Abstract
Regional anesthesia and pain management have experienced advances in recent years, especially with the advent of fascial plane blocks. The erector spinae plane block is one of the newest techniques to be described. In the past two years, publications referring to ESP block have increased significantly. The objective of this review is to analyze the articles about ESP block that have been published to date. We performed a search in the main databases and identified 368 articles. After a selection of the relevant articles, 125 studies were found eligible and were included in the review. The ESP block is performed by depositing the local anesthetic in the fascial plane, deeper than the erector spinae muscle at the tip of the transverse process of the vertebra. Many cases of its use have been described with satisfactory results in the treatment of both acute pain and chronic pain. The applicability of the technique covers many clinical scenarios. Of the 98 case reports reviewed, 12 and 87 articles, respectively described the technique as a treatment for chronic pain and acute pain. The single-shot was the most frequently used technique. As described in the articles published to date, the technique is easy to perform and has a low rate of complications. However, despite the effectiveness of the technique, further studies are necessary to obtain more evidence of its actions.
Keywords: Erector spinae plane block, ESP block, Fascial plane block, Pain, Regional anesthesia
Introduction
Fascial plane blocks are techniques used to manage pain, both in the perioperative period and in the treatment of chronic pain. In recent years, different types of fascial blocks have been described and there has been an increase in their clinical applications. The main advantages offered by these techniques include the ease of performing them, the analgesic efficacy, and the low risk of complications. One of the newest techniques that have been described recently is the erector spinae plane (ESP) block. It was first described by Forero et al. [1] in 2016 for the treatment of chronic thoracic neuropathic pain and postoperative pain in thoracic surgery. Since then, many articles have been published describing the application of the technique for a wide variety of clinical scenarios. The objective of this review is to analyze the articles about ESP block that have been published to date. Through the study of these articles, we intend to describe its procedural technique, indications, effectiveness, and possible complications in the different scenarios reported.
Anatomy
The erector spinae muscle (ESM) is a complex formed by the spinalis, longissimus thoracis, and iliocostalis muscles that run vertically in the back (Fig. 1). The ESP block is performed by depositing the local anesthetic (LA) in the fascial plane, deeper than the ESM at the tip of the transverse process of the vertebra. Hence, LA is distributed in the cranio-caudal fascial plane one dermatome a median of each 3.4 ml of injected volume [2]. Additionally, it diffuses anteriorly to the paravertebral and epidural spaces, and laterally to the intercostal space at several levels [3–5]. The LA exerts its effect on the ventral and dorsal ramus of the spinal nerve. The ventral ramus (intercostal nerve) is divided into the anterior and lateral branches. Its terminal branches provide the sensory innervation of the entire anterolateral wall. The dorsal ramus is divided into 2 terminal branches and it gives the sensory innervation to the posterior wall. Furthermore, the diffusion of LA to the paravertebral space through the costotransverse foramina and the intertransverse complex (intertransverse and costotransverse ligaments: levators, rotators, and intercostal muscles) provides both visceral and somatic analgesia. This diffusion into the epidural space and the neural foramina has been reported in anatomical studies that examined 2 to 5 vertebral levels that were centered near the injection site. However, this diffusion was not observed consistently in all cadaver studies.
Fig. 1.
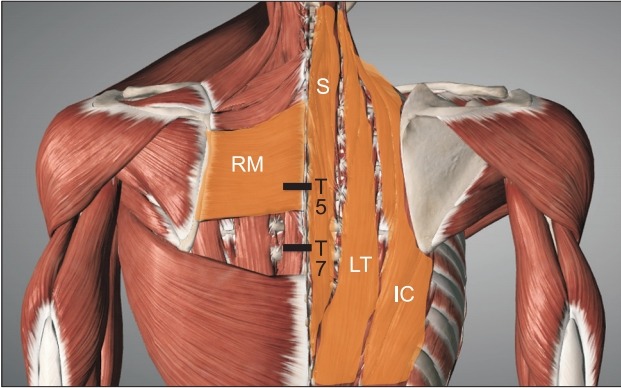
Anatomy of the erector spinae muscle. RM: Rhomboid major muscle; Erector spinae muscle (spinalis [S], longissimus thoracis [LT], and iliocostalis [IC]), T7: Thoracic vertebral 7, T5: Thoracic vertebral 5.
Technique
The position of the patient for the realization of the block includes: sitting, lying on the side, or lying prone. The technique can be performed with the patient awake or under the effects of general anesthesia. In pediatric patients, it is advisable to perform the procedure after the induction of anesthesia. However, there is no consensus about the best method for adult patients. The awake technique provides the advantage of being able to assess the efficacy and level of analgesia by means of a skin sensitivity test. However, the poor correlation between analgesia and skin sensitivity has been reported [6].
Although cases of blind puncture or under fluoroscopy have been described [7], the technique is usually guided by ultrasound. Usually, a high-frequency linear ultrasound transducer is used to block the thoracic level, and a convex transducer is used to block the lumbar level. The probe is placed in a transverse orientation to identify the spinous process. Once the level is identified, the probe is moved 3 cm laterally until the transverse process is identified. The probe should be rotated 90 degrees on the transverse process by placing it in a parasagittal plane. Three muscles must be identified as superficial to the hyperechoic transverse process shadow, and they include the trapezius, rhomboid major, and erector spinae (Fig. 2). These three muscles are visualized at the level of the fifth thoracic vertebra (standard level for a thoracic block); however, the rhomboid major muscle disappears at the level of the seventh thoracic vertebra (in lower blocks). The needle is inserted in the plane. The procedure can be performed in the cranio-caudal or opposite direction depending on the conditions and the region to be treated. Moreover, the block can be administered by a single shot or with a catheter insertion for continuous infusion; with the target as the transverse process. A hydrodissection should also be carried out with saline solution, and the local anesthetic must be deposited in the fascial plane, deeper than ESM at the tip of the transverse process of the vertebra (Fig. 3).
Fig. 2.
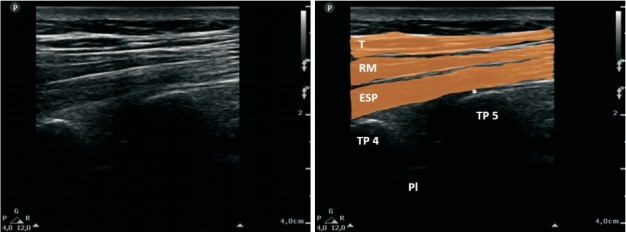
Sonoanatomy of the ESP block at T5 level. TP: transverse process, T: trapezius, RM: Rhomboid major, ESP: erector spinae, Pl: Pleura. *Needle tip place.
Fig. 3.
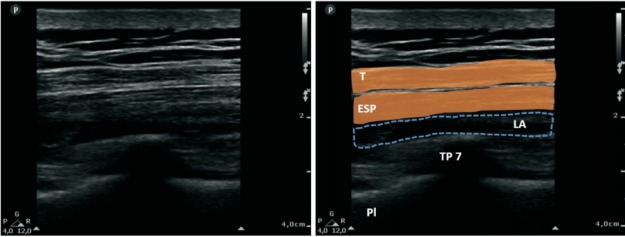
Sonoanatomy of ESP block at T7 level with LA diffusion shown in the dashed area. T: trepezius, ESP: erector spinae, LA: local anesthetic, TP: transverse process, Pl: pleura.
Materials and Methods
This is a narrative review. We performed a literature search for articles related to the ESP block in Medline, PubMed, Cochrane Library, and Google Scholar. The search period was from January 1, 2016, to December 1, 2018. The inclusion criteria were the articles related to ESP block that were identified in the search; these articles included letters to the editor, commentaries, case reports, case series, cadaver studies, observational studies, reviews, and clinical trials in adult and pediatric patients. The exclusion criteria included non-English language articles, duplicates articles, animal studies, irrelevant articles or articles that were not related to the ESP block. The search terms used included: “Erector Spinae Plane Block,” “ESP block,” and “Erector Spinae block.”
Initially, we identified 368 articles, out of which 233 articles were excluded because they were duplicates; however, 4 additional articles were identified from a different source and included in the review. Of the 139 remaining articles, 2 were excluded after reading the abstracts [126,127] which revealed that they were not related to ESP blocks. One was a review of adjuvant nerve blocks, and the other was an anatomical study of a different type of block. We eventually completed the reading of 137 articles, out of which 12 were excluded [128–139] for their irrelevance for this review. Finally, 125 studies were included in this review (Fig. 4). The data extracted in the case reports includes the following: type of pain and painful region, intervention performed, number of subjects treated, level of realization of blockage, use of catheter or single shot, unilateral or bilateral, local anesthetic used, average numerical rating scale (NRS) for pain, and presence of complications and other relevant observations. The average NRS included in the table was calculated by calculating the mean of the first NRS value reported in each case (in the cases where the pain was described in the first 12 hours post-block). The most relevant findings from clinical trials and observational studies are described in the results.
Fig. 4.
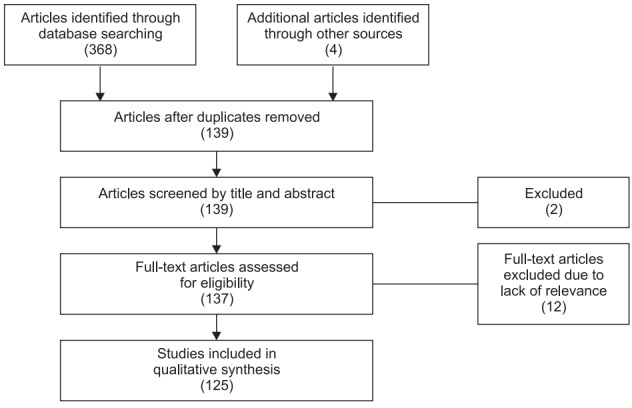
Algorithm of the different phases of articles inclusion criteria in the review.
Results
The 125 articles finally included in this review included: 6 randomized controlled trials [104–109], 1 consecutive controlled before-and-after study [110], 2 observational studies [111,112], 3 review articles [2,113,121], 5 anatomical studies [3–5,124,125], 98 case reports [1,7–103], and 10 opinion articles [6,114–120,122–126]. The case reports are described in Table 1 [1,7–103]. All case reports included a total of 211 patients in 98 articles. Of these case reports, 12 and 87 articles respectively described the technique as a treatment for chronic pain and acute pain. However, both scenarios described cases where the block was utilized for therapy at the cervical level, upper limbs, thoracic level, abdominal level, and lower limbs. The single-shot technique was most frequently used, while the most commonly used local anesthetics were bupivacaine and ropivacaine. The mean NRS for analgesia measurement reported in all cases was ≤ 3, and the only complications described were incomplete analgesia, pneumothorax, and motor blockade.
Table 1.
Reported Cases of ESP Block
| Pain | Region | Intervention | N | Level | SS vs. Catheter | Side | Local anesthetic | Average NRS* | Complications | Notes |
|---|---|---|---|---|---|---|---|---|---|---|
| Chronic | Cervical | Neuropathic pain [8] | 1 | T2 | 1SS | 1UL | B | 0 | No | Plus S |
| Upper limbs | Shoulder pain [9] | 1 | T2–T3 | 1SS | 1UL | B, R | 0.3 | No | Plus S+ times | |
| Thorax | Neuropathic pain [1,8,10–16] | 17 | T2–T6 | 13SS/4C | 17UL | B, R, LB | 1.4 | No | Plus S [11,15] + times [14,15] | |
| Bilevel [13] | ||||||||||
| Abdomen | Post-surgical visceral pain [17] | 1 | T10 | 1SS | 1UL | B | - | No | MRI study | |
| Lower limbs | Zoster [18], CRPS [19] | 2 | L3–L4 | 1SS/1C | 2UL | B + L, R | 2 | No | Plus S | |
| Acute | Cervical | Spine surgery [20] | 2 | T2–T3 | 2SS | 2BL | LB | - | No | - |
| CEA [21] | 2 | T2–T3 | 2SS | 2UL | LB | - | No | Anesthesia | ||
| Burn [22], zoster [23] | 2 | T2 | 1SS/1C | 2UL | B + L, LB | 0 | No | Plus S [23] | ||
| Upper limbs | Amputation [24] | 1 | C6 | 1C | 1UL | R | 0 | No | - | |
| Thorax | Breast surgery [8,25–38] | 30 | T4–T5 | 23SS/7C | 27UL/3BL | B, R, LB, B + L, R + M, B Lip | 0.9 | Incomplete analgesia [26] | Anesthesia [30–32] | |
| Plus S [31] | ||||||||||
| Pneumothorax [38] | Combined blockade [25–27] | |||||||||
| Bilevel [37] | ||||||||||
| VATS [1,8,39–45] | 26 | T5 | 4SS/22C | 25UL/1BL | B, R, LB, B + L, R + L | 1.6 | No | Pediatric [45] | ||
| Rib fractures [7,29,46–48] | 9 | T3/T5/T8 | 3SS/6C | 8UL/1BL | B, R, LB | 2.3 | No | Fluoroscopic guidance [7] | ||
| Thoracotomy [49–59] | 17 | T5/T6/T9 | 6SS/11C | 15UL/2BL | B, R, LB | 2.2 | No | Pediatric [56–59] | ||
| Costal Wall surgery [60–65] | 8 | T1/T2/T4/T5/T8 | 8SS | 6UL/2BL | B, B + L | 0.3 | No | Pediatric [63–65] + times [60] | ||
| Anesthesia [61,62] | ||||||||||
| ICU loss stay [64] | ||||||||||
| Valve surgery [66,67] | 3 | T2/T3/T7 | 2SS/1C | 3UL | B, LB | 3 | No | - | ||
| Spine surgery [68,69] | 3 | T4/T5 | 3SS | 3BL | B, LB | - | No | Interfascial Rhomboid-ESM [69] | ||
| Abdomen | Laparoscopy surgery [70–76] | 18 | T7–T9/T11 | 2SS/1C | 6UL/2BL | B, R, B + L | 1.3 | No | Plus S [72] | |
| Pediatric [73–75] | ||||||||||
| Open surgery [76–84] | 16 | T7–T9/T11/T12 | 11SS/5C | 6UL/10BL | B, R, B + L | 2.1 | Motor blockade [79] | Pediatric [84] | ||
| Abdominal Wall surgery [8,32,76,85–91] | 23 | T6–T10/L1 | 11SS/5C | 6UL/10BL | B, R, B + L, L | 2.3 | No | Pediatric [89–91] + times [88] | ||
| Anesthesia [85,86] | ||||||||||
| No USG [85] | ||||||||||
| Spine surgery [92,93] | 7 | T10/T12 | 4SS/3C | 7BL | B, R, LB | 0.1 | No | Plus S [92,93] | ||
| Plus DXM [92] | ||||||||||
| Miscellanea [94–97] | 4 | T6/T8/T10 | 3SS/1C | 2UL/2BL | B, R, B + L | 2 | No | Pancreatitis [94], zoster [95], fracture [96], nephrolithotomy [97] | ||
| Lower limbs | Hip surgery [98–102] | 17 | T12/L4 | 14SS/3C | 17UL | R, B + L | 3 | No | Pediatric [100] | |
| Anesthesia [99] | ||||||||||
| Combined blockade [99] | ||||||||||
| Thigh lift surgery [103] | 1 | L2 | 1SS | 1BI | R | 0 | No | - |
SS: single Shot, C: catheter, NRS: numbering rating scale, UL: unilateral, BL: bilateral, B: bupivacaine, R: ropivacaine, LB: levobupivacaine, L: lidocaine, M: mepivacaine, Lip: liposomal, S: steroids, DXM: dexmedetomidine, MRI: magnetic resonance imaging, CRPS: complex regional pain syndrome, CEA: carotid endarterectomy, VATS: video-assisted thoracoscopic surgery, ICU: intensive care unit.
FLACC or CHPPS scales in pediatric surgery.
Only six prospective trials were identified in this review. Tulgar et al. [104] evaluated the ESP block for postoperative analgesia in laparoscopic cholecystectomy. They compared 30 patients in two groups (ESP group and a control group). Their results included consumption of tramadol, as well as a score on the NRS scale lower in the ESP group during the first 3 h. Gürkan et al. [105] evaluated the ESP block for postoperative analgesia in breast surgery. They compared 50 patients in two groups (ESP group and control group). Total morphine consumption in block group decreased by 65% at 24 h compared to the control group (5.76 ± 3.80 mg vs. 16.60 ± 6.92 mg), but there was no statistically significant difference between the groups in terms of NRS scores. Oksuz et al. [106] also compared the bilateral ESP block with tumescent anesthesia for postoperative analgesia in 43 patients undergoing reduction mammoplasty. The NRS scores and the requirement for additional analgesia were statistically significantly lower in the ESP group. Altiparmak et al. [107] compared the effects of modified pectoral nerve (PECS) block and ESP block after radical mastectomy surgery. They concluded that PECS block reduced postoperative tramadol consumption (132.78 ± 22.44 mg vs. 196.00 ± 27.03 mg) and NRS scores after the postoperative 1 h, 2 h, 12 h, and 24 h more effectively than the ESP block. Nagaraja et al. [108] compared the continuous thoracic epidural with bilateral ESP block in cardiac surgery among 50 patients. The NRS scores were statistically significantly lower in the ESP group at 24 h, 36 h, and 48 h. Incentive spirometry, ventilator, and intensive care unit duration were comparable between the groups. Krishna et al. [109] evaluated the ESP block for postoperative analgesia in cardiac surgery. They compared 106 patients in two groups (ESP group and control group) and concluded that ESP block provided significantly better pain relief at rest (NRS were significantly lesser at all measured time points) and for a longer duration than the control group (8.98 ± 0.14 hours vs. 4.60 ± 0.12 hours).
One consecutive, patient-matched, controlled before-and-after study was included in this review. Macaire et al. [110] compared 67 patients undergoing cardiac surgery in 2 groups: a historical group of 20 patients who received intravenous morphine (0.5 mg/h) and nefopam (100 mg/24 h) with a group of 47 patients who received continuous bilateral ESP block. The ESP group was associated with less pain and lower opioid consumption (40 [25–45] mg in the control group vs. 0 [0–0] mg in the ESP group [P < 0.001]). In addition, the mobilization of the patients and the removal of the thoracic tube was performed earlier in the ESP group.
Two observational studies were identified in this review. Tulgar et al. [111] reported their results of comparing the single or bi-level application of ESP block in 12 patients undergoing thoracotomy. They observed that the NRS scores in the first 12 h were higher in the single level group than in the bi-level group. While the average fentanyl use in patients in the single level group was 37.5 mg in the first postoperative hour, no patient in the bi-level group required fentanyl. Additionally, tramadol use was lesser in patients undergoing bi-level ESP block. Ueshima et al. [112] compared 41 patients undergoing lumbar spinal surgery in a retrospective study. They observed that the NRS scores and the amount of fentanyl administered were lower in the ESP block group than in the control group at all measured time points, with no significant difference in the incidence of complications between the two groups. The 9 studies described are summarized in Table 2.
Table 2.
Reported Studies of ESP Block
| Type of study | Intervention | N | Groups | NRS | Opioid consumption | Conclusion | |
|---|---|---|---|---|---|---|---|
| Tulgar et al. [104] | RCT | Laparoscopic Cholecystectomy | 30 | ESPB vs. control | 0–3 h: 1.00 ± 1.13 vs. 2.88 ± 1.79 (P < 0.01) | Fentanyl use: 6.66 ± 11.44 μg vs. 32.33 ± 22.69 μg (P < 0.001) | Bilateral ultrasound guided ESPB leads to effective analgesia and a decrease in opioid requirement in first 12 h |
| Gürkan et al. [105] | RCT | Breast surgery | 50 | ESPB vs. control | No statistically significant difference | Morphine at 24 h: 5.76 ± 3.80 mg vs. 16.60 ± 6.92 mg (P < 0.001) | ESPB exhibits a significant analgesic effect in patients undergoing breast cancer surgery. |
| Oksuz et al. [106] | RCT | Breast surgery | 43 | ESPB vs. Tumescent anesthesia | 0–24 h, all NRS of the ESPB group were significantly lower (P < 0.001) | Tramadol: 122.00 ± 56.74 mg vs. 196.00 ± 67.30 mg (P < 0.05) | Bilateral ESPB in breast reduction surgery was more effective than tumescent anesthesia concerning opioid consumption and pain scores. |
| Altiparmak et al. [107] | RCT | Breast surgery | 38 | ESPB vs. PECS | 1–24 h, all NRS of the PECS group were significantly lower (P < 0.05) | Tramadol: 196.00 ± 27.03 mg vs. 132.78 ± 22.44 mg (P = 0.001) | Modified PECS block reduced postoperative tramadol consumption and pain scores more effectively than ESPB after radical mastectomy. |
| Nagaraja et al. [108] | RCT | Cardiac surgery | 50 | ESPB vs. TEA | 0–12 h comparable NRS in both groups. 24–48 h NRS of the ESPB group were significantly lower (P < 0.05) | ESPB is a promising alternative to TEA in optimal perioperative pain management in cardiac surgery. | |
| Krishna et al. [109] | RCT | Cardiac surgery | 106 | ESPB vs. control | 0–24 h, all NRS of the ESPB group were significantly lower (P < 0.001) | Fentanyl use: 82.92 ± 4.29 μg vs. 214.25 ± 5.09 μg (P < 0.001) | ESPB provided significantly better pain relief for longer duration as compared to intravenous paracetamol and tramadol. |
| Macaire et al. [110] | CBAS | Cardiac surgery | 67 | ESPB vs. control | 2 h after chest tube removal 1 [0–2] vs. 2 [1.5–2.5], and 1 month after surgery 0.5 [0–3] vs. 2 [1–4] (P < 0.05) | Morphine in the first 48 h | ESPB is associated with a significant decrease in intraoperative and postoperative opioid consumption, optimized rapid patient mobilization, and chest tube removal after open cardiac surgery. |
| 0 [0–0] mg vs. 40 [25–45] mg (P < 0.001) | |||||||
| Tulgar et al. [111] | POS | Thoracotomy | 12 | Single level vs. Bilevel | First 12 h 2.66 [0–6] vs. 1.05 [1–3] | Tramadol (mg/day) 146.6 [100–270] vs. 60 [30–140] | Bi-level ESPB may possibly have an improved effect for postoperative analgesia when compared to conventional single level ESPB |
| Ueshima et al. [112] | ROS | Lumbar spine surgery | 41 | ESPB vs. control | 0–24 h, all NRS of the ESPB group were significantly lower (P < 0.05) | Fentanyl use: 40 [40–60] μg vs. 100 [80–100] μg (P < 0.05) | ESPB provides effective postoperative analgesic effect for 24 hours in patients undergoing lumbar spinal surgery. |
NRS: numbering rating scale, RCT: randomized controlled trial, CBAS: controlled before-and-after study, POS: prospective observational study, ROS: retrospective observational study, ESPB: erector spinae plane block, PECS: pectoral nerve block, TEA: thoracic epidural analgesia.
Discussion
Regional anesthesia and pain management have experienced advances in recent years with the advent of fascial plane blockages. One of the newest techniques described in the literature has been the ESP block. In the past two years, the publications referring to ESP block have increased significantly [113,114].
Furthermore, most published articles are case reports; hence, from the study of these reports, it can be concluded that the ESP block is an effective analgesic technique in a variety of clinical scenarios. It can be utilized successfully in the treatment of acute and chronic pain. Likewise, it has also been effective for analgesia at the cervical, thoracic, and abdominal levels. Likewise, studies indicate that it can provide adequate analgesia in the upper or lower limbs if it is performed at the high thoracic and lumbar levels, respectively. The procedure has mostly been described for postoperative analgesia at the thoracic level. Additionally, it has a low rate of reported complications. However, given the majority of case reports reported in this review, the evidence of the description is low and there is a risk of publication bias (since it is possible that the studies with unsuccessful blockade were not published). Another limitation of our review is the lack of prospective studies. Prospective randomized controlled trials that compared the technique with a control group revealed that the ESP technique reduces both the pain scale score and the need for additional analgesia. However, other studies that compared the ESP block with another technique were not unanimous in their favor of it. The difference in analgesic effectiveness, which differs according to the scenario and comparative technique, means that more prospective studies are needed to help improve the evidence of its use.
Most authors affirm that ESP block is a technique that has great advantages over conventional techniques performed close to the neuroaxis. First, it is an easy technique to perform as the visualization of the target by ultrasound is very simple and it is not difficult to direct the needle towards it. Second, the technique has a low risk of complications. Important structures (such as main vessels, pleura, or medulla) whose injury can cause serious complications, are far from the target of blockage. Although several authors have postulated that the ESP block is the same technique as the retrolaminar block [117,118] or an “accidental paravertebral block” [119,120], both clinical and anatomical studies (in vivo and cadaveric) seem to indicate that it is a different technique [3,121,124,125]. Moreover, it is performed differently, the objective is different in all cases and the diffusion of LA differs between them.
Given that this procedure is easy to perform and is relatively safe, several authors have expressed the opinion that it could be part of the multimodal analgesia of the enhanced recovery after surgery programs [110]. Additionally, catheter insertion has been described as an easy procedure to perform; hence, the possibility of performing the technique for prolonged analgesia is available. However, being such a novel blockade technique, the lack of more well-designed prospective studies makes recommending its use in these programs has not yet occurred.
Therefore, we can conclude that ESP block seems to be an effective analgesic technique at many levels. This offers us the opportunity to utilize it in many clinical situations. Although it is not the technique of first choice in most situations, it is a suitable alternative, especially in scenarios in which the technique of first choice constitutes an important risk or is directly contraindicated. Moreover, ESP block has been described as an effective alternative when paravertebral or epidural block are contraindicated due to rejection by the patient [33,45,56,83], thrombocytopenia [39,41], antiplatelet [52] or anticoagulant treatments [53], or coagulopathy [58]. Other authors have shown its effectiveness as a second line therapy after the unsuccessful insertion of an epidural catheter [41] or its failure [49,51]. Additionally, it has been reported to successfully induce anesthesia in patients with a high risk of adverse effects from general anesthesia [30,31,85,86,99]. However, more randomized controlled trials are necessary to establish the best indications of ESP block as an analgesic technique, in chronic, acute, and postoperative pain.
Footnotes
No potential conflict of interest relevant to this article was reported.
Authors’ contribution
Pablo Kot (Conceptualization; Data curation; Validation; Visualization; Writing – original draft; Writing – review & editing)
Pablo Rodriguez (Conceptualization; Supervision; Validation)
Manuel Granell (Conceptualization; Supervision; Validation; Visualization)
Beatriz Cano (Conceptualization)
Lucas Rovira (Data curation; Supervision; Validation; Visualization)
Javier Morales (Conceptualization)
Ana Broseta (Conceptualization)
Jose De Andrés (Supervision; Validation; Visualization)
Supplementary Material
References
- 1.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 2.De Cassai A, Tonetti T. Local anesthetic spread during erector spinae plane block. J Clin Anesth. 2018;48:60–1. doi: 10.1016/j.jclinane.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector spinae plane block versus retrolaminar block: a magnetic resonance imaging and anatomical study. Reg Anesth Pain Med. 2018;43:756–62. doi: 10.1097/AAP.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 4.Ueshima H, Hiroshi O. Spread of local anesthetic solution in the erector spinae plane block. J Clin Anesth. 2018;45:23. doi: 10.1016/j.jclinane.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Vidal E, Giménez H, Forero M, Fajardo M. Erector spinae plane block: a cadaver study to determine its mechanism of action. Rev Esp Anestesiol Reanim. 2018;65:514–9. doi: 10.1016/j.redar.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Muñoz-Leyva F, Mendiola WE, Bonilla AJ, Cubillos J, Moreno DA, Chin KJ. In reply to "Continuous erector spinae plane (ESP) block: optimizing the analgesia technique". J Cardiothorac Vasc Anesth. 2018;32:e3–4. doi: 10.1053/j.jvca.2018.03.033. [DOI] [PubMed] [Google Scholar]
- 7.Jadon A, Swarupa CP, Amir M. Fluoroscopic-guided erector spinae plane block: a feasible option. Indian J Anaesth. 2018;62:806–8. doi: 10.4103/ija.IJA_411_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jain K, Jaiswal V, Puri A. Erector spinae plane block: Relatively new block on horizon with a wide spectrum of application - A case series. Indian J Anaesth. 2018;62:809–13. doi: 10.4103/ija.IJA_263_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Forero M, Rajarathinam M, Adhikary SD, Chin KJ. Erector spinae plane block for the management of chronic shoulder pain: a case report. Can J Anaesth. 2018;65:288–93. doi: 10.1007/s12630-017-1010-1. [DOI] [PubMed] [Google Scholar]
- 10.Aydin T, Balaban O, Acar A. Ultrasound guided continuous erector spinae plane block for pain management in pulmonary malignancy. J Clin Anesth. 2018;46:63–4. doi: 10.1016/j.jclinane.2018.01.023. [DOI] [PubMed] [Google Scholar]
- 11.Fusco P, DI Carlo S, Scimia P, Luciani A, Petrucci E, Marinangeli F. Could the new ultrasound-guided erector spinae plane block be a valid alternative to paravertebral block in chronic chest pain syndromes? Minerva Anestesiol. 2017;83:1112–3. doi: 10.23736/S0375-9393.17.12109-7. [DOI] [PubMed] [Google Scholar]
- 12.Ueshima H, Otake H. Erector spinae plane block for pain management of wide post-herpetic neuralgia. J Clin Anesth. 2018;51:37. doi: 10.1016/j.jclinane.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 13.Balaban O, Aydın T. Ultrasound guided bi-level erector spinae plane block for pain management in Herpes Zoster. J Clin Anesth. 2019;52:31–2. doi: 10.1016/j.jclinane.2018.08.016. [DOI] [PubMed] [Google Scholar]
- 14.Ahiskalioglu A, Alici HA, Ciftci B, Celik M, Karaca O. Continuous ultrasound guided erector spinae plane block for the management of chronic pain. Anaesth Crit Care Pain Med. 2017 doi: 10.1016/j.accpm.2017.11.014. Advance Access published on Dec 15, 2017. doi: 10.1016/j.accpm.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Forero M, Rajarathinam M, Adhikary S, Chin KJ. Erector spinae plane (ESP) block in the management of post thoracotomy pain syndrome: a case series. Scand J Pain. 2017;17:325–9. doi: 10.1016/j.sjpain.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 16.Ramos J, Peng P, Forero M. Long-term continuous erector spinae plane block for palliative pain control in a patient with pleural mesothelioma. Can J Anaesth. 2018;65:852–3. doi: 10.1007/s12630-018-1097-z. [DOI] [PubMed] [Google Scholar]
- 17.Schwartzmann A, Peng P, Maciel MA, Forero M. Mechanism of the erector spinae plane block: insights from a magnetic resonance imaging study. Can J Anaesth. 2018;65:1165–6. doi: 10.1007/s12630-018-1187-y. [DOI] [PubMed] [Google Scholar]
- 18.Alici HA, Ahiskalioglu A, Aydin ME, Ahiskalioglu EO, Celik M. High volume single injection lumbar erector spinae plane block provides effective analgesia for lower extremity herpes zoster. J Clin Anesth. 2019;54:136–7. doi: 10.1016/j.jclinane.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 19.Chung K, Kim ED. Continuous erector spinae plane block at the lower lumbar level in a lower extremity complex regional pain syndrome patient. J Clin Anesth. 2018;48:30–1. doi: 10.1016/j.jclinane.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 20.Ueshima H, Otake H. Blocking of multiple posterior branches of cervical nerves using an erector spinae plane block. J Clin Anesth. 2018;46:44. doi: 10.1016/j.jclinane.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 21.Ueshima H, Hiroshi O. Erector spinae plane block for carotid endarterectomy. J Clin Anesth. 2018;48:11. doi: 10.1016/j.jclinane.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Ueshima H, Otake H. Continuous erector spinae plane block for pain management of an extensive burn. Am J Emerg Med. 2018;36:2130. doi: 10.1016/j.ajem.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 23.Tekin E, Ahiskalioglu A, Aydin ME, Sengun E, Bayramoglu A, Alici HA. High-thoracic ultrasound-guided erector spinae plane block for acute herpes zoster pain management in emergency department. Am J Emerg Med. 2019;37:375. doi: 10.1016/j.ajem.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 24.Tsui BCH, Mohler D, Caruso TJ, Horn JL. Cervical erector spinae plane block catheter using a thoracic approach: an alternative to brachial plexus blockade for forequarter amputation. Can J Anaesth. 2019;66:119–20. doi: 10.1007/s12630-018-1170-7. [DOI] [PubMed] [Google Scholar]
- 25.Kumar A, Hulsey A, Martinez-Wilson H, Kim J, Gadsden J. The use of liposomal bupivacaine in erector spinae plane block to minimize opioid consumption for breast surgery: a case report. A A Pract. 2018;10:239–41. doi: 10.1213/XAA.0000000000000674. [DOI] [PubMed] [Google Scholar]
- 26.Ueshima H, Otake H. Limitations of the Erector Spinae Plane (ESP) block for radical mastectomy. J Clin Anesth. 2018;51:97. doi: 10.1016/j.jclinane.2018.08.013. [DOI] [PubMed] [Google Scholar]
- 27.Ueshima H, Otake H. A combination of an erector spinae plane block and a transversus thoracic muscle plane block for partial mastectomy. J Clin Anesth. 2019;54:1. doi: 10.1016/j.jclinane.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 28.Veiga M, Costa D, Brazão I. Erector spinae plane block for radical mastectomy: a new indication? Rev Esp Anestesiol Reanim. 2018;65:112–5. doi: 10.1016/j.redar.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Jones MR, Urits I, Shnider MR, Matyal R. Confirmation of erector spinae plane block analgesia for 3 distinct scenarios: a case report. A A Pract. 2019;12:141–4. doi: 10.1213/XAA.0000000000000865. [DOI] [PubMed] [Google Scholar]
- 30.De Cassai A, Marchet A, Ori C. The combination of erector spinae plane block and pectoralis blocks could avoid general anesthesia for radical mastectomy in high risk patients. Minerva Anestesiol. 2018;84:1420–1. doi: 10.23736/S0375-9393.18.13031-8. [DOI] [PubMed] [Google Scholar]
- 31.Kimachi PP, Martins EG, Peng P, Forero M. The erector spinae plane block provides complete surgical anesthesiain breast surgery: a case report. A A Pract. 2018;11:186–8. doi: 10.1213/XAA.0000000000000777. [DOI] [PubMed] [Google Scholar]
- 32.Balaban O, Aydin T, Yaman M. Is ultrasound guided erector spinae plane block sufficient for surgical anesthesia in minor surgery at thoracal region? J Clin Anesth. 2018;47:7–8. doi: 10.1016/j.jclinane.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 33.Bonvicini D, Tagliapietra L, Giacomazzi A, Pizzirani E. Bilateral ultrasound-guided erector spinae plane blocks in breast cancer and reconstruction surgery. J Clin Anesth. 2018;44:3–4. doi: 10.1016/j.jclinane.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 34.Ohgoshi Y, Ikeda T, Kurahashi K. Continuous erector spinae plane block provides effective perioperative analgesia for breast reconstruction using tissue expanders: a report of two cases. J Clin Anesth. 2018;44:1–2. doi: 10.1016/j.jclinane.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 35.Singh S, Chowdhary NK. Erector spinae plane block an effective block for post-operative analgesia in modified radical mastectomy. Indian J Anaesth. 2018;62:148–50. doi: 10.4103/ija.IJA_726_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bonvicini D, Giacomazzi A, Pizzirani E. Use of the ultrasound-guided erector spinae plane block in breast surgery. Minerva Anestesiol. 2017;83:1111–2. doi: 10.23736/S0375-9393.17.12015-8. [DOI] [PubMed] [Google Scholar]
- 37.Finneran JJ 4th, Gabriel RA, Khatibi B. Erector spinae plane blocks provide analgesia for breast and axillarysurgery: a series of 3 cases. Reg Anesth Pain Med. 2018;43:101–2. doi: 10.1097/AAP.0000000000000695. [DOI] [PubMed] [Google Scholar]
- 38.Ueshima H. Pneumothorax after the erector spinae plane block. J Clin Anesth. 2018;48:12. doi: 10.1016/j.jclinane.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 39.Wilson JM, Lohser J, Klaibert B. Erector spinae plane block for postoperative rescue analgesia in thoracoscopic surgery. J Cardiothorac Vasc Anesth. 2018;32:e5–7. doi: 10.1053/j.jvca.2018.06.026. [DOI] [PubMed] [Google Scholar]
- 40.Hu B, Zhou H, Zou X. The erector spinae plane block (ESPB) for non-intubated video-assisted thoracoscopic surgery. J Clin Anesth. 2019;54:50–1. doi: 10.1016/j.jclinane.2018.10.032. [DOI] [PubMed] [Google Scholar]
- 41.Luis-Navarro JC, Seda-Guzmán M, Luis-Moreno C, López-Romero JL. The erector spinae plane block in 4 cases of video-assisted thoracic surgery. Rev Esp Anestesiol Reanim. 2018;65:204–8. doi: 10.1016/j.redar.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 42.Ince I, Ozmen O, Aksoy M, Zeren S, Ulas AB, Aydin Y. Erector spinae plane block catheter insertion under ultrasound guidance for thoracic surgery: case series of three patients. Eurasian J Med. 2018;50:204–6. doi: 10.5152/eurasianjmed.2018.18147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Scimia P, Basso Ricci E, Droghetti A, Fusco P. The ultrasound-guided continuous erector spinae plane block for postoperative analgesia in video-assisted thoracoscopic lobectomy. Reg Anesth Pain Med. 2017;42:537. doi: 10.1097/AAP.0000000000000616. [DOI] [PubMed] [Google Scholar]
- 44.Taketa Y, Irisawa Y, Fujitani T. Ultrasound-guided erector spinae plane block elicits sensory loss around the lateral, but not the parasternal, portion of the thorax. J Clin Anesth. 2018;47:84–5. doi: 10.1016/j.jclinane.2018.03.023. [DOI] [PubMed] [Google Scholar]
- 45.Adhikary SD, Pruett A, Forero M, Thiruvenkatarajan V. Erector spinae plane block as an alternative to epidural analgesia for post-operative analgesia following video-assisted thoracoscopic surgery: a case study and a literature review on the spread of local anaesthetic in the erector spinae plane. Indian J Anaesth. 2018;62:75–8. doi: 10.4103/ija.IJA_693_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hamilton DL, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017;118:474–5. doi: 10.1093/bja/aex013. [DOI] [PubMed] [Google Scholar]
- 47.Luftig J, Mantuani D, Herring AA, Dixon B, Clattenburg E, Nagdev A. Successful emergency pain control for posterior rib fractures with ultrasound-guided erector spinae plane block. Am J Emerg Med. 2018;36:1391–6. doi: 10.1016/j.ajem.2017.12.060. [DOI] [PubMed] [Google Scholar]
- 48.Nandhakumar A, Nair A, Bharath VK, Kalingarayar S, Ramaswamy BP, Dhatchinamoorthi D. Erector spinae plane block may aid weaning from mechanical ventilation in patients with multiple rib fractures: case report of two cases. Indian J Anaesth. 2018;62:139–41. doi: 10.4103/ija.IJA_599_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Raft J, Chin KJ, Belanger ME, Clairoux A, Richebé P, Brulotte V. Continuous Erector Spinae Plane Block for thoracotomy analgesia after epidural failure. J Clin Anesth. 2019;54:132–3. doi: 10.1016/j.jclinane.2018.10.024. [DOI] [PubMed] [Google Scholar]
- 50.Ciftci B, Ekinci M, Demiraran Y. Ultrasound-guided single-shot preemptive erector spinae plane blockfor postoperative pain management. J Cardiothorac Vasc Anesth. 2019;33:1175–6. doi: 10.1053/j.jvca.2018.10.040. [DOI] [PubMed] [Google Scholar]
- 51.Forero M, Rajarathinam M, Adhikary S, Chin KJ. Continuous erector spinae plane block for rescue analgesia in thoracotomy after epidural failure: a case report. A A Case Rep. 2017;8:254–6. doi: 10.1213/XAA.0000000000000478. [DOI] [PubMed] [Google Scholar]
- 52.De Cassai A, Ieppariello G, Ori C. Erector spinae plane block and dual antiplatelet therapy. Minerva Anestesiol. 2018;84:1230–1. doi: 10.23736/S0375-9393.18.12815-X. [DOI] [PubMed] [Google Scholar]
- 53.Adhikary SD, Prasad A, Soleimani B, Chin KJ. Continuous erector spinae plane block as an effective analgesic option in anticoagulated patients after left ventricular assist device implantation: a case series. J Cardiothorac Vasc Anesth. 2019;33:1063–7. doi: 10.1053/j.jvca.2018.04.026. [DOI] [PubMed] [Google Scholar]
- 54.Tanaka N, Ueshima H, Otake H. Erector spinae plane block for combined lovectomy and radical mastectomys. J Clin Anesth. 2018;45:27–8. doi: 10.1016/j.jclinane.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 55.Ueshima H, Otake H. Erector spinae plane block provides effective pain management during pneumothorax surgery. J Clin Anesth. 2017;40:74. doi: 10.1016/j.jclinane.2017.04.016. [DOI] [PubMed] [Google Scholar]
- 56.Ueshima H, Otake H. Clinical experiences of erector spinae plane block for children. J Clin Anesth. 2018;44:41. doi: 10.1016/j.jclinane.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 57.De la Cuadra-Fontaine JC, Concha M, Vuletin F, Arancibia H. Continuous Erector Spinae Plane block for thoracic surgery in a pediatric patient. Paediatr Anaesth. 2018;28:74–5. doi: 10.1111/pan.13277. [DOI] [PubMed] [Google Scholar]
- 58.Wyatt K, Elattary T. The erector spinae plane block in a high-risk Ehlers-Danlos syndrome pediatric patient for vascular ring repair. J Clin Anesth. 2019;54:39–40. doi: 10.1016/j.jclinane.2018.10.031. [DOI] [PubMed] [Google Scholar]
- 59.Gaio-Lima C, Costa CC, Moreira JB, Lemos TS, Trindade HL. Continuous erector spinae plane block for analgesia in pediatric thoracic surgery: a case report. Rev Esp Anestesiol Reanim. 2018;65:287–90. doi: 10.1016/j.redar.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 60.de Haan JB, Hernandez N, Sen S. Erector spinae block for postoperative analgesia following axillary hidradenitis suppurativa resection: a case report. Local Reg Anesth. 2018;11:87–90. doi: 10.2147/LRA.S179830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ahiskalioglu A, Yayik AM, Celik EC, Ahiskalioglu EO, Emsen M. Two plane two block for surgical anesthesia: ultrasound-guided serratus and Erector Spinae Plane Blocks. J Clin Anesth. 2018;47:19–20. doi: 10.1016/j.jclinane.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 62.Cesur S, Ay AN, Yayık AM, Naldan ME, Gürkan Y. Ultrasound-guided erector spinae plane block provides effective perioperative analgesia and anaesthesia for thoracic mass excision: a report of two cases. Anaesth Crit Care Pain Med. 2019;38:189–90. doi: 10.1016/j.accpm.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 63.Hernandez MA, Palazzi L, Lapalma J, Forero M, Chin KJ. Erector spinae plane block for surgery of the posterior thoracic wall in a pediatric patient. Reg Anesth Pain Med. 2018;43:217–9. doi: 10.1097/AAP.0000000000000716. [DOI] [PubMed] [Google Scholar]
- 64.Nardiello MA, Herlitz M. Bilateral single shot erector spinae plane block for pectus excavatum and pectus carinatum surgery in 2 pediatric patients. Rev Esp Anestesiol Reanim. 2018;65:530–3. doi: 10.1016/j.redar.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 65.Muñoz F, Cubillos J, Bonilla AJ, Chin KJ. Erector spinae plane block for postoperative analgesia in pediatric oncological thoracic surgery. Can J Anaesth. 2017;64:880–2. doi: 10.1007/s12630-017-0894-0. [DOI] [PubMed] [Google Scholar]
- 66.Ueshima H, Hiroshi O. Transapical transcatheter aortic valve implantation performed with an erector spinae plane block. J Clin Anesth. 2018;46:84. doi: 10.1016/j.jclinane.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 67.Leyva FM, Mendiola WE, Bonilla AJ, Cubillos J, Moreno DA, Chin KJ. Continuous erector spinae plane (ESP) block for postoperative analgesia after minimally invasive mitral valve surgery. J Cardiothorac Vasc Anesth. 2018;32:2271–4. doi: 10.1053/j.jvca.2017.12.020. [DOI] [PubMed] [Google Scholar]
- 68.Chin KJ, Lewis S. Opioid-free analgesia for posterior spinal fusion surgery using erector spinae plane (ESP) blocks in a multimodal anesthetic regimen. Spine (Phila Pa 1976) 2019;44:E379–83. doi: 10.1097/BRS.0000000000002855. [DOI] [PubMed] [Google Scholar]
- 69.Ueshima H, Otake H. Clinical experiences of ultrasound-guided erector spinae plane block for thoracic vertebra surgery. J Clin Anesth. 2017;38:137. doi: 10.1016/j.jclinane.2016.12.028. [DOI] [PubMed] [Google Scholar]
- 70.Tulgar S, Selvi O, Kapakli MS. Erector spinae plane block for different laparoscopic abdominal surgeries: case series. Case Rep Anesthesiol. 2018;2018:3947281. doi: 10.1155/2018/3947281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hannig KE, Jessen C, Soni UK, Børglum J, Bendtsen TF. Erector spinae plane block for elective laparoscopic cholecystectomyin the ambulatory surgical setting. Case Rep Anesthesiol. 2018;2018:5492527. doi: 10.1155/2018/5492527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Petsas D, Pogiatzi V, Galatidis T, Drogouti M, Sofianou I, Michail A, et al. Erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a case report. J Pain Res. 2018;11:1983–90. doi: 10.2147/JPR.S164489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Aksu C, Gürkan Y. Ultrasound-guided bilateral erector spinae plane block could provide effective postoperative analgesia in laparoscopic cholecystectomy in paediatric patients. Anesth Crit Care Pain Med. 2018;38:87–8. doi: 10.1016/j.accpm.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 74.Thomas DT, Tulgar S. Ultrasound-guided erector spinae plane block in a child undergoing laparoscopic cholecystectomy. Cureus. 2018;10:e2241. doi: 10.7759/cureus.2241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Aksu C, Gürkan Y. Erector spinae plane block: a new indication with a new approach and a recommendation to reduce the risk of pneumothorax. J Clin Anesth. 2019;54:130–1. doi: 10.1016/j.jclinane.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 76.Luis-Navarro JC, Seda-Guzmán M, Luis-Moreno C, Chin KJ. Erector spinae plane block in abdominal surgery: case series. Indian J Anaesth. 2018;62:549–54. doi: 10.4103/ija.IJA_57_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Temirov T, Ben-David B, Mustafin A, Viderman D. Erector spinae plane block in management of pain after kidney transplantation. Pain Med. 2019;20:1053–4. doi: 10.1093/pm/pny221. [DOI] [PubMed] [Google Scholar]
- 78.Yamak Altinpulluk E, García Simón D, Fajardo-Pérez M. Erector spinae plane block for analgesia after lower segment caesarean section: case report. Rev Esp Anestesiol Reanim. 2018;65:284–6. doi: 10.1016/j.redar.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 79.Selvi O, Tulgar S. Ultrasound guided erector spinae plane block as a cause of unintended motor block. Rev Esp Anestesiol Reanim. 2018;65:589–92. doi: 10.1016/j.redar.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 80.Aksu C, Gürkan Y. Ultrasound guided erector spinae block for postoperative analgesia in pediatric nephrectomy surgeries. J Clin Anesth. 2018;45:35–6. doi: 10.1016/j.jclinane.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 81.Hacibeyoglu G, Topal A, Arican S, Kilicaslan A, Tekin A, Uzun ST. USG guided bilateral erector spinae plane block is an effective and safe postoperative analgesia method for living donor liver transplantation. J Clin Anesth. 2018;49:36–7. doi: 10.1016/j.jclinane.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 82.Tulgar S, Senturk O. Ultrasound guided low thoracic erector spinae plane block for postoperative analgesia in radical retropubic prostatectomy, a new indication. J Clin Anesth. 2018;47:4. doi: 10.1016/j.jclinane.2018.02.013. [DOI] [PubMed] [Google Scholar]
- 83.Restrepo-Garces CE, Chin KJ, Suarez P, Diaz A. Bilateral continuous erector spinae plane block contributes to effective postoperative analgesia after major open abdominal surgery: a case report. A A Case Rep. 2017;9:319–21. doi: 10.1213/XAA.0000000000000605. [DOI] [PubMed] [Google Scholar]
- 84.Munshey F, Rodriguez S, Diaz E, Tsui B. Continuous erector spinae plane block for an open pyeloplasty in an infant. J Clin Anesth. 2018;47:47–9. doi: 10.1016/j.jclinane.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 85.Elkoundi A, Chouikh C, Baite A, Bensghir M, Bakkali H, Lalaoui SJ. Successful erector spinae plane block without ultrasound guidance in a severely cardiovascular compromised patient. J Clin Anesth. 2019;53:50. doi: 10.1016/j.jclinane.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 86.Tulgar S, Thomas DT, Deveci U. Erector spinae plane block provides sufficient surgical anesthesia for ileostomy closure in a high-risk patient. J Clin Anesth. 2018;48:2–3. doi: 10.1016/j.jclinane.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 87.Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72:452–60. doi: 10.1111/anae.13814. [DOI] [PubMed] [Google Scholar]
- 88.Chung K, Kim ED. Erector spinae plane block at the lower thoracic level for postoperative pain management after spinal cord stimulation implantation. Pain Med. 2018;19:2330–2. doi: 10.1093/pm/pny076. [DOI] [PubMed] [Google Scholar]
- 89.Hernandez MA, Palazzi L, Lapalma J, Cravero J. Erector spinae plane block for inguinal hernia repair in preterm infants. Paediatr Anaesth. 2018;28:298–9. doi: 10.1111/pan.13325. [DOI] [PubMed] [Google Scholar]
- 90.Aksu C, Gürkan Y. Opioid sparing effect of Erector Spinae Plane block for pediatric bilateral inguinal hernia surgeries. J Clin Anesth. 2018;50:62–3. doi: 10.1016/j.jclinane.2018.06.048. [DOI] [PubMed] [Google Scholar]
- 91.Aksu C, Gürkan Y. Aksu approach for lumbar erector spinae plane block for pediatric surgeries. J Clin Anesth. 2019;54:74–5. doi: 10.1016/j.jclinane.2018.10.043. [DOI] [PubMed] [Google Scholar]
- 92.Melvin JP, Schrot RJ, Chu GM, Chin KJ. Low thoracic erector spinae plane block for perioperative analgesia in lumbosacral spine surgery: a case series. Can J Anaesth. 2018;65:1057–65. doi: 10.1007/s12630-018-1145-8. [DOI] [PubMed] [Google Scholar]
- 93.Calandese F, Adduci A. Erector spinae plane block for acute postoperative pain management after anterior thoracolumbar spine surgery. J Clin Anesth. 2019;52:55–6. doi: 10.1016/j.jclinane.2018.08.014. [DOI] [PubMed] [Google Scholar]
- 94.Elkoundi A, Eloukkal Z, Bensghir M, Belyamani L, Lalaoui SJ. Erector spinae plane block for hyperalgesic acute pancreatitis. Pain Med. 2019;20:1055–6. doi: 10.1093/pm/pny232. [DOI] [PubMed] [Google Scholar]
- 95.Ahiskalioglu A, Alici HA, Ari MA. Ultrasound guided low thoracic erector spinae plane block for management of acute herpes zoster. J Clin Anesth. 2018;45:60–1. doi: 10.1016/j.jclinane.2017.12.018. [DOI] [PubMed] [Google Scholar]
- 96.Ahiskalioglu A, Kocak AO, Doymus O, Sengun E, Celik M, Alici HA. Erector spinae plane block for bilateral lumbar transverse process fracture in emergency department: a new indication. Am J Emerg Med. 2018;36:1927. doi: 10.1016/j.ajem.2018.06.072. [DOI] [PubMed] [Google Scholar]
- 97.Kim E, Kwon W, Oh S, Bang S. The erector spinae plane block for postoperative analgesia after percutaneous nephrolithotomy. Chin Med J (Engl) 2018;131:1877–8. doi: 10.4103/0366-6999.237408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tulgar S, Selvi O, Senturk O, Ermis MN, Cubuk R, Ozer Z. Clinical experiences of ultrasound-guided lumbar erector spinae plane block for hip joint and proximal femur surgeries. J Clin Anesth. 2018;47:5–6. doi: 10.1016/j.jclinane.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 99.Tulgar S, Ermis MN, Ozer Z. Combination of lumbar erector spinae plane block and transmuscular quadratus lumborum block for surgical anaesthesia in hemiarthroplasty for femoral neck fracture. Indian J Anaesth. 2018;62:802–5. doi: 10.4103/ija.IJA_230_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Darling CE, Pun SY, Caruso TJ, Tsui BC. Successful directional thoracic erector spinae plane block after failed lumbar plexus block in hip joint and proximal femur surgery. J Clin Anesth. 2018;49:1–2. doi: 10.1016/j.jclinane.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 101.Bugada D, Zarcone AG, Manini M, Lorini LF. Continuous Erector Spinae Block at lumbar level (L4) for prolonged postoperative analgesia after hip surgery. J Clin Anesth. 2019;52:24–5. doi: 10.1016/j.jclinane.2018.08.023. [DOI] [PubMed] [Google Scholar]
- 102.Tulgar S, Senturk O. Ultrasound guided Erector Spinae Plane block at L-4 transverse process level provides effective postoperative analgesia for total hip arthroplasty. J Clin Anesth. 2018;44:68. doi: 10.1016/j.jclinane.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 103.Goodman DA. Erector spinae block at L2 for thigh lift surgery, a new application. J Clin Anesth. 2019;52:82. doi: 10.1016/j.jclinane.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 104.Tulgar S, Kapakli MS, Senturk O, Selvi O, Serifsoy TE, Ozer Z. Evaluation of ultrasound-guided erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a prospective, randomized, controlled clinical trial. J Clin Anesth. 2018;49:101–6. doi: 10.1016/j.jclinane.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 105.Gürkan Y, Aksu C, Kuş A, Yörükoğlu UH, Kılıç CT. Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: a randomized controlled study. J Clin Anesth. 2018;50:65–8. doi: 10.1016/j.jclinane.2018.06.033. [DOI] [PubMed] [Google Scholar]
- 106.Oksuz G, Bilgen F, Arslan M, Duman Y, Urfalıoglu A, Bilal B. Ultrasound-guided bilateral erector spinae block versus tumescent anesthesia for postoperative analgesia in patients undergoing reduction mammoplasty: a randomized controlled study. Aesthetic Plast Surg. 2019;43:291–6. doi: 10.1007/s00266-018-1286-8. [DOI] [PubMed] [Google Scholar]
- 107.Altıparmak B, Korkmaz Toker M, Uysal Aİ, Turan M, Gümüş Demirbilek S. Comparison of the effects of modified pectoral nerve block and erector spinae plane block on postoperative opioid consumption and pain scores of patients after radical mastectomy surgery: a prospective, randomized, controlled trial. J Clin Anesth. 2019;54:61–5. doi: 10.1016/j.jclinane.2018.10.040. [DOI] [PubMed] [Google Scholar]
- 108.Nagaraja PS, Ragavendran S, Singh NG, Asai O, Bhavya G, Manjunath N, et al. Comparison of continuous thoracic epidural analgesia with bilateral erector spinae plane block for perioperative pain management in cardiac surgery. Ann Card Anaesth. 2018;21:323–7. doi: 10.4103/aca.ACA_16_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Krishna SN, Chauhan S, Bhoi D, Kaushal B, Hasija S, Sangdup T, et al. Bilateral erector spinae plane block for acute post-surgical pain in adult cardiac surgical patients: a randomized controlled trial. J Cardiothorac Vasc Anesth. 2019;33:368–75. doi: 10.1053/j.jvca.2018.05.050. [DOI] [PubMed] [Google Scholar]
- 110.Macaire P, Ho N, Nguyen T, Nguyen B, Vu V, Quach C, et al. Ultrasound-guided continuous thoracic erector spinae plane block within an enhanced recovery program is associated with decreased opioid consumption and improved patient postoperative rehabilitation after open cardiac surgery-a patient-matched, controlled before-and-after study. J Cardiothorac Vasc Anesth. 2019;33:1659–67. doi: 10.1053/j.jvca.2018.11.021. [DOI] [PubMed] [Google Scholar]
- 111.Tulgar S, Selvi O, Ozer Z. Clinical experience of ultrasound-guided single and bi-level erector spinae plane block for postoperative analgesia in patients undergoing thoracotomy. J Clin Anesth. 2018;50:22–3. doi: 10.1016/j.jclinane.2018.06.034. [DOI] [PubMed] [Google Scholar]
- 112.Ueshima H, Inagaki M, Toyone T, Otake H. Efficacy of the erector spinae plane block for lumbar spinal surgery: a retrospective study. Asian Spine J. 2019;13:254–7. doi: 10.31616/asj.2018.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Tsui BC, Fonseca A, Munshey F, McFadyen G, Caruso TJ. The erector spinae plane (ESP) block: a pooled review of 242 cases. J Clin Anesth. 2019;53:29–34. doi: 10.1016/j.jclinane.2018.09.036. [DOI] [PubMed] [Google Scholar]
- 114.El-Boghdadly K, Pawa A. The erector spinae plane block: plane and simple. Anaesthesia. 2017;72:434–8. doi: 10.1111/anae.13830. [DOI] [PubMed] [Google Scholar]
- 115.De la Cuadra-Fontaine JC, Altermatt FR. Continuous Erector Spinae Plane (ESP) block: optimizing the analgesia technique. J Cardiothorac Vasc Anesth. 2018;32:e2–3. doi: 10.1053/j.jvca.2018.03.034. [DOI] [PubMed] [Google Scholar]
- 116.Noss C, Anderson KJ, Gregory AJ. Erector spinae plane block for open-heart surgery: a potential tool for improved analgesia. J Cardiothorac Vasc Anesth. 2019;33:376–7. doi: 10.1053/j.jvca.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 117.Ueshima H, Otake H. Similarities between the retrolaminar and erector spinae plane blocks. Reg Anesth Pain Med. 2017;42:123–4. doi: 10.1097/AAP.0000000000000526. [DOI] [PubMed] [Google Scholar]
- 118.Murouchi T. Consideration of block nomenclature: erector spinae plane block or retrolaminar block? Reg Anesth Pain Med. 2017;42:124. doi: 10.1097/AAP.0000000000000525. [DOI] [PubMed] [Google Scholar]
- 119.Hamilton DL, Manickam B. The erector spinae plane block. Reg Anesth Pain Med. 2017;42:276. doi: 10.1097/AAP.0000000000000565. [DOI] [PubMed] [Google Scholar]
- 120.Cornish PB. Erector spinae plane block: the "happily accidental" paravertebral block. Reg Anesth Pain Med. 2018;43:644–5. doi: 10.1097/AAP.0000000000000825. [DOI] [PubMed] [Google Scholar]
- 121.Chin KJ, Forero M, Adhikary SD. Reply to Dr Ueshima and Dr Murouchi. Reg Anesth Pain Med. 2017;42:124–5. doi: 10.1097/AAP.0000000000000531. [DOI] [PubMed] [Google Scholar]
- 122.Josh Luftig PA, Mantuani D, Herring AA, Dixon B, Clattenburg E, Nagdev A. The authors reply to the optimal dose and volume of local anesthetic for erector spinae plane blockade for posterior rib fractures. Am J Emerg Med. 2018;36:1103–4. doi: 10.1016/j.ajem.2018.03.051. [DOI] [PubMed] [Google Scholar]
- 123.Kose HC, Kose SG, Thomas DT. Lumbar versus thoracic erector spinae plane block: similar nomenclature, different mechanism of action. J Clin Anesth. 2018;48:1. doi: 10.1016/j.jclinane.2018.03.026. [DOI] [PubMed] [Google Scholar]
- 124.Yang HM, Choi YJ, Kwon HJ, O J, Cho TH, Kim SH. Comparison of injectate spread and nerve involvement between retrolaminar and erector spinae plane blocks in the thoracic region: a cadaveric study. Anaesthesia. 2018;73:1244–50. doi: 10.1111/anae.14408. [DOI] [PubMed] [Google Scholar]
- 125.Ivanusic J, Konishi Y, Barrington MJ. A cadaveric study investigating the mechanism of action of erector spinae blockade. Reg Anesth Pain Med. 2018;43:567–71. doi: 10.1097/AAP.0000000000000789. [DOI] [PubMed] [Google Scholar]
- 126.Chong MA, Berbenetz NM, Lin C, Singh S. Perineural versus intravenous dexamethasone as an adjuvant for peripheral nerve blocks: a systematic review and meta-analysis. Reg Anesth Pain Med. 2017;42:319–26. doi: 10.1097/AAP.0000000000000571. [DOI] [PubMed] [Google Scholar]
- 127.Elsharkawy H, Maniker R, Bolash R, Kalasbail P, Drake RL, Elkassabany N. Rhomboid intercostal and subserratus plane block: a cadaveric and clinical evaluation. Reg Anesth Pain Med. 2018;43:745–51. doi: 10.1097/AAP.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 128.Aygun H, Thomas DT, Tulgar S. Reply to Goodman: Lumbar erector spinae plane block for thigh lift surgery: which level, which block and which procedure? J Clin Anesth. 2019;53:75. doi: 10.1016/j.jclinane.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 129.Bonvicini D, Tagliapietra L. Reply to DR. De Cassai et al. J Clin Anesth. 2018;49:131. doi: 10.1016/j.jclinane.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 130.Chaudhary NK, Singh S. The right plane for drug injection in ultrasound-guided erector spinae plane block. Indian J Anaesth. 2018;62:405. doi: 10.4103/ija.IJA_229_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Chin KJ, Adhikary S, Forero M. Is the erector spinae plane (ESP) block a sheath block? A reply. Anaesthesia. 2017;72:916–7. doi: 10.1111/anae.13926. [DOI] [PubMed] [Google Scholar]
- 132.Costache I, de Neumann L, Ramnanan CJ, Goodwin SL, Pawa A, Abdallah FW, et al. The mid-point transverse process to pleura (MTP) block: a new end-point for thoracic paravertebral block. Anaesthesia. 2017;72:1230–6. doi: 10.1111/anae.14004. [DOI] [PubMed] [Google Scholar]
- 133.De Cassai A, Stefani G, Ori C. Erector spinae plane block and brachial plexus. J Clin Anesth. 2018;45:32. doi: 10.1016/j.jclinane.2017.12.017. [DOI] [PubMed] [Google Scholar]
- 134.Greenhalgh K, Womack J, Marcangelo S. Injectate spread in erector spinae plane block. Anaesthesia. 2019;74:126–7. doi: 10.1111/anae.14523. [DOI] [PubMed] [Google Scholar]
- 135.Hamilton DL, Manickam BP. Is the erector spinae plane (ESP) block a sheath block? Anaesthesia. 2017;72:915–6. doi: 10.1111/anae.13912. [DOI] [PubMed] [Google Scholar]
- 136.Hamilton DL. Pneumothorax following erector spinae plane block. J Clin Anesth. 2019;52:17. doi: 10.1016/j.jclinane.2018.08.026. [DOI] [PubMed] [Google Scholar]
- 137.Kashani HH, Grocott HP. Clarity needed as to the optimal dose and volume of local anesthetic for erector spinae plane blockade for posterior rib fractures. Am J Emerg Med. 2018;36:1102–3. doi: 10.1016/j.ajem.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 138.Tulgar S, Balaban O. Local anaesthetic injection point of erector spinae plane block. Indian J Anaesth. 2018;62:403–4. doi: 10.4103/ija.IJA_200_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Tulgar S, Ahiskalioglu A, Balaban O. Reply to Dr. Ueshima: The relationship of local anesthetic volume and dermatomal spread of sensorial block in erector spinae plane blocks: a new dilemma. J Clin Anesth. 2019;52:57. doi: 10.1016/j.jclinane.2018.09.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


