across the full sample, 227 of 441 (51.5%) offspring replied yes to living with mother and living with father, but the exact living conditions are unknown. For example, the adolescent might have been living with both the biological mother and father but in separate houses under a joint custody arrangement, or together in the same house. Frequencies of sociodemographic and clinical characteristics by class are shown in Table S2. Importantly, HR and control youth were distributed across all classes of family environment—described below—indicating there is not a single ‘signature’ BD family type; moreover, a large number of HR youth identified a healthy family environment (see Table S2).
Table 1.
Offspring demographic and clinical characteristics in the Bipolar High-Risk Study
| Total Sample (n=441) | High-Risk (n=266) |
Controls (n=175) |
p-value | |
|---|---|---|---|---|
| Age, mean years ± SD | 16.73 ± 2.85 | 16.59 ± 2.84 | 16.95 ± 2.87 | 0.115 |
| Sex, n (%) | 0.858 | |||
| Male | 227 (51.47) | 136 (51.13) | 91 (52.00) | |
| Female | 214 (48.53) | 130 (48.87) | 84 (48.00) | |
| Race, n (%) | 0.063 | |||
| White | 393 (89.12) | 243 (91.35) | 150 (85.71) | |
| Non-White | 48 (10.88) | 23 (8.65) | 25 (14.29) | |
| Country, n (%) | 0.830 | |||
| United States | 320 (72.56) | 194 (72.93) | 126 (72.00) | |
| Australia | 121 (27.44) | 72 (27.07) | 49 (28.00) | |
| Home environment, n (%) | ||||
| (n=402) | (n=243) | (n=159) | ||
| Living with Mother | 358 (81.18) | 218 (81.95) | 140 (80.00) | 0.602 |
| (n=346) | (n=203) | (n=143) | ||
| Living with Father | 244 (53.33) | 154 (57.89) | 90 (51.54) | 0.009 |
| n=402 | n=245 | n=157 | ||
| Offspring BD, n (%) | 35 (8.71) | 34 (13.88) | 1 (0.64) | <0.001 |
Note: BD, bipolar disorder; SD, standard deviation. Percentages are within column.
Family Environment Profiles
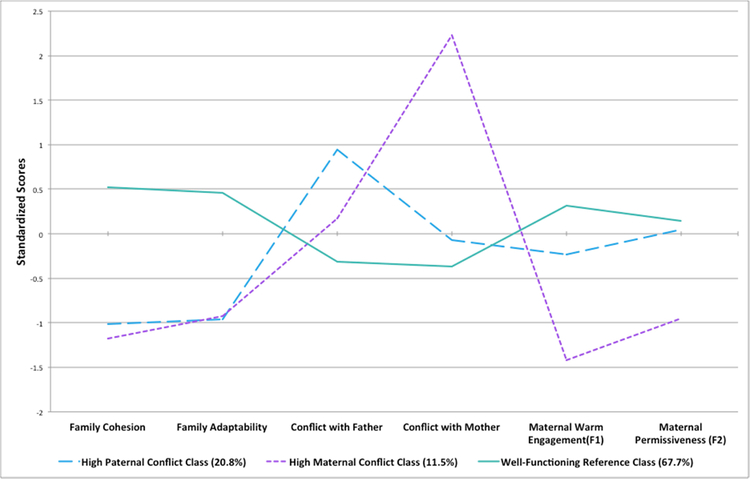
We found a three-class model best fitted the data based on the BIC (Figure S1) and LMR (Table 2) (Nylund et al., 2007). The three family environment profiles are displayed in Figure 1 using standardized scores (z-scores). Raw mean scores of the six indicators across the three profiles are in Table 3.
Table 2.
Class enumeration: offspring-perceived family environment fit indices
|
J classes |
# free parameters | Smallest Class n (%) |
LL | BIC | Entropy | VLMR p-value |
LMR adjusted p-value |
|---|---|---|---|---|---|---|---|
| 1 class | 12 | −6096.988 | 12267.045 | ||||
| 2 class | 19 | 66 (15) | −5843.097 | 11801.887 | 0.92 | 0.0000 | 0.0000 |
| 3 class | 26 | 50 (11) | −5733.552 | 11625.42 | 0.828 | 0.0038 | 0.0043 |
| 4 class | 33 | 37 (8) | −5679.846 | 11560.63 | 0.833 | 0.1516 | 0.1583 |
| 5 class | 40 | 22 (5) | −5641.866 | 11527.293 | 0.839 | 0.0561 | 0.0595 |
Note: BIC, Bayesian Information Criterion; LL, log likelihood; LMR, Lo-Mendell-Rubin adjusted likelihood ratio test; VLMR, Vuong-Lo-Mendell-Rubin likelihood ratio test
Figure 1.
Three profiles of offspring-perceived family environment
Table 3.
Raw scores for indicators across family environment classes
| Class Indicator | Class Mean Score (95% Confidence Interval) | ||
|---|---|---|---|
| High Paternal Conflict | High Maternal Conflict | Well-Functioning | |
| Family Cohesiona | 44.4 (40.7, 48.1) | 42.7 (39.3, 46.0) | 60.7 (59.4, 62.1) |
| Family Adaptabilitya | 35.3 (32.8, 37.9) | 35.7 (33.2, 38.1) | 47.6 (46.4, 48.9) |
| Conflict with Fatherb | 8.8 (6.1, 11.4) | 5.0 (3.2, 6.7) | 2.6 (1.9, 3.2) |
| Conflict with Motherb | 3.1 (2.3, 3.9) | 13.6 (12.2, 15.0) | 1.8 (1.3, 2.2) |
| Maternal Warm Engagementc | −0.27 (−0.46, −0.08) | −1.20 (−1.44, −0.95) | 0.16 (0.06, 0.25) |
| Maternal Permissivenessc | 0.01 (−0.18, 0.21) | −0.78 (−1.10, −0.47) | 0.09 (−0.001, 0.19) |
Note: Class enumeration conducted on full sample (N=441), with 20.8% (n=92), 11.5% (n=50), and 67. % (n=299) in the High Paternal Conflict, High Maternal Conflict, and Well-Functioning reference classes, respectively.
FACES-II subscale
CBQ subscale
HEIC factor score
The largest class of youth (67.7% of sample) perceived lower conflict with parents and higher cohesion, adaptability, maternal warm engagement, and permissiveness compared to two smaller classes. This reference class, which we labeled ‘well-functioning’ family environment, experienced their families as essentially nurturing, flexible, and low-conflict. The two smaller classes, in contrast, were characterized by significantly higher conflict and lower cohesion and adaptability than the reference class. We labeled the medium-sized class ‘High Paternal Conflict’ (20.8% of sample, roughly n=92) and the smallest class ‘High Maternal Conflict’ (11.5% of sample, roughly n=50).
Differences across the family environment profiles based on the contributing class indicators (CBQ, FACES subscales, and HEIC factor scores) are shown in Figure 1 and Table 3 and detailed below. On the CBQ, youth in the High Paternal Conflict class reported approximately 3 times higher mean conflict with their father than the reference class but did not significantly differ on paternal conflict from the High Maternal Conflict class. The High Maternal Conflict class reported conflict with their mothers that was, on average, over 4 times higher than the High Paternal Conflict class, and 7.5 times higher than the reference class, all significantly different. On the FACES, the High Conflict classes were not different from each other on cohesion and adaptability, but were both significantly lower than the reference class. On the HEIC, the well-functioning class reported higher-than-average maternal warm engagement, the High Paternal Conflict class reported lower-than-average warm engagement, and the High Maternal Conflict class reported a full standard deviation lower warm engagement than the High Paternal Conflict class. Youth in the High Maternal Conflict class reported significantly lower maternal permissiveness, indicating potential rigidity or criticism in the maternal-child relationship, compared to the High Paternal Conflict and reference classes. Thus, a distinguishing element in the conflict classes was the quality of the mother-child relationship.
Predictors of Family Environment
As shown in Table 4, maternal BD was significantly associated with increased likelihood of membership in the High Maternal Conflict class. Youth with a mother with BD were 2.83 times (95% CI 1.14–7.05; p=0.025) more likely to perceive a High Maternal Conflict family environment than a well-functioning one, adjusting for age, sex, race, country of residence, whether the offspring lived with either biological parent at the time of assessment, and offspring BD diagnosis. No other correlate was associated with family environment in fully adjusted models, which are presented in Table 4 (n=303).
Table 4.
Predictors of offspring-perceived family environment latent class membership
| High Paternal Conflict versus Well-Functioning Family Environment | High Maternal Conflict versus Well-Functioning Family Environment | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | Est. | SE | p | OR | Est. | SE | p | |
| Adjusted Models | ||||||||
| Age | 1.07 (0.94, 1.21) | 0.065 | 0.066 | 0.325 | 1.13 (0.97, 1.32) | 0.123 | 0.080 | 0.124 |
| Female | 0.97 (0.40, 2.39) | −0.030 | 0.459 | 0.949 | 1.91 (0.82, 4.43) | 0.646 | 0.429 | 0.131 |
| Non-White | 0.57 (0.10, 3.22) | −0.555 | 0.879 | 0.528 | 2.55 (0.74, 8.83) | 0.936 | 0.634 | 0.140 |
| Australia | 0.57 (0.21, 1.58) | −0.555 | 0.518 | 0.284 | 1.20 (0.42, 3.46) | 0.182 | 0.540 | 0.737 |
| Living with Mother | 0.42 (0.09, 1.92) | −0.875 | 0.779 | 0.261 | 1.64 (0.29, 9.20) | 0.492 | 0.881 | 0.576 |
| Living with Father | 0.81 (0.26, 2.52) | −0.210 | 0.578 | 0.717 | 0.49 (0.20, 1.22) | −0.710 | 0.463 | 0.126 |
| Maternal BD | 1.67 (0.69, 4.05) | 0.511 | 0.453 | 0.259 | 2.83 (1.14, 7.05) | 1.041 | 0.466 | 0.025 |
| Offspring BD | 1.22 (0.28, 5.29) | 0.200 | 0.748 | 0.789 | 1.61 (0.41, 6.37) | 0.474 | 0.703 | 0.500 |
| Age | 1.07 (0.93, 1.22) | 0.063 | 0.068 | 0.353 | 1.14 (0.97, 1.33) | 0.128 | 0.081 | 0.114 |
| Female | 0.96 (0.41, 2.28) | −0.037 | 0.439 | 0.934 | 1.91 (0.81, 4.51) | 0.647 | 0.439 | 0.140 |
| Non-White | 0.53 (0.08, 3.34) | −0.634 | 0.938 | 0.499 | 2.43 (0.64, 9.25) | 0.888 | 0.682 | 0.193 |
| Australia | 0.60 (0.23, 1.59) | −0.510 | 0.498 | 0.305 | 1.08 (0.32, 3.66) | 0.078 | 0.622 | 0.900 |
| Living with Mother | 0.48 (0.10, 2.20) | −0.739 | 0.779 | 0.343 | 1.61 (0.23, 11.25) | 0.473 | 0.994 | 0.634 |
| Living with Father | 0.82 (0.27, 2.48) | −0.200 | 0.565 | 0.723 | 0.56 (0.22, 1.46) | −0.573 | 0.484 | 0.236 |
| Paternal BD | 0.36 (0.07, 1.95) | −1.011 | 0.857 | 0.238 | 0.46 (0.08, 2.81) | −0.776 | 0.924 | 0.401 |
| Offspring BD | 1.53 (0.34, 6.87) | 0.424 | 0.767 | 0.580 | 2.40 (0.60, 9.57) | 0.877 | 0.705 | 0.213 |
Notes: BD, bipolar disorder; Est., effect estimate; OR, odds ratio; p, p-value; SE, standard error. Values in bold significant at p<0.05 level. In the two adjusted (i.e., multivariable regression) models, each covariate in model is adjusted for effect of all other covariates. Maternal BD and paternal BD, based on the sex of the proband parent, were tested separately. N=303 for the adjusted models.
Discussion
We found three profiles of family environment perceived by 441 youth with either a parent with BD or parents with no major psychiatric disorders, and found that maternal but not paternal BD was significantly associated with family environment. Specifically, we found one large class of youth with essentially ‘well-functioning’ family environment, characterized by nurturance, flexibility, and low conflict, and two smaller classes characterized by high conflict and low warmth and cohesion, with substantial separation based on either high conflict with the father (High Paternal Conflict) or very high conflict and rigidity with the mother (High Maternal Conflict). Maternal BD was significantly associated with High Maternal Conflict, adjusted for offspring BD and sociodemographic characteristics.
While maternal BD was significantly associated with increased risk of High Maternal Conflict over and above offspring BD, paternal BD was not associated with membership in the conflict classes. Indeed, though not statistically significant, paternal BD appeared to be protective rather than being associated with increased risk of conflicted environments. One possibility is that in the families in which the father has BD, at least for this generation, the mothers may have taken on a larger proportion of caregiving behaviors or provided additional support that buffers the offspring from stress associated with paternal BD. Additionally, mothers and fathers with BD may leave children’s daily lives at different thresholds of pathology. In the context of parental serious mental illness (SMI), it is not rare for offspring to live with a single mother with SMI, but it is rare for offspring to live with a single father with SMI (Ranning et al., 2016). The fathers with BD participating in our study may have less severity of illness than the mothers, or they may have been more engaged or motivated than average, as we observed a higher proportion of HR than control youth reporting their father being part of the home environment. In the event that mothers are the primary caregivers, there may be greater negative effect when the mother has BD. Finally, there were fewer BD fathers than BD mothers in our study. Any of these reasons or a combination thereof, or societal or biologic factors outside the scope of this study, could explain the different associations found between maternal and paternal BD in relation to family environment.
Other BD high-risk studies, using a variable-centered framework, have reported null associations between offspring-reported family environment and parent diagnostic group (Doucette et al., 2013; Lau et al., 2018; Petti et al., 2004; Tarullo et al., 1994; Vance et al., 2008). It is possible that taking a person-centered approach with empirically derived subgroups using several measures is more sensitive than comparing mean scores on individual measures with offspring grouped by parent diagnosis. It is also possible that testing the association of maternal and paternal BD separately allowed for uncovering the association of maternal BD with offspring-perceived family environment.
Offspring perceptions of their family environment may serve as a conduit of familial risk (Grych and Fincham, 1990), rather than risk being a direct corollary of parent diagnosis. Additionally, while family environment and parent-child relationships likely influence offspring psychopathology, the mental health status of adolescents may influence their perceptions of family environment and relationships. These bidirectional influences occur dynamically over time, in line with transactional theories of child development and family systems (Sameroff and Fiese, 2000; Schermerhorn and Cummings, 2008). Extended longitudinal studies of younger offspring of BD parents are needed to examine the premorbid impact of family environment on development of mood disorders, as well as to gain insight into course. It would be especially informative to study evolving parent-child relationships from childhood (see, e.g., Thorup et al., 2018), over the arc of adolescence, and past the peak years for mood disorder onset. In addition to longitudinal study of offspring, it would be salient to track the duration and timing of parental disorders in relation to offspring development, including periods of remission, metrics of severity, and other comorbidities known to affect family environment, such as substance misuse.
This study contributes to the literature on BD high-risk family environment in several ways. First, we focused on offspring reports, which are relatively understudied compared to parent reports, and thus offer considerable insight into the link between offspring perceptions and developmental outcomes. The offspring and parents in this study were well-phenotyped, and current, rather than retrospective, perceptions of family functioning were captured We included multiple covarying domains of family environment in our measurement model, taking a person- centered approach to capturing heterogeneity of experience without making a priori assumptions regarding environmental differences by splitting offspring into groups according to parent diagnosis. There is a robust literature on the importance of warmth, firmness, and psychological autonomy granting in the parent-child relationship (Steinberg, 2001), the children’s perceptions of which were captured, in addition to communication conflict and family dynamics. The adolescent offspring under study were old enough to provide information less susceptible to suggestion, confabulation, or response bias due to dichotomous thinking seen in younger children (Taber, 2010). Finally, we tested the effects of paternal and maternal BD separately.
Limitations
Offspring did not report directly on sibling relationships or the intraparental relationship, but did report on the family unit and parent-child relationships. Thus, it is possible that our family environment measurement model was mis-specified, although the domains covered by our measures reflect those identified as important in the extant literature. Our sample was mostly White, and a convenience/volunteer sample; however, demographic characteristics were not significantly different between HR and control groups, and our overall sample was large and international. The number of offspring diagnosed with BD was modest, though distributed across classes. Indeed, the mean age of offspring was just under the age of peak onset for BD, although in a nationally representative US sample, approximately 10% of BD cases report onset before age 13 and one-third before age 18 (Merikangas et al., 2007), with higher prevalence of early onset reported in clinical samples (Birmaher et al., 2009; Danner et al., 2009; Perlis et al., 2004). If additional offspring developed BD over time, the power to detect associations with family environment may increase. Importantly, different needs and observations concerning the home environment and parenting may be generated at different offspring ages (ranging from 12 to 21 years in current study) and these age-specific observational differences were not examined here due to limited power. Current symptomatology (Hammen et al., 1987), dimensional measures of psychiatric functioning, objective measures of attachment, other psychiatric disorders, genetics, and temperament and personality are important considerations when studying family dynamics, though these were not the focus of the present study. We note that the factor analysis used to quantify the HEIC was derived from the current dataset, and therefore the factors identified have not been independently validated. Lastly, our cross-sectional analysis means that we cannot deduce causality.
Implications and Conclusion
There does not appear to be one homogenous ‘signature’ of the BD high-risk family environment—high-risk and control youth were distributed across classes of family environment, and parental BD was not universally associated with negative family environment. Family environments associated with parental BD may differ depending on whether the mother or father has BD. Maternal BD was associated with higher odds of offspring perceiving a troubled mother-child relationship—i.e., higher conflict, lower cohesion and warm engagement, and lower flexibility/higher rigidity—but paternal BD was not. Though the group of offspring identifying a High Maternal Conflict environment was relatively small, our exploratory findings suggest that some mothers with BD may need additional psychosocial support, perhaps related to reducing conflictual communication style, increasing flexibility or responsive caregiving behaviors, or identifying and modifying other sources of strain on the family unit. Randomized controlled trials focused on improving family communication and dynamics may provide more definitive data on the impact of perceived conflict on development of offspring psychopathology. Additionally, psychosocial therapies (e.g., Goldstein et al., 2014; Miklowitz et al., 2011) may help offspring to understand context and contributing factors to their family environment and help them process it, in addition to offering potential for prevention of symptoms or their exacerbation and related sequelae within the family unit. Finally, further research is needed on the association of paternal BD and family environment. Parental engagement is fundamental to healthy youth development, but the health of the parent matters in the process. Thus, it is important to support parents not only in their own treatment and self-care, but also in linking them to parenting and family resources.
Supplementary Material
Acknowledgments
We wish to acknowledge and thank the families who participated in this project. We further acknowledge Carrie Fisher, Christine Brucksch, and Andrew Frankland for detailed data collection and quality assurance.
Funding:
This analysis was supported by the National Institute of Mental Health and Johns Hopkins Bloomberg School of Public Health [T32MH014592; PI: Peter P. Zandi], as part of the first author’s (EKS) doctoral dissertation. Additionally, EKS received support from the Intramural Research Program at the National Institute of Mental Health.
The primary study was funded by the National Institute of Mental Health [collaborative R01s MH68009 (PI: John Nurnberger), MH073151 (PI: Anne Glowinski), and MH068006 (PI: Melvin McInnis), with a subcontract to Johns Hopkins University]. Recruitment of the Australian cohort and genotyping of the entire 5-site sample was supported by the Australian National Health and Medical Research Council (Program Grant number 1037196, PI: Philip B. Mitchell and Project Grant 1066177, PI: Janice M. Fullerton) and the Lansdowne Foundation, with support from the Janette Mary O’Neil Research Fellowship (to JMF).
Role of the Funding Source:
The funding sources had no involvement in study design; collection, analysis, or interpretation of data; in writing of the report; and in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could appect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest:
John I. Nurnberger, MD has participated as investigator in research studies funded by Assurex and by Janssen. All other authors deny any potential conflicts of interest.
All authors have approved the final article.
References
- American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders, fifth ed. American Psychiatric Association, Arlington. [Google Scholar]
- Backer C, Murphy R, Fox JRE, Ulph F, Calam R, 2017. Young children’s experiences of living with a parent with bipolar disorder: Understanding the child’s perspective. Psychol Psychother, 90, 212–228. [DOI] [PubMed] [Google Scholar]
- Barron E, Sharma A, Le Couteur J, Rushton S, Close A, Kelly T, Grunze H, Ferrier IN Le Couteur A, 2014. Family environment of bipolar families: a UK study. J Affect Disord, 152–154, 522–525. [DOI] [PubMed] [Google Scholar]
- Basic Behavioral Science Task Force of the National Advisory Mental Health Council [NAMHC], 1996. Basic behavioral science research for mental health: Family processes and social networks. Am. Psychol 51, 622–630. [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Monk K, Kalas C, Goldstein B, Hickey MB, Obreja M, Ehmann MA, Iyengar S, Shamseddeen W, Kupfer D, Brent D, 2009. Lifetime psychiatric disorders in school-aged offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring study. Arch Gen Psychiatry, 66, 287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J, 1969. Attachment and Loss, Volume 1: Attachment. Basic Books, New York. [Google Scholar]
- Chang KD, Blasey C, Ketter TA, Steiner H, 2001. Family environment of children and adolescents with bipolar parents. Bipolar Disord. 3, 73–78. [DOI] [PubMed] [Google Scholar]
- Chilcoat HD and Breslau N, 1997. Does psychiatric history bias mothers’ reports? An application of a new analytic approach. J Am Acad Child Adolesc Psychiatry, 36, 971–979 [DOI] [PubMed] [Google Scholar]
- Cohen S and Wills TA, 1985. Stress, social support, and the buffering hypothesis. Psychol Bull, 98, 310–357. [PubMed] [Google Scholar]
- Craddock N and Jones I, 1999. Genetics of bipolar disorder. J Med Genet, 36, 585–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danner S, Fristad MA, Arnold LE, Youngstrom EA, Birmaher B, Horwitz SM,Demeter C, Findling RF, LAMS Group, 2009. Early-onset bipolar spectrum disorders: diagnostic issues. Clin Child Fam Psychol Rev,12, 271–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doucette S, Horrocks J, Grof P, Keown-Stoneman C, Duffy A, 2013. Attachment and temperament profiles among the offspring of a parent with bipolar disorder. J. Affect. Disord 150, 522–526. [DOI] [PubMed] [Google Scholar]
- Du Rocher Schudlich TD, Youngstrom EA, Calabrese JR, Findling RL, 2008. The role of family functioning in bipolar disorder in families. J. Abnorm. Child Psychol. 36, 849–863. [DOI] [PubMed] [Google Scholar]
- Ellenbogen MA and Hodgins S, 2009. Structure provided by parents in middle childhood predicts cortisol reactivity in adolescence among the offspring of parents with bipolar disorder and controls. Psychoneuroendocrinology. 34, 773–785. [DOI] [PubMed] [Google Scholar]
- Ferreira GS, Moreira CRL, Kleinman A, Nader ECGP, Gomes BC, Teixeira AMA,Rocca CCA, Nicoletti M, Soares JC, Busatto GF, Lafer B, Caetano SC, 2013. Dysfunctional family environment in affected versus unaffected offspring of parents with bipolar disorder. Aust. N. Z. J. Psychiatry 47, 1051–1057. [DOI] [PubMed] [Google Scholar]
- Fullerton JM, Donald JA, Mitchell PB, Schofield PR, 2010. Two-dimensional genome scan identifies multiple genetic interactions in bipolar affective disorder. Biol. Psychiatry 67, 478–486. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Fersch-Podrat R, Axelson DA, Gilbert A, Hlastala SA, Birmaher B, Frank E, 2014. Early intervention for adolescents at high risk for the development of bipolar disorder: Pilot study of Interpersonal and Social Rhythm Therapy (IPSRT). Psychotherapy. 51, 180–189. [DOI] [PubMed] [Google Scholar]
- Grych JH and Fincham FD, 1990. Marital conflict and children’s adjustment: a cognitive- contextual framework. Psychol. Bull 108, 267–290. [DOI] [PubMed] [Google Scholar]
- Hammen C, Adrian C, Gordon D, Burge D, Jaenicke C, Hiroto D, 1987. Children of depressed mothers: Maternal strain and symptom predictors of dysfunction. J. Abnorm. Psychol 96, 190–198. [DOI] [PubMed] [Google Scholar]
- Johnson SB, Riley AW, Granger DA, Riis J, 2013. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics. 131, 319–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouneski EF, 2000. The family circumplex model, FACES II, and FACES III: Overview of research and applications. University of Minnesota, St. Paul: Cited 2015 March 25. Available from: http://www.facesiv.com. [Google Scholar]
- Lau P, Hawes DJ, Hunt C, Frankland A, Roberts G, Wright A, Costa DSJ, Mitchell PB, 2018. Family environment and psychopathology in offspring of parents with bipolar disorder. J. Affect. Disord 226, 12–20. [DOI] [PubMed] [Google Scholar]
- McAuley EZ, Blair IP, Liu Z, Fullerton JM, Scimone A, Van Herten M, Evans MR, Kirkby KC, Donald JA, Mitchell PB, Schofield PR, 2009. A genome screen of 35 bipolar affective disorder pedigrees provides significant evidence for a susceptibility locus on chromosome 15q25–26. Mol. Psychiatry 14, 492–500. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M,Kessler RC, 2007. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry, 64, 543–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Chang KD, Taylor DO, George EL, Singh MK, Schneck CD,Dickinson LM, Howe ME, Garber J, 2011. Early psychosocial intervention for youth at risk for bipolar I or II disorder: A one-year treatment development trial. Bipolar Disord. 13, 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO, 1998–2012. Mplus User’s Guide, seventh ed. Muthén & Muthén, Los Angeles. [Google Scholar]
- Nurnberger JI Jr, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, Severe JB, Malaspina D, Reich T, 1994. Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH Genetics Initiative. Arch. Gen. Psychiatry 51, 849–59; discussion 863–4. [DOI] [PubMed] [Google Scholar]
- Nurnberger JI Jr, McInnis M, Reich W, Kastelic E, Wilcox HC, Glowinski A, Mitchell P, Fisher C, Erpe M, Gershon ES, Berrettini W, Laite G, Schweitzer R, Rhoadarmer K, Coleman VV, Cai X, Azzouz F, Liu H, Kamali M, Brucksch C, Monahan PO, 2011. A high-risk study of bipolar disorder. Childhood clinical phenotypes as precursors of major mood disorders. Arch. Gen. Psychiatry 68, 1012–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO, 2007. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Modeling, 14, 535–569. [Google Scholar]
- Olson DH, Bell RQ, Portner J, 1982. FACES II: Family Adaptability and Cohesion Evaluation Scales. Available from Life Innovations, Inc., P. O. Box 190, Minneapolis, MN 55440.
- Park MH, Chang KD, Hallmayer J, Howe ME, Kim E, Hong SC, Singh MK, 2015Preliminary study of anxiety symptoms, family dysfunction, and the brain-derived neurotrophic factor (BDNF) Val66Met genotype in offspring of parents with bipolar disorder. J Psychiatr Res, 61, 81–88. [DOI] [PubMed] [Google Scholar]
- Perich T, Lau P, Hadzi-Pavlovic D, Roberts G, Frankland A, Wright A, Green M,Breakspear M, Corry J, Radlinska B, McCormack C, Joslyn C, Levy F, Lenroot R, Nurnberger JIJ, Mitchell PB, 2015. What clinical features precede the onset of bipolar disorder? J. Psychiatr. Res 62, 71–77. [DOI] [PubMed] [Google Scholar]
- Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, Bowden CL, Sachs G, Nierenberg AA, STEP-BD Investigators, 2004. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry, 55, 875–881. [DOI] [PubMed] [Google Scholar]
- Petti T, Reich W, Todd RD, Joshi P, Galvin M, Reich T, DePaulo JR, Nurnberger J Jr., 2004. Psychosocial variables in children and teens of extended families identified through bipolar affective disorder probands. Bipolar Disord. 6, 106–114. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Foster S, Kent RN, O’Leary KD, 1979. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. J. Appl. Behav. Anal 12, 691–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranning A, Munk Laursen T, Thorup A, Hjorthøj C, Nordentoft M, 2016. Children of parents with serious mental illness: With whom do they grow up? A prospective, population-based study. J Am Acad Child Adolesc Psychiatry, 55, 953–961. [DOI] [PubMed] [Google Scholar]
- Reich W and Earls F, 1987. Rules for making psychiatric diagnoses in children on the basis of multiple sources of information: Preliminary strategies. J. Abnorm. Child Psychol 15, 601–606. [DOI] [PubMed] [Google Scholar]
- Reich W, Earls F, Powell J, 1988. A comparison of the home and social environments of children of alcoholic and non-alcoholic parents. Br. J. Addict 83, 831–839. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE, 2002. Risky families: family social environments and the mental and physical health of offspring. Psychol. Bull 128, 330–366. [PubMed] [Google Scholar]
- Ringoot AP, Tiemeier H, Jaddoe VW, So P, Hofman A, Verhulst FC, Jansen PW, 2015. Parental depression and child well-being: Young children’s self-reports helped addressing biases in parent reports. J Clin Epidemiol, 68, 928–938. [DOI] [PubMed] [Google Scholar]
- Robin AL and Foster SL, 1989. Negotiating parent-adolescent conflict: A behavioral-family systems approach. The Guilford Press, New York. [Google Scholar]
- Robins LN, Schoenberg SP, Holmes SJ, Ratcliff KS, Benham A, Works J, 1985. Early home environment and retrospective recall: a test for concordance between siblings with and without psychiatric disorders. Am. J. Orthopsychiatry 55, 27–41. [DOI] [PubMed] [Google Scholar]
- Romero S, DelBello MP, Soutullo CA, Stanford K, Strakowski SM, 2005. Family environment in families with versus families without parental bipolar disorder: A preliminary comparison study. Disord. 7, 617–622. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ and Fiese BH, 2000. Transactional regulation: The developmental ecology of early intervention, in: Shonkoff JP and Meisels SJ (Eds.), Handbook of Early Childhood Intervention, second ed. Cambridge University Press, New York, pp. 135–159. [Google Scholar]
- Schafer JL and Graham JW, 2002. Missing data: Our view of the state of the art. Psychol. Methods 7, 147–177. [PubMed] [Google Scholar]
- Schermerhorn AC and Cummings EM, 2008. Transactional family dynamics: a new framework for conceptualizing family influence processes. Adv. Child Dev. Behav 36, 187–250. [DOI] [PubMed] [Google Scholar]
- StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP [Google Scholar]
- Steinberg L, 2001. We know some things: Parent–adolescent relationships in retrospect and prospect. J. Res. Adolesc 11, 1–19. [Google Scholar]
- Taber SM, 2010. The veridicality of children’s reports of parenting: A review of factors contributing to parent–child discrepancies. Clin Psychol Rev, 30, 999–1010. [DOI] [PubMed] [Google Scholar]
- Tarullo LB, DeMulder EK, Martinez PE, Radke-Yarrow M, 1994. Dialogues with preadolescents and adolescents: mother-child interaction patterns in affectively ill and well dyads. J. Abnorm. Child Psychol. 22, 33–51. [DOI] [PubMed] [Google Scholar]
- Thorup AAE, Hemager N, Søndergaard A, Gregersen M, Prøsch ÅK, Krantz MF,Brandt JM, Carmichael L, Melau M, Ellersgaard DV, Burton BK, Greve AN, Uddin MJ, Ohland J, Nejad AB, Johnsen LK, Ver Loren van Themaat AH, Andreassen AK, Vedum L, Knudsen CB, Stadsgaard H, M Jepsen JR, Siebner HR, Østergaard L, Bliksted VF, Plessen KJ, Mors O, Nordentoft M, 2018. The Danish High Risk and Resilience Study-VIA 11: Study Protocol for the First Follow-Up of the VIA 7 Cohort −522 Children Born to Parents With Schizophrenia Spectrum Disorders or Bipolar Disorder and Controls Being Re-examined for the First Time at Age 11. Front Psychiatry, 9, 661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vance YH, Jones SH, Espie J, Tai S, Bentall R, 2008. Parental communication style and family relationships in children of bipolar parents. British Journal of Clinical Psychology. 47, 355–359. [DOI] [PubMed] [Google Scholar]
- Weintraub S, 1987. Risk factors in schizophrenia: the Stony Brook High-Risk Project. Schizophr. Bull 13, 439–450. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Orvaschel H, Padian N, 1980. Children’s symptom and social functioning self-report scales. Comparison of mothers’ and children’s reports. J Nerv Ment Dis, 168, 736–740. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.