Abstract
Background:
Breast cancer (BC) is the most common cancer among women globally and also in India. Early detection by screening is likely to reduce mortality and improve survival. To study the determinants of compliance to BC screening and referral by women in a community based BC screening programme in urban India.
Methods:
A community-based one-time cancer screening programme, implemented in the urban slums of Mumbai, India. The programme involves screening for breast cancer by Clinical Breast Examination (CBE) performed by trained primary health workers (PHWs), referral of screen-positive women to the nodal hospital for further investigations, confirmation of diagnosis and treatment. Univariate and multivariate logistic regression analysis in SPSS version 16 was used.
Results:
The compliance to screening, referral and treatment were 90.58%, 74.22% and 100% respectively. The results of multivariate logistic regression analysis demonstrate literate women, having family history of cancer, with tobacco habit, being treated for breast abnormalities, being ever pregnant and having history of contraceptive use were positive predictors while, women belonging to Muslim religion or speaking mother-tongue other than Marathi or Hindi were negative predictors of participation to screening. Educational status was the only significant predictor of compliance to referral. Screen-positive women with education of secondary school level or more were more likely to comply with referral.
Conclusions:
The programme ensured good compliance with screening, referral and treatment indicating feasibility and acceptability of CBE based BC screening programme by the community.
Keywords: Awareness, breast cancer, compliance, counseling, screening
Introduction
Globally, breast cancer is the leading cancer among women.[1] The age standardized rate (ASR) in terms of incidence of breast cancer among women globally and in India are 43.1 and 25.8 respectively, while the ASR in terms of mortality from breast cancer among women globally and in India are 12.9 and 12.7 respectively.[2] The incidence rates of breast cancer are high in the more developed regions. However there are more breast cancer cases in the less developed regions because of larger population size. The less developed regions show higher mortality and low survival rates of breast cancer, due to the absence of effective screening and treatment facilities. Breast cancer is the most frequent cause of cancer death in women in less developed regions (324,000 deaths, 14.3% of total).[3]
In India, the incidence of breast cancer has been steadily increasing over the past decade. and is now the leading cancer among women surpassing the cervical cancer.[2] Nearly all breast cancer cases in India are clinically detected, with majority presenting as locally advanced disease.[4] In India breast cancers are detected at younger age as compared to the western population, mainly because of younger population structure. Hence, it is crucial to identify a screening modality which may be apt to the Indian scenario.
Early detection can improve the treatment outcome and also increase the survival of breast cancer cases.[1] However there is no population-based nationwide screening programme for early detection and control of breast cancer in India. Mammography-based breast cancer screening is expensive and hence only feasible to be implemented in the high socio-economic regions. Also, mammography does not seem to have any added benefit over physical examination among women from 40-59 years of age group.[5,6] In recent years, the benefits of screening Mammography have been debated and it is advised that the harms and benefits of mammography screening need to be properly explained to the women.[7] Also clinical breast examination (CBE) detects additional cancers that may be missed by Mammography and those cancers are usually more aggressive.[8]
A community-based, cluster randomized controlled cohort study on screening for breast cancer by CBE in Mumbai,[9] demonstrated the feasibility of implementing CBE in low resource settings like India.
According to the WHO, social determinants of health are described as the parameters reflecting the living conditions of people including the conditions in which they are born and brought up. These parameters are molded by the distribution of money, power and resources at global, national and local levels.[10] The poor compliance with screening of breast cancer among Asian women have been linked to culture, education, income and language barriers.[11]
Hence, in this paper we study the effect of various socio-demographic factors on participation in screening, referral and treatment among the urban Indian women.
Materials and Methods
This is a community based breast cancer screening programme being implemented in the selected urban slums of Mumbai, India since July 2010. This is a service programme, aimed at early detection of common cancers in women by screening them with low-cost technologies. This is a service programme, aimed at early detection of common cancers in women by screening them with low-cost technologies. This study was implemented as a part of eleventh five year plan of the Government of India and was funded by the Dept. of Atomic Energy (DAE) to be implemented in the low socioeconomic population residing in the slums of Mumbai, India. The total population of Mumbai is 18.4 million. Around 41% of the population resides in the slums in Mumbai which vary in size from huge slum colonies to small colonies. We identified 50 slum clusters wherein no cancer awareness and/or screening was previously conducted and by convenience selected 10 amongst these which were near each other for the implementation of screening. The programme envisages covering a total population of 100,000, comprising nearly 48,000 female population of which around 16,000 were eligible for breast, uterine cervix and oral cancers screening, over a period of five years.
The outreach team comprised of Medical Officers, Medical Social Workers (MSWs), Primary Health Workers (PHWs) and Porters. The MSWs were graduates/postgraduates and primarily responsible for identifying communities for screening, sensitization of local stake holders, identifying community places for conducting screening camps, conducting door to door household survey, conducting interviews of eligible women and delivering Health Education session. The PHWs were school/high school educated women who were trained to perform the screening for breast, cervical and oral cancers. Both MSWs and PHWs played an important role in counseling the women to comply with the screening and referral.
Only the findings related to breast cancer screening are discussed in this paper. Household surveys were conducted in the selected clusters to enlist the eligible population for screening. The women in the age group of 30 and 64 years, residing in these slums and who did not suffer from any cancer in the past were eligible to participate in the breast cancer screening. A list of all such women was prepared. On the planned days of the screening camps, the MSWs went door to door, contacted the eligible women, explained the programme and invited them to participate. The informed consent form (ICF) was explained thoroughly by a MSW to the eligible women. The ICF included all information about the screening methodology, tests to be performed, information about other methods of screening breast cancers, referral mechanism and treatment modalities and facilities. They were given sufficient time to read and understand the ICF. If any woman had any question about the programme, they were answered by the programme team including PHWs, MSWs and Doctors. The eligible women consenting to participate voluntarily, signed the ICF or put their left thumb impression in the presence of a witness and were enrolled in the programme. Since this was a service programme implemented for the benefit of the community, local ethics committee approval was not sought.
After obtaining the informed consent, the enrolled participants were given unique participant identity code. The MSWs interviewed the enrolled women and recorded their socio-demographic (like age, literacy level, family income, occupation, etc), history of tobacco use, previous medical and surgical history and reproductive history (like age at menarche and menopause, marital status, no. of children, breast feeding duration, etc) on a pre-designed proforma questionnaire. This interview was performed at the woman's house and lasted for over 15-20 minutes on an average.
After the survey of one cluster pocket was completed, screening camps were held. A suitable large place like community function hall, temple yard, school halls, meeting rooms, gymnasiums in the community preferably within reach of 15 min from the houses of all women in that cluster were identified. The screening camps including activities like detailed health education session, screening for breast cancer and counseling sessions for women referred to higher centre were held at these places.
The women were then invited to a screening camp place. At the camp place, the MSWs conducted health education session [Figure 1] on risk factors, signs and symptoms, methods of early detection and prevention of breast, uterine cervix and oral cancers to the eligible women and answered their queries. They were explained about the screening procedures. The trained female PHWs performed CBE to screen the participant women for breast cancers, followed by demonstration of the technique of breast self-examination (BSE) to each woman. The women detected to have lesion suspicious of breast cancer (screen positive women) were referred to the nodal hospital for further diagnostic work up. A positive screening result was defined as any one of the following findings in one/both breasts on clinical breast examination by primary health workers: 1. Lump: All lumps excluding freely mobile lump in premenopausal women, any lump/localized thickening/asymmetrical nodular breast in postmenopausal women (women who had never had menses for the last 12 months were labeled as post-menopausal). 2. Nipple discharge- single duct serous/single or multiple duct blood stained. 3. Recent retraction of nipple. 4. Breast skin dimpling. 5. Nipple eczema. 6. Palpable supra-clavicular/axillary lymph nodes. The PHW recorded their findings of the screening on the proforma. All women who participated in screening were given an identity card with their photograph pasted on it. A transport vehicle was arranged to ferry the referred women to the nodal hospital and drop them back to their houses after completing the investigations at the nodal hospital. Also a PHW was retained at the nodal hospital to assist the women through the diagnostic workup.
Figure 1.

Health education session
The women received counseling [Figure 2] at various levels of the screening programme namely; for participating in screening, for attending referral after a positive screening result and for accepting treatment if diagnosed as a cancer case. The counseling sessions were conducted both by MSWs as well as doctors. A transport vehicle was arranged to ferry the referred women to the nodal hospital and drop them back to their houses after completing the investigations at the nodal hospital. Also a PHW was retained at the nodal hospital to assist the women through the diagnostic workup. The women found to have normal findings on CBE were advised monthly BSE and annual follow-up screening at any near-by municipal or government facility. All screen positive women who complied with the referral were examined by CBE at the Preventive Oncology screening clinic at the nodal hospital and were advised mammography/ultrasonography (USG) of the breast. The women confirmed negative after referral investigations and consultation were advised regular follow-up screening. The women diagnosed with breast malignancy were referred to the breast services for further management.
Figure 2.

Counseling by project staff
On completion of field work in each slum cluster (each cluster has a natural boundary like a road, a pipeline or railway line as boundary), the proforma questionnaires were transported to the project office, entered into the computer in the SQL software and analyzed in STATA or SPSS. The final report generated for each cluster was discussed periodically to identify the lacunae/errors if any and were improvised upon in the next cluster.
Results
The results achieved with respect to outcome of breast cancer screening at various levels are summarized in Figure 3.
Figure 3.
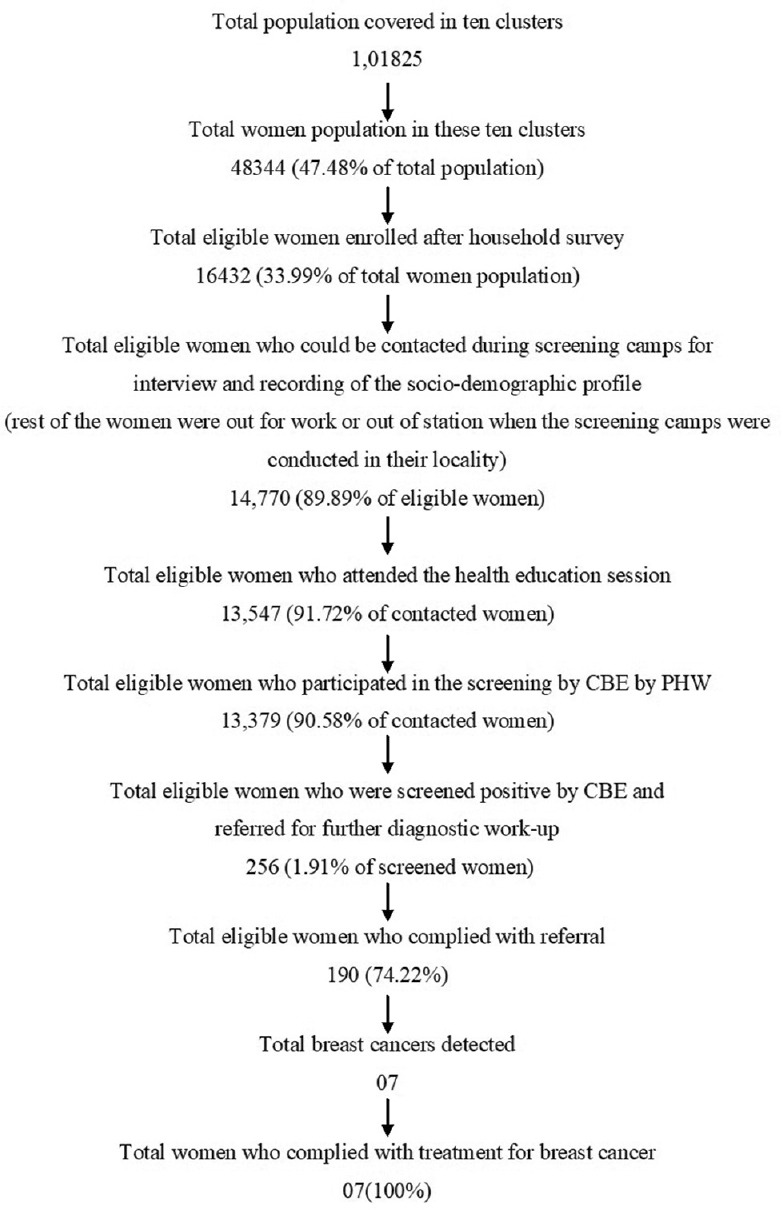
Outcome of the breast cancer screening programme
Table 1 gives the details of the compliance of eligible women in each cluster with respect to health education programme, breast cancer screening and referral.
Table 1.
Compliance to health education, screening and referral
| Cluster number | Total women | Total eligible for breast cancer screening (percentage of total women) | Total contacted (percentage of eligibles) | Total received health education (percentage of eligibles) | Total complied to screening (percentage of eligibles) | Total referred (percentage of screened) | Total complied to referral (percentage of referred) |
|---|---|---|---|---|---|---|---|
| 1 | 2957 | 1278 (43.22) | 1230 (96.24) | 1125 (91.46) | 1116 (90.73) | 45 (4.03) | 37 (82.22) |
| 2 | 1337 | 562 (42.03) | 532 (94.66) | 480 (90.23) | 480 (90.23) | 21 (4.38) | 16 (76.19) |
| 3 | 1957 | 685 (35.00) | 640 (93.43) | 573 (89.53) | 565 (88.28) | 36 (6.37) | 26 (72.22) |
| 4 | 1422 | 464 (32.63) | 427 (92.03) | 385 (90.16) | 382 (89.46) | 11 (2.88) | 5 (45.45) |
| 5 | 2373 | 691 (29.12) | 625 (90.45) | 594 (95.04) | 586 (93.76) | 9 (1.54) | 6 (66.67) |
| 6 | 8262 | 2893 (35.02) | 2398 (82.89) | 2206 (91.99) | 2149 (89.62) | 34 (1.58) | 21 (61.76) |
| 7 | 14811 | 5044 (34.06) | 4431 (87.85) | 4056 (91.54) | 4016 (90.63) | 48 (1.20) | 35 (72.92) |
| 8 | 8191 | 2406 (29.37) | 2217 (92.14) | 2026 (91.38) | 1999 (90.17) | 33 (1.65) | 28 (84.85) |
| 9 | 4475 | 1433 (32.02) | 1350 (94.21) | 1248 (92.44) | 1238 (91.70) | 8 (0.65) | 7 (87.50) |
| 10 | 2554 | 976 (38.21) | 920 (94.26) | 854 (92.83) | 848 (92.17) | 11 (1.30) | 8 (72.73) |
| Total | 48339 | 16432 (33.99) | 14770 (89.89) | 13547 (91.72) | 13379 (90.58) | 256 (1.91) | 189 (73.83) |
Univariate and multivariate logistic regression analysis were performed to correlate the relation of different socio-demographic and reproductive factors with the screening uptake behaviour [Table 2].
Table 2.
Univariate and multivariate logistic regression analysis for correlation of different variables with the compliance to screening
| Variables | Total women | Screened Number of women (%) |
Not screened Number of women (%) |
Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | CI | P | OR | CI | P | |||||
| Age | ||||||||||
| 30-35 | 4014 | 3652 (90.98) | 362 (9.02) | 1 | - | - | - | - | - | - |
| 36-41 | 3498 | 3177 (90.82) | 321 (9.18) | 0.981 | 0.838-1.149 | 0.812 | - | - | - | - |
| 42-47 | 3140 | 2839 (90.41) | 301 (9.59) | 0.935 | 0.796-1.098 | 0.411 | - | - | - | - |
| 48-53 | 2212 | 1991 (90.01) | 221 (9.99) | 0.893 | 0.749-1.065 | 0.208 | - | - | - | - |
| 54-59 | 1181 | 1076 (91.11) | 105 (8.89) | 1.016 | 0.809-1.275 | 0.893 | - | - | - | - |
| 60-64 | 725 | 644 (88.83) | 81 (11.17) | 0.788 | 0.611-1.017 | 0.067 | - | - | - | - |
| Education | ||||||||||
| Illiterate | 4144 | 3663 (88.39) | 481 (11.61) | 1 | - | - | 1 | - | - | - |
| Literate without formal education | 1025 | 928 (90.54) | 97 (9.46) | 1.256 | 0.998-1.581 | 0.052 | 1.388 | 1.098 | 1.755 | 0.006 |
| Primary school | 1251 | 1145 (91.53) | 106 (8.47) | 1.418 | 1.138-1.768 | 0.002 | 1.413 | 1.128 | 1.771 | 0.003 |
| Secondary school | 7299 | 6993 (95.81) | 606 (8.30) | 1.45 | 1.278-1.646 | 0 | 1.542 | 1.349 | 1.762 | 0 |
| Jr college | 619 | 563 (90.95) | 56 (9.05) | 1.32 | 0.987-1.765 | 0.061 | 1.483 | 1.092 | 2.015 | 0.012 |
| Sr college and above | 432 | 387 (89.58) | 45 (10.42) | 1.129 | 0.818-1.56 | 0.461 | 1.415 | 0.993 | 2.019 | 0.055 |
| Religion | ||||||||||
| Hindu | 10,481 | 9553 (91.15) | 928 (8.85) | 1 | 0.616-0.81 | - | 1 | - | - | |
| Muslim | 2531 | 2225 (87.91) | 306 (12.09) | 0.706 | 0.893-1.314 | 0 | 0.655 | 0.540 | 0.795 | 0 |
| Buddhists | 1555 | 1427 (91.77) | 128 (8.23) | 1.083 | 0.391-0.869 | 0.418 | 0.999 | 0.816 | 1.224 | 0.994 |
| Others | 203 | 174 (85.71) | 29 (14.29) | 0.583 | 0.616-0.81 | 0.008 | 0.743 | 0.489 | 1.130 | 0.165 |
| Mother tongue | ||||||||||
| Marathi | 9705 | 8897 (91.67) | 808 (8.33) | 1 | - | - | 1 | - | - | - |
| Hindi | 3508 | 3138 (89.45) | 370 (10.55) | 0.770 | 0.677-0.877 | 0 | 1.120 | 0.925 | 1.357 | 0.245 |
| Others | 1557 | 1344 (86.32) | 213 (13.68) | 0.573 | 0.488-0.673 | 0 | 0.706 | 0.590 | 0.844 | 0 |
| Occupation | ||||||||||
| Housewife/student/ | 11,776 | 10695 (90.82) | 1081 (9.18) | 1 | - | - | - | - | - | - |
| retired from service | ||||||||||
| Manual labour | 1809 | 1623 (89.72) | 186 (10.28) | 0.882 | 0.748-1.039 | 0.134 | - | - | - | - |
| Service | 673 | 610 (90.64) | 63 (9.36) | 0.979 | 0.749-1.278 | 0.874 | - | - | - | - |
| Self employed | 512 | 451 (88.09) | 61 (11.91) | 0.747 | 0.568-0.983 | 0.038 | - | - | - | - |
| Monthly income | ||||||||||
| <5000 | 5529 | 5002 (90.47) | 527 (9.53) | 1 | - | - | - | - | - | - |
| 5001-10000 | 8209 | 7437 (90.60) | 765 (9.32) | 1 | 0.798-1.253 | 0.997 | - | - | - | - |
| >10000 | 1039 | 940 (90.47) | 99 (9.53) | 1.024 | 0.822-1.276 | 0.834 | - | - | - | - |
| Marital status | ||||||||||
| Single | 263 | 223 (84.79) | 40 (15.21) | 1 | - | - | ||||
| Married | 12,494 | 11364 (90.96) | 1130 (9.040) | 1.804 | 1.281-2.540 | 0.001 | ||||
| Widows | 1775 | 1584 (89.24) | 191 (10.76) | 1.488 | 1.029-2.150 | 0.035 | ||||
| Separated/divorced | 238 | 208 (87.39) | 30 (12.61) | 1.244 | 0.747-2.070 | 0.402 | ||||
| Tobacco habits | ||||||||||
| Yes | 6893 | 6343 (92.02) | 550 (7.98) | 1 | - | - | 1 | - | - | - |
| No | 7877 | 7036 (89.32) | 841 (10.68) | 0.725 | 0.648-0.812 | 0 | 0.714 | 0.632 | 0.807 | 0 |
| Family h/o cancer | ||||||||||
| Yes | 1304 | 1237 (94.86) | 67 (5.14) | 10.497 | - | - | 1 | - | - | - |
| No | 13,466 | 12142 (90.17) | 1324 (9.83) | 0.386-0.639 | 0 | 0.511 | 0.394 | 0.661 | 0 | |
| History of cancer screening | ||||||||||
| Yes | 333 | 0 | 0 | 1 | - | - | 1 | - | - | - |
| No | 14,437 | 13058 (90.45) | 1379 (9.55) | 0.354 | 0.198-0.632 | 0 | 0.556 | 0.293 | 1.056 | 0.073 |
| History of screening for | ||||||||||
| Breast cancer | 141 | 139 (98.58) | 2 (1.42) | 1 | - | - | 1 | - | - | - |
| Other cancers | 14,629 | 13240 (90.51) | 1389 (9.49) | 0.137 | 0.034-0.554 | 0.005 | 0.473 | 0.099 | 2.260 | 0.348 |
| Menstrual status | ||||||||||
| Premenopausal | 9059 | 8219 (90.73) | 840 (9.27) | 1 | - | - | - | - | - | - |
| Perimenopausal/postmenopausal | 5711 | 5160 (90.35) | 551 (9.65) | 0.957 | 0.855-1.072 | 0.447 | - | - | - | - |
| History of pregnancy | ||||||||||
| Yes | 14,108 | 12815 (90.83) | 1293 (9.17) | 1 | - | - | 1 | - | - | - |
| No | 399 | 341 (85.46) | 58 (14.54) | 0.593 | 0.446-0.788 | 0 | 0.703 | 0.522 | 0.947 | 0.020 |
| History of treatment for breast abnormalities | ||||||||||
| Yes | 166 | 164 (98.80) | 2 (1.20) | 1 | - | - | 1 | - | - | - |
| No | 14,604 | 13215 (90.49) | 1389 (9.51) | 0.116 | 0.029-0.468 | 0.002 | 0.183 | 0.044 | 0.757 | 0.019 |
| History of use of contraceptives | ||||||||||
| Yes | 9817 | 9007 (91.75) | 810 (8.25) | 1 | - | - | 1 | - | - | - |
| No | 4690 | 4149 (88.46) | 541 (11.54) | 0.69 | 0.615-0.774 | 0 | 0.761 | 0.673 | 0.859 | 0 |
OR=Odds ratio, CI=Confidence interval
Compliance to screening
In the present programme, the overall compliance to screening was 90.58% with the compliance varying between 88.28% and 93.76% in the various project clusters. The univariate logistic regression analysis was performed on the relevant socio-demographic and reproductive variables. According to the results of univariate analysis, being school level educated, being married or widowed, being tobacco-user, having Marathi mother tongue, having family history of cancer, having participated in any cancer screening or breast cancer screening in the past, being ever pregnant, being treated for breast abnormalities in the past or having history of contraceptive use were positively associated with participation in screening. While Muslim women and women belonging to religion other than Hindu or Buddhists and women who were self-employed had lower participation to screening. According to multivariate analysis literate women, having family history of cancer, with tobacco habit, being treated for breast abnormalities, being ever pregnant and having history of contraceptive use were positive predictors of participation in screening. While Muslim women and women with mother-tongue other than Marathi or Hindi were negative predictors of participation in screening. The multivariate analysis did not demonstrate any relation between age of women, occupation, income, menstrual status, marital status, history of ever participated in cancer screening or breast cancer screening with compliance to screening with CBE.
Table 3 represents the results of univariate and multivariate logistic regression analysis to correlate the different socio-demographic variables with the referral uptake.
Table 3.
Univariate and multivariate logistic regression analysis for correlation of different variables with the compliance to referral
| Variables | Total women | Complied to referral Number of women (%) |
Not complied to referral Number of women (%) |
Univariate analysis | Multivariate analysis | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | CI | P | OR | CI | P | ||||||
| Age | |||||||||||
| 30-35 | 45 | 37 (82.22) | 8 (17.78) | 1 | - | - | - | - | - | - | - |
| 36-41 | 36 | 31 (86.11) | 513.(89) | 1.341 | 0.398 | 4.518 | 0.636 | - | - | - | - |
| 42-47 | 67 | 47 (70.15) | 20 (29.85) | 0.508 | 0.201 | 1.283 | 0.152 | - | - | - | - |
| 48-53 | 45 | 35 (77.78) | 10 (22.22) | 0.757 | 0.268 | 2.137 | 0.599 | - | - | - | - |
| 54-59 | 47 | 29 (61.70) | 18 (38.30) | 0.348 | 0.133 | 0.914 | 0.032 | - | - | - | - |
| 60-64 | 16 | 10 (62.50) | 6 (37.50) | 0.360 | 0.101 | 1.281 | 0.115 | - | - | - | - |
| Education | |||||||||||
| < Secondary school | 132 | 88 (66.67) | 44 (33.33) | 1 | - | - | - | 1 | - | - | - |
| ≥ Secondary school | 124 | 101 (81.45) | 23 (18.55) | 2.196 | 1.230 | 3.920 | 0.008 | 1.955 | 1.077 | 3.548 | 0.027 |
| Religion | |||||||||||
| Hindu | 189 | 137 (72.49) | 52 (27.51) | 1 | - | - | - | - | - | - | - |
| Muslim | 45 | 34 (75.56) | 11 (24.44) | 1.173 | 0.554 | 2.486 | 0.677 | - | - | - | - |
| Others | 22 | 18 (81.82) | 4 (18.18) | 1.708 | 0.552 | 5.285 | 0.353 | - | - | - | - |
| Mother tongue | |||||||||||
| Marathi | 175 | 135 (77.14) | 40 (22.86) | 1 | - | - | - | - | - | - | - |
| Hindi | 46 | 35 (76.09) | 11 (23.91) | 0.556 | 0.275 | 1.121 | 0.101 | - | - | - | - |
| Others | 35 | 24 (68.57) | 11 (31.43) | 0.646 | 0.292 | 1.433 | 0.283 | - | - | - | - |
| Occupation | |||||||||||
| Working | 210 | 156 (74.29) | 54 (25.71) | 1 | - | - | - | - | - | - | - |
| Nonworking | 46 | 33 (71.74) | 13 (28.26) | 0.879 | 0.431 | 1.792 | 0.722 | - | - | - | - |
| Monthly income | |||||||||||
| <5000 | 107 | 73 (68.22) | 34 (31.78) | 1 | - | - | - | - | - | - | - |
| 5001-10000 | 128 | 96 (75.00) | 32 (25.00) | 1.397 | 0.790 | 2.472 | 0.251 | - | - | - | - |
| >10000 | 21 | 20 (95.24) | 1 (4.76) | 9.315 | 1.200 | 72.299 | 0.033 | - | - | - | - |
| Marital status | |||||||||||
| Married/widowed | 209 | 157 (75.12) | 52 (24.88) | 1 | - | - | - | - | - | - | - |
| Separated/divorced/single | 47 | 32 (68.09) | 15 (31.91) | 0.707 | 0.355 | 1.407 | 0.323 | - | - | - | - |
| Tobacco habits | |||||||||||
| Yes | 116 | 87 (75.00) | 29 (25.00) | 1 | - | - | - | - | - | - | - |
| No | 140 | 102 (72.86) | 38 (27.14) | 0.510 | 1.569 | 0.895 | 0.698 | - | - | - | - |
| Family History of cancer | |||||||||||
| Yes | 29 | 25 (86.21) | 4 (13.79) | 1 | - | - | - | - | - | - | - |
| No | 227 | 164 (72.25) | 63 (27.75) | 0.417 | 0.139 | 1.245 | 0.117 | - | - | - | - |
| History of cancer screening | |||||||||||
| Yes | 14 | 10 (71.43) | 4 (28.57) | 1 | - | - | - | - | - | - | - |
| No | 242 | 179 (73.97) | 63 (26.03) | 1.137 | 0.344 | 3.753 | 0.834 | - | - | - | - |
| History of screening for | |||||||||||
| Breast cancer | 8 | 6 (75.00) | 2 (25.00) | 1 | - | - | - | - | - | - | - |
| Other cancers | 248 | 183 (73.79) | 65 (26.21) | 0.938 | 0.185 | 4.767 | 0.938 | - | - | - | - |
| Menstrual status | |||||||||||
| Premenopausal | 102 | 83 (81.37) | 19 (18.63) | 1 | - | - | - | 1 | - | - | - |
| Perimenopausal/postmenopausal | 154 | 106 (68.83) | 48 (31.17) | 0.506 | 0.276 | 0.925 | 0.027 | 0.592 | 0.318 | 1.105 | 0.100 |
| History of pregnancy | |||||||||||
| Yes | 245 | 181 (73.88) | 64 (26.12) | 1 | - | - | - | - | - | - | - |
| No | 7 | 4 (57.14) | 342.(86) | 0.471 | 0.103 | 2.164 | 0.333 | - | - | - | - |
| History of treatment for breast abnormalities | |||||||||||
| Yes | 10 | 9 (90.00) | 1 (10.00) | 1 | - | - | - | - | - | - | - |
| No | 246 | 180 (73.17) | 66 (26.83) | 0.303 | 0.038 | 2.438 | 0.262 | - | - | - | - |
| History of use of contraceptives | |||||||||||
| Yes | 178 | 134 (75.28) | 44 (24.72) | 1 | - | - | - | - | - | - | - |
| No | 74 | 51 (68.92) | 23 (31.08) | 0.728 | 0.400 | 1.325 | 0.299 | - | - | - | - |
OR=Odds ratio, CI=Confidence interval
Compliance to referral
Overall 256 women with referral rate of 1.91% were screened positive and were advised further diagnostic referral after CBE by the PHWs. The referral rate to the nodal hospital varied from 0.65% to 6.37% in different slum clusters. 189 (73.83%) screen positive women complied with the referral. The compliance to referral varied from 54.55% to 87.50%. Univariate and Multivariate logistic regression analysis was performed to assess the association of different socio-demographic variables with the referral uptake.
According to results of univariate analysis, women with secondary school level or more education and with monthly income more than Rs. 10,000/- were more likely to comply with referral while women in the age group of 54 to 59 years and peri or postmenopausal women were less likely to comply with referral. However according to the results of multivariate logistic regression analysis the only factor that was significant predictor of compliance to referral was educational status. Women with education of secondary school level or more were more likely to comply with referral compared to other women.
Compliance to treatment
Among 189 women who complied with referral to the nodal hospital for diagnostic work-up, seven malignant cases were detected. All the breast cancer cases complied with both the initiation and completion of the entire treatment. This was irrespective of the stage at diagnosis of breast cancer or the differences in the socio-demographic variables. As the diagnostic tests were conducted only for the screen positive patients who complied for referral, we can have only an indirect estimate of false positives and the false negatives. Amongst the 189 screen positive patients who complied for referral, seven were true positives i.e., detected to have breast cancer, rest 182 were found to have no breast cancer and were labeled as false positives. Similarly, amongst the 13123 women who participated in breast cancer screening but were screened negative, 5 women were later detected with breast cancer in the subsequent 5 years and can be labelled as false negatives. Of the women who did not comply with referral at the nodal hospital, few visited nearby clinics/hospitals for investigations.
Discussion
Overall compliance
This paper presents the influence of different socio-demographic factors that affect the screening and referral uptake behavior of women in a community-based cancer screening programme. For a screening programme to be successful, it is essential that the programme ensures high participation of the eligible population throughout and the screening methods adopted in the screening programme are simple and acceptable to the eligible population. Failure at any level will lead to collapse of the entire programme. The present study achieved satisfactory compliance of the eligible population at all levels of the programme activities; namely, screening, referral and treatment completion. The compliance of women participating in the screening programme was 90.58%. This high rate of participation was ensured by adopting a systematic approach in implementing the programme like proper introduction of the programme to the eligible women, explaining them significance of getting screened, counseling the women to attend HE session and participate in the screening, holding camps at places within short distance from the women's houses, arranging evening camps for working women. WHO mentions participation of over 70% of the target population in the screening programme as one of the criteria for the screening programme to be successful.[12] Various trials of breast cancer screening with different modalities, conducted across India and abroad, indicate varied compliance with screening. The Mumbai study of screening with CBE demonstrated 75.62% compliance in the first round,[9] A population-based screening programme implemented in Denmark demonstrated a participation rate of 76.4% in the first round of screening with mammography[13] while the Trivandrum trial had 97% compliance to CBE in the first screening round.[14]
The present study demonstrated 73.83% compliance to referral diagnostic work up. This high compliance to referral was ensured by appropriate counseling to the women about the completing the diagnostic workup, arranging a transport vehicle to ferry these women and PHW assistance at nodal hospital. This saved substantial time as well as travel costs of the women, and also relieved their anxiety and thus ensured they get their work up completed. The Mumbai RCT of screening with CBE had 73% compliance to referral diagnostic work up among the breast screen positive women.[15]
Compliance to screening
The present study did not find any relation of age with compliance to screening. A RCT of breast and cervix cancer screening in Mumbai, showed younger women to be more compliant to both screening with CBE and referral.[9] Trivandrum trial reported younger women (between 30-39 years of age) to be more compliant with screening with CBE (than women ≥40 years).[14] This may be because of more awareness among younger women about health or because the older women do not perceive it to be important for them to get screened or due to inability of the elderly women to visit the camp place. In the present study, literate women elucidated better compliance to screening as compared to illiterate women. This was significant for all women educated up to graduation level. This may be attributed to the reason that education increases awareness about health-care utilization and disease prevention. This was also seen in the Mumbai CBE study,[9] while in the Trivandrum trial illiterate women showed better compliance to screening as compared to the literate women.[14] In Iran, illiterate or less educated women had poor uptake of CBE and Mammography as compared to educated counterparts[16] while the Iranian study with mammography reflect significantly higher compliance to screening among women with higher education.[17]
The present study indicates poor participation in screening among Muslim women similar to Trivandrum.[14] The Mumbai study shows higher participation to screening among women belonging to religions other than Hindu and Muslim.[9] According to the present study women speaking languages other than Marathi and Hindi had significantly poor participation in screening. The Mumbai study for breast and cervix cancers demonstrated higher participation among Marathi speaking women.[9]
The present study revealed no significant association of occupation with compliance to screening similar to the Mumbai study.[9] Housewives demonstrated higher compliance with BSE among the Turkish women.[18] While in the rural Kerala study at Ernakulum, working women adhered more to screening.[19] In Trivandrum trial, women involved in manual work were most likely to participate in CBE.[14] The present study did not reveal any association of income with compliance to screening. The Mumbai study[9] and the Trivandrum study demonstrate that women from lower income families are more compliant with screening.[14] In a study from Tehran, Iran women from middle income families participated more in mammography as compared to others.[17]
The present study reflects lower participation to screening among women not using tobacco. This may be because of the women's self-perception that being a non-tobacco user may not have predisposed them to have breast cancer. A study in Brazil demonstrated lower compliance to screening among current smoker women.[20] A study in Israel, non-smoking was strongly associated with having three or more mammograms done during the 6 year study period.[21] Whereas, no relation between smoking status and practice of BSE was seen among Turkish women.[18] In the present study women with family history of cancer had better compliance to screening, similar to the findings of the Trivandrum trial,[15] the Iranian mammography study,[17] and US trial among Chinese immigrant women.[22] The present study showed no relation of menstrual status and marital status to participation in screening. Several studies show that being married is a significant predictor of participation in CBE.[14,19,22,23] A study implemented in Mexico demonstrated no association of menstrual status with compliance to breast cancer screening.[24] There was no relation seen between women having ever participated in screening for any cancer in the past and their current participation in screening. According to the study conducted in Brazil to have undergone previous biopsy was not found to be a predictor of compliance to screening.[20]
In present study being ever pregnant was a positive predictor of participation in screening. In the Trivandrum trial women with more than three pregnancies were more likely to participate in screening.[14] In the present study, similar to previous screening trial in Mumbai,[9] women with previously consultation for any breast condition were more likely to comply with screening. Women with history of contraceptive use demonstrated a greater compliance to screening similar to findings of the Trivandrum trial.[14]
Compliance to referral
There was no association of age with compliance to referral in the present study, similar to the findings of the Trivandrum trial.[14] While, in the Mumbai study, younger women complied better to referral.[15] In the present study, women educated with secondary school or more education were more likely to comply with referral to the nodal hospital. In the Mumbai study,[15] school level educated women and in the Kerala hospital study, women with higher education had better compliance to referrals for further diagnostic confirmation.[25] In the present study, no association was seen for religion and mother tongue to compliance with referral. However, in the previous Mumbai study women belonging to Christian religion complied poorly, while Marathi speaking women complied better to referral.[15] No significant association of occupation with compliance to referral is seen in the present study. Whereas, in the Mumbai study women in service or self-employed women had better compliance to referral.[15] Income was not a determining factor of acceptance of referral in the present study, similar to the findings of the Mumbai study,[15] whereas, income was directly associated with better compliance to referral according to the Kerala hospital study.[25] Marital status did not influence women's adherence to referral in the present study as also depicted in the Mumbai study.[15] However in the Kerala hospital study married women were more likely to seek medical attention for onset of symptoms of breast cancer.[25] No association was seen between family history of cancer and the referral uptake in the present study. Contrary to these findings, in the Trivandrum study,[14] women with positive family history of cancer were more likely to comply with referral. There was no significant association noted between history of prior treatment for breast abnormalities and compliance to referral similar to the Mumbai study.[15] No association was seen between history of tobacco use, history of participation in cancer screening or breast cancer screening in the past, menstrual status, being ever pregnant and history of contraceptive use with compliance to referral.
Before initiating any cancer screening programme, it is important to identify appropriate facilities for adequate diagnosis and treatment of screen detected cases. This is important for the success of the screening programme. The present trial showed 100% compliance with initiation and completion of treatment among the screen detected breast malignant cases. The Mumbai study demonstrated 95.3% compliance to initiation and 95.06% compliance to completion of treatment among the diagnosed breast cancer cases.[15] In a Nigerian study, age, marital status and religion were not significantly associated with acceptance of mastectomy.[26]
The programme achieved good coverage of the eligible population as shown by the high rates of contacting the eligible women and good participation of the women in health education, screening and referral services. An effective health education programme and good counseling is important to achieve good compliance with different stages of the programme. Also tailoring the programme activities as per the community needs and convenience ensures programme success. India is a country with vast population and major cultural diversity. We have learnt that to implement a screening programme at national level all of these factors related to designing and implementation of the programme need to be factored in. Also focused approaches with respect to predictors of good/poor compliance as shown in this study may be useful. This one time screening programme was implemented as a service programme strictly according to the planned protocol and the resources available. However we recognize that follow-up awareness and screening round is important and will try our best to implement it within next few years. This will also help throw light on what happened to the screen positive but not complied women for diagnostic investigations and screen negative women in the interim period.
Conclusions
The programme ensured good compliance with screening, referral and treatment indicating feasibility and acceptability of CBE based banker cancer screening programme by the community. Socio-demographic factors largely determine the compliance to screening, referral and treatment in a screening programme. It is therefore very essential to identify the factors which promote participation or which act as barriers to participation in screening. These can be considered for successful formulation of the national health policies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Breast Cancer: Prevention and Control. [Last accessed on 2014 Jun 03]. Available from: http://www.who.int/cancer/detection/breastcancer/en/
- 2.Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. Lyon, France: International Agency for Research on Cancer; 2013. [Last accessed on 2014 Jun 03]. GLOBOCAN 2012 v1.0. Cancer Incidence and Mortality Worldwide: IARC CancerBase No 11. Available from: http://www.globocan.iarc.fr . [Google Scholar]
- 3.IARC Release the Latest World Cancer Statistics, Sharp rise in Breast Cancer worldwide. 2013. Dec 12, [Last accessed on 2018 Sep 04]. Available from: https://www.uicc.org/iarc-release-latest-worldcancer-statistics .
- 4.Leong SP, Shen ZZ, Liu TJ, Agarwal G, Tajima T, Paik NS, et al. Is breast cancer the same disease in Asian and Western countries? World J Surg. 2010;34:2308–24. doi: 10.1007/s00268-010-0683-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA, et al. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian national breast screening study: Randomised screening trial. BMJ. 2014;348:g366. doi: 10.1136/bmj.g366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Health Quality Ontario. Screening mammography for women aged 40 to 49 years at average risk for breast cancer: An evidence-based analysis. Ont Health Technol Assess Ser. 2007;7:1–32. [PMC free article] [PubMed] [Google Scholar]
- 7.Løberg M, Lousdal ML, Bretthauer M, Kalager M. Benefits and harms of mammography screening. Breast Cancer Res. 2015;17:63. doi: 10.1186/s13058-015-0525-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Provencher L, Hogue JC, Desbiens C, Poirier B, Poirier E, Boudreau D, et al. Is clinical breast examination important for breast cancer detection? Curr Oncol. 2016;23:e332–9. doi: 10.3747/co.23.2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dinshaw K, Mishra G, Shastri S, Badwe R, Kerkar R, Ramani S, et al. Determinants of compliance in a cluster randomised controlled trial on screening of breast and cervix cancer in Mumbai, India 1.Compliance to screening. Oncology. 2007;73:145–53. doi: 10.1159/000126497. [DOI] [PubMed] [Google Scholar]
- 10.Social determinants of Health. [Last accessed on 2014 Dec 01]. Available from: http://www.who.int/social_determinants/sdh_definition/en/
- 11.Ahmadian M, Samah AA. A literature review of factors influencing breast cancer screening in Asian countries. Life Sci J. 2012;9:585–94. [Google Scholar]
- 12.Cancer: Screening. [Last accessed on 2018 Sep 04, 5:42 am]. Available from: http://www.who.int/cancer/prevention/diagnosis-screening/screening/en/
- 13.Lynge E, Bak M, von Euler-Chelpin M, Kroman N, Lernevall A, Mogensen NB, et al. Outcome of breast cancer screening in Denmark. BMC Cancer. 2017;17:897. doi: 10.1186/s12885-017-3929-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grosse Frie K, Ramadas K, Anju GA, Mathew BS, Muwonge R, Sauvaget CS, et al. Determinants of participation in a breast cancer screening trial in Trivandrum district, India. Asian Pac J Cancer Prev. 2013;14:7301–7. doi: 10.7314/apjcp.2013.14.12.7301. [DOI] [PubMed] [Google Scholar]
- 15.Dinshaw K, Mishra G, Shastri S, Badwe R, Kerkar R, Ramani S, et al. Determinants of compliance in a cluster randomised controlled trial on screening of breast and cervix cancer in Mumbai, India 2.Compliance to referral and treatment. Oncology. 2007;73:154–61. doi: 10.1159/000126498. [DOI] [PubMed] [Google Scholar]
- 16.Harirchi I, Azary S, Montazeri A, Mousavi SM, Sedighi Z, Keshtmand G, et al. Literacy and breast cancer prevention: A population-based study from Iran. Asian Pac J Cancer Prev. 2012;13:3927–30. doi: 10.7314/apjcp.2012.13.8.3927. [DOI] [PubMed] [Google Scholar]
- 17.Samah AA, Ahmadian M. Socio-demographic correlates of participation in mammography: A survey among women aged between 35-69 in Tehran, Iran. Asian Pac J Cancer Prev. 2012;13:2717–20. doi: 10.7314/apjcp.2012.13.6.2717. [DOI] [PubMed] [Google Scholar]
- 18.Doganer YC, Aydogan U, Kilbas Z, Rohrer JE, Sari O, Usterme N, et al. Predictors affecting breast self-examination practice among Turkish women. Asian Pac J Cancer Prev. 2014;15:9021–5. doi: 10.7314/apjcp.2014.15.20.9021. [DOI] [PubMed] [Google Scholar]
- 19.Sreedevi A, Quereshi MA, Kurian B, Kamalamma L. Screening for breast cancer in a low middle income country: Predictors in a rural area of Kerala, India. Asian Pac J Cancer Prev. 2014;15:1919–24. doi: 10.7314/apjcp.2014.15.5.1919. [DOI] [PubMed] [Google Scholar]
- 20.Caleffi M, Ribeiro RA, Bedin AJ, Jr, Viegas-Butzke JM, Baldisserotto FD, Skonieski GP. Adherence to a breast cancer screening program and its predictors in underserved women in Southern Brazil. Cancer Epidemiol Biomarkers Prev. 2010;19:2673–9. doi: 10.1158/1055-9965.EPI-10-0338. [DOI] [PubMed] [Google Scholar]
- 21.Katz D, Tengekyon AJ, Kahan NR, Calderon-Margalit R. Patient and physician characteristics affect adherence to screening mammography: A population-based cohort study. PLoS One. 2018;13:e0194409. doi: 10.1371/journal.pone.0194409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee-Lin F, Menon U, Nail L, Lutz KF. Findings from focus groups indicating what Chinese American immigrant women think about breast cancer and breast cancer screening. J Obstet Gynecol Neonatal Nurs. 2012;41:627–37. doi: 10.1111/j.1552-6909.2012.01348.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dahlui M, Gan DE, Taib NA, Pritam R, Lim J. Predictors of breast cancer screening uptake: A pre intervention community survey in Malaysia. Asian Pac J Cancer Prev. 2012;13:3443–9. doi: 10.7314/apjcp.2012.13.7.3443. [DOI] [PubMed] [Google Scholar]
- 24.Gonzalez P, Castaneda SF, Mills PJ, Talavera GA, Elder JP, Gallo LC, et al. Determinants of breast, cervical and colorectal cancer screening adherence in Mexican-American women. J Community Health. 2012;37:421–33. doi: 10.1007/s10900-011-9459-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ali R, Mathew A, Rajan B. Effects of socio-economic and demographic factors in delayed reporting and late-stage presentation among patients with breast cancer in a major cancer hospital in South India. Asian Pac J Cancer Prev. 2008;9:703–7. [PubMed] [Google Scholar]
- 26.Okobia MN, Bunker CH, Okonofua FE, Osime U. Knowledge, attitude and practice of Nigerian women towards breast cancer: A cross-sectional study. World J Surg Oncol. 2006;4:11. doi: 10.1186/1477-7819-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]


