Abstract
Background
Little is known regarding the burden of comorbidities among older people with intellectual disability (ID) who have affective and anxiety disorders. Therefore, we aimed to investigate the occurrence and risk of psychiatric and somatic comorbidities with affective and/or anxiety disorders in older people with ID compared to the general population.
Methods
This population study was based on three Swedish national registers over 11 years (2002–2012). The ID group was identified in the LSS register, which comprises of data on measures in accordance with the Act Concerning Support and Service for Persons with Certain Functional Impairments (n = 7936), and a same-sized reference cohort from the Total Population Register was matched by sex and year of birth. The study groups consisted of those with affective (n = 918) and anxiety (n = 825) disorder diagnoses. The information about diagnoses were collected from the National Patient Register based on ICD-10 codes.
Results
The rate of psychiatric comorbidities with affective and anxiety disorders was approximately 11 times higher for people with ID compared to the general reference group. The two most common psychiatric comorbidities occurred with affective and anxiety disorders were Unspecified non-organic psychosis and Other mental disorders due to brain damage and dysfunction and to physical disease (8% for each with affective disorders and 7 and 6% with anxiety disorders, respectively). In contrast, somatic comorbidity comparisons showed that the general reference group was 20% less likely than the ID cohort to have comorbid somatic diagnoses. The most commonly occurring somatic comorbidities were Injury, poisoning and certain other consequences of external causes (49 and 47% with affective and anxiety disorders, respectively) and Signs and symptoms and abnormal clinical and laboratory findings not elsewhere classified (44 and 50% with affective and anxiety disorders, respectively).
Conclusion
Older people with ID and with affective and anxiety diagnoses are more likely to be diagnosed with psychiatric comorbidities that are unspecified, which reflects the difficulty of diagnosis, and there is a need for further research to understand this vulnerable group. The low occurrence rate of somatic diagnoses may be a result of those conditions being overshadowed by the high degree of psychiatric comorbidities.
Keywords: Depression, Developmental disability, Intellectual disability, Mood disorders, Learning disabilities, Prevalence, Comorbidity
Background
Depression and anxiety are significant public health issues that affect older people and present a great burden for individuals, families and society [1]. These conditions may cause an increased burden for people in the highly vulnerable group with intellectual disability (ID) due to their communication difficulties [2]. It is acknowledged that the percentage of older people in the world is growing rapidly, both in general and in regards to individuals with ID [3]. With increased age comes ageing-related diseases, which add burden to ID-related illnesses that emerge during early childhood as well as those that develop in adulthood [4]. Thus, older people with ID suffer from advanced and complex somatic and psychiatric comorbidities, and accurate diagnosis and management can be difficult due to the person’s decreased ability to understand and express his or her illness, leading to inappropriate service and care [4, 5]. The World Health Organization (WHO) reports that depression and anxiety are two of the most common mental disorders affecting older people, with 7 and 3.8% of the world’s older population being affected, respectively [1]. Furthermore, depression and anxiety are considered to be common disorders in individuals with ID, and they frequently occur together [6, 7].
However, the results from studies of the general population cannot be directly generalized to older people with ID because there are major differences between the groups [8]. The communication deficits that limit the ability of people with IDs to describe and report their symptoms to health care providers result in unsatisfactory clinical consultations and poor treatment choices [9–11]. These problems may increase with the severity of the ID and limit the appropriate diagnosis of affective and anxiety disorders [7, 12, 13]. A Dutch study compared the prevalence of depression and anxiety in older people with ID to that in the general population, and it reported that depression and anxiety disorders increase with age and are more common among people with ID than they are in the general population [7]. Additionally, psychiatric conditions such as affective and anxiety disorders may be associated with a higher risk of other psychiatric and somatic diseases [6]. Our research group investigated the occurrence of psychiatric diagnoses in a specialist care setting among older people with ID in relation to the general population. We found that people with ID had more than double the risk of affective disorders (OR = 1.74) and anxiety disorders (OR = 1.36) [14]. In this study, we considered comorbidities to understand the disease burden of older people with ID who also have affective and/or anxiety disorders.
Understanding the differences in the diagnoses and comorbidities of older people with ID compared to the general population is important for developing appropriate policy strategies and reducing differences in health care interventions [8]. While there has been an increase in the literature on the health issues of people with ID, strong epidemiological studies on a population level with large sample sizes and appropriate diagnostic criteria are still needed to identify the occurrence rates of most common disorders as they relate to affective and anxiety diagnoses for older people with ID [4]. Moreover, to the best of our knowledge, there have been no recent studies investigating the occurrence rates of affective and anxiety disorders with other psychiatric and somatic comorbidities in older people with ID compared to the general population. Therefore, the aim of this study was to investigate the co-occurrence and risk of psychiatric and somatic comorbidities with affective and/or anxiety disorders in older people with intellectual disability compared to people of the same age and sex in the general population without ID.
Methods
This study is a retrospective population study from Sweden based on register data from three national registers over 11 years.
Swedish national registers used in the study
1) The LSS register is based on a supportive measure that comes from the Act Concerning Support and Service for Persons with Certain Functional Impairments (LSS) [15]. The LSS law gives people with significant and permanent functional impairments or disabilities the right to receive special support and services with the purpose of providing them with living conditions equal to those experienced by individuals without these disabilities. The LSS register contains three groups; individuals having intellectual disability, autism or resembling autism (Person group 1); individuals having intellectual disability as a result of permanent brain damage in adulthood (Person group 2); finally, individuals having other physical or mental impairment that is clearly not due to normal aging (Person group 3). This study included Person group 1, which applies to individuals with intellectual disability, autism or autism spectrum disorders [15].
2) The Swedish National Patient Register (NPR register) was established in 1987, and it requires the mandatory registration of inpatient and outpatient specialist care patients. It contains information about medical data, listing one main diagnosis and up to 21 secondary diagnoses [16]. In this study, we identified individuals who had at least one diagnosis of affective and/or anxiety disorders with other comorbidities. The diagnostic information is coded according to the International Classification of Diseases (ICD-10) codes. The National Board of Health and Welfare is the authority responsible for both the LSS and NPR registers.
3) The Swedish Total Population Register (TPR register) was created in 1968, and it contains information about Sweden’s general population. In the TPR register, data are maintained by Statistics Sweden, which is the official source for population statistics [17].
Study groups
ID study group
The study group comprised individuals with ID, autism, and autism spectrum disorders (Person group 1), as identified in the LSS register. The ID group was selected from an identified population aged 55 years and older that was alive and living in Sweden as of December 31, 2012 (n = 7936). The definition of older age in this study (55 years and older) was based on previous research showing that people with ID age earlier than the general population [18]. Of those with ID, we included individuals who were also diagnosed with affective (F3) and/or anxiety (F4) disorders, as coded according to the ICD-10 and collected from the NPR register over the course of eleven years (2002–2012).
General reference group (gRef)
The second study group was selected from the general population via one-to-one matching to each case in the ID population (n = 7936) by sex and year of birth during the same time period (2002 to 2012). The matching procedure was performed by Statistic Sweden. This study group (gRef) was similar to the ID study group in that its members had at least one diagnosis of affective and anxiety disorders. Figure 1 shows the procedure used for sampling from the three registers and the number of cases diagnosed with each affective (F3) and anxiety (F4) disorder in the older people with ID group and in the gRef group. The total study group consisted of 1743 people in both cohorts.
Fig. 1.
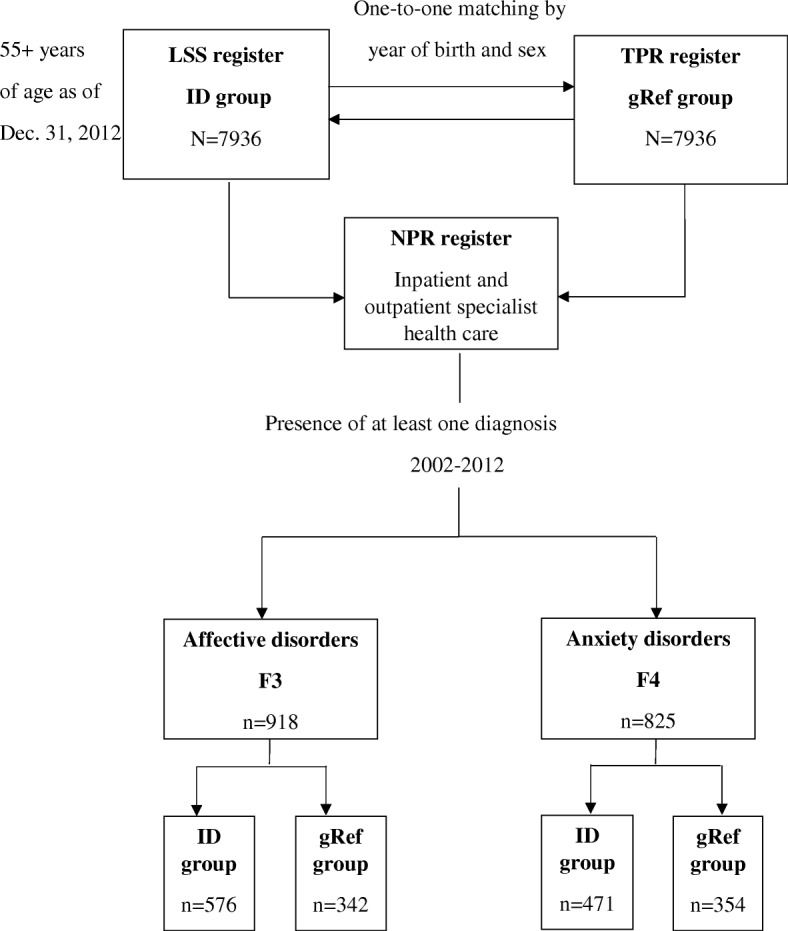
Flow chart on the sampling procedure of the study group
Affective disorders are disorders caused by a change in the affect or mood of the person (ICD-10, 2016). Most affective disorders are recurrent, and the onset of episodes can be related to stressful situations (ICD-10, 2016). Anxiety disorders are stress-related disturbances that cause significant maladaptation in social, occupational or personal function (ICD-10, 2016). The subdivisions of affective and anxiety diagnoses (using two-digitICD-10 codes) are shown in Table 1. The percentage of individuals with at least one affective disorder was higher among the older people with ID compared to the gRef (n = 576, 7.3% and n = 352, 4.3%, respectively). Depressive episode disorders (F32), Bipolar affective disorders (F31) and Recurrent depressive disorders (F33) were the most common affective disorders in the ID group. Furthermore, the percentage of individuals with at least one anxiety disorder was higher among people with ID compared to the gRef (n = 417, 5.9% and n = 354, 4.5%, respectively). The most common anxiety disorders were Other anxiety disorders (F41) and Reaction to severe stress and adjustment disorders (F43).
Table 1.
The affective and anxiety disorders in the study groups of older people with intellectual disability (ID) (7936) and in the general population from the same cohort (7936), from 2002 to 2012a
| ID n = 7936 |
gRef n = 7936 |
|||
|---|---|---|---|---|
| n | % | n | % | |
| Affective Disorders (F3) | ||||
| (F30) Manic episode | 32 | 0.4% | <5 | 0.0% |
| (F31) Bipolar affective disorder | 170 | 2.1% | 42 | 0.5% |
| (F32) Depressive episode | 358 | 4.5% | 254 | 3.2% |
| (F33) Recurrent depressive disorder | 116 | 1.5% | 116 | 1.5% |
| (F34) Persistent mood [affective] disorders | 21 | 0.3% | 23 | 0.3% |
| (F38) Other mood [affective] disorders | < 5 | 0.0% | 5 | 0.1% |
| (F39) Unspecified mood [affective] disorder | 35 | 0.4% | 17 | 0.2% |
| At least one F3 | 576 | 7.3% | 342 | 4.3% |
| Anxiety Disorders (F4) | ||||
| (F40) Phobic anxiety disorders | 36 | 0.5% | 16 | 0.2% |
| (F41) Other anxiety disorders | 289 | 3.7% | 196 | 2.5% |
| (F42) Obsessive-compulsive disorder | 74 | 0.9% | 10 | 0.1% |
| (F43) Reaction to severe stress, adjustment disorders | 81 | 1.0% | 143 | 1.8% |
| (F44) Dissociative [conversion] disorders | 27 | 03% | <5 | 0.0% |
| (F45) Somatoform disorders | 31 | 0.4% | 48 | 0.6% |
| (F48) Other neurotic disorders | 11 | 0.1% | 5 | 0.1% |
| At least one F4 | 471 | 5.9% | 354 | 4.5% |
aReference: “Psychiatric diagnoses in older people with intellectual disability in comparison with the general population: a register study” by Axmon, A., Björne, P., Nylander, L., & Ahlström, G. (2017), Epidemiology And Psychiatric Sciences, 1–13. 10.1017/S2045796017000051
Outcome measure
We identified all other psychiatric and somatic comorbidities that were found in the NPR register between 2002 and 2012 by using the ICD-10 diagnoses. The psychiatric comorbidities consisted of all diagnoses in the mental and behavioural chapter, excluding affective and anxiety disorders (F3, F4), behavioural and emotional disorders with onset usually occurring in childhood and adolescence (F9), disorders of psychological development (F8) and intellectual disability (F7) because they were included in the selected study groups.
The included psychiatric comorbidities were based on the ICD-10 block subdivisions with 2 digits (i.e., F20 Schizophrenia, F60 Specific personality disorders) because affective and anxiety disorders are included in the same chapter of mental and behavioural diagnoses. The somatic comorbidities were considered separately from the psychiatric diagnoses in this study; therefore, they are presented as ICD-10 chapter levels (i.e., II Neoplasms, VI Diseases of the nervous system). All somatic comorbidities were included except those in chapter XXI, Factors influencing health status and contact with health services, as that chapter contains information about health care services and is not a diagnosis of comorbidities.
Statistical analysis
In addition to the descriptive statistics, logistic regression was used to estimate the odds ratio and 95% confidence intervals to assess whether age and sex were significantly associated with at least one affective and anxiety diagnosis in the ID group and the gRef group. To compare the occurrence rates and the risk of having psychiatric and somatic comorbidities with affective and anxiety disorders in the ID and gRef groups, logistic regression was used to estimate the odds ratio with 95% confidence intervals. Regarding comorbidities, values less than 5 were not reported. Statistical analysis was performed using IBM SPSS Statistics version 24.0.
Results
The age range of the patients included in the study was 55 to 96 years as of December 31, 2012. As shown in Table 2, the younger age groups were more likely than the oldest age groups to have at least one affective or anxiety diagnosis. Furthermore, logistic regression showed that the odds ratio was higher for the ID group to have at least one affective or anxiety diagnosis, but the relationship was not statistically significant in any age group compared to individuals who were less than 64 years old. More females than males were diagnosed with affective and anxiety disorders, except in the ID group, where the males were diagnosed with at least one anxiety diagnosis (n = 247, 52% and n = 224, 48%, respectively) (Table 2). Furthermore, among individuals with at least one anxiety disorder, the odds ratio for the ID group was significant only for females (OR = 0.6, 95% CI 0.5–0.8), Table 2. For the ID group with affective and/or anxiety diagnoses, the result shows that the occurrence of psychiatric comorbidities is approximately 11 times higher for older people with ID compared to the general study group (Table 3). In contrast, the comparison of somatic comorbidities showed 80% more somatic diagnoses in the general reference group (gRef) than in the ID group.
Table 2.
Age and sex of older people with intellectual disability (ID) and a reference sample from the general population (gRef), stratified by the presence of at least one diagnosis of affective or anxiety disorder
| Age in 2012 and sex | At least one F3 | At least one F4 | ||||
|---|---|---|---|---|---|---|
| n = 918 | n = 825 | |||||
| ID n = 576 | gRef n = 342 | OR (95% CI) | ID n = 471 | gRef n = 354 | OR (95% CI) | |
| Age, n (%) | ||||||
| <64 | 376 (65%) | 219 (64%) | Reference* | 342 (73%) | 248 (70%) | Reference* |
| 65–74 | 172 (30%) | 87 (25%) | 2.5 (0.7–9.2) | 112 (24%) | 81 (23%) | 1.8 (0.4–8.2) |
| 75–84 | 24 (4%) | 30 (9%) | 2.9 (0.8–10.7) | 14 (3%) | 21 (6%) | 1.8 (0.4–8.4) |
| >84 | 4 (1%) | 6 (2%) | 1.2 (0.3–4.7) | 3 (1%) | 4 (1%) | 0.8 (0.17–4.5) |
| Sex, n (%) | ||||||
| Male | 279 (48%) | 165 (48%) | Reference * | 247 (52%) | 150 (42%) | Reference* |
| Female | 297 (52%) | 177 (52%) | 0.9 (0.7–1.2) | 224 (48%) | 204 (58%) | 0.6 (0.5–0.8) |
*Reference
Note. Statistically significant ORs are marked in bold
Table 3.
Occurrence of at least one psychiatric comorbidity and somatic comorbidity with at least one affective (F3) and anxiety (F4) diagnosis among older people with intellectual disability (ID) and the general population (gRef)
| Comorbidity | At least one F3 diagnosis (n = 918) | At least one F4 diagnosis (n = 825) | ||||
|---|---|---|---|---|---|---|
| ID (n = 576) n(%) | gRef (n = 342) n(%) | ID v gRefOR (95% CI) | ID (n = 471) n(%) | gRef (n = 354) n(%) | ID v gRefOR (95% CI) | |
| At least one psychiatric comorbidity | 520 (90%) | 159 (47%) | 10.69 (7.55–15.14) | 414 (88%) | 139 (39%) | 11.23 (7.92–15.94) |
| At least one somatic comorbidity | 479 (83%) | 294 (86%) | 0.81 (0.55–1.17) | 391 (83%) | 302 (85%) | 0.84 (0.58–1.23) |
Note. Statistically significant ORs are marked in bold
Psychiatric comorbidities
Table 4 summarizes the occurrence rates of psychiatric comorbidities in patients with at least one affective and/or anxiety diagnosis in the ID group and the gRef based on two categories of Mental and behavioural disorders in Chapter V. The most common comorbidities in the ID group with affective diagnoses were Other mental disorders due to brain damage and dysfunction and to physical disease (F06), Unspecified nonorganic psychosis (F29) and Specific personality disorders (F60) (8%, n = 44; 8%, n = 44; and 6%, n = 35, respectively). As shown in Table 4, the higher risk was only statistically significantly higher for F06 (OR = 3.45, 95% CI 1.61–7.43) and F23 (OR = 3.06, CI 1.16–8.07) comorbidities with at least one affective diagnosis in the ID group.
Table 4.
Occurrence of psychiatric comorbidities with at least one affective (F3) and anxiety (F4) diagnosis among older people with intellectual disability (ID) and the general population (gRef) based on two-digit mental and behavioural diagnoses from the ICD-10 coding system
| Psychiatric comorbidity | At least one F3 diagnosis (n = 918) | At least one F4 diagnosis (n = 825) | ||||
|---|---|---|---|---|---|---|
| ID (n = 576) n(%) | gRef (n = 342) n(%) | ID v gRef OR (95% CI) | ID (n = 471) n(%) | gRef (n = 354) n(%) | ID v gRef OR (95% CI) | |
| F00_Dementia in Alzheimer disease | 5 (1%) | <5 | NC* | <5 | <5 | NC* |
| F01_Vascular dementia | 11 (2%) | <5 | NC* | <5 | <5 | NC* |
| F03_Unspecified dementia | 29 (5%) | 8 (2%) | 2.21 (1.00–4.90) | 13 (3%) | <5 | NC* |
| F06_Other mental disorders due to brain damage and dysfunction and to physical disease | 44 (8%) | 8 (2%) | 3.45 (1.61–7.43) | 27 (6%) | 7 (2%) | 3.01 (1.30–7.00) |
| F07_Personality and behavioural disorders due to brain disease, damage and dysfunction | 10 (2%) | <5 | NC* | 9 (2%) | <5 | NC* |
| F09 _Unspecified organic or symptomatic mental disorder | 6 (1%) | <5 | NC* | 6 (1%) | <5 | NC* |
| F10_Mental and behavioural disorders due to use of alcohol | 34 (6%) | 53 (16%) | 0.34 (0.22–0.54) | 32 (7%) | 46(13%) | 0.49 (0.31–0.79) |
| F11_Mental and behavioural disorders due to use of opioids | 6 (1%) | 11 (3%) | 0.32 (0.12–0.86) | <5 | 10 (3%) | NC* |
| F13_Mental and behavioural disorders due to use of sedatives and hypnotics | <5 | 22 (6%) | NC* | < 5 | 21 (6%) | NC* |
| F17_Mental and behavioural disorders due to use of tobacco | 13 (2%) | 13 (4%) | 0.58 (0.27–1.28) | 10 (2%) | 13 (4%) | 0.57 (0.25–1.31) |
| F19_Mental and behavioural disorders due to multiple drug use and use of other psychoactive substance | 10 (2%) | 17 (5%) | 0.34 (0.15–0.77) | 8 (2%) | 15 (4%) | 0.39 (0.16–0.93) |
| F20_Schizophrenia | 25 (4%) | <5 | NC* | 29 (6%) | <5 | NC* |
| F22_Persistent delusional disorders | 22 (4%) | 6 (2%) | 2.22 (0.89–5.54) | 20 (4%) | <5 | NC* |
| F23_Acute and transient psychotic disorders | 25 (4%) | 5 (2%) | 3.06 (1.16–8.07) | 19 (4%) | 5 (1%) | 2.93 (1.09–7.94) |
| F25_Schizoaffective disorders | 17 (3%) | <5 | NC* | 14 (3%) | <5 | NC* |
| F28_Other nonorganic psychotic disorders | <5 | <5 | NC* | 5 (1%) | <5 | NC* |
| F29_Unspecified nonorganic psychosis | 44 (8%) | <5 | NC* | 34 (7%) | <5 | NC* |
| F51_Nonorganic sleep disorders | <5 | 9 (3%) | NC* | <5 | 6 (2%) | NC* |
| F60_Specific personality disorders | 35 (6%) | 14 (4%) | 1.52 (0.80–2.86) | 35 (7%) | 14 (4%) | 1.95 (1.03–3.68) |
| F63_Habit and impulse disorders | 5 (1%) | <5 | NC* | 6 (1%) | <5 | NC* |
*NC (not calculated) indicates that one cell contains a value that is less than 5 or that there were zero observations
Note. Statistically significant ORs are marked in bold
Among those with at least one anxiety diagnosis in the ID group, the most common comorbidities were Specific personality disorders (F60), 7%; Unspecified nonorganic psychosis (F29), 7%; and Other mental disorders due to brain damage and dysfunction and to physical disease (F06), 6% (n = 35, n = 34, and n = 27, respectively). These comorbidities were similar to those seen with the affective diagnosis, as shown above. However, Mental and behavioural disorders due to the use of alcohol (F10) were the most common psychiatric comorbidities in the general reference group (gRef), with at least one affective diagnosis in 16% (n = 53) and with at least one anxiety diagnosis in 13% (n = 46), Table 4. A significantly higher risk of having psychiatric comorbidities with at least one anxiety diagnosis in the ID group was observed in patients with F06 (OR = 3.01, CI 1.30–7.00), F23 (OR = 2.93, CI 1.09–7.94) and F60 (OR = 1.95, CI 1.03–3.68) comorbidities (Table 4).
Somatic comorbidities
As summarized in Table 4, somatic comorbidities were categorized based on the chapters of the ICD-10 coding system. The most common comorbidities with affective diagnoses in the ID group were Injury, poisoning and certain other consequences of external causes (49%, Chapter XIX); Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (44%, Chapter XVIII); and Diseases of the digestive system (33%, Chapter XI), (n = 280, n = 251, n = 188, respectively). Moreover, there was a significantly higher risk of being diagnosed with a disease of the nervous system (Chapter VI, OR = 1.66, CI = 1.20–2.28), a disease of the genitourinary system (Chapter XIV, OR = 1.41, 95% CI = 1.01–1.96) or Injury, poisoning and certain other consequences of external causes (Chapter XIX, OR = 1.37, CI = 1.04–1.79) in the ID group with at least one affective diagnosis (Table 5).
Table 5.
Occurrence of somatic comorbidities with at least one affective (F3) and anxiety (F4) diagnosis among older people with intellectual disability (ID) and the general population (gRef) based on the chapters of the ICD-10 coding system
| Chapter | Somatic comorbidity | At least one F3 diagnosis (n = 918) | At least one F4 diagnosis (n = 825) | ||||
|---|---|---|---|---|---|---|---|
| ID (n = 576) n(%) | gRef (n = 342) n(%) | ID v gRef OR (95% CI) | ID (n = 471) n(%) | gRef (n = 354) n(%) | ID v gRef OR (95% CI) | ||
| I | Certain infectious and parasitic diseases | 68 (12%) | 34 (10%) | 1.21 (0.79–1.87) | 52 (11%) | 25 (7%) | 1.63 (0.99–2.67) |
| II | Neoplasms | 71 (12%) | 53 (16%) | 0.77 (0.52–1.13) | 39 (8%) | 48 (14%) | 0.58 (0.37–0.90) |
| III | Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 41 (7%) | 31 (9%) | 0.77 (0.47–1.25) | 23 (5%) | 24 (7%) | 0.71 (0.39–1.27) |
| IV | Endocrine, nutritional and metabolic diseases | 168 (29%) | 112 (33%) | 0.85 (0.63–1.12) | 120 (26%) | 91 (26%) | 0.99 (0.72–1.36) |
| VI | Diseases of the nervous system | 170 (30%) | 69 (20%) | 1.66 (1.20–2.28) | 138 (29%) | 60 (17%) | 2.03 (1.44–2.86) |
| VII | Diseases of the eye and adnexa | 117 (20%) | 62 (18%) | 1.15 (0.82–1.62) | 89 (19%) | 52 (15%) | 1.35 (0.93–1.97) |
| VIII | Diseases of the ear and mastoid process | 24 (4%) | 16 (5%) | 0.89 (0.46–1.70) | 22 (5%) | 22 (6%) | 0.74 (0.40–1.36) |
| IX | Diseases of the circulatory system | 159 (28%) | 151 (44%) | 0.49 (0.36–0.64) | 134 (29%) | 130 (37%) | 0.69 (0.51–0.92) |
| X | Diseases of the respiratory system | 149 (26%) | 104 (30%) | 0.80 (0.60–1.07) | 130 (28%) | 109 (31%) | 0.86 (0.63–1.16) |
| XI | Diseases of the digestive system | 188 (33%) | 133 (39%) | 0.76 (0.58–1.01) | 172 (37%) | 136 (38%) | 0.92 (0.69–1.23) |
| XII | Diseases of the skin and subcutaneous tissue | 37 (6%) | 17 (5%) | 1.31 (0.73–2.37) | 26 (6%) | 16 (5%) | 1.23 (0.65–2.33) |
| XIII | Diseases of the musculoskeletal system and connective tissue | 126 (22%) | 134 (39%) | 0.44 (0.32–0.58) | 124 (26%) | 141 (40%) | 0.54 (0.40–0.72) |
| XIV | Diseases of the genitourinary system | 143 (25%) | 65 (19%) | 1.41 (1.01–1.96) | 125 (27%) | 58 (16%) | 1.84 (1.30–2.61) |
| XVII | Congenital malformations, deformations and chromosomal abnormalities | 39 (7%) | < 5 | NC* | 31 (7%) | < 5 | NC* |
| XVIII | Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 251 (44%) | 170 (50%) | 0.79 (0.60–1.02) | 236 (50%) | 182 (51%) | 0.95 (0.72–1.25 |
| XIX | Injury, poisoning and certain other consequences of external causes | 280 (49%) | 140 (41%) | 1.37 (1.04–1.79) | 220 (47%) | 133 (38%) | 1.46 (1.10–1.93) |
*NC (not calculated) indicates that one cell contains a value that is less than 5 or that there were zero observations
Note. Statistically significant ORs are marked in bold
Furthermore, the most common comorbidities with at least one anxiety diagnosis were Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (50%, Chapter XVIII, n = 236); Injury, poisoning and certain other consequences of external causes (47%, Chapter XIX, n = 220); and Diseases of the digestive system (37%, Chapter XI, n = 172). In the general study group, Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (Chapter XVIII), was the most common somatic comorbidity in patients with at least one affective diagnosis (50%, n = 170) and at least one anxiety diagnosis (51%, n = 182) (Table 5).
In patients with at least one anxiety diagnosis, there was a significantly higher risk of having a diagnosis of Disease of the nervous system (Chapter VI, OR = 2.03, CI = 1.44–2.86), Disease of the genitourinary system (Chapter XIV, OR = 1.84, CI = 1.30–2.61) or an Injury, poisoning and certain other consequences of external causes diagnosis (Chapter XIX, OR = 1.46, CI = 1.10–1.93), Table 5.
Discussion
The findings of this study show that the odds of being diagnosed with one psychiatric comorbidity was eleven times higher among older people with ID and affective and/or anxiety disorders compared to the general population. Older people with ID and affective and/or anxiety disorders have a higher rate of unspecified psychiatric and somatic comorbidities than the general population, which indicates that people with ID are a more vulnerable group that presents an evident need for collaboration between health and social services [19, 20]. Moreover, we found that the most common psychiatric and somatic comorbidities were similar for patients with affective and anxiety disorders. This finding can be explained by the fact that mood disorders such as depression and anxiety are associated with one another [21]. Regarding somatic comorbidities, we found that the ID group was approximately 20% less likely to have a comorbid somatic diagnosis with affective and anxiety disorders than the general population.
Psychiatric comorbidities
Among the findings of this study, it is interesting to note that the most common psychiatric comorbidities are unspecified or categorized as other disorders. These findings align fairly well with those of Baxter et al. [22] that people with ID are at risk of having an unidentified diagnosis; this further supports the clinical experience that it is difficult for health care professionals to recognize health problems in patients with severe and profound types of ID and psychiatric comorbidities. In addition, the health care provider often attributes the symptoms of the psychiatric disorders to ID symptoms, when in fact the problems are actually related to a comorbid psychiatric diagnosis. The main factor contributing to health care providers’ low level of knowledge regarding people with ID and psychiatric comorbidities was a lack of sufficient training and experience in the assessment and treatment of people with ID and with psychiatric disorders [23, 24]. As a consequence, the presence of affective and anxiety disorders with other comorbidities might be hidden and thus underestimated by health care providers [25].
In addition, patients with more severe ID have a limited ability to describe their symptoms [26–28]. Furthermore, the calming effect of the psychotropic medications commonly used for individuals with ID may hide the symptoms of psychiatric disorders and make it more difficult for health care providers to diagnose comorbidities [29–31]. This may suggest an increased vulnerability among older people with ID.
We found a significantly lower risk of substance abuse comorbidities, such as alcohol, opioid, smoking and psychoactive drug abuse in older people with ID, which is in line with what McCarron et al. [5] reported in their study of multimorbidity in older people with ID. In contrast, other studies have found that a higher rate of alcohol misuse in individuals with ID [32, 33]. These contradictory results can be explained by the different conditions, settings and characteristics of the studies’ sample populations, e.g., younger age groups are at an increased risk of substance abuse; patients with mild-to-moderate ID are at higher risk of substance abuse than those with more severe ID; and the inclusion of primary care data may affect results as people are more often treated for alcohol misuse in that setting.
Somatic comorbidities
Regarding somatic comorbidities, older people with ID and affective and/or anxiety disorders had a lower percentage of somatic comorbidities than the general population. However, the results showed a higher risk of diseases of the nervous system or genitourinary system and injury/poisoning in older people with ID with affective and anxiety disorders.
Furthermore, our results regarding the higher occurrence rates of diseases of the neurological and digestive systems within the ID group support previous reports [5]. For example, in a previous study, comorbid epilepsy, constipation, and dyspepsia [33] occurred more frequently in individuals with ID. However, in our study, Diseases of the digestive system occurred more frequently in the general population than in older people with ID. A possible explanation might be that health care providers miss the diagnosis and symptoms of the digestive system, and therefore, less-severe somatic problems are not detected.
Moreover, our findings share some similarities with previous studies that show lower rates of cardiovascular, cancer, and pulmonary disease [5, 33, 34]. The rates of cardiovascular disease increase significantly with age in the general population, but in our study, cardiovascular disease was less prevalent in older people with ID and affective and/or anxiety disorders. One possible explanation consistent with previous research is under diagnosis or unidentified diagnoses in the ID population [35]. Another explanation for the lower rates of cardiovascular disease in our study could be related to the lower rates of substance use (i.e., smoking and alcohol) in our population. Lower cardiovascular and stroke rates have been previously reported to be associated with light drinking and less smoking among older people [36].
Furthermore, this study found that the risk of injuries and poisoning is higher in people with affective and/or anxiety disorders. This indicates that older people with ID and affective and/or anxiety disorders are more vulnerable and prone to injuries. Therefore, our recommendation is to develop strategies and policies to promote health and prevent injuries in older people with ID. Cox et al. (2010) found several risk factors for injuries and falls in people with ID. These risk factors include hypertension, visual impairment, polypharmacy and the use of psychotropic medications [37]. Older people are also more likely to be prescribed multiple medications, such as antipsychotics and benzodiazepine, which are associated with a wide range of side effects [36, 38]. Additionally, studies report that the use or misuse of prescribed benzodiazepine and prescription sedatives in older people has been associated with an increased risk of falls [39, 40].
This study shows that patients with ID and anxiety and depression are less frequently diagnosed with signs and symptoms of somatic diseases and are less likely to have abnormal clinical findings compared to the general population. However, when compared with the prevalence of the other somatic comorbidities in the ID group, signs, symptoms and abnormal clinical findings were the second-most prevalent comorbidities. Some signs and symptoms, such as headache, musculoskeletal pain and pain related to the circulatory and respiratory systems, were less likely to be diagnosed in older people with ID [41]. This may be because those symptoms require good communication skills to relay them to health care providers, and individuals with ID may not be able to describe their problem sufficiently [41]. Furthermore, pain related to the urinary system is more likely to be diagnosed in older people with ID because it is easier to diagnose using laboratory tests and cultures [41]. These findings can explain our study results regarding the more frequent occurrence of diseases of the genitourinary system among older people with ID compared to the general population.
Previous research regarding comorbidities in older people with ID has reported a lower occurrence of cardiovascular diseases [5] and a lower risk of being diagnosed with musculoskeletal and cardiovascular pain [41]. Older people with ID need good communication skills to describe their symptoms to health care providers when accessing health care. This may explain why diseases of the musculoskeletal and circulatory systems are less likely to be reported in older people with ID with affective and/or anxiety disorders compared to the general population.
Jakovljevic (2009) showed that people with comorbid mental or somatic disorders experience problems receiving care both because some psychiatrists fail to recognize somatic diseases and because somatic specialists do not recognize mental disorders, and therefore they do not provide adequate treatment [42]. The comorbid occurrence of mental disorders with other psychiatric and somatic disorders is also presented in a recently growing body of literature about multimorbidity in the ageing population [43–45]. For example, a pattern of multimorbidity was identified by the presence of relationships between mental and neurological diseases and gastrointestinal and mental and neurological diseases in older people with ID [5] This could contribute to a better understanding of the complexity of comorbidities in people with ID and affective and anxiety disorders [43].
Methodological considerations
This paper provides information about all psychiatric and somatic diagnoses that co-occur with affective and anxiety disorders in older people with ID in inpatient and outpatient specialist care. Our study was based on national register data coded by ICD-10 profiles in the ID population and general population, while previous studies focused on a single or small number of comorbidities, used self-reported data and did not make any comparison with the general population [8]. Another strength of this study is the high validity of the NPR registry, which is based on inpatient and outpatient care data and has required mandatory registration for physicians for more than 30 years [46]. Furthermore, studies with data from the NPR registry regarding diagnoses with affective and anxiety disorders such as bipolar, obsessive compulsive disorders and tic disorders have more than 90% positive predictive value [47–50]. Additionally, using both the LSS register, which was developed specifically for people with intellectual disability, and the Swedish total population register is an advantage of this study because both data sources have mandatory registration and high population coverage.
The registers used in the study were designed as administrative registers; thus, they minimize the ability to observe the individuals in the study and thereby identify other possible risk factors that could affect the diagnosis by health care providers. Another limitation is the lack of information from the primary health care provider, which limits information about comorbidities as the NPR register does not include any data about primary health care. Data files about primary health care in Sweden are collected on the county level and were often started in the last decade by the 21 county councils. However, the Swedish government plans to make a decision that will include data on primary health care in the NPR. The current absence of national data needs to be taken into consideration given that affective and anxiety disorders are usually treated in the primary health care setting. One recent study based on data from the Primary Care Register in nine counties included 72% of the Swedish population and reported that 80% of depression and anxiety disorders were diagnosed only by the primary health care provider [51]. This result confirms that depression and anxiety are more often diagnosed in the primary health care setting. However, that study focused on the general population, and it is unknown whether the pattern is the same for people with ID.
In the present study, we investigated the occurrence of affective and anxiety disorders with other comorbidities without taking into consideration the level of ID in our study population. The risk of multimorbidity has been previously reported to increase with the severity of ID [52]. ID severity can complicate the assessment of clinical manifestations and the diagnosis of other psychiatric disorders and can increase the length of stay in a medical facility [8, 53]. Also, with severe level of ID, the utility of different diagnostic criteria used in people with ID becomes very limited because is based on verbal expression. The diagnosis of psychiatric disorders in people with severe to profound levels of ID is more complicated because the symptoms of the disease are usually masked by behavioural disturbances, which lead to problems in the identification and treatment of additional diagnoses [54]. Finally, we chose to analyse different levels of diagnostic specificity for somatic and psychiatric comorbidities due to our focus on psychiatric diagnoses in this study. This should be taken into consideration when interpreting the results regarding somatic diagnoses.
Conclusion
This study indicated that older people with ID and affective and/or anxiety disorders are approximately eleven times more likely to be diagnosed with at least one another psychiatric comorbidity compared with the general population without ID. This study highlighted the high occurrence rates of other and unspecified psychiatric comorbidities and the low occurrence rates of somatic diagnoses in this study group of older people with ID. The findings suggest that more attention should be paid to comorbidities in older patients with affective and/or anxiety disorders and ID. More in-depth knowledge is needed regarding whether comorbidities generate an increased burden for older people with ID. Future research can therefore focus on health care utilization for ageing people with ID and other comorbidities.
Acknowledgements
We would like to thank Anna Axmon, associate professor, Lund University, Lund, Sweden, who performed data management and completed a critical review of an early draft of the manuscript.
Abbreviations
- gRef
General Reference Group
- ICD-10
International Classification of Diseases-10th Revision
- ID
Intellectual Disability
- LSS
The Act Concerning Support and Service for Persons with Certain Functional Impairments
- NPR
National Patient Register
- TPR
Total Population Register
Authors’ contributions
GA (PI of the project) initiated the research project, made the ethical applications and managed the acquisition of resources and data. NeM designed the study in collaboration with GA and JE. NeM performed the statistical analyses and wrote the draft of the manuscript. All authors took part in the interpretation of data and revision of the manuscript. All authors approved the final version of the manuscript.
Authors’ information
NeM is an experienced psychiatric nurse and is currently a PhD student. JE is an MD, PhD and associate professor experienced in clinical psychiatric health care and research. GA is a nurse, PhD and professor with extensive experience in research regarding disability and health care for the elderly, as well as psychiatric care.
Funding
This study was funded by The Jordanian South Society for Special Education and Forte; the Swedish Research Council for Health, Working Life and Welfare (2014–4753).
Availability of data and materials
This study contains sensitive information about a vulnerable group of people with intellectual disability. Although the data files are anonymized, they still contain details that enable the possible identification of single individuals. If access to the database is requested for other researchers, the PI (Gerd Ahlström) would have to ask the Regional Ethical Review Board in Lund before could provide the data. This is due to considerable restrictions regarding access to the data that were placed on the study prior to approval. However, the database was compiled by three national registers, which other researchers can recreate by contacting the Swedish National Board of Health and Welfare and Statistics Sweden.
Ethics approval and consent to participate
The study was approved by the Regional Ethical Review Board in Lund (diary no. 2013/15), and the research was performed in accordance with the Declaration of Helsinki (World Medical Association 2013). Both the National Board of Health and Welfare and Statistic Sweden made separate secrecy reviews, and the data were anonymized before being given to the PI (Gerd Ahlström). The study design did not include informed written consent from the participants; instead, information about the study and how to withdraw from it was advertised in two major national newspapers in Sweden. One of these newspapers was published by the Swedish National Association for Persons with Intellectual Disability (FUB). The other was a well-known national newspaper (Dagens Nyheter). No one refused participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nadia El Mrayyan, Phone: +46-46-222-18-01, Email: nadia.el_mrayyan@med.lu.se.
Jonas Eberhard, Email: jonas.eberhard@med.lu.se.
Gerd Ahlström, Email: Gerd.Ahlstrom@med.lu.se.
References
- 1.Mental health of older adults [http://www.who.int/en/news-room/fact-sheets/detail/mental-health-of-older-adults].
- 2.Tuffrey-Wijne I, McEnhill L. Communication difficulties and intellectual disability in end-of-life care. Int J Palliat Nurs. 2008;14(4):189–194. doi: 10.12968/ijpn.2008.14.4.29133. [DOI] [PubMed] [Google Scholar]
- 3.Fisher K, Kettl P. Aging with mental retardation: increasing population of older adults with MR require health interventions and prevention strategies. Geriatrics. 2005;60(4):26–29. [PubMed] [Google Scholar]
- 4.Perkins EA, Moran JA. Aging adults with intellectual disabilities. Jama. 2010;304(1):91–92. doi: 10.1001/jama.2010.906. [DOI] [PubMed] [Google Scholar]
- 5.McCarron M, Swinburne J, Burke E, McGlinchey E, Carroll R, McCallion P. Patterns of multimorbidity in an older population of persons with an intellectual disability: results from the intellectual disability supplement to the Irish longitudinal study on aging (IDS-TILDA) Res Dev Disabil. 2013;34(1):521–527. doi: 10.1016/j.ridd.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 6.Cooper S-A, Smiley E, Morrison J, Williamson A, Allan L. Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry. 2007;190(1):27–35. doi: 10.1192/bjp.bp.106.022483. [DOI] [PubMed] [Google Scholar]
- 7.Hermans H, Beekman AT, Evenhuis HM. Prevalence of depression and anxiety in older users of formal Dutch intellectual disability services. J Affect Disord. 2013;144(1–2):94–100. doi: 10.1016/j.jad.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 8.Hermans H, Evenhuis HM. Multimorbidity in older adults with intellectual disabilities. Res Dev Disabil. 2014;35(4):776–783. doi: 10.1016/j.ridd.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 9.Lennox N, Diggens J, Ugoni A. The general practice care of people with intellectual disability: barriers and solutions. J Intellect Disabil Res. 1997;41(5):380–390. doi: 10.1111/j.1365-2788.1997.tb00725.x. [DOI] [PubMed] [Google Scholar]
- 10.Esbensen AJ, Rojahn J, Aman MG, Ruedrich S. Reliability and validity of an assessment instrument for anxiety, depression, and mood among individuals with mental retardation. J Autism Dev Disord. 2003;33(6):617–629. doi: 10.1023/b:jadd.0000005999.27178.55. [DOI] [PubMed] [Google Scholar]
- 11.Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, Murphy AW. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011;28(5):516–523. doi: 10.1093/fampra/cmr013. [DOI] [PubMed] [Google Scholar]
- 12.Reid K, Smiley E, Cooper SA. Prevalence and associations of anxiety disorders in adults with intellectual disabilities. J Intellect Disabil Res. 2011;55(2):172–181. doi: 10.1111/j.1365-2788.2010.01360.x. [DOI] [PubMed] [Google Scholar]
- 13.Marston G, Perry D, Roy A. Manifestations of depression in people with intellectual disability. J Intellect Disabil Res. 1997;41(6):476–480. doi: 10.1111/j.1365-2788.1997.tb00739.x. [DOI] [PubMed] [Google Scholar]
- 14.Axmon A, Björne P, Nylander L, Ahlström G. Psychiatric diagnoses in older people with intellectual disability in comparison with the general population: a register study. Epidemiology and psychiatric sciences. 2018;27(5):479–491. doi: 10.1017/S2045796017000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Swedish code of statutes SFS 1993:387: The act concerning support and Service for Persons with certain functional impairments (LSS) in.; 2014.
- 16.The National Board of Health and Welfare: the National Patient Register. In.; 2016.
- 17.Ludvigsson JF, Almqvist C, Bonamy A-KE, Ljung R, Michaëlsson K, Neovius M, Stephansson O, Ye W. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol. 2016;31(2):125–136. doi: 10.1007/s10654-016-0117-y. [DOI] [PubMed] [Google Scholar]
- 18.Coppus A. People with intellectual disability: what do we know about adulthood and life expectancy? Developmental disabilities research reviews. 2013;18(1):6–16. doi: 10.1002/ddrr.1123. [DOI] [PubMed] [Google Scholar]
- 19.Holst G, Johansson M, Ahlstrom G. Signs in people with intellectual disabilities: interviews with managers and staff on the identification process of dementia. Healthcare (Basel, Switzerland) 2018;6:3. doi: 10.3390/healthcare6030103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ouellette-Kuntz H, Martin L, Burke E, McCallion P, McCarron M, McGlinchey E, Sandberg M, Schoufour J, Shooshtari S, Temple B. How best to support individuals with IDD as they become frail: development of a consensus statement. J Appl Res Intellect Disabil. 2019;32(1):35–42. doi: 10.1111/jar.12499. [DOI] [PubMed] [Google Scholar]
- 21.Hermans H, Evenhuis HM. Factors associated with depression and anxiety in older adults with intellectual disabilities: results of the healthy ageing and intellectual disabilities study. International journal of geriatric psychiatry. 2013;28(7):691–699. doi: 10.1002/gps.3872. [DOI] [PubMed] [Google Scholar]
- 22.Baxter H, Lowe K, Houston H, Jones G, Felce D, Kerr M. Previously unidentified morbidity in patients with intellectual disability. Br J Gen Pract. 2006;56(523):93–98. [PMC free article] [PubMed] [Google Scholar]
- 23.Costello H, Bouras N, Davis H. The role of training in improving community care staff awareness of mental health problems in people with intellectual disabilities. J Appl Res Intellect Disabil. 2007;20(3):228–235. [Google Scholar]
- 24.Werner S, Stawski M. Mental health: knowledge, attitudes and training of professionals on dual diagnosis of intellectual disability and psychiatric disorder. J Intellect Disabil Res. 2012;56(3):291–304. doi: 10.1111/j.1365-2788.2011.01429.x. [DOI] [PubMed] [Google Scholar]
- 25.Mason J, Scior K. Diagnostic overshadowing’ amongst clinicians working with people with intellectual disabilities in the UK. J Appl Res Intellect Disabil. 2004;17(2):85–90. [Google Scholar]
- 26.Ali A, Scior K, Ratti V, Strydom A, King M, Hassiotis A. Discrimination and other barriers to accessing health care: perspectives of patients with mild and moderate intellectual disability and their carers. PLoS One. 2013;8(8):e70855. doi: 10.1371/journal.pone.0070855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ward RL, Nichols AD, Freedman RI. Uncovering health care inequalities among adults with intellectual and developmental disabilities. Health Soc Work. 2010;35(4):280–290. doi: 10.1093/hsw/35.4.280. [DOI] [PubMed] [Google Scholar]
- 28.Wullink M, Veldhuijzen W, van Schrojenstein Lantman-de HM, Metsemakers JF, Dinant G-J. Doctor-patient communication with people with intellectual disability-a qualitative study. BMC Fam Pract. 2009;10(1):82. doi: 10.1186/1471-2296-10-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stolker JJ, Koedoot PJ, Heerdink ER, Leufkens HG, Nolen WA. Psychotropic drug use in intellectually disabled group-home residents with behavioural problems. Pharmacopsychiatry. 2002;35(1):19–23. doi: 10.1055/s-2002-19838. [DOI] [PubMed] [Google Scholar]
- 30.Hermans H, Jelluma N, van der Pas FH, Evenhuis HM. Feasibility, reliability and validity of the Dutch translation of the anxiety, depression and mood scale in older adults with intellectual disabilities. Res Dev Disabil. 2012;33(2):315–323. doi: 10.1016/j.ridd.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 31.Espie CA, Watkins J, Curtice L, Espie A, Duncan R, Ryan JA, Brodie MJ, Mantala K, Sterrick M. Psychopathology in people with epilepsy and intellectual disability; an investigation of potential explanatory variables. J Neurol Neurosurg Psychiatry. 2003;74(11):1485–1492. doi: 10.1136/jnnp.74.11.1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Duijvenbode N, VanDerNagel JE, Didden R, Engels RC, Buitelaar JK, Kiewik M, de Jong CA. Substance use disorders in individuals with mild to borderline intellectual disability: current status and future directions. Res Dev Disabil. 2015;38:319–328. doi: 10.1016/j.ridd.2014.12.029. [DOI] [PubMed] [Google Scholar]
- 33.Cooper S-A, McLean G, Guthrie B, McConnachie A, Mercer S, Sullivan F, Morrison J. Multiple physical and mental health comorbidity in adults with intellectual disabilities: population-based cross-sectional analysis. BMC Fam Pract. 2015;16(1):110. doi: 10.1186/s12875-015-0329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hermans H, Beekman AT, Evenhuis HM. Comparison of anxiety as reported by older people with intellectual disabilities and by older people with normal intelligence. Am J Geriatr Psychiatry. 2014;22(12):1391–1398. doi: 10.1016/j.jagp.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 35.Merrick J, Davidson PW, Morad M, Janicki MP, Wexler O, Henderson CM. Older adults with intellectual disability in residential care centers in Israel: health status and service utilization. Am J Ment Retard. 2004;109(5):413–420. doi: 10.1352/0895-8017(2004)109<413:OAWIDI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 36.Schulte MT, Hser Y-I. Substance use and associated health conditions throughout the lifespan. Public Health Rev. 2013;35(2):3. doi: 10.1007/BF03391702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cox C, Clemson L, Stancliffe R, Durvasula S, Sherrington C. Incidence of and risk factors for falls among adults with an intellectual disability. J Intellect Disabil Res. 2010;54(12):1045–1057. doi: 10.1111/j.1365-2788.2010.01333.x. [DOI] [PubMed] [Google Scholar]
- 38.Axmon A, Kristensson J, Ahlstrom G, Midlov P. Use of antipsychotics, benzodiazepine derivatives, and dementia medication among older people with intellectual disability and/or autism spectrum disorder and dementia. Res Dev Disabil. 2017;62:50–57. doi: 10.1016/j.ridd.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 39.Sorock GS, Shimkin EE. Benzodiazepine sedatives and the risk of falling in a community-dwelling elderly cohort. Arch Intern Med. 1988;148(11):2441–2444. [PubMed] [Google Scholar]
- 40.Ham AC, Swart KM, Enneman AW, van Dijk SC, Oliai Araghi S, van Wijngaarden JP, van der Zwaluw NL, Brouwer-Brolsma EM, Dhonukshe-Rutten RA, van Schoor NM, et al. Medication-related fall incidents in an older, ambulant population: the B-PROOF study. Drugs Aging. 2014;31(12):917–927. doi: 10.1007/s40266-014-0225-x. [DOI] [PubMed] [Google Scholar]
- 41.Axmon Anna, Ahlström Gerd, Westergren Hans. Pain and Pain Medication among Older People with Intellectual Disabilities in Comparison with the General Population. Healthcare. 2018;6(2):67. doi: 10.3390/healthcare6020067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jakovljevic M. Psychopharmacotherapy and comorbidity: conceptual and epistemiological issues, dilemmas and controversies. Psychiatr Danub. 2009;21(3):333–340. [PubMed] [Google Scholar]
- 43.Kirchberger I, Meisinger C, Heier M, Zimmermann AK, Thorand B, Autenrieth CS, Peters A, Ladwig KH, Doring A. Patterns of multimorbidity in the aged population. Results from the KORA-age study. PLoS One. 2012;7:e30556. doi: 10.1371/journal.pone.0030556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abad-Díez JM, Calderón-Larrañaga A, Poncel-Falcó A, Poblador-Plou B, Calderón-Meza JM, Sicras-Mainar A, Clerencia-Sierra M, Prados-Torres A. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. 2014;14(1):75. doi: 10.1186/1471-2318-14-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mino-Leon D, Reyes-Morales H, Doubova SV, Perez-Cuevas R, Giraldo-Rodriguez L, Agudelo-Botero M. Multimorbidity patterns in older adults: an approach to the complex interrelationships among chronic diseases. Arch Med Res. 2017;48(1):121–127. doi: 10.1016/j.arcmed.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 46.Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim J-L, Reuterwall C, Heurgren M, Olausson PO. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11(1):450. doi: 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rück C, Larsson KJ, Lind K, Perez-Vigil A, Isomura K, Sariaslan A, Lichtenstein P, Mataix-Cols D. Validity and reliability of chronic tic disorder and obsessive-compulsive disorder diagnoses in the Swedish National Patient Register. BMJ Open. 2015;5:6. doi: 10.1136/bmjopen-2014-007520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sellgren C, Landén M, Lichtenstein P, Hultman CM, Långström N. Validity of bipolar disorder hospital discharge diagnoses: file review and multiple register linkage in Sweden. Acta Psychiatr Scand. 2011;124(6):447–453. doi: 10.1111/j.1600-0447.2011.01747.x. [DOI] [PubMed] [Google Scholar]
- 49.Ekholm B, Ekholm A, Adolfsson R, Vares M, Ösby U, Sedvall GC, Jönsson EG. Evaluation of diagnostic procedures in Swedish patients with schizophrenia and related psychoses. Nordic Journal of Psychiatry. 2005;59(6):457–464. doi: 10.1080/08039480500360906. [DOI] [PubMed] [Google Scholar]
- 50.Dalman C, Broms J, Cullberg J, Allebeck P. Young cases of schizophrenia identified in a national inpatient register. Soc Psychiatry Psychiatr Epidemiol. 2002;37(11):527–531. doi: 10.1007/s00127-002-0582-3. [DOI] [PubMed] [Google Scholar]
- 51.Sundquist J, Ohlsson H, Sundquist K, Kendler KS. Common adult psychiatric disorders in Swedish primary care where most mental health patients are treated. BMC Psychiatry. 2017;17(1):235. doi: 10.1186/s12888-017-1381-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bratek A, Krysta K, Kucia K. Psychiatric comorbidity in older adults with intellectual disability. Psychiatr Danub. 2017;29(Suppl 3):590–593. [PubMed] [Google Scholar]
- 53.Lunsky Y, Balogh R. Dual diagnosis: a National Study of psychiatric hospitalization patterns of people with developmental disability. Can J Psychiatr. 2010;55(11):721–728. doi: 10.1177/070674371005501106. [DOI] [PubMed] [Google Scholar]
- 54.Myrbakk E, von Tetzchner S. Psychiatric disorders and behavior problems in people with intellectual disability. Res Dev Disabil. 2008;29(4):316–332. doi: 10.1016/j.ridd.2007.06.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This study contains sensitive information about a vulnerable group of people with intellectual disability. Although the data files are anonymized, they still contain details that enable the possible identification of single individuals. If access to the database is requested for other researchers, the PI (Gerd Ahlström) would have to ask the Regional Ethical Review Board in Lund before could provide the data. This is due to considerable restrictions regarding access to the data that were placed on the study prior to approval. However, the database was compiled by three national registers, which other researchers can recreate by contacting the Swedish National Board of Health and Welfare and Statistics Sweden.


