Abstract
Flow diverter malapposition has been described as a technical complication during endovascular procedures and can be associated with, potentially delayed, life-threatening aneurysm rupture or ischemic events.
We performed a retrospective review of our flow diverter database to identify all patients in whom device malapposition was detected on follow-up angiogram immediately after device deployment. Feasibility and technical success of different endovascular approaches aiming to correct the inadequate vessel wall apposition were evaluated. Successful endovascular techniques for manipulation of the flow diverter included use of wires, catheters and additional flow diverter/stent devices.
In our practice, we found six successful endovascular techniques for device manipulation, which allowed us to safely achieve good flow diverter wall apposition.
Keywords: Wall apposition, flow diverter, aneurysm, malapposition, stent, balloon angioplasty
Introduction
Flow diversion technology is an elegant endovascular approach, which, after placement of the device across the aneurysm neck, aims to redirect blood flow away from the aneurysm and over time results in complete aneurysm occlusion and parent vessel remodeling.
Proper wall apposition of the device is essential for adequate modification of the blood inflow pattern, which will progress from reduced inflow to stagnation of flow and ultimately to aneurysm obliteration. In addition, it prevents endoleaks.
Potential complications of flow diverter malapposition include delayed stroke related complications due to device migration and delayed aneurysm rupture due to failure to achieve stable intrasaccular thrombus formation.1–7
There are no clear guidelines for the management of inadequate flow diverter wall apposition but the neurointerventionalist should consider device malapposition as a source for potential life-threatening complications.
Here, we describe our endovascular techniques for manipulation of flow diverters in order to achieve good vessel wall apposition.
Methods
We retrospectively analyzed our neurointerventional database for all patients who were treated with the pipeline embolization device (PED) and in whom malapposition of the device was detected on follow-up angiography immediately after device deployment and prior to completion of the endovascular procedure.
We then evaluated technical success and feasibility of different endovascular approaches aimed to correct the inadequate vessel wall apposition.
Successful endovascular techniques for manipulation of the device included use of wires, catheters and additional placement of flow diverters/stents.
Proper wall apposition of the device was confirmed with 3D multiplanar cone-beam computed tomography reconstruction images (Vaso-CT) prior to completion of the interventional procedure.
Results
A total of 215 procedures were performed between March 2011 and May 2018.
Balloon angioplasty was needed in 27 cases, 9 cases had additional stents placed and 2 patients had a second PED implanted for malapposition. We only used one corrective attempt per case. The corrective attempt was successful in all cases which was confirmed with Vaso-CT. We neither observed any technical complications related to the different techniques described nor any symptomatic complications affecting patient outcome.
We identified six successful endovascular techniques, which can be used to achieve better flow diverter wall apposition:
Use of a wire with a J-, pigtail- or S-shaped tip
In case of incomplete opening of the device, the tip of a wire can be passed through the device in a back and forth motion in order to fully expand it. Passing the wire through the narrowed (incompletely opened) portion of the device can help the braided device to open up and conform to the vessel wall. Care should be taken to use a high quality roadmap to ascertain that the wire is within the device and does not extend between the vessel wall and the device or subintimal.
Manipulation with a microcatheter
It is important not to lose access after deployment of the flow diverter, especially in an incompletely open device. The distal pusher wire can be re-accessed when pushing the microcatheter over the delivery wire. The vessel curvature can be used to push the microcatheter against it and press the flow diverter against the vessel wall. Afterwards, the delivery system can be safely removed. Care should be taken in order to avoid damage to the cut edge of the braid (entanglement) during catheter-mediated maneuvers.
Manipulation with an intermediate catheter
The new intermediate catheters, such as the Catalyst 5 (Stryker Neurovascular, Fremont, CA, USA) or Navien (Covidien Vascular Therapies, Mansfield, MA, USA) are more navigable while being relatively atraumatic and can be advanced further distally into the cervical and intracranial vasculature.
The intermediate catheter can be used to climb into the device over the delivery microcatheter. The intermediate catheter can then be used to “bump” the device along the outer curvatures for better device opening and wall apposition (Figure 1).
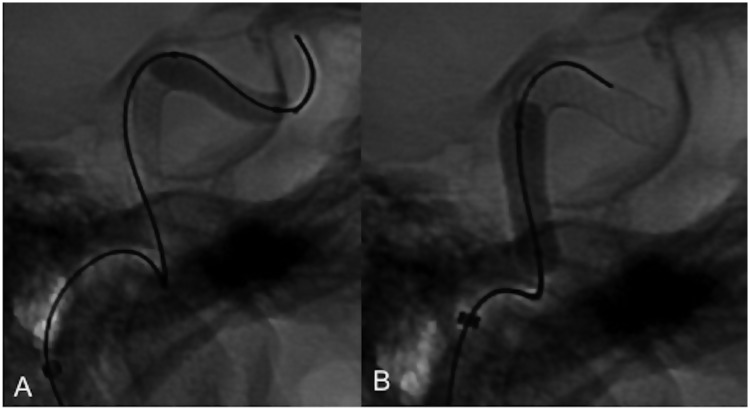
Figure 1.
Guide catheter. An intracranial guide catheter can be used to help appose the proximal edges of the pipeline embolization device by sliding the catheter along the edges of the device and pressing them against the vessel wall.
Secondly, the ledge between the intermediate catheter and the delivery system can sometimes be used to push the proximal edge of the device. This is especially useful in the occasionally capacious cavernous segment of the internal carotid artery.
Balloon angioplasty
Balloon angioplasty can be used to better appose the flow diverter to the vessel wall. This is especially useful at the aneurysm neck where attaining proper wall apposition is key to good occlusion outcomes. Caution should be taken while performing balloon angioplasty as it might foreshorten the device and cause device migration. In precarious situations, it is advisable to perform first an angioplasty and embed the most precariously placed segment of the device. Caution should be taken not to do an angioplasty outside the confines of the device to prevent vascular damage. Usually compliant/semi-compliant balloons are used for the purposes of attaining better wall apposition. This is different from the need for non-compliant balloons to open a semi-twisted or torqued device. The use of balloons is for better wall apposition for appropriately sized devices (Figure 2(a) and (b)); they do not compensate for undersized devices.
Placement of a second flow diverter in telescopic fashion
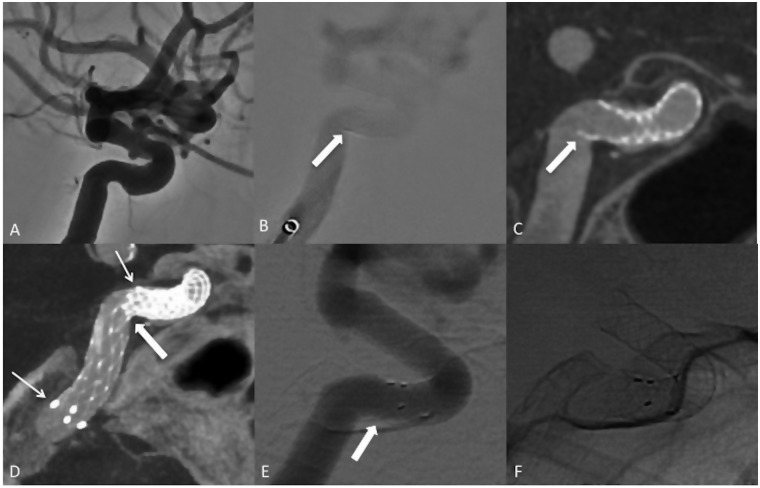
Figure 2.
Balloon angioplasty. Balloon angioplasty can be used to better appose the distal (a) or proximal (b) edges of a pipeline embolization device.
Placement of a second PED can be considered in certain cases. The second PED will be then placed in telescopic fashion into the first device. Given the significant amount of metal coverage at the site of device overlap, this technique might not be possible in the perforator rich regions due to risk of vessel occlusion. Also, placement of a second flow diverter is a relatively costly undertaking.
Placement of a telescoping open-cell stent
Similar to placement of a second flow diverter, the stent is placed in a telescopic fashion either overlapping the proximal or distal portion of the PED or jailing the unopposed edge against the vessel wall. The open-cell design and high outward radial force are favorable physical properties of the stent, which allow for jailing of the malappositioned portion of the flow diverter but also for maintaining adequate wall apposition of the stent itself (Figure 3(a) to (f)).
Figure 3.
Open-cell stent. Left ophthalmic and superior hypophyseal artery aneurysms (a). Device malapposition at the proximal aspect of the pipeline embolization device (PED) (b, arrow). Malapposition of the PED detected on cone-beam computed tomography images post device placement (c, arrow). Confirmed overlap of the proximal to mid portion of the open-cell stent (d, thin arrows) with the proximal aspect of the PED on multiplanar 3D reconstruction images acquired after stent placement. Resolution of the previously seen malapposition (d, thick arrow). Despite the PED remaining partly incompletely apposed, the main goal of apposing the proximal tip of the device was achieved so that it no longer protrudes into the vessel and potentially acts as a source for thromboembolic complications. The chronic outward radial force of the laser cut stent was on a 1.5-year follow-up enough to attain better wall apposition with the flow diverter (e and f, arrow in e).
Conclusions
Flow diverter malapposition can be successfully and safely addressed by the neurointerventionalist prior to completion of the interventional procedure using a variety of endovascular techniques.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Chalouhi N, Satti SR, Tjoumakaris S, et al. Delayed migration of a pipeline embolization device. Neurosurgery 2013; 72: 229–234. [DOI] [PubMed] [Google Scholar]
- 2.Chalouhi N, Tjoumakaris SI, Gonzalez LF, et al. Spontaneous delayed migration/shortening of the pipeline embolization device: report of 5 cases. AJNR Am J Neuroradiol 2013; 34: 2326–2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen JE, Gomori JM, Moscovici S, et al. Delayed complications after flow-diverter stenting: reactive in-stent stenosis and creeping stents. J Clin Neurosci 2014; 21: 1116–1122. [DOI] [PubMed] [Google Scholar]
- 4.Heller R, Calnan DR, Lanfranchi M, et al. Incomplete stent apposition in Enterprise stent-mediated coiling of aneurysms: persistence over time and risk of delayed ischemic events. J Neurosurg 2013; 118: 1014–1022. [DOI] [PubMed] [Google Scholar]
- 5.Lubicz B, Collignon L, Raphaeli G, et al. Flow-diverter stent for the endovascular treatment of intracranial aneurysms: a prospective study in 29 patients with 34 aneurysms. Stroke 2010; 41: 2247–2253. [DOI] [PubMed] [Google Scholar]
- 6.Pierot L, Wakhloo AK. Endovascular treatment of intracranial aneurysms: current status. Stroke 2013; 44: 2046–2054. [DOI] [PubMed] [Google Scholar]
- 7.Rahal JP, Dandamudi VS, Heller RS, et al. Use of concentric Solitaire stent to anchor Pipeline flow diverter constructs in treatment of shallow cervical carotid dissecting pseudoaneurysms. J Clin Neurosci 2014; 21: 1024–1028. [DOI] [PubMed] [Google Scholar]