Abstract
In Kienböck's disease, radius shortening osteotomy is the most common treatment. The Camembert procedure is a wedge osteotomy that shortens only the radius facing the lunate. Its aim is to offload the lunate by redirecting the compression stress of the grip forces toward the scaphoid. The purpose of this study was to determine if the Camembert osteotomy is effective in improving clinical symptoms and limits lunate collapse. The series include 10 patients who underwent a Camembert osteotomy for Kienböck's disease between 2002 and 2012 (one bilaterally). They are six men and four women, aged 40.6 years. Five patients had an additional ulnar shortening osteotomy if ulnar variance was neutral or positive. The mean follow-up is 7 years. Preoperatively, range of motion, grip strength, pain, and functional scores were poor. All osteotomies healed within 3 months. Extension, ulnar deviation, grip, functional scores improved significantly. In 10 cases, there were improvement in the T1 and T2 signals on the magnetic resonance imaging (MRI). There was no lunate collapse. This series shows good results with no worsening of the lunate shape. There was no ulnocarpal impingement. The Camembert osteotomy proposes to offload the lunate and redirect strains toward the scaphoid. The supposed interest is to protect the lunate from collapse. In this small series, the Camembert osteotomy improved function in patients with early stage Kienböck's disease. MRI aspects improve in most cases and no patients collapsed. Camembert can be used in combination with a Sennwald's ulnar shortening when ulnar variance is neutral or positive. Authors propose this procedure for Lichtman's stages 1–2–3A if there are no cartilage or ligament lesions. This is a Level IV, case series study.
Keywords: Kienböck's disease, radius, osteotomy, Camembert
In Kienböck's disease, lunate necrosis may progress to fracture and collapse. Many osteotomies have been proposed to avoid this evolution by decompressing the lunate. Most of these osteotomies are performed on the radius. 1 2 3 4 5 6 7 They all shorten the radius transversely, possibly by reorienting the radial facet. This allows a shortening of the radius facing the lunate but also the scaphoid. The shortening of the capitate is also proposed to decompress the lunate but on its distal side. 8 9 However, this also decompresses the scaphoid. 10 11
The Camembert osteotomy, described in 2012, 12 shortens only the radius facing the lunate, and not the scaphoid, so that the intracarpal axial compression loads are redirected toward the scaphoid. In case of a long ulna, a Sennwald's type shortening can be associated. 12
The authors present a series of 11 wrists operated on 10 patients, with radioclinical analysis, with an average follow-up of 7 years. The purpose of this paper was to determine if the osteotomy is effective at decreasing symptoms and second, if it prevents further lunate collapse.
Patients and Methods
The study is retrospective, comparing pre- and postoperative objective clinical data (mobility, strength), subjective data (pain, PRWE [Patient-Rated Wrist Evaluation], and SANE [Single Assessment Numerical Evaluation] scores 13 14 15 16 ), and radiographic data (radio and magnetic resonance imaging [MRI]).
Thirteen patients were operated between 2002 and 2012 in one center by the same operator, using the Camembert osteotomy technique. 12 All patients gave their informed consent to this procedure after the different surgical options were explained to them. They also consented for us to use the clinical data.
In the Camembert osteotomy, the approach is dorsal through the fourth compartment. The radius and ulna are exposed and their contours are checked. A bone corner of radius with medial base and distal subchondral apex, facing the scapholunate crest, is defined using a pin whose position is verified under fluoroscopy 12 ( Fig. 1A ). This corner is then cut with an oscillating saw. The remaining bone block, corresponding to the lunar facet of the radius, is mobilized proximally ( Fig. 1B ). After closure of the osteotomy by distal osteoclasia, osteosynthesis is performed with a compression bone staple ( Fig. 2 ), a Memoclip staple (Stryker) in most cases. However, this staple is no longer available and we now use the Easyclip staple (Stryker).
Fig. 1.
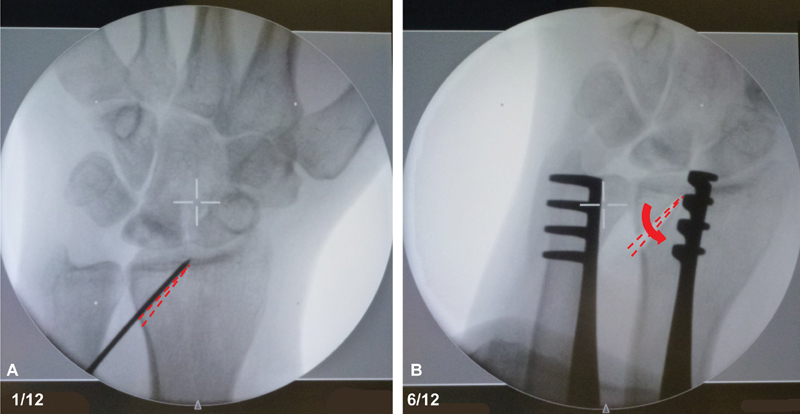
Surgical procedure. (A) Pin used to design osteotomy. Dotted line: shape of bone corner to remove. (B) Radius after bone corner removal. The arrow illustrates the movement of lunate facet of the radius.
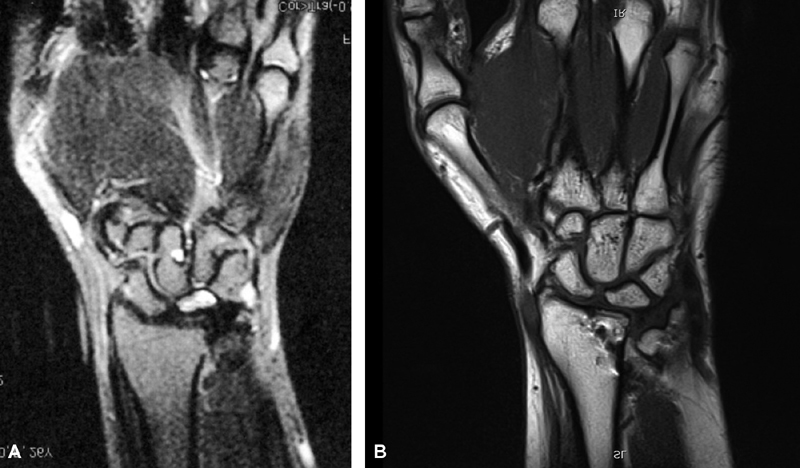
Fig. 2.

Camembert osteotomy. Fixation with dorsal staple.
Three patients were lost to follow-up. The series consists of 11 wrists operated on 10 patients, six men and four women. The average age at the time of the intervention was 40.6 years (range, 26–59 years). The preoperative time between the onset of clinical disorders and the procedure was 9 months (range, 3–14 months). The average follow-up was 7 years (range, 5–15 years). In five cases, an ulnar shortening osteotomy as described by Sennwald et al 12 17 was done with fixation using a compression screw ( Fig. 3 ). This corresponded to wrists with neutral or positive radioulnar index four times, and in one case, it was done to decrease strains on a tense TFCC (triangular fibro cartilaginous complex) that prevented mobilization of the radial block and closure of the osteotomy.
Fig. 3.

Association with Sennwald's ulnar osteotomy. Fixation with a compression screw.
Preoperative mobility ( Table 1 ) was measured using a goniometer. Flexion/extension was decreased compared with the healthy side, while frontal inclinations and pronosupination were preserved. Grip strength was evaluated using Jammar's dynamometer; pain was evaluated using the visual analog scale (VAS). These measures, as well as the PRWE and SANE functional scores, were poor ( Table 1 ).
Table 1. Preoperative data.
| Cases | Preoperative data | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Sex | Age (y) | Lichtman's stage | MRI stage | Time before surgery (mo) | Type of surgery (radius [R] or radius + ulna [RU]) | Flexion | Extension | Radial deviation | Ulnar deviation | Pronation | Supination | Grasp | Pain (VAS) | PRWE score (/150) | SANE score | Stahl's index |
| 1 | F | 26 | 3A | B | 8 | RU | 42 | 50 | 20 | 20 | 90 | 90 | 11 | 7 | 51 | 20 | 0.497 |
| 2 | F | 39 | 1 | A | 7 | RU | 37 | 41 | 9 | 12 | 85 | 90 | 8 | 10 | 77 | 25 | 0.466 |
| 3 | M | 33 | 3A | B | 10 | R | 28 | 33 | 6 | 17 | 80 | 80 | 14 | 10 | 59 | 30 | 0.293 |
| 4 | F | 59 | 3A | B | 3 | R | 45 | 40 | 12 | 28 | 90 | 90 | 17 | 9 | 68 | 40 | 0.369 |
| 5 | F | 38 | 1 | B | 12 | RU | 90 | 65 | 30 | 50 | 75 | 90 | 31 | 8 | 63 | 40 | 0.482 |
| 6 | M | 34 | 2 | B | 9 | R | 56 | 65 | 18 | 32 | 85 | 85 | 22 | 9 | 110 | 30 | 0.517 |
| 7 | M | 47 | 2 | B | 11 | R | 49 | 47 | 10 | 18 | 70 | 80 | 12 | 8 | 104 | 30 | 0.526 |
| 8 | M | 57 | 2 | B | 14 | RU | 46 | 40 | 8 | 27 | 90 | 90 | 5 | 6 | 101 | 15 | 0.505 |
| 58 | 2 | B | 6 | RU | 60 | 50 | 12 | 20 | 90 | 90 | 7 | 8 | 79 | 15 | 0.59 | ||
| 9 | M | 38 | 2 | B | 8 | R | 38 | 42 | 12 | 15 | 90 | 90 | 9 | 8 | 79 | 35 | 0.482 |
| 10 | M | 26 | 3A | B | 12 | R | 42 | 50 | 16 | 20 | 75 | 70 | 12 | 8 | 115 | 13 | 0.35 |
| Average | M = 6 | 41.4 | 1 = 2 | A = 1 | 9,1 | RU = 5 | 48.5 | 47.5 | 13.9 | 23.5 | 83.6 | 85.9 | 13.5 | 8.3 | 82.4 | 26.6 | 0.46 |
| F = 4 | 2 = 5 | B = 10 | R = 6 | ||||||||||||||
| 3A = 4 | |||||||||||||||||
Abbreviations: F, female; M, male; MRI, magnetic resonance imaging; PRWE, patient-rated wrist evaluation; SANE, single assessment numerical evaluation; VAS, visual analogue scale.
X-ray analysis showed two patients at Lichtman's stage 1, five patients at stage 2, and four patients at stage 3A. 18 The MRI analysis 18 showed one purely edematous lunate stage A and 10 heterogenous lunate stage B.
Differences in pre- and postoperative data were calculated. A Student's t -test was used for statistical analysis.
Results
Table 2 compares pre- and postoperative results. There was a nonsignificant gain in flexion and radial inclination, a significant gain in extension, ulnar inclination and grip, a nonsignificant loss of pronosupination, a significant decrease in pain, and a significant improvement in PRWE and SANE scores ( Table 2 ).
Table 2. Postoperative evolution.
| postoperative evolution (post op data / preop data) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Follow up | Flexion | Extension | Radial deviation | Ulnar Deviation | Pronation | Supination | grasp | Pain (VAS) | PRWE Score (/150) | SANE Score | Postop Stahl index | Stahl index difference postop-preop | MRI Stage | Lunate balance (N = neutral) |
| 1 | 120 | 26 | 10 | 12 | 20 | 0 | 0 | 15 | −7 | −51 | 80 | 0,491 | −0,006 | Normal | N |
| 2 | 78 | 13 | 25 | 19 | 13 | −10 | −34 | 18 | −8 | −49 | 65 | 0,43 | −0,036 | Normal | Visi |
| 3 | 92 | 22 | 22 | 14 | 3 | 0 | 10 | 26 | −8,5 | −52 | 70 | 0,374 | 0,081 | Normal | Visi |
| 4 | 156 | 9 | 20 | 4 | 22 | 0 | 0 | 7 | −8 | −37 | 55 | 0,505 | 0,136 | Hetero | N |
| 5 | 66 | −16 | −5 | 0 | −8 | −5 | −5 | −4,5 | −5 | −3 | 40 | 0,48 | −0,002 | Hetero | N |
| 6 | 78 | 12 | −3 | −4 | −2 | −5 | −15 | 10 | −7 | −97 | −30 | 0,499 | −0,018 | Hetero | N |
| 7 | 62 | −1 | −10 | −2 | 11 | 6 | −5 | 24 | −6 | −71 | −30 | 0,462 | −0,064 | Hetero | N |
| 8 | 69 | 9 | 20 | 7 | 3 | 0 | 0 | 33 | −4 | −80 | 60 | 0,596 | 0,091 | Hetero | N |
| 61 | −12 | 12 | 4 | 8 | 0 | 0 | 29 | −6 | −65 | 60 | 0,589 | −0,001 | Normal | N | |
| 9 | 72 | 7 | 13 | 18 | 22 | 0 | 0 | 26 | −6 | −31 | 50 | 0,461 | −0,021 | Hetero | Visi |
| 10 | 100 | 8 | −5 | −6 | 32 | 15 | 20 | 13 | −8 | −99 | 77 | 0,385 | 0,035 | Hetero | visi |
| average | 86,9 | 6,9 | 10,1 | 6 | 7,8 | −1,6 | −5,4 | 17,5 | −6,6 | −56,1 | 41,1 | 0,48 | 0,02 | N = 4 | N = 7 |
| H = 7 | Visi = 4 | ||||||||||||||
Abbreviations: MRI, magnetic resonance imaging; postop, postoperative; preop, preoperative; PRWE, patient-rated wrist evaluation; SANE, single assessment numerical evaluation; VAS, visual analogue score; VISI, volar intercalated segment instability.
The comparative analysis of the simple radial osteotomy group (R − U) and the radial and ulnar osteotomy group (R + U) do not show any significant difference in pre- and postoperative pronosupination measures. However, there is a significant improvement in grip for patients in the R − U group ( p = 0.035); the improvement is not significant ( p = 0.051) for the R + U group.
Radiographically, the lunate evolved without collapse, or aggravation of its trabecular state, in all cases. It improved in most cases with reconstruction of spans (case N1, Fig. 4 ). In one case, an initial sagittal fracture healed after 4 years (case 3, Fig. 5 ). Stahl's index was preoperatively 0.46 and postoperatively 0.48. The difference is not significant ( p = 0.35).
Fig. 4.

Case 1: Self reconstruction of the lunate (A) at procedure time, (B) at 1-year follow-up, (C) at 10 years.
Fig. 5.

Healing of a sagittal fracture (A) at 6-month follow-up, (B) at 4-year follow-up, and (C) at 8 years.
On MRI, the signal was also improved in 10 cases, with lunate considered normal in four cases ( Fig. 6 ), and with persistence of heterogeneity in six cases ( Fig. 7 ), but less than before the procedure.
Fig. 6.
Clinical case with MRI normalization (A) before procedure and (B) after procedure at 120 months. MRI, magnetic resonance imaging.
Fig. 7.
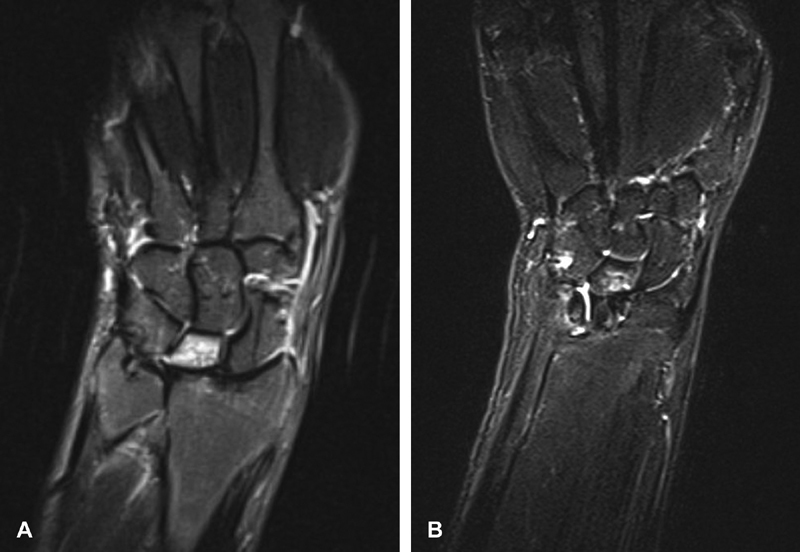
Clinical case with MRI improvement but persistent abnormalities (A) before procedure and (B) after procedure at 72 months. MRI, magnetic resonance imaging.
The overall results were excellent or good in eight cases and moderate in two cases. A bad case (N 7) evolved into a painful lunocapitate arthritis ( Fig. 8 ) and was reoperated. The complications were mainly related to discomfort caused by the dorsal staple, which was removed in four cases. There was no radius or ulna necrosis, no sepsis, no complex regional pain syndrome (CRPS), no nonunion.
Fig. 8.
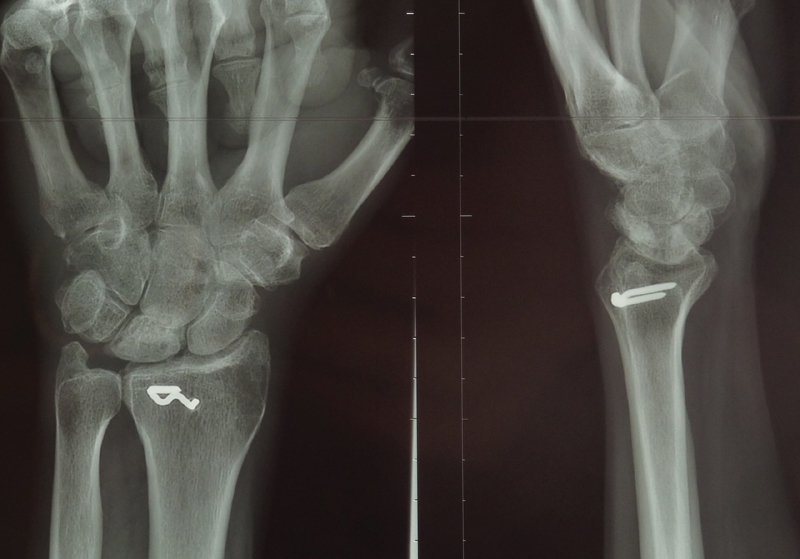
Lunocapitate arthritis evolution in the bad case.
Discussion
Radial shortening decompression is the oldest proposal of treatment, following work suggesting that Kienböck's disease was linked to a negative radioulnar index. 19 This would correspond to a kind of radial impingement syndrome, by radiocarpal hyperpressure; actually, this is unlikely. In a localized hyperpressure conflict, degenerative damage begins with cartilage. In these cases, the bone anomalies are located at the stress zone without affecting the entire bone. In Kienböck's disease, edema usually affects the entire bone from stage 1 and cartilage is not affected until later. 20 On the other hand, it is true that lunate collapse occurs facing the radius. This seems essentially due to the difference in Young's modulus of the radius and the TFCC which proximally cover the lunate. Cortical bone of the radius has a Young's modulus of 13.8 to 16 GPa, 21 22 23 cartilage 10 to 15 MPa, 23 24 25 26 and TFCC only 10 KPa. 27 This leads to intraosseous shearing in the spans of the lunate which crushes against the hardest area. We believe that a distinction must be made between the causes of necrosis and the causes of collapse. Necrosis could be caused by intraosseous hyperpressure with vascular edema. 28 Collapse could be due to excessive mechanical stresses of the lunate, resulting from the action of the forearm muscles, whose longitudinal direction transmits the compression to the radius via the scaphoid and lunate. 29 The decompression must, therefore, allow interruption of mechanical stresses by the lunate. It is thus necessary to redirect these stresses so that they circumvent the lunate, by interrupting the osseous continuity facing it, but by preserving the continuity on both radial and ulnar pathways. The axial stress then follows a line through the scaphoid. If this deviation of the stress probably does not cure vascular necrosis, it protects the lunate from this intraosseous shearing and collapse, the time for a possible revascularization.
The lunocapitate arthritis that marked the only bad evolution of the series developed on an unfragmented lunate. It is probable that this midcarpal degradation is possibly related to pre-existing ligament lesions at the osteotomy. The radiographic assessment before the second surgical procedure indeed shows signs of static scapholunate instability without gap, with a ring sign of the scaphoid visible in ulnar inclination, and on profile view a decreased scapholunate angle ( Fig. 8 ). An arthroscopy performed before the osteotomy could have revealed possible lesions that would have contraindicated this procedure. 20 We did not perform arthroscopy for this indication at that time. This has been part of the International Federation of Societies for Surgery of the Hand (IFSSH) recommendations since 2010. 18
Radial glenoid morphology may be involved in the etiopathogenicity of Kienböck's disease. A lunar fossa with an axis close to the horizontal line (less than 12 degrees) is considered a risk factor for necrosis. 30 31 The Camembert osteotomy, by raising the lunar fossa of the radius, partially reverticalizes its axis which passes above 12 degrees, and decompresses the lunate without decompressing the scaphoid. Radial transverse osteotomy can be considered as gold standard, due to the number of publications concerning this technique. For Salmon et al the radial shortening “does not reverse or halt Kienböck's disease, it slows down the rate of degenerative change.” 3 For van Leeuwen et al, “the average progression is slight and radial shortening does not have a large effect on that progression.” 32 For Afshar and Eivaziatashbeik, radial shortening osteotomy does not affect the shape of the lunate directly. In their study, Afshar and Eivaziatashbeik noticed one progression of the disease on nine cases treated with osteotomy after 6 years. 33 Calfee et al noticed seven radiographic progression of the disease on 31 cases after 5 years. 34 If we compare with our series, we found one bad evolution with arthritis, but the lunate didn't collapse at the time of reoperation. This ratio of degenerative evolution is not worse than other series.
The transverse osteotomies of the capitate, 9 10 shortening the entire bone, interrupt the continuity between the capitate and the scaphoid. The Moritomo's osteotomy, in order not to decompress the scaphoid, partially shortens the capitate. 11 The shortening only concerns the lunar surface of the capitate but it creates a step. If one takes into account the inclination movements of the midcarpal joint, 35 this could cause a conflict during radial inclination of the wrist between the edge of the capitate osteotomy and the lunate. In the Camembert osteotomy, there is no step at glenoid level. The dorsal staple sometimes caused irritation. Using a buried screw could limit this. But we prefer a compression perpendicular to the osteotomy plan, which the screw hardly allows.
Performing a radial or radioulnar osteotomy in relation to the distal radio ulnar joint (DRUJ) could compromise pronosupination. However, this is true for all radial or ulna osteotomies, as soon as joint congruence is modified. The radial shortening is small, approximately 2 mm on its ulnar side. The possibility of shortening the ulna allows the ulnar head to follow the radial incisure, and thus to maintain joint congruence. Analysis of the results shows that there is no significant loss of pronosupination, neither in patients undergoing isolated radial shortening, nor associated with ulnar shortening. We recommend associating ulnar shortening as soon as loss of congruence is detected after an isolated Camembert osteotomy. This concerns the positive radioulnar index, the anatomy of the distal radioulnar Tolat et al's type 2 or 3, 36 the impossibility of closing the radial osteotomy by a high TFCC tension.
This study presents weaknesses. Currently the benefit compared with transverse osteotomy is not proven yet. This series is the first midterm series about this procedure in the literature. Because this is a single operator series, the subset of patients is reduced, but the midterm of 7 years is interesting. The patients' selection may be biased, particularly for stage 1 patients, whose treatment is not always surgical. For the patients operated on here, conservative treatment was ineffective on pain and function. The superior benefit of the Camembert procedure is a hope, but the evolution with improvement of most of the lunates in encouraging.
Conclusion
The decompression of the lunate by radial Camembert osteotomy, possibly associated with ulnar shortening, appears to protect the lunate and carpus, from fracture aggravation, or collapse. This osteotomy is accompanied by significant pain reduction and good improvement in functional scores. MRI confirms the revascularization and sometimes the healing of the lunate. There are few complications, the most frequent being intolerance to the staple requiring its removal. The patient satisfaction rate is very good. We continue to use this osteotomy in cases where the lunate can be preserved and in the absence of cartilage or ligament injury found at arthroscopy.
Footnotes
Conflict of Interest None declared.
References
- 1.Dautel G. Treatment of Kienböck's disease. Round Table.33rd GEM-SFCM meeting. La Main. 1999;4:143–71. [Google Scholar]
- 2.Schuind F, Eslami S, Ledoux P. Kienbock's disease. J Bone Joint Surg Br. 2008;90(02):133–139. doi: 10.1302/0301-620X.90B2.20112. [DOI] [PubMed] [Google Scholar]
- 3.Salmon J, Stanley J K, Trail I A. Kienböck's disease: conservative management versus radial shortening. J Bone Joint Surg Br. 2000;82(06):820–823. doi: 10.1302/0301-620x.82b6.10570. [DOI] [PubMed] [Google Scholar]
- 4.Weiss A P, Weiland A J, Moore J R, Wilgis E F. Radial shortening for Kienböck disease. J Bone Joint Surg Am. 1991;73(03):384–391. [PubMed] [Google Scholar]
- 5.Garcia-Elias M, An K N, Cooney W P, Linscheid R L. Lateral closing wedge osteotomy for treatment of Kienböck's disease. A clinical and biomechanical study of the optimum correcting angle. Chir Main. 1998;17(04):283–290. doi: 10.1016/s0753-9053(98)80027-6. [DOI] [PubMed] [Google Scholar]
- 6.Nakamura R, Tsuge S, Watanabe K, Tsunoda K. Radial wedge osteotomy for Kienböck disease. J Bone Joint Surg Am. 1991;73(09):1391–1396. [PubMed] [Google Scholar]
- 7.Gomis R, Martin B, Idoux O, Chammas M, Allieu Y. [Kienböck disease: treatment by shortening osteotomy of the radius] Rev Chir Orthop Repar App Loc. 1994;80(03):196–204. [PubMed] [Google Scholar]
- 8.Waitayawinyu T, Chin S H, Luria S, Trumble T E. Capitate shortening osteotomy with vascularized bone grafting for the treatment of Kienböck's disease in the ulnar positive wrist. J Hand Surg Am. 2008;33(08):1267–1273. doi: 10.1016/j.jhsa.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 9.Rabarin F, Saint Cast Y, Cesari B, Raimbeau G, Fouque P A. [Capitate osteotomy in Kienböck's disease in twelve cases.Clinical and radiological results at five years follow-up] Chir Main. 2010;29(02):67–71. doi: 10.1016/j.main.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Moritomo H. Switzerland: Springer; 2016. Wrist biomechanics as applied to the lunate and Kienböck's disease; pp. 41–51. [Google Scholar]
- 11.Moritomo H, Murase T, Yoshikawa H. Operative technique of a new decompression procedure for Kienböck disease: partial capitate shortening. Tech Hand Up ExtremSurg. 2004;8(02):110–115. doi: 10.1097/01.bth.0000126571.20944.47. [DOI] [PubMed] [Google Scholar]
- 12.Camus E J, Van Overstraeten L. Surgical technique of a radial wedge “Camembert” osteotomy in Kienböck disease. Tech Hand Up ExtremSurg. 2012;16(02):75–79. doi: 10.1097/BTH.0b013e3182492e9e. [DOI] [PubMed] [Google Scholar]
- 13.MacDermid J C, Turgeon T, Richards R S, Beadle M, Roth J H. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(08):577–586. doi: 10.1097/00005131-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Williams G N, Gangel T J, Arciero R A, Uhorchak J M, Taylor D C. Comparison of the single assessment numeric evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(02):214–221. doi: 10.1177/03635465990270021701. [DOI] [PubMed] [Google Scholar]
- 15.Williams G N, Taylor D C, Gangel T J, Uhorchak J M, Arciero R A. Comparison of the single assessment numeric evaluation method and the Lysholm score. ClinOrthopRelat Res. 2000;(373):184–192. doi: 10.1097/00003086-200004000-00022. [DOI] [PubMed] [Google Scholar]
- 16.Lee C H, Choi W S, Kim S J, Kim J H, Lee K H. Correlation between patient-rated outcome questionnaire and single assessment numerical evaluation score in the fracture of distal radius. J Hand Surg Am. 2018;43 02:SS37–SS38. [Google Scholar]
- 17.Sennwald G R, Lauterburg M, Zdravkovic V. A new technique of reattachment after traumatic avulsion of the TFCC at its ulnar insertion. J Hand Surg [Br] 1995;20(02):178–184. doi: 10.1016/s0266-7681(05)80046-4. [DOI] [PubMed] [Google Scholar]
- 18.Lichtman D M, Pientka W F, II, Bain G I. Kienböck Disease: A New Algorithm for the 21st Century. J Wrist Surg. 2017;6(01):2–10. doi: 10.1055/s-0036-1593734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hulten O. Uber Anatomische variationen Der Hand-gelenkknochen: Ein beitrag zur kenntnis der genesezwei verschiedener mondbeinveranderungen. Acta Radiol Scand. 1928;9:155–168. [Google Scholar]
- 20.Bain G I, Begg M. Arthroscopic assessment and classification of Kienbock's disease. Tech Hand Up Extrem Surg. 2006;10(01):8–13. doi: 10.1097/00130911-200603000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Bosisio M R, Talmant M, Skalli W, Laugier P, Mitton D. Apparent Young's modulus of human radius using inverse finite-element method. J Biomech. 2007;40(09):2022–2028. doi: 10.1016/j.jbiomech.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 22.Mow V C, Huiskes R. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. Basic Orthopaedic Biomechanics and Mechano-Biology. 3rd Ed; pp. 453–454. [Google Scholar]
- 23.Ledoux P, Lamblin D, Wuilbaut A, Schuind F. A finite-element analysis of Kienbock's disease. J Hand Surg Eur Vol. 2008;33(03):286–291. doi: 10.1177/1753193408090757. [DOI] [PubMed] [Google Scholar]
- 24.Anderson D D, Deshpande B R, Daniel T E, Baratz M E. A three-dimensional finite element model of the radiocarpal joint: distal radius fracture step-off and stress transfer. Iowa Orthop J. 2005;25:108–117. [PMC free article] [PubMed] [Google Scholar]
- 25.Edwards W B, Troy K L. Finite element prediction of surface strain and fracture strength at the distal radius. Med Eng Phys. 2012;34(03):290–298. doi: 10.1016/j.medengphy.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 26.Richard F, Villars M, Thibaud S.Comportement viscoélastique du cartilage articulaire humain normal et arthrosique: modélisation et caractérisation à l'aide d'essais d'indentation instrumentéeÈcongrès Français Mécanique. Available at:http://documents.irevues.inist.fr/bitstream/handle/2042/52735/a_X27S34ZP.pdf?sequence=1. 2013
- 27.Bae W C, Ruangchaijatuporn T, Chang E Y et al. MR morphology of triangular fibrocartilage complex: correlation with quantitative MR and biomechanical properties. Skeletal Radiol. 2016;45(04):447–454. doi: 10.1007/s00256-015-2309-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Watson H K, Guidera P M. Aetiology of Kienböck's disease. J Hand Surg [Br] 1997;22(01):5–7. doi: 10.1016/s0266-7681(97)80004-6. [DOI] [PubMed] [Google Scholar]
- 29.Camus E J. France: Sauramps medical–Montpellier; 2006. Aspect biomécanique et conséquences des arthrodèses intra-carpiennes; pp. 165–177. [Google Scholar]
- 30.Matsushita K, Firrell J C, Tsai T M. X-ray evaluation of radial shortening for Kienböck's disease. J Hand Surg Am. 1992;17(03):450–455. doi: 10.1016/0363-5023(92)90346-q. [DOI] [PubMed] [Google Scholar]
- 31.Thienpont E, Mulier T, Rega F, De Smet L. Radiographic analysis of anatomical risk factors for Kienböck's disease. Acta Orthop Belg. 2004;70(05):406–409. [PubMed] [Google Scholar]
- 32.van Leeuwen W F, Janssen S J, Ring D. Radiographic progression of Kienböck disease: radial shortening versus no surgery. J Hand Surg Am. 2016;41(06):681–688. doi: 10.1016/j.jhsa.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 33.Afshar A, Eivaziatashbeik K. Long-term clinical and radiological outcomes of radial shortening osteotomy and vascularized bone graft in Kienböck disease. J Hand Surg Am. 2013;38(02):289–296. doi: 10.1016/j.jhsa.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 34.Calfee R P, Van Steyn M O, Gyuricza C, Adams A, Weiland A J, Gelberman R H. Joint leveling for advanced Kienböck's disease. J Hand Surg Am. 2010;35(12):1947–1954. doi: 10.1016/j.jhsa.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Camus E J, Millot F, Larivière J, Rtaimate M, Raoult S.Le carpe à double cupule: illustration de la géométrie variable du carpe Chir Main 2008270112–19.. doi: 10.1016/j.main.2007.10.005 [DOI] [PubMed] [Google Scholar]
- 36.Tolat A R, Sanderson P L, De Smet L, Stanley J K. The gymnast's wrist: acquired positive ulnar variance following chronic epiphyseal injury. J Hand Surg [Br] 1992;17(06):678–681. doi: 10.1016/0266-7681(92)90200-l. [DOI] [PubMed] [Google Scholar]


