Abstract
Background:
The need to consider anticipatory preventive care for people with chronic obstructive pulmonary disease (COPD) has been highlighted in UK guidelines and policy.
Aims:
To explore stakeholder views of the utility and design of a community-based anticipatory care service (CBACS) for COPD.
Methods:
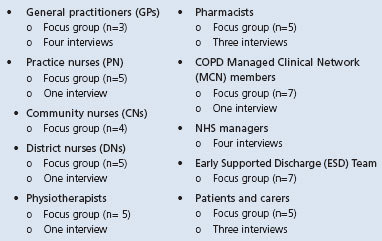
This was a qualitative study using focus groups and in-depth interviews in North-East Scotland. Key stakeholders were purposively sampled: GPs (n=7), practice nurses (n=6), community nurses (n=4), district nurses (n=6), physiotherapists (n=6), pharmacists (n=8), COPD Managed Clinical Network members (n=8), NHS managers (n=4), the COPD Early Supported Discharge (ESD) Team (n=7), patients and carers (n=7). Data were analysed using framework analysis.
Results:
A CBACS for COPD was broadly acceptable to most participants although not all wished direct involvement. Patient education and empowerment, clear roles, effective communication across traditional service boundaries, generic and clinical skills training, ongoing support and a holistic service were seen as crucial. Potential issues included: resources; anticipatory care being in conflict with the ‘reactive’ ethos of NHS care; and the breadth of clinical knowledge required.
Conclusion:
A CBACS for COPD requires additional resources and professionals will need to adapt to a new model of service delivery for which they may not be ready.
Keywords: chronic obstructive pulmonary disease, primary care, qualitative study, anticipatory care
Introduction
Chronic obstructive pulmonary disease (COPD) is a slowly progressive disorder. The largest cost associated with COPD is due to unplanned inpatient hospitalisation resulting from exacerbations,1 which occur with all severities of COPD.2 COPD exacerbations are a principal cause of the pressure on acute hospital beds in winter,3 and have a negative impact on prognosis4–6 and patient quality of life.2 After smoking cessation, preventing exacerbations is the key factor in improving morbidity and mortality for COPD patients.4,7 Thus, the development of an ‘anticipatory care’ service which prevents COPD exacerbations — and hence hospitalisation — could reduce pressure on secondary care services and improve patient outcomes, and enable patients to stay in their own home.8 Evidence supports home care as a cost-effective alternative to hospital care to prevent admissions or support early discharge9–11 but, to the best of our knowledge, there have been no studies of anticipatory interventions targeted at supporting COPD patients before first exacerbation other than those focusing mainly on pulmonary rehabilitation.12 Given suboptimal attendance and high patient drop-out rates from pulmonary rehabilitation,13 it is critical to look at other methods of anticipatory care such as ways to optimise treatment to control symptoms and hence delay or reduce first admissions.
The need for anticipatory preventive care has been highlighted by the British Thoracic Society, who called for studies to investigate the impact of anticipatory care for COPD on hospital admission/readmission, A&E attendance and/or unscheduled GP visits. The Scottish Government Ministerial Task Force (http://www.scotland.gov.uk/Publications/2007/12/11103453/0) has stated the need to pilot, assess, and roll out — if successful — anticipatory approaches to healthcare across Scotland. Applying this to COPD care means more community-based services aimed not only at responding to symptoms but also at health improvement/promotion to prevent exacerbations.13
The development of any new service involves a process of change.14 The importance of people as a source of inertia and a source of leverage for change is highlighted by many models of change and may be particularly significant in the context of healthcare services as influential groups embrace or resist change.15,16 For example, a community-based anticipatory care service (CBACS) for COPD may be perceived as a threat to traditional healthcare provider roles or welcomed as an additional resource; as undermining a particular specialism or an opportunity for professional development.17 Furthermore, the components which need to be addressed to maximise the effectiveness of any new service must be defined.18
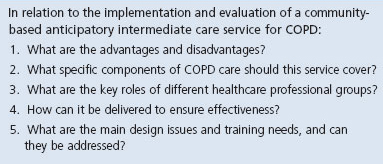
The aim of the current project was to explore attitudes and views of key stakeholders to the utility and design of a CBACS for COPD. The specific research questions are presented in Table 1.
Table 1. Study research questions.
Methods
In the absence of relevant prior research, we selected qualitative methods to explore views on a CBACS for patients with COPD.
Focus groups were selected as these generate data regarding perceptions, values, and beliefs.19,20 Focus groups also ensure that the discussion topics are directed by participants rather than just by the researchers’ agendas.21 Individual interviews were used to target those groups felt to be under-represented in focus group discussions or to accommodate those who preferred an individual interview.
Participants
Participants were selected purposively on the basis of their involvement in delivery or receipt of COPD care. People from each of the following groups of stakeholders were invited to take part: general practitioners (GPs), community, district and practice nurses, community pharmacists, physiotherapists involved in delivering pulmonary rehabilitation, COPD patients and their carers, Community Health Partnerships and other UK National Health Service (NHS) managers, members of the Early Supported Discharge (ESD) team, and members of the Managed Clinical Network for COPD, which included a secondary care consultant, a secondary care manager, and a secondary care Clinical Service Lead (10 focus groups). Invitations and information outlining the background and purpose of the study were sent out via Clinical Specialty Leads, Team Leads, NHS Grampian or, for patients, via pulmonary rehabilitation classes and the local Breathe Easy (patient support) group.
We approached participants working and/or living in three different Community Health Partnerships (which manage community health services in Scotland) covering city and shires (Aberdeen, Aberdeenshire and Moray). Those who expressed interest in taking part were then contacted by the researchers.
Written informed consent for data collection and publication of anonymised data was obtained from all participants.
Data collection
Focus groups and interviews were carried out between October 2009 and July 2010, held at locations convenient to participants (often on their workplace site).
We used the same semi-structured discussion guide for all data collection. Based on our understanding of COPD itself and the literature on implementing new NHS services, we devised questions to stimulate discussion on perceived roles, benefits and concerns, breadth of service, implementation/delivery, main design and training issues involved in setting up a CBACS for COPD (see Table 1). The discussion guide started with an example of a CBACS, so participants were able to understand what they were being asked to discuss (see Appendix 1, available online at www.thepcrj.org).
Analysis
The discussions were audiotaped and transcribed verbatim for analysis using framework analysis.22 Data analysis was inductive (systematic analysis for recurrent themes). Two focus group transcripts were selected for initial analysis and each was analysed independently by two co-applicants who then met with the study researcher to discuss these initial independent analyses and to compare, contrast, and negotiate themes and subthemes. This process led to the development of a full coding framework which was used to code all the transcripts.
Results
Sixty-four people took part with four to eight participants from each group of key stakeholders contributing data (see Table 2). Forty-six people took part in nine focus groups. One focus group was carried out per group of participants other than with NHS managers. Eighteen individual interviews were carried out, four with NHS managers and the remainder supplementing the focus group data from participant groups other than community nurses and the ESD Team.
Table 2. Participant groups and those taking part in focus groups or individual interviews.
Four broad themes were identified: (1) the advantages and disadvantages of a CBACS for COPD; (2) what this service should cover and who should deliver it; (3) main design issues; and (4) training needs.
Advantages and disadvantages
The main advantage of community-based anticipatory care was the potential means of keeping patients with COPD out of hospital or delaying time to first admission. Participants felt that much is known about the natural course of COPD, so deterioration can be anticipated and supports set up:
“Anticipatory care should be highlighting your problem patients and creating a plan for them … or you should be identifying a group at a certain stage and then planning for the next stage.” [Pharmacist Focus Group]
Participants believed that hospitalisation medicalises COPD and takes away patient control, so another advantage of an anticipatory service is that it helps keep patients at home. However, participants were also aware that admission was sometimes entirely appropriate, and the role of a CBACS would then be to support the patient by facilitating timely admission.
Patients would be known to this service, which would provide opportunities for patient education as an ongoing process involving repeating and reinforcing key messages at every opportunity.
“… when I first started this job I used to think, my God, what sort of nurse did you see last time? … But when they come back the following year and you know you showed them and they still can't do it, something implies it's them and not us — never assume anything … that was a real eye opener for me. I genuinely thought these people had not been taught properly.” [Pharmacist Focus Group]
The continuity of care which could be provided by a CBACS was also seen as an advantage. Patients saw this as a means of building up trust and confidence between the patient and services. Professionals saw it as a means of facilitating holistic care, including assessment of social care, as well as healthcare needs:
“You're also able to deal with those issues as well, though, because, in the hospital, you don't know that they've got that cold house or damp house and, even if you did know it, you wouldn't necessarily be able to do anything about it. But when you're working with community you can contact social work or housing and address the issues that are exacerbating the condition.” [Community Nurse Focus Group]
Who should deliver this service?
Assuming the resource was found to set up a new service (see later), a multidisciplinary specialist team was favoured, and each professional group had clear ideas about what they could contribute, from specific tasks to not seeing themselves as directly involved. Views were based not only on existing workload but also on skills level, not seeing a CBACS as their responsibility, and lack of decision-making expertise or experience. Some groups of professionals seemed more empowered than others in terms of discussing potential input to a CBACS. For example, pharmacists and physiotherapists could see clear roles for themselves whereas district and community nurses did not:
GPs believed that their skills level was required in this service, but they did not have time to contribute:
GP1: “Also I suppose there's some sort of, within all the chronic disease, there's just sort of similarity and you know things that need to be covered and a lot of people with COPD may have another chronic disease so you don't want someone going in saying ‘I'm only here for the COPD’, when their sugar is up at 30. No wonder they are short of breath, you know, so someone I suppose with experience with chronic disease management and, as [other speaker] mentioned as well, all chronic diseases are associated with mental health problems and we know that anxiety and stress can bring on symptoms like an exacerbation, so I suppose you need to, you know, be sure that it is an exacerbation — actually an exacerbation — and I think that's always been a wee bit, even when people are admitted you know, it's often like ‘Well there's not much change, we've got them on oxygen but obviously they're going to feel better’. I think you want someone … someone trained, quite skilled.” GP2: “And when you've covered all those bases, the question is: If someone can do all that, then what difference are they from being a GP?” GP1: “Well, because we don't have the time.” GP2: “Well, I know.” [GP Focus Group]
Most patients and carers did not see a role for GPs or, indeed, practice nurses in a CBACS due to perceived lack of time and focus on other matters:
“[GPs] dinna have time … if you're in the doctor's five minutes, you're out. ‥ practice nurses sometimes can be so busy ticking government boxes and guidelines that they don't have time for this sort of thing either.” [Patient Interview 1]
What should this service cover?
The key focus was seen as patient and carer education.
“Yes, I'm much the same, thinking about a huge amount of education, not just for the patient but for the carer … And it's just having that whole process and then giving the patient confidence just to say: ‘I can do this on my own’. Yes. And they'll never do it the first time on their own, they'll have a little blip in and out, but if they can gain their confidence to look after their own condition …” [Physiotherapy Focus Group]
Overwhelmingly, all stakeholders stated that patient and carer education should not just be in terms of knowledge and understanding of COPD and its progression, but also patient and carer empowerment. Reassuring patients that their responses were correct (e.g. contacting the service was the right thing) was seen as empowering patients and reinforcing self-efficacy:
“I think through education you can give someone ownership of their illness, let them take control, and give them the tools to do so.” [ESD Team Focus Group]
Thus, patient education was seen not just as straightforward information-giving. Education and empowerment were also discussed by reference to perceived norms: the general NHS model of care is reactive, but educating and empowering patients is a proactive approach to healthcare. Many participants believed that patients see the UK NHS, particularly doctors, as there to ‘fix’ them, while NHS staff view themselves as ‘fixers’. ‘Fixing’ a problem is less time-consuming in the short term than tackling the problem properly:
“… if you put them into hospital that means that all you have to do is just deal with the admission. You don't actually have to put in the work and the effort to rectify the situation.” [Community Nurse Focus Group]
The other key role of a CBACS for COPD was coordinating services and developing effective systems of communication between the CBACS, practices, secondary care, the out-of-hours (OOH) service and all other healthcare professionals involved in the patient's care (e.g. pharmacists).
“You can have as good care going in on a Monday to Friday basis but sometimes the weekends seem a long time to people and they're calling an out of hours service that doesn't necessarily know what the anticipatory care plan is and they might just admit them. We have to make sure this is communicated.” [District Nurse Focus Group]
Communication and coordination with the OOH service was seen as being the key to effectiveness since many admissions occur out-of-hours, due (at least in part) to doctors not knowing the patients and/or the organisation of the OOH service:
“The other thing is the distance that an out-of-hours doctor has to go. There is no doubt about it, if folk are honest, if you've just travelled 20 miles to a patient and they're on a bit of a … will I admit them or won't I admit them, seesaw, you … if you're really honest, I would think that if there's a chance that you might well be called back there in three hours’ time because they've gone off and are worse, you're going to end up admitting them. But you've already been travelling 30, 40 miles; I would suspect that the threshold for admitting them on the first visit is an awful lot lower than if you just had to go round a corner. And I'm quite sure there's quite a few patients admitted … I wouldn't say unnecessarily, but maybe a bit quicker than they should have been.” [GP Interview 2]
Main design issues and training needs
The main barrier to implementing this service was limited resources: no professional group considered that it was possible to deliver a new service without additional resources as people are already fully committed to existing service delivery and ‘fire fighting’:
“Well, do you know what, congratulations, you can now do anticipatory care for our COPD patients [on top of your existing work] — that's a no go.” [Pharmacist Focus Group]
Participants discussed other aspects of service design to maximise effectiveness. CBACS team members must have power to take decisions regarding the admission of patients into hospital versus supporting them at home, arranging social care assessment, and referring them on to existing services. Setting up the service so patients had a named contact, preferably a nurse — with the rationale that patients are more likely to contact someone they know and are more likely to contact a nurse than a doctor — was favoured:
“I think certainly the older population, you know, the doctor's a very important man and I'll stick with this as long as I possibly can [before getting in contact].” [Physiotherapist Focus Group]
The capacity to carry out home visits was considered essential, as this enabled assessment of social care needs as well as healthcare needs, echoing the belief that a CBACS should have a holistic focus (see earlier). However, discussions also acknowledged the need to bring patients into centres/practices if at all possible to maintain patient independence.
“And sometimes we've thought, well, would it not make more sense if we put on transport, if GP surgeries could provide transport to bring patients to the surgery for, say, a clinic, that might save the burden of the patient going to the hospital because a lot of our patients if they can't come to the surgery, would just go, default to going to the hospital, because they can get transport, and it might actually be more cost effective to have transport going down to the surgery. [Manager Interview]
Referral to the CBACS should be straightforward, rapid, and not limited to a narrow range of professional groups. Existing systems can — and indeed should — be used to identify suitable patients (e.g. flagging up patients who do not attend for review or spirometry data):
“You would know by audit and, you know, how many people were, you know, going into … were ending up having to go into hospital or were having to have, you know, have, you know, call outs or GP visits.” [Practice Nurse Interview] “I think anticipatory care can only be in people that we know have COPD … I think that's a very important feature because otherwise you'll get in a mess. You'll have people you think have got COPD and they don't, and they die of a heart attack or something.” [Chest Clinic Consultant]
Most professional groups viewed a geographical service as most appropriate due, in part, to the relatively low numbers of COPD patients outside the main population centres.
Finally, the key role for the CBACS of coordinating services and communicating across traditional boundaries, and educating patients and carers, raised generic training needs (e.g. communication skills) as well as the need for clinical knowledge and skills. With training, most participants believed that different healthcare professionals would be able to deliver this service as part of a multidisciplinary team, although GP or hospital specialist back-up for the team was seen as potentially useful. As presented earlier, GPs felt their level of skills and knowledge was required due to the often complex clinical needs of COPD patients with multiple co-morbidities and, as a result, they seemed unsure of the ability of other healthcare professionals to lead a CBACS.
Discussion
Main findings
The findings from this study indicate that a CBACS for COPD was broadly acceptable to most key stakeholders. The key benefits of this service were seen to be reducing hospitalisation, educating patients in self-management in order to improve self-care and reduce acute admissions, and coordination of health and social care. The CBACS was viewed as engaging directly with existing services, particularly secondary care services, in order to facilitate admission where required. However, the challenge of which professional groups would contribute to this service stimulated discussion and highlighted a range of practical issues. Additional resources were seen as essential, as was the need for CBACS team members to have a broad level of skills and knowledge — both generic skills (e.g. communication skills, problem-solving) and clinical skills/knowledge. This was associated with co-morbidities and complications common to COPD (e.g. congestive heart failure, diabetes23); healthcare professionals in any COPD service need a broad understanding of these to provide holistic and appropriate care. Some participants felt that, due to the wide medical knowledge required, such a service had to be led by medically trained staff.
Barriers to implementing such an anticipatory service — other than limited existing resources — focused on the need to change patient and provider attitudes and to change approaches towards chronic disease management within the NHS from reactive to proactive. Some professional groups (GPs, practice nurses, community nurses) did not wish to embrace this as an opportunity for professional development, not because they did not see themselves as appropriate professionals but because they had no capacity for additional clinical, managerial, or organisational responsibilities. This was also acknowledged by patients. Physiotherapists and community pharmacists could see clear roles for themselves in the favoured model of a specialist community-based team.
Strengths and limitations of this study
The main strength of the study is the range of participants, representing all professional groups involved in COPD care. However, our focus on the views of community-based practitioners meant the involvement of only a few participants from secondary care; it might have been useful to have gathered more data from this group. The focus groups were organised by professional group, and differing opinions may not have been reported due to peer pressure stifling minority views. Our sampling procedure means we have no data on those who did not participate. We triangulated the interview and focus group data where applicable and found them to be very similar. Our study was undertaken within one geographical area of the UK, so our findings may not be wholly representative of views and attitudes in other areas where existing respiratory services may be more or less developed. However, by focusing in one geographical area, we were able to gain multiple perspectives on the potential contribution of a CBACS. The process of data collection was iterative so points considered important by one group were included in the discussion guide, and hence data analysis, for further groups and interviews.
Interpretation of findings in relation to previously published work
The critical design features of a CBACS discussed by participants reflected key components of other successful interventions with COPD patients (e.g. named contacts, home visits, ongoing support, 24 hour access).8,10,11,14,24 The need for trusted professionals supporting self-care and coordinating services resonates strongly with work exploring the boundary between self-care and professional care.25 Other design issues reflect traditional service delivery boundaries in the UK setting (e.g. ‘stand-alone’ out-of-hours services, channels of communication). These echo the UK government's desire to develop team-working across traditional agency boundaries26 and resonate with work highlighting the need for multidisciplinary team-working in designing new respiratory services.27 The views of participants on the essential features of a CBACS dovetail with those identified by Peytremann-Bridevaux et al.28 as a prerequisite for successful chronic disease management programmes — namely, multifaceted, educational (including follow-up), and multiprofessional.
Patient education was seen as the cornerstone of a CBACS. Healthcare provider education, in terms of changing attitudes and approaches towards chronic disease management within the NHS, was also discussed widely. However, specific ideas for how these goals could be achieved were not explored.29,30
Implications for future research, policy and practice
While supportive of the service development, community nurses did not wish to be directly involved, in misalignment with the Scottish Government's proposals of extended community nursing roles including coordinating services and anticipatory care.31 General practitioners also did not support the development of a CBACS, possibly due to concerns about yet another extended role proposed for other healthcare professionals about whose capabilities they doubt32 and/or their acknowledgement of the complex nature of COPD care due to co-morbidities and their impact on outcomes. Their views need to be explored further. These findings suggest that a substantial process of change is required before new ways of working in clinical practice will be fully embraced. The study data will underpin the design and implementation of a CBACS for COPD to assess feasibility, effectiveness, and cost-effectiveness.
Conclusions
The development of a CBACS for COPD involves a substantial process of change. Many of the concerns expressed by our participants reflect the anxiety engendered by the ‘unfreeze’ phase of transitional change16 as professionals are forced to question the value of their traditional service in the light of an evolving context, identify those components that will contribute to the new service (and by implication discard those that do not), and develop new skills that can enhance their role. A prerequisite of successful transition involves understanding the issues from the perspective of all the stakeholders, as shown in the current study.
Acknowledgments
Handling editor Arnulf Langhammer
Funding This study was funded by the Chief Scientist's Office, Scottish Executive (CZG/2/365).
Ethics approval Ethics approval for the study was given by the North of Scotland Research Ethics Committee (09/S0802/55).
The authors thank those who took part in the study and the researchers who helped with data collection. They also thank Dr Pauline Strachan for her support in the early stages of the project and Dr Hilary Pinnock for her valuable comments on earlier versions of the manuscript.
Appendix 1. Focus group and interview schedule
Can a community-based intermediate care service reduce exacerbations and prevent hospitalisations in COPD patients?
Welcome
Welcome and thank you for volunteering for this study
You have been asked because your point of view is important
We appreciate your time in helping with this study
Introduction/Scene setting
My name is … and I am a …
The purpose of this discussion is to determine your opinions about how a community-based intermediate care service could reduce exacerbations and prevent hospitalisations in COPD patients
This study is being funded by a small grant from the Chief Scientist's Office
Anonymity
Despite being recorded, I would like to assure you that the discussion will be anonymous
After the discussion, the recordings will be transcribed from digital memory card to paper
During this, you will be assigned a false name. You will therefore remain anonymous
The memory cards will be kept safely in a locked drawer and will be kept in accordance with research governance policies
I would appreciate it if you would refrain from discussing the comments of other group members outside the focus group
Ground rules
The most important rule is that only one person speaks at a time. There may be a temptation to jump in when someone is talking but please wait until they have finished. Valuable material can be lost on the tape recording if several people talk at the same time
There are no right or wrong answers
You do not have to speak in any particular order
When you do have something to say, please do so. There are many of you in the group and it is important that everyone has the chance to contribute
You do not have to agree with the views of other people in the group
Finally, because of limited time, I may need to re-direct our discussion with a few questions
Does anyone have any questions?
OK, let's begin
Introductory questions
What do you understand by the term anticipatory care? (Encourage broad discussion of this introductory question)
Present the following background information to focus group participants
In COPD, preventing exacerbations is the single key factor that improves morbidity and mortality. You may be most familiar with Early Supported Discharge (ESD) services for people with COPD (explanation of local service provided if required by participants). There is a good evidence base for ESD, but what is important for this discussion is that ESD can only be accessed by patients who have had an exacerbation which has resulted in hospitalisation
Responding after first intervention may help increase the time to next exacerbation, but it is a bit like locking the stable door after the horse has bolted. Some other studies have intervened with COPD patients who have been considered for admission as well as those already hospitalised, but there is no work to date in COPD which assesses the effectiveness of not only responding to symptoms and exacerbations but also addressing health improvement/promotion and preventing exacerbations in the first place.
You may know already that the Scottish Government Ministerial Task Force has stated the need to pilot, assess and roll out, if successful, anticipatory approaches to healthcare across Scotland, working in partnership with Community Health Partnerships, to tackle local health priorities with groups including patients with long-term conditions such as COPD. The need for anticipatory preventive care (i.e. to delay or reduce first admissions) has also been highlighted by the British Thoracic Society Guideline Development Group, who have called for studies to investigate the impact of anticipatory preventive care on hospital admission/readmission, A&E attendance and/or unscheduled GP visits.
We are interested in your views of what a community-based anticipatory care intervention for COPD would look like. To help with this discussion, we have developed an example of one such intervention. We would like to explore your views on this proposed intervention.
Example: Anticipatory Care Intervention
There are three points of entry of patients into the intervention: (1) already on the practice COPD register; (2) newly diagnosed with COPD; and (3) patients in hospital who have been assessed as suitable for Early Supported Discharge.
The cornerstone of the intervention is patient education so, on entry to the intervention, the patient completes a self-assessment knowledge questionnaire which is revisited annually or after trigger for review (e.g. an exacerbation leading to admission). The Anticipatory Care Plan also includes details of likely reasons for admission (where relevant), the Care Manager's contact details, date of last review, significant information that will help with decision-making (e.g. non-weight bearing, isolated location), brief history, medication, GP contact details, and so on.
The Healthcare Community Team (HCCT) identifies the most appropriate member of the team to act as the Case Manager. The Case Manager is either the District Nurse or the GP where the patient's issues are predominantly health. Where the issues are primarily social, this will be the Care Manager or Home Care Supervisor. In the absence of a Single Shared Assessment (SSA), the Case Manager will instigate this.
The focus of the Anticipatory Care Plan is to enable the patient to stay at home or as close to home as possible, and to determine how they can work with their GP and HCCT to maintain or improve their health. Family and carers are encouraged to be involved in meetings between the patient and Care Manager.
The Anticipatory Care Plan focuses on self-care, initiating or increasing community care (social or healthcare partnership is key to the intervention), care within a community facility (hospital or care/nursing home), or admission to an acute hospital. Draft plans are taken to the Practice Team for discussion and agreement.
Once finalised and signed off by the Practice Team and patient, copies of the Anticipatory Care Plan are placed in the patient notes, the yellow folder if the patient has a SSA, and faxed to the out-of-hours service. Where the patient does not have a SSA, a copy of the Anticipatory Care Plan will be kept in the patient's house using the ‘Message in a bottle’ system.
Questions for discussion
What are the advantages and disadvantages of this intervention?
Does it cover all the necessary specific components of COPD care? Are there any design issues, and can they be addressed?
Is the format of delivery such to ensure effectiveness? Is there a role for telemedicine in the proposal intervention?
What factors might help/hinder the set-up of such a community-based anticipatory care intervention for COPD? This question should be broken down to ensure participants discuss environmental constraints such as time, timing, feeling isolated from colleagues, as well as any practical constraints such as any perceived difficulties carrying out home visits.
How difficult or easy would it be for this service to be successful? Would there be any potential pressures or barriers? Are the key roles of different healthcare professional groups appropriate? Would role boundaries be an issue?
What skills and knowledge do you think the people delivering this service would need? On the whole, and to the best of your knowledge, do they possess these skills and knowledge or would they need training/support? If so, what training/support would be most useful?
Would any individual characteristics be important for implementing and delivering this intervention?
What other pathways or procedures, if any, would need to be set in place to ensure and evaluate the effectiveness of the proposed intervention?
Summary
Provide participants with a summary of the discussion so far and ask participants for their feedback on the summary and whether there is anything they would like to add.
Concluding question
Of all the things we've discussed today, what would you say are the most important issues?
Conclusion
Thank you for participating
This has been a very successful discussion
Your opinions will be a valuable asset to the study
We hope you have found the discussion interesting
I would like to remind you that any comments featuring in this report will be anonymous
Footnotes
The authors declare that they have no conflicts of interest in relation to this article.
References
- Wouters EF. Economic analysis of the Confronting COPD survey: an overview of results. Respir Med 2003;97(Suppl C):S3–14. http://dx.doi.org/10.1016/S0954-6111(03)80020-3 [DOI] [PubMed] [Google Scholar]
- O'Reilly JF, Williams AE, Rice L. Health status impairment and costs associated with COPD exacerbation managed in hospital. Int J Clin Pract 2007;61:1112–20. http://dx.doi.org/10.1111/j.1742-1241.2007.01424.x [DOI] [PubMed] [Google Scholar]
- Damiani M, Dixon J. Managing the pressure: emergency hospital admissions in London, 1997-2001. 2002. Publisher?
- Donaldson GC, Seemungal TAR, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2002;57:847–52. http://dx.doi.org/10.1136/thorax.57.10.847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seemungal TAR, Donaldson GC, Bhowmik A, Jeffries DJ, Wedzicha WA. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2000;161:1608–13. [DOI] [PubMed] [Google Scholar]
- Seemungal TAR, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;157:1418–22. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence (NICE). Chronic pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. London: NICE, 2004. [Google Scholar]
- Sheppard S, Harwood D, Jenkinson C, Gray A, Vessey M, Morgan P. Randomised controlled trial comparing hospital at home care with inpatient care. 1: Three month follow up of health outcomes. BMJ 1998;316:1786–91. http://dx.doi.org/10.1136/bmj.316.7147.1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram FS, Wedzicha JA, Wright J, Greenstone M. Hospital at home for patients with acute exacerbations of chronic obstructive pulmonary disease: systematic review of the evidence. BMJ 2004;329:315–19. http://dx.doi.org/10.1136/bmj.38159.650347.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skwarska E, Cohen G, Skwarski KM, et al. Randomized controlled trial of supported discharge in patients with exacerbations of chronic obstructive pulmonary disease. Thorax 2000;55:907–12. http://dx.doi.org/10.1136/thorax.55.11.907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourbeau J, Julien M, Maltais F, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Arch Intern Med 2003;163:585–91. http://dx.doi.org/10.1001/archinte.163.5.585 [DOI] [PubMed] [Google Scholar]
- Effing T, Monninkhof EEM, van der Valk PPDLPM, et al. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No: CD002990. http://dx.doi.org/10.1002/14651858.CD002990.pub2 [DOI] [PubMed]
- Fischer MJ, Scharloo M, Abbink JJ, et al. Dropout an attendance in pulmonary rehabilitation: the role of clinical and psychosocial variables. Respir Med 2009;103:1564–71. http://dx.doi.org/10.1016/j.rmed.2008.11.020 [DOI] [PubMed] [Google Scholar]
- Smith BJ. Chronic obstructive pulmonary disease management trials, including coordinated care, outreach nusing, and other attempted care innovations. Respir Med: COPD Update 2006;2:60–3. http://dx.doi.org/10.1016/jTmedu.2006.07.002 [Google Scholar]
- Iles V, Sutherland K. Organisational change: a review for health care managers, professionals and researchers. London: National Co-ordinating Centre for NHS Service Delivery and Organisation (NCCSDO), 2001. [Google Scholar]
- Clark L. The essence of change. Hemel Hempstead: Prentice Hall, 1994. [Google Scholar]
- Moffat MA, Sheikh A, Price DB, et al. Can a GP be a generalist and a speclialist? Stakeholder views on a respiratory general practitioner with a special interest service in the UK. BMC Health Services Res 2006;6:62. http://dx.doi.org/10.1186/1472-6963-6-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig N, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzinger J. Focus groups with users and providers of health care. In: Pope C, Mays N, eds. Qualitative research in health care. 2nd ed. London: BMJ, 2002. [Google Scholar]
- Farquhar C. Are focus groups suitable for “sensitive” topics? In: Barbour R, Kitzinger J, eds. Developing focus group research: Politics, theory, and practice. London: Sage, 1999: p.47–63. [Google Scholar]
- Stringer E. Action research in education. Upper Saddle River, NJ: Pearson Education, 2004. [Google Scholar]
- Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess R, eds. Analysing qualitative data. London: Routledge 1994: p.173–94. http://dx.doi.org/10.4324/9780203413081_chapter_9 [Google Scholar]
- Rice KL, Dewan N, Bloomfield HE, et al. Disease management progam for chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2010;182:890–6. http://dx.doi.org/10.1164/rccm.200910-1579OC [DOI] [PubMed] [Google Scholar]
- Ram FSF, Jones A, Fay JK. Primary care based clinics for asthma (Cochrane review). In: The Cochrane Library, Issue 2, 2004. [DOI] [PubMed]
- Kielmann T, Huby G, Powell A, Sheikh A, Price DW, Pinnock H. From support to boundary: a qualitative study of the border between self care and professional care. Patient Educ Counsel 2010;79:55–61. http://dx.doi.org/10.1016/j.pec.2009.07.015 [DOI] [PubMed] [Google Scholar]
- Department of Health. Working across boundaries. 9 Feb 2007.
- Pinnock H, Huby G, Tierney A, et al. Is multi-disciplinary teamwork the key? A qualitative study of the development of respiratory services in the UK. J R Soc Med 2009;102:378–90. http://dx.doi.org/10.1258/jrsm.2009.080356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peytremann-Bridevaux I, Staeger P, Bridevaux PO, Ghali WA, Burnand B. Effectiveness of chronic obstructive pulmonary disease-management programs: systematic review and meta-analysis. Am J Med 2008;121:433–43. http://dx.doi.org/10.1016/j.amjmed.2008.02.009 [DOI] [PubMed] [Google Scholar]
- Hardeman W, Johnston M, Johnston DW, Bonetti D, Wareham NJ, Kinmonth AL. Application of the theory of planned behaviour in behaviour change interventions: a systematic review. Psychol Health 2002;17:123–58. http://dx.doi.org/10.1080/08870440290013644a [Google Scholar]
- Michie S, Johnston M. Changing clinical behaviour by making guidelines specific. BMJ 2004;328:343–5. http://dx.doi.org/10.1136/bmj.328.7435.343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scottish Executive. Visible, accessible and integrated care: Report of the review of nursing in the community in Scotland. 2006.
- Wilson A, Pearson D, Hassey A. Barriers to developing the nurse practitioner role in primary care — the GP perspective. Fam Pract 2002;19:641–6. http://dx.doi.org/10.1093/fampra/19.6.641 [DOI] [PubMed] [Google Scholar]


