Abstract
Background:
Applying guidelines is a universal challenge that is often not met. Intelligent software systems that facilitate real-time management during a clinical interaction may offer a solution.
Aims:
To determine if the use of a computer-guided consultation that facilitates the National Institute for Health and Clinical Excellence-based chronic obstructive pulmonary disease (COPD) guidance and prompts clinical decision-making is feasible in primary care and to assess its impact on diagnosis and management in reviews of COPD patients.
Methods:
Practice nurses, one-third of whom had no specific respiratory training, undertook a computer-guided review in the usual consulting room setting using a laptop computer with the screen visible to them and to the patient. A total of 293 patients (mean (SD) age 69.7 (10.1) years, 163 (55.6%) male) with a diagnosis of COPD were randomly selected from GP databases in 16 practices and assessed.
Results:
Of 236 patients who had spirometry, 45 (19%) did not have airflow obstruction and the guided clinical history changed the primary diagnosis from COPD in a further 24 patients. In the 191 patients with confirmed COPD, the consultations prompted management changes including 169 recommendations for altered prescribing of inhalers (addition or discontinuation, inhaler dose or device). In addition, 47% of the 55 current smokers were referred for smoking cessation support, 12 (6%) for oxygen assessment, and 47 (24%) for pulmonary rehabilitation.
Conclusions:
Computer-guided consultations are practicable in general practice. Primary care COPD databases were confirmed to contain a significant proportion of incorrectly assigned patients. They resulted in interventions and the rationalisation of prescribing in line with recommendations. Only in 22 (12%) of those fully assessed was no management change suggested. The introduction of a computer-guided consultation offers the prospect of comprehensive guideline quality management.
Keywords: computer, COPD, diagnosis, guideline, management, primary care
Introduction
Chronic obstructive pulmonary disease (COPD) poses an immense challenge to healthcare systems and health resources, not least in the UK where it is estimated that there are more than three million people living with COPD.1,2 Optimising chronic disease management is central to health strategy in the UK and is a core component of the General Medical Services (GMS) contract.3,4 Primary care is expected to provide most of the chronic disease management which requires patients to be identified on a disease register, but current GP databases may not be accurate.5 Much chronic disease management is undertaken through nurse-based review, yet most practice nurses have not received the necessary specialty training.6
A national audit has confirmed that many of the proven National Institute for Health and Clinical Excellence (NICE) guideline1 interventions such as pulmonary rehabilitation and inhaled medications that alter health outcomes and patient quality of life are not reaching patients.7 COPD is a priority issue for the health service with a published outcomes strategy.8 Key components of the strategy include optimisation of care, which must be tailored to the individual, and thorough follow-up of patients. It is envisaged that the GMS contract will evolve through the Quality Outcomes Framework (QOF) mechanism which will be aligned to the published NICE quality outcomes, encouraging implementation and driving COPD management and services.9
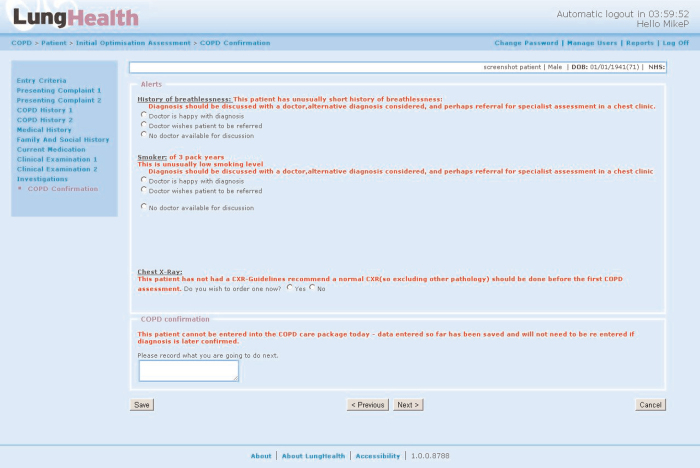
We have developed a guideline-based computer-guided consultation designed to facilitate COPD management. The COPD software application enables management by incorporating algorithms, based on the NICE guidance, that prompt the clinician throughout the review. This facilitates diagnostic confirmation and prompts — but does not make — clinical decisions or actions. The system uses the medical model and forms an electronic consultation. Unlike a simple electronic case sheet, the embedded algorithms guide the consultation, aiding the clinician diagnostically and with management options (see Boxes 1 and 2). The intelligent software stratifies the interventions after disease confirmation and prompts the clinician to consider 11 areas of guideline-based management. In those patients with normal or restrictive spirometry or if the clinical history raises another issue or diagnosis, review by an appropriate diagnostician (either the GP or a specialist physician) is prompted.
Software features.
Electronic consultation using the medical model guides a purposeful history to support accurate diagnoses
Creates a standardised electronic record of their condition that can be used for future care, both elective and acute.
Does not make decisions: the embedded algorithms prompt clinicians towards NICE guideline-based interventions and therapy
Data gathered form a population database
Database created is fully password-protected and can be based on a local NHS server or on the NHS N3 network
Caldicott principles can therefore easily be maintained
Can be customised to use local formularies as priorities while not excluding individual management
Embedded software algorithms.
Guided history, examination and investigation
Diagnosis: challenge and confirmation
Spirometry interpretation
Pharmacological interventions
Inhaler technique check and correct
Pulmonary rehabilitation
Oxygen assessment
Vaccinations
Smoking cessation
Self-management plan
Exacerbation management
All data are recorded and appropriate reminder prompts repeated at subsequent consultations. This removes the necessity constantly to refer to guidelines as they are embedded. It also promotes quality since the consultation progresses only after key clinical issues are addressed.
We have piloted this approach to determine (1) whether a guideline-based computer-guided consultation is a practical way of standardising assessments; (2) whether it can be used by practice nurses (with or without specific COPD training); and (3) the number of patients in whom changes in their diagnosis and/or management were made.
Methods
Patients
We performed an optimisation review on 293 patients randomly drawn from the COPD registers of 16 practices in three primary care organisations (PCOs). Practices were selected to give a cross-section of urban, semi-rural, and rural locations. The work was discussed with the local ethics committee who indicated that they regarded this as a service development and that ethics approval was not required. Nevertheless, at the beginning of each consultation the patients were invited to take part and gave consent to the use of the system, to their records being held electronically and their data being used anonymously for reports. Patients who were due for routine COPD review were invited to take part in the guided consultation, so consecutive patients who attended were interviewed. No patient who attended declined to take part in the consultation. The only difference was that 45-min appointment slots were apportioned. This length was required because 15 mins of the time was allotted to performing spirometry to accredited standards and to allow a clinical examination.
Study design
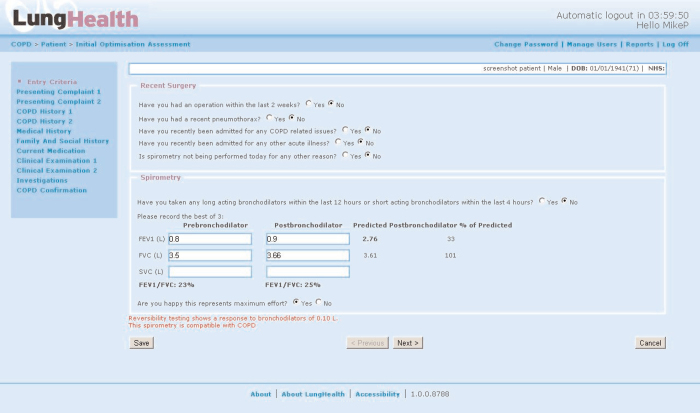
Eighteen nurses in the 16 practices (maximum of two in any one practice) undertook the consultations with the laptop screen visible to them and the patient using computer-guided consultation software (Figures 1 and 2). Whenever possible, spirometry was performed as part of the consultation. Changes to the primary diagnosis and recommendations for management interventions were recorded. The time required to train in the use of the software was also noted. One-third of the practice nurses had no specific respiratory training; this group was asked to comment on the system and how long they felt was needed to be competent in using it.
Figure 1.
Screen shot spirometry screen
Figure 2.
Screen shot diagnostic confirmation screen
Results
No consultation took longer than the allotted 45 mins. The mean (SD) age of the 293 patients assessed was 69.7 (10.1) years and 163 (55.6%) were male. Thirty-two patients (11%) had never smoked. In 57 patients no spirometry was obtained: two patients declined, in five patients it was contraindicated appropriately (two with recent eye surgery, three with chest injuries), and in 50 cases it was not performed for a variety of reasons (25 with a recent exacerbation, two with aneurysm, three failed blows, eight deferred for cardiac reasons (n=4) or asthma assessment (n=4), and in four cases no reason was given for not performing spirometry). The decision whether or not to perform spirometry on the day was at the discretion of the nurse.
A full assessment using the computer-guided consultation was completed in 236 patients (Table 1). Of these, the primary diagnosis was revised in 69 (29%). Thirty patients had normal spirometry, 15 had restrictive function, and 24 with obstructive spirometry were referred for other assessments based on the prompted clinical history (asthma (n=12), cardiac problems (n=10), bronchiectasis (n=2)). A total of 191 patients were confirmed as having COPD and appropriately classified into COPD severity groups based on forced expiratory volume in 1 second percent predicted. In 88% of these cases drawn from the COPD register the consultation prompted additional management recommendations, pharmacological and non-pharmacological. In those with mild or moderate COPD (n=130) the recommendations included the addition of a short-acting bronchodilator in four patients (2%), a long-acting bronchodilator (either an anti-muscarinic (LAMA) or a beta-agonist (LABA)) in 35 patients (27%), and a long-acting beta-agonist/inhaled corticosteroid combination (LABA/ICS) in three (2%). In 56 patients the recommendation was to discontinue various inhaled medications and in 42 patients (32%) these were LABA/ICS combinations. In those with severe and very severe COPD (n=61) the recommendations were for addition of a long-acting bronchodilator in 17 patients (29%) and a LABA/ICS combination in 19 (31%). No reductions were recommended, but correction of the drug dose and/or device occurred in 23 patients (38%), 10 of whom needed to be switched to a dry powder device. In addition, 27 (47%) of the 55 patients who were smokers accepted referral for smoking cessation support. Twelve patients (6%) with hypoxia (SaO2 <92% on air) had an oxygen assessment arranged and 47 (24%) were referred to pulmonary rehabilitation. The clinicians were prompted to provide a written educational pack and a formal crisis management plan in all cases. The inhaler technique was deficient in 25% of the 191 patients and was addressed.
Table 1. Lung function results and patient stratification.
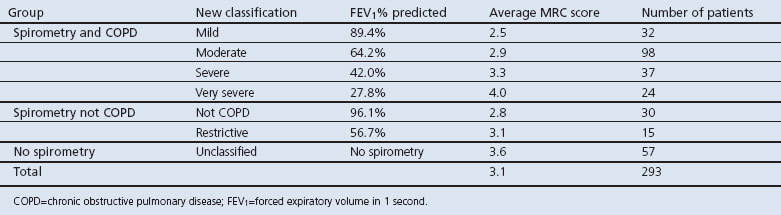
Of the 236 full reviews, 45 did not have COPD and 24 had other conditions as the predominant problem. In total, 169 had therapeutic changes and only 22 (9%) had no changes from the computer-based guided consultation.
Seven of the 18 nurses who participated in the pilot had no specialty respiratory training and were instructed in the use of the system during a 2-day mentoring period when they had support from a trained respiratory nurse. They were asked to evaluate the system using a Likert scale and the results are shown in Box 3. They agreed that the system would help to standardise care and all confirmed they were comfortable using it alone after 2 days of support.
Nurses' questionnaires on the system.
Q1. Use of the software will help standardise patient care: 6/7 agree; 1/7 tend to agree
Q2. The flow ensures no aspect of assessment is omitted: 5/7 agree; 2/7 tend to agree
Q3. Using the software will aid accurate diagnosis: 4/7 agree; 3/7 tend to agree
Q4. I would need the following training to use the software: 7/7 ticked 1–2 days
Scale: agree, tend to agree, tend to disagree, disagree
Discussion
Main findings
This experience of introducing a computer-guided consultation in a number of practices and with a group of nurses of whom some had no formal post-qualification training in COPD confirms that this approach is feasible in primary care. The high diagnostic revision rate and the large proportion of patients (88%) being offered at least one guideline intervention indicates that use of the guided consultation software impacts positively on the management of patients. It also suggests that a full intelligent computer-guided consultation may provide an information technology (IT) foundation to ensure guideline-based care.
The nurses using the system were happy that the system helped to standardise care, although they were more neutral regarding the impact on diagnosis despite the proportion of patients that were found not to have COPD. In a third of the pilot centres the nurses had no formal post-qualification training in COPD; the results from these were the same as in the two-thirds of nurses who did have formal COPD training. While this is not a substitute for workforce training, the prompting does seem to enable delivery of a guideline quality management. However, as the system does not make decisions but rather prompts the clinician, we believe this enhances skilling rather than the opposite. The 45 mins allowed for the assessment was not exceeded even though the consultations included time for spirometry, a cardiopulmonary examination and check of inhaler technique; this is not longer than is reported for a full assessment using a traditional approach.10
Strengths and limitations of this study
The study was conducted as a ‘proof of principle’ and, as such, it does not have the features of a randomised controlled trial. However, as we wished to assess feasibility and acceptability, the numbers entered provide significant practice exposure and, given that the whole consultation was guided, it represents considerable experience in the use of the approach. The number of clinical management changes prompted is substantial (at least one change in 88% of patients) and suggests a significant impact for the good of individual patients as well as the practice and locality in terms of outcomes. Given that the patients were already on the register, it seems likely that a standard review would not have delivered anything like the diagnostic revisions and interventions without the application. A trial of this approach versus traditional care may now be powered to assess the effect on interventions and impacts. The application was shown to work with nurses with COPD training and those without. The practices selected were in urban, semi-rural, and rural settings, again suggesting the potential for the universal introduction of this and similar programmes to drive the implementation of guideline care.
We did assess acceptability, but only in the nurses who had no specialist COPD training. The decision to enquire about this was made during the phase when non-experts were using the software. This question was prompted by a query from one of the sponsoring companies. We did not go back to the other nurses as those practices had completed the reviews and the gap would have been more than a month, so it was felt to be inappropriate because of selective recall and other potential confounders. We have no reason to expect that the views would be different but future work should assess this.
The software application used was the beta version, so updating of data required for QOF was not automated. This required manual updating in the GP system with five pieces of COPD data and the placing of the electronic patient summary PDF on the desktop in the patient file which takes about 1 min. This may have negatively affected opinions on the impact. The final version of the application automates this and automatically draws down patient information such as demographics and contacts from existing GP systems.
Interpretation of findings in relation to previously published work
The finding that 19% of patients on a COPD register do not have airway obstruction has been shown before5 and supports the new UK Strategy's focus on quality spirometry. However, in addition, the intelligent algorithms supplement this and prompted nurses to detect a further 10% of patients who have other diagnoses that may be more important than mild airway obstruction. Many older patients have more than one pathology, and the package ensures this is not overlooked. Despite the stress on spirometry, there were 57 who did not have spirometry at this visit and in only a few cases were the reasons clear. Given the centrality of spirometry to COPD management, the computer package design ensures that this is not forgotten and the nurse will be reminded at the next visit to make up the deficiency and perform spirometry.
Despite being on GP registers and having had previous assessments, patient care was not being managed according to guidelines. Interventions recommended ranged from adding drugs to providing education and from smoking advice to rehabilitation referral. However, not all of the 88% of patients with therapy changes were additive. Reduced pharmacotherapy was advised for over 40% with mild/moderate disease and in those without airway disease, so optimising the use of health resources. We report the first visit data so do not know if all the recommendations were put in place or all patients acted on the offers of smoking cessation or pulmonary rehabilitation. However, an additional benefit of the system is that it leaves an audit trail confirming that such interventions were offered, ensuring quality, and reminds clinicians at follow-up to ask and record the outcomes of the changes.
Embedding intelligent algorithms into the clinical consultation means that the clinician is facilitated at each step of the review. As the consultation progresses, an electronic case record is created and the algorithms prompt the next step consistently. The embedded intelligence is across the consultation process so, rather than referring to a pathway or guideline, it is intrinsic to the process. There are a number of IT approaches to support care and standards; these include audit search tools such as Miquest-based systems, guideline summaries such as Map of Medicine,11 and some attempts at decision support tools described as Computer-Interpretable Guidelines or CIGs.12
Implications for future research, policy and practice
We propose that a comprehensive computer-guided consultation evolves the concept of IT use and is the logical development beyond current IT offerings such as audit tools, desktop summary pathways, or decision support tools which relate to a small part of a pathway such as drugs. Thus, in the context of a full optimisation review, each step has decision-supporting algorithms underpinning it as the consultation progresses. The results obtained here suggest that this is easily usable and that this approach is a step towards comprehensive support of the clinician in delivering a guideline level of management. Specifically, given the objective of ensuring that patients were appropriately on the COPD register, the computer-guided consultation adds to spirometry in improving diagnostic accuracy and provides a more logical base with which to plan care. Also, management was brought into line with guidelines while still respecting the autonomy of the clinician and the right of patients to decline interventions. In the COPD outcomes strategy a key feature is to have effective review of patients where the NICE guidance-based management can be offered. We believe intelligent decision-making software such as we describe can support the clinician in delivering this challenge. What is also interesting to consider is the extent to which a non-clinician or even the patient could, once a diagnosis is confirmed, use such a system to facilitate and inform a discussion on management. It has already been suggested to us that pulmonary function technicians or pharmacists could use a version of this application to enable the healthcare community to achieve guideline standard care for as many patients as possible.
One PCO involved in the pilot is currently introducing the system as a standard across all its practices and others are about to start. This PCO had a universal audit of COPD care prior to introducing the software, and it is intended that this will be repeated after the patients have been reviewed to see what this implementation achieves in terms of guideline implementation and health outcomes in years 2 and 3 as, by this time, most of the COPD population in the PCO will have received this level of review. The software is now hosted on the UK NHS N3 website. This means that it is possible for intermediate care teams and secondary care also to have access to these records if the GP teams so wish. Indeed, with the hosting in the NHS net, the system could potentially be made available to any NHS team interested in using IT to support COPD care.
Finally, given the initial impact of this approach in standardising management in the COPD population, similar programmes are being developed for asthma and other chronic diseases. Future research priorities may be planned comparing routine clinical care with that using a comprehensive computer-guided consultation. Implementation of the guidelines would be a key end point, but maintenance of guideline practice and clinical outcomes such as impact on admissions and costs should be included. Given the size of changes seen here, if such research confirms our observations the corollary may be that clinical care will ultimately be based on these systems rather than relying on clinicians and the expertise they may or may not bring.
Conclusions
We suggest that this report demonstrates ‘proof of principle’ regarding the use of a computer-guided consultation. The COPD-guided consultation software application clearly impacts on clinical care, improving diagnostics and triggering the comprehensive delivery of guideline interventions. As such, it may not be overstating these observations to suggest that a full computer-guided consultation may represent a new paradigm in the use of IT in healthcare.
Acknowledgments
Handling editors Alan Crockett and Aziz Sheikh
Statistical review Gopal Netuveli
The authors acknowledge the help of Dr Stan Shepherd, Tina Hargadon and Elizabeth Thompson.
Funding AstraZeneca, Boehringer Ingelheim and GlaxoSmithKline provided unrestricted grants to support this work.
Footnotes
The software was developed personally with no NHS investment and four of the authors (RMA, LD, EM and MGP) have formed a company LungHealth to commercialise the software as the NHS would not support the development cost. We performed the research in our professional capacity and LungHealth is not mentioned in the paper.
References
- National Institute for Health and Clinical Excellence. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. London: National Clinical Guideline Centre. 2010. http://guidance.nice.org.uk/CG101/Guidance/pdf/English [Google Scholar]
- Shahab L, Jarvis MJ, Britton J, et al. Chronic obstructive pulmonary disease: prevalence, diagnosis and relation to tobacco dependence of chronic obstructive pulmonary disease in a nationally representative population sample. Thorax 2006;61(12):1043–7. http://dx.doi.org/10.1136/thx.2006.064410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHS Confederation, British Medical Association. New GMS Contract, 2003.
- Department of Health. Chronic obstructive pulmonary disease (COPD) indicator set: dataset and business rules: new GMS Contract QOF implementation (Version 14.0). London: Department of Health, 2009. [Google Scholar]
- Jones RCM, Dickson-Spillmann M, Mather MJC, Marks D, Shackell B. Accuracy of diagnostic registers and management of chronic obstructive pulmonary disease: the Devon primary care audit. Respir Res 2008;9:62. http://dx.doi.org/10.1186/1465-9921-9-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upton J, Madoc-Sutton H, Sheikh A, Frank TL, Walker S, Fletcher M. National survey on the roles and training of primary care respiratory nurses in the UK in 2006: are we making progress? Prim Care Respir J 2007;16:284–90. http://dx.doi.org/10.3132/pcrj.2007.00068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royal College of Physicians of London, British Thoracic Society and British Lung Foundation. Report 5 of the national chronic obstructive pulmonary disease audit 2008: survey of COPD care within UK general practices. December 2008.
- Department of Health. An outcomes strategy for chronic obstructive pulmonary disease (COPD) and asthma. London: Department of Health, 2011. Gateway Reference 16249 [Google Scholar]
- National Institute for Health and Clinical Excellence. http://publications.nice.org.uk/chronic-obstructive-pulmonary-disease-quality-standard-qs10
- Gupta J, Gupta A. Improving outcomes for COPD patients in primary care through joint working. Guidelines in Practice 2011;14:27–34. [Google Scholar]
- Map of Medicine. http://eng.mapofmedicine.com
- Greenes RA, ed. Clinical Decision Support: the road ahead. Academic Press, Waltham, Massachusetts, 2006. [Isbn 978-0-12-369377-8] [Google Scholar]