Abstract
Objective:
Beliefs about illness have been shown to shape health practices and coping efforts. The present study investigated illness perceptions among patients undergoing hematopoietic stem cell transplant (HSCT). We also examined the extent to which perceptions predicted health practices and mental health following transplant.
Methods:
Participants (N=332) completed measures of illness perceptions (beliefs about cancer consequences and course, personal and treatment control over cancer, and understanding of one’s cancer) prior to HSCT. Health practices (diet, physical activity, alcohol use) and mental health (depression, anxiety, psychological well-being) were assessed pre-transplant and at 1, 3, 6, and 12 months post-transplant.
Results:
On average, HSCT recipients felt they understood their cancer, viewed their cancer to be a chronic condition with severe consequences, and believed they had moderate personal control over their cancer but that medical treatment provided more control. Perceptions varied by transplant type. Mixed-effects linear regression models revealed that HSCT recipients who perceived the consequences of their cancer to be more serious experienced more depression and anxiety, less well-being, and ate a healthier diet, but were less physically active during the year following transplant. Those with greater personal and treatment control ate a healthier diet and reported greater well-being. Patients with a better understanding of their cancer also ate a healthier diet and reported less depression, less anxiety, and greater well-being.
Conclusions:
Perceptions of cancer shape HSCT recipients’ health practices and psychological well-being during the critical first year of recovery after transplant.
Keywords: anxiety, cancer, depression, hematopoietic stem cell transplant, illness perceptions, oncology
Background
Leventhal’s self-regulation theory proposes that cognitive representations of illness influence behavioral responses and guide coping efforts. 1, Cognitive representations include beliefs about cause, severity of consequences, course (e.g, acute, chronic, recurrent), and ability to exert control over one’s illness. Indeed, illness perceptions have been shown to shape health practices and psychological adjustment for individuals with a variety of illnesses.2–5 A recent meta-analysis of 254 studies found support for the effect of illness perceptions on important outcomes, including distress, well-being, physical, role, and social functioning, and even disease states.6 In particular, greater perceived control was consistently related to functional and disease-related outcomes.
Illness perceptions have been well-studied in a number of cancer populations, including breast, gynecologic, prostate, colorectal, lung, hematologic, and head and neck cancers.2,7–12 Patients’ perceptions of cancer have been shown to predict health care utilization9, treatment adherence13, health practices including activity, diet, tobacco and alcohol use, cancer screening, and sun exposure12,14,15, and completion of advance directives.16 For example, breast cancer patients who perceived severe consequences of their cancer and those who attributed the cause of their cancer to health practices or stress reported more physical activity and reduced alcohol use and stress during the final phases of treatment.17 Illness representations, including perceptions of poor health status and serious consequences, have even been associated with increased mortality among individuals with cancer.8,18
A large body of work has also shown illness perceptions to be predictive of psychological distress and adjustment to cancer.19,20 For example, perceiving more severe consequences and seeing one’s disease as chronic are associated with greater distress21,22, depression5,23, anxiety24, and fear of recurrence.25 In contrast, having a better understanding of one’s disease and perceiving greater control over one’s cancer were linked to less distress and better social, emotional, and functional well-being.26
Few studies have examined illness perceptions among patients undergoing hematopoietic stem cell transplantation (HSCT). HSCT is an intensive treatment for hematologic cancers, including leukemia, lymphoma, and multiple myeloma. Patients receive their own previously harvested stem cells or a donor’s stem cells following high-dose chemotherapy. HSCT recipients frequently experience treatment complications, physical side effects, and psychological sequelae, which can persist long after transplant.28,29 HSCT is a particularly important population for understanding illness beliefs because of the high prevalence and persistence of psychological distress and influence of health practices on long-term recovery. Specifically, diet, physical activity, and substance use can exacerbate or alleviate side effects and complications30 and affect the likelihood of successful clinical outcomes.31,32
Among HSCT recipients, perceiving a greater sense of control and fewer consequences of one’s illness has been linked to better quality of life and less distress.33-36 In addition, patients who perceived they had a good understanding of their cancer experienced less depression and anxiety and better social, emotional, and functional well-being during the first 90 days post-HSCT.26 However, links to health practices have not been well-examined. Moreover, research has been limited by cross-sectional designs or brief follow-ups, and most studies focused on only one or two illness beliefs.
The present study had two primary aims. We first sought to characterize HSCT patients’ perceptions of their cancer using Leventhal’s framework, including beliefs about disease consequences, personal and treatment control over one’s disease, understanding one’s disease, and disease course. We also conducted an exploratory examination of differences in perceptions between allogeneic and autologous transplant recipients. Allogeneic and autologous transplants differ with respect to indications, risks, side effects, and recovery time, and therefore illness perceptions may differ.. The second aim was to investigate relationships between pre-transplant illness perceptions and health practices (diet, physical activity, alcohol and tobacco use) and mental health (depression, anxiety, psychological well-being) at key milestones during the year following transplant. We took advantage of the study’s prospective, longitudinal design to better understand how patients’ perceptions of their cancer may impact health practices and psychological adjustment after HSCT. Based on existing literature, we hypothesized that a better understanding of one’s cancer and perceiving less severe consequences, a more acute disease course, and greater control over one’s cancer would be associated with better health practices and mental health outcomes.
Method
Participants
Participants were 332 adults receiving HSCT at the University of Wisconsin Carbone Cancer Center who were enrolled in a larger study examining psychological factors and recovery following HSCT. Approximately 80% of patients approached agreed to participate. Common reasons for declining included not having enough time and feeling overwhelmed or too unwell. Data from participants who completed the pre-transplant assessment and at least one follow-up were included in analyses. Study attrition and missing data resulted in fewer patients at the 1 (95.2%), 3 (86.8%), 6 (77.7%), and 12 (67.8%) month assessments. Reasons for attrition included death (n=36) and drop out (n=4). Participants were an average of 53 years of age (range=19 to 74). Other demographic and medical characteristics are summarized in Table 1.
Table 1.
Patient Characteristics (N=332)
| Characteristics | % | n |
|---|---|---|
| Sex | ||
| Men | 61.1 | 203 |
| Women | 38.9 | 129 |
| Ethnicity | ||
| Caucasian | 96.1 | 318 |
| Native American | 1.2 | 4 |
| African American | 1.5 | 5 |
| Latino/Hispanic | 0.6 | 2 |
| Unknown | 0.6 | 3 |
| Relationship Status | ||
| Married/Partnered | 84.6 | 281 |
| Single | 7.2 | 24 |
| Divorced/Separated | 6.4 | 21 |
| Widowed | 1.8 | 6 |
| Education | ||
| <12 years | 3.6 | 12 |
| High School | 27.2 | 90 |
| Some College/Trade School | 28.7 | 95 |
| College | 23.9 | 79 |
| Post-Graduate | 16.6 | 55 |
| Unknown | 0.0 | 1 |
| Employment | ||
| Employed Full/Part-time | 43.1 | 143 |
| Disabled | 28.6 | 95 |
| Retired | 22.6 | 75 |
| Homemaker | 3.6 | 12 |
| Student | 0.3 | 1 |
| Unknown | 1.8 | 6 |
| Income | ||
| <25,000 | 11.8 | 39 |
| 25,001–55,000 | 28.6 | 95 |
| 55,001–85,000 | 27.1 | 90 |
| >85,000 | 27.4 | 91 |
| Unknown | 5.1 | 17 |
| Graft Type | ||
| Autologous | 58.1 | 193 |
| Allogeneic | 41.9 | 139 |
| Myeloablative | 26.5 | 88 |
| Sibling Donor | 12.7 | 42 |
| Unrelated Donor | 13.9 | 46 |
| Nonmyeloablative | 15.4 | 51 |
| Sibling Donor | 6.6 | 22 |
| Unrelated Donor | 8.7 | 29 |
| Diagnosis | ||
| Leukemias | 33.7 | 111 |
| MDS | 20.7 | 23 |
| AML | 47.8 | 53 |
| ALL | 19.8 | 22 |
| CML | 3.6 | 4 |
| CLL | 7.2 | 8 |
| Lymphomas | 33.4 | 110 |
| Hodgkin | 20.0 | 20 |
| Non-Hodgkin | 80.0 | 88 |
| Multiple Myeloma | 32.5 | 108 |
Procedures
The study received IRB approval (H-2007–0020). Participants provided informed consent and completed self-report measures assessing illness perceptions, mental health, and health practices pre-transplant and 1, 3, 6, and 12 months post-transplant in clinic or at home. Participants who did not return questionnaires promptly received reminder calls.
Measures
Illness perceptions.
Participants completed the Illness Perceptions Questionnaire-Revised (IPQ-R) prior to transplant. This instrument assesses beliefs about cancer course, cancer consequences, personal and treatment control over cancer, and understanding one’s cancer (coherence).37 Beliefs are rated on a scale from 1(strongly disagree) to 5(strongly agree). High scores on cancer course and consequences are indicative of strongly held beliefs about a chronic, long-term course and more significant negative consequences of cancer. High scores on personal control, treatment control, and understanding one’s cancer represent strongly held beliefs about a high level of controllability of cancer and a clearer understanding of one’s illness. Reliability in the present study was generally good (α=.63-.90).
Mental health.
Participants completed the 64-item Inventory of Depression and Anxiety Symptoms (IDAS) at each assessment point. This questionnaire assesses symptoms of depression and anxiety as well as psychological well-being.38 We focused on the dysphoria (cognitive and affective depressive symptoms), panic (somatic anxiety symptoms), and psychological well-being scales. Scales demonstrated good reliability in our sample (α=.85-.90).
Health practices.
Participants reported health practices at each assessment point. Participants estimated daily servings of fruits and vegetables (diet), number of alcoholic beverages consumed per week (alcohol use), whether they smoke tobacco products and packs per week (tobacco use), and amount of time engaged in moderate and vigorous physical activities. Scores for physical activity were calculated by multiplying the number of hours of weekly activity by estimates of relative energy expenditure for moderate and vigorous activities.39 These questions have been used successfully in prior studies with similar populations.12,17 Tobacco use was not included in subsequent analyses due to the low base rate of use in this sample.
Statistical analyses
STATA statistical package was used to analyze data. Two-sided tests were employed and results considered significant at p<0.05. Participants’ scores on illness perceptions scales were summarized with descriptive statistics (see Table 1). Differences in perceptions between allogeneic and autologous transplant recipients were examined. We also compared perceptions between those who had transplants with intent for cure versus delaying disease progression.
Mixed-effects linear regression models assessed whether each pre-transplant illness perception predicted each health practices and mental health outcome, as well as trajectories of these outcomes, through 12 months post-transplant. Type of transplant (allogeneic or autologous) was selected as a covariate a priori given different risks, side effect profiles, and recovery timelines. Other demographic and medical variables were evaluated for inclusion in the models based on relationships with illness perceptions. Illness perceptions differed by diagnostic category, F values=4.03–94.06, p values<0.05, sex (women reported poorer understanding of their cancer, t=4.97, p<0.001, and less personal and treatment control, t=3.16, p<0.001; t=3.30, p<0.001), and age (older participants were more likely to view their illness as a chronic condition, r=0.33, p<0.001). Therefore, diagnosis, sex, and age were included as covariates in all models.
Mixed-effects linear regression models were run with the ‘xtmixed’ routine in STATA. Separate models were run for each IPQ-outcome pair. All models included time since transplant as a categorical variable and transplant type, sex, age, and diagnosis as covariates. Models were estimated using full information maximum likelihood estimation and unstructured covariance matrices. Initial models estimated both main effects and illness perception by time interactions. Interaction terms that were not significant were removed from the models. Time-varying health practices and psychological outcomes were standardized based on 12-month post-transplant means and standard deviations before being entered into models to improve coefficient interpretability. Coefficients for main effects therefore represent the change in standard deviation units of the outcome measure for each 1-point increase in the illness perception score.
Results
Pre-Transplant Illness Perceptions
On average, HSCT recipients believed they understood their cancer (M=3.86, SD=.75), viewed their cancer as a more chronic than acute condition (M=3.29, SD=.95), perceived their cancer to have severe consequences (M=3.99, SD=.57), and believed they had moderate personal control over their cancer (M=3.61, SD=.71) and that treatment could control their cancer (M=3.99, SD=.55). Figure 1 illustrates participants’ perceptions for both autologous and allogeneic transplant recipients. Allogeneic transplant recipients perceived greater treatment control (t=4.94, p<0.001) and were less likely to view their illness as a chronic condition (t=−5.14, p<0.001). The same pattern was observed for patients whose transplants were performed with curative intent versus for the purpose of delaying disease progression. Patients receiving a transplant with curative intent perceived greater treatment control (t=5.55, p<0.001) and were less likely to view their illness as a chronic condition (t=−7.97, p<0.001).
Figure 1.
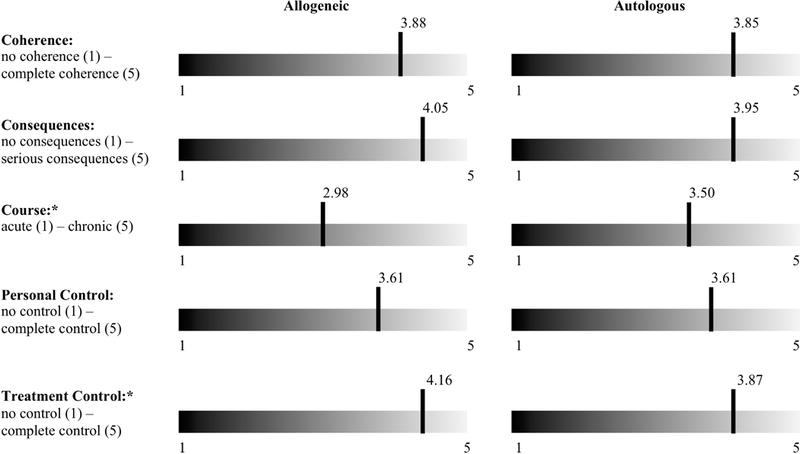
Pre-transplant mean illness perception dimension scores depicted for autologous and allogeneic transplant recipients. Significant differences (p<.05) in illness perceptions by transplant type are indicated with asterisks.
Descriptive statistics for health practices and mental health outcomes are shown in Supplemental Table 1.
Illness Perceptions Predict Health Practices and Mental Health
Table 2 depicts results of mixed-effects regression models examining the main effect of each illness perception measure and its interaction with time on each health practice and mental health outcome over the five assessments.
Table 2.
Illness Perceptions Predicting Health Practices and Mental Health
| Predictors | Diet | Physical Activity | Alcohol Use | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coef | z | p | Coef | z | p | Coef | z | p | ||
| Coherence | Main Effect | .19 | 3.20 | .001 | −.00 | −0.12 | .908 | −.00 | −0.10 | .917 |
| Interaction | .27 | 2.58 | .010 | |||||||
| Consequences | Main Effect | .17 | 2.18 | .029 | −.12 | −2.46 | .014 | .03 | 0.64 | .520 |
| Interaction | .24 | 2.38 | .017 | |||||||
| Course | Main Effect | −.01 | −0.12 | .905 | −.06 | −1.72 | .085 | −.04 | −0.99 | .324 |
| Interaction | .28 | 2.36 | .018 | |||||||
| Personal Control | Main Effect | .12 | 2.00 | .045 | −.00 | −0.09 | .929 | −.08 | −1.75 | .080 |
| Interaction | .24 | 2.21 | .027 | |||||||
| Treatment Control | Main Effect | .19 | 2.24 | .025 | .09 | 1.56 | .118 | −.01 | −0.13 | .895 |
| Interaction | .21 | 2.09 | .037 | |||||||
| Predictors | Anxiety | Depression | Well-being | |||||||
| Coef | z | p | Coef | z | p | Coef | z | p | ||
| Coherence | Main Effect | −.17 | −3.13 | .002 | −.24 | −3.96 | .000 | .31 | 5.26 | .000 |
| Interaction | ||||||||||
| Consequences | Main Effect | .22 | 3.07 | .002 | .41 | 5.39 | .000 | −.27 | −3.52 | .000 |
| Interaction | ||||||||||
| Course | Main Effect | .05 | 0.99 | .322 | .15 | 2.77 | .006 | −.11 | −2.01 | .045 |
| Interaction | ||||||||||
| Personal Control | Main Effect | −.03 | −0.55 | .585 | −.07 | −1.09 | .277 | .17 | 2.71 | .007 |
| Interaction | ||||||||||
| Treatment Control | Main Effect | −.23 | −3.00 | .003 | −.43 | −5.01 | .000 | .54 | 6.53 | .000 |
| Interaction | ||||||||||
Note. Separate models were run for each illness perception-outcome pair. All models covaried for time since transplant, transplant type, diagnosis, sex, and centered age. Health practices and psychological outcomes were standardized. Coefficients for main effects therefore represent the change in standard deviation units of the outcome measure for each 1-point increase in the illness perception score. Models were run with the main effect and interaction terms included in the model. Interaction terms that were not significant were removed from the model and main effects were reported without the non-significant interaction term.
With regard to health practice outcomes, participants who reported having a better understanding of their cancer, a greater sense of personal control over their cancer, and believed treatment could control their cancer were more likely to report eating a healthy diet. Those who perceived the consequences of the cancer to be more serious also reported eating a healthier diet but also reported less physical activity. Beliefs about illness course or chronicity were not related to health practices.
There were no significant interactions between illness perceptions and diet or physical activity, suggesting that pre-transplant perceptions did not predict changes over time in these health practices. However, there were significant interactions between each illness perception and time in models predicting alcohol use, with larger effects of illness perceptions on alcohol use at the later time points. An examination of plots of alcohol use by illness perception (see Figure 2) showed that patients reporting low personal control, those who perceived more severe consequences, and those who believed their cancer was more chronic reported greater alcohol use at 6 and 12 months post-transplant but not earlier. Those who reported having a poorer understanding of their cancer reported more alcohol use at 3 months post-transplant. Participants who perceived low treatment control reported greater alcohol use primarily between 3 and 6 months post-transplant and looked similar to those who perceived better treatment control by the 12-month follow-up.
Figure 2.
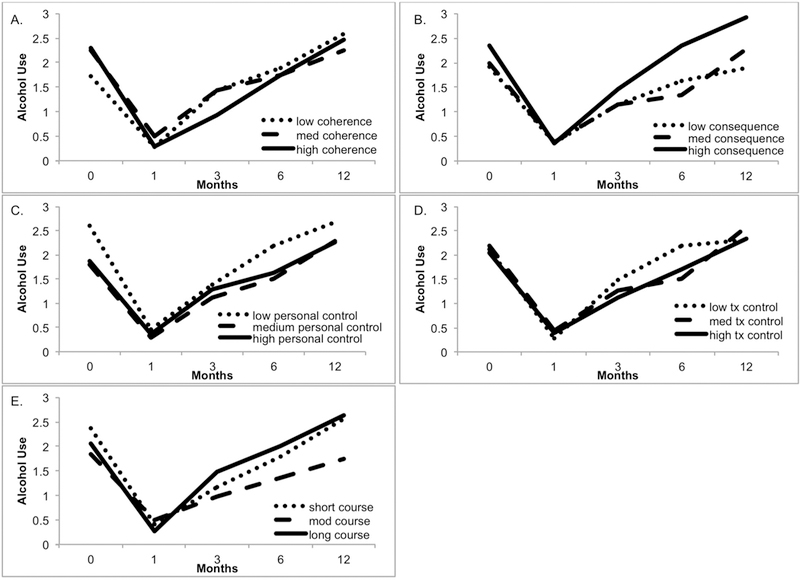
Changes over time in mean alcohol use (drinks/week) for participants in upper, middle, and lower tertiles on illness perception dimension scores are depicted here to illustrate significant interactions between illness perception dimensions and time. All models depicted had significant interactions, with larger effects of illness perceptions on alcohol use at the later time points.
With regard to mental health outcomes, participants with a greater understanding of their cancer reported less depression, less anxiety, and greater psychological well-being across the assessment points. Similarly, those who perceived the consequences of the cancer to be less severe and those with stronger beliefs that treatment could control their cancer reported less depression, less anxiety, and greater psychological well-being. Patients with a greater sense of personal control reported greater psychological well-being. Finally, those who viewed their cancers as chronic reported greater depression and less psychological well-being.
An examination of the interaction of illness perceptions and time indicated that none of the illness perceptions predicted trajectories of mental health measures over time.
Discussion
Findings suggest that HSCT recipients’ beliefs about their cancer prior to transplant may influence health practices and mental health during the year following transplant. HSCT recipients reported that they understood their illness, perceived serious consequences, and viewed their cancer as a more chronic than acute condition. Direct comparisons of the magnitude of this association with findings of previous studies are difficult due to variability in measures and illness perceptions assessed and reported. In the present study, patients believed they had a moderate amount of personal control over their illness but believed the treatment had greater control. This is consistent with findings from Frick et al (2007) who reported that some patients attributed control over their illness to their clinical providers.36
We also found differences between autologous and allogeneic HSCT recipients and transplants performed with and without curative intent. Patients who received an autologous HSCT and those who received a transplant for the purpose of delaying disease progression perceived their cancer to be a more chronic condition and perceived less treatment control. This finding is consistent with the typically more chronic course of diseases treated with autologous transplant. These patients are also more likely to have had multiple failed treatment regimens, which may explain lower confidence in ability of the treatment to control disease. There were no differences between autologous and allogeneic HSCT recipients or transplants performed with or without curative intent in understanding of illness, perception of serious consequences, or beliefs about personal control over cancer. Our study is one of few to have investigated HSCT recipients’ illness perceptions, and is the first to compare perceptions by type of transplant and curative intent.
Illness perceptions measured pre-transplant were robustly predictive of mental health during the post-transplant recovery, and the effects were relatively consistent across the assessment points. Having a greater understanding of one’s cancer, perceiving less severe consequences, perceiving cancer as a more acute condition, and believing that oneself or treatment can control cancer predicted fewer psychological symptoms and better psychological well-being during the post-transplant recovery. These prospective, longitudinal findings extend prior cross-sectional research linking illness perceptions to psychological outcomes among HSCT recipients26,35,36 to show that perceptions measured prior to transplant predict psychological outcomes both acutely and during later recovery.
The current study is among the first to evaluate links between illness perceptions and health practices in the context of HSCT. Findings were most robust for healthy eating post-transplant. Specifically, participants who endorsed a better understanding of their cancer, believed their cancer had serious consequences, and perceived a greater sense of personal and treatment control over their cancer reported eating a healthier diet across the year-long follow-up. This pattern of results is consistent with previous literature exploring links between cancer perceptions and healthy eating12,40 and suggests that this profile of illness beliefs may motivate positive health behavior change following transplant. In contrast, illness perceptions assessed in the current study did not predict physical activity. During early post-transplant recovery, physical activity may be more reflective of treatment complications or fatigue, with illness perceptions less salient. It may be more feasible for HSCT patients to make good dietary choices than to engage in moderate or vigorous physical activity.
The predictive capability of illness perceptions varied over time for alcohol use, with the strongest effects occurring during later recovery. Participants who endorsed a poorer understanding of their cancer, perceived more severe consequences, perceived low personal and treatment control, and perceived cancer course to be very acute or chronic, as opposed to a more moderate course, reported higher alcohol consumption. Our data indicate that most participants entirely avoided or had very limited amounts of alcohol during the early pre-transplant recovery, likely due to treatment side effects, extended hospitalization, and contraindication with medications. It may be that effects of illness perceptions are not seen until participants return to their more typical levels of alcohol consumption later in post-transplant recovery.
Clinical Implications
In sum, our findings suggest that some beliefs appear to be adaptive for both positive health practices and more optimal mental health, including perceiving greater personal and treatment control over one’s cancer and endorsing a good understanding of one’s disease. The belief that one’s cancer has severe consequences was associated with healthier eating but also with poorer mental health outcomes and greater alcohol consumption during later recovery. Similarly, believing one’s cancer is a chronic condition was associated with better health practices but poorer mental health and greater alcohol consumption. It may be that distress associated with these perceptions can motivate positive health practices. These findings also support a complex clinical picture in which the strength and direction of the illness perception is dependent on the outcome assessed. Moreover, effects for alcohol use appear to track more closely with mental health outcomes rather than other health practices.
Study Limitations
There were several limitations of the current study. We were unable to investigate tobacco use, an important cancer-relevant health practice, due to the low base rate in the sample. In addition, our sample was relatively homogenous with respect to racial and ethnic diversity, limiting our ability to generalize to non-White groups. It is also important to note that this is an observational study, and causality cannot be definitively established. We were, however, able to take advantage of the prospective, longitudinal design to begin to tease apart the temporal dynamics of relationships between illness perceptions, measured prior to transplant, and psychological and health practice outcomes across several post-transplant time points.
In sum, findings suggest that HSCT recipients’ pre-transplant beliefs about their cancer are important in shaping some health practices post-transplant. Thus, it is likely an important time for health care providers to discuss patients’ perceptions of their disease and prognosis. The findings further lay the groundwork for developing and testing an intervention to determine whether changing patient perceptions can improve post-transplant health practices or mental health outcomes.
Supplementary Material
Acknowledgements
This work was supported by Grants R21 CA133343 and K07 CA136966 to E. Costanzo from the NCI, KL2 RR0205012 to E. Costanzo and UL1RR025011 from the Clinical and Translational Science Award program of the National Center for Research Resources, an award from the Forward Lymphoma Foundation to E. Costanzo, and P30 CA014520 to the UW Carbone Cancer Center from the NCI.
Footnotes
Conflict of Interest Statement
The authors have no conflicts to disclose.
References
- 1.Leventhal H, Diefenbach M, & Leventhal EA (1992). Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cognitive Therapy and Research, 16(2), 143–163. 10.1007/BF01173486 [DOI] [Google Scholar]
- 2.Scharloo M, Baatenburg de Jong R. J., Langeveld TPM, van Velzen-Verkaik E, Doorn-Op den Akker MM, & Kaptein AA (2010). Illness cognitions in head and neck squamous cell carcinoma: predicting quality of life outcome. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer, 18(9), 1137–1145. 10.1007/s00520-009-0728-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rozema H, Völlink T, & Lechner L (2009). The role of illness representations in coping and health of patients treated for breast cancer. Psycho-Oncology, 18(8), 849–857. 10.1002/pon.1488 [DOI] [PubMed] [Google Scholar]
- 4.Knibb RC, & Horton SL (2008). Can illness perceptions and coping predict psychological distress amongst allergy sufferers? British Journal of Health Psychology, 13(Pt 1), 103–119. 10.1348/135910706X173278 [DOI] [PubMed] [Google Scholar]
- 5.Llewellyn CD, McGurk M, & Weinman J (2007). Illness and treatment beliefs in head and neck cancer: is Leventhal’s common sense model a useful framework for determining changes in outcomes over time? Journal of Psychosomatic Research, 63(1), 17–26. 10.1016/j.jpsychores.2007.01.013 [DOI] [PubMed] [Google Scholar]
- 6.Hagger MS, Koch S, Chatzisarantis NLD, & Orbell S (2017). The common sense model of self-regulation: Meta-analysis and test of a process model. Psychological Bulletin, 143(11), 1117–1154. 10.1037/bul0000118 [DOI] [PubMed] [Google Scholar]
- 7.Andersen MR, Afdem K, Hager S, Gaul M, Sweet E, & Standish LJ (2017). The “cause” of my cancer, beliefs about cause among breast cancer patients and survivors who do and do not seek IO care. Psycho-Oncology, 26(2), 248–254. 10.1002/pon.4028 [DOI] [PubMed] [Google Scholar]
- 8.Greer JA, Pirl WF, Jackson VA, Muzikansky A, Lennes IT, Gallagher ER, … Temel JS (2014). Perceptions of health status and survival in patients with metastatic lung cancer. Journal of Pain and Symptom Management, 48(4), 548–557. 10.1016/j.jpainsymman.2013.10.016 [DOI] [PubMed] [Google Scholar]
- 9.Mols F, Lemmens V, Bosscha K, van den Broek W, & Thong MSY (2014). Living with the physical and mental consequences of an ostomy: a study among 1–10-year rectal cancer survivors from the population-based PROFILES registry. Psycho-Oncology, 23(9), 998–1004. 10.1002/pon.3517 [DOI] [PubMed] [Google Scholar]
- 10.Husson O, Thong MSY, Mols F, Oerlemans S, Kaptein AA, & van de Poll-Franse LV (2013). Illness perceptions in cancer survivors: what is the role of information provision? Psycho-Oncology, 22(3), 490–498. 10.1002/pon.3042 [DOI] [PubMed] [Google Scholar]
- 11.Traeger L, Penedo FJ, Benedict C, Dahn JR, Lechner SC, Schneiderman N, & Antoni MH (2013). Identifying how and for whom cognitive-behavioral stress management improves emotional well-being among recent prostate cancer survivors. Psycho-Oncology, 22(2), 250–259. 10.1002/pon.2074 [DOI] [PubMed] [Google Scholar]
- 12.Costanzo ES, Lutgendorf SK, Bradley SL, Rose SL, & Anderson B (2005). Cancer attributions, distress, and health practices among gynecologic cancer survivors. Psychosomatic Medicine, 67(6), 972–980. 10.1097/01.psy.0000188402.95398.c0 [DOI] [PubMed] [Google Scholar]
- 13.Iskandarsyah A, de Klerk C, Suardi DR, Soemitro MP, Sadarjoen SS, & Passchier J (2014). Psychosocial and cultural reasons for delay in seeking help and nonadherence to treatment in Indonesian women with breast cancer: a qualitative study. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 33(3), 214–221. 10.1037/a0031060 [DOI] [PubMed] [Google Scholar]
- 14.van Broekhoven MECL, de Rooij BH, Pijnenborg JMA, Vos MC, Boll D, Kruitwagen RFPM, … Ezendam NPM (2017). Illness perceptions and changes in lifestyle following a gynecological cancer diagnosis: A longitudinal analysis. Gynecologic Oncology, 145(2), 310–318. 10.1016/j.ygyno.2017.02.037 [DOI] [PubMed] [Google Scholar]
- 15.Zivković MV, Dediol I, Ljubičić I, & Situm M (2012). Sun behaviour patterns and perception of illness among melanoma patients. Journal of the European Academy of Dermatology and Venereology: JEADV, 26(6), 724–729. 10.1111/j.1468-3083.2011.04154.x [DOI] [PubMed] [Google Scholar]
- 16.Croom AR, Hamann HA, Kehoe SM, Paulk E, & Wiebe DJ (2013). Illness perceptions matter: understanding quality of life and advanced illness behaviors in female patients with late-stage cancer. The Journal of Supportive Oncology, 11(4), 165–173. 10.12788/j.suponc.0014 [DOI] [PubMed] [Google Scholar]
- 17.Costanzo ES, Lutgendorf SK, & Roeder SL (2011). Common-sense beliefs about cancer and health practices among women completing treatment for breast cancer. Psycho-Oncology, 20(1), 53–61. 10.1002/pon.1707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thong MSY, Kaptein AA, Vissers PAJ, Vreugdenhil G, & van de Poll-Franse LV (2016). Illness perceptions are associated with mortality among 1552 colorectal cancer survivors: a study from the population-based PROFILES registry. Journal of Cancer Survivorship: Research and Practice, 10(5), 898–905. 10.1007/s11764-016-0536-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wiener CH, Cassisi JE, Paulson D, Husson O, & Gupta RA (2017). Information support, illness perceptions, and distress in survivors of differentiated thyroid cancer. Journal of Health Psychology, 1359105317692143. 10.1177/1359105317692143 [DOI] [PubMed] [Google Scholar]
- 20.Dempster M, McCorry NK, Brennan E, Donnelly M, Murray L, & Johnston BT (2012). Psychological distress among survivors of esophageal cancer: the role of illness cognitions and coping. Diseases of the Esophagus: Official Journal of the International Society for Diseases of the Esophagus, 25(3), 222–227. 10.1111/j.1442-2050.2011.01233.x [DOI] [PubMed] [Google Scholar]
- 21.Fischer MJ, Wiesenhaan ME, Does-den Heijer A, Kleijn WC, Nortier JWR, & Kaptein AA (2013). From despair to hope: a longitudinal study of illness perceptions and coping in a psycho-educational group intervention for women with breast cancer. British Journal of Health Psychology, 18(3), 526–545. 10.1111/j.2044-8287.2012.02100.x [DOI] [PubMed] [Google Scholar]
- 22.McCorry NK, Dempster M, Quinn J, Hogg A, Newell J, Moore M, … Kirk SJ (2013). Illness perception clusters at diagnosis predict psychological distress among women with breast cancer at 6 months post diagnosis. Psycho-Oncology, 22(3), 692–698. 10.1002/pon.3054 [DOI] [PubMed] [Google Scholar]
- 23.Westbrook TD, Maddocks K, & Andersen BL (2016). The relation of illness perceptions to stress, depression, and fatigue in patients with chronic lymphocytic leukaemia. Psychology & Health, 31(7), 891–902. 10.1080/08870446.2016.1158259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dempster M, McCorry NK, Brennan E, Donnelly M, Murray LJ, & Johnston BT (2011). Do changes in illness perceptions predict changes in psychological distress among oesophageal cancer survivors? Journal of Health Psychology, 16(3), 500–509. 10.1177/1359105310386633 [DOI] [PubMed] [Google Scholar]
- 25.Freeman-Gibb LA, Janz NK, Katapodi MC, Zikmund-Fisher BJ, & Northouse L (2017). The relationship between illness representations, risk perception and fear of cancer recurrence in breast cancer survivors. Psycho-Oncology, 26(9), 1270–1277. 10.1002/pon.4143 [DOI] [PubMed] [Google Scholar]
- 26.Pillay B, Lee SJ, Katona L, De Bono S, Burney S, & Avery S (2015). A prospective study of the relationship between sense of coherence, depression, anxiety, and quality of life of haematopoietic stem cell transplant patients over time. Psycho-Oncology, 24(2), 220–227. 10.1002/pon.3633 [DOI] [PubMed] [Google Scholar]
- 27.Zhang N, Fielding R, Soong I, Chan KKK, Tsang J, Lee V, … Lam WWT (2016). Illness perceptions among cancer survivors. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer, 24(3), 1295–1304. 10.1007/s00520-015-2914-3 [DOI] [PubMed] [Google Scholar]
- 28.Copelan EA (2006). Hematopoietic stem-cell transplantation. The New England Journal of Medicine, 354(17), 1813–1826. 10.1056/NEJMra052638 [DOI] [PubMed] [Google Scholar]
- 29.Andrykowski MA, Bishop MM, Hahn EA, Cella DF, Beaumont JL, Brady MJ, … Wingard JR (2005). Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 23(3), 599–608. 10.1200/JCO.2005.03.189 [DOI] [PubMed] [Google Scholar]
- 30.Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, … Gansler T (2012). Nutrition and physical activity guidelines for cancer survivors. CA: A Cancer Journal for Clinicians, 62(4), 243–274. 10.3322/caac.21142 [DOI] [PubMed] [Google Scholar]
- 31.Kabat GC, Matthews CE, Kamensky V, Hollenbeck AR, & Rohan TE (2015). Adherence to cancer prevention guidelines and cancer incidence, cancer mortality, and total mortality: a prospective cohort study. The American Journal of Clinical Nutrition, 101(3), 558–569. 10.3945/ajcn.114.094854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Warren GW, Sobus S, & Gritz ER (2014). The biological and clinical effects of smoking by patients with cancer and strategies to implement evidence-based tobacco cessation support. The Lancet. Oncology, 15(12), e568–580. 10.1016/S1470-2045(14)70266-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baliousis M, Rennoldson M, Dawson DL, Mills J, & das Nair R (2017). Perceptions of Hematopoietic Stem Cell Transplantation and Coping Predict Emotional Distress During the Acute Phase After Transplantation. Oncology Nursing Forum, 44(1), 96–107. 10.1188/17.ONF.96-107 [DOI] [PubMed] [Google Scholar]
- 34.Goetzmann L, Klaghofer R, Wagner-Huber R, Halter J, Boehler A, Muellhaupt B, … Buddeberg C (2007). Psychosocial vulnerability predicts psychosocial outcome after an organ transplant: results of a prospective study with lung, liver, and bone-marrow patients. Journal of Psychosomatic Research, 62(1), 93–100. 10.1016/j.jpsychores.2006.07.023 [DOI] [PubMed] [Google Scholar]
- 35.Mah K, Khoraych M, Lipton JH, Messner HA, Khoraych G, Krawiec K, … Devins GM (2008). Do allogeneic bone marrow transplant candidates match coping to controllability of pre-treatment stressors? Psychology, Health & Medicine, 13(3), 337–345. 10.1080/13548500701513724 [DOI] [PubMed] [Google Scholar]
- 36.Frick E, Fegg MJ, Tyroller M, Fischer N, & Bumeder I (2007). Patients’ health beliefs and coping prior to autologous peripheral stem cell transplantation. European Journal of Cancer Care, 16(2), 156–163. 10.1111/j.1365-2354.2006.00725.x [DOI] [PubMed] [Google Scholar]
- 37.Moss-Morris R, Weinman J, Petrie K, Horne R, Cameron L, & Buick D (2002). The Revised Illness Perception Questionnaire (IPQ-R). Psychology & Health, 17(1), 1–16. 10.1080/08870440290001494 [DOI] [Google Scholar]
- 38.Watson D, O’Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, … Stuart S (2007). Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychological Assessment, 19(3), 253–268. 10.1037/1040-3590.19.3.253 [DOI] [PubMed] [Google Scholar]
- 39.Kohl HW, Blair SN, Paffenbarger RS, Macera CA, & Kronenfeld JJ (1988). A MAIL SURVEY OF PHYSICAL ACTIVITY HABITS AS RELATED TO MEASURED PHYSICAL FITNESS. American Journal of Epidemiology, 127(6), 1228–1239. 10.1093/oxfordjournals.aje.a114915 [DOI] [PubMed] [Google Scholar]
- 40.Anagnostopoulos F, & Spanea E (2005). Assessing illness representations of breast cancer: a comparison of patients with healthy and benign controls. Journal of Psychosomatic Research, 58(4), 327–334. 10.1016/j.jpsychores.2004.09.011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


