Abstract
Background
The prevalence of persons who are born with primary and secondary male sexual characteristics but feel that they are female (trans women) is ca. 5.48 per 100 000 males in Germany. In this article, we provide a detailed overview of the currently available data on quality of life after male-to-female sex reassignment surgery.
Methods
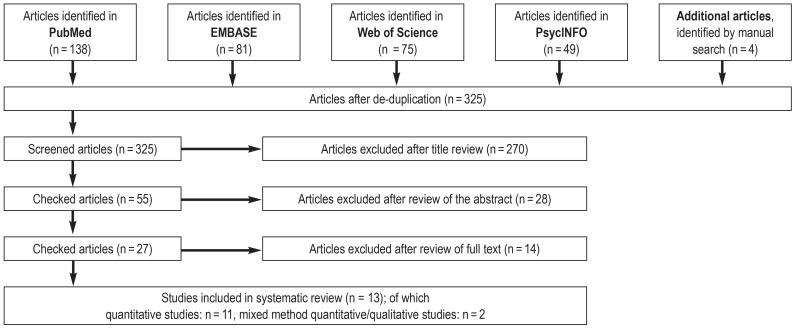
This review is based on publications retrieved by a systematic literature search that was carried out in the PubMed, EMBASE, Web of Science, and PsycINFO databases in March 2017.
Results
The 13 articles (11 quantitative and 2 mixed quantitative/qualitative studies) that were found to be suitable for inclusion in this review contained information on 1101 study participants. The number of trans women in each study ranged from 3 to 247. Their mean age was 39.9 years (range: 18–76). Seven different questionnaires were used to assess postoperative quality of life. The findings of the studies permit the conclusion that sex reassignment surgery beneficially affects emotional well-being, sexuality, and quality of life in general. In other categories (e.g., “freedom from pain”, “fitness”, and “energy”), some of the studies revealed worsening after the operation. All of the studies were judged to be at moderate to high risk of bias. The drop-out rates, insofar as they were given, ranged from 12% to 77% (median: 56%).
Conclusion
Current studies indicate that quality of life improves after sex reassignment surgery. The available studies are heterogeneous in design. In the future, prospective studies with standardized methods of assessing quality of life and with longer follow-up times would be desirable.
The term “gender incongruence” (GI) describes the situation in which a person does not identify with the gender they were assigned at birth on the basis of physical sexual characteristics and that they consequently experience “a marked and persistent incongruence between. .. experienced gender and the assigned sex” (1). The term trans women describes persons with congenital primary and secondary male sexual characteristics (assigned male at birth) who feel/identify as women. Trans men are persons who feel/identify as men but who have primary and secondary female sexual characteristics (assigned female at birth). Persons who fully identify with the sex/gender they were assigned at birth are known as cis women and cis men.
A data analysis from 2000 showed a prevalence in Germany of 4.26 trans persons/100 000 population (5.48 trans women/100 000 of the male population and 3.12 trans men/100 000 of the female population) (2). We are not aware of any more recent data for Germany.
If persons with gender incongruence develop clinically relevant biopsychosocial suffering, they have gender dysphoria (GD), according to the DSM-5 classification (3). For many trans persons, physical transition is the best option for alleviating the symptoms of gender dysphoria (4). Sex/gender reassignment hormone treatment as well as surgery have a central role in this setting (5). The latter comprise surgical procedures involving the genitals (sex reassignment surgery) (box), the breasts, and the face and vocal cords, as well as hair epilation (6).
BOX. Principle of male-to-female sex reassignment surgery.
Bilateral orchiectomy
Preparation of the glans (head) of the penis with the complete neurovascular bundle
Preparation of the urethra
Subtotal resection of the cavernous bodies (corpora cavernosa) and the corpus spongiosum of the penis
-
Vaginoplasty
Preparation of the neovaginal space in the perineal area between rectum and urethra/bladder
-
Lining the space by using
Penile inversion vaginoplasty (pedicle flap from the skin of the penal shaft: gold standard)
If required, use of free split-thickness skin grafts
-
Alternatively, construction of a neo-vagina using intestinal vaginoplasty:
In selected cases, this is the primary indication—for example, in trans women with penoscrotal hypoplasia or at the patient’s wish (for better natural secretion).
This procedure can also be used as a secondary intervention in patients after unsatisfactory penile inversion vaginoplasty.
Construction of a neo-clitoris from the glans (head) of the penis
Construction of a urethral neo-meatus after urethral shortening as required
Construction of labia from the remaining scrotal skin, possibly also labia minora
A US study showed that from 2000 to 2011, the rate of surgical sex reassignment measures among trans persons rose from 72% to 83.9% (7). These data move the question of the effectiveness of such operations increasingly into the focus of clinical attention and awareness (8– 11).
In the context of evidence-based medicine, the consensus is now that the success of medical procedures should not be studied merely in terms of objective results (survival and complication rates, measurements of functionality, etc), but that patients’ personal wellbeing should be included in assessing the success of any procedure (12, 13). Review articles to date have shown that sex reassignment hormone treatment has a positive effect on the quality of life of trans persons (14, 15). By contrast, an overall assessment of quality of life after sex reassignment surgery is so far lacking. In this article we will attempt to provide a review of current studies, and on this basis we will investigate the question of quality of life after sex reassignment surgery.
For the review to be as representative as possible, this article deals with trans women only, whose incidence is notably higher than that of trans men (0.41 male to female/100 000 total male population in Germany and 0.26 female to male/100 000 total female population in Germany) (2).
Methods
We conducted as systematic literature search in PubMed, EMBASE, Web of Science, and PsycINFO in March 2017. GW and DGN independently undertook the article search on the basis of the recommendations summarized in the PRISMA statement (16). Details of the methods are described in the eMethods section.
Inclusion criteria
We included only articles on the subject of the quality of life of trans women after sex reassignment surgery. GW, RF, and DGN operationalized (etable 1) the search terms in an iterative process according to the PICO method (e1) and set out a search string (etable 2).
eTable 1. Search terms*.
| Population | transsexualism, transgender, transgenderism, gender identity disorder, transgender persons, sexual transition, gender transition, male-to-female, gender non-conform, gender-transform, gender incongruence |
| Intervention | reassignment surgery, sex reassignment, sex reassignment surgery, sex change, gender reassignment surgery, sex reassignment operation, gender transformation operation, penile inversion vaginoplasty |
| Comparison | – |
| Outcome | quality of life |
* Key words used in accordance with the PI(C)O method
eTable 2. Search string*.
| EMBASE | “transsexualism” OR “transgender” OR “transgenderism” AND (“reassignment surgery” OR “sex reassignment”) AND “quality of life” |
| PsycINFO | (DE “Transgender” OR DE “Transsexualism” OR DE “Gender Identity Disorder”) AND (DE “Sex Change” OR DE “Surgery” OR “reassignment surgery” OR “sex reassignment”) AND “quality of life” |
|
PubMed 1. Catch phrase search (MeSH terms) 2. Key word search |
(“Transsexualism”[Mesh]) AND (“Sex Reassignment Surgery”[Mesh]) AND (“Quality of Life”[Mesh]) ((“Transgender Persons”[Mesh]) OR “Transsexualism”[Mesh]) AND (“Quality of Life”[Mesh]) (“Quality of life”) AND (“gender reassignment surgery” OR “sex reassignment operation” OR “gender transformation operation” OR “sex reassignment surgery” OR “penile inversion vaginoplasty” AND sex* AND chang* OR sex* AND reassign* OR gender-reassign*) AND (gender-dysphor* OR transsex* OR gender-nonconform* OR gender-non-conform* OR transgend* OR transident* OR gender-incongruence OR gender-varian* OR gender-transform* OR gender-identity-disorder* OR sexual-transition OR gender-transition OR sexual-dysphor* OR transvest* OR autogyn* OR trans-sex* OR trans-gend* OR trans-ident* OR “male-to-female”) |
| Web of Science | (gender-dysphor* OR transsex* OR gender-nonconform* OR gender-non-conform* OR trans-gend* OR trans-ident* OR gender-incongruence OR gender-varian* OR gender-transform* OR gender-identity-disorder* OR sexual-transition OR gender-transition OR sexual-dysphor* OR transvest* OR autogyn* OR trans-sex* OR trans-gend* OR trans-ident* OR “male-to-female”) AND (“gender reassignment surgery” OR “sex reassignment operation” OR “gender transformation operation” OR “sex reassignment surgery” OR “penile inversion vaginoplasty” OR sex* chang* OR sex* reassign* OR gender-reassign*) AND (“quality of life”) |
* Catch phrases and key words used in the literature search
Exclusion criteria
Among others, we excluded studies that did not focus exclusively on trans persons or that didn’t collect data on quality of life by using a standardized questionnaire. We also excluded studies in underage trans people.
Screening process
The Figure shows the study selection process.
Figure.
Flow chart illustrating the study selection process
Study analysis
All included articles are non-randomized studies with an evidence level of III (e2). In the case of studies that reported on the quality of life of trans women as well as trans men (17– 21) we ensured that the data for trans women were evaluated separately or that the ratio of M–F/F–M favored trans women. Table 1 shows further key study data; Table 2 shows the quality characteristics of the studies.
Table 1. Key data from included studies.
|
Authors (reference) |
Publication year | Study design |
Number of patients*1 (M–F)*2 |
Mean follow-up period (range) |
Patients‘ mean age in years (range) |
Evaluation of quality of life (abbreviations of questionnaires used) |
| Ainsworth et al. (22) | 2010 | Cross sectional study | n = 247 | Not available | 50 | SF-36 |
| Bouman et al. (27) | 2016 | Cross sectional study | n = 31 |
2.2 years (0.8–7.5) |
19.1 (18.3–45.0) |
SHS, SWLS, CLLS |
| Cardoso da Silva et al. (26) | 2016 | Prospective cohort study | n = 47 | At least 1 year |
31.23 (16–54) |
WHOQOL-100 |
| Castellano et al. (17) | 2015 | Case–control study |
n = 120 (46 M–F and 14 F–M) |
At least 2 years |
39.0 (18–65) |
WHOQOL-100 |
|
(Control group: 45 cis women and 15 cis men) |
Control group: 40.2 (18–65) |
|||||
| Jokic-Begic et al. (18) | 2014 | Cross sectional study |
n = 6 (3 M–F and 3 F–M) |
At least 3 months |
33.83 (24–42) |
SF-36, semi-structured interview |
| Kuhn et al. (19) | 2009 | Case–control study |
n = 75 (52 M–F and 3 F–M) |
15 years (8–23) |
51 (39–62) |
KHQ, VAS |
|
Control group: (20 cis women) |
Control group: 49 (37–60) |
|||||
| Lindqvist et al. (23) | 2016 | Prospective cohort study | n = 190 |
3 years (1–5) |
36 (19–76) |
SF-36 |
| Papadopulos et al. (29) | 2017 | Cross sectional study | n = 47 |
19 months (6–58) |
38,3 (18–57) |
FLZ |
| Parola et al. (20) | 2010 | Cross sectional study |
n = 30 (15 M–F and 15 F–M) |
At least 2 years |
48,5 (32–65) |
SF-36, semi-structured interview |
| van der Sluis et al. (28) | 2016 | Cohort study | n = 9 |
29.6 years (17.2–34.3) |
58 (50–73) |
SHS, SWLS, CLLS |
| Weyers et al. (24) | 2009 | Cohort study | n = 50 | At least 6 months | 43.06 | SF-36, VAS |
| Yang et al. (25) | 2016 | Cross sectional study | n = 209 | Not available |
26.7 (18–45) |
SF-36 |
| Zimmermann et al. (21) | 2006 | Cross sectional study |
n = 40 (24 M–F and 16 F–M) |
3.1 years (0.5–19) |
38 (23–51; 41.0 years for M–F) |
FLZ |
Table 2. Quality characteristics of the studies.
|
Author (reference) |
Dropout rate | Reasons for dropout | Confounding variables | Estimated risk of bias (e3) |
| Ainsworth et al. (22) |
— | — | n = 25 (10.12%) M–F*1 had sex reassignment surgery n = 47 (19.02%) had sex reassignment surgery and facial feminization surgery n = 28 (11.3%) had facial feminization surgery n = 147 (59.51%) had no surgery Time of survey not stated, hormone therapy |
Moderate to high: selection bias, classification bias, bias owing to deviations in interventions |
| Bouman et al. (27) |
20.51% | Non-respondents n = 6 (15.38%) Lost to follow-up n = 1 (2.56%) Deceased n = 1 (2.56%) |
27 M–F (= 87.1%) completed the QoL questionnaire, hormone therapy | Moderate to high: selection bias |
| Cardoso da Silva et al. (26)*2 |
75.26%*3 (n= 30 M–F [15.7%] excluded) |
— | Dropout rate very high, no reasons given 31 M–F (65.95%) had corrective surgery, hormone therapy |
Moderate to high: selection bias, attrition bias |
| Castellano et al. (17) |
11.76% | Non-respondents n= 8 (11.76%) | Only the domain general quality of life score and subdomains ‧sexuality and body were requested, hormone therapy | Moderate to high: selection bias Moderate: detection bias |
| Jokic-Begic et al. (18) |
25% | Lost to follow-up n = 1 (12.5%) Refused participation n = 1 (12.5%) |
Very small study population, socioeconomic and clinical circumstances, psychotherapy, hormone therapy | Moderate to high: selection bias |
| Kuhn et al. (19) |
— | — | No detail on interventions in the control group,no separate data analysis for M–F and F–M, hormone therapy | Moderate to high: selection bias, bias owing to deviations in interventions |
| Lindqvist et al. (23)*2 |
77.37%*4 | Deceased or moved without changing address and entry in residents‘ register | Very high dropout rate, only 17 patients completed the questionnaire at all 4 follow-up points, hormone therapy | Moderate to high: selection bias, attrition bias |
| Papadopulos et al. (29) |
61.15% | Unavailable/incorrect phone number n = 38 (31.40%) Refused participation n = 14 (11.57%) Quesionnaire not completed n = 22 (18.18%) |
Inclusion criteria: only patients who had had corrective surgery or those who did not require such surgery, hormone therapy | Moderate to high: selection bias |
| Parola et al. (20) |
— | — | Hormone therapy | Moderate to high: selection bias |
| van der Sluis et al. (28) |
62.5% | Non-respondents n = 6 (25%) Lost to follow-up n = 3 (12.5%) Deceased n = 5 (20.84%) Refused participation n = 1 (4.16%) |
Small study population Secondary vaginoplasty Hormone therapy |
Moderate to high: selection bias |
| Weyers et al. (24) |
28.57% | Non-respondents n= 17 (24.29%) Refused participation n=3 (4.29%) |
Hormone therapy | Moderate to high: selection bias |
| Yang et al. (25) |
— | — | n = 73 (34.92%) had facial feminization surgery n = 43 (20.57%) had breast augmentation surgery Only n = 4 (1.91%) had sex reassignment surgery Socioeconomic and clinical circumstances Hormone therapy in only n = 37 (17.7%) |
Moderate to high: selection bias, bias owing to deviations in interventions |
| Zimmermann et al. (21) |
55.56% | Non-respondents n = 45 (50%) Incomplete questionnaire n = 3 (3.34%) Inclusion criteria not met n = 2 (2.23%) |
Absolute values from FLZ questionnaire not shown, only p-values reported, no separate evaluation of FLZ questionnaire for F–M and M–F, hormone therapy | Moderate to high: selection bias |
*1 M–F male to female; F–M female to male, reassignment surgery
*2 Prospective study design
*3 Of originally 190 participants, n = 160 (84.21%) completed the questionnaire preoperatively and n = 47 (24.73%) postoperatively
*4 Out of a total of 190 study participants, n = 146 (76.84%) completed the questionnaire preoperatively, n = 108 (56.84%) 1 year postoperatively, n = 64 (33.68%) 3 years postoperatively, and n = 43 (22,63%) 5 years postoperatively. Most of the 190 participants completed the questionnaire at least at two follow-up points.
Results
The studies made use of the following instruments:
6 studies used the Short Form 36 Health Survey (SF-36) (18, 20, 22– 25);
2 studies used the World Health Organization’s Quality of Life 100 questionnaire (WHOQOL-100) (17, 26);
2 studies used the Subjective Happiness Scale (SHS) in combination with the Satisfaction with Life Scale (SWLS) and the Cantrils Ladder of Life Scale (CLLS) (27, 28);
2 studies used the FLZ questionnaire (Fragebogen zur Lebenszufriedenheit) (21, 29); and
1 study used the King’s Health Questionnaire (KHQ) (19).
None of the questionnaires constitutes an investigative tool that is specifically tailored to trans persons. Table 3 shows the result scales. Table 2 shows the confounding variables and, as far as it is possible to assess this, the risk of bias.
Table 3. Simplified result scales of the SF-36, WHOQOL-100, SHS, SWLS, and CLLS instruments*.
| Questionnaire | Composition of score values | Minimum value | Maximum value |
| SF-36 (18, 20, 22– 25) | 36 items | 0 | 100 |
| WHOQOL-100 (26, 17) | 100 items | 0 | 100 |
| SHS (35– 37) | VAS, 4 items on a 7 point Likert scale | 4 | 28 |
| SWLS (35– 37) | VAS, 5 items on a 7 point Likert scale | 5 | 35 |
| CLLS (35– 37) | VAS, short scale (L-1) | 0 | 10 |
*For the studies referenced in parentheses, it was not possible to calculate effect sizes
Quality of life
The SF-36 and WHOQOL-100 are validated, reliable and disease–non-specific instruments for measuring health-related quality of life (30, 31). They can be used to gain information on the individual health status and allow for observing disease-related stresses over time. The questionnaires collect data on numerous aspects of daily life, which in their totality reflect quality of life. They are used internationally and therefore make cross-cultural studies an option (32).
Studies that used the SF-36 to answer the question of postoperative quality of life (18, 20, 22– 25) observed after sex reassignment surgery an improvement in “social functioning”, “physical” and “emotional role functioning”, “general health perceptions”, “vitality”, and “mental health” (p = 0.025 to p >0.05). In two of these studies (22, 24), “mental health” in trans women after sex reassignment surgery did not differ significantly from the standard sample. This explains the formally non-significant result. Ainsworth and Spiegel (22) showed that trans women without surgical intervention when compared indirectly with cis women from the SF-36 standard sample reported significantly poorer “mental health” (39.5 vs 48.9; p <0.05). Lindqvist et al. (23) and Weyers et al. (24) found an improvement in “self-perceived health” in the first postoperative year (p <0.05 and p <0.009), which deteriorated later but did not fall as low as its original score (p <0.0001). Furthermore, the studies concluded that “physical pain” increased postoperatively and “physical functioning” decreased; the postoperative follow-up periods varied between 3 months (18) and 5 years (23). According to Lindqvist et al. (23), “physical pain” in trans women five years postoperatively was comparable to that in the standard population (72.5 vs 72.7; SD 26.5).
Studies that used the WHOQOL-100 came up with the following results: Cardoso da Silva et al. (26) observed postoperatively an increase in “sexual activity” (p = 0.000) compared with the preoperative evaluation (prospective study design). Furthermore they found a postoperative improvement in the “psychological domain” (p = 0.041) and “social relationships” (p = 0.007), but a deterioration in “physical health” (p = 0.002) and “independence” (p = 0.031). Accordingly, deteriorations were seen in the areas of “energy” and “fatigue”, “sleep”, “negative feelings”, “mobility”, and “activities of daily living” (p <0.05). Castellano et al. (17) found after sex reassignment surgery for the group of trans women compared with the group of cis women no significant differences relating to “sexual activity” (65.85 vs 66.28; p >0.05), “body image” (64.64 vs 65.47; p >0.05), and the “quality of life score” (67.87 vs 69.49; p >0.05).
Quality of life and urinary incontinence
The King’s Health Questionnaire (KHQ) is a validated questionnaire for evaluating the impact of urinary incontinence on quality of life (33), a topic of central importance for trans persons (34). This questionnaire interrogates the quality of life domains always in association with urinary incontinence as the main problem. Kuhn et al. (19) showed that “general health” in trans persons was experienced as poorer to a relevant extent (Cohen’s d = 4.126; p = 0.019), and “physical” (d = -7.972; p <0.0001) and “personal limitations” (d = -7.016; p <0.001) were experienced to a greater extent. In contrast to this, trans persons felt less limited in terms of “role limitation” (d = 3.311; p = 0.046). For “emotions”, “sleep”, “incontinence”, and “symptom severity”, the differences to the control group did not reach significance. The control group consisted of cis women who had undergone abdominopelvic surgery. The evaluation of the visual analogue scale (VAS) showed a lower (d = 14.136; p <0.0001) degree of general life satisfaction in the group of trans persons.
Life satisfaction
The SHS (35), SWLS (36), and CLLS (37) are validated and internationally used visual analogue scales to evaluate life satisfaction. The SHS evaluates individual happiness and associated physical, mental, and social wellbeing (35). The SWLS was used as a short-form scale in the cited studies (also known as L-1) and included only the question on general life satisfaction (36). The CLLS evaluates emotional wellbeing associated with life satisfaction as well as subjective health (37).
Studies that used the SHS, SWLS, and CLLS (27, 28) to evaluate postoperative life satisfaction reported a high degree of “subjective happiness” (5.6; SD 1.4 and 5.9; SD 0.6), of “satisfaction with life“ (27.7; SD 5.8 and 27.1; SD 2.1) and “subjective wellbeing” (8.0 [range: 4–10] and 7.9; SD 0.7) in trans women after intestinal vaginoplasty. The studies cited earlier differ with regard to the following items: Bouman et al. (27) studied a population of young trans women (mean age: 19.1 years) with penoscrotal hypoplasia after primary laparoscopic intestinal vaginoplasty. The study participants had received puberty blockers during their transition therapy, which resulted in penoscrotal hypoplasia and made penile inversion vaginoplasty (box) impossible. Van der Sluis et al. (28) studied an older population (mean age: 58 years) of trans women after secondary intestinal vaginoplasty—that is, patients who required secondary intestinal reconstruction owing to vaginal stenosis or insufficient vaginal length after penile inversion vaginoplasty. The postoperative follow-up period varied between 1–7.5 years (27) and 17.2–34.3 years (28). In spite of the different patient populations, these studies found that sex reassignment surgery had a positive effect on life satisfaction.
The FLZ is a validated multidimensional questionnaire for evaluating individual general life satisfaction (38). It is used in life quality and rehabilitation research and enables the recording of changes if administered repeatedly. It is available in a German language version only; for this reason, its results apply only to German speaking populations.
Studies that used the FLZ questionnaire (21, 29) found that the postoperative life satisfaction of trans women in terms of “health” does not differ from that of the general population. Additionally, Papadopoulos et al. (29) found no differences for “friends”, “hobbies”, “income”, “work”, and “relationship.” A subanalysis of the module “health” found postoperatively in both studies a relevant decrease in “fitness” (d = 0.521; p <0.001) and “energy” (d = 0.494; p <0.003). Zimmerman et al. (21) additionally found a significant decrease in “ability to relax/equilibrium” (p = 0.002), “fearlessness/absence of anxiety” (p = 0.015), and “absence of discomfort/pain” (p = 0.037). Both studies (21, 29) were retrospective surveys that were undertaken once only in a time period between 6 months and 58 months postoperatively. Papadopoulos et al. (29) included only subjects into the study who did not require any further corrective surgery after sex reassignment surgery or who had already undergone a second procedure for the purpose of minor corrections.
Discussion
Two prospective studies documented postoperatively a notable improvement in quality of life (23, 26). Four studies found that the life quality of trans women after sex reassignment surgery was no different from that of cis women (17, 20, 22, 24). Sex reassignment surgery has also been shown to have a positive effect on life satisfaction (27, 28)—the exception was urinary incontinence, in which case life satisfaction dropped (19). Lindqvist et al. (23) and Weyers et al. (24) observed an improvement in self-perceived health in the first postoperative year, which then drops, albeit not all the way down to its original level. This is consistent with the honeymoon phase described by De Cuypere et al. (39), which has been described as a euphoric period in the first year after surgery. Several studies (18, 20– 25) showed that physical pain increased after surgery and physical functioning deteriorated. This is easily explained by the surgery itself, however; the postoperative follow-up periods in these studies varied between 3 months (18) and 5 years (23).
Altogether the study results imply that sex reassignment surgery has an overall positive effect on partial aspects, such as mental health, sexuality, life satisfaction, and quality of life.
These results were confirmed by Barone et al. (40) and Murad et al. (15) in their review articles, which were published in 2017 and 2010, respectively. Barone et al. (40) in a systematic review evaluated patient reported results after sex reassignment surgery; among others, regarding life satisfaction. Murad et al. (15) in a meta-analysis focused on quality of life and psychosocial health after hormone therapy (main aspect) and sex reassignment surgery. In sum, both studies found improvements in quality of life and life satisfaction after sex reassignment surgery, and an improvement at the psychosocial level. Hess et al. (11) concluded that the study participants benefited from sex reassignment surgery—they too found high rates of satisfaction postoperatively in Germany.
As sex reassignment surgery often constitutes the final step of sex reassignment measures, hormone therapy as well as accompanying psychotherapy may have had a confounding effect. Not all studies adjusted for confounding factors. A lack of randomization and control or the use of a matched control group (17, 19) in the studies also introduced methodological bias (table 2). Furthermore, the high dropout rates of 12% (17) to 77% (23) (median: 56%), which are mainly due to non-respondents, should be assessed critically. In our experience, however, the patient population of trans women is often reticent and is not interested in study participation because of personal reasons (“to not be reminded of that time”). Other authors have shared this observation (18, 24), which may also explain the occasionally high dropout rates. There is also the possibility that dissatisfied patients were among the dropouts. Owing to socioeconomic and clinical conditions, the studies from Croatia (18) and China (25) need to be evaluated separately. On the one hand, the authors of both studies draw attention to the public’s lack of awareness and understanding (and the associated psychological stress for trans women) in these countries, and, on the other hand, statutory sickness funds did not cover the costs of all treatments, which were therefore accessible to only few patients. This explains the notably lower participant numbers of 3 (18) and 4 (25) male-to-female transitions after sex reassignment surgery. None of the included studies reported potential suicide rates.
The strength of this review lies in the fact that we included only studies that used standardized questionnaires. Tests (such as the SF-36 or WHOQOL-100) represent validated and reliable measuring instruments, for some of which reference standard populations exist, and they enable international and intercultural comparison. Furthermore, standardized questionnaires have the advantage of a high degree of objectivity in terms of conducting, evaluating, and interpreting studies.
Conclusion
The available study data show that sex reassignment surgery has a positive effect on partial aspects—such as mental health/wellbeing, sexuality, and life satisfaction—as well as on quality of life overall.
It should be noted that the studies are almost exclusively retrospective analyses of mostly uncontrolled and small cohorts, for which no valid or specific measuring instruments are available to date. Because of the high dropout and non-response rates, the current data should be interpreted with caution.
In spite of the essentially positive results, the data are not satisfactory at this point in time. Due to the studies’ limited follow-up times, no conclusions can be drawn as yet about the long term consequences of such procedures. Furthermore, many studies did not use standardized questionnaires and/or scores, which makes comparisons between individual studies difficult.
Supplementary Material
eMETHODS
Additional points regarding the study method
We conducted a systematic key word guided literature search of four databases (PubMed, EMBASE, Web of Science, PsycINFO) in March 2017 in order to identify the current medical literature relating to our research question. Among the search terms we used were “transsexualism”, “reassignment surgery”, and “quality of life” (etable 1). The article search was adapted to the technical requirements (for example, the option of using MeSH terms) of each database and undertaken by GW and DGN independently, supported by the recommendations summarized in the PRISMA statement (16).
Inclusion criteria
We included only articles that focused on the topic of the quality of life of trans women who had had sex reassignment surgery, independently of the studies’ population sizes and publication dates. GW, RF, and DGN operationalized the search terms by using an iterative process following the PICO method (e1) (etable 1) and a search string was created with these (eTabelle 2). The search for publications intentionally identified only studies reported in English or German.
Exclusion criteria
Studies that did not exclusively focus on trans persons (for example, LGBT [= lesbian, gay, bisexual, and transgender] studies) or that did not evaluate quality of life by using a standardized questionnaire were not considered. Furthermore, this review did not include review articles, published dissertations, nor congress presentations/commentaries. Studies of trans persons who were under age were excluded too.
Screening process
During the study selection process we excluded according to the mentioned criteria those studies that were not able to contribute to answering our research question (figure). Furthermore, we searched the reference lists of all selected articles in order to be able to include further studies that were not found in the databases. This yielded four additional studies that met the inclusion criteria. In a parallel and independent process, DGN checked the results of this search. In cases where discrepancies were found, a solution pertaining to the inclusion of the relevant study was found by consensus.
Study analysis
After the study selection process we viewed full-text articles and collated important key study data (table 1). According to the definitions in the PICO scheme (e1) we collated all relevant parameters from the individual studies in further full-text reviews. The first author extracted the data, and DGN checked these in a second, independent process. All included articles are non-randomized studies of evidence level III (e2). Some studies (17– 21) reported on the quality of life of trans women as well as trans men. In these cases we ensured that the data evaluation for trans women was done separately or the ratio M–F/F–M was in favor of trans women. Where information was lacking or lack of clarity existed in individual studies, we contacted the authors. Table 2 shows the quality characteristics of the included studies.
Key messages.
Trans persons suffer from the tension between their biologically characterized body and their experienced sex/gender.
Undergoing medical and/or social transition seems for many trans persons the best possible solution for alleviating their gender dysphoria symptoms.
Results from studies imply that sex reassignment surgery on the one hand has positive effects in terms of partial aspects of quality of life, such as mental health, sexuality, and life satisfaction, and, on the other hand, on quality of life overall.
Because of the studies’ high dropout rates (12–77%; median 56%), the results should be interpreted with caution.
The studies did not include information on potential suicide rates.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Garcia Nuñez D, Nieder TO. Geschlechtsinkongruenz und -dysphorie. J Gynakol Endokrinol. 2017;15:5–13. [Google Scholar]
- 2.Meyer zu Hoberge S. Prävalenz, Inzidenz und Geschlechterverhältnis der Transsexualität anhand der bundesweit getroffenen Entscheidungen nach dem Transsexuellengesetz in der Zeit von 1991 bis 2000. www.macau.uni-kiel.de/receive/dissertation_diss_00004825?lang=de (last accessed on 20 September 2018) [Google Scholar]
- 3.Falkai P. Diagnostische Kriterien DSM-5®. Göttingen: Hogrefe. 2015 [Google Scholar]
- 4.Hage JJ, Karim RB. Ought GIDNOS get nought? Treatment options for nontranssexual gender dysphoria. Plast Reconstr Surg. 2000;105:1222–1227. doi: 10.1097/00006534-200003000-00063. [DOI] [PubMed] [Google Scholar]
- 5.Coleman E, Bockting W, Botzer M, et al. Standards of Care - Versorgungsempfehlung für die Gesundheit von transsexuellen, transgender und geschlechtsnichtkonformen Personen. www.wpath.org/site_page.cfm?pk_association_webpage_menu=1351&pk_association_webpage=43812012 (last accessed on 20 October 2017) [Google Scholar]
- 6.Fisher AD, Maggi M. Endocrine treatment of transsexual male-to-female persons Management of gender dysphoria. In: Trombetta C, Liguori G, Bertolotto M, editors. Springer. Milano: 2015. 86 pp. [Google Scholar]
- 7.Canner JK, Harfouch O, Kodadek LM, et al. Temporal trends in gender-affirming surgery among transgender patients in the united states. JAMA Surg. 2018;153:609–616. doi: 10.1001/jamasurg.2017.6231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Cuypere G, T‘Sjoen G, Beerten R, et al. Sexual and physical health after sex reassignment surgery. Arch Sex Behav. 2005;34:679–690. doi: 10.1007/s10508-005-7926-5. [DOI] [PubMed] [Google Scholar]
- 9.Klein C, Gorzalka BB. Sexual functioning in transsexuals following hormone therapy and genital surgery: a review. J Sex Med. 2009;6:2922–2939. doi: 10.1111/j.1743-6109.2009.01370.x. quiz 40-1. [DOI] [PubMed] [Google Scholar]
- 10.Gijs L, Brewaeys A. Surgical treatment of gender dysphoria in adults and adolescents: recent developments, effectiveness, and challenges. Annu Rev Sex Res. 2007;18:178–224. [Google Scholar]
- 11.Hess J, Rossi Neto R, Panic L, Rübben H, Senf W. Satisfaction with male-to-female gender reassignment surgery—results of a retrospec-tive analysis. Dtsch Arztebl Int. 2014;111:795–801. doi: 10.3238/arztebl.2014.0795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bolton MA, Pruzinsky T, Cash TF, Persing JA. Measuring outcomes in plastic surgery: body image and quality of life in abdominoplasty patients. Plast Reconstr Surg. 2003;112:619–625. doi: 10.1097/01.PRS.0000070972.57000.08. discussion 26-7. [DOI] [PubMed] [Google Scholar]
- 13.Sinno H, Dionisopoulos T, Slavin SA, Ibrahim AM, Chung KC, Lin SJ. The utility of outcome studies in plastic surgery. Plast Reconstr Surg Glob Open. 2014;2 doi: 10.1097/GOX.0000000000000104. e189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.White Hughto JM, Reisner S. A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgend Health. 2016;1:21–31. doi: 10.1089/trgh.2015.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murad M, Elamin M, Garcia M, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol. 2010;72:214–231. doi: 10.1111/j.1365-2265.2009.03625.x. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 17.Castellano E, Crespi C, Dell‘Aquila C, et al. Quality of life and hormones after sex reassignment surgery. J Endocrinol Invest. 2015;38:1373–1381. doi: 10.1007/s40618-015-0398-0. [DOI] [PubMed] [Google Scholar]
- 18.Jokic-Begic N, Korajlija A, Jurin T. Psychosocial adjustment to sex reassignment surgery: a qualitative examination and personal experiences of six transsexual persons in Croatia. Sci. World J. 2014;2014 doi: 10.1155/2014/960745. 960745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuhn A, Bodmer C, Stadlmayr W, Kuhn P, Mueller MD, Birkhäuser M. Quality of life 15 years after sex reassignment surgery for transsexualism. Fertil Steril. 2009;92:1685–1689. doi: 10.1016/j.fertnstert.2008.08.126. [DOI] [PubMed] [Google Scholar]
- 20.Parola N, Bonierbale M, Lemaire A, Aghababian V, Michel A, Lançon C. Study of quality of life for transsexuals after hormonal and surgical reassignment. J Sexol. 2010;19:24–28. [Google Scholar]
- 21.Zimmermann A, Zimmer R, Kovacs L, et al. Transsexuals‘ life satisfaction after gender transformation operations. Chirurg. 2006;77:432–438. doi: 10.1007/s00104-005-1138-3. [DOI] [PubMed] [Google Scholar]
- 22.Ainsworth TA, Spiegel JH. Quality of life of individuals with and without facial feminization surgery or gender reassignment surgery. Qual Life Res. 2010;19:1019–1024. doi: 10.1007/s11136-010-9668-7. [DOI] [PubMed] [Google Scholar]
- 23.Lindqvist EK, Sigurjonsson H, Möllermark C, Rinder J, Farnebo F, Lundgren TK. Quality of life improves early after gender reassignment surgery in transgender women. Eur J Plast Surg. 2017;40:223–226. doi: 10.1007/s00238-016-1252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weyers S, Elaut E, De Sutter P, et al. Long-term assessment of the physical, mental, and sexual health among transsexual women. J Sex Med. 2009;6:752–760. doi: 10.1111/j.1743-6109.2008.01082.x. [DOI] [PubMed] [Google Scholar]
- 25.Yang X, Zhao L, Wang L, et al. Quality of life of transgender women from China and associated factors: a cross-sectional study. J Sex Med. 2016;13:977–987. doi: 10.1016/j.jsxm.2016.03.369. [DOI] [PubMed] [Google Scholar]
- 26.Cardoso da Silva D, Schwarz K, Fontanari AM, et al. WHOQOL-100 before and after sex reassignment surgery in brazilian male-to-female transsexual individuals. J Sex Med. 2016;13:988–993. doi: 10.1016/j.jsxm.2016.03.370. [DOI] [PubMed] [Google Scholar]
- 27.Bouman MB, van der Sluis WB, van Woudenberg Hamstra LE, et al. Patient-reported esthetic and functional outcomes of primary total laparoscopic intestinal vaginoplasty in transgender women with penoscrotal hypoplasia. J Sex Med. 2016;13:1438–1444. doi: 10.1016/j.jsxm.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 28.van der Sluis WB, Bouman MB, de Boer NK, et al. Long-term follow-up of transgender women after secondary intestinal vaginoplasty. J Sex Med. 2016;13:702–710. doi: 10.1016/j.jsxm.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 29.Papadopulos NA, Lellé JD, Zavlin D, et al. Quality of life and patient satisfaction following male-to-female sex reassignment surgery. J Sex Med. 2017:721–730. doi: 10.1016/j.jsxm.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 30.Morfeld M, Kirchberger I, Bullinger M. Fragebogen zum Gesundheitszustand (SF-36) Göttingen: Hogrefe. 2011 [Google Scholar]
- 31.Gunzelmann T, Brähler E, Angermeyer C, Kilian R, Matschinger H. Deutschsprachige Version der WHO Instrumente zur Erfassung von Lebensqualität WHOQOL-100 und WHOQOL-BREFM. Z med Psychol. 2002:44–48. [Google Scholar]
- 32.Lehmann I. Procedures to measure quality of life. Z med Psychol. 2007;16:5–23. [Google Scholar]
- 33.Bjelic-Radisic V, Dorfer M, Tamussino K, et al. Der King‘s Fragebogen zur Erfassung der Lebensqualität von Patientinnen mit Harninkontinenz (deutsche Version) Geburtshilfe Frauenheilkd. 2005;65:1042–1050. [Google Scholar]
- 34.Kuhn A, Hiltebrand R, Birkhauser M. Do transsexuals have micturition disorders? Eur J Obstet Gynecol Reprod Biol. 2007;131:226–230. doi: 10.1016/j.ejogrb.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 35.Swami V, Stieger S, Voracek M, Dressler S, Eisma L, Furnham A. Psychometric evaluation of the tagalog and German Subjective Happiness Scales and a cross-cultural comparison. Soc Indic Res. 2009;93 [Google Scholar]
- 36.Glaesmer H, Grande G, Braehler E, Roth M. The German version of the Satisfaction with Life Scale (SWLS): Psychometric properties, validity, and population-based norms. Eur J Psychol Assess. 2011;27:127–132. [Google Scholar]
- 37.Levin K, Currie C. Reliability and validity of an adapted version of the Cantril Ladder for use with adolescent samples. Soc Indic Res. 2014;119 [Google Scholar]
- 38.Fahrenberg J, Myrtek M, Schuhmacher J, Brähler E. Fragebogen zur Lebenszufriedenheit (FLZ) Göttingen: Hogrefe. 2000 [Google Scholar]
- 39.De Cuypere G, Elaut E, Heylens G, et al. Long-term follow-up: psychosocial outcome of Belgian transsexuals after sex reassignment surgery. Sexologies. 2006;15:126–133. [Google Scholar]
- 40.Barone M, Cogliandro A, Di Stefano N, Tambone V, Persichetti P. A systematic review of patient-reported outcome measures following transsexual surgery. Aesthetic Plast Surg. 2017;41:700–713. doi: 10.1007/s00266-017-0812-4. [DOI] [PubMed] [Google Scholar]
- E1.Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. 2007;7 doi: 10.1186/1472-6947-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E2.Oxford Uo. CEBM Levels of Evidence 2011. www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf (last accessed on 25 November 2018) [Google Scholar]
- E3.Cochrane Deutschland, Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften - Institut für Medizinisches Wissensmanagement. „Bewertung des Biasrisikos (Risiko systematischer Fehler) in klinischen Studien: ein Manual für die Leitlinienerstellung“. 1st edition 2016. www.cochrane.de/de/rob-manual; AWMF: www.awmf.org/leitlinien/awmf-regelwerk/ll-entwicklung.html (last accessed on 30 November 2018) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMETHODS
Additional points regarding the study method
We conducted a systematic key word guided literature search of four databases (PubMed, EMBASE, Web of Science, PsycINFO) in March 2017 in order to identify the current medical literature relating to our research question. Among the search terms we used were “transsexualism”, “reassignment surgery”, and “quality of life” (etable 1). The article search was adapted to the technical requirements (for example, the option of using MeSH terms) of each database and undertaken by GW and DGN independently, supported by the recommendations summarized in the PRISMA statement (16).
Inclusion criteria
We included only articles that focused on the topic of the quality of life of trans women who had had sex reassignment surgery, independently of the studies’ population sizes and publication dates. GW, RF, and DGN operationalized the search terms by using an iterative process following the PICO method (e1) (etable 1) and a search string was created with these (eTabelle 2). The search for publications intentionally identified only studies reported in English or German.
Exclusion criteria
Studies that did not exclusively focus on trans persons (for example, LGBT [= lesbian, gay, bisexual, and transgender] studies) or that did not evaluate quality of life by using a standardized questionnaire were not considered. Furthermore, this review did not include review articles, published dissertations, nor congress presentations/commentaries. Studies of trans persons who were under age were excluded too.
Screening process
During the study selection process we excluded according to the mentioned criteria those studies that were not able to contribute to answering our research question (figure). Furthermore, we searched the reference lists of all selected articles in order to be able to include further studies that were not found in the databases. This yielded four additional studies that met the inclusion criteria. In a parallel and independent process, DGN checked the results of this search. In cases where discrepancies were found, a solution pertaining to the inclusion of the relevant study was found by consensus.
Study analysis
After the study selection process we viewed full-text articles and collated important key study data (table 1). According to the definitions in the PICO scheme (e1) we collated all relevant parameters from the individual studies in further full-text reviews. The first author extracted the data, and DGN checked these in a second, independent process. All included articles are non-randomized studies of evidence level III (e2). Some studies (17– 21) reported on the quality of life of trans women as well as trans men. In these cases we ensured that the data evaluation for trans women was done separately or the ratio M–F/F–M was in favor of trans women. Where information was lacking or lack of clarity existed in individual studies, we contacted the authors. Table 2 shows the quality characteristics of the included studies.