Abstract
Background:
Continuity of care is widely regarded as an important marker of quality in the management of patients with long-term conditions. New services that integrate telemonitoring into care pathways have potential to change aspects of continuity in both positive and negative ways.
Aims:
A telemonitoring service for patients with chronic obstructive pulmonary disease (COPD) was introduced in Lothian, Scotland, in 2009. A qualitative study, nested within the TELESCOT COPD randomised control trial, was undertaken to explore the views of patients and professionals on telemonitoring. The perceived impact of telemonitoring on continuity of care was investigated as part of the research.
Methods:
Semi-structured interviews were undertaken with 38 patients (47% male, mean age 67.5 years). A maximum variation sample in relation to age, sex, socio-economic background, disease severity, and compliance with telemonitoring was recruited. Thirty-two stakeholders (healthcare professionals and managers) were interviewed. Transcribed coded data were analysed thematically using the framework approach. Interpretation was supported by multidisciplinary discussion.
Results:
Patients and healthcare professionals considered that relationship-based continuity of care was important in the delivery of telemonitoring services. Managers placed emphasis on improved continuity of clinical management as a means of reducing healthcare costs. However, professionals described many operational challenges arising from the ‘bolting-on’ of telemonitoring provision to existing usual care provision which, they considered, resulted in the proliferation of additional managerial discontinuities.
Conclusions:
Managers and healthcare professionals face major challenges in meeting demands for both relationship continuity and continuity of clinical management in the development of telemonitoring services.
Keywords: COPD, telehealth, primary care, qualitative research
Introduction
Policy makers and healthcare professionals have emphasised the importance of continuity of care, although precisely what is meant by this term is open to interpretation.1,2 Increasingly, discussion has centred on two types of continuity of care: ‘relationship continuity’, a continuous caring relationship with a clinician, and ‘continuity of clinical management’ including providing and sharing information, care planning, and coordination of care.3
Sustained continuity of care improves quality of life and reduces hospitalisations for patients with long-term conditions.4 There is, however, growing concern over the cost of continuity, both in terms of sustaining long-term patient-practitioner relationships and of providing ‘seamless care’. Of particular concern is the future sustainability of current clinician-centred models of care management for patients with long-term conditions.5
Patient self-management is increasingly promoted as a means of redistributing both the responsibility and cost of healthcare provision for people living with long-term health conditions. Policy makers and healthcare planners are adopting telemonitoring technologies* to support patient self-management as a means of both ‘minimising unnecessary face-to-face contact with health services’ and cutting costs.6,7 However, there are concerns regarding how telemonitoring fits with existing practice and services.8 Implementation of ‘standalone’ telemetric systems may challenge continuity of clinical management which, in turn, undermines continuity within patient-practitioner relationships.
In 2009, NHS Lothian set up a telemonitoring service for people with chronic obstructive pulmonary disease (COPD) with three aims: (1) to prevent hospital admissions resulting from delayed management of exacerbations; (2) to foster increased patient self-management of their condition; and (3) as a result of both these objectives to reduce healthcare costs.
The telemonitoring service used the Intel Health Guide (IHG)9 which enabled patients to assess their symptoms using an online touch-screen questionnaire. Linked pulse oximeter, peak flow meter and electronic weighing scales transmitted physiological measurements to the device either directly or using Bluetooth® technology. Patients were instructed to complete the questionnaire and measure oxygen saturation daily, and to use the peak flow device and scales on a weekly basis. Broadband Internet, installed in patients' homes, transmitted data from the device to remote monitoring centres.
The four geographical regions of Lothian adopted different models of monitoring incoming data for patients in their catchment area. The majority of patients were looked after by community respiratory physiotherapists or by community nurses providing anticipatory care services, with the remainder monitored by practice administrative staff who referred to a general practitioner (GP) for advice on management if necessary. Some patients were monitored by practitioners known to them prior to telemonitoring (e.g. their own GP) while others were monitored by professionals with whom they had no prior clinical relationship (e.g. physiotherapy and nursing teams).
All patients were monitored on weekdays. Professionals telephoned patients to address any matters arising from the transmitted data. Telemonitoring was additional to existing professional roles and responsibilities.
The ongoing TELESCOT randomised controlled trial which aims to investigate the impact of the service on hospital admissions10 contained a nested qualitative study to explore the views of patients and professionals on the implementation of telemonitoring. As part of the qualitative study, respondents were asked to discuss their views on the impact (if any) of telemonitoring on continuities of care.
Methods
Ethical approval
This study had ethical approval from the Lothian Research Ethics Committee (reference 08/S1101/60).
Semi-structured interviews
Semi-structured interviews were undertaken to explore the views of patients and professionals involved or associated with the trial telemonitoring service in Lothian. Data were collected between March 2010 and February 2011.
Sampling and recruitment
Patients
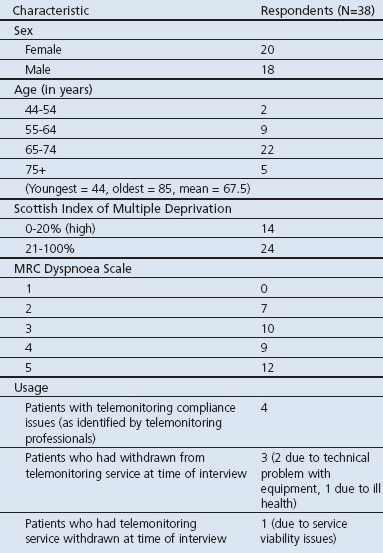
The patient sample was derived from those who agreed to participate in the TELESCOT trial.11 A maximum variation sample in relation to age, sex, socio-economic background (determined using the Scottish Index of Multiple Deprivation12), disease severity (using the MRC dyspnoea scale13) and compliance with telemonitoring (as identified by monitoring professionals) was undertaken to secure a diverse representation of the trial population.
Patients were invited by post to interview midway during their participation year in the trial. This enabled the collection of data from patients who had gained some familiarity with the technology and the monitoring service (earlier pilot work had acquired the perspectives of patients at entry point to the telemonitoring service14). Patients from the control group of the trial were also interviewed for comparative purposes. Reminder letters were sent to non-respondents one month after the dispatch of the first invitation.
Patient interviews occurred face-to-face within the person's home or by telephone. Interviews were conducted by a male postgraduate trained social researcher. The positioning of the researcher as investigator at ‘arms' length’ to primary care and the telemetric intervention helped facilitate open discussion. The researcher had family experience of COPD and his knowledge of the condition supported dialogue and understanding with respondents. The researcher had no prior contact with the patients involved in this study before invitation to interview.
Some patient participants requested that their partner/family member be present and contribute to the interview. Interview dyads were undertaken in those circumstances.
Professionals
Healthcare professionals with several months experience of delivering the service were interviewed. In addition to interviewing professionals with monitoring responsibilities, interviews were conducted with service managers, information technology suppliers, support staff (with training or administrative functions in relation to the telemonitoring service), nurses (those in primary and secondary care involved with COPD trial participants, COPD trial research nurses) as well as GPs who declined trial involvement in order to acquire a wide range of views. Healthcare professionals were interviewed either in their workplace or by telephone.
Interviews were undertaken until it was considered that data saturation had been reached.
Interview guides
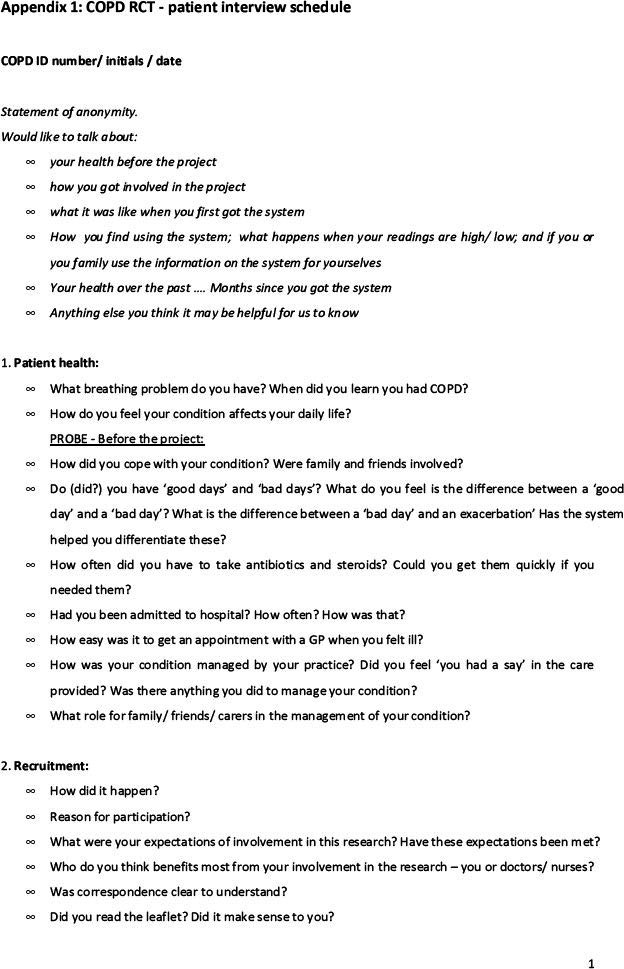
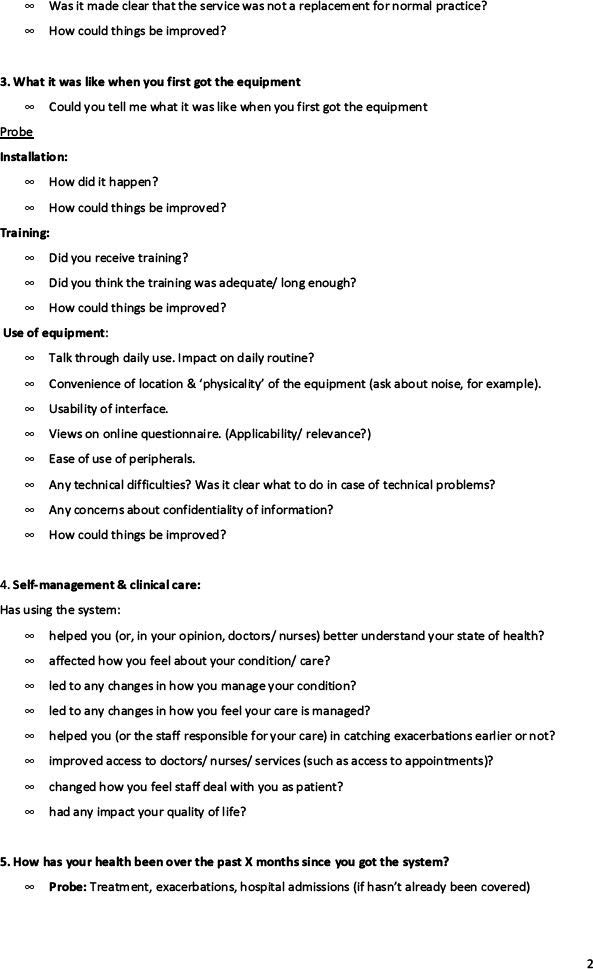
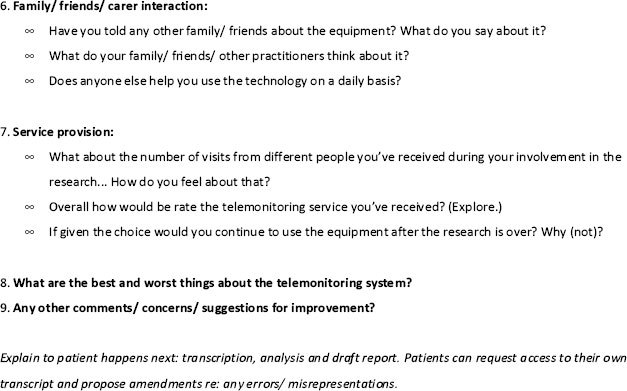
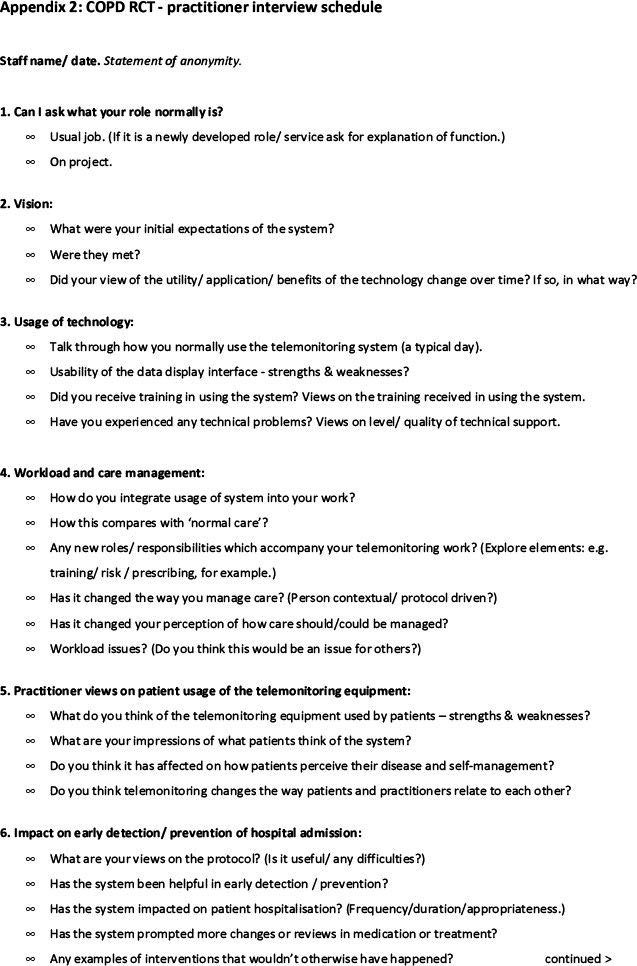
Interview guides were used to frame discussion. The initial guides were based on themes identified from the literature and from earlier pilot work undertaken within the TELESCOT programme.15 The guides were reviewed and refined iteratively during the process of data collection and analysis. The interviews explored patients' experiences of telemonitoring and their views on how telemonitoring compared with ‘usual care’. Professionals were asked their views on telemonitoring, how it affected practice or management (if at all), and the relationship between telemonitoring and usual care provision. (The interview guides are presented in appendices 1 & 2, available online at www.thepcrj.org)
Data collection
All interviews were audio recorded. Interviews were transcribed verbatim. Transcriptions were checked against the audio recordings.
Data analysis
Qualitative research is exploratory rather than confirmatory and conditional rather than conclusive. It is a means of providing answers to open research questions about phenomena that may be hard to predict and measure. Findings identified through qualitative study are not proof, but provide a description and an interpretation of social phenomena.16 In order to ensure that the results of qualitative research are meaningful and potentially transferable, it is important that the context in which the study took place is adequately described.
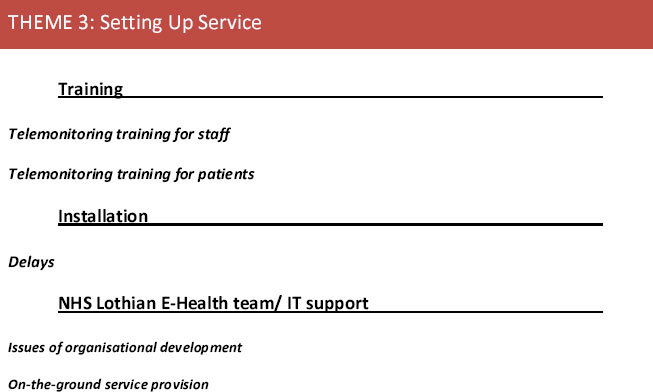
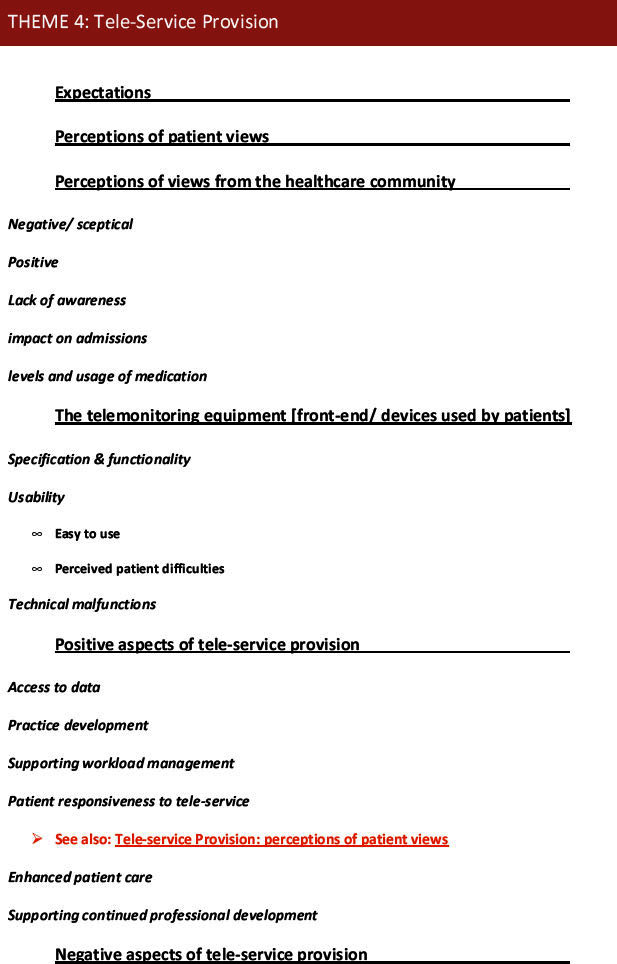
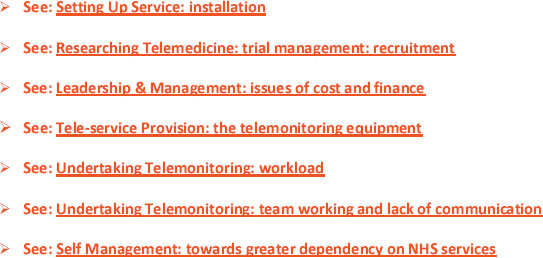
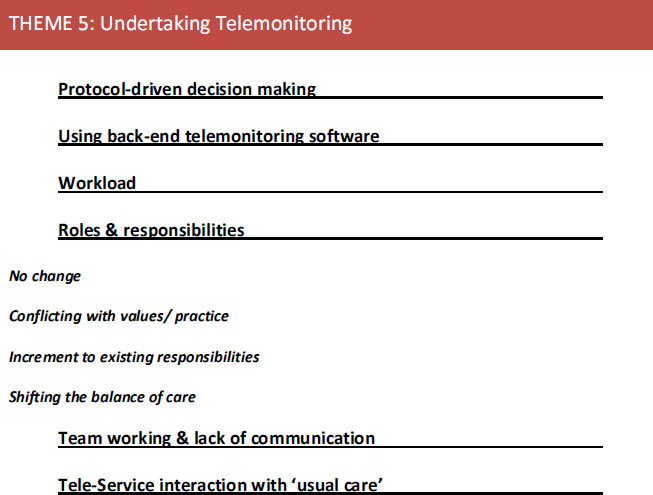
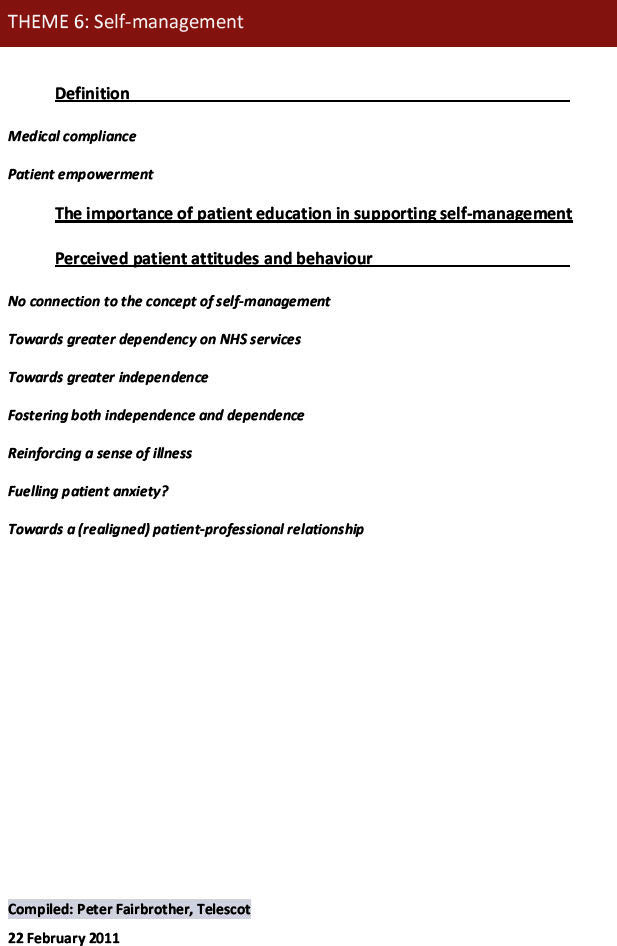
In this study the ‘Framework’ approach17 to data analysis was employed, given its applicability for applied or policy-relevant qualitative research. This approach involved researchers becoming immersed in the data and identifying a thematic framework based partly on the research questions, as well as data from the respondents. The data were then indexed by applying the framework to the whole dataset. The themes were subsequently charted into overarching themes and used to define concepts. Explanations of the data were considered by drawing on the original research objectives as well as the themes. Constant comparison (checking experiences against those of others in the sample) was undertaken to ensure that the thematic analysis represented all perspectives.
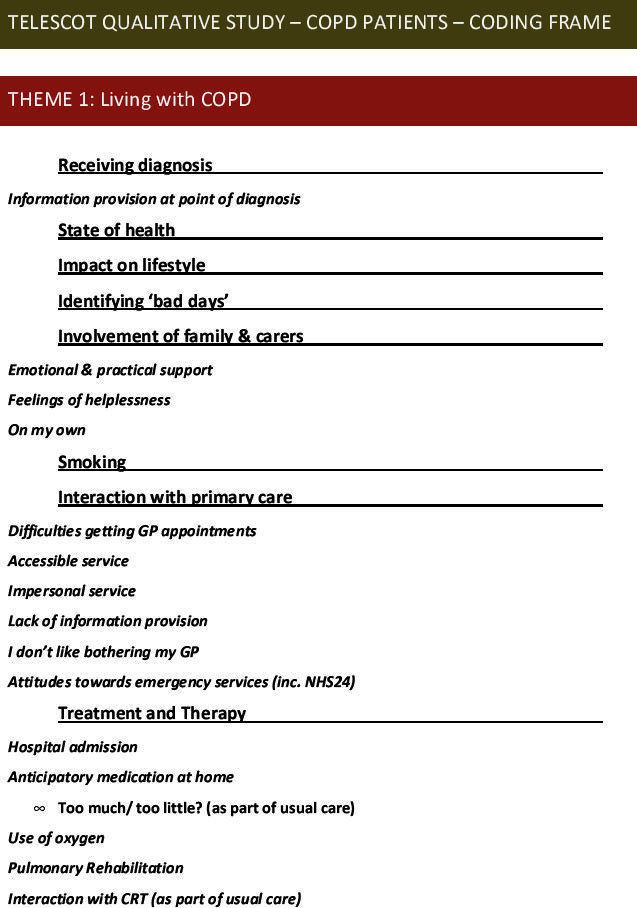
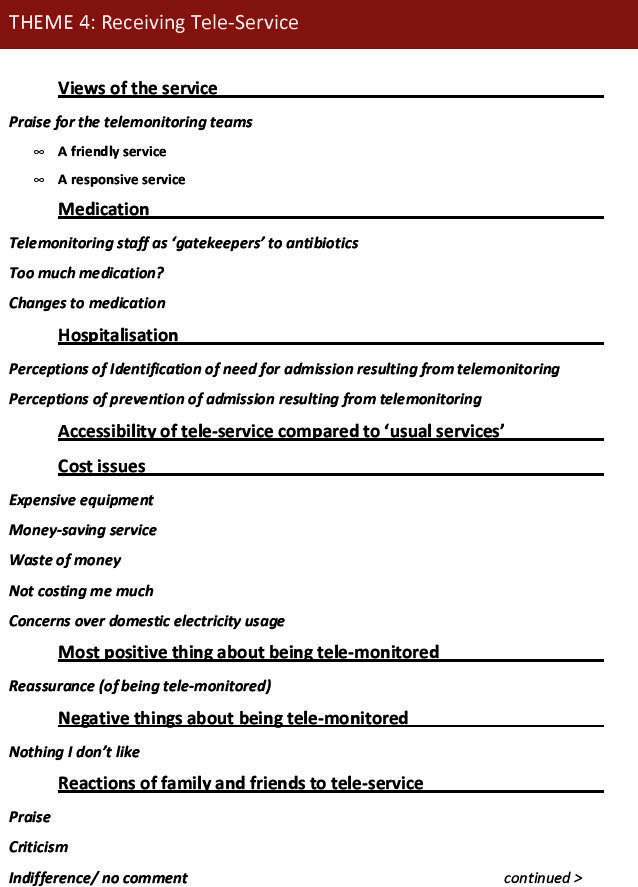
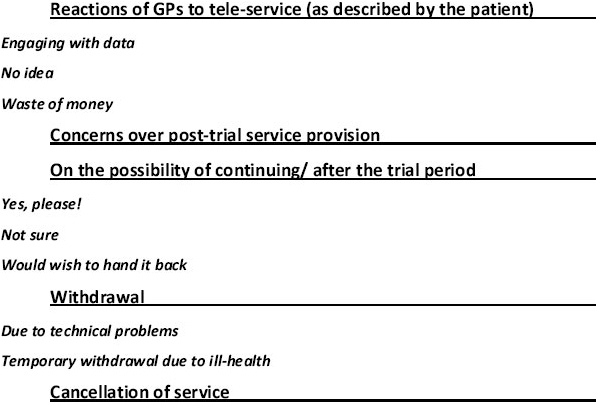
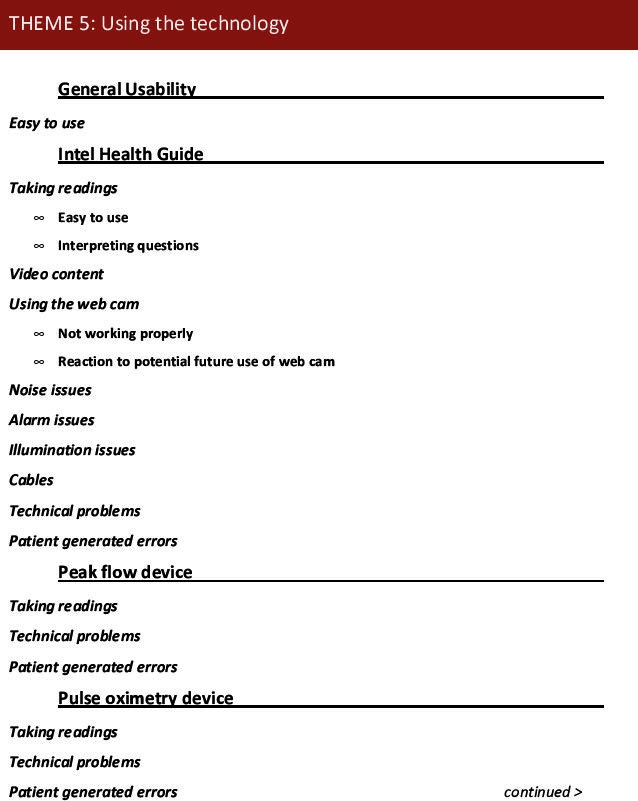
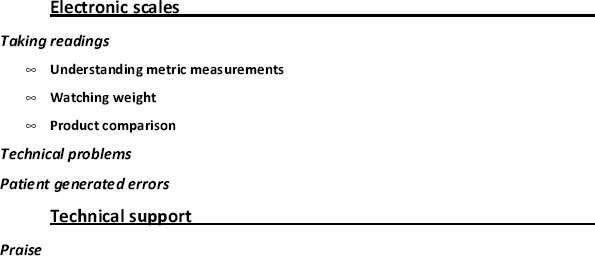
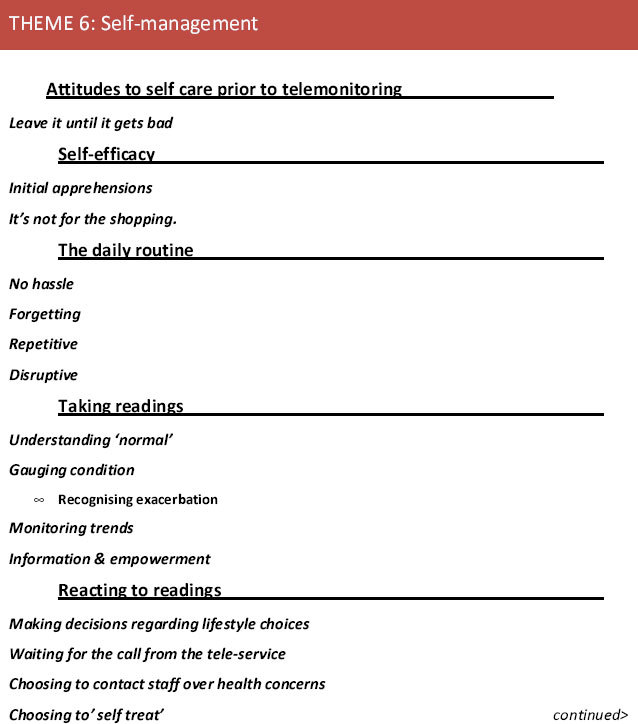
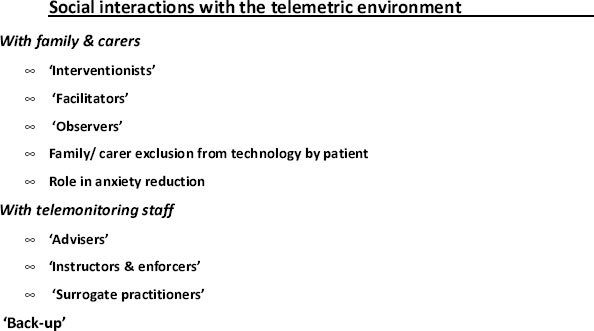
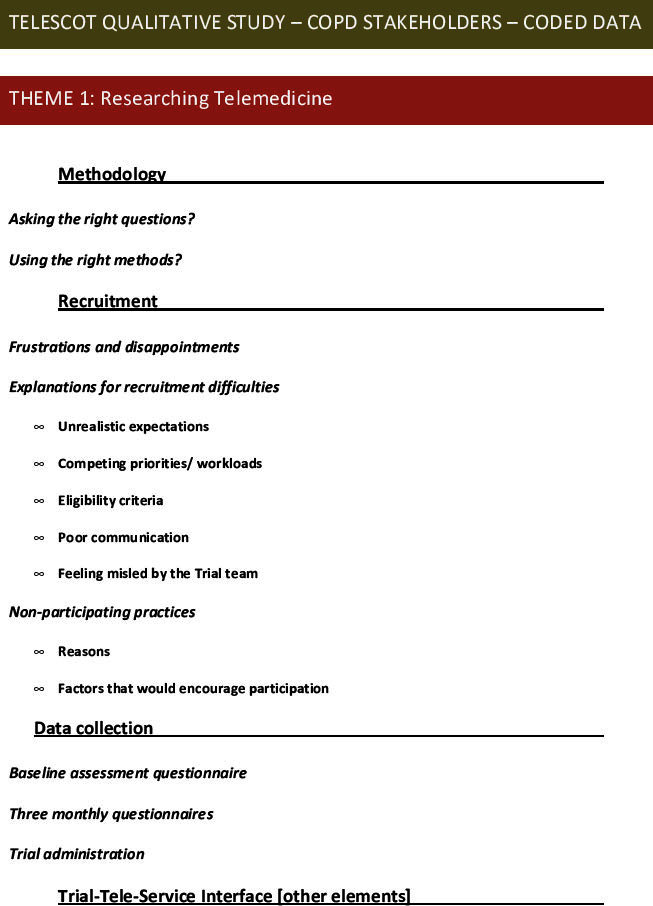
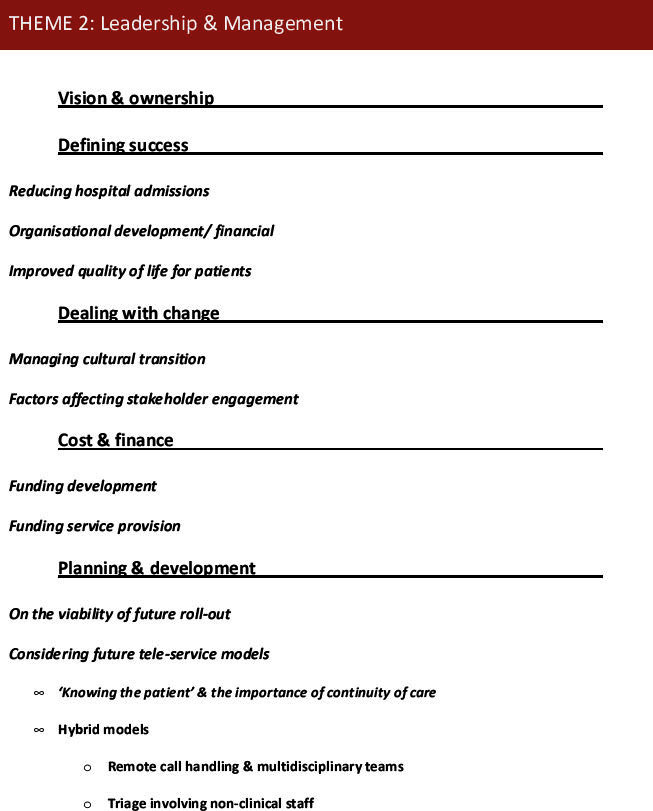
NVivo 7 software was used to assist with initial coding of the transcripts. Interpretation was supported by feedback from interview respondents, a coding review meeting involving TELESCOT colleagues, and multidisciplinary discussion. (The initial coding frames developed for this study are presented in appendices 3 & 4, available online at www.thepcrj.org.)
Results
A total of 38 patients (67% of the 49 patients invited, 47% male, mean age 67.5 years) and 32 healthcare professionals provided 70 interviews. Partners/family members of patients were present and contributed to eight of the interviews. The demographic characteristics of the patient participants are presented in Table 1. The average interview duration was 30 mins.
Table 1. Demographic characteristics of patient respondents.
The findings are presented within the context of four main themes relating to continuity of care: (1) reassurance, accessibility and trust; (2) knowing the patient; (3) discontinuities; and (4) issues of cost and continuity.
Reassurance, accessibility and trust
For many, the telemonitoring service was seen as an improvement to standard care owing to its greater accessibility, the friendly manner in which it was provided, and its responsiveness to individual needs. The service was extremely popular with patients who reported a sense of reassurance in having someone ‘watching over them’.
I think it's very good. It makes you feel like somebody's looking after you. If anything goes wrong, you can get in touch with them any time you want … you've got the confidence that they're going to get something done. I can't fault them anyway. (Male, 79 years)
Relationship continuities between patient and professional within telemetric provision underpinned patient satisfaction. Patients commented favourably on the approachability of the telemonitoring professionals. The frequency of interaction between professional and patient, often triggered by the transmission of telemonitoring data, enabled many patients to get to know their designated telemonitoring professional and form bonds of trust with them. The majority of patients expressed gratitude for the personalised help, advice and support provided by telemonitoring professionals.
I mean these girls [telemonitoring professionals] can't [be] more on the ball … if I need anything at all I've just to phone up … it's a good service … really good, first class. The highlight is I've got somebody feeding back and talking to me. (Male, 69 years)
Patients described the role of the telemonitoring professional as a helpful intermediary between themselves and their GP. Relationship continuities formed between patients and telemonitoring professionals often bridged barriers perceived to exist in usual care. For example, many patients spoke of the involvement of telemonitoring professionals in liaising with GPs to arrange timely appointments, home visits, renegotiation of existing medication regimes, and the provision of anticipatory medicine at home.
I'd say you get better [service] because if [telemonitoring professional's first name] comes on the phone and she'll say “I think you're needing to speak to the doctor”, she's just giving me a warning that she's going to get the doctor to phone me. And they'll either say “Well, I think you're needing to have some antibiotics” or “I think maybe we should pop over and just see you.” (Female, 69 years)
Knowing the patient
Relationship continuities were also important to the professionals. For many practitioners, effective telemonitoring could only be accomplished by ‘getting to know’ the patient.
I think it's probably best if [telemonitoring is done by] people that are dealing with the patients every single day and have that bit of a relationship with them … people are more trusting and it is something a bit more personable for the patient. (Telemonitoring physiotherapist, ID29)
Practitioners considered clinical expertise important in interpreting and contextualising telemonitoring data relative to the individual's ‘normal’ readings over time.
… it's about putting everything into perspective with a COPD patient. It's knowing that somebody may normally have sats [oxygen saturation] of 85, … I think somebody who is an administrator may look at that and panic. It's knowing the baseline and a bit more about the disease … (Nurse, secondary care, ID22)
Discontinuities
While patients and professionals both identified benefits arising from relationship-based continuity of care in telemonitoring, many discontinuities in clinical management relating to telemonitoring provision were also identified.
Coordination and team work
Professionals reported operational difficulties concerning coordination and team work, citing lack of communication between procurement, installation and IT support functions. Practitioners indicated that there was little information sharing between the telemonitoring teams and little awareness of the practices of other telemonitoring colleagues in the management of patients.
[The problem is with] the communication between all the different parties who are involved, because you have IT involved in the installation and you have the company that install it. Then you've got a different person from a totally different background, who works in a totally different area, going in to do the training, and then you have another person monitoring … (Practice administrator involved in telemonitoring, ID7)
Records management and data interoperability
A major problem for many telemonitoring professionals was the lack of interoperability between the (stand-alone) telemonitoring system and existing patient information systems used in primary and secondary care. Many indicated frustration with the limited functionality of the telemetric information systems and the compartmentalisation of data between telemetric and usual care records which prevented information sharing with colleagues in related services. Professionals also commented on the volume of paperwork arising from the case management of telemonitored patients. Some described triplicate data entry in different information systems resulting from ‘non-joined up’ systems.
You spend a lot of time filling in forms to show that you're actually doing something. You're saving time [through telemonitoring] and, by filling the form, you're wasting time. (Telemonitoring professional, ID15)
Cross-boundary working and differences in practice
Professionals were divided on the effectiveness of cross-boundary working between telemonitoring and normal primary care services. While some felt that telemonitoring shifted pressure from hard-pressed GP and hospital services, for others interaction between services proved problematic because clinical roles and responsibilities were not delineated. While some GPs appreciated sharing communication about patients and working in partnership with telemonitoring professionals, others found the involvement of non-medical community-based telemonitoring professionals intrusive, unwelcome and unhelpful.
People have really liked our service … Yes, we've crossed a few boundaries and a few people have thrown their toys out the cot. “I do that, why are you coming and doing that?” I think we've managed it quite well by going “We can all work together”. (Telemonitoring physiotherapist, ID18) … where community teams are involved with our COPD patients, we get a lot more contact, a lot more calls, a lot of those are not appropriate in our eyes. A lot of buck passing. I think potentially that's quite damaging to patient care. (‘Usual care’ GP, ID9)
A number of professionals described sharp contrasts in practice. For example, some GPs and nurses expressed concern over use of anticipatory medication by non-medical telemonitoring professionals. Of particular concern was the perceived over-medication of telemonitored patients. This issue was also reflected by one of the practice-based professionals involved in telemonitoring.
Patients often have two standby courses of treatment in their home … My concern is they then get [repeat] prescriptions for further standby medication. Are professionals aware of how many courses of treatments that individuals are [taking]? (Telemonitoring professional, ID8)
Issues of cost and continuity
While professionals expressed concern about management discontinuities relating to the development and implementation of telemonitoring services, healthcare managers focused on the potential economic benefits of using telemonitoring as a means of driving down service costs. Some considered telemonitoring to be a solution to problems caused by diminishing budgets.
… we're probably going to be operating with 20% less revenue within about four years from now so if ever there was a need to look to technology to support more remote delivery and patient self-management, then [now] is the time … cost efficiency … is crucial … (Manager, ID14)
Managers considered that telemonitoring could deliver cost savings through workload management efficiencies. This was based on the supposition that the cost of the telemonitoring technologies would reduce over time and that service re-engineering would bring considerable cost savings through the centralisation of telemonitoring provision. Managers considered that the development of regional ‘call centre’ hubs would eventually reduce levels of clinician involvement in ‘front line’ service provision.
… how do we minimise some of the heavy clinician input that was put into the service model that we have ended up with? You can send initial triaging of information to a [centralised] non-clinical body who can do that in a much more cost effective way and release the clinician resource to do other things, the things they're meant to do. (Manager, ID23)
Professionals and patients both opposed the vision of centralised regional models of telemonitoring provision. They considered integration of telemetric provision with local practitioner services preferable to centralised ‘call centre’-type provision, emphasising the value of relational continuity over cost benefits associated with centralisation.
I don't know what to make of the fact that people consider sending it to call centres for monitoring … I find that quite extraordinary really because you need to know the patients as a professional to be able to do the monitoring effectively … (Telemonitoring physiotherapist, ID19)
The proposition of the development of some form of regional ‘call centre’-type service reinforced one GP's concerns about telemonitoring. The respondent, from a practice not participating in the trial, considered that the remote telemonitoring of patient data, undertaken outwith the parameters of established practice, compromised patient care.
I think [it's important that] the whole, holistic approach towards patients is not given away … singling out a few values … many kilometres away … in a control room with various remote criteria … but we are not quite sure what that means in the clinical context and how it is perceived by the patient. (‘Usual care’ GP, ID11)
Patients related their experiences of the national telephone healthcare service, NHS24, when asked for their views on the proposition of a centralised model of telemonitoring provision. They spoke of poor service provision and experiences of alleged misdiagnosis. One carer related her hesitancy in seeking assistance from the service at the weekend, outside practice hours:
You're on the phone [to NHS24] for about an hour. Really, it's a joke … I mean at weekends usually if he's taken ill he tried to hang off to the Monday. (Carer, ID1)
Discussion
Main findings
Patients and healthcare professionals considered that relationship-based continuity of care was important in the delivery of telemonitoring services. Managers placed emphasis on improved continuity of clinical management as a means of reducing healthcare costs. However, professionals described many operational challenges arising from the ‘bolting-on’ of telemetric provision to unreconstructed usual care provision which, they claimed, resulted in the proliferation of additional managerial discontinuities.
Strengths and limitations of this study
This research was undertaken as part of a randomised controlled trial evaluating a ‘live’ clinical service as a complex intervention.18 This presented the opportunity to collect the views of patients and professionals at the point of service delivery. A pragmatic approach was taken to data collection and analysis. We strived to obtain a maximum variation sample from the patients and professionals involved in or associated with the telemonitoring service so that the widest range of views could be represented in the research. However, we acknowledge that we may not have encompassed all relevant views.
Similarly, data analysis meetings involving local researchers and healthcare professionals with an interest or involvement in telemonitoring were held to acquire multidisciplinary feedback. Again, we strived for inclusivity of relevant participants at these meetings. Subsequent data recoding and analysis was undertaken to support a balanced interpretation of the data.
The wider technological and service environment has significant bearing on the contextualisation of the research findings. This research has occurred against a backdrop of rapid advances in telemonitoring technology and corresponding NHS service developments. This study, undertaken in one health board region, presents an investigation of the views of patients and professionals on telemonitoring of COPD at an early stage in the development of both the technology and the application of the technology in an operational context. Indeed, the service evolved and changed significantly during the lifetime of the trial as it adapted to suit local services and preferences. This enabled the research to explore the views of a wide range of stakeholders involved in the development and provision of the service. Over time it is envisaged that the emergence of alternative technologies may open new avenues in telemonitoring service provision which may change the perceptions of those involved.
Interpretation of findings in relation to previously published work
Relationship continuity between patient and practitioner is often cited as an important factor affecting patient satisfaction in primary care.19 Patients emphasise the importance of receiving care from a ‘known and trusted’ practitioner.20 A key reason attributed to this preference is the assumed better medical knowledge and understanding by the ‘known practitioner’ of the patient's personal and family background.21 Recent research has indicated that relationship continuity is also important for patients receiving home-based telecare.22
In this study, patients and professionals valued relationship continuity within telemonitoring provision. It is worth noting that many of the patients had no prior professional relationship with the telemonitoring professionals engaged in their care (particularly among those telemonitored by the community respiratory physiotherapists and the community nursing team). However, both patients and professionals reported that trusted patient-practitioner relationships developed quickly over the course of the trial period. Professionals attributed this in part to telemonitoring: the regular checking of telemonitoring data enabled an understanding of the patient's condition which, many professionals considered, would have taken longer to acquire without access to such data. This was thought to support pre-existing professional practices that facilitated relationship continuity, such as home visits and telephone consultations.
Continuity of care is often viewed as ‘seamless care’ involving coordination, teamwork, cross-boundary working, good record systems, and the timely communication of relevant information between care providers and with patients and carers.23 Within the context of the trial service, telemonitoring operated as compartmentalised care, in some cases developed and tested by new community-based teams operating as a supplement to, but outwith, established primary care provision. The role of some groups of telemonitoring professionals as ‘go-between’, facilitating service provision between patients and ‘usual care’ providers, proved something of a double-edged sword. On the one hand, patients greatly appreciated the efforts of telemonitoring professionals to bridge perceived service difficulties in established care provision. On the other, the addition of telemonitoring activities within an unreconstructed usual care arena highlighted many differences in practice. Sometimes this created conflict — not solely because of differences in care provision arising from telemetric versus usual care practices but also due to the contrasting philosophies and perspectives of the professionals operating the services, themselves from a variety of occupational groupings. Therefore, a key challenge faced by those involved in telemonitoring was the management of professional and organisational relationships. Many acknowledged that the decision to operate telemonitoring as an adjunct to usual care (in some cases) added complexity to efforts to achieve and maintain continuity of care.
The organisational approach to care management — notably the management of change — had a significant impact on the continuity of clinical management. In this trial service, change was not instigated by a ‘guiding coalition’24 of professionals wishing to instigate developments in practice or by patients lobbying for different/improved service. The decision to pilot telemonitoring was initiated at the managerial level. The impact of this was that professionals, regardless of the type of service they were providing, often felt that the introduction of telemonitoring was something ‘done to them’, not involving them. The disconnect between the aims and aspirations for the telemonitoring service as formulated by managers and the practical concerns of professionals further exacerbated discontinuities of clinical management. While professionals worked hard to provide a ‘seamless’ service to patients, discontinuities resulting from the initial organisational management of the service left many to query the longer term viability of the service set-up.
May et al. outlined the high failure rate of telemetric services to ‘normalise’ within clinical service provision, stating that many products and services do not last beyond the pilot stage.25 Among the factors affecting implementation and take-up they note the importance of effective translation of technologies into practice by cohesive cooperative groups and stabilisation of telemetric systems through integration of professional knowledge and practice. The results of this study indicate that further work is required in the development of a shared vision of telemonitoring and continuity of care by stakeholder groups, and the integration of both into practice. To paraphrase Guthrie et al., if managers and professionals are serious about the importance of continuity of care, as they claim to be, ‘then they need to ensure that organisational change promotes it.’26
Implications for future research, policy and practice
Major questions challenge the development of both the telemonitoring and ‘continuities’ agendas in primary care. Should future implementation of telemonitoring provision place emphasis on the importance of relationship continuities in implementing safe and effective telemonitoring through localised practitioner-led services? Alternatively, should future development comprise centralised provision potentially enabling minimised practitioner involvement in order to realise economies of scale?
Conclusions
The contrasting views of patients and telemonitoring professionals versus those of healthcare managers, as presented in this research, represent the dichotomy at the heart of current healthcare policy regarding implementation of telemonitoring and its impact on continuities of care. Continuity, but at what cost?
New models of telemonitoring provision (and related practices) are required that both retain the benefits of relationship continuity, as valued by the respondents in this research, in addition to realising managerial and cost reduction benefits from the integration of telemetric technologies into ‘normalised’ practice within the current economic climate.
Acknowledgments
Handling editor Anthony D'Urzo
Statistical review Gopal Netuveli
Funding Chief Scientist Office, Scottish Government Health Directorates, UK. NHS Lothian provided the telemonitoring equipment and the clinical services. HP and BMcK were in receipt of a Primary Care Research Career Award from the Chief Scientist Office of the Scottish Government during the course of the project.
We wish to acknowledge the kindness, support and cooperation of the patients and healthcare professionals who participated in this study. We are grateful to Professor Sir Lewis Richie (chairman), University of Aberdeen; Professor Chris Griffiths, Queen Mary University of London; Professor Anne Louise Kinmonth, University of Cambridge; and Graeme Campbell, Chief Scientist Office, Scottish Government for their advice and support as members of the TELESCOT Independent Trial Steering Committee.
TELESCOT programme team: Professor Brian McKinstry (Programme Lead), Dr Janet Hanley, Jim Forrest, Dr John McKnight, Professor William MacNee, Dr Paul Padfield, Dr Claudia Pagliari, Dr Hilary Pinnock, Professor Aziz Sheikh, Dr Cathie Sudlow, Dr Sarah Wild, Dr Stephanie Lewis (Statistician), Dr Marjon van der Pol (Health Economist), Dr Lucy McCloughan (Programme Manager) and Allison Todd (Trial Manager).
Appendix 1.
Appendix 2.
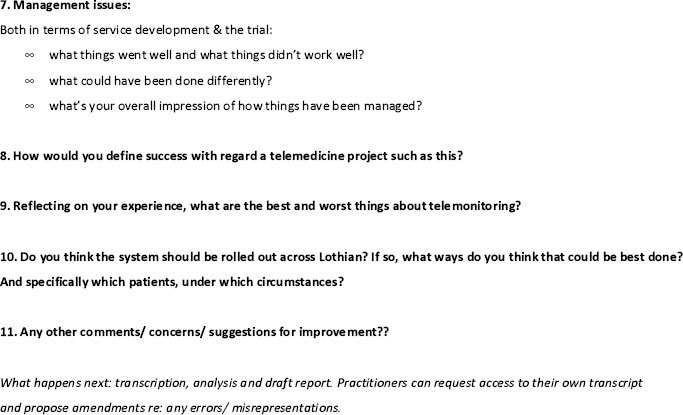
Appendix 3.
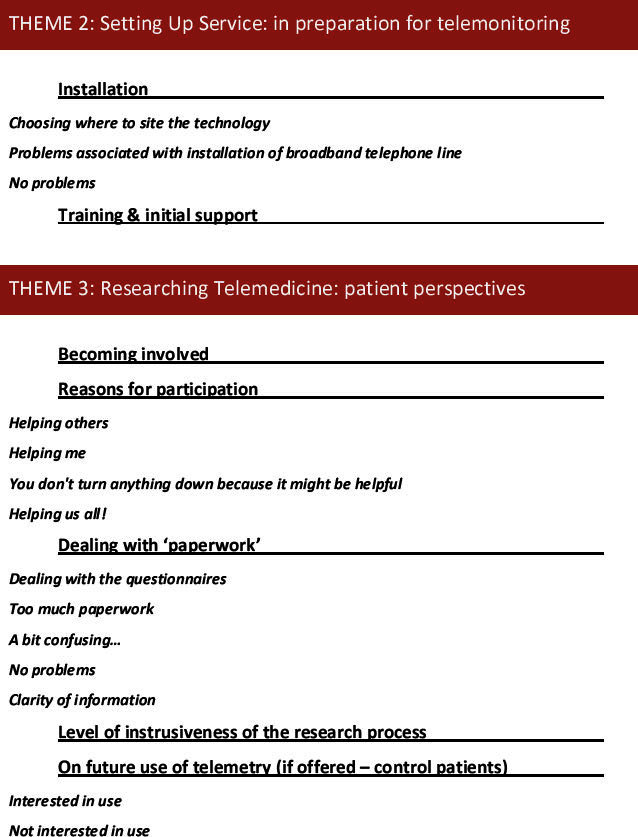
Appendix 4.
Footnotes
AS is Joint Editor-in-Chief, and HP is an Associate Editor, of the PCRJ; neither were involved in the editorial review of, nor the decision to publish, this article. The authors declare that they have no conflicts of interest in relation to this article.
References
- Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE. Continuity of care: a multidisciplinary review. BMJ 2003;327(7425):1219–21. http://dx.doi.org/10.1136/bmj.327.7425.1219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starfield B. Continuous confusion? Editorial. Am J Public Health 1980;70:117–19. http://dx.doi.org/10.2105/AJPH.70.2.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman G, Hughes J. Continuity of care and the patient experience. London: King's Fund, 2010. [Google Scholar]
- Walraven CV, Oake N, Jenning A, Forster MD. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract 2010;16:947–56. http://dx.doi.org/10.1111/j.1365-2753.2009.01235.x [DOI] [PubMed] [Google Scholar]
- Wanless D. Securing our future health: taking a long-term view. London: HM Treasury, 2002. [Google Scholar]
- Scottish Government. Scotland: Better Health, Better Care, 2007. Available from: http://www.scotland.gov.uk/Publications/2007/12/11103453/0 (accessed 14 Feb 2012).
- Scottish Government and Long Term Conditions Alliance Scotland. Scotland: Gaun yersel — the self management strategy for Scotland, 2008. Available from: http://www.ltcas.org.uk/self_man_gaun.html (accessed 14 Feb 2012).
- Goodwin N. The state of telehealth and telecare in the UK: prospects for integrated care. J Integrated Care 2010;18(6):3–10. http://dx.doi.org/10.5042/jic.2010.0646 [Google Scholar]
- Intel. The Intel Health Guide — Overview. Available from: http://www.intel.com/corporate/healthcare/emea/eng/healthguide/index.htm (accessed 14 Feb 2012).
- TELESCOT. Scotland: The impact of a telemetric COPD monitoring service. Available from: http://www.telescot.org/ (accessed 14 Feb 2012).
- Pinnock H, Hanley J, Lewis S, et al. on behalf of the TELESCOT programme group. The impact of a telemetric chronic obstructive pulmonary disease monitoring service: randomised controlled trial with economic evaluation and nested qualitative study. Prim Care Respir J 2009;18(3):233–5. http://dx.doi.org/10.4104/pcrj.2009.00040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scottish Government. Scotland: Scottish Index of Multiple Deprivation. Available from: http://simd.scotland.gov.uk/ (accessed 14 Feb 2012).
- Fletcher CM. The clinical diagnosis of pulmonary emphysema—an experimental study. Proc R Soc Med 1952;45:577–84. [PubMed] [Google Scholar]
- Ure J, Pinnock H, Hanley J, et al. Piloting telemonitoring in COPD: a mixed methods exploration of issues in design and implementation. Prim Care Respir J 2012;12(1):57–64. http://dx.doi.org/10.4104/pcrj.2011.00065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ure J, Kidd G, Tarling A. A qualitative overview of telemetry supported care for COPD patients in the Lothian region. TELESCOT, 2009.
- Hamberg K, Johansson E, Lindgren G, Westman G. Scientific rigour in qualitative research — examples from a study of women's health in family practice. Fam Pract 1994;11:176–81. http://dx.doi.org/10.1093/fampra/11.2.176 [DOI] [PubMed] [Google Scholar]
- Ritchie J, Lewis J, eds. Qualitative research practice: a guide for social science students and researchers. London: Sage Publications, 2003. [Google Scholar]
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. A synthesis of the concept of “continuity of care” in the health and policy literature. BMJ 2003;327:1219–21. http://dx.doi.org/10.1136/bmj.327.7425.1219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker R, Boulton M, Windridge K, Tarrant C, Bankart J, Freeman GK. Interpersonal continuity of care: a cross-sectional survey of primary care patients' preferences and their experiences. Br J Gen Pract 2007;57:283–9. [PMC free article] [PubMed] [Google Scholar]
- Schers H, Webster S, van den Hoogen H, Avery A, Grol R, van den Bosch W. Continuity of care in general practice: a survey of patients' views. Br J Gen Pract 2002;52:459–62. [PMC free article] [PubMed] [Google Scholar]
- Horton K. The use of telecare for people with chronic obstructive pulmonary disease: implications for management. J Nurs Manag 2008;16(2):173–80. http://dx.doi.org/10.1111/j.1365-2834.2008.00845.x [DOI] [PubMed] [Google Scholar]
- Haggerty JL, Pineault R, Beaulieu M-D, et al. Practice features associated with patient-reported accessibility, continuity, and coordination of primary health care. Ann Fam Med 2008;6:116–23. http://dx.doi.org/10.1370/afm.802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotter JP. Leading Change. Harvard Business School Press, 1996. [Google Scholar]
- May C, Harrison R, Finch T, MacFarlane A, Mair F, Wallace P. Understanding the normalization of telemedicine services through qualitative evaluation. JAMIA 2203;10:596–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guthrie B, Wyke S. Controversy in primary care: does continuity in general practice really matter? BMJ 2000;321:734–6. http://dx.doi.org/10.1136/bmj.321.7263.734 [DOI] [PMC free article] [PubMed] [Google Scholar]


