Abstract
Recent studies show that higher-order appetitive neural circuitry may contribute to restricted eating in anorexia nervosa (AN) and overeating in bulimia nervosa (BN). The purpose of this study was to determine whether sensitization effects might underlie pathologic eating behavior when a taste stimulus is administered repeatedly. Recovered AN (RAN, n=14) and BN (RBN, n=15) subjects were studied in order to avoid the confounding effects of altered nutritional state. Functional magnetic resonance imaging (fMRI) measured higher-order brain response to repeated tastes of sucrose (caloric) and sucralose (non-caloric). To test sensitization, the neuronal response to the first and second administration was compared. RAN patients demonstrated a decreased sensitization to sucrose in contrast to RBN patients who displayed the opposite pattern, increased sensitization to sucrose. However, the latter was not as pronounced as in healthy control women (n=13). While both eating disorder subgroups showed increased sensitization to sucralose, the healthy controls revealed decreased sensitization. These findings could reflect on a neuronal level the high caloric intake of RBN during binges and the low energy intake for RAN. RAN seem to distinguish between high energy and low energy sweet stimuli while RBN do not.
Keywords: eating disorders, fMRI, sensitization, habituation, taste
1. Introduction:
Anorexia nervosa (AN) and bulimia nervosa (BN) are disorders of multidimensional etiology and have their onset often during adolescence (APA, 2000). They are characterized by dysfunctional eating behavior and distorted body image, and have high rates of chronicity, morbidity, and mortality. AN patients show severe emaciation and two relatively distinct types of eating behaviors: caloric restriction (restricting-type AN) and alternating restrictive eating and episodes of purging and/or binge eating (binging/purging-type AN). In contrast, individuals with BN are not emaciated, maintaining an average body weight (ABW) above 85% of minimum suggested guidelines, with typical episodes of overeating followed by compensatory behaviors such as vomiting, fasting, misuse of laxatives, or over-exercising.
Few studies have investigated gustatory processing in subjects with AN or BN simultaneously. However, a considerable number of studies have suggested that neuronal activation of gustatory pathways involving the anterior insula, orbitofrontal cortex (OFC), anterior cingulate cortex (ACC), striatum, and amygdala may contribute to disturbed appetite regulation in eating disorders (Bohon and Stice, 2011; Cowdrey et al., 2011; Frank et al., 2011; Frank et al., 2013; Oberndorfer et al., 2013; Radeloff et al., 2012; Vocks et al., 2011; Wagner et al., 2008).
Theoretically, differences in pathological eating behaviors in AN and BN could be related to altered perception and/or modulation of satiety and habituation. For example, feeding may elicit exaggerated satiety in AN and reduced satiety in BN (Oberndorfer et al., 2013). The decrease of the hedonic response to a food that is repeatedly consumed, known as sensory-specific satiety (Rolls et al., 1981), has been shown to have a neural basis. Kringelbach et al. (Kringelbach et al., 2003) reported decreased activation of regions within the OFC to repeated food consumption in individuals with AN.
In the present study, we applied two separate runs of a sequential stimulus paradigm to subjects who were recovered from AN and BN and compared their response to the first and second administration of a sweet stimulus to detect possible underlying sensitization (initial increase in response) and related habituation effects (later reduction in response). We hypothesized strong sensitization patterns in subjects with BN, in contrast to minimal sensitization in subjects with AN. This would indicate a neural basis for these motivated eating patterns and potentially may help to explain differences in pathologic eating behavior in these two groups. By testing both sucralose and sucrose, we could also determine if these mechanisms were particularly sensitive to sweet taste and/or energy content. Sucralose (Splenda©)was chosen as the non-caloric sweet contrast condition because it is similar to sucrose in taste, molecular make-up, and recognition by tongue sweet receptors (Chandraskekar et al., 2006), but lacks its caloric properties (Knight, 1994).
In order to avoid the confounding effects of altered nutritional state, we recruited recovered AN and BN subjects. It is important to emphasize that core temperament and personality traits persist after recovery from both AN and BN and are similar to symptoms described premorbidly in childhood (Wagner et al., 2006b). Thus, psychophysiological disturbances may be traits. However, even if these disturbances are “scars,” this can aid in our understanding of processes pertinent to these disorders.
2. Methods:
2.1. Study Participants:
We studied 14 women recovered from anorexia nervosa (RAN), 15 women recovered from bulimia nervosa (RBN), and compared them to 13 volunteer ‘control women’ (CW) of similar age and weight (Table 1). All participants gave written informed consent, and the UCSD institutional review board approved this study. Recovery intervals were similar for RAN and RBN (Table 1). Trained clinicians administered the Structured Clinical Interview for DSM-IV Axis I Disorders to assess inclusion/exclusion criteria (First et al., 1996). RAN lost weight purely by restricted dieting and had no history of binge eating or purging. RBN individuals had a history of past binge eating and purging behaviors, but had never been emaciated and had maintained a weight above 85% average body weight (ABW). RAN and RBN subjects must have had: (a) No restrictive eating or other eating disorder related behaviors in the preceding 12 months; (b) A stable weight (± 3.0 kg) between 90% and 120% ABW for at least 12 months (Metropolitan Life Insurance Company, 1959); (c) Regular menstrual cycles for the preceding 12 months; and (d) Normal plasma b-hydroxybutyric acid (BHBA), glucose, and insulin concentrations during the evaluation phase as previously described (Kaye et al., 1991;Kaye et al., 1998; Srinivasagam et al., 1995). CW had no history of an eating disorder or any psychiatric or serious medical or neurological illness, no first-degree relatives with an eating disorder, and had been within normal weight range since menarche. All subjects had normal menses and were studied during the early follicular phase of the menstrual cycle. Subjects were not allowed to be on medication within 30 days prior to the study.
Table 1.
Demographic variables of group.
| Variable | CW (n=13) | RAN (n=15) | RBN (n=14) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | F | p | Group Differences | |
| Study age (years) | 26.3 | 5.9 | 26.4 | 5.4 | 27.4 | 6.8 | .122 | 0.886 | |
| Current BMI (kg/m2) | 22.4 | 1.5 | 20.9 | 2.8 | 22.5 | 2.0 | 2.252 | 0.120 | |
| Lowest past BMI (kg/m2) | 20.8 | 1.4 | 14.8 | 2.6 | 19.6 | 1.5 | 36.12 | <0.001 | RAN<CW,RBN |
| Highest past BMI (kg/m2) | 23.2 | 1.6 | 23.6 | 3.7 | 25.0 | 2.0 | 1.667 | 0.203 | |
| Age of onset (years) | 16.3 | 3.8 | 17.5 | 3.7 | .760 | 0.312 | |||
| Length of recovery (mths) | 58.4 | 69.4 | 44.3 | 47.2 | .346 | 0.562 | |||
| BDI (Total) | 3.4 | 2.9 | 6.5 | 3.4 | 4.4 | 4.5 | 2.520 | 0.094 | |
| Novelty Seeking / TCI | 21.5 | 5.4 | 18.4 | 6.2 | 22.1 | 4.2 | 1.978 | 0.152 | |
| Harm Avoidance / TCI | 9.6 | 4.7 | 13.9 | 7.0 | 14.6 | 6.7 | 2.480 | 0.097 | |
| Spielberger State Anxiety | 26.6 | 9.0 | 28.6 | 10.2 | 31.0 | 12.2 | 0.584 | 0.563 | |
| Y-BOCS (Total) | 0.0 | 0.0 | 6.6 | 8.3 | 5.6 | 8.7 | .321 | 0.052 | |
Table 1: Group comparisons by one-way analysis of variance (ANOVA) are presented.
CW =healthy control women; RAN =women recovered from anorexia nervosa, restricting type; RBN = women recovered from bulimia nervosa; BDI=Beck Depression Inventory; TCI=Temperament and Character Inventory; Y-BOCS=Yale Brown Obsessive Compulsive Scale
2.2. Assessments:
A comprehensive description of the battery is described elsewhere (Wagner et al., 2006b). In brief, current symptoms were assessed by the Beck Depression Inventory (BDI)(Beck et al., 1961), Yale- Brown Obsessive Compulsive Scale (Y-BOCS)(Goodman et al., 1989), State Trait Anxiety Inventory (STAI-Y)(Spielberger et al., 1970) and the Temperament and Character Inventory (TCI) (Cloninger et al., 1994).
2.3. Brain Imaging Procedures:
Subjects were instructed to fast overnight and arrived at the fMRI facility between 7 and 8 AM. Subjects received a standardized breakfast of 600 total calories.
2.4. Taste Solution Delivery:
Sucrose and Splenda© (generic sucralose) solutions were delivered with a programmable syringe pump (J-Kem Scientific, St. Louis MO) in 1 mL per second stimulations (Frank et al., 2003). Two sterile silicone tubes were placed securely in the center of the tongue immediately adjacent to each other. Subjects were told that they were going to experience sweet tastes every 20 seconds. They were instructed to keep their eyes closed during the scan, to swish once and swallow after each taste stimulus, and to avoid sucking on the tubes. Four blocks of sweet taste stimulation were applied: two runs of sucrose and two runs of sucralose. Sucrose runs used a 10% concentration of sucrose (Mallinckrodt, USA). Sucralose runs used a sucralose solution individually matched to sweet taste perception of the sucrose solution (detailed description see Frank et al., 2008; Oberndorfer et al., 2013). Sweet tastes were delivered in pseudo-randomized order. Each block consisted of 20 one-mL taste stimulations 20 seconds apart, all taste stimulations within a given trial were either sucrose or sucralose.
2.5. Sensitization Analysis:
To test sensitization we compared activation from the first administration of a solution (sucrose/sucralose) to the second administration of the solution. In detail, for each subject and for each region, a mean time series was extracted from first and second administration for the given solution. The mean signal for each trial type (condition by administration) and for each region was then calculated. The mean time series across all blocks was used to test the effect of condition type (sucrose/sucralose), and the difference in signal across the blocks (first administration/second administration) was used to test for sensitization and related habituation effects. Sensitization was treated as a categorical phase so as to avoid colinearity with the noise regressors of no interest in the deconvolution (i.e., linear regressor).
The data presented in this study are derived solely from these blocks. Individuals also experienced two pseudo-randomized blocks where 10 stimulations were sucrose and 10 stimulations were sucralose. The data from this analysis have been presented in a separate manuscript (Oberndorfer et al., 2013). All blocks were delivered randomly and the session order did not significantly affect sensitization results. Subjects ingested a total of 6 grams sucrose (24 Kcal) over 30 minutes.
2.6. FMRI Acquisition:
Imaging experiments were performed on a 3T GE CXK4 Magnet, with a three-plane scout scan (16 seconds), a sagitally acquired spoiled gradient recalled (SPGR) sequence (T1-weighted, 172 slices thickness 1mm, TI=450ms, TR=8ms, TE=4ms, flip angle=12°, FOV=250×250mm,192×256 matrix interpolated to 256×256), and T2* weighted echo-planar imaging (EPI) scans to measure BOLD functional activity during taste stimulation (3.43×3.43×2.6 mm voxels, TR=2 seconds, TE=30ms, flip angle=90°, and 32 axial slices, 64×64 matrix, 2.6mm slice thickness and 1.4mm gap).
2.7. FMRI Preprocessing:
Images were processed with the Analysis of Functional NeuroImages (AFNI) software (Cox, 1996). In order to minimize motion artifact, echo-planar images were realigned to the 100th acquired scan. Data points beyond 1mm from the 100th scan, in x/y/z, were censored from further analysis. Additionally, data were time-corrected for slice acquisition order, and spikes in the hemodynamic time course were removed and replaced with an interpolated value from adjacent time points using 3dDespike. A multiple regression model was used whereby regressors derived from the experimental paradigm were convolved with a prototypical hemodynamic response function (Boynton et al., 1996), including five nuisance regressors: three movement regressors to account for residual motion (in the roll, pitch, and yaw directions), and regressors for baseline and linear trends to account for signal drifts. To account for individual anatomical variations, a Gaussian filter with full width at half maximum 6.0 mm was applied to the voxel-wise percent signal change data. All functional data were normalized to Talairach coordinates.
2.8. FMRI Analysis:
A whole brain analysis was applied in which a cluster/threshold method was used to control for multiple comparisons. In detail, voxel-wise percent signal change data for the whole brain was analyzed using linear mixed effects model using AFNI function 3dLME with group(CW/RAN/RBN), substance (SUC/SPL), and sensitization (1st Administration/2nd Administration) as fixed factors and subject as a random factor. Brain effects for significant sensitization, group × sensitization, and group × substance × sensitization effects were examined. The group, group × substance effects and substance effects have been previously published in an almost identical group (Oberndorfer et al., 2013), and to avoid duplication are not included in this manuscript. To determine voxel level effects on the extracted regions from the main analysis three additional LMEs were performed in each group with just substance and sensitization. A threshold adjustment method based on Monte-Carlo simulations was used to guard against identifying false positive areas of activation. A priori voxel-wise probability of p< 0.05 in a cluster of 1920mm3(30 voxels) resulted in an a-posteriori probability of p <0.05. Thus only contiguous voxels, a group of at least 30 voxels, are reported. The T value for each voxel was extracted and the average T value across these contiguous voxels is reported in the tables. To allow for post-hoc correlations, the average percent signal difference (for all voxels in the cluster) was extracted from regions of activation that were found to survive this threshold/cluster method. All analyses for the behavioral data were carried out with SPSS 18.0. To determine whether variance in neural activation for group or task clusters could be explained by psychological variables, we correlated percent signal change during taste processing phases with response to psychological measures.
3. Results:
3.1. Imaging Analysis:
3.1.1. Sensitization Results:
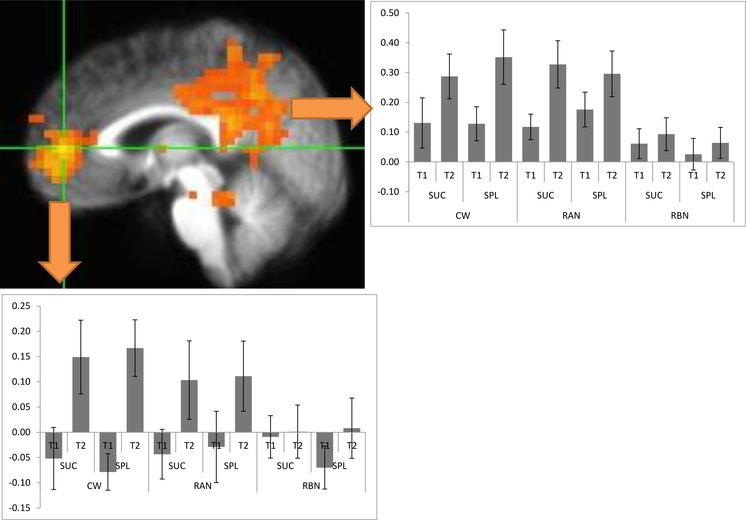
The sensitization analysis showed significant effects in the right posterior cingulate, right medial frontal gyrus, right thalamus, left thalamus, left precentral gyrus, and right culmen (Table 2). As can be seen in Figure 1, while all groups showed some sensitization effects in regions, such as the posterior cingulate and medial frontal gyrus, these effects were least obvious in the RAN group (Fs<1.3 except culmen at F=3.4) and showed little differentiation between the CW and RBN groups (Fs>5 all ROIs both groups).
Table 2.
Sensitization Results
| Within | BA | Vol(mm3) | x | y | z | stat |
|---|---|---|---|---|---|---|
| Right Posterior Cingulate | 31 | 34752 | 2 | −46 | 34 | 11.69 |
| Right Medial Frontal Gyrus | 10 | 19968 | 7 | 48 | 5 | 13.91 |
| Right Thalamus | 7680 | 19 | −17 | 8 | 12.18 | |
| Left Thalamus | 3968 | −9 | −16 | −2 | 12.30 | |
| Left Precentral Gyrus | 6 | 3840 | −38 | −13 | 29 | 13.21 |
| Right Culmen | 2048 | 8 | −34 | −18 | 11.15 |
Table 2: Summary of sensitization results (1st versus 2nd administration, coordinates of local maxima) in talairach space.
Figure 1:
Sagittal view of the right posterior cingulate (2, −6, 34; F= 11.69) and right middle frontal gyrus (7, 48, 5; F= 13.91) as a result of significant sensitization effects with corresponding mean percent signal changes for the first (T1) and second (T2) administration demonstrated for each group (CW, healthy women; RAN, recovered women from anorexia nervosa; RBN, recovered women from bulimia nervosa) and each condition (SUC, sucrose; SPL, splenda=sucralose). Significant sensitization differences were observed between RAN and RBN groups in the Right Medial Frontal Gyrus for both the SUC and SPL conditions, as well as in the Right Precuneus for the SPL condition. No other significant group differences were observed between these groups in these regions.
3.1.2. Group by Sensitization Results:
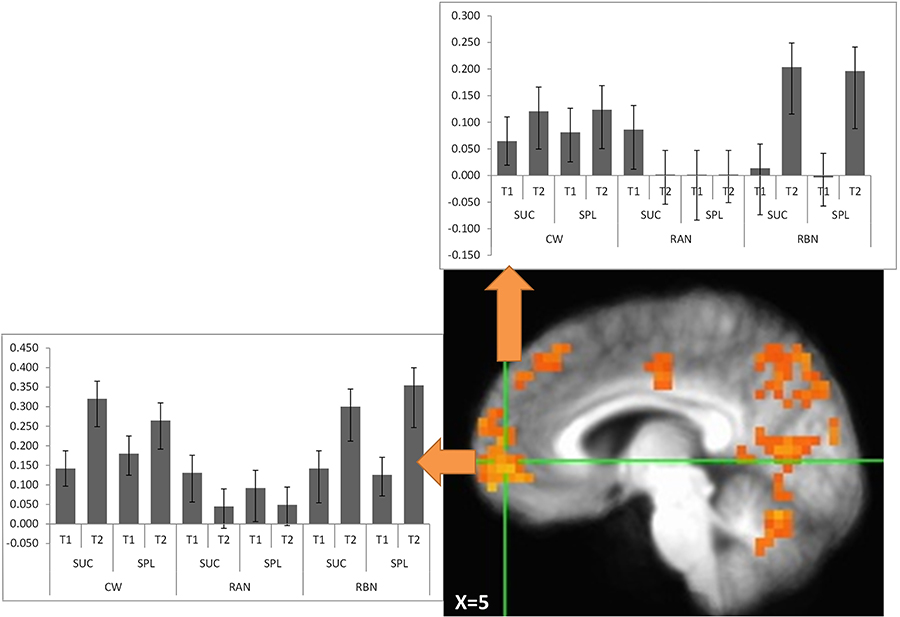
The group by sensitization analysis showed significant effects in the right cuneus, left medial frontal gyrus, right medial frontal gyrus, right parahippocampal gyrus, left cuneus, right cingulate gyrus, right precentral gyrus, left precuneus, left thalamus, and left superior temporal gyrus (see Table 3). While all groups showed some sensitization effects in some conditions in key regions, such as the medial frontal gyrus (Figure 2), these effects were limited in the RAN group showing decreased sensitization in the sucrose condition (Fs<1.0 for medial frontal gyrus to time effect). The CW (Fs>2.8 for medial frontal gyrus) and RBN groups showed little differentiation, however there was the strongest sensitization in the RBN group (Fs>7.6 for medial frontal gyrus).
Table 3.
Group by sensitization results
| Within | BA | Vol(mm3) | x | Y | z | Stat |
|---|---|---|---|---|---|---|
| Right Cuneus | 18 | 31936 | 17 | −68 | 16 | 4.37 |
| left Medial Frontal Gyrus | 8 | 13632 | −6 | 35 | 42 | 4.43 |
| Right Medial Frontal Gyrus | 10 | 9344 | 5 | 54 | 3 | 4.74 |
| Right Parahippocampal Gyrus | 19 | 7232 | 27 | −53 | −4 | 4.09 |
| Left Cuneus | 17 | 6464 | −20 | −83 | 12 | 3.93 |
| Right Cingulate Gyrus | 24 | 5056 | 14 | −6 | 41 | 4.20 |
| Right Precentral Gyrus | 6 | 4096 | 41 | 4 | 37 | 4.59 |
| Left Precuneus | 39 | 3200 | −35 | −65 | 35 | 4.64 |
| Left Thalamus | 2560 | −7 | −32 | 11 | 4.01 | |
| Left Superior Temporal Gyrus | 22 | 2560 | −39 | −50 | 22 | 4.00 |
Table 3: Summary of group by sensitization analysis results (1st versus 2nd administration, coordinates of local maxima) in talairach space.
Figure 2:
Sagittal view of the medial frontal gyrus (−6, 35, 42; F= 4.43 and 5, 54, 3; F= 4.74) as a result of significant group by sensitization analysis with corresponding mean percent signal changes for the first (T1) and second (T2) administration demonstrated for each group (CW, healthy women; RAN, recovered women from anorexia nervosa; RBN, recovered women from bulimia nervosa) and each condition (SUC, sucrose; SPL, splenda=sucralose). Significant sensitization differences were observed between RAN and RBN groups in the Right and Left Medial Frontal Gyrus for both the SUC and SPL conditions, as well as in the Left Medial Frontal Gyrus for the SPL condition when comparing CW and RBN. No other significant group differences were observed between these groups in these regions.
3.1.3. Group by Substance by Sensitization Results:
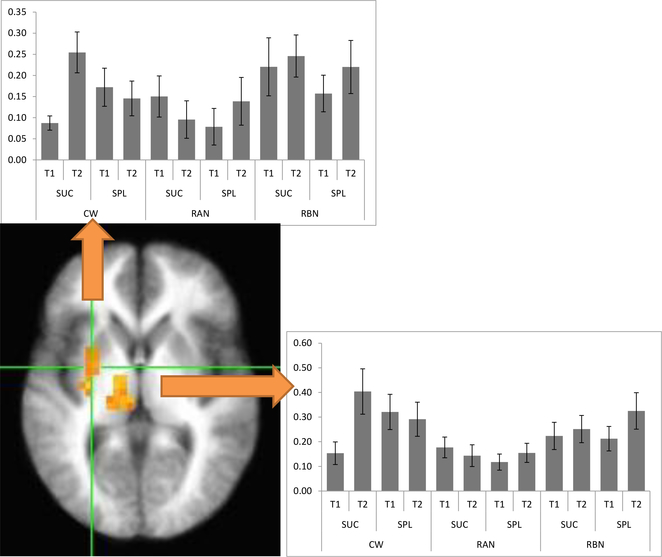
The group by substance by sensitization analysis showed significant effects in left thalamus, left lentiform nucleus, left cerebellum, right cingulate gyrus, and right precuneus (Table 4). All groups showed some sensitization effects (Figure 3), the general trend of the CW (Fs>5 for both thalamus and lentiform in the substance by sensitization contrast) was that of increased sensitization to sucrose. In this interaction the CW initially showed less activation to sucrose than to sucralose before increasing their response over time. However, the RAN (Fs<2 for both thalamus and lentiform) and RBN (Fs<1 for both thalamus and lentiform) groups showed the inverse effect in key regions, such as lentiform nucleus and thalamus.
Table 4.
Group by Substance by Sensitization Results
| Within | BA | Vol(mm3) | x | y | z | stat |
|---|---|---|---|---|---|---|
| Left Thalamus | 5504 | −15 | −18 | 11 | 4.14 | |
| Left Lentiform Nucleus | 2816 | −28 | −2 | 5 | 3.90 | |
| Left Cerebellum | 2752 | −9 | −31 | −31 | 4.47 | |
| Right Cingulate Gyrus | 24 | 2432 | 4 | 3 | 28 | 3.97 |
| Right Precuneus | 7 | 2048 | 14 | −42 | 57 | 4.12 |
Table 4: Summary of group by condition by sensitization analysis results (1st versus 2nd administration, coordinates of local maxima) in talairach space.
Figure 3:
Axial view of the left thalamus (−15, −18, 11; F= 4.14) and left lentiform nucleus (−28, −2, 5; F= 3.90) as a result of significant group by condition by sensitization analysis with corresponding mean percent signal changes for the first (T1) and second (T2) administration demonstrated for each group (CW, healthy women; RAN, recovered women from anorexia nervosa; RBN, recovered women from bulimia nervosa) and each condition (SUC, sucrose; SPL, splenda=sucralose). Significant sensitization differences were observed between CW and RAN groups in the Left Thalamus and Left Lentiform Nucleus for the SUC condition, as well as between the CW and RBN groups in the Left Thalamus for the SUC condition. No other significant group differences were observed between these groups in these regions.
3.1.4. Correlations:
Two regions were selected from each analysis and correlated with Depression (BDI) and Trait Anxiety (STAI): the posterior cingulate and medial frontal gyrus (i.e., the two key regions from the sensitization analysis (Table 2) from the sensitization analysis; the medial frontal gyrus from the group by sensitization analysis; and the lentiform nucleus and thalamus from the group by substance by sensitization analysis). Significant group differences were found in the both the thalamus and lentiform nucleus for the substance by sensitization contrast for correlations with Trait Anxiety (Table 5) but no significant relationship was observed for depression. In addition, no significant correlations were found with age, Body Mass Index (BMI), and age onset and regions of interest (Table 4). While a significant positive correlation was found between BMI and age of onset in AN, a negative correlation was found in BN (see supplement).
Table 5.
Correlations of Trait Anxiety and brain activation in the lentiform nucleus and thalamus.
| Region of contrast | All | CW | RAN | RBN | Sig Diff |
|---|---|---|---|---|---|
| SPL-SUC Sensitization Thalamus | 0.041 | −0.483 | 0.393 | −0.085 | RAN>CW |
| SPL Sensitization Thalamus | 0.015 | −0.263 | 0.066 | 0.009 | |
| SUC Sensitization Thalamus | −0.043 | 0.286 | −0.380 | 0.223 | |
| SPL-SUC Sensitization Lentiform | 0.104 | −0.454 | 0.502 | −0.072 | RAN>CW |
| SPL Sensitization Lentiform | 0.210 | −0.217 | 0.419 | 0.149 | |
| SUC Sensitization Lentiform | 0.025 | 0.361 | −0.357 | 0.235 |
Table 5: Summary of correlations of trait anxiety and brain activation from the group by condition by sensitization analysis. CW =healthy control women; RAN =women recovered from anorexia nervosa, restricting type; RBN = women recovered from bulimia nervosa; SUC= sucrose, SPL=sucralose(Splenda® )
4. Discussion
To our knowledge, this is the first study assessing sensitization effects in subjects recovered from AN and BN. Subjects with eating disorders differed significantly in their sensitization patterns to sucrose from CW in taste-related regions. Specifically, subjects recovered from AN revealed decreased sensitization to sucrose; in contrast, subjects recovered from BN displayed an increased sensitization to sucrose. However, BN sensitization was not as pronounced as in CW. While both eating disorder subgroups showed increased sensitization to the artificial sweetener sucralose, CW revealed minimal sensitivity to taste stimuli.
Sensitization and habituation effects are related phenomena and occur when one specific stimulus is presented repeatedly. Sensitization is defined as the initial increase in response to a stimulus and occurs prior to the later reduction in response to repeated stimuli, which is defined habituation. Sensitization has been observed for salivary responses to gustatory cues (Wisniewski et al., 1997) and is related to hunger, craving, and physiologic reactivity. Research has shown that animals and humans habituate on a variety of behavioral and physiological responses to repeated presentations of food cues, and habituation is related to amount of food consumed, satiety, and the subsequent cessation of eating (Benson and Raynor, 2014; Epstein et al., 2008; Rolls et al., 1986; Rolls, 1989; Temple et al., 2008).
Neuronal response to repeated exposures of various stimuli are associated with sensitization (gradually increasing BOLD signal) and/or habituation (gradually decreasing BOLD signal or blood oxygen level dependent signal)(Christmann et al., 2007; Coen et al., 2007; Wagner et al., 2006a; Yousem et al., 1997). Sensitization as an increased signal was found bilaterally in the ACC during water swallowing and in the inferior parietal gyrus (IPG) during sour swallowing. Habituation, or a gradually decreasing BOLD signal, was observed in the IPG with water (Humbert and Joel, 2012). A similar model of “incentive sensitization” is observed in numerous structures in neuroimaging studies in drug addiction with rapid signal increases after drug application, including the nucleus accumbens, caudate/putamen, indicating an enhancing responsiveness towards rewards/motivation (Breiter et al., 1997; Robinson and Berridge, 2000).
In the present study, RBN individuals showed significant sensitization and, potentially, would show more delayed habituation. This mechanism could reflect clinically observed high caloric binge eating, often of single food items, which clinically defines bulimia nervosa. In contrast, RAN individuals demonstrated the opposite neural response, with less or no sensitization, consequently, suggesting more rapid habituation leading to restricted food intake that likewise clinically defines anorexia nervosa.
The current findings are consistent with the observation that AN individuals did not show any detectable reduction in the subjective hedonic rating of a sweet taste after consuming a large amount of glucose (Rodin et al., 1990). In addition, BN individuals failed to demonstrate salivary habituation in response to repeated gustatory presentations of a palatable food (Wisniewski et al., 1997). Taken together, these studies demonstrate the behavioral pattern that mirrors the significant neural sensitization in frontal and thalamic structures observed in the current study.
Interestingly, CW demonstrated a decreased sensitization to sucralose in the thalamic regions, potentially reflecting a physiological response to a non-energy stimulus from a survival perspective. In addition, if sensitization and habituation could be argued as evolutionary relevant phenomena, our results could also reflect the attempt to maintain the illness in eating disordered patients. Although the brain seems to respond differently to caloric and non-caloric versions of a sweet taste, it is still unclear whether observed differences are due to caloric content or sensory profile (Smeets et al., 2011). In contrast, both eating disorder subgroups showed an increased sensitization effect to sucralose. For RBN, who showed the same increased sensitization pattern to both sweet tastes, this might suggest that they are not able to distinguish in terms of sensitization patterns between high and low calorie sweet stimuli and might not be able to stop eating either of them during binge episodes. RAN subjects, on the other hand, displayed the opposite sensitization pattern to sucralose than to sucrose. One potential hypothesis for this finding is that the RAN neuronal response might be anxiety driven, showing a higher sensitization to a non–anxiety provoking, low energy sweet stimulus in comparison to a decreased sensitization to an anxiety provoking, high energy sweet stimulus. This hypothesis is in concordance with the significant correlations between trait anxiety and brain activation for RAN (Table 5), which was not observed in CW. Another hypothesis for the differential brain responses could be conditioning associated with repeated illness-behaviors (e.g., prone to calorie counting) and illness duration. While the behavioral aspects of this sensitization has been observed in current and remittent patients, it is still unclear if the sensitization response in eating disorders could be interpreted as either a predisposing trait, symptom feature, or “scar”.
There is evidence that pre-meal anxiety and caloric intake are strongly associated among weight restored individuals with AN, suggesting that reducing pre-meal anxiety may improve eating behavior (Steinglass et al., 2010). However, the question of whether exposure or response prevention techniques are useful remains uncertain (Boutelle, 1998; Steinglass et al., 2012). Our data suggests that anxiety plays a central role in sensitization effects in RAN. Issues, such as time of exposure or consuming foods that might be less prone to stimulate anxiety could serve as targets for future studies.
Sweet taste seems to be recognized by specific receptors in the mouth and distributed via cranial nerves through the brain stem into the thalamus. Thalamic efferents project to the insula and frontal operculum, which represent the primary taste cortex (Ogawa, 1994; Schoenfeld et al., 2004). The insula is situated next to the posterior OFC at the operculum, which is reciprocally connected with the medial prefrontal cortex, that includes the ACC. The insula also projects to the striatum (Chikama et al., 1997; Fudge et al., 2005) as well as amygdala. While the insula is associated with the sensory processing of food (Rolls, 2005), the OFC and ACC are linked to pleasant properties of food (Rolls et al., 2003). The anterior ventral striatum is thought to translate sensory-interoceptive-hedonic aspects of feeding into motivated motor behavior (approach or avoidance) of highly palatable foods (Kelley et al., 2002). Thus, these regions should be involved in sensitization behaviors to a sweet taste. Animal studies indicate that dopamine in the striatum and putamen corresponds to motivational aspects of stimuli (Montague et al., 2004). Hence, in conjunction with the OFC and ACC, these thalamic and striatal regions appear to compose the sensitization network that is differentially responding in the current study.
Our study revealed sensitization effects in brain regions associated with the hedonic and motivational aspects of gustatory processing such as frontal, cingulate, and striatal regions. These data are consistent with our method establishing study in CW (Wagner et al., 2006a). Repeated consumption of energy-dense food was associated with a reduced response to milkshake receipt in reward-related regions in healthy adolescents (Burger and Stice, 2012; 2014). Imaging studies in AN have demonstrated persistence of hypoactivation of the food related network in response to food cues when hunger and satiety states were compared (Holsen et al., 2012; Nikendei et al., 2012), while others showed differences in activation patterns in response to feelings of hunger or satiety with a stronger response during the satiety state (Santel et al., 2006) or hunger state (Gizewski et al., 2010). These studies differed from the current protocol in that a complex food was administered until satiety was reached, then neuronal response was measured to the one specific stimulus. This is in contrast to the current study in which we administered small amounts of the same repeated macronutrient.
Sensory-specific satiety is a phenomenon that is related to, but distinguishable from, sensitization and habituation. After satiety to a specific food there is a reduction in the pleasantness of its taste. In fact, neurons in the OFC decrease their response to the food that is eaten to satiety, but remain responsive to other foods. O’Doherty et al. found sensory-specific satiety effects in the insula, amygdala, and ACC (O’Doherty et al., 2000). Similarly, OFC, middle insula, and rostral ACC activity relate to a subject’s level of subjective thirst (De Araujo et al., 2003). After sensory-specific satiety, greater ACC and reduced striatal activation correlated with reduced volitional intake of additional associated food but not for the other tastes (Spetter et al., 2012).
It is important to note that the insula is a primary gustatory and physiological region (Ogawa, 1994; Schoenfeld et al., 2004). The absence of significant changes in the insula suggests that all three groups received similar signals regarding the change in gustatory signal over the course of the experiment. The sensitization and habituation effects observed are occurring at this level but are primarily occurring in appraisal circuits in the medial frontal cortex in the majority of the analysis. However, it is important to note that in the group by substance by time analysis, we observed changes in deeper brain structures that have efferent connections to the insula (Dupont et al., 2003). This result suggests that while there may be subtle perturbations in the body signals, these are not perceived as dramatically influencing the gustatory evaluation in the current study.
4.1. Limitations:
This study had a number of limitations. First, we assessed recovered patients and the sample from each group was relatively modest. While the overall sample of 42 subjects can provide informative data, this research should be considered a preliminary sample that requires further replication to determine if these findings would differentiate from or generalize to other samples or the general population. To get a more specific understanding of the neuronal response in these patient groups it could also be of interest to assess an additional aversive substance. Second, only two runs of each substance were administered so only a limited subsample of the total neurobehavioral response could be assessed. With the current sample significant sensitization occurred; however, if more administrations were assessed, we would anticipate that as satiety is reached, habituation patterns would be observable. It is important to note that in obtaining the data reported in this paper, we delivered sweet tastes using two separate paradigms. One was pseudorandom, in which we delivered tastes of sucrose pseudorandomly alternating with a comparison solution (Oberndorfer et al., 2013; Wagner et al., 2006a). In the other, subjects were administered the same stimulus sequentially, 20 times in a row. We previously reported, using the sequential paradigm, CW showed habituation in regions such as insula, prefrontal cortex, amygdala, and hippocampus to sucrose. In contrast, for the pseudorandom paradigm, the CW showed no habitation in these regions. These data suggest that habituation patterns in CW may depend on the frequency and regularity of stimulus administration (Wagner et al., 2006a).
4.2. Summary:
To our knowledge, this is the first study in recovered eating disorder subjects demonstrating disturbed sensitization patterns in response to sweet taste stimuli on a neuronal level, that might explain their eating behavior and shed light on contributing factors. It could be argued that current treatments that attempt to normalize eating behaviors tend to either be slow to make changes, or are not effective in a substantial number of patients. The paradigms in this paper offer a method to study brain mechanisms related to habituation, as a better understanding of the biology in disordered eating might lead to more specific treatments.
Subjects with BN showed similar sensitization patterns to a high caloric as well as a non-caloric sweet stimulus. Therefore, decreasing the energy density of food consumed (with low-caloric sweets) may help target disturbances in women with BN during binges, and this could potentially lower the risk of secondary compensatory behaviors such as purging.
Supplementary Material
Highlights:
A method to study brain mechanisms related to sensitization is presented
Recovered patients with anorexia nervosa display a decreased sensitization to sucrose
Recovered patients with bulimia nervosa show an increased sensitization to sucrose
Only recovered patients with anorexia nervosa differ between high and low caloric sweet stimuli
Disturbed sensitization effects might underlie pathologic eating behavior
Acknowledgement
The authors want to thank Eva Gerardi for the manuscript preparation. The authors are indebted to the participating subjects for their contribution of time and effort in support of this study.
Grant acknowledgement: Support by grants from National Institute of Mental Health (NIMH) MH46001, MH42984, K05-MD01894, NIMH Training Grant T32-MH18399 and the Price Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- APA., 2000. Diagnostic & Statistical Manual of Mental Disordes: DSM:VI-TR, 4th edition. Washington, DC. [Google Scholar]
- Beck AT, Ward M, Mendelson M, Mock J, & Erbaugh J, 1961. An Inventory for measuring depression. Archives of General Psychiatry 4, 561–571. [DOI] [PubMed] [Google Scholar]
- Benson K, Raynor H, 2014. Occurrence of habituation during repeated food exposure via the olfactory and gustatory systems. Eating Behaviors 15, 331–333. [DOI] [PubMed] [Google Scholar]
- Bohon C, Stice E, 2011. Reward abnormalities among women with full and subthreshold bulimia nervosa: a functional magnetic resonance imaging study. International Journal of Eating Disorders 44, 585–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutelle K, 1998. The use of exposure with response prevention in a male anorexic. Journal of Behavior Therapy and Experimental Psychiatry 29, 79–84. [DOI] [PubMed] [Google Scholar]
- Boynton G, Engel S, Glover G, Heeger D, 1996. Linear systems analysis of functional magnetic resonance imaging in human V1. Journal of Neuroscience 16, 4207–4221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breiter H, Gollub R, Weisskoff R, Kennedy D, Markris N, Berke J, Goodman J, Kantor H, Gasfriend D, Riorden J, Mathew R, Rosen B, Hyman S, 1997. Acute effects of cocaine on human brain activity and emotion. Neuron 19, 591–611. [DOI] [PubMed] [Google Scholar]
- Burger K, Stice E, 2012. Frequent ice cream consumption is associated with reduced striatal response to receipt of an ice cream-based milkshake. American Journal of Clinical Nutrition 95, 810–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burger K, Stice E, 2014. Greater striatopallidal adaptive coding during cue-reward learning and food reward habituation predict future weight gain. Neuroimage 99, 122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandraskekar J, Hoon M, Ryba N, Zuker C, 2006. The receptors and cells for mammalian taste. Nature 444, 288–294. [DOI] [PubMed] [Google Scholar]
- Chikama M, McFarland N, Amaral DH, SN., 1997. Insular cortical projections to functional regions of the striatum correlate with cortical cytoarchitectonic organization in the primate. Journal of Neuroscience 17, 9686–9705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christmann C, Koeppe C, Braus D, Ruf M, Flor H, 2007. A simultaneous EEG–fMRI study of painful electric stimulation. Neuroimage 34, 1428–1437. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD, 1994. The Temperament and Character Inventory (TCI): A Guide to its Development and Use, pp. 19–28. St. Louis, MO: Center for Psychobiology of Personality, Washington University [Google Scholar]
- Coen S, Gregory L, Yaguez L, Amaro E Jr, Brammer M, Williams S, Aziz Q, 2007. Reproducibility of human brain activity evoked by esophageal stimulation using functional magnetic resonance imaging. American Journal of Physiology Gastrointestal and Liver Physiology 293, G188–G197. [DOI] [PubMed] [Google Scholar]
- Cowdrey F, Park R, Harmer C, McCabe C, 2011. Increased neural processing of rewarding and aversive food stimuli in recovered anorexia nervosa. Biological Psychiatry 70, 736–743. [DOI] [PubMed] [Google Scholar]
- Cox R,1996. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Computers and Biomedical Research 29, 162–173. [DOI] [PubMed] [Google Scholar]
- De Araujo I, Kringelbach M, Rolls ET, McGlone F, 2003. Human cortical responses to water in the mouth, and the effects of thirst. Journal of Neurophysiology 90, 1865–1876. [DOI] [PubMed] [Google Scholar]
- Dupont S, Bouilleret V, Hasboun D, Semah F, Baulac M, 2003. Functional anatomy of the insula: new insights from imaging. Surgical and Radiologic Anatomy 25, 113–119. [DOI] [PubMed] [Google Scholar]
- Epstein L, Robinson J, Temple JR, J, Marusewski A, Nadbrzuch R, 2008. Sensitization and habituation of motivated behavior in overweight and non-overweight children. Learning and Motivation 39, 243–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, 1996. Users guide for the structured clinical interview for DSM-IV Axis I disorders- research version (SCID-I, version 2.0, February 1996 FINAL VERSION). New York: Biometrics Research Department, New York State Psychiatric Institute. [Google Scholar]
- Frank GK, Kaye W, Carter C, Brooks S, May C, Fissel K, Stenger V, 2003. The evaluation of brain activity in response to taste stimuli--a pilot study and method for central taste activation as assessed by event related fMRI. Journal of Neuroscience Methods 131, 99–105. [DOI] [PubMed] [Google Scholar]
- Frank GK, Oberndorfer TA, Simmons AN, Paulus MP, Fudge JL, Yang TT, Kaye WH,2008. Sucrose actives human taste pathways differently from artificial sweetener. Neuroimage 39, 1559–1569. [DOI] [PubMed] [Google Scholar]
- Frank GK, Reynolds J, Shott M, O’Reilly R, 2011. Altered temporal difference learning in bulimia nervosa. Biological Psychiatry 70, 728–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank S, Kullmann S, Veit R, 2013. Food related processes in the insular cortex. Frontiers in Human Neuroscience 7, 499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fudge J, Breitbart M, Danish M, Pannoni V, 2005. Insular and gustatory inputs to the caudal ventral striatum in primates. Journal of Comparative Neurology 490, 101–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gizewski E, Rosenberger C, de Greiff A, Moll A, senf W, Wanke I, Forting M, Herpertz S, 2010. Influence of satiety and subjective valence rating on cerebral activation patterns in response to visual stimulation with high-calorie stimuli among restrictive anorectic and control women. Neuropsychobiology 62, 182–192. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS, 1989. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry 46, 1006–1011. [DOI] [PubMed] [Google Scholar]
- Holsen L, Lawson E, Blum K, Ko E, Makris N, Fazeli P, Klibanski A, Goldstein J, 2012. Food motivation circuitry hypoactivation related to hedonic and nonhedonic aspects of hunger and satiety in women with active anorexia nervosa and weight-restored women with anorexia nervosa. Journal of Psychiatry and Neuroscience 37, 322–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humbert I, Joel S, 2012. Tactile, gustatory, and visual biofeedbackstimuli modulate neural substrates of deglutition. Neuroimage 59, 1485–1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye WH, Greeno CG, Moss H, Fernstrom J, Fernstrom M, Lilenfeld LR, Weltzin TE, Mann JJ, 1998. Alterations in serotonin activity and psychiatric symptomatology after recovery from bulimia nervosa. Archives of General Psychiatry 55, 927–935. [DOI] [PubMed] [Google Scholar]
- Kaye WH, Gwirtsman HE, George DT, Ebert MH, 1991. Altered serotonin activity in anorexia nervosa after long-term weight restoration. Does elevated cerebrospinal fluid 5hydroxyindoleacetic acid level correlate with rigid and obsessive behavior? Archives of General Psychiatry 48, 556–562. [DOI] [PubMed] [Google Scholar]
- Kelley A, Bakshi P, Haber S, Steininger T, Will M, Zhang M, 2002. Opioid modulation of taste hedonics within the ventral striatum. Physiology and Behavior 76, 365–377. [DOI] [PubMed] [Google Scholar]
- Knight I, 1994. The development and applications of sucralose, a new high-intensity sweetener. Canadian Journal of Physiology and Pharmacology 72, 435–439. [DOI] [PubMed] [Google Scholar]
- Kringelbach ML, O’Doherty J, Rolls E, Andrews C, 2003. Activation of the human orbitofrontal cortex to a liquid food stimulus is correlated with its subjective pleasantness. Cerebral Cortex 13, 1064–1071. [DOI] [PubMed] [Google Scholar]
- Metropolitan Life Insurance Company, 1959. New weight standards for men and women. Statistical Bulletin Metropolitan Life Insurance Company 40, 1–11. [Google Scholar]
- Montague R, Hyman S, Cohen J, 2004. Computational roles for dopamine in behavioural control. Nature 431, 760–767. [DOI] [PubMed] [Google Scholar]
- Nikendei C, Friederich H, Weisbrod M, Walther S, Sharma A, Herzog W, Zipfel S, & Bender S, 2012. Event-related potentials during recognition of semantic and pictorial food stimuli in patients with anorexia nervosa and healthy controls with varying internal states of hunger. Psychosomatic Medicine 74, 136–145. [DOI] [PubMed] [Google Scholar]
- O’Doherty J, Rolls ET, Francis S, Bowtell R, McGlone F, Kobal G, Renner B, Ahne G, 2000. Sensory-specific satiety-related olfactory activation of the human orbitofrontal cortex. Neuroreport 11, 893–897. [DOI] [PubMed] [Google Scholar]
- Oberndorfer T, Frank G, Fudge J, Simmons A, Paulus M, Wagner A, Yang T, Kaye W, 2013. Altered insula response to sweet taste processing after recovery from anorexia and bulimia nervosa. American Journal of Psychiatry 214, 132–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogawa H, 1994. Gustatory cortex of primates: anatomy and physiology. Neuroscience Research 20, 1–13. [DOI] [PubMed] [Google Scholar]
- Radeloff D, Willmann K, Otto L, Lindner M, Putnam K, van Leeuwen S, Kaye W, Poustka F, Wagner A, 2014. High-fat taste challenge reveals altered striatal response in women recovered from bulimia nervosa - a pilot study. World Journal of Biological Psychiatry 15, 307–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson T, Berridge K, 2000. The psychology and neurobiology of addiction: an incentive-sensitization view. Addiction 95, 91–117. [DOI] [PubMed] [Google Scholar]
- Rodin J, Bartoshuk L, Peterson C, Schank D, 1990. Bulimia and taste: possible interactions. Journal of Abnormal Psychology 99, 32–39. [DOI] [PubMed] [Google Scholar]
- Rolls B, Rolls E, Rowe E, Sweeney K, 1981. Sensory specific satiety in man. Physiology and Behavior 27, 137–142. [DOI] [PubMed] [Google Scholar]
- Rolls E, Murzi EY, S, Thorpe S, Simpson S, 1986. Sensory-specific satiety: food-specific reduction in responsiveness of ventral forebrain neurons after feeding in the monkey. Brain Research 368, 79–86. [DOI] [PubMed] [Google Scholar]
- Rolls ET, 1989. Information processing in the taste system of primates. J Exp Biol, 146, 141–164. [DOI] [PubMed] [Google Scholar]
- Rolls ET, 2005. Taste, olfactory, and food texture processing in the brain, and the control of food intake. Physiology and Behavior 85, 45–56. [DOI] [PubMed] [Google Scholar]
- Rolls ET, O’Doherty J, Kringelbach ML, Francis S, Bowtell R, McGlone F, 2003. Representations of pleasant and painful touch in the human orbitofrontal and cingulate cortices. Cerebral Cortex 13, 308–317. [DOI] [PubMed] [Google Scholar]
- Santel S, Baving L, Krauel K, Munte T, Rotte M, 2006. Hunger and satiety in anorexia nervosa: fMRI during cognitive processing of food pictures. Brain Research 1114, 138–148. [DOI] [PubMed] [Google Scholar]
- Schoenfeld M, Neuer G, Tempelmann C, Schussler K, Noesselt T, Hopf J, Heinze H, 2004. Functional magnetic resonance tomography correlates of taste perception in the human primary taste cortex. Neuroscience 127, 347–353. [DOI] [PubMed] [Google Scholar]
- Smeets P, Weijzen P, de Graaf C, Viergever M, 2011. Consumption of caloric and non-caloric versions of a soft drink differentially affects brain activation during tasting. Neuroimage 54, 1367–1374. [DOI] [PubMed] [Google Scholar]
- Spetter M, de Graaf C, Viergever M, Smeets P, 2012. Anterior cingulate taste activation predicts ad libitum intake of sweet and savory drinks in healthy, normal-weight men. Journal of Nutrition 142, 795–802. [DOI] [PubMed] [Google Scholar]
- Spielberger C, Gorsuch R, & Lushene R, 1970. STAI Manual for the State Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Srinivasagam NM, Kaye WH, Plotnicov KH, Greeno C, Weltzin TE, Rao R, 1995. Persistent perfectionism, symmetry, and exactness after long-term recovery from anorexia nervosa. American Journal of Psychiatry 152, 1630–1634. [DOI] [PubMed] [Google Scholar]
- Steinglass J, Albano A, Simpson H, Carpenter K, Schebendach J, Attia E, 2012. Fear of food as a treatment target: Exposure and response prevention for anorexia nervosa in an open series. International Journal of Eating Disorders 45, 615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinglass J, Sysko R, Mayer L, Berner L, Schebendach J, Wang Y, Chen H, Albano A, Simpson H, Walsh B, 2010. Pre-meal anxiety and food intake in anorexia nervosa. Appetite 55, 214–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple J, Legierski C, Giacomelli A, Salvy S, Epstein L, 2008. Overweight children find food more reinforcing and consume more energy than do nonoverweight children. American Journal of Clinical Nutrition 87, 1121–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vocks S, Herpertz S, Rosenberger C, Senf W, Gizewski E, 2011. Effects of gustatory stimulation on brain activity during hunger and satiety in females with restricting-type anorexia nervosa: An fMRI study. Journal of Psychiatric Research 45, 395–403. [DOI] [PubMed] [Google Scholar]
- Wagner A, Aizenstein H, Frank GK, Figurski J, May JC, Putnam K, Bailer UF, Fischer L, Henry SE, McConaha C, Kaye WH, 2008. Altered insula response to a taste stimulus in individuals recovered from restricting-type anorexia nervosa. Neuropsychopharmacology 33, 513–523. [DOI] [PubMed] [Google Scholar]
- Wagner A, Aizenstein H, Frank GK, Figurski J, May JC, Putnam K, Bailer UF, Fischer L, McConaha C, Kaye WH, 2006a. Neural correlates of habituation to taste stimuli in healthy women. Psychiatry Research 147, 57–67. [DOI] [PubMed] [Google Scholar]
- Wagner A, Barbarich N, Frank G, Bailer U, Weissfeld L, Henry S, Achenbach S, Vogel V, Plotnicov K, McConaha C, Kaye W, Wonderlich S, 2006b. Personality traits after recovery from eating disorders: Do subtypes differ? International Journal of Eating Disorders 39, 276–284. [DOI] [PubMed] [Google Scholar]
- Wisniewski L, Epstein LH, Marcus MD, Kaye W, 1997. Differences in salivary habituation to palatable foods in bulimia nervosa patients and controls. Psychosomatic Medicine 59, 427–433. [DOI] [PubMed] [Google Scholar]
- Yousem D, William S, Howard R, Andrew C, Simmons A, Alin M, 1997. Functional MR imaging during odor stimulation: preliminary data. Radiology 204, 833–838. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.