Abstract
For the past several decades, the phenomenon of depression largely has been defined, classified, and thus assessed and analyzed, according to criteria based on the Diagnostic and Statistical Manual (now DSM5). A substantial body of knowledge on epidemiology, course, risk factors, correlates, consequences, assessment, and intervention for youth depression is based on this classical nosological approach to conceptualizing depression. Yet, recent structural and classification approaches, such as latent dimensional bifactor models (e.g., P factor model; Caspi et al., 2014) and hierarchical organizations (e.g., HiTOP; Kotov et al., 2017), have been proposed and supported as alternative options to characterize features of depression. This paper considers conceptualizations of depression among youth with a particular focus on validity: how important clinical outcomes and risks (genetic, neural, temperament, early pubertal timing, stress, and cognitive) relate to depression when ascertained via traditional DSM-defined depression versus more recent latent dimensional model approaches. The construct validity of depression, in terms of associations within respective nomological networks, varies by depression conceptualization. Clinical scientists and applied practitioners need to clearly think through the nature of what depression is and how the latent construct is conceptualized and measured. Conclusions reached for research, teaching, and evidence-based clinical work are affected and may not be the same across different conceptual and nosological organizational schemes.
I suspect I am like many of you. Depending on when you did your formative graduate level training and education, you likely have strong, firmly rooted beliefs in the fundamental nature of psychopathology--how disorders are classified and conceptualized, and how psychological distress is assessed and intervened. I began my PhD training in clinical psychology in the mid 1990s, right after publication of DSM-IV (1994), to study and understand depression—its developmental trajectories and patterns, etiologies, risks; all in the hopes that this knowledge would inform translations to improve evidence-based assessments and interventions. I have focused on the development of depression given evidence showing that depressive symptoms as well as DSM-defined episodes rise dramatically from childhood into adolescence and early adulthood (e.g., Hankin et al., 2015; Petersen et al., 1993). A developmental psychopathological emphasis on youth depression promises hope for early identification of risk and prevention to reduce the substantial distress, impairment, and cost associated with depression. Back then as well as now, I self-identify as a “depression researcher.” For the last few years, one of the single most important questions frequently on my mind is, “What is depression?” This paper considers how conceptualizing the nature of “what depression is” fundamentally affects the validity of our basic scientific knowledge and translationally applied evidence-base concerning descriptive patterns, clinical outcomes, risks, etiological theories, assessment, and intervention.
Despite considerable knowledge and inquiry focused on DSM-defined depression (Abela & Hankin, 2008; DeRubeis & Strunk, 2017; Gotlib & Hammen, 2008), I wonder what is the fundamental nature of depression. Recent work shows that depression and closely related internalizing problems can be structured via latent dimensional models, and many have demonstrated this empirical structural model across developmental ages (Caspi & Moffitt, 2018; Kotov et al., 2017; Lahey, Krueger, Rathouz, Waldman, & Zald, 2017). As opposed to DSM-defined depression in which individuals are categorized as being depressed or not based on cutoffs using polythetic criteria, latent dimensional models emphasize that individuals’ experience and report of emotional, behavioral, and cognitive symptoms can best be organized continuously across a dimension, and these symptoms can be structured via latent factors that represent what features are shared in common. Most studies focused on these recently proposed alternative models have largely emphasized the reliability of obtaining a consistent factor structure as an empirical approach to organize depression and emotional and behavioral problems.
With increasingly accumulating evidence for the consistency of such a structure across studies to efficiently organize psychopathology, it is time to bring validity into focus and consideration. It is frequently stated that reliability is necessary for validity, and as a result, considerable attention appropriately is paid to reliability. Enhancing reliability of psychiatric classification was a primary motivating force behind the creation of the modern DSM nomenclature starting in 1980. Although many clinical researchers frequently obtain good reliability for assessing DSM-based MDD using semi-structured diagnostic interviews, the DSM5 field trials showed concerning and questionable reliability for MDD (kappa = .28; Freedman et al., 2013). Reliability of a measure, or classification system, can provide an upper limit to validity, but high reliability does not ensure validity. At the same time, it is essential to consider validity as a key value in any scientific and clinical enterprise, whether that be measurement (e.g., Clark & Watson, 1995) or psychiatric classification (e.g., Uher & Rutter, 2012). Although it is challenging to define validity precisely and quantitatively, the most traditional and well-accepted approach is via construct validity (Cronbach & Meehl, 1955), in which relations among a set of associations of latent constructs and processes, that are believed to make theoretical sense given a conceptual model, are evaluated and supported within a nomological network.
Importantly, there are potential different etiological explanations and implied conclusions that result from a traditional DSM perspective vs. a latent dimensional psychopathology approach to conceptualizing depression. Findings from various fields (e.g., genetics, neuroscience, temperament, cognition, stress and adverse experiences) suggest different associations between risks and depression conceptualized via DSM-defined singular syndrome and latent dimensional factors; such work has important implications for the construct validity and conceptualization of what depression is. Taken together, the results from both structural studies on the organization of common emotional and behavioral psychopathologies as well as new validity studies promote the present thought piece focused on the nature of what depression is. The inquiry and answers to this question have clear, significant implications for all fundamental components and activities in clinical psychological science, psychiatry and allied mental health disciplines, including classification, assessment, epidemiology, etiology, and interventions.
The title of this paper is purposeful. There exist multiple options for choosing how to conceptualize what is depression in youth. At present and given the current state of evidence and conceptual work, there exists no clear, robust, and definitive answer as to the most valid approach. The main purpose of this paper is to consider conceptually and empirically viable options that clinical scientists and applied practitioners have for conceptualizing depression. Received facts, research conclusions, and our knowledge base about depression depend heavily on how depression is conceptualized, assessed, and analyzed. The construct validity for depression depends on how one conceptualizes depression within a particular classification scheme; this decision to define the nature of depression then informs assessment and analysis, which finally affects the construct validity, utility, and meaning of depression in a larger nomological network.
As such, consideration of “what depression is” does not present merely as a set of academic, ivory tower concerns. Translation from basic science into evidence-based assessment and intervention is firmly rooted in optimal organizational systems of psychopathology that guide empirical research to focus on the best options to conceptualize, identify, assess, understand, and intervene on the appropriate phenomenon and clinical features. Descriptive psychopathology, as embodied in a classification structure, does not merely describe surface-level features of depression and related symptoms; rather the choice of conceptualizing and measuring “what depression is” guides clinically-relevant information that is not simply redundant and contained within the description of depression itself. Choosing how to conceptualize and assess depression affects which adventure a clinical scientist will embark on, what will be found, and the meaning of those discoveries. Having an optimal structure and classification system for how depression and related features fit together not only summarizes known information but opens opportunities to recognize and discover the new.
DSM-based and latent dimensional hierarchical approaches to depression
The presently predominant conceptualization of depression since 1980 (starting with DSM III) has defined depression as a disorder according to clinically based authorities’ and experts’ psychiatric nosological system (e.g., currently DSM-5, American Psychiatric Association & American Psychiatric Association, 2013). A diagnosis of depressive disorder is based on a polythetic criterial set of symptoms and distress/impairment criteria that must be met for a minimum duration. The symptoms are acknowledged to vary quantitatively, although an individual youth must exhibit a minimum number of symptoms to pass clinically determined thresholds to be diagnosed categorically. For example, according to DSM-5, to diagnose an individual with a Major Depressive Episode (MDE), that person must endorse at least five out of a list of nine symptoms, and at least one of these symptoms must come from a necessary list (i.e., depressed or irritable mood, anhedonia); all of these symptoms must last “most of the day, nearly every day” for a minimum of two weeks.
Various alternatives to the DSM approach have been proposed (Clark, Cuthbert, Lewis-Fernández, Narrow, & Reed, 2017). Recently promoted and supported approaches emphasize a dimensional structural model (Lahey et al. 2017) that organizes psychopathology at a latent level across different hierarchies (Kotov et al., 2017). For example, bifactor modeling has been used to organize variance in emotional and behavioral problems. Simply, bifactor models seek to organize the variance from different manifest items into: (1) a general, common latent factor as well as (2) particular unique latent factors. A common example includes bifactor models of intelligence: the covariance that is common across all measured intelligence items is captured in a single general latent factor (i.e., g), and then orthogonal unique latent factors (e.g., fluid and crystallized intelligence, processing speed) characterize remaining specific variance that covaries among intelligence items after accounting for the general variance that is shared across all items.
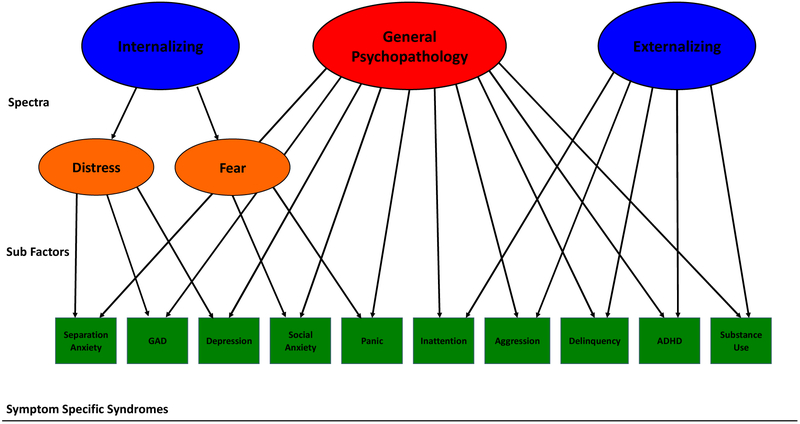
This bifactor modeling approach has been applied to psychopathological symptom and disorder data. Numerous studies consistently and reliably find that common forms of psychopathology, including mood, anxiety, behavioral and substance use problems, and disordered thought, can best be explained and structured by a general psychopathology latent factor along with orthogonal unique internalizing and externalizing latent factors (Caspi & Moffitt, 2018; Lahey et al., 2017). Caspi and colleagues (2014) named this general psychopathology liability component the “p factor”. This structural solution has been replicated across different age groups ranging from prepubertal children (e.g., Hankin et al., 2017; Olino et al., 2014) and adolescents (e.g., Laceulle, Vollebergh, & Ormel, 2015; Snyder et al., 2017) to adults (Caspi & Moffitt, 2018). Thus, the p factor accounts for what is common across all measured psychopathology symptoms in a single latent variable. Then after explaining shared common variance across all psychopathology symptoms via the p factor, the unique remaining covariance among psychopathology symptoms is organized by specific latent internalizing and externalizing liability dimensions (Figure 1; top row of spectra). Still, despite such replicability, recent critiques note that traditional model fit criteria can favor bifactor models (e.g., Bonifay, Lane, & Reise, 2017; Morgan, Hodge, Wells, & Watkins, 2015; Watts, Poore, & Waldman, 2019). While in a sense, “all models are wrong but some can be useful” (Snyder & Hankin, 2017), I agree that focusing solely on model fit is not the best way to adjudicate amongst options. For this reason, it is important to emphasize and evaluate validity of latent dimensional models such as the bifactor model.
Figure 1.
Illustration of the latent dimensional bifactor model (top, spectra level) integrated with a hierarchical perspective, as adapted from conceptual work (Hankin et al., 2016; Kotov et al., 2017).
Construct validity of depression within DSM-based and latent dimensional model nomological networks
In the rest of this paper, construct validity for both the traditional DSM-defined approach to depression as well as recent alternative, latent dimensional models are considered from two perspectives. First is the extent to which other clinically relevant mental health and impairment outcomes are associated with DSM-based depression or latent dimensions. Second includes a consideration of various risk factors and vulnerabilities that have been frequently proposed in etiological models offered to explain ontogeny of depression.
Before considering the literature with respect to these two perspectives, it is important to explicitly emphasize that the latent dimensions of psychopathology (i.e., spectra of the p factor, the specific latent internalizing and externalizing dimensions; subfactors; and any syndrome-specific factors) and DSM-defined psychiatric disorders (Berenbaum, 2013; Skinner, 1981) are all latent constructs. As such, neither the latent dimensions from bifactor models nor any DSM-defined psychiatric disorder are “real” entities in nature (Kendell, 1975; Kendler, 2012). Both the latent variables from dimensional bifactor models and the DSM psychiatric disorders are logically and conceptually reasonable, and they start on equal footing as latent theoretical constructs. Therefore, the validity for any conceptualization is evaluated via construct validation approaches and associations in their nomological networks (Cronbach & Meehl, 1955).
Construct validity: Associations with other mental health and impairment outcomes
Studies have evaluated how latent psychopathology dimensions relate to clinically relevant mental health outcomes, and some have compared criterion validity estimates with the DSM-based nosological approach (cf., Naragon-Gainey & Watson 2011; Sunderland & Slade 2015; Waszcuk et al., 2017). For example, Eaton and colleagues (2013) used data from the National Epidemiologic Survey on Alcohol and Related Conditions, a nationally representative data set with over 43,000 adults, and found that two sub-factor dimensions of the internalizing spectrum (fear and distress) best represented seven DSM-based internalizing disorders (major depression, dysthymia, panic disorder, GAD, social phobia, specific phobia, and Bipolar I) across gender, assessment points, and time frame of psychopathology assessment. Specifically, the latent fear and distress dimensions predicted future internalizing problems, suicide attempts, and medical outcomes, whereas the individual DSM-defined disorders, including depression diagnosis, did not (see also Kim & Eaton, 2015 for similar enhanced predictive findings with latent dimensions of psychopathology). Also, a series of papers by Lahey and colleagues show criterion validity for the p factor and specific internalizing and externalizing dimensions (e.g., Lahey et al., 2017; Pettersson, Lahey, Larsson, & Lichtenstein, 2018). For example, in a prospective study of adolescent girls, latent psychopathology dimensions were associated concurrently and prospectively with outcomes, including teacher ratings of academic performance, behavior, and mood (Lahey et al., 2015). In summary, this corpus of research consistently shows construct validity in that latent dimensions of psychopathology are associated with and predict future mental health, academic, and medical outcomes better than categorical, DSM-based depression.
Construct validity: Associations with risks and vulnerabilities
Many vulnerabilities to depression have been proposed and studied, especially with respect to depression conceptualized as a DSM-based syndrome or disorder (e.g., Hankin, 2012, 2015). I briefly review empirical work of how select vulnerabilities relate to depression across these two conceptualizations to place these risks in respective nomological networks to evaluate construct validity for both the DSM-based and latent psychopathology dimension approach. The bottom line conclusion across these studies is that risks are significantly associated with DSM-based depression when other co-occuring psychopathologies are not controlled, yet when such overlapping emotional and behavioral problems are covaried, relations between risk and DSM-based syndromes diminish or disappear. In contrast, risks are associated with the latent dimensions of psychopathology (p and internalizing) in ways that reveal a novel perspective on how depression can be conceptualized and characterized.
Early pubertal timing
First, meta-analytic research demonstrates that early pubertal timing is robustly associated with DSM-based depression as well as several other psychopathological syndromes (Ullsperger & Nikolas, 2017), yet the degree of specificity has not been clearly resolved. Hamlat and colleagues (in press) examined associations between early pubertal timing and depression by conceptualizing and analyzing depression across three different levels: 1. The p factor model with general psychopathology and specific internalizing and externalizing latent factors, 2. Traditional 2-factor Achenbach internalizing and externalizing dimensions (no general psychopathology dimension), and 3. DSM-based depression syndrome along with other traditionally measured psychopathological syndromes. Simple bivariate correlations showed that early pubertal timing related to depression across hierarchical levels: as a DSM-based syndrome; traditional internalizing and externalizing dimensions; and the bifactor model latent factors of p, specific internalizing and externalizing. However, when depression as a DSM-based syndrome was examined in a multivariate model in which all other measured common DSM psychopathologies (e.g., social anxiety, panic symptoms, ADHD, conduct problems, oppositional symptoms, etc.) were controlled, pubertal timing no longer was specifically associated with depression. These results suggest that early pubertal timing is associated with what depression shares in common with other psychopathologies, and such conjoint symptom features can best be represented via latent dimensions of psychopathology (e.g., p factor and internalizing specific).
Stress exposure and generation
Second, stress exposure and generation have been consistently linked with depression (Hammen, 2015), yet stress is also associated with other internalizing and externalizing psychopathologies (Grant et al., 2003). Recent research investigated associations between chronic stress and psychopathology when assessed and analyzed via latent dimensions of psychopathology and traditional DSM-based syndromes. First and consistent with all past stress exposure and generation research, Snyder et al (in press) showed that a DSM-based depression syndrome predicted, and was predicted by, chronic stress. Importantly, though, when stress and psychopathology associations were analyzed at the dimensional spectrum level, both chronic stress (Snyder, Young & Hankin, in press) and victimization (Schaefer et al., 2018) were associated with the p-factor and only the specific externalizing dimension (not internalizing specific dimension). These results suggest that stress-depression associations, in terms of exposure and generation, are not specific to DSM-based depression syndrome, per se, but rather are associated transdiagnostically with what depression shares in common with general psychopathology.
Neural risk
The third example is cortical thinning of grey matter volume (GMV). Past research (Wise et al., 2017) shows greater reduction in GMV in prefrontal cortex regions and limbic (e.g., amygdala, hippocampus) areas when comparing DSM-defined depressed patients to controls. Yet reduced GMV has been found in many other DSM-based psychopathologies as well (Goodkind et al., 2015). In a large sample of prepubertal children (Snyder, Hankin, Sandman, Head, & Davis, 2017), reduced GMV was observed in prefrontal and limbic areas for DSM-based depression syndrome. Prefrontal GMV was also diminished in the broad internalizing and externalizing dimensions as assessed via Achenbach scales.This pattern of findings suggests that reduced GMV in prefrontal regions may not relate to depression specific features. Consistent with this, Snyder et al (2017) showed that reduced GMV in prefrontal regions was associated with the p-factor, whereas the internalizing-specific latent dimension was association with reduced GMV in limbic areas.
Temperament risk
Fourth are individual differences in temperament, including negative emotionality/ affectivity (NA), positive emotionality/affectivity (PA), and effortful (cognitive) control (EC). High levels of NA (Ormel et al., 2013) and low levels of EC (Snyder, Miyake, & Hankin, 2015) are broadly associated with all DSM-based psychiatric disorders, including depression and comorbid disorders; low PA is associated with depression and some co-occurring syndromes (e.g., social anxiety; Kotov, Gamez, Schmidt, & Watson, 2010). Such findings indicative of broad risk and poor diagnostic specificity, especially for NA and EC with respect to DSM-based depression, suggest that these individual differences may be associated with the general psychopathology dimension, and perhaps the specific internalizing dimension. Indeed, extant research bears out this expectation. Olino and colleagues (2014), in a community sample of preschoolers, showed that the general psychopathology factor was negatively associated with EC and positively with NA; the internalizing specific dimension was associated with lower surgency (a specific aspect of PA). Replicating these patterns in two independent samples of youth, high NA and low EC related to the p factor, and high NA and low PA associated with the internalizing specific factor (Hankin et al., 2017). Such findings are particularly intriguing in light of the pattern of associations reviewed regarding neural risk (GMV) and latent psychopathology dimensions. Poor effortful (cognitive) control shows robust links with PFC activity, and greater negative affectivity is associated with limbic area (e.g., amygdala) activity. There may be convergence of empirical patterns across units and levels of analysis: the p factor associates with poor EC and reduced PFC GMV; the internalizing specific latent dimension relates to higher NA and reduced GMV in limbic areas.
Cognitive risks
Fifth are cognitive vulnerabilities, such as rumination, dysfunctional attitudes, and negative cognitive style. Such cognitive risks were originally theorized as depression-specific vulnerabilities, yet more recent work shows broader associations not only with DSM-based depression but also with anxiety symptoms and disorders as well as some externalizing problems (Hankin, Snyder & Gulley, 2016). Novel structural research has demonstrated that all of these cognitive vulnerabilities can be organized via a bifactor model that includes a common cognitive risk latent factor (dubbed the “c factor”) and remaining unique factors for several of these cognitive vulnerabilities (Schweizer, Hankin, & Snyder, in press). The c factor, representing common cognitive risk, related to high NA, low PA, concurrent DSM-based depression syndrome and anxious arousal, as well as future onset of DSM-ascertained MDE. This new structural model of cognitive risks, including the c factor, was replicated and shown to associate strongly with the internalizing specific dimension and moderately with the p factor (Schweizer, Young, & Hankin, 2019). These results reveal an intriguing pattern for the latent dimensions of psychopathology as these cognitive vulnerabilities were originally theorized as depression-specific risks, and associations were strongest with the specific internalizing dimension (which includes both depression and anxiety). This furthers understanding of construct validity: unlike many other risks and vulnerabilities that tend to show stronger associations with the p factor and moderate relations with internalizing specific dimension, the opposite pattern is observed with these cognitive vulnerabilities that are potently linked particularly with internalizing specific variance.
Maternal depression
Sixth is maternal history of depression, which has long been considered one of the most potent risks to youth depression. Traditionally many have presumed that the intergenerational transmission of offspring risk would show relative specificity to depression. Yet, past work shows that maternal depression confers broad risk to youth psychopathology, including multiple DSM-based syndromes and disorders as well as both internalizing and externalizing dimensions (Goodman et al., 2011). These past findings of more transdiagnostic transmission are consistent with latent dimensional models of psychopathology as opposed to conferring risk to depression specifically. Recent research shows associations between maternal depression and youth symptoms as assessed across levels: Maternal depression was associated with offspring depression as DSM-based syndrome, traditional Achenbach measures of internalizing (and externalizing), and the p-factor and internalizing specific latent factors (Davis, Hankin, Swales, & Hoffman, 2018). Similar findings with respect to the intergenerational effect of maternal psychopathology were found by Martel and colleagues (2016), who showed that a parental p factor associated with p-factor in offspring, and by Starr and colleagues (2014), who found the latent factor of internalizing psychopathology was significantly related between mother and child.
Genetic risk
Last is genetic risk as investigated via behavioral and molecular genetic research. It is well-established that depression, especially in adolescents and adults, is moderately heritable when depression is defined and examined as a singular DSM-based syndrome or disorder. Yet, both behavioral (e.g., Kendler et al., 2011) and large-scale molecular genetic psychiatric consortia (Brainstorm Consortium, 2018; Cross-Disorder Group of the Psychiatric Genomics Consortium et al., 2013) data indicate considerable overlap at the genetic level among DSM-based psychiatric disorders, including MDD, suggesting shared genetic etiology and possibly common pathophysiologies across psychiatric syndromes. When MDD was included in a hierarchical bifactor model of psychopathology in behavioral genetic research with youth, there was no unique DSM-based depression-specific heritability; rather the latent genetic risk and environmental (shared and nonshared) influences for MDD were explained by depression loading onto the p-factor (Waldman, Poore, van Hulle, Rathouz, & Lahey, 2016). In addition to research investigating latent heritability, a recent large multi-sample analysis of molecular genetic risk variants found that a single higher order genetic factor (a so-called “polygenic p factor”) accounted for most of the variance in multiple psychiatric disorders, and MDD genetic susceptibilities loaded highly on this polygenic p factor (Selzam et al., 2018).
In summary, all of these examples demonstrate how putative depression-specific risks may not be associated with traditional DSM-based depression as a specific singular syndrome, per se, whether assessed dimensionally or as a categorical disorder. Rather, many of these supposed depression-specific vulnerabilities are associated with those features that depression shares in common with other psychopathologies. Thus, numerous supposed depression-specific risks relate across levels in a hierarchical dimensional model of psychopathology (see Hankin et al., 2016).
Conclusion and Future Directions
In this paper I focused on evaluating the construct validity of depression, when conceptualized via the traditional DSM-defined approach and newer alternative latent dimensional models of psychopathology. For decades, investigators have examined validity for the latent construct of depression, as conceptualized via the DSM nosology as the underlying conceptual model, and an enormous literature has accumulated that supports validity of DSM-defined depression when evaluated via the nomological net in which MDD shows significant associations with other relevant mental health and impairment outcomes as well as depression risks. A strong appeal to using a DSM-based approach with MDD is as a heuristic to conceptualize and assess the core symptoms of depression; modern DSM starting in 1980 sought reliability, sensitivity and specificity to define MDD. The validity of DSM-based depression should thus be located in a nomological net whereby individuals with DSM-defined depression characteristics can be efficiently and reliably identified and discriminated from others with different psychiatric disorders or mental health. Yet, in contrast to this perspective, the strength and specificity of these findings, as qualitatively reviewed herein, suggests that the construct validity of depression, when conceptualized via DSM-defined approach, may be weaker than previously believed. Otherwise significant relations between DSM-based depression and risks disappeared, or the effect sizes were reduced considerably when other co-occurring emotional and behavioral psychopathologies were included in models alongside the traditional DSM-based depression syndrome. In contrast, the associations between these same clinical outcomes and vulnerabilities with latent dimensions that capture core features of depression were consistently obtained.
There are likely many reasons why latent dimensions of psychopathology appear to outperform DSM-based depression in terms of construct validity. One is the known heterogeneity within a diagnosis of depression according to DSM’s polythetic critiera. Two individuals can have the same diagnosis and share no symptoms in common; there are up to 1030 combinations of DSM-based symptoms that can uniquely characterize a depression diagnosis (Fried, 2017). Second, DSM-depression is highly comorbid with many other DSM diagnoses, especially internalizing problems such as anxiety disorders, yet most psychopathology research does not clearly address the fact of rampant co-occurrence. Thus, individuals receiving a DSM-based diagnosis of depression are not a homogenous group, so when mental health research uses case control designs (the most common design) to compare depressed to healthy controls on some etiological risk or clinical outcome variable, the ensuing validity coefficients will likely be lower given considerable heterogeneity and inclusion of comorbid cases. Third, it is well-known that categorization of a latent dimension results in a loss of information and precision and that using all severity information across the full dimension will enhance reliability, power to detect effects, and precision. Depression, even when using DSM’s criteria, is known to be dimensionally distributed at the latent level (Hankin et al., 2005), so using DSM-based categorical diagnoses results in loss of information. In summary, dimensional models that characterize the commonalities across co-occuring symptoms using latent factors would thus be expected to outperform DSM-based diagnoses.
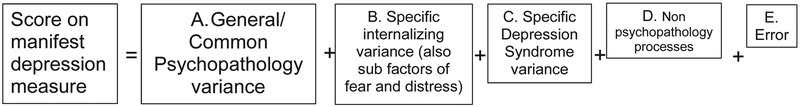
These findings suggest that the validity of depression conceptualization and assessment could be enhanced by moving beyond traditional legacy measures of depression that have historically been presumed to capture only DSM-defined depressive symptoms. To illustrate this, Figure 2 portrays the various sources of variance that are likely contained in a putatively singular manifest measure of DSM-based depression. The field should not continue to assume and believe that a single depression assessment captures only DSM-based depression specific symptom variance, nor should clinical scientists equate the DSM-based conceptualization isomorphically with its measurement. Instead, the reliability and validity of depression as a latent construct can be advanced by recognizing that depression consists of multiple sources and factors, including psychopathological dimensions across hierarchical levels (general psychopathology, an internalizing-specific dimension that includes fear and distress subfactors, and lower order specific depression features) as well as non-psychopathology sources, and error. These hierarchically organized components (general psychopathology, internalizing specific including factors of fear and distress, lower order depression specific features) together comprise the latent construct of depression. These various constituent components comprising the nature of depression can be measured, analyzed, and conceptualized separately to better understand the construct validity of what depression is and how its different features behave across levels in a nomological network, such as demonstrated here with clinical outcomes and numerous risk factors and mechanisms.
Figure 2.
Illustration that scores on any manifest measure of depression do not only operationally assess DSM-based depressive symptoms variance. Rather, the manifest depression measure is comprised of different sources of variance that likely correspond to various hierarchies in proposed latent dimensional hierarchical models of psychopathology (e.g., Hankin et al., 2016; Kotov et al., 2017), including a general psychopathology dimension (e.g, p factor), specific internalizing dimension, then specific depression symptoms as well as processes unrelated to the core psychopathological phenomenon, and other unspecified error. This is meant to illustrate that a single manifest score on a depression assessment does not represent a singular property, but rather is comprised of various latent constructs and processes that can be disambiguated to relate meaningfully to other risks and outcomes that can be studied via construct validation procedures in a nomological network (Cronbach & Meehl, 1955).
The present state of knowledge suggests that essential features of depression, and commonly co-occurring emotional, behavioral and thought problems, that frequently characterize the nature of depression can be represented hierarchically across levels of analysis from higher order latent dimensions (spectra) to lower order symptom specific syndromes (Hankin et al., 2016). Note that this approach appears wholly consistent with the recently articulated hierarchical taxonomy of psychopathology (HiTOP) model (Kotov et al., 2017). This review of outcomes and risks supports this conceptual model and provides a burgeoning base for expanding the nomological net and thus the construct validity of latent dimensional models to represent, capture, and assess features of depression in youth.
Should the reliability and validity of hierarchical latent dimensional models to organize psychopathologies, such as depression, continue to be supported in future research, there are clear next steps for additional scholarly inquiry. First will require concentrated focus on evidence-based assessment and interventions that center on these dimensions across hierarchies. Future work is needed to clinically translate these structural models of psychopathology to flesh out and characterize the measurement and treatment of “depressed” youth practically for health care practioners; the outlines of such an enterprise are beginning (cf., Forbes et al., 2019; Ruggero et al., 2019). Additionally, future research is need to formally and systematically apply a developmentally sensitive approach to these hierarchical structural models of psychopathology from early in childhood, through adolescence and adulthood. This review included many studies using child and adolescent samples, but many questions remain to establish a developmentally informed model. While initial research suggests that these latent psychopathology dimensions exhibit strong stability over time in youth (Snyder et al., 2017) and adulthood (Greene & Eaton, 2017), little is known about how these latent psychopathology factors change and develop, the manifest form these dimensions may take at different stages (see Hankin et al., 2016 for discussion), and the developmental sequalae of these hierarchical psychopathology dimensions. This is an exciting time to be a developmental clinical scientist as the field is experiencing change that can advance progress in classification of psychopathology, etiological risk research, and evidence-based clinical practice.
Highlights.
This paper considers how classification models conceptualize depression in youth and how the validity of risk factors for depression depend on the conceptualization of depression in a nomological network.
Acknowledgements:
The writing of this paper was supported by the National Institute of Mental Health (NIMH) Grants 5R01MH077195, MH109662 and R01MH105501 awarded to Benjamin Hankin.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abela JRZ, & Hankin BL (2008). Handbook of Depression in Children and Adolescents. Guilford Press. [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Berenbaum H (2013). Classification and psychopathology research. Journal of Abnormal Psychology, 122(3), 894–901. [DOI] [PubMed] [Google Scholar]
- Bonifay W, Lane SP, & Reise SP (2016). Three concerns with applying a bifactor model as a structure of psychopathology. Clinical Psychological Science, 5, 184–186. [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, … Moffitt TE (2014). The p Factor: One General Psychopathology Factor in the Structure of Psychiatric Disorders? Clinical Psychological Science : A Journal of the Association for Psychological Science, 2(2), 119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, & Moffitt TE (2018). All for One and One for All: Mental Disorders in One Dimension. American Journal of Psychiatry, 175(9), 831–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, & Watson D (1995). Constructing validity: Basic issues in objective scale development. Psychological Assessment, 7(3), 309–319. [Google Scholar]
- Clark LA, Cuthbert B, Lewis-Fernández R, Narrow WE, & Reed GM (2017). Three Approaches to Understanding and Classifying Mental Disorder: ICD-11, DSM-5, and the National Institute of Mental Health’s Research Domain Criteria (RDoC). Psychological Science in the Public Interest, 18(2), 72–145. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ, & Meehl PE (1955). Construct validity in psychological tests. Psychological Bulletin, 52(4), 281–302. [DOI] [PubMed] [Google Scholar]
- Cross-Disorder Group of the Psychiatric Genomics Consortium, Lee SH, Ripke S, Neale BM, Faraone SV, … Wray NR (2013). Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nature Genetics, 45(9), 984–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EP, Hankin BL, Swales DA, & Hoffman MC (2018). An experimental test of the fetal programming hypothesis: Can we reduce child ontogenetic vulnerability to psychopathology by decreasing maternal depression? Development and Psychopathology, 30(3), 787–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRubeis RJ, & Strunk DR (2017). The Oxford Handbook of Mood Disorders. OUP. [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Wall M, Hasin DS, Markon KE, … Grant BF (2013). The Structure and Predictive Validity of the Internalizing Disorders. Journal of Abnormal Psychology, 122(1), 86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman R, Lewis DA, Michels R, Pine DS, Schultz SK, Tamminga CA, … Yager J (2013). The Initial Field Trials of DSM-5: New Blooms and Old Thorns. American Journal of Psychiatry, 170(1), 1–5. [DOI] [PubMed] [Google Scholar]
- Fried E (2017). Moving forward: How depression heterogeneity hinders progress in treatment and research. Expert Review of Neurotherapeutics, 17, 423–425. [DOI] [PubMed] [Google Scholar]
- Forbes MK, Rapee RM, & Krueger RF (2019). Opportunities for the Prevention of General Psychopathology. Behavior Research and Therapy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, … Etkin A (2015). Identification of a Common Neurobiological Substrate for Mental Illness. JAMA Psychiatry, 72(4), 305–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, & Heyward D (2011). Maternal depression and child psychopathology: a meta-analytic review. Clinical Child and Family Psychology Review, 14(1), 1–27. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, & Hammen CL (2008). Handbook of Depression, 2nd Edition. Guilford Press. [Google Scholar]
- Grant KE, Compas BE, Stuhlmacher AF, Thurm AE, McMahon SD, & Halpert JA (2003). Stressors and child and adolescent psychopathology: moving from markers to mechanisms of risk. Psychological Bulletin, 129(3), 447–466. [DOI] [PubMed] [Google Scholar]
- Greene AL, & Eaton NR (2017). The temporal stability of the bifactor model of comorbidity: an examination of moderated continuity pathways. Comprehensive psychiatry, 72, 74–82. [DOI] [PubMed] [Google Scholar]
- Hamlat E, Snyder H, Young JF, & Hankin BL (In Press). Pubertal timing as a transdiagnostic risk for psychopathology in youth. Clinical Psychological Science. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen CL (2015). Stress and depression: old questions, new approaches. Current Opinion in Psychology, 4, 80–85. [Google Scholar]
- Hankin BL (2012). Future directions in vulnerability to depression among youth: Integrating risk factors and processes across multiple levels of analysis. Journal of Clinical Child and Adolescent Psychology, 41 (5) (2012), p. 695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL (2015). Depression from childhood through adolescence: Risk mechanisms across multiple systems and levels of analysis. Current Opinion in Psychology, 4, 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL (2017). Depression During Childhood and Adolescence In DeRubeis RJ and Strunk DR (Eds), The Oxford Handbook of Mood Disorders. ppg 276–286. Oxford University Press. [Google Scholar]
- Hankin BL, Davis EP, Snyder H, Young JF, Glynn LM, & Sandman CA (2017). Temperament factors and dimensional, latent bifactor models of child psychopathology: Transdiagnostic and specific associations in two youth samples. Psychiatry Research, 252, 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Fraley RC, Lahey BB, & Waldman ID (2005). Is depression best viewed as a continuum or discrete category? A taxometric analysis of childhood and adolescent depression in a population-based sample. Journal of abnormal psychology, 114(1), 96. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Snyder HR, & Gulley LD (2016). Cognitive risks in developmental psychopathology In Cicchetti D (Ed.) Developmental Psychopathology 3rd Ed. Pgs 312–385. Hoboken, NJ: Wiley. [Google Scholar]
- Hankin BL, Snyder HR, Gulley LD, Schweizer TH, Bijttebier P, Nelis S, … Vasey MW (2016). Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Development and Psychopathology, 28(4pt1), 987–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Young JF, Abela JR, Smolen A, Jenness JL, Gulley LD, … & Oppenheimer CW (2015). Depression from childhood into late adolescence: influence of gender, development, genetic susceptibility, and peer stress. Journal of abnormal psychology, 124(4),803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendell RE (1975). The role of diagnosis in psychiatry. Oxford, England: Blackwell Scientific Publications. [Google Scholar]
- Kendler K (2012). The dappled nature of causes of psychiatric illness: replacing the organic–functional/hardware–software dichotomy with empirically based pluralism. Molecular Psychiatry, 17(4), 377–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler Kenneth S., Aggen SH, Knudsen GP, Røysamb E, Neale MC, & Reichborn-Kjennerud T (2011). The Structure of Genetic and Environmental Risk Factors for Syndromal and Subsyndromal Common DSM-IV Axis I and All Axis II Disorders. The American Journal of Psychiatry, 168(1), 29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, & Zaslavsky AM (2011). The role of latent internalizing and externalizing predispositions in accounting for the development of comorbidity among common mental disorders. Current Opinion in Psychiatry, 24(4), 307–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, & Eaton NR (2015). The hierarchical structure of common mental disorders: Connecting multiple levels of comorbidity, bifactor models, and predictive validity. Journal of abnormal psychology, 124(4), 1064. [DOI] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, & Watson D (2010). Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychological Bulletin, 136(5), 768–821. [DOI] [PubMed] [Google Scholar]
- Kotov R, Waszczuk MA, Krueger RF, Forbes MK, Watson D, … Zimmerman M (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. [DOI] [PubMed] [Google Scholar]
- Krueger RF (1999). The structure of common mental disorders. Archives of General Psychiatry, 56(10), 921–926. [DOI] [PubMed] [Google Scholar]
- Laceulle OM, Vollebergh WAM, & Ormel J (2015). The structure of psychopathology in adolescence: Replication of a general psychopathology factor in the trails study. Clinical Psychological Science, 3(6), 850–860. [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, & Rick J (2004). The structure of child and adolescent psychopathology: generating new hypotheses. Journal of Abnormal Psychology, 113(3), 358–385. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 143(2), 142–186. 10.1037/bul0000069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Keenan K, Stepp SD, Loeber R, & Hipwell AE (2015). Criterion Validity of the General Factor of Psychopathology in a Prospective Study of Girls. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 56, 415–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Pan PM, Hoffmann MS, Gadelha A, do Rosário MC, Mari JJ, … Salum GA (2017). A general psychopathology factor (P factor) in children: Structural model analysis and external validation through familial risk and child global executive function. Journal of Abnormal Psychology, 126(1), 137–148. [DOI] [PubMed] [Google Scholar]
- Morgan GB, Hodge KJ, Wells KE, & Watkins MW (2015). Are fit indices biased in favor of bi-factor models in cognitive ability research?: A comparison of fit in correlated factors, higher-order, and bi-factor models via Monte Carlo simulations. Journal of Intelligence, 3(1), 2–20. [Google Scholar]
- Naragon-Gainey K, & Watson D (2011). The anxiety disorders and suicidal ideation: accounting for co-morbidity via underlying personality traits. Psychological medicine, 41(7), 1437–1447. [DOI] [PubMed] [Google Scholar]
- Olino TM, Dougherty LR, Bufferd SJ, Carlson GA, & Klein DN (2014). Testing Models of Psychopathology in Preschool-aged Children Using a Structured Interview-based Assessment. Journal of Abnormal Child Psychology, 42(7), 1201–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J, Jeronimus BF, Kotov R, Riese H, Bos EH, Hankin B, … Oldehinkel AJ (2013). Neuroticism and common mental disorders: Meaning and utility of a complex relationship. Clinical Psychology Review, 33(5), 686–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen AC, Compas BE, Brooks-Gunn J, Stemmler M, Ey S, & Grant KE (1993). Depression in adolescence. American psychologist, 48(2), 155. [DOI] [PubMed] [Google Scholar]
- Pettersson E, Lahey BB, Larsson H, & Lichtenstein P (2018). Criterion Validity and Utility of the General Factor of Psychopathology in Childhood: Predictive Associations With Independently Measured Severe Adverse Mental Health Outcomes in Adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 57(6), 372–383. [DOI] [PubMed] [Google Scholar]
- Ruggero CJ, Kotov R, Hopwood CJ et al. (2019). Integrating a dimensional hierarchical taxonomy of psychopathology into clinical practice. Under review. [Google Scholar]
- Schaefer JD, Moffitt TE, Arseneault L, Danese A, Fisher HL, Houts R, … Caspi A (2018). Adolescent Victimization and Early-Adult Psychopathology: Approaching Causal Inference Using a Longitudinal Twin Study to Rule Out Noncausal Explanations. Clinical Psychological Science, 6(3), 352–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweizer TH, Young JF, & Hankin BL (2019). Links between common and specific dimensions of cognitive risk and psychopathology in adolescents. Journal of Consulting and Clinical Psychology. [Google Scholar]
- Schweizer TH, Hankin BL, & Snyder HR (in press). A reformulated architecture of cognitive risks: Common and specific factors and links to internalizing outcomes in adolescence. Assessment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selzam S, Coleman JRI, Caspi A, Moffitt TE, & Plomin R (2018). A polygenic p factor for major psychiatric disorders. Translational Psychiatry, 8(1), 205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA (1981). Toward the integration of classification theory and methods. Journal of Abnormal Psychology, 90(1), 68–87. [DOI] [PubMed] [Google Scholar]
- Snyder HR, Gulley LD, Bijttebier P, Hartman CA, Oldehinkel AJ, Mezulis A, … Hankin BL (2015). Adolescent emotionality and effortful control: Core latent constructs and links to psychopathology and functioning. Journal of Personality and Social Psychology, 109(6),1132–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, & Hankin BL (2017). All models are wrong, but the p factor model is useful: Reply to Widiger and Oltmanns (2017) and Bonifay, Lane, and Reise (2017). Clinical Psychological Science, 5(1), 187–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Hankin BL, Sandman CA, Head K, & Davis EP (2017). Distinct patterns of reduced prefrontal and limbic grey matter volume in childhood general and internalizing psychopathology. Clinical Psychological Science, 5(6), 1001–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Miyake A, & Hankin BL (2015). Advancing understanding of executive function impairments and psychopathology: bridging the gap between clinical and cognitive approaches. Frontiers in Psychology, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017). Strong homotypic continuity in common psychopathology-, internalizing-, and externalizing-specific factors over time in adolescents. Clinical Psychological Science, 5(1), 98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (in press). Chronic stress exposure and generation are related to the p-factor and externalizing specific psychopathology in youth. Journal of Clinical Child & Adolescent Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr LR, Conway CC, Hammen CL, & Brennan PA (2014). Transdiagnostic and disorder-specific models of intergenerational transmission of internalizing pathology. Psychological Medicine, 44(1), 161–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunderland M, & Slade T (2015). The relationship between internalizing psychopathology and suicidality, treatment seeking, and disability in the Australian population. Journal of Affective Disorders, 171, 6–12. [DOI] [PubMed] [Google Scholar]
- Uher R, & Rutter M (2012). Basing psychiatric classification on scientific foundation: problems and prospects. International Review of Psychiatry, 24(6, 591–605. [DOI] [PubMed] [Google Scholar]
- Ullsperger JM, & Nikolas MA (2017). A meta-analytic review of the association between pubertal timing and psychopathology in adolescence: Are there sex differences in risk? Psychological Bulletin, 143(9), 903–938. [DOI] [PubMed] [Google Scholar]
- Waldman ID, Poore HE, van Hulle C, Rathouz PJ, & Lahey BB (2016). External validity of a hierarchical dimensional model of child and adolescent psychopathology: Tests using confirmatory factor analyses and multivariate behavior genetic analyses. Journal of Abnormal Psychology, 125(8), 1053–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waszczuk MA, Kotov R, Ruggero C, Gamez W, & Watson D (2017). Hierarchical structure of emotional disorders: From individual symptoms to the spectrum. Journal of Abnormal Psychology, 126(5), 613–634. [DOI] [PubMed] [Google Scholar]
- Watts AL, Poore H, & Waldman I (2019). Riskier Tests of the Validity of the Bifactor Model of Psychopathology. psyARXIV. [Google Scholar]
- Wise T, Radua J, Via E, Cardoner N, Abe O, Adams TM, … Arnone D (2017). Common and distinct patterns of grey-matter volume alteration in major depression and bipolar disorder: evidence from voxel-based meta-analysis. Molecular Psychiatry, 22(10), 1455–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]