This study of a nationally representative cross-sectional annual household-based probability sample of noninstitutionalized residents estimates disparities in smoking prevalence associated with the number of socioeconomic and health-related disadvantages faced by US adults from 2008 to 2017.
Key Points
Question
Are US disparities in smoking prevalence associated with the cumulative number of socioeconomic or health-related disadvantages faced, and have such disparities widened over time?
Findings
In this nationally representative cross-sectional annual household-based probability sample of US noninstitutionalized residents, the mean current smoking prevalence among 279 559 adults 25 years or older collapsed across 2008 to 2017 was successively higher with each additional form of disadvantage faced. Odds of current vs never smoking decreased from 2008 to 2017 for groups with 0 to 2 disadvantages but did not significantly change for groups facing 3 or more disadvantages.
Meaning
Multidisadvantaged groups may constitute a disproportionate percentage of US smokers, a disparity that recently widened.
Abstract
Importance
Understanding emerging patterns of smoking disparities among disadvantaged populations can guide tobacco control policy.
Objective
To estimate disparities in smoking prevalence associated with the number of socioeconomic and health-related disadvantages faced by a population among US adults from 2008 to 2017.
Design, Setting, and Participants
Nationally representative cross-sectional annual household-based probability sample of US noninstitutionalized residents. Polytomous regression estimated associations of disadvantage variables, survey year, and their interaction with the following 3 pairwise contrasts: current vs never smoking (estimate of overall disparities), current vs former smoking (unique contribution of disparities in smoking cessation), and former vs never smoking (unique contribution of disparities in smoking initiation). The setting was in-home face-to-face interviews. Participants were respondents in 2008 to 2017 survey years who were aged 25 years or older (N = 279 559).
Exposures
Self-reported past-year unemployment, income below the federal poverty line, absence of high school diploma, disability/limitation interfering with daily functions, serious psychological distress on the Kessler 6-item screen, and at least 60 past-year heavy drinking days, each coded yes or no. These indicators were summed in a cumulative disadvantage index (0, 1, 2, 3, 4, or 5 or 6).
Main Outcomes and Measures
Self-reported current, former (ever smoked ≥100 cigarettes, had since quit, and not currently smoking), and never (<100 cigarettes) smoking.
Results
Among 278 048 respondents (mean [SD] age, 51.9 [16.8] years; 55.7% female) with data on smoking history (99.5% of the sample), the mean current smoking prevalence across 2008 to 2017 compared with populations without disadvantages was successively higher among populations with 1 disadvantage (21.4% vs 13.8%; current vs never smoking adjusted odds ratio [OR], 2.34; 95% CI, 2.27-2.43), 2 disadvantages (26.6% vs 13.8%; OR, 3.55; 95% CI, 3.39-3.72), 3 disadvantages (35.1% vs 13.8%; OR, 5.35; 95% CI, 5.05-5.66), 4 disadvantages (45.7% vs 13.8%; OR, 8.59; 95% CI, 7.91-9.34), or 5 or 6 disadvantages (58.2% vs 13.8%; OR, 14.70; 95% CI, 12.30-17.50). In current vs former and former vs never smoking status contrasts, ORs were lower but also showed successively greater associations with increasing cumulative disadvantage. Current (vs never) smoking odds significantly declined each year among populations with 0 (OR, 0.95; 95% CI, 0.94-0.96), 1 (OR, 0.96; 95% CI, 0.95-0.97), or 2 (OR, 0.98; 95% CI, 0.97-0.99) disadvantages but did not change across 2008 to 2017 among those with 3 or more disadvantages.
Conclusions and Relevance
Results of this study demonstrate that US disparities in smoking prevalence from 2008 to 2017 were successively larger with each additional disadvantage faced, were expressed in higher smoking initiation odds and lower smoking cessation odds, and widened over time.
Introduction
Cigarette smoking is unduly common in those facing socioeconomic or health-related disadvantages, such as poverty or behavioral health conditions, which contributes to inequities in morbidity and mortality.1 Understanding emerging patterns of disparities in smoking prevalence can guide priorities for tobacco control.
Epidemiologic analyses of smoking disparities typically focus on groups defined by a single type of disadvantage. However, various forms of socioeconomic and health-related disadvantages tend to co-occur and could cumulatively increase risk of smoking.2,3 Whether smoking prevalence successively increases as the cumulative number of disadvantages faced by a population rises or whether odds of smoking level off at a certain threshold of cumulative disadvantage is unknown. Also undetermined is whether US smoking disparities associated with cumulative disadvantage have widened recently and are manifested by differential odds of smoking initiation or smoking cessation, which could highlight needs for smoking prevention programs or quit smoking treatment services, respectively.
To inform national public health policies to reduce tobacco-related health disparities, this study estimates associations of cumulative disadvantage with disparities in smoking prevalence in the United States from 2008 to 2017 and evaluates whether such disparities widened over this decade. The accumulation of the following 6 different socioeconomic or health-related disadvantages that are linked with smoking and designated by US public health organizations as tobacco use disparity populations is the focus: unemployment, poverty, low education, disability/limitation, serious psychological distress, and heavy alcohol consumption.2,3,4,5 In addition to comparisons of current vs never smoking, which aim to estimate overall disparities, current vs former smoking and former vs never smoking analyses were conducted to examine whether disproportionate odds of smoking cessation or initiation, respectively, contribute to smoking disparities in multidisadvantaged populations.
Methods
Sample and Procedure
In this study of a nationally representative cross-sectional annual household-based probability sample of US noninstitutionalized residents, data from National Health Interview Survey (NHIS)6 respondents 25 years or older from 2008 to 2017 were pooled (N = 279 559). In total, 278 048 respondents with smoking data constituted the analytic sample. The age restriction excludes those below legal drinking age and without sufficient opportunity to progress in education, employment, and income. Data were collected by in-home face-to-face computer-assisted interviews. Respondents provided verbal informed consent, and the National Center for Health Statistics Research Ethics Review Board approved the protocol.
Measures
Questionnaire items are included in the eMethods in the Supplement. The number of missing observations per variable is also given.
Smoking Status
Participants reporting ever smoking fewer than 100 cigarettes were classified as “never smokers.”7 Those reporting 100 or more lifetime cigarettes, which they had since quit and now do not smoke cigarettes at all, were classified as “former smokers.” Persons who reported smoking 100 or more lifetime cigarettes and now smoking cigarettes on some days or every day were “current smokers.”
Disadvantage
Six forms of disadvantage, each recategorized as binary variables (yes or no), were assessed in the NHIS. This was based on previously applied classifications.2,7,8,9,10,11,12,13,14
Current Unemployment
Participants were considered unemployed if they did not have any job in the past 12 months. Relevant reasons included layoff, temporary inability to work for health reasons, off-season job, or disability.
Poverty
Poverty for a given year was classified according to family size. It was also based on household annual income relative to the preceding year’s US federal poverty line.
Low Education
Low education was defined as not having earned a high school diploma or equivalent degree or higher. A passing grade on a test of General Educational Development (GED) was considered an equivalent degree.
Disability/Limitation
Respondents reported whether they had any conditions or health problems that caused difficulty in performing specific day-to-day activities (eg, walking a quarter mile, sitting for about 2 hours, and participating in social activities). Conditions qualifying as disabilities/limitations in this study correspond with definitions applied in prior NHIS epidemiologic analyses of smoking15 and are detailed in the eMethods in the Supplement.
Serious Psychological Distress
Serious psychological distress was defined using the Kessler 6-item screen,16 which assesses past-month nervousness, hopelessness, and other depressive symptoms. Participants with a score of 13 or higher were categorized as having serious psychological distress.17
Heavy Drinking
Heavy drinking was defined according to the US Substance Abuse and Mental Health Services Administration threshold of 5 or more heavy drinking days per 30-day interval over the preceding 12-month span (ie, ≥60 past-year heavy drinking occasions). For men, heavy drinking days were defined as 5 or more drinks per drinking day in all survey years. Due to a questionnaire change, heavy drinking days were specified as 5 or more drinks in 2008 to 2013 surveys and as 4 or more drinks after 2014 for women. Current smoking prevalence trends did not differ between 2008 to 2013 and 2014 to 2017 among female heavy drinkers and nonheavy drinkers, indicating negligible association of the questionnaire change with study results (eResults and eFigure 1 in the Supplement).
Cumulative Disadvantage Index
Status (yes or no) for each of the 6 disadvantages defined above was summed in a cumulative disadvantage index, which was the primary exposure variable in this study, as in previous research.18 Respondents with 5 or 6 disadvantages were collapsed into a single group because of low frequencies.
Covariates
To address confounding of cumulative disadvantage with other demographics or temporal trends,19,20,21,22,23,24 the following were included as covariates: sex, race/ethnicity (non-Hispanic white, Hispanic, or non-Hispanic other), age, survey year (2008-2009, 2010-2011, 2012-2013, 2014-2015, or 2016-2017), and region in which the respondent resided (Northeast, Midwest, South, or West). Further description of survey race/ethnicity question response options is given in the eMethods in the Supplement.
Statistical Analysis
Polytomous regression (logistic regression for nominal outcomes with ≥3 categories) was used to estimate odds ratios (ORs) with 95% CIs for the association of disadvantage variables with smoking status, presented as 3 pairwise contrasts. Each contrast provided unique information about the disparity as follows: (1) current vs never contrasts provide an overall disparity estimate; (2) current vs former contrasts provide an estimate of the unique association with smoking persistence vs cessation, excluding the contribution of disparities in smoking initiation; and (3) former vs never contrasts provide an estimate of the unique association with smoking initiation, excluding the contribution of disparities in cessation. Cumulative disadvantage was modeled as a nominal variable providing 5 contrasts of each level of disadvantage (1, 2, 3, 4, or 5 or 6) to the reference group with 0 disadvantages. To provide a mean estimate of disparities over the 10-year period, models were used to estimate the association of the cumulative disadvantage index and adjustment covariates with smoking status collapsed across survey years. To estimate whether changes in current (vs never) smoking prevalence over time differed by cumulative disadvantage, we then added the 6 respective contrasts for the cumulative disadvantage × continuous 10-level survey year (2008-2017) interaction terms to the model, followed by stratum-specific estimates of the univariable association of survey year with smoking status at each level of cumulative disadvantage. Secondary analyses investigating what forms of disadvantage were associated with smoking involved multivariable polytomous regression models that included the 6 binary disadvantage variables as simultaneous regressors and time trend analyses of each disadvantage indicator as above. Additional sensitivity analyses are described below.
Models included survey year as a regressor and were adjusted for sex, race/ethnicity, age, and region. Results applied sampling weights based on the sociodemographics of the US 2010 Census. Missing data were accounted for using multiple imputation,25 whereby available data were used to estimate and impute plausible values for missing observations in 5 multiply imputed data sets. The association estimates from models tested in each imputed data set were pooled and presented as a single estimate. Analyses were conducted using statistical software (Stata, version 15.1; StataCorp LP).26 Two-tailed tests were used, with statistical significance based on a multiple testing correction using the Benjamini-Hochberg method27 to maintain a study-wise false discovery rate of 0.05.
Results
Descriptive Analyses
Sample sociodemographics by smoking status and survey year in the pooled analytic sample of 278 048 respondents (mean [SD] age, 51.9 [16.8] years; 55.7% female) with data on smoking history available (99.5% of the sample) are listed in Table 1 and show characteristic differences in smoking status by sex, race/ethnicity, and age. Current smoking prevalence, which was 20.8% in 2008-2009, fell to 15.8% by 2016-2017. Former smoking prevalence was 25.0% in 2008-2009 and 25.6% in 2016-2017. Never smoking prevalence rose from 54.2% in 2008-2009 to 58.6% in 2016-2017.
Table 1. Sample Descriptive Statistics and Association of Covariates With Smoking Status.
| Covariate | Prevalence, No. | Prevalence of Smoking Stratified By Covariate Status, Row %a | Association With Smoking Status, OR (95% CI)a,b | ||||
|---|---|---|---|---|---|---|---|
| Never Smoker | Former Smoker | Current Smoker | Current vs Never Smoker | Current vs Former Smoker | Former vs Never Smoker | ||
| Sex | |||||||
| Male | 123 273 | 50.3 | 29.1 | 20.7 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Female | 154 775 | 61.9 | 21.9 | 16.1 | 0.65 (0.63-0.67)c | 1.14 (1.10-1.17)c | 0.57 (0.56-0.58)c |
| Race/ethnicity | |||||||
| Non-Hispanic white | 176 248 | 52.2 | 28.6 | 19.2 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Hispanic | 43 467 | 69.5 | 17.5 | 13.0 | 0.51 (0.49-0.53)c | 0.91 (0.86-0.95)c | 0.56 (0.54-0.58)c |
| Non-Hispanic other | 58 333 | 65.6 | 16.7 | 17.8 | 0.72 (0.69-0.75)c | 1.38 (1.32-1.44)c | 0.52 (0.51-0.54)c |
| Age, y | |||||||
| 25-34 | 53 617 | 64.2 | 13.9 | 21.9 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 35-44 | 50 568 | 62.2 | 17.3 | 20.5 | 0.96 (0.92-1.00)c | 0.75 (0.72-0.79)c | 1.28 (1.22-1.33)c |
| 45-54 | 52 372 | 56.0 | 21.2 | 22.8 | 1.14 (1.10-1.19)c | 0.68 (0.65-0.71)c | 1.68 (1.61-1.75)c |
| 55-64 | 51 315 | 51.0 | 29.6 | 19.4 | 1.06 (1.01-1.10)c | 0.42 (0.40-0.44)c | 2.53 (2.43-2.63)c |
| ≥65 | 70 176 | 51.5 | 39.2 | 9.2 | 0.50 (0.48-0.53)c | 0.15 (0.14-0.16)c | 3.37 (3.25-3.50)c |
| Survey year | |||||||
| 2008-2009 | 44 206 | 54.2 | 25.0 | 20.8 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 2010-2011 | 53 815 | 55.6 | 24.8 | 19.6 | 0.92 (0.89-0.96)c | 0.96 (0.91-1.01) | 0.96 (0.92-1.00)c |
| 2012-2013 | 62 009 | 56.3 | 25.2 | 18.5 | 0.87 (0.83-0.90)c | 0.91 (0.86-0.95)c | 0.96 (0.92-0.99)c |
| 2014-2015 | 63 811 | 58.2 | 25.2 | 16.6 | 0.76 (0.73-0.79)c | 0.83 (0.79-0.87)c | 0.91 (0.88-0.95)c |
| 2016-2017 | 54 207 | 58.6 | 25.6 | 15.8 | 0.73 (0.69-0.77)c | 0.79 (0.75-0.84)c | 0.92 (0.88-0.96)c |
| Region | |||||||
| Northeast | 46 235 | 56.6 | 27.0 | 16.5 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Midwest | 60 223 | 53.2 | 26.0 | 20.9 | 1.27 (1.20-1.35)c | 1.28 (1.20-1.36)c | 1.00 (0.95-1.04) |
| South | 100 247 | 56.9 | 23.9 | 19.3 | 1.20 (1.14-1.27)c | 1.27 (1.20-1.34)c | 0.95 (0.91-0.99)c |
| West | 71 343 | 60.0 | 25.1 | 14.9 | 0.89 (0.83-0.95)c | 0.93 (0.87-0.98)c | 0.96 (0.92-1.00) |
Abbreviation: OR, odds ratio.
Weighted to the US population.
Association between respective covariate and respective smoking status pairwise contrast in multivariable polytomous regression models that included sex, race/ethnicity, age, survey year, and region as simultaneous regressors.
Statistically significant after Benjamini-Hochberg correction to maintain studywise false discovery rate at .05.
As summarized in Table 2, the most and least common disadvantages were disability/limitation (20.0%) and heavy drinking (2.6%), respectively. Twenty-one percent reported 1 disadvantage, and 14.4% were multidisadvantaged, including those facing 2 (8.5%), 3 (3.9%), 4 (1.6%), or 5 or 6 (0.4%) disadvantages.
Table 2. Prevalence of Disadvantages and Smoking Status Stratified by Disadvantage Status Collapsed Across Survey Years, 2008 to 2017.
| Variable | Prevalence of Disadvantage, No. (Column %)a | Prevalence of Smoking Stratified by Disadvantage Status, %a | ||
|---|---|---|---|---|
| Never Smoker | Former Smoker | Current Smoker | ||
| Cumulative Disadvantage Indexb | ||||
| 0 Disadvantages | 152 174 (65.1) | 61.8 | 24.4 | 13.8 |
| 1 Disadvantage | 51 542 (20.5) | 50.3 | 28.3 | 21.4 |
| 2 Disadvantages | 22 558 (8.5) | 46.8 | 26.6 | 26.6 |
| 3 Disadvantages | 10 121 (3.9) | 40.0 | 24.9 | 35.1 |
| 4 Disadvantages | 4433 (1.6) | 32.5 | 21.9 | 45.7 |
| 5 Or 6 disadvantages | 968 (0.4) | 24.0 | 17.8 | 58.2 |
| Difference in Prevalence (95% CI) | ||||
| 1 vs 0 Disadvantages | NA | −11.5 (−12.2 to −10.8) | 3.9 (3.3 to 4.5) | 7.6 (7.1 to 8.1) |
| 2 vs 0 Disadvantages | NA | −15.0 (−15.9 to −14.1) | 2.2 (1.4 to 2.9) | 12.9 (12.1 to 13.6) |
| 3 vs 0 Disadvantages | NA | −21.8 (−23.0 to −20.7) | 0.5 (−0.5 to 1.5) | 21.3 (20.1 to 22.5) |
| 4 vs 0 Disadvantages | NA | −29.3 (−31.1 to −27.6) | −2.6 (−4.1 to −1.1) | 31.9 (30.1 to 33.7) |
| 5 Or 6 vs 0 disadvantages | NA | −37.8 (−40.7 to −34.9) | −6.7 (−9.4 to −3.9) | 44.4 (40.7 to 48.2) |
| Individual Forms of Disadvantagec | ||||
| Unemployed | ||||
| Yes | 21 910 (7.7) | 38.8 | 25.6 | 35.6 |
| No | 248 315 (92.3) | 58.3 | 25.4 | 16.4 |
| Difference in prevalence (95% CI) | NA | −19.5 (−20.3 to −18.7) | 0.2 (−0.5 to 0.9) | 19.3 (18.5 to 20.1) |
| Poverty | ||||
| Yes | 38 160 (13.1) | 49.4 | 18.8 | 31.8 |
| No | 219 596 (86.9) | 57.5 | 26.0 | 16.5 |
| Difference in prevalence (95% CI) | NA | −8.1 (−8.9 to −7.3) | −7.2 (−7.8 to −6.7) | 15.3 (14.7 to 16.0) |
| Low education | ||||
| Yes | 42 195 (13.3) | 50.1 | 24.7 | 25.2 |
| No | 234 555 (86.7) | 57.6 | 25.3 | 17.1 |
| Difference in prevalence (95% CI) | NA | −7.5 (−8.3 to −6.8) | −0.6 (−1.2 to 0.0) | 8.1 (7.5 to 8.7) |
| Disability/limitationd | ||||
| Yes | 56 296 (20.0) | 44.2 | 31.8 | 24.0 |
| No | 221 592 (80.0) | 59.8 | 23.5 | 16.7 |
| Difference in prevalence (95% CI) | NA | −15.6 (−16.1 to −15.0) | 8.3 (7.8 to 8.8) | 7.3 (6.8 to 7.8) |
| Serious psychological distress | ||||
| Yes | 10 352 (3.7) | 36.8 | 21.4 | 41.7 |
| No | 261 451 (96.3) | 57.3 | 25.4 | 17.3 |
| Difference in prevalence (95% CI) | NA | −20.5 (−21.6 to −19.4) | −3.9 (−4.9 to −3.0) | 24.4 (23.3 to 25.5) |
| Heavy drinking | ||||
| Yes | 6744 (2.6) | 27.1 | 24.0 | 48.9 |
| No | 266 439 (97.4) | 57.6 | 25.3 | 17.2 |
| Difference in prevalence (95% CI) | NA | −30.5 (−31.8 to −29.1) | −1.3 (−2.4 to −0.1) | 31.7 (30.3 to 33.2) |
Abbreviation: NA, not applicable.
Weighted to the US population. Differences in prevalence estimates were calculated using data to the hundredths decimal and may not equal differences in presented prevalence in the table because presented values are rounded to tenth place.
Total number of the following disadvantages faced: unemployed, poverty, low education, disability/limitation, serious psychological distress, and heavy drinking.
The Methods section gives the operational definition of each form of disadvantage.
The eMethods in the Supplement describes disability/limitation.
Primary Analysis of the Cumulative Disadvantage Index
Mean Disparities in Smoking Collapsed Across 2008 to 2017
The mean current smoking prevalence collapsed across the 10-year period was successively higher among populations facing 0 (13.8%), 1 (21.4%), 2 (26.6%), 3 (35.1%), 4 (45.7%), or 5 or 6 (58.2%) disadvantages. Table 2 lists differences in never, former, and current smoking prevalence at each level of cumulative disadvantage.
Covariate-adjusted models of associations collapsed across 2008 to 2017 are summarized on the left side of Table 3 and demonstrate compounding increases in odds of current (vs never) smoking with increasing cumulative disadvantage: for 1 vs 0 disadvantages, the OR is 2.34; 95% CI, 2.27-2.43; for 2 vs 0 disadvantages, the OR is 3.55; 95% CI, 3.39-3.72; for 3 vs 0 disadvantages, the OR is 5.35; 95% CI, 5.05-5.66; for 4 vs 0 disadvantages, the OR is 8.59; 95% CI, 7.91-9.34; and for 5 or 6 vs 0 disadvantages, the OR is 14.70; 95% CI, 12.30-17.50. A similar pattern of compounding increases in odds with successively higher levels of cumulative disadvantage was observed with current (vs former) and former (vs never) smoking contrasts, but the ORs were smaller than the ORs for the current vs never smoking contrasts (Table 3).
Table 3. Association of Cumulative Disadvantage Index and Survey Year With Smoking Status Among 278 048 Respondents, 2008 to 2017.
| No. of Disadvantages | Association of Cumulative Disadvantage With Smoking Status Collapsed Across Survey Years, OR (95% CI)a | Time Trend Analysis for Association With Current vs Never Smoking Statusb | |||
|---|---|---|---|---|---|
| Current vs Never Smoker | Current vs Former Smoker | Former vs Never Smoker | Disadvantage × Survey Year Interaction Variable, P Valuec,d,e | Survey Year Variable Stratified by Disadvantage Status, OR (95% CI)c,e | |
| 0 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 0.95 (0.94-0.96)f |
| 1 | 2.34 (2.27-2.43)f | 1.82 (1.75-1.88)f | 1.29 (1.25-1.33)f | .03f | 0.96 (0.95-0.97)f |
| 2 | 3.55 (3.39-3.72)f | 2.58 (2.44-2.73)f | 1.38 (1.32-1.43)f | <.001f | 0.98 (0.97-0.99)f |
| 3 | 5.35 (5.05-5.66)f | 3.52 (3.31-3.75)f | 1.52 (1.43-1.61)f | .001f | 0.99 (0.97-1.01) |
| 4 | 8.59 (7.91-9.34)f | 4.79 (4.33-5.30)f | 1.79 (1.60-2.01)f | .002f | 1.00 (0.97-1.03) |
| 5 or 6 | 14.70 (12.30-17.50)f | 7.12 (5.80-8.74)f | 2.06 (1.61-2.64)f | .69 | 0.96 (0.90-1.04) |
Abbreviation: OR, odds ratio.
Association between regressor and respective smoking status pairwise contrast in multivariable polytomous regression models that included the respective disadvantage variable and with adjustment for sex, race/ethnicity, age, survey year, and region weighted to the US population.
Time trend analysis of footnote a.
Year treated as a 10-level continuous variable (2008-2017).
Interaction term added in subsequent model; all other results are from models that excluded interaction term.
Total number of the following disadvantages faced: unemployed, poverty, low education, disability/limitation, serious psychological distress, and heavy drinking. The Methods section gives the operational definition of each form of disadvantage. The eMethods in the Supplement describes disability/limitation.
Statistically significant after Benjamini-Hochberg correction to maintain studywise false discovery rate at 0.05.
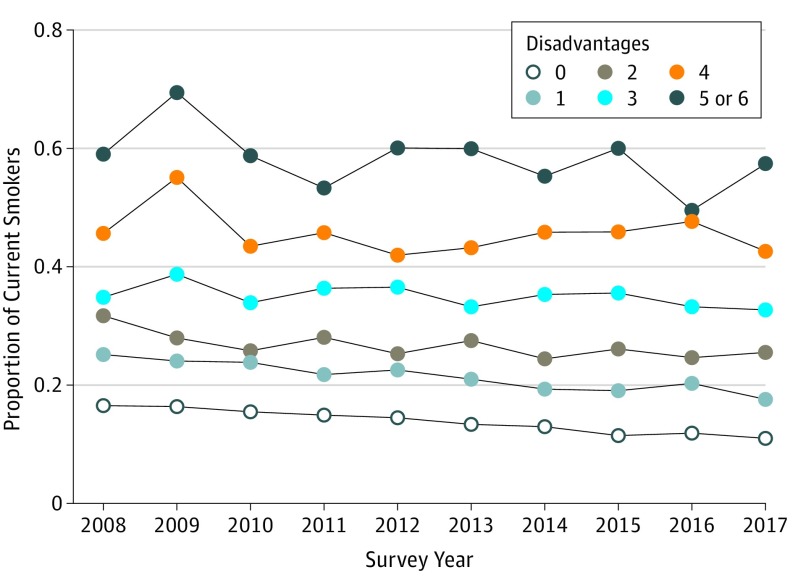
Association of Cumulative Disadvantage With Smoking Trends Over Time
Current smoking prevalence across 2008 to 2017 at each level of cumulative disadvantage is shown in the Figure. Results of time trend analyses are summarized on the right-hand side of Table 3 and show that the change in covariate-adjusted odds of current (vs never) smoking per year from 2008 to 2017 significantly differed by cumulative disadvantage, evidenced by significant disadvantage × survey year terms for each interaction contrast, except for the 5 or 6 (vs 0) disadvantages contrast. A significant annual reduction in current (vs never) smoking odds from 2008 to 2017 was found for populations with 0 (OR for the change in odds of smoking per year, 0.951; 95% CI, 0.944-0.958), 1 (OR, 0.96; 95% CI, 0.95-0.97), or 2 (OR, 0.98; 95% CI, 0.97-0.99) disadvantages. Odds of current (vs never) smoking did not significantly change across 2008 to 2017 among those with 3 (OR for the change in odds of smoking per year, 0.99; 95% CI, 0.97-1.01), 4 (OR, 1.00; 95% CI, 0.97-1.03), or 5 or 6 (OR, 0.96; 95% CI, 0.90-1.04) disadvantages.
Figure. Proportion of Current Smokers by Cumulative Disadvantagea in Each Year, National Health Interview Survey, 2008 to 2017b.
aTotal number of the following disadvantages: unemployed, poverty, no high school degree, disability/limitation, serious psychological distress, and heavy drinking. The Methods section gives the operational definition of each form of disadvantage. The eMethods in the Supplement describes disability/limitation.
bWeighted to the US population (n = 241 796).
Secondary Analyses of Each Type of Disadvantage
The left side of Table 4 summarizes results of a multivariable model that included the 6 disadvantages as simultaneous regressors, adjusting for their co-occurrence and other covariates collapsed across years. Positive associations with current (vs never), current (vs former), and former (vs never) smoking were observed for each form of disadvantage, indicating nonredundant sources of smoking disparities across disadvantage indicators, except for a null association of poverty with former (vs never) smoking. As summarized on the right-hand side of Table 4 and in eFigure 2 in the Supplement, covariate-adjusted interactions of survey year with unemployment, poverty, low education, disability/limitation, and serious psychological distress were each significantly associated with current (vs never) smoking, indicating the magnitude of reduction in current smoking odds across 2008 to 2017 was slower among those with (vs without) the respective disadvantage. Trends in current (vs never) smoking over time did not significantly differ by heavy drinking. Additional analyses reported in the eResults in the Supplement indicated that multicollinearity among disadvantage variables had no substantive association with the accuracy of association estimates from the model.
Table 4. Association of Each Form of Disadvantage With Smoking Status Among 278 048 Respondents, 2008 to 2017.
| Disadvantage | Association With Smoking Status Collapsed Across Survey Years, OR (95% CI)a | Time Trend Analysis for Association With Current vs Never Smoking Statusb | |||
|---|---|---|---|---|---|
| Current vs Never Smoker | Current vs Former Smoker | Former vs Never Smoker | Disadvantage × Survey Year Interaction Variable, P Valuec,d | Survey Year Variable Stratified by Disadvantage Status, OR (95% CI)c | |
| Unemployed | |||||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 0.96 (0.95-0.96)e |
| Yes | 1.83 (1.73-1.93)e | 1.44 (1.36-1.52)e | 1.27 (1.21-1.33)e | .002e | 0.98 (0.96-0.99)e |
| Poverty | |||||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 0.96 (0.95-0.96)e |
| Yes | 1.81 (1.74-1.88)e | 1.89 (1.81-1.97)e | 0.96 (0.92-1.00) | <.001e | 0.98 (0.97-0.99)e |
| Low education | |||||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 0.96 (0.95-0.96)e |
| Yes | 1.69 (1.63-1.76)e | 1.60 (1.50-1.64)e | 1.08 (1.04-1.12)e | <.001e | 0.99 (0.98-1.00) |
| Disability/limitation | |||||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 0.95 (0.95-0.96)e |
| Yes | 1.42 (1.37-1.47)e | 1.13 (1.08-1.18)e | 1.26 (1.22-1.30)e | <.001e | 0.98 (0.97-0.99)e |
| Serious psychological distress | |||||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 0.96 (0.95-0.96)e |
| Yes | 2.25 (2.12-2.38)e | 1.83 (1.71-1.95)e | 1.23 (1.15-1.32)e | .02e | 0.98 (0.96-1.00)e |
| Heavy drinking | |||||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 0.96 (0.95-0.96)e |
| Yes | 4.83 (4.48-5.21)e | 2.47 (2.29-2.66)e | 1.96 (1.80-2.13)e | .42 | 0.97 (0.94-0.99)e |
Abbreviation: OR, odds ratio.
Association between regressor and respective smoking status pairwise contrast in multivariable polytomous regression models that included unemployment, poverty, low education, disability/limitation, serious psychological distress, and heavy drinking as simultaneous regressors adjusted for sex, race/ethnicity, age, survey year, and region weighted to the US population. The Methods section gives the operational definition of each form of disadvantage. The eMethods in the Supplement describes disability/limitation.
Time trend analysis of footnote a.
Year treated as a 10-level continuous variable (2008-2017).
Interaction term added in subsequent model; all other results are from models that excluded interaction term.
Statistically significant after Benjamini-Hochberg correction to maintain studywise false discovery rate at 0.05.
Sensitivity Analyses Testing Alternate Specifications of Cumulative Disadvantage
Sensitivity analyses were performed comparing the association with smoking status across different specifications of the cumulative disadvantage variable. The categorical 6-level specification used above was optimal relative to 4 alternate specifications due to high parsimony, without sacrificing precision (eResults and eTable in the Supplement).
Discussion
This study reveals an emerging pattern of smoking disparities in the United States among populations facing multiple forms of disadvantage. Previous publications on this topic found additive associations of certain combinations of markers of low socioeconomic status and behavioral health conditions with current smoking.2,3 Those studies did not report estimates of smoking risk along a continuum of cumulative disadvantage, trends over time, or distinctions between former and never smoking, which are addressed herein.
New evidence is provided in this study that indicates the probability of smoking successively increases as the cumulative number of disadvantages faced by a population rises, without leveling off at any threshold of disadvantage. The 6 disadvantages included in this study’s cumulative disadvantage index each represent different groups specified by public health organizations as “tobacco use disparity populations” that merit priority in tobacco control policy.2,3,4,5 While these disadvantages are heterogeneous in certain respects (eg, health related vs socioeconomic), they share commonalities of being unduly stigmatized and being associated with high risk of smoking. The present findings suggest that considering such disadvantages distinctly in tobacco control and regulatory policy agendas may overlook a broader pattern occurring recently in the epidemiology of smoking in the United States such that (1) disadvantage is a common denominator across various populations at risk for smoking and (2) disparities in smoking vary along a continuum in which the cumulative number of different disadvantages faced aligns with the magnitude of disparity. How this pattern can inform a cohesive policy agenda is unknown, but it is clear from these findings that the crux of the recently expanding tobacco-related health disparity problem in the United States is not tied to groups facing merely a single form of disadvantage.
Evidence reported herein that cumulative disadvantage is associated with both current vs former and former vs never smoking contrasts suggests that smoking disparities in multidisadvantaged populations reflect a combination of reduced odds of smoking cessation and increased odds of smoking initiation. The corresponding implication that prevention and cessation may both be needed to appreciably reduce smoking disparities is merited with qualifications. First, the NHIS provides an annual cross-sectional snapshot of the US population; some former smokers may later relapse back to smoking, and some current smokers will quit, which cannot be addressed without follow-up. Second, this study does not identify the timing of smoking initiation or cessation. Third, relative to current vs never smoker contrasts, the ORs for current vs former smoker contrasts were smaller, and the ORs for former vs never smoker contrasts were considerably reduced.
This study is among the first published articles with updated national estimates of smoking disparities through 2017. Much has changed in the US tobacco landscape recently, including increases in the marketing and use of noncigarette tobacco products, higher cigarette prices, more clean indoor air laws, new antismoking public education campaigns, and other tobacco control policy and systems-level changes that discourage smoking.15,28 Concurrent with such changes was a marked reduction in smoking prevalence among the overall US population from 2008 to 2017, which according to the present findings was driven mainly by substantial declines in smoking rates among those with 0 or 1 disadvantage. Whether multidisadvantaged groups are exposed to fewer tobacco control and regulatory efforts than the general population or whether antismoking measures are simply less effective in lowering smoking rates or less likely to reach multidisadvantaged populations warrants consideration. Some locations have fewer tobacco use–deterring policies or preventive health services that discourage smoking.29 While national region was adjusted for in the present analysis, differences in tobacco control and regulatory measures by county, city, or neighborhood exist,30 which may be a possible source of the disparities associated with cumulative advantage found in this study. In smoking cessation clinical trials in which intervention exposures are standardized across study participants, socioeconomic and health-related disadvantages still predict poorer quit outcomes.4 Consequently, reduced effectiveness in promoting behavior change (and not merely reduced reach) of some tobacco control and regulatory measures might be one contributor to the disparities observed herein.
The reason why smoking is disproportionately common in multidisadvantaged populations may be attributable to the accumulation of multiple bidirectional mechanisms of association.4 At the environmental level, disadvantaged communities may be more densely populated with tobacco retailers, exposed to targeted tobacco industry advertising, marketed cigarettes with higher nicotine levels, and characterized by social acceptance of smokers.4,31 At the individual level, socioeconomic or health-related disadvantages may cause stress, interfere with healthy decisions prioritizing longevity over smoking, or reduce opportunities for pleasure and life satisfaction, leading individuals to resort to smoking as a coping mechanism or key source of enjoyment.32,33 Pathways from smoking to disadvantage have been reported. Smoking lowers subsequent odds of gaining employment and expendable income.34,35 Nicotine dysregulates neural circuitry implicated in mental illness36 and may increase desire to drink alcohol.37 While smoking certainly causes disease, including some conditions involved in this study’s disability/limitation variable,1 smoking-related illness can also motivate some smokers to quit,38 which might explain why the disparity in quitting estimates (ie, current vs former smoking) by disability/limitation observed herein was modest.
Limitations
This study is subject to some limitations. The cross-sectional design precludes temporal or causal inferences. Also, this study did not address smoking heaviness, chronicity, or dependence level or use of noncigarette tobacco products and biomarkers of tobacco exposure, which may overlap with disadvantage.31 Because our study aimed to provide a parsimonious operationalization of cumulative disadvantage, some tobacco use disparity populations were not incorporated due to methodological and conceptual complexities (eg, incarcerated individuals are not sampled in the NHIS, and the complex association of race/ethnicity or sex/gender identity with smoking cannot be operationalized as a binary variable like the other disadvantage indicators).4 Furthermore, data on population density, which is associated with smoking,30 were not available. In addition, the behavioral health measures were assessed using brief screeners and may not capture certain manifestations of mental health problems or illicit drug use disorders associated with smoking.39,40
Finally, the objective of our study was to quantify (but not explain the root causes of) disparities in smoking prevalence. Accordingly, bivariate associations were tested, which do not accurately model the complex etiological mechanisms underlying multiple disadvantage, smoking, and their association. The troubling reality of health and social inequity is that different forms of disadvantage influence one another and smoking in complex reciprocal cycles (eg, heavy drinking may lead to and result from psychological distress, both of which may cause employment termination, loss of income, and disability, as well as increase smoking).32 Descriptive analyses of disparities in smoking prevalence like those presented herein are capable of identifying which populations should be prioritized in tobacco control interventions. Identifying interventions that are most likely to be successful will necessitate future hypothesis-driven work aimed to model and explain the mechanisms underlying tobacco-related health disparities.
Conclusions
Results of this study demonstrate that recent disparities in the prevalence of smoking among US adults who were 25 years or older are disproportionately accounted for by populations facing multiple forms of socioeconomic or health-related disadvantage. The present results also indicate that such disparities are likely due to increased probability of smoking initiation and lower probability of smoking cessation. In addition, this study demonstrates that the magnitude of disparities in current smoking associated with cumulative disadvantage has widened from 2008 to 2017. Successful prevention of smoking initiation and promotion of smoking cessation in multidisadvantaged populations would substantially reduce the smoking-related public health burden in the United States.
eMethods. Supplemental Methods
eResults. Supplemental Results
eFigure 1. Percentage of Current Smokers Among Females by Heavy Drinking Status, 2008-2013
eFigure 2. Proportion of Current Smokers in Each Survey Year, by Each Form of Disadvantage, National Health Interview Survey, 2008-2017
eTable. Pseudo R2 Values From Regression Models With Alternate Specifications of Cumulative Disadvantage
References
- 1.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General Atlanta, GA: Centers for Disease Control and Prevention; 2014. Reports of the Surgeon General. Medline: 24455788 [PubMed] [Google Scholar]
- 2.Higgins ST, Kurti AN, Redner R, et al. Co-occurring risk factors for current cigarette smoking in a U.S. nationally representative sample. Prev Med. 2016;92:110-117. doi: 10.1016/j.ypmed.2016.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaalema DE, Leventhal AM, Priest JS, Higgins ST. Understanding individual differences in vulnerability to cigarette smoking is enhanced by attention to the intersection of common risk factors. Prev Med. 2018;117:38-42. doi: 10.1016/j.ypmed.2018.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Cancer Institute Monograph 22: A Socioecological Approach to Addressing Tobacco-Related Health Disparities. Bethesda, MD: National Cancer Institute, National Institutes of Health, US Dept of Health and Human Services; 2017. [Google Scholar]
- 5.Williams JM, Steinberg ML, Griffiths KG, Cooperman N. Smokers with behavioral health comorbidity should be designated a tobacco use disparity group. Am J Public Health. 2013;103(9):1549-1555. doi: 10.2105/AJPH.2013.301232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parsons VL, Moriarity C, Jonas K, Moore TF, Davis KE, Tompkins L. Design and estimation for the national health interview survey, 2006-2015. Vital Health Stat 2. 2014;(165):1-53. [PubMed] [Google Scholar]
- 7.Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current cigarette smoking among adults: United States, 2005-2015. MMWR Morb Mortal Wkly Rep. 2016;65(44):1205-1211. doi: 10.15585/mmwr.mm6544a2 [DOI] [PubMed] [Google Scholar]
- 8.Clarke TC, Christ SL, Soler-Vila H, et al. Working with cancer: health and employment among cancer survivors. Ann Epidemiol. 2015;25(11):832-838. doi: 10.1016/j.annepidem.2015.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flint AJ, Novotny TE. Poverty status and cigarette smoking prevalence and cessation in the United States, 1983-1993: the independent risk of being poor. Tob Control. 1997;6(1):14-18. doi: 10.1136/tc.6.1.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cuffe SP, Moore CG, McKeown R. ADHD and health services utilization in the National Health Interview Survey. J Atten Disord. 2009;12(4):330-340. doi: 10.1177/1087054708323248 [DOI] [PubMed] [Google Scholar]
- 11.Kaplan MS, Huguet N, Newsom JT, McFarland BH. The association between length of residence and obesity among Hispanic immigrants. Am J Prev Med. 2004;27(4):323-326. doi: 10.1016/j.amepre.2004.07.005 [DOI] [PubMed] [Google Scholar]
- 12.Syamlal G, King BA, Mazurek JM. Tobacco use among working adults: United States, 2014-2016. MMWR Morb Mortal Wkly Rep. 2017;66(42):1130-1135. doi: 10.15585/mmwr.mm6642a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang N, Gonzalez M, Ling PM, Glantz SA. Relationship of smokefree laws and alcohol use with light and intermittent smoking and quit attempts among US adults and alcohol users. PLoS One. 2015;10(10):e0137023. doi: 10.1371/journal.pone.0137023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phillips E, Wang TW, Husten CG, et al. Tobacco product use among adults: United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66(44):1209-1215. doi: 10.15585/mmwr.mm6644a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jamal A, Phillips E, Gentzke AS, et al. Current cigarette smoking among adults: United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(2):53-59. doi: 10.15585/mmwr.mm6702a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184-189. doi: 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959-976. doi: 10.1017/S0033291702006074 [DOI] [PubMed] [Google Scholar]
- 18.Appleyard K, Egeland B, van Dulmen MH, Sroufe LA. When more is not better: the role of cumulative risk in child behavior outcomes. J Child Psychol Psychiatry. 2005;46(3):235-245. doi: 10.1111/j.1469-7610.2004.00351.x [DOI] [PubMed] [Google Scholar]
- 19.England P, Garcia-Beaulieu C, Ross M. Women’s employment among blacks, whites, and three groups of Latinas: do more privileged women have higher employment? Gend Soc. 2004;18(4):494-509. doi: 10.1177/0891243204265632 [DOI] [Google Scholar]
- 20.Bratter JL, Eschbach K. Race/ethnic differences in nonspecific psychological distress: evidence from the National Health Interview Survey. Soc Sci Q. 2005;86(3):620-644. doi: 10.1111/j.0038-4941.2005.00321.x [DOI] [Google Scholar]
- 21.Hardaway CR, McLoyd VC. Escaping poverty and securing middle class status: how race and socioeconomic status shape mobility prospects for African Americans during the transition to adulthood. J Youth Adolesc. 2009;38(2):242-256. doi: 10.1007/s10964-008-9354-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hughes N, Closs SJ, Clark D. Experiencing cancer in old age: a qualitative systematic review. Qual Health Res. 2009;19(8):1139-1153. doi: 10.1177/1049732309341715 [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Berglund PA, Bruce ML, et al. The prevalence and correlates of untreated serious mental illness. Health Serv Res. 2001;36(6, pt 1):987-1007. [PMC free article] [PubMed] [Google Scholar]
- 24.Lui CK, Kerr WC, Mulia N, Ye Y. Educational differences in alcohol consumption and heavy drinking: an age-period-cohort perspective. Drug Alcohol Depend. 2018;186:36-43. doi: 10.1016/j.drugalcdep.2017.12.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Hoboken, NJ: John Wiley & Sons; 2004. [Google Scholar]
- 26.StataCorp LP Stata Base Reference Manual, Release 15.1. College Station, TX: Stata Press; 2015. [Google Scholar]
- 27.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57(1):289-300. https://www.jstor.org/stable/2346101. Accessed July 15, 2018. [Google Scholar]
- 28.Farrelly MC, Chaloupka FJ, Berg CJ, et al. Taking stock of tobacco control program and policy science and impact in the United States. J Addict Behav Ther. 2017;1(2):8. [PMC free article] [PubMed] [Google Scholar]
- 29.Tauras JA, Chaloupka FJ, Farrelly MC, et al. State tobacco control spending and youth smoking. Am J Public Health. 2005;95(2):338-344. doi: 10.2105/AJPH.2004.039727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Drope J, Liber AC, Cahn Z, et al. Who’s still smoking? disparities in adult cigarette smoking prevalence in the United States. CA Cancer J Clin. 2018;68(2):106-115. doi: 10.3322/caac.21444 [DOI] [PubMed] [Google Scholar]
- 31.Higgins ST, Redner R, Priest JS, Bunn JY. Socioeconomic disadvantage and other risk factors for using higher-nicotine/tar-yield (regular full-flavor) cigarettes. Nicotine Tob Res. 2017;19(12):1425-1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leventhal AM. The sociopharmacology of tobacco addiction: implications for understanding health disparities. Nicotine Tob Res. 2016;18(2):110-121. doi: 10.1093/ntr/ntv084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bickel WK, Moody L, Quisenberry AJ, Ramey CT, Sheffer CE. A Competing Neurobehavioral Decision Systems model of SES-related health and behavioral disparities. Prev Med. 2014;68:37-43. doi: 10.1016/j.ypmed.2014.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prochaska JJ, Michalek AK, Brown-Johnson C, et al. Likelihood of unemployed smokers vs nonsmokers attaining reemployment in a one-year observational study. JAMA Intern Med. 2016;176(5):662-670. doi: 10.1001/jamainternmed.2016.0772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Widome R, Joseph AM, Hammett P, et al. Associations between smoking behaviors and financial stress among low-income smokers. Prev Med Rep. 2015;2:911-915. doi: 10.1016/j.pmedr.2015.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jackson KJ, Muldoon PP, De Biasi M, Damaj MI. New mechanisms and perspectives in nicotine withdrawal. Neuropharmacology. 2015;96(Pt B):223-234. . doi: 10.1016/j.neuropharm.2014.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Verplaetse TL, McKee SA. An overview of alcohol and tobacco/nicotine interactions in the human laboratory. Am J Drug Alcohol Abuse. 2017;43(2):186-196. doi: 10.1080/00952990.2016.1189927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Buchbinder M, Wilbur R, Zuskov D, McLean S, Sleath B. Teachable moments and missed opportunities for smoking cessation counseling in a hospital emergency department: a mixed-methods study of patient-provider communication. BMC Health Serv Res. 2014;14:651. doi: 10.1186/s12913-014-0651-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weinberger AH, Pilver CE, Desai RA, Mazure CM, McKee SA. The relationship of dysthymia, minor depression, and gender to changes in smoking for current and former smokers: longitudinal evaluation in the U.S. population. Drug Alcohol Depend. 2013;127(1-3):170-176. doi: 10.1016/j.drugalcdep.2012.06.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Higgins ST. Editorial: 3rd Special Issue on behavior change, health, and health disparities. Prev Med. 2016;92:1-5. doi: 10.1016/j.ypmed.2016.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Supplemental Methods
eResults. Supplemental Results
eFigure 1. Percentage of Current Smokers Among Females by Heavy Drinking Status, 2008-2013
eFigure 2. Proportion of Current Smokers in Each Survey Year, by Each Form of Disadvantage, National Health Interview Survey, 2008-2017
eTable. Pseudo R2 Values From Regression Models With Alternate Specifications of Cumulative Disadvantage