Abstract
Background
The effects of conditional cash transfer (CCT) programs on maternal and child health (MCH) service use in conflicted affected countries such as Afghanistan are not known.
Methods
We conducted a non-randomised population based intervention study in six Afghanistan districts from December 2016 to December 2017. Six control districts were purposively matched. Women were eligible to be included in the baseline and endline evaluation surveys if they had given birth to one or more children in the last 12 months.
The intervention was a CCT program including information, education, communication (IEC) program about CCT to community members and financial incentives to community health workers (CHWs) and families if mothers delivered their child at a health facility. Control districts received standard care.
The primary objective was to assess the effect of CCT on use of health facilities for delivery. Secondary objectives were to assess the effect of CCT on antenatal care (ANC), postnatal care (PNC) and CHW motivation to perform home visits.
Outcomes were analysed at 12 months using multivariable difference-in-difference linear regression models adjusted for clustering and socio demographic variables.
Results
Overall, facility delivery increased in intervention villages by 14.3% and control villages by 8.4% (adjusted mean difference [AMD] 3.3%; 95% confidence interval [− 0.14 to 0.21], p value 0.685). There was no effect in the poorest quintile (AMD 0.8% [− 0.30 to 0.32], p value 0.953). ANC (AMD 45.0% [0.18 to 0.72] p value 0.004) and PNC (AMD 31.8% [− 0.05 to 0.68] p value 0.080) increased in the intervention compared to the control group. CHW home visiting changed little in intervention villages (− 3.0%) but decreased by − 23.9% in control villages (AMD 12.2% [− 0.27 to 0.51], p value 0.508). CCT exposure was 27.3% (342/1254) overall and 10.2% (17/166) in the poorest quintile.
Conclusions
Our study demonstrated that a CCT program provided to women aged 16–49 years can be implemented in a highly conservative conflict affected population. CCT should be scaled up for the poorest women in Afghanistan.
Keywords: Maternal and newborn health, Inequalities, Cash transfer
Background
There have been considerable improvements in maternal and newborn health across Asia [1, 2]. However, inequities in access and use of maternal and newborn health services remain widespread. Barriers include: cost, distance, perceived quality of care and poor awareness of healthcare options [1, 2]. ‘Demand side financing’ has been used for many years to incentivise families to use primary care services [3]. The type of scheme varies from unconditional transfers (e.g. money provided following the birth of a child), vouchers (reimbursable for a range of services) and conditional cash transfer (CCT) schemes (payment for specific services) [4].
Many low and middle income countries have implemented CCT schemes. Two systematic reviews have examined impact on use of maternal and child health services in the last 10 years including studies from 17 countries [5, 6]. The authors of the systematic reviews concluded that CCT can have important short term impacts on antenatal care and facility delivery but that effects are dependent on family ‘exposure’ and awareness of the scheme, access to transport, efficiency of payments and staffing in health facilities [5, 6]. Monitoring of non-incentivised services is also important as coverage of non incentivised services may decrease as more attention is provided to incentivised services. However, to date there appears to be only one small study from India which specifically assessed the effects of CCT on non incentivised maternity services (antenatal care [ANC] and postnatal care [PNC]) [7].
No CCT studies also appear to have been conducted in conflict affected areas, though one study in Afghanistan has assessed feasibility [8]. We recently reported that barriers to MCH use in Afghanistan are similar to other Asian countries but lack of decision making ‘power’ of women in the family and the presence of anti-government elements in small villages are also important determinants [9, 10]. Families in conflict affected countries such as Afghanistan are likely to require additional assistance to enable them to use financial incentives. This includes community level support [11].
Thus, in 2015, the Ministry of Public Health (MoPH) in Afghanistan in partnership with Unicef, developed a CCT intervention to assist rural Afghanistan women to access health facilities for maternal and newborn health services in rural areas.
The primary objective of this study was to assess the effectiveness of the MoPH CCT intervention on use of health facilities for delivery. Secondary objectives were to assess effects on (i) maternal care seeking for non-incentivised services such as ANC and PNC and (ii) community health worker (CHW) motivation to perform home visits. In addition we assessed effects in the poorest and least poor quintiles.
Methods
Design
This was a non-randomised, population based intervention study conducted over a 12 month period from November 2016 to December 2017. The intervention was implemented from December 2016 to December 2017. For the evaluation the baseline survey was conducted over a 1 month period in November 2016 and the endline survey was conducted in December 2017. All pregnant women aged 16 years and above who were resident in the study districts were eligible to receive the intervention. Women were only eligible to be included in the baseline and endline surveys if they were postpartum and had given birth to one or more children in the last 12 months.
Setting
Afghanistan has a population of 32 million people and is mountainous and landlocked. It is prone to natural disasters including avalanches, earthquakes and flooding [12, 13]. Many roads become in accessible in winter seasons. Conflict and violence has increased over the last two years [14]. Although access to health facilities has improved over the last fifteen years, in 2016 over 50% of families had to travel two or more hours to reach a primary health care centre [15].
In Afghanistan, the basic health system includes district hospitals, health centres and outreach services including vaccination teams. There are also volunteer CHWs based at ‘health posts’ (usually the CHW home) in each village. The CHWs are trained to provide basic health care such as health promotion advice, referral of sick women and children and information, education, communication (IEC) for preventive services such as immunisation, ANC, PNC and facility delivery. They also provide basic medicines such as iron and folic acid, antibiotics for pneumonia and oral rehydration therapy (ORS) for diarrhoea. Their basic training includes intensive preservice training over a three month period and yearly one week refresher training. Each CHW is supervised by a paid Ministry community health supervisor (CHS). The CHS provides supportive supervision, monitoring and reporting functions [16, 17]. 5% of health facilities provide private fee paying services. The remaining 95% are public facilities providing free services including MCH [16]. More details are presented in Appendices 1 and 2.
This project was based in three provinces of Afghanistan (Badghis, Bamyan and Kandahar). The project team purposively selected two intervention districts per province to ensure conflict affected areas and geographically hard to reach areas were represented (Badghis [Abkamary, Moqur], Bamyan [Waras, Kahmard], and Kandahar [Dand, Daman]). Two control districts per province were then chosen with similar socio demographics, access, clinic density and security (Badghis [Qades, Jawand], Bamyan [Punjab, Saighan], Kandahar [Arghandaab, Spin Boldak]). Figure 1 displays the map of the study area. Table 1 and Appendix 1 display profile data for the study area.
Fig. 1.
Map of Afghanistan. (https://commons.wikimedia.org/wiki/File:Blank_map_of_Afghanistan_districts.svg) [18] with amendments to show geographic distribution of the intervention and control districts
Table 1.
Sociodemographic characteristics of women included in the study compared between intervention and control villages
| Number (%) of mothers in intervention villages | Number (%) of mothers in control villages | |||
|---|---|---|---|---|
| Baseline | Endline | Baseline | Endline | |
| (n = 1199) | (n = 1254) | (n = 1242) | (n = 1237) | |
| Province | ||||
| Bamyan | 421 (35.1%) | 403 (32.1%) | 413 (33.3%) | 403 (32.6%) |
| Badghis | 387 (32.3%) | 400 (31.9%) | 412 (33.2%) | 404 (32.7%) |
| Kandahar | 391 (32.6%) | 451 (36.0%) | 417 (33.6%) | 430 (34.8%) |
| Maternal education | ||||
| Primary school (year 1–6) | 38 (3.2%) | 46 (3.7%) | 74 (6.0%) | 86 (7.0%) |
| Secondary school (year 7–9) | 33 (2.8%) | 34 (2.7%) | 40 (3.2%) | 38 (3.1%) |
| High school (year 10–12) | 32 (2.7%) | 72 (5.7%) | 57 (4.6%) | 73 (5.9%) |
| Advanced education (year 12+) | 12 (1.2%) | 20 (1.6%) | 22 (1.8%) | 49 (4.0%) |
| No education | 1082 (90.2%) | 1057 (84.3%) | 1038 (83.6%) | 983 (79.5%) |
| Not known | 0 (0.0%) | 25 (2.0%) | 11 (0.9%) | 8 (0.7%) |
| Maternal literacy | ||||
| Literate | 223 (18.6%) | 412 (32.8%) | 279 (22.5%) | 382 (30.9%) |
| Not literate | 976 (81.4%) | 842 (67.2%) | 963 (77.5%) | 855 (69.1%) |
| Mother’s age | ||||
| 16–24 years | 469 (39.1%) | 496 (39.6%) | 455 (36.6%) | 391 (31.6%) |
| 25–29 years | 407 (33.9%) | 307 (24.5%) | 346 (27.9%) | 386 (31.2%) |
| 30–39 years | 213 (17.8%) | 364 (29.0%) | 145 (11.7%) | 282 (22.8%) |
| 40 years or older | 108 (9.0%) | 86 (6.9%) | 70 (5.6%) | 47 (3.8%) |
| Not known | 2 (0.2%) | 1 (0.1%) | 226 (18.2%) | 131 (10.6%) |
| Mother’s parity | ||||
| 1 | 112 (9.3%) | 138 (11.0%) | 96 (7.7%) | 188 (15.2%) |
| 2 | 161 (13.4%) | 165 (13.2%) | 183 (14.7%) | 238 (19.2%) |
| 3 | 209 (17.4%) | 160 (12.8%) | 242 (19.5%) | 208 (16.8%) |
| 4 | 174 (14.5%) | 203 (16.2%) | 209 (16.8%) | 150 (12.1%) |
| 5 or more | 543 (45.3%) | 588 (46.9%) | 512 (41.2%) | 453 (36.6%) |
| Wealth quintile | ||||
| Quintile 1 (poorest) | 111 (9.3%) | 166 (13.2%) | 358 (28.8%) | 258 (20.9%) |
| Quintile 2 | 223 (18.6%) | 255 (20.3%) | 228 (18.4%) | 169 (13.7%) |
| Quintile 3 | 294 (24.5%) | 201 (16.0%) | 165 (13.3%) | 223 (18.0%) |
| Quintile 4 | 241 (20.1%) | 200 (16.0%) | 220 (17.7%) | 222 (18.0%) |
| Quintile 5 (least poor) | 239 (19.9%) | 270 (21.5%) | 212 (17.1%) | 152 (12.3%) |
| Missing | 91 (7.6%) | 162 (12.9%) | 59 (4.8%) | 213 (17.2%) |
| Access to any health facility | ||||
| Less than 30 mins | 422 (35.2%) | 419 (33.4%) | 299 (24.1%) | 376 (30.4%) |
| 30 mins to 1 h | 405 (33.8%) | 509 (40.6%) | 595 (47.9%) | 531 (42.9%) |
| 1–2 h | 172 (14.4%) | 236 (18.8%) | 183 (14.7%) | 211 (17.1%) |
| 2 h to half a day | 124 (10.3%) | 65 (5.2%) | 25 (2.0%) | 35 (2.8%) |
| More than half a day | 29 (2.4%) | 1 (0.1%) | 10 (0.8%) | 54 (4.4%) |
| Not known | 47 (3.9%) | 24 (1.9%) | 130 (10.5%) | 30 (2.4%) |
CCT intervention
The intervention was a CCT program with three key elements: (i) information, education, communication (IEC) program about CCT to community members; (ii) financial incentives to CHWs if they visited pregnant women at home and assisted them to travel to health facilities for delivery; (iii) financial incentives to mothers if they delivered their child at a health facility. The CCT program was based on prior intensive formative research [9]. There were no private birthing facilities in the study area thus the intervention only involved public facilities.
The IEC program focused on four key issues: the importance of health facility delivery, the resources (including CHWs) available to assist with travel to health facilities for delivery, the mother’s cash incentive for health facility delivery and the CHW’s cash incentive if he or she facilitated referral. The IEC program used four delivery channels: billboards, brochures, CHWs and village leaders. A dedicated graphic designer developed and pretested key messages for billboards and brochures which were displayed in each village and each health facility. In November 2016 all CHWs from each village in the intervention districts and their supervisors (CHSs) received a one day training course in the CCT intervention, especially the use of the CCT IEC material and key issues (the importance of health facility delivery, the resources [including CHWs] available to assist with transfer to health facilities for delivery, the mother’s cash incentive if she delivered at health facility and the CHWs cash incentive if they facilitated referral). They were also trained in the importance of providing home visits and visiting disadvantaged hard to reach families, including fathers, male heads of households and women of reproductive age. They were also trained in CCT referral record keeping. Village leaders also received a similar one day training course in November 2016. After consultation with key MoPH stakeholders, the importance of ANC and PNC services was also included in all training programs and IEC messaging.
The mother received a cash transfer of 1000 Afghani (approximately USD $15) if she delivered at a health facility regardless of the transport mechanism she chose. CHWs received a cash transfer of 300 Afghani (approximately USD $5) if they accompanied the mother to the health facility or if the mother provided a CHW referral slip when she arrived for delivery. Funds were provided to both mother and CHW at the health facility before the mother was discharged home.
Control areas
The control areas in Badghis [Qades Jawand], Bamyan [Punjab Saighan] and Kandahar [Arghandaab, Spin Boldak]) received standard care and did not receive our CCT intervention. Health facilities in control and intervention districts were provided with a health system strengthening (HSS) package over 24 months prior to the intervention delivery and throughout the intervention period. This included the UNICEF/WHO training package in essential newborn care (ENC) and Basic and Emergency Obstetric and Newborn Care (BEmONC). Women did not have to pay for delivery at any facilities in the control areas.
Definitions
The primary outcome measure was the proportion of women who delivered in a health facility in the study area.
Secondary outcome measures were: the proportion of women who received at least one ANC visit, proportion of women who received at least one PNC visit and the proportion of women who received at least one CHW home visit.
A composite measure of ‘treatment’ (or ‘exposure’) (i.e. receipt of the intervention) was defined as a mother who reported that she knew (i) there was any program that would give her money if she delivered in a health facility or (ii) she would receive our CCT intervention if she delivered in a health facility. A composite measure of ‘non treatment’ was also defined as a mother who reported that she did not know (i) or (ii). We did this because there are many programs in Afghanistan which provide financial incentives for health care and we felt in our study area mothers are not likely to know which particular ‘organization’ is providing the funds. We wanted to be careful to capture all women who felt they would receive any funds, as we felt that was the most accurate representation of ‘exposure’. We considered that women who answered ‘yes’ to (ii) should also answer ‘yes’ to (i). However we felt that women might not understand question (i) so we thought it would be most conservative to include (ii) as well into the composite measure as a combined response. The questions referred to any births (previous or future). Other study definitions are presented in Appendix 2.
Data collection
We randomly selected households to be visited for baseline and endline data collection in each district using a standard two stage sampling method with probability of selection proportional to size (i.e. random selection of villages followed by random selection of households) [19, 20]. Use of the same cooking hearth was used to define a household. Villages in Afghanistan do not use household listings, so we selected survey respondents using the ‘random walk’ method [21]. This method involved enumerators starting at a community landmark, spinning a bottle, walking in the direction the bottle points, and stopping at every third household to select a survey respondent.
Baseline and endline data were collected from women who were less than 12 months postpartum using a standardised structured survey questionnaire. Survey domains included self reported: education level, ownership of specific assets, sanitation facilities; service use for ANC, delivery, PNC; any home visits received from CHWs; and knowledge of the CCT intervention as defined above.
A separate independent team of female data collectors were trained over a five-day period and were supervised by two independent data supervisors. The data supervisors performed spot (unscheduled) checks of approximately 10% of the surveys together with a member of the study team. An additional 10% of surveys were selected for repeat survey. The data supervisors reviewed each survey form. Forms were not submitted for data entry until they were considered complete and without error. An additional random subsample of 10% of survey forms were also reviewed in the first week of data collection.
Data analysis
For the outcome evaluation we assessed mean differences in key variables (delivery in a health facility), from baseline (data collection immediately prior to the intervention) to endline (data collection 12 months after the intervention commenced) and compared effects in the intervention areas compared to control areas.
We calculated that we required a sample size of 3395 women to provide 90% power at a 5% significance level for the primary outcome [22]. These calculations were based on recent data at the provincial level, which indicated that there would be a baseline level of facility delivery of 50%, and previous studies that indicated that there would be at least a 25% change in service use due to the intervention [5, 16]. We also assumed that there would be one eligible woman per household. We calculated that this sample size would provide adequate power for the secondary outcomes as well.
We used the multivariable “difference-in-differences” (DiD) approach to estimate the mean effect of the intervention on each outcome [23, 24]. The “difference-in-differences” approach is based on comparing mean differences in the intervention group (before and after the intervention) to mean differences in the control group (before and after the intervention) and assumes that trends in both groups are the same in the absence of the intervention. We also assessed two key DiD assumptions (i) parallel trends in the primary and secondary outcomes pre and post intervention (using additional data from the Health Management Information System (HMIS) from 2013 to 2014) and (ii) stable distribution of covariates between intervention and control groups from baseline to endline [23–25].
Principal components analysis was used to create the wealth quintiles using standard methods [26]. Multivariable linear regression models were constructed to adjust for clustering by district and potential confounders decided a priori (maternal age, parity, education, quintile, access to health facilities) and to calculate adjusted mean differences (AMD), 95% confidence intervals (95% CI) and corresponding p values.
In addition, we performed a ‘treatment on the treated’ analysis with a restricted sample [27]. In this analysis intervention women were restricted to only women who were “treated” (i.e. who received the intervention composite measure as defined above). Control women were restricted to only women who did not receive the intervention (i.e. who were “not treated”). The restrictions were applied to endline mothers only. The restrictions were not applied to baseline mothers because baseline mothers had not been exposed to the intervention. Stata version 14.2 was used for all analyses.
Results
General characteristics
Of 2540 women aged 16 years and above invited to participate in the baseline evaluation survey, 2441 agreed to participate (96.1%). Of 2505 women approached at endline 2491 agreed to participate (99.4%). A total of 4929 women were recruited, 2453 intervention (1199 baseline, 1254 endline) and 2476 control (1242 baseline 1234 endline) (Table 1). 33.1% (1632) were from Bamyan, 32.2% (1588) from Badghis, and 34.3% (1681) from Kandahar. 36.7% (1811) women were aged 16–24 years, 10.8% (534) had only one child, 84.4% (4160) had no education, 534 (10.8%) had only one child, and 893 (18.1%) were in the poorest quintile (Table 1), Overall, 10.9% (525/4929) of mothers had missing data for quintile and 360/4929 (7.1%) had missing data for maternal age.
Exposure
The composite measure of CCT program exposure (mother reported that she knew (i) there were any programs that would give her money if she delivered in a health facility or (ii) she would receive our CCT incentive if she delivered in a health facility) was low overall 342/1254 (27.3%) (Table 2). (17.9% (224) knew only (i) (that there were any programs that would give a mother money) plus 4.5% (57) knew only (ii) (about our CCT program) plus 4.9% (61) knew both (i) and (ii)).
Table 2.
Intervention exposure and contamination
| Number (%) of mothers in intervention villages at endline (‘exposure’) n = 1254 | Number (%) of mothers in control villages at endline (‘contamination’) n = 1237 | |
|---|---|---|
| Mother reports that there are active programs promoting institutional delivery in her area and: | ||
| There are any programs that give money to a mother if she delivers in a public health centreb | 285/1228a (23.2%) | 95/1189a (8.0%) |
| The programs give money to a mother for transportation to a health centre for delivery | 231/1228 (18.8%) | 97/1189 (8.2%) |
| The programs give money to CHWs if mothers deliver in a health centre | 130/1228 (10.6%) | 51/1189 (4.3%) |
| The programs provide information about the importance of delivering a baby in a health centre | 95/1228 (7.7%) | 159/1189 (13.4%) |
| The programs provide transportation to a health centre | 380/1228 (30.9%) | 194/1189 (16.3%) |
| Mother reported that she knew she would receive our CCT incentive if she delivered in a health facilityb | 118/1254 (9.4%) | 119/1237 (9.6%) |
| Composite measure of CCT program exposurec | 342/1254 (27.3%) | 195/1237 (15.8%) |
CCT conditional cash transfer
a 26 women in intervention villages and 48 women in control villages reported they “did not know” and were excluded
b Included in the composite measure
c Mother reported that she knew (i) there were programs that would give her money if she delivered in a health facility or (ii) she would receive our conditional cash transfer (CCT) incentive if she delivered in a health facility
Exposure was lowest in the poorest quintile (10.2%, 17/166 women with known wealth quintile data) compared to the least poor women in quintile five (64.8%, 175/270). 195/1237 (15.8%) of the control group also appeared to have also been exposed (‘contaminated’) (Table 2). Contamination was similarly lowest in the poorest quintile (8.1%, 21/258 women with known wealth quintile data) compared to the least poor women in quintile five (38.8%, 59/152).
Facility delivery
Baseline facility delivery rates were low, 62.9% (744) in the intervention group and 58.7% (726) in the control group. Overall, facility delivery increased in intervention villages by 14.3% and control villages by 8.4%, adjusted mean difference (AMD) 3.3%; 95% confidence Interval (95% CI) (− 0.14 to 0.21), p value 0.685 (Table 3). In the least poor quintile the proportion of women who delivered in a health facility increased in the intervention villages by 29.9% and increased in the control villages by 15.4% (AMD 6.6% [− 0.20 to 0.33], p value 0.602) (Table 3). In the poorest quintile the proportion of women who delivered in a health facility increased in the intervention villages by 22.5% and increased in the control villages by 22.4% (AMD 0.8% [− 0.30 to 0.32], p value 0.953).
Table 3.
Institutional delivery compared between intervention and control areas by quintile
| Number (%) of mothers in intervention | Number (%) of mothers in control | Crude mean difference (95% CI) | P value | Adjusted mean differencea (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Unrestricted analysis | ||||||
| Overall | n = 2432 | n = 2469 | n = 4901 | n = 3883 | ||
| Baseline (n = 2441) | 744/1182 (62.9%) | 726/1236 (58.7%) | ||||
| Endline (n = 2491) | 965/1250 (77.2%) | 827/1233 (67.1%) | ||||
| Difference | 14.3% | 8.4% | 5.9% (0.01–0.11) | 0.027 | 3.3% (−0.14–0.21) | 0.685 |
| Quintile 1 (poorest) | n = 888 | n = 708 | ||||
| Baseline (n = 465) | 55/111 (49.6%) | 165/354 (46.6%) | ||||
| Endline (n = 423) | 119/165 (72.1%) | 178/258 (69.0%) | ||||
| Difference | 22.5% | 22.4% | 0.1% (−0.14–0.14) | 0.979 | 0.8% (− 0.30–0.32) | 0.953 |
| Quintile 2 | n = 869 | n = 753 | ||||
| Baseline (n = 446) | 141/220 (64.1%) | 125/226 (55.3%) | ||||
| Endline (n = 423) | 192/254 (75.6%) | 105/169 (62.1%) | ||||
| Difference | 11.5% | 6.8% | 4.7% (−0.08–0.18) | 0.475 | 5.4% (− 0.14–0.24) | 0.541 |
| Quintile 3 | n = 878 | n = 801 | ||||
| Baseline (n = 455) | 190/290 (65.5%) | 99/165 (60.0%) | ||||
| Endline (n = 423) | 149/200 (74.5%) | 153/223 (68.6%) | ||||
| Difference | 9.0% | 8.6% | 0.4% (−0.12–0.13) | 0.954 | −3.0% (− 0.27–0.20) | 0.781 |
| Quintile 4 | n = 876 | n = 780 | ||||
| Baseline (n = 459) | 153/239 (64.0%) | 161/220 (73.2%) | ||||
| Endline (n = 417) | 142/142 (71.3%) | 135/218 (61.9%) | ||||
| Difference | 7.3% | −11.3% | 18.6% (0.06–0.31) | 0.003 | 10.7% (−0.20–0.42) | 0.465 |
| Quintile 5 | n = 869 | n = 841 | ||||
| Baseline (n = 447) | 150/235 (63.8%) | 143/212 (67.5%) | ||||
| Endline (n = 422) | 253/270 (93.7%) | 126/152 (82.9%) | ||||
| Difference | 29.9% | 15.4% | 14.4% (0.03–0.26) | 0.011 | 6.6% (−0.20–0.33) | 0.602 |
| Restricted analysisb | ||||||
| Overall | n = 1524 | n = 2275 | n = 3799 | n = 2938 | ||
| Baseline (n = 2418) | 744/1182 (62.9%) | 726/1236 (58.7%) | ||||
| Endline (n = 1381) | 291/342 (85.1%) | 690/1039 (66.4%) | ||||
| Difference | 22.2% | 7.7% | 14.5% (0.08–0.21) | < 0.001 | 6.1% (− 0.17–0.29) | 0.575 |
| Quintile 1 (poorest) | n = 128 | n = 591 | n = 719 | n = 542 | ||
| Baseline (n = 465) | 55/111 (49.6%) | 165/354 (46.6%) | ||||
| Endline (n = 254) | 13/17 (76.5%) | 165/237 (69.6%) | ||||
| Difference | 26.9% | 23.0% | 3.9% (−0.20–0.28) | 0.746 | −0.7% (− 0.42–0.41) | 0.971 |
| Quintile 2 | n = 238 | n = 366 | n = 604 | n = 491 | ||
| Baseline (n = 446) | 141/220 (64.1%) | 125/226 (55.3%) | ||||
| Endline (n = 158) | 17/18 (94.4%) | 89/140 (63.6%) | ||||
| Difference | 30.3% | 8.3% | 22.0% (0.06–0.38) | 0.007 | 21.4% (0.07–0.36) | 0.008 |
| Quintile 3 | n = 329 | n = 352 | n = 681 | n = 607 | ||
| Baseline (n = 455) | 190/290 (65.5%) | 99/165 (60.0%) | ||||
| Endline (n = 226) | 28/39 (71.8%) | 131/187 (70.1%) | ||||
| Difference | 6.3% | 10.1% | −3.8% (−0.22–0.14) | 0.684 | −5.8% (−0.35–0.24) | 0.673 |
| Quintile 4 | n = 295 | n = 408 | n = 703 | n = 609 | ||
| Baseline (n = 459) | 153/239 (64.0%) | 161/220 (73.2%) | ||||
| Endline (n = 244) | 40/56 (71.4%) | 114/188 (60.6%) | ||||
| Difference | 7.4% | −12.6% | 20.0% (0.04–0.36) | 0.016 | 6.3% (−0.30–0.42) | 0.709 |
| Quintile 5 | n = 410 | n = 305 | n = 715 | n = 689 | ||
| Baseline (n = 447) | 150/235 (63.8%) | 143/212 (67.5%) | ||||
| Endline (n = 268) | 168/175 (96.0%) | 71/93 (76.3%) | ||||
| Difference | 32.2% | 8.8% | 23.4% (0.11–0.36) | < 0.001 | 13.5% (−0.21–0.48) | 0.404 |
aAdjusted for clustering by district, maternal age, parity, maternal education, quintile and access to health facilities
bIntervention endline population restricted to mothers who reported that she knew (i) there were any programs that would give her money if she delivered in a health facility or (ii) she would receive our CCT incentive if she delivered in a health facility; intervention baseline population not restricted. Control endline population restricted to mothers who reported that she did not know (i) or (ii); control baseline population not restricted
Restricting the analysis to women who were known to have received the intervention (treatment on the treated analysis) had little effect overall (AMD 6.1% [− 0.17 to 0.29], p value 0.575) or within each quintile (Table 3).
Antenatal and postnatal care
The proportion of women who had received at least one ANC visit at baseline was 64.8% (760) in the intervention group and 87.3% (1039) in the control group (Table 4). The proportion of women who had received at least one PNC visit at baseline was much lower; 49.1% (571) in the intervention group and 65.0% (764) in the control group.
Table 4.
ANC, PNC and CHW home visiting compared between intervention and control areas by quintile
| Number (%) of mothers in intervention villages | Number (%) of mothers in control villages | Crude mean difference (95% CI) | P value | Adjusted mean differencea (95% CI) | P value | |
|---|---|---|---|---|---|---|
| ANC | ||||||
| Overall | n = 2427 | n = 2425 | n = 4852 | n = 3871 | ||
| Baseline (n = 2363) | 760/1173 (64.8%) | 1039/1190 (87.3%) | ||||
| Endline (n = 2489) | 957/1254 (76.3%) | 729/1235 (59.0%) | ||||
| Difference | 11.5% | −28.3% | 39.8% (0.35–0.45) | < 0.001 | 45.0% (0.18–0.72) | 0.004 |
| Quintile 1 (poorest) | n = 273 | n = 599 | n = 872 | n = 706 | ||
| Baseline (n = 449) | 70/107 (65.4%) | 288/342 (84.2%) | ||||
| Endline (n = 423) | 88//166 (53.0%) | 101/257 (39.3%) | ||||
| Difference | −12.4% | −44.9% | 32.5% (0.19–0.46) | < 0.001 | 43.2% (−0.17–1.03) | 0.145 |
| Quintile 2 | n = 467 | n = 378 | n = 845 | n = 746 | ||
| Baseline (n = 421) | 138/212 (65.1%) | 192/209 (91.9%) | ||||
| Endline (n = 424) | 153/255 (60.0%) | 74/169 (43.8%) | ||||
| Difference | 5.1% | −48.1% | 43.0% (0.31–0.55) | < 0.001 | 55.4% (0.10–1.00) | 0.021 |
| Quintile 3 | n = 353 | n = 384 | n = 872 | n = 800 | ||
| Baseline (n = 448) | 179/287 (62.4%) | 151/161 (93.8%) | ||||
| Endline (n = 424) | 174/201 (86.6%) | 143/223 (64.1%) | ||||
| Difference | 24.2% | −29.7% | 53.9% (0.43–0.64) | < 0.001 | 58.0% (0.23–0.94) | 0.004 |
| Quintile 4 | n = 440 | n = 435 | n = 875 | n = 780 | ||
| Baseline (n = 453) | 162/240 (67.5%) | 171/213 (80.3%) | ||||
| Endline (n = 422) | 174/200 (87.0%) | 144/222 (64.9%) | ||||
| Difference | 19.5% | −15.4% | 34.9% (0.24–0.46) | < 0.001 | 29.0% (−0.08–0.66) | 0.112 |
| Quintile 5 | n = 508 | n = 358 | n = 866 | n = 839 | ||
| Baseline (n = 445) | 157/238 (66.0%) | 183/207 (88.4%) | ||||
| Endline (n = 421) | 260/270 (96.3%) | 125/151 (82.8%) | ||||
| Difference | 30.3% | −5.6% | 35.9% (0.26–0.46) | < 0.001 | 28.8% (−0.04–0.61) | 0.077 |
| PNC | ||||||
| Overall | n = 2415 | n = 2407 | n = 4822 | n = 3850 | ||
| Baseline (n = 2339) | 571/1164 (49.1%) | 764/1175 (65.0%) | ||||
| Endline (n = 2483) | 905/1251 (72.3%) | 690/1232 (56.0%) | ||||
| Difference | 23.2% | −9.0% | 32.3% (0.27–0.38) | < 0.001 | 31.8% (− 0.05–0.68) | 0.080 |
| Quintile 1 (poorest) | n = 273 | n = 596 | n = 869 | n = 707 | ||
| Baseline (n = 445) | 56/107 (52.3%) | 241/338 (71.3%) | ||||
| Endline (n = 424) | 78/166 (47.0%) | 99/258 (38.4%) | ||||
| Difference | −5.3% | −32.9% | 27.6% (0.13–0.42) | < 0.001 | 37.5% (− 0.38–1.13) | 0.296 |
| Quintile 2 | n = 467 | n = 373 | n = 840 | n = 743 | ||
| Baseline (n = 418) | 112/212 (52.8%) | 145/206 (70.4%) | ||||
| Endline (n = 422) | 140/255 (54.9%) | 73/167 (43.7%) | ||||
| Difference | 2.1% | −26.7% | 28.7% (0.15–0.42) | < 0.001 | 43.7% (− 0.16–1.04) | 0.137 |
| Quintile 3 | n = 482 | n = 383 | n = 865 | n = 791 | ||
| Baseline (n = 444) | 142/282 (50.4%) | 115/162 (71.0%) | ||||
| Endline (n = 421) | 163/200 (81.5%) | 133/221 (60.2%) | ||||
| Difference | 31.1% | −10.8% | 41.9% (0.30–0.54) | < 0.001 | 45.8% (−0.47–096) | 0.071 |
| Quintile 4 | 437 | n = 433 | n = 870 | n = 775 | ||
| Baseline (n = 448) | 120/237 (50.6%) | 113/211 (53.6%) | ||||
| Endline (n = 422) | 177/200 (88.5%) | 141/222 (63.5%) | ||||
| Difference | 37.9% | 9.9% | 27.9% (0.16–0.40) | < 0.001 | 21.6% (−0.25–0.68) | 0.332 |
| Quintile 5 | n = 506 | n = 535 | n = 859 | n = 834 | ||
| Baseline (n = 437) | 106/236 (44.9%) | 99/201 (49.3%) | ||||
| Endline (n = 422) | 260/270 (96.3%) | 125/152 (82.2%) | ||||
| Difference | 51.4% | 32.9% | 18.4% (0.07–0.30) | 0.002 | 8.4% (−0.41–0.58) | 0.716 |
| CHW home visiting | ||||||
| Overall | n = 2433 | n = 2436 | n = 4869 | n = 3860 | ||
| Baseline (n = 2414) | 529/1186 (44.6%) | 637/1228 (51.9%) | ||||
| Endline (n = 2455) | 519/1247 (41.6%) | 338/1208 (28.0%) | ||||
| Difference | −3.0% | −23.9% | 20.9% (0.15–0.26) | < 0.001 | 12.2% (−0.27–0.51) | 0.508 |
| Quintile 1 (poorest) | n = 275 | n = 611 | n = 886 | n = 707 | ||
| Baseline (n = 466) | 71/110 (64.6%) | 219/356 (61.5%) | ||||
| Endline (n = 420) | 19/165 (11.5%) | 32/255 (12.6%) | ||||
| Difference | −53.1% | −48.9% | −4.1% (−0.16–0.08) | 0.511 | −1.9% (− 0.76–0.72) | 0.954 |
| Quintile 2 | n = 473 | n = 392 | n = 865 | n = 750 | ||
| Baseline (n = 444) | 121/218 (55.5%) | 105/226 (46.5%) | ||||
| Endline (n = 421) | 36/255 (14.1%) | 28/166 (16.9%) | ||||
| Difference | −41.4% | −29.6% | −11.8% (−0.24- -0.00) | 0.049 | 6.4% (−0.53–0.66) | 0.819 |
| Quintile 3 | n = 489 | n = 377 | n = 866 | n = 790 | ||
| Baseline (n = 456) | 142/291 (48.8%) | 66/165 (40.0%) | ||||
| Endline (n = 410) | 73/198 (36.9%) | 61/212 (28.8%) | ||||
| Difference | −11.9% | − 11.2% | −0.7% (−0.14–0.12) | 0.916 | −2.8% (−0.60–0.55) | 0.917 |
| Quintile 4 | n = 436 | n = 432 | n = 868 | n = 773 | ||
| Baseline (n = 448) | 92/239 (38.5%) | 91/219 (41.6%) | ||||
| Endline (n = 410) | 92/197 (46.7%) | 78/213 (36.6%) | ||||
| Difference | 8.2% | −5.0% | 13.1% (0.00–0.26) | 0.050 | 0.0% (−0.35–0.35) | 0.999 |
| Quintile 5 | n = 509 | n = 359 | n = 868 | n = 840 | ||
| Baseline (n = 447) | 61/239 (25.5%) | 111/208 (53.4%) | ||||
| Endline (n = 421) | 242/270 (89.6%) | 101/151 (66.9%) | ||||
| Difference | 64.1% | 13.5% | 50.5% (0.38–0.63) | < 0.001 | 34.5% (−0.18–0.87) | 0.175 |
ANC antenatal care, PNC postnatal care, CHW community health worker
aAdjusted for clustering by district, maternal age, parity, maternal education, quintile and access to health facilities
Overall, the proportion of women with at least one ANC visit increased in the intervention villages by 11.5% but decreased in the control villages by 28.3% (AMD 45.0% [0.18 to 0.72], p value 0.004) (Table 4). In the least poor quintile, the proportion of women with at least one ANC visit increased by 30.3% in the intervention villages and decreased in the control villages by 5.6% (AMD 28.8% [− 0.04 to 0.61], p value 0.077). In contrast, in the poorest quintile, ANC decreased in both the intervention villages (− 12.4%) and the control villages (− 44.9%) (AMD 43.2% [− 0.17 to 1.03] p value 0.145).
Overall, the proportion of women with at least one PNC visit increased in the intervention villages by 23.2% and decreased in the control villages by 9.0% (AMD 31.8% [− 0.05 to 0.68], p value 0.080) (Table 4). In the least poor quintile the proportion of women with at least one PNC visit increased in the intervention villages by 51.4% and increased in the control villages by 32.9% (AMD 8.4% [− 0.41 to 0.58] p value 0.716). In contrast, in the poorest quintile, PNC decreased in both the intervention (− 5.3%) and the control villages (− 32.9%) (AMD -37.5% [− 0.38 to 1.13] p value 0.296).
CHW home visiting
Less than half of families received any visits from a CHW at baseline, 44.6% (529) in the intervention group and 51.9% (637) in the control group (Table 4). Overall, CHW home visiting decreased more in the control villages (− 23.9%) compared to the intervention villages (− 3.0%) though the difference did not reach statistical significance (AMD -12.2% [− 0.27 to 0.51], p value 0.508) (Table 4).
In the least poor quintile CHW home visiting in the intervention districts increased from 25.5% at baseline to 89.6% at endline (AMD 34.5% [− 0.18 to 0.87]) p value 0.175). However, in the poorest quintile CHW home visiting decreased in both intervention (− 53.1%) and control districts (− 48.9%) (AMD -1.9% [− 0.76 to 0.72] p value 0.954) (Table 4).
Other analyses
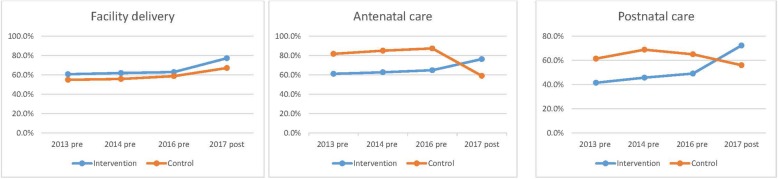
The two key DiD assumptions appeared to hold (Figs. 1 and 2). There were parallel trends in the primary and secondary outcomes pre and post intervention (i.e. we tested for and did not reject the null of parallel trends prior to intervention onset for facility delivery [p value = 0.0748], ANC [p value = 0.0685] and PNC [p value = 0.1029] [Fig. 1]). There was also stable distribution of covariates between intervention and control groups from baseline to endline (Appendix 3). Because 10.9% (525/4929) of mothers had missing data for socio economic status and 360/4929 (7.1%) had missing data for maternal age, we performed sensitivity analyses including the missing data with no change to any outcomes (Appendix 4).
Fig. 2.
Trends in facility delivery, antenatal care and postnatal care in the study area pre and post intervention
Discussion
Baseline rates of MCH service use were concerningly low in our study area in rural Afghanistan, only 61% of women delivered in a health facility and 76% received at least one ANC visit. Despite increasing levels of conflict, CCT provided to women aged 16–49 years in our study was associated with increases in maternal and newborn service use and CHW home visiting, though only the change in ANC was statistically significant. There was some evidence of greater effect in the least poor quintile compared to the poorest quintile. Program exposure was low, especially in the poorest quintile.
Overall, there was only a 3% increase in facility delivery associated with the CCT intervention, and this increase was not statistically significant. This contrasts with effects of 10–20% reported in other Asian studies [5, 6]. We feel that low CCT program exposure was an important reason for the modest effect of our intervention. Only 27% of women in intervention areas reported that they had heard about financial incentives or our CCT program. When we performed a ‘per protocol’ analysis (i.e. an analysis restricted to women who knew they would receive money if they delivered in a health facility) [26], the effect size increased though results were still not statistically significant. It is important to understand the reasons for the limited impact of our CCT intervention on institutional delivery (i.e. the incentivized behavior). An indepth analysis of ‘implementation’ ‘process’ data is needed, i.e. to understand the ‘reach’ of our IEC delivery channels including billboards, brochures, CHWs and village leaders. This will be reported in a separate manuscript.
Prior to the onset of the study we conducted detailed formative research and our interviewees (women of reproductive age, male heads of households, village leaders) provided consistent feedback that home visiting from CHWs would be of most use to families. An important part of our planned exposure was home visits from CHWs to raise awareness and to plan transport and assistance for facility delivery and cash transfer. Our CHW data demonstrate the complex nature of working in Afghanistan. Conflict has increased over the 12 months since program implementation [14], and has restricted the movements of the Afghanistan volunteer CHW workforce [28]. In our study, CHW home visits reduced in both intervention and control areas over the intervention period but the decrease was greater in the control areas. This suggests that our CCT intervention may have improved CHW motivation in the intervention areas despite the increasing conflict. Ongoing Afghanistan HMIS surveillance [17] will help to understand further trends. We also feel that our CHWs could be better trained in home visiting as a recent study indicates this is an important way of accessing pregnant and postpartum women in Afghanistan and can significantly improve ANC, facility delivery and PNC [29]. Due to funding constraints we only allocated one day to the CHW training and had to cover many topics from record keeping to IEC messages. Future work must include longer training periods and pre and post training assessments.
We actively monitored impact on ANC and PNC services because we were concerned that their coverage might decrease. However, surprisingly, our intervention was associated with improvements in both ANC and PNC coverage, though only the change in ANC was statistically significant. This is most likely due to the effectiveness of the ANC and PNC messages that were included in our IEC campaigns. Our findings are also consistent with previous studies in Afghanistan reporting the effectiveness of basic ANC and PNC messages communicated by CHWs [29, 30]. Also, in Asian studies, mothers report that they prefer travelling for ANC visits compared to PNC or facility delivery because there is more choice of clinic site and timing [31]. Our formative research indicates that the situation is similar in Afghanistan [9].
Disappointingly the effect of our CCT intervention was consistently lowest in the poorest quintile. The low rate of program exposure in the poorest women was also of concern. Poor uptake of CCT interventions in the most disadvantaged communities is reported in many other studies [3, 31]. The importance of designing CCT programs so they are appropriate to the local context and meet the needs of the poorest families is clearly described [31]. We included remote areas and trained CHW to prioritise the poorest families in their home visiting. However, the CHWs reported difficulties in accessing the poorest families due to lack of trust and the distances they needed to travel. More work is needed in our study area to ensure that our interventions are truly progressive and understand the perspectives of the most disadvantaged families.
We are very aware that quality of health service provision is a driver of demand [32, 33]. At the health facility level our CCT intervention focused on efficiency of payments to the family and CHW. We did implement a HSS package in both the intervention and control health facilities but this focused on training and quality of care and we were not able to increase staffing levels. The mothers who participated in our formative research reported that sometimes no midwives were present to assist with deliveries after hours [9]. In Afghanistan, due to low wages, some doctors and nurses work in private clinics in the afternoons and evenings. However, in our study, these problems were likely to be non-differential across intervention and control groups. Most importantly, the MoPH is working to improve workforce conditions and staffing levels for MCH services.
We encountered other challenges especially conflict reducing access to onsite training of CHWs and community leaders. This delayed the start of the project by six months. Monitoring is a challenge for all programs across Afghanistan due to conflict and mountainous regions [34]. However, in our study we included additional funds for overnight accommodation and for male staff to accompany our largely female data collectors and supervisors. We also included a dedicated independent field worker to monitor the cash transfer.
Our study had some limitations. It was non-randomised. Our study findings can only be generalised to public health facilities because there were no private facilities in our study area. Intervention and control districts were purposively chosen to ensure similar socio economic status of families but there were still baseline differences in socio demographic characteristics in the intervention and control districts. However, ‘difference-in-differences’ analyses were used to account for potentially differing trends in control and intervention areas. We also adjusted for all potential confounding factors though residual confounding was still possible. We were not able to collect cost data from families or perform a cost effectiveness analysis. Outcome data were self-reported and verification was not possible due to project restrictions, however we consider that any recall bias was likely to be non-differential. We also only allowed 12 months for implementation and we are aware that CCT projects can take time to embed. Some women might have only been exposed to the intervention for a limited period before they delivered. However, the CCT message was quite simple so we feel that the duration of intervention was of limited importance. We also consider that exposure rates were underestimated in our study. The intervention was delivered to all family members but the ascertainment of ‘exposure’ data relied solely on maternal self report. Literacy (26.2%) and education rates (15.6%) were low in our study and mothers may not have understood some of the more complex exposure questions. If we had been able to ascertain exposure more accurately we may have been able to show a greater impact ‘per protocol’. 10% of our quintile and 7% of our maternal age data were missing however no change to results were observed when these data were included in the primary and secondary analyses.
Difference-in-differences’ analyses require two main assumptions to be fulfilled: ‘common shocks’ and ‘parallel trends’ [23, 35]. We showed stable distribution of covariates between intervention and control groups from baseline to endline indicating no disparate changes in the intervention compared to the control group. There were also no differential policy shocks or changes between the intervention and control groups during the intervention period. However there has been a major escalation in conflict in both the intervention and control districts over the study period. We feel that that the CCT had an important effect in maintaining ANC, PNC and CHW homevisiting levels in the intervention group and without the CCT program the ANC, PNC and CHW levels would have been the same level as the control group. We consider that facility delivery was preserved in the intervention and control districts as there has been a major focus on facility delivery across Afghanistan from the MoPH. We also tested for and did not reject the null of parallel trends. Though it is important to note that there were some systematic differences between intervention and control groups, and our sample size did not provide enough statistical precision to conclusively reject the null.
Strengths included our prospective community and population based design, large sample size and high response rate (94%). We had an intensive data quality and supervision plan which included scheduled and unscheduled revisits. Overall, our study demonstrated that a CCT program provided to women aged 16–49 years can be implemented in a highly conservative conflict affected population and can include fathers and male heads of households as well as female family members. It is likely that if we can improve our focus on the poorest families, CCT will have important impacts on facility delivery, ANC and PNC.
Conclusions
Almost 400 million women and children are estimated to live in conflict-affected areas globally and these numbers are increasing [36]. Our innovative study demonstrates the important ‘proof of principle’ that CCT for mothers and newborns can be implemented in emergency situations and fragile states. There is an imperative to implement and evaluate novel and ‘outside the box’ interventions for the mothers and children that live in deprived and conflict affected communities across the world. We encourage other governments and researchers to also implement and evaluate CCT in conflict affected areas.
Acknowledgements
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
This study was funded by the Japanese International Cooperation Agency (JICA). The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to the lack of an online platform but are available from the corresponding author on reasonable request.
Abbreviations
- 95% CI
95% confidence intervals
- AMD
Adjusted mean difference
- ANC
Antenatal care
- BEmONC
Basic and emergency obstetric and newborn care
- CCT
Conditional cash transfer
- CHS
Community health supervisor
- CHW
Community health worker
- DiD
Difference-in-differences
- ENC
Essential newborn care
- HMIS
Health management information system
- HSS
Health systems strengthening
- IEC
Information, education, communication
- MCH
Maternal and child health
- MD
Mean difference
- MoPH
Ministry of Public Health
- ORS
Oral rehydration therapy
- PNC
Postnatal care
Appendix 1
Table 5.
Characteristics of intervention and control districts
| Intervention districts (n = 6) | Control districts (n = 6) | |
|---|---|---|
| Population | ||
| Total population | 544,191 | 657,906 |
| Mean (sd) population | 10,884 (11,824) | 15,300 (17,418) |
| Total number of pregnant women | 21,767 | 26,316 |
| Mean (sd) number of pregnant women per district | 3628 (1857) | 4386 (2231) |
| Total number of children under five years | 108,838 | 131,581 |
| Mean (sd) number of children under five years per district | 181,40 (9282) | 21,930 (11,154) |
| Sociodemographicsa | ||
| Mean (sd) % poorest wealth quintile | 843 (917) | 1012 (965) |
| Mean (sd) % no female education | 1638 (2004) | 2380 (3052) |
| Accessa | ||
| % Remote | 100% | 100% |
| % Mountainous | 86.0% | 81.4% |
| % High security risk | 24.0% | 34.9% |
| Health servicesa | ||
| Total number of fixed health facilities (SHC, BHC, CHC, DH) | 50 | 43 |
| Number of sub health centres | 16 | 12 |
| Mean (sd) sub health centres per district | 4.0 (4.2) | 3.0 (1.8) |
| Mean (sd) population per sub health centre | 24,481 (21,330) | 25,830 (25,427) |
| Number of basic health centres | 21 | 18 |
| Mean (sd) basic health centres per district | 3.5 (1.4) | 3.0 (1.8) |
| Mean (sd) population per basic health centre | 58,632 (40055) | 50,430 (42355) |
| Number of comprehensive health centres | 4 | 6 |
| Mean (sd) comprehensive health centres per district | 1.0 (0.0) | 1.2 (0.4) |
| Mean (sd) population per comprehensive health centre | 17,851 (16,209) | 33,140 (32,561) |
| Number of district hospitals | 1 | 2 |
| Mean (sd) district hospitals per district | – | 1.0 (0.0) |
| Mean (sd) population per district hospital | 12,472 (0) | 34,048 (27,969) |
| Health facility density (population per health facility) | 10,268 | 15,300 |
| Health facility density (pregnant women and children under five population per health facility) | 2612 | 3672 |
| Number of vaccination outreach services | 4 | 6 |
| Number of mobile health teams | 4 | 5 |
| Number of community health workers | 7 | 8 |
| Number of mini ambulances | 1479 | 1353 |
sd standard deviation, SHC sub health centre, BHC basic health centre, CHC comprehensive health centre, DH district hospital
a See Appendix 2 for definitions
Appendix 2
Table 6.
Definitions of terms and covariates used in the study
| Health services | |
| Sub health centre (SHC) |
Targeted to whole population Staffed by generalist nurse, vaccinator, midwife Provide antenatal care, postnatal care, growth monitoring, vaccination and integrated management of childhood illness (IMCI) clinics but no delivery care or emergency care (emergency cases are stabilised and referred to BHC, CHC or DH) [15]. |
| Basic health centre (BHC) |
Targeted to whole population Staffed by generalist nurse, vaccinator, midwife Provide services as above, but also assistance to normal deliveries (emergency cases are stabilised and referred to BHC, CHC or DH) [15]. |
| Comprehensive health centre (CHC) |
Targeted to whole population Staffed by generalist nurse, vaccinator, midwife, doctor Provide services as above, but also basic emergency obstetric care from a midwife which includes manual removal of placenta and retained products, blood transfusion, basic laboratory services. Also provides vaccination outreach (one outreach service per CHC) [15] |
| District hospital (DH) |
Targeted to whole population Staffed by generalist nurse, vaccinator, midwife, doctor Provide services as above, but also comprehensive emergency obstetric care from a doctor or nurse which includes surgery, anaesthesia and Caesarean section. No outreach vaccination service [15]. |
| Health facility density | Population per health facility |
| Socio-demographics | |
| Poorest wealth quintile | Women scored in asset index as being in the lowest 20% of the population [20]. |
| No female education | Women with no formal education [20]. |
| Any female | |
| Access | |
| Remote | District centre more than 2 h by any form of transport from provincial capital [14]. |
| Mountainous | More than 1800 km elevation at highest point of district [14]. |
| High security risk | Use of armed force between warring parties in a conflict dyad, state-based or non-state, resulting in deaths). 25 deaths or less in the previous 12 months is categorised as low intensity security risk, 25–100 is categorised as moderate intensity security risk and 100+ is categorised as high intensity security risk [13]. |
SHC sub health centre, BHC basic health centre, CHC comprehensive health centre, DH district hospital
Appendix 3
Table 7.
Difference in difference analysis of sociodemographic characteristics of women included in the study compared between intervention and control villages
| Number (%) of mothers in intervention villages | Number (%) of mothers in control villages | Difference in intervention compared to control at baseline | Number (%) of mothers in intervention villages | Number (%) of mothers in control villages | Difference in intervention compared to control at endline | Difference in difference analysis between baseline and endline Crude mean difference (95% CI) | |
|---|---|---|---|---|---|---|---|
| Baseline | Baseline | Endline | Endline | ||||
| (n = 1199) | (n = 1242) | (n = 1254) | (n = 1237) | ||||
| Province | |||||||
| Bamyan | 421 (35.1%) | 413 (33.3%) | − 1.8% | 403 (32.1%) | 403 (32.6%) | 0.5% | −2.3% (− 0.08–0.03) |
| Badghis | 387 (32.3%) | 412 (33.2%) | 0.9% | 400 (31.9%) | 404 (32.7%) | 0.8% | 0.1% (−0.05–0.05) |
| Kandahar | 391 (32.6%) | 417 (33.6%) | 1.0% | 451 (36.0%) | 430 (34.8%) | −1.2% | 2.2% (− 0.03–0.07) |
| Maternal education | |||||||
| Primary school (year 1–6) | 38 (3.2%) | 74 (6.0%) | 2.8% | 46 (3.7%) | 86 (7.0%) | 3.3% | −0.4% (− 0.03–0.02) |
| Secondary school (year 7–9) | 33 (2.8%) | 40 (3.2%) | 0.4% | 34 (2.7%) | 38 (3.1%) | 0.4% | 0.1% (−0.02–0.02) |
| High school (year 10–12) | 32 (2.7%) | 57 (4.6%) | 1.9% | 72 (5.7%) | 73 (5.9%) | 0.2% | 1.7% (−0.01–0.04) |
| Advanced education (year 12+) | 14 (1.2%) | 22 (1.8%) | 0.6% | 20 (1.6%) | 49 (4.0%) | 2.4% | −1.8% (−0.03- -0.001) |
| No education | 1082 (90.2%) | 1038 (83.6%) | −6.6% | 1057 (84.3%) | 983 (79.5%) | −4.8% | −1.8% (−0.06–0.02) |
| Literacy | |||||||
| Literate | 223 (18.6%) | 279 (22.5%) | 3.9% | 412 (32.8%) | 382 (30.9%) | −1.9% | 5.8% (0.01–0.11) |
| Not literate | 976 (81.4%) | 963 (77.5%) | −3.9% | 842 (67.2%) | 855 (69.1%) | 1.9% | −5.8% (−0.11- -0.01) |
| Mother’s age | |||||||
| 16–24 years | 469 (39.1%) | 455 (36.6%) | −2.5% | 496 (39.6%) | 391 (31.6%) | −8.0% | 5.4% (−0.01–0.11) |
| 25–29 years | 407 (33.9%) | 346 (27.9%) | −6.0% | 307 (24.5%) | 386 (31.2%) | 6.7% | −12.8% (−0.17–0.07) |
| 30–39 years | 213 (17.8%) | 145 (11.7%) | −6.1% | 364 (29.0%) | 282 (22.8%) | −6.2% | 0.1% (−0.04–0.05) |
| 40 years or older | 108 (9.0%) | 70 (5.6%) | −3.4% | 86 (6.9%) | 47 (3.8%) | 3.1% | −0.3% (− 0.03–0.02) |
| Mother’s parity | |||||||
| 1 | 112 (9.3%) | 96 (7.7%) | −1.6% | 138 (11.0%) | 188 (15.2%) | 4.2% | −5.8% (−0.09–0.02) |
| 2 | 161 (13.4%) | 183 (14.7%) | 1.3% | 165 (13.2%) | 238 (19.2%) | 6.0% | −4.7% (− 0.09–0.01) |
| 3 | 209 (17.4%) | 242 (19.5%) | 2.1% | 160 (12.8%) | 208 (16.8%) | 4.0% | −2.0% (− 0.06–0.02) |
| 4 | 174 (14.5%) | 209 (16.8%) | 2.3% | 203 (16.2%) | 150 (12.1%) | −4.1% | 6.4% (−0.02–0.10) |
| 5 or more | 543 (45.3%) | 512 (41.2%) | −4.1% | 588 (46.9%) | 453 (36.6%) | −10.3% | 6.2% (−0.01–0.12) |
| Wealth quintile | |||||||
| Quintile 1 (poorest) | 111 (9.3%) | 358 (28.8%) | 19.5% | 166 (13.2%) | 258 (20.9%) | 7.7% | 11.9% (−0.08–0.16) |
| Quintile 2 | 223 (18.6%) | 228 (18.4%) | −0.2% | 255 (20.3%) | 169 (13.7%) | −6.6% | 6.4% (0.02–0.11) |
| Quintile 3 | 294 (24.5%) | 165 (13.3%) | −11.2% | 201 (16.0%) | 223 (18.0%) | 2.0% | −13.2% (0.18- -0.09) |
| Quintile 4 | 241 (20.1%) | 220 (17.7%) | −2.4% | 200 (16.0%) | 222 (18.0%) | 2.0% | −4.3% (0.09- -0.01) |
| Quintile 5 (least poor) | 239 (19.9%) | 212 (17.1%) | −2.8% | 270 (21.5%) | 152 (12.3%) | −9.2% | 6.4% (−0.02–0.11) |
| Access to any health facility | |||||||
| Less than 30 mins | 422 (35.2%) | 299 (24.1%) | −11.1% | 419 (33.4%) | 376 (30.4%) | −3.0% | −8.1% (0.13- -0.03) |
| 30 mins to 1 h | 405 (33.8%) | 595 (47.9%) | 14.1% | 509 (40.6%) | 531 (42.9%) | 2.3% | 11.8% (−0.06–0.17) |
| 1–2 h | 172 (14.4%) | 183 (14.7%) | 0.3% | 236 (18.8%) | 211 (17.1%) | −1.7% | 2.1% (− 0.02–0.06) |
| 2 h to half a day | 124 (10.3%) | 25 (2.0%) | −8.3% | 65 (5.2%) | 35 (2.8%) | −2.4% | −6.1% (0.09- -0.04) |
| More than half a day | 29 (2.4%) | 10 (0.8%) | −1.6% | 1 (0.1%) | 54 (4.4%) | 4.3% | −6.0 (0.08- -0.04) |
Appendix 4
Table 8.
Sensitivity analysis including missing data
| Number (%) of mothers in intervention villages | Number (%) of mothers in control villages | Crude mean difference (95% CI) | P value | Adjusted mean differencea (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Facility delivery quintile 3 | ||||||
| Excluding missing data | n = 878 | n = 801 | ||||
| Baseline (n = 455) | 190/290 (65.5%) | 99/165 (60.0%) | ||||
| Endline (n = 423) | 149/200 (74.5%) | 153/223 (68.6%) | ||||
| Difference | 9.0% | 8.6% | 0.4% (−0.12–0.13) | 0.954 | −3.0% (− 0.27–0.20) | 0.781 |
| Including missing data | n = 739 | n = 660 | n = 1399 | n = 1256 | ||
| Baseline (n = 621) | 245/377 (65.0%) | 132/224 (58.9%) | ||||
| Endline (n = 798) | 259/362 (71.6%) | 283/436 (64.9%) | ||||
| Difference | 6.6% | 6.0% | 0.6% (−0.98–0.11) | 0.912 | −0.5% (− 0.18–0.17) | 0.951 |
| Excluding missing data | n = 353 | n = 384 | n = 872 | n = 800 | ||
| Baseline (n = 448) | 179/287 (62.4%) | 151/161 (93.8%) | ||||
| Endline (n = 424) | 174/201 (86.6%) | 143/223 (64.1%) | ||||
| Difference | 24.2% | −29.7% | 53.9% (0.43–0.64) | < 0.001 | 58.0% (0.23–0.94) | 0.004 |
| Including missing data | n = 739 | n = 655 | n = 1394 | n = 1256 | ||
| Baseline (n = 595) | 233/376 (62.0%) | 205/219 (93.6%) | ||||
| Endline (n = 799) | 282/363 (77.7%) | 285/436 (65.4%) | ||||
| Difference | 15.7% | −28.2% | 43.9% (0.35–0.53) | < 0.001 | 49.4% (0.21–0.77) | 0.003 |
| PNC quintile 3 | ||||||
| Excluding missing data | n = 482 | n = 383 | n = 865 | n = 791 | ||
| Baseline (n = 444) | 142/282 (50.4%) | 115/162 (71.0%) | ||||
| Endline (n = 421) | 163/200 (81.5%) | 133/221 (60.2%) | ||||
| Difference | 31.1% | −10.8% | 41.9% (0.30–0.54) | < 0.001 | 45.8% (−0.47–096) | 0.071 |
| Including missing data | n = 732 | n = 652 | n = 1384 | n = 1245 | ||
| Baseline (n = 591) | 177/372 (47.6%) | 166/219 (75.8%) | ||||
| Endline (n = 793) | 250/360 (69.4%) | 252/433 (58.2%) | ||||
| Difference | 21.8% | −17.6% | 39.4% (0.29–0.50) | < 0.001 | 49.8% (−0.01–1.00) | 0.054 |
| CHW home visiting quintile 3 | ||||||
| Excluding missing data | n = 489 | n = 377 | n = 866 | n = 790 | ||
| Baseline (n = 456) | 142/291 (48.8%) | 66/165 (40.0%) | ||||
| Endline (n = 410) | 73/198 (36.9%) | 61/212 (28.8%) | ||||
| Difference | −11.9% | −11.2% | −0.7% (−0.14–0.12) | 0.916 | −2.8% (− 0.60–0.55) | 0.917 |
| Including missing data | n = 740 | n = 642 | n = 1382 | n = 1239 | ||
| Baseline (n = 599) | 184/380 (48.4%) | 111/219 (50.7%) | ||||
| Endline (n = 783) | 130/360 (36.1%) | 99/423 (23.4%) | ||||
| Difference | −12.3% | −27.3% | 15.0% (0.04–0.25) | 0.005 | 16.0% (−0.49–0.81) | 0.596 |
aAdjusted for clustering by district, maternal age, parity, maternal education, quintile and access to health facilities
Authors’ contributions
KE designed the evaluation, synthesized the data and wrote the first draft of the paper. AF, FF, MN, AHS designed and monitored and assisted with the subsequent drafts of the paper. NS, JB analysed the data. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethical approval was obtained from the Afghanistan Ministry of Public Health Institutional Review Board (IRB) for the implementation and evaluation of this study (study number 335540, received 28 October 2016). Informed verbal consent was obtained from all mothers prior to the baseline and endline surveys.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Karen M. Edmond, Phone: +93 730 71 7600, Email: kedmond@unicef.org
Abo Ishmael Foshanji, Email: hefd.foshanji@gmail.com.
Malalai Naziri, Email: mnaziri@unicef.org.
Ariel Higgins-Steele, Email: ahiggins@unicef.org.
Jane Machlin Burke, Email: machlin.burke@gmail.com.
Natalie Strobel, Email: natalie.strobel@uwa.edu.au.
Farhad Farewar, Email: hefd.farewar@gmail.com.
References
- 1.Countdown to 2030 Collaboration. Countdown to 2030: tracking progress towards universal coverage for reproductive, maternal, newborn, and child health. Lancet. 2018. [DOI] [PubMed]
- 2.Akseer N, Kamali M, Bakhache N, Mirza M, Mehta S, Al-Gashm S, Bhutta ZA. Status and drivers of maternal, newborn, child and adolescent health in the Islamic world: a comparative analysis. Lancet. 2018;391(10129):1493–1512. doi: 10.1016/S0140-6736(18)30183-1. [DOI] [PubMed] [Google Scholar]
- 3.Atun R, de Andrade LO, Almeida G, Cotlear D, Dmytraczenko T, Frenz P, Garcia P, Gómez-Dantés O, Knaul FM, Muntaner C, de Paula JB, Rígoli F, Serrate PC, Wagstaff A. Health-system reform and universal health coverage in Latin America. Lancet. 2015;385(9974):1230–1247. doi: 10.1016/S0140-6736(14)61646-9. [DOI] [PubMed] [Google Scholar]
- 4.Murray SF, Hunter BM, Bisht R, Ensor T, Bick D. Effects of demand-side financing on utilisation, experiences and outcomes of maternity care in low- and middle-income countries: a systematic review. BMC Pregnancy Childbirth. 2014;14:30. doi: 10.1186/1471-2393-14-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gopalan SS, Mutasa R, Friedman J, Das A. Health sector demand-side financial incentives in low- and middle-income countries: a systematic review on demand-and supply-side effects. Soc Sci Med. 2014;100:72–83. doi: 10.1016/j.socscimed.2013.10.030. [DOI] [PubMed] [Google Scholar]
- 6.Hunter BM, Harrison S, Portela A, Bick D. The effects of cash transfers and vouchers on the use and quality of maternity care services: a systematic review. PLoS One. 2017;12(3):e0173068. doi: 10.1371/journal.pone.0173068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lim SS, Dandona L, Hoisington JA, James SL, Hogan MC, Gakidou E. India's Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet. 2010;375(9730):2009–2023. doi: 10.1016/S0140-6736(10)60744-1. [DOI] [PubMed] [Google Scholar]
- 8.Lin A, Salehi AS Stimulating demand: effects of a conditional cash transfer programme on increasing maternal and child health-service utilisation in Afghanistan, a quasi-experimental study. Global Health Metrics & Evaluation: Data, Debates, Directions Meeting Abstract Special Issue. Lancet 2013;S84.
- 9.Higgins-Steele A, Burke J, Foshanji AI, Farewar F, Naziri M, Seddiqi S, Edmond KM. Barriers associated with care-seeking for institutional delivery among rural women in three provinces in Afghanistan. BMC Pregnancy Childbirth. 2018;18(1):246. doi: 10.1186/s12884-018-1890-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins-Steele A, Lai D, Chikvaidze P, Yousufi K, Anwari Z, Peeperkorn R, Edmond K. Humanitarian and primary healthcare needs of refugee women and children in Afghanistan. BMC Med. 2017;15(1):196. doi: 10.1186/s12916-017-0961-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gopalan SS, Das A, Howard N. Maternal and neonatal service usage and determinants in fragile and conflict-affected situations: a systematic review of Asia and the middle-east. BMC Womens Health. 2017;17(1):20. doi: 10.1186/s12905-017-0379-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Afghanistan Central Statistics Organisation 2016 . http://cso.gov.af/en. Accessed 23 Mar 2018.
- 13.Afghanistan Social Demographic and Economic Survey 2016. (SDES) http://cso.gov.af/en/page/1500/1494/sociodemographic-economic. Accessed 23 Mar 2018.
- 14.The World Bank Data 2018. Fragile and conflict affected situations. https://data.worldbank.org/region/fragile-and-conflict-affected-situations. Accessed 24 Apr 2018.
- 15.Afghanistan Living Conditions Survey ALCS. 2016. http://cso.gov.af/en/page/1500/1494/nrav-report. Accessed 23 Mar 2018.
- 16.Central Statistics Organisation (CS0). Ministry public health (MoPH) and ICF 2017. Demographic and health survey 2015. Kabul Afghanistan. Central Statistics Organization.
- 17.Afghanistan Health Management Information System. (HMIS) 2017. http://moph.gov.af/en/documents/category/health-management-information-system Accessed 23 Mar 2018.
- 18.Blank map of Afghanistan districts. Wikimedia Commons. https://commons.wikimedia.org/wiki/File:Blank_map_of_Afghanistan_districts.svg Accesseed 20 Apr 2019.
- 19.Bierrenbach AL. World Health Organization. Geneva. http://www.who.int/tb/advisory_bodies/impact_measurement_taskforce/meetings/prevalence_survey/psws_probability_prop_size_bierrenbach.pdf. Accessed 25 Nov 2017.
- 20.Lance PM, Hattori A. Sampling and evaluation, a guide to sampling for program impact evaluation. Chapel Hill, North Carolina: MEASURE Evaluation, University of North Carolina; 2016. [Google Scholar]
- 21.Bennett S. A simplified general method for cluster sample surveys of health in developing countries. http://apps.who.int/iris/bitstream/10665/47585/1/WHSQ_1991_44(3)_98-106_eng.pdf. [PubMed]
- 22.Centers for Disease Control and Prevention, Atlanta. Epi Info for Windows Version 7.2 2016. https://www.cdc.gov/epiinfo/support/downloads.html. Accessed 2 Jan 2016.
- 23.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401–2402. doi: 10.1001/jama.2014.16153. [DOI] [PubMed] [Google Scholar]
- 24.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 25.Wing C, Simon K, Bello-Gomez RA. Designing Difference in Difference Studies: Best Practices for PublichHealth Policy Research. Annu Rev Public Health. 2018;39(1):453–469. doi: 10.1146/annurev-publhealth-040617-013507. [DOI] [PubMed] [Google Scholar]
- 26.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data--or tears. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 27.Cochrane collaboration. Cochrane handbook, 2018. Per protocol analysis. http://handbook-5-1.cochrane.org/chapter_8/8_13_1_rationale_for_concern_about_bias.htm. Accessed 6th July 2018.
- 28.Burki T. Conflict in Afghanistan takes an increasing toll on civilians. Lancet. 2016;388(10040):117–118. doi: 10.1016/S0140-6736(16)31023-6. [DOI] [PubMed] [Google Scholar]
- 29.Edmond KM, Yousufi K, Anwari Z, Sadat SM, Staniczai SM, Higgins-Steele A, Bellows A, Smith ER. Can community health worker home visiting improve care seeking and maternal and newborn care practices in fragile states such as Afghanistan? A population based intervention study. BMC Med. 2018;16(1):106. doi: 10.1186/s12916-018-1092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Najafizada SAM, Labonté R, Bourgeault IL. Community health workers of Afghanistan: a qualitative study of a national program. Confl Heal. 2014;8:26. doi: 10.1186/1752-1505-8-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gopalan SS, Das A, Mutasa R. What makes Health Demand-Side Financing Schemes Work in Low-and Middle-Income Countries? A Realist Review. J Public Health Res. 2014;3(3):304. doi: 10.4081/jphr.2014.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frost A, Wilkinson M, Boyle P, Patel P, Sullivan R. An assessment of the barriers to accessing the Basic Package of Health Services (BPHS) in Afghanistan: was the BPHS a success? Glob Health. 2016;12(1):71. doi: 10.1186/s12992-016-0212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schouten LM, Hulscher ME, van Everdingen JJ, Huijsman R, Grol RP. Evidence for the impact of quality improvement collaboratives: systematic review. BMJ. 2008;336(7659):1491–1494. doi: 10.1136/bmj.39570.749884.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Edward Anbrasi, Kumar Binay, Kakar Faizullah, Salehi Ahmad Shah, Burnham Gilbert, Peters David H. Configuring Balanced Scorecards for Measuring Health System Performance: Evidence from 5 Years' Evaluation in Afghanistan. PLoS Medicine. 2011;8(7):e1001066. doi: 10.1371/journal.pmed.1001066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gertler, PJ, Martinez S, Premand P, Rawlings LB, Vermeersch CMJ. Impact evaluation in practice, second edition 2016. Washington, DC: Inter-American Development Bank and World Bank. https://openknowledge.worldbank.org/handle/10986/25030. Accessed 15 Jul 2018.
- 36.Bahgat K, Dupuy K, Østby G. Children and armed conflict. What existing data can tell us. Peace research institute Oslo. 2017. https://www.prio.org/utility/DownloadFile.ashx?id=1550&type=publicationfile. Accessed 30 Apr 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to the lack of an online platform but are available from the corresponding author on reasonable request.