Abstract
Introduction:
Headache is a common reason for visiting emergency departments, and pain control is a major therapeutic goal in patients with headaches.
Objective:
The present study was conducted to examine the effectiveness of the concurrent intravenous administration of dexamethasone and metoclopramide in pain control in patients presenting to emergency departments with complaints of primary headache.
Methods:
This quasi-experimental study examined patients with moderate to severe headache attacks presenting to emergency departments. An 8-mg dose of dexamethasone and a 10-mg dose of metoclopramide were intravenously administered to the patients. The degree of headache was measured and recorded using the Numeric Rating Scale (NRS) upon admission and one hour and two hours after the injection.
Results:
A total of 51 patients with a mean age of 38.3±10.5 years participated in the study. The patients’ mean pain score was 8.4±1.3 upon admission and reduced to 6.2±2.3 one hour after the administration of the medication and to 3.1±2.9 two hours after the administration, suggesting significant reductions on both occasions (P<0.05). The therapeutic success was 39.2% one hour after the administration of the medication and 84.3% two hours after the administration.
Conclusion:
Based on these findings, the concurrent administration of dexamethasone and metoclopramide appears to affect the control of headache intensity in patients with primary headaches presenting to emergency departments.
Key Words: Dexamethasone, Emergency department, Headache, Metoclopramide, Pain control
INTRODUCTION
Headache is a common cause of presenting to emergency departments and accounts for 2% of all the visits to these units (1). Headache has different types and has so far been divided into 150 categories. Tension headaches and migraine headaches are the two most common categories of headache, in respective order. Headaches with serious pathologies constitute only 1% of acute cases of headache presenting to emergency departments (1-3). Most of the patients presenting to emergency departments suffer from severe headache and require rapid and effective treatments for alleviating their symptoms in addition to proper diagnostic measures (4). Different agents are used to treat these types of headache, including nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, caffeine, anti-nausea medications and antipsychotics (5-7). Corticosteroids are believed to play a key role in reducing the intensity and frequency of headaches through the suppression of the inflammatory response. Dexamethasone is an anti-inflammatory corticosteroid that is used to treat other inflammatory disorders of the central nervous system (CNS), such as acute bacterial meningitis and vasogenic cerebral edema caused by CNS tumor. Compared to other corticosteroids, dexamethasone offers additional advantages such as a high potency, a long duration of action and a better penetration into the CNS (8). Dopamine antagonists such as metoclopramide, alone or in combination with other medications, and serotonin agonists such as sumatriptan have been increasingly used in recent years to treat headaches (9). The use of metoclopramide reduces the severity of headache, although its effectiveness is controversial (10). Despite the different guidelines for the treatment of headache, there is still a lot of disagreement on this subject, which leaves room for extensive research on the subject with no limitations (11-13). Pain control in patients with headache presenting to emergency departments is a controversial research topic that needs to be further investigated despite the numerous studies. The present study was conducted to investigate the effectiveness of the concurrent administration of dexamethasone and metoclopramide in controlling the severity of headache in patients with primary headache.
METHODS
Study design
The present quasi-experimental study was conducted in 2017 at the emergency department of Shohada-e Tajrish Hospital in Tehran, Iran. The study was carried out according to the ethical principles stipulated in the Declaration of Helsinki. All the eligible patients were informed about the medication used and asked to sign written consent forms. The research project was also approved by the ethical committee of Shahid Beheshti University of Medical Sciences and the code IR.SBMU.MSP.REC.1394.190 assigned to it.
Study population
Eligible patients aged 18 and above who presented to the emergency department with complaints of headache were interviewed by the researcher and included in the study if meeting the diagnostic criteria for primary headaches defined in the International Classification of Headache Disorders. The patients’ medical history was taken and they were excluded in case of having conditions such as cardiac dysrhythmia, hypertension, cardiac ischemia, peptic ulcer, inflammatory bowel diseases, obsessive-compulsive disorders, pregnancy, breastfeeding, coagulation disorders, renal failure, liver failure and sleep disorders. Convenience sampling was used to select the subjects and the sample size was estimated as 51 with a confidence interval of 95%, a test power of 90%, α=0.05 and β=0.2.
Intervention
The patients were examined in terms of their pain score and received intravenous (IV) headache control medications if showing moderate to severe pain. The patients’ pain was measured and recorded using the Numeric Rating Scale (NRS). A total of 8 mg of dexamethasone and 10 mg of metoclopramide were then intravenously administered to the patients. The pain intensity was measured one and two hours after the administration of the medication. The medication administration and the pain intensity assessment within the first two hours after administration were by no means an obstacle to the diagnostic measures taken at the treating physician’s discretion. Opioid medications were used as a second-line therapy if pain control was not achieved.
Definitions
The NRS is a simple tool for evaluating pain intensity using a ruler scaled from 0 to 10. The absence of pain is marked by a score of 0 and the highest imaginable pain by 10. A score of 1-3 indicates slight pain, 4-6 moderate pain and 7-10 severe pain (14). Therapeutic success was defined in the present research as a reduction of at least 3 points in the pain score compared to the score obtained upon admission (15, 16).
Statistical analysis
The statistical analysis of the data was performed using IBM®-SPSS®-Statistics-V22.0 software. Measures including the mean, standard deviation, median and middle quartile were used to describe the continuous variables, while frequency and percentage were used to describe the categorical variables. Mann-Whitney’s U-test and the Wilcoxon test were used to analyze the difference in the pain score. P<0.05 was set as the level of statistical significance.
RESULTS
Of the total of 51 patients with a mean age of 38.3±10.5 years treated with a combination of dexamethasone and metoclopramide, 30 (58.8%) were female. Table 1 presents the demographic details of the studied patients. As shown, the highest prevalence of primary headache is observed in the 30-39 age group.
Table 1.
The baseline characteristics of the studied patients
| Variable | Number (%) |
|---|---|
| Gender | |
| Male | 21 (41.2) |
| Female | 30 (58.8) |
| Age (year) | |
| 18-29 | 11 (21.6) |
| 30-39 | 21 (41.2) |
| 40-49 | 11 (21.6) |
| 50-59 | 7 (13.7) |
| ≥60 | 1 (1.9) |
| Analgesic consumption before admission | |
| Yes | 43 (84.3) |
| No | 8 (15.7) |
Figure 1 presents the variations in the intensity of pain in the patients over the two-hour follow-up. The score of perceived pain intensity was 8.4±1.3 upon admission. The pain score reduced to 6.2±2.3 (P=0.041) one hour after the administration of the medication and to 2.9±3.1 (P<0.001) two hours thereafter.
Figure 1.
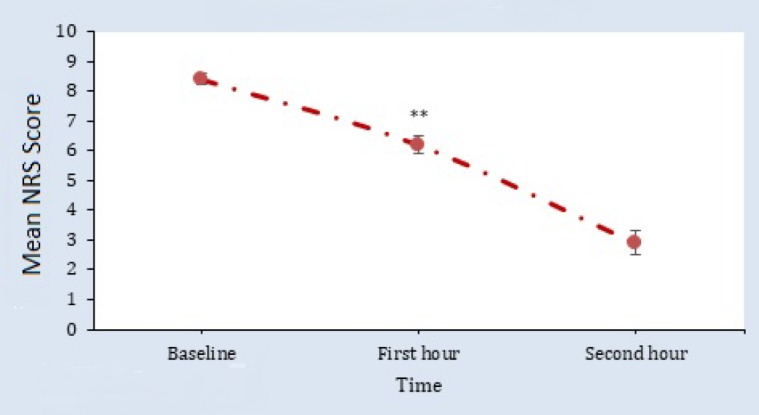
Variations in the mean pain score in the patients during the assessment
Based on the definition provided, therapeutic success was 39.2% in the first hour after medication administration in the dexamethasone-metoclopramide group and 84.3% in the second hour. Eight (15.7%) of the patients showed a pain relief less than 3 scores in the second hour of the follow-up, although all the patients had an NRS score ≤3 after the treatment, which indicates slight pain.
No cases of treatment intolerance or side-effects such as tachycardia, hypertension, itching, nausea and vomiting, pain at the injection site and irritability were reported in the patients during their hospitalization, which shows the safety of the concurrent IV administration of dexamethasone and metoclopramide in the study population.
DISCUSSION
The present findings showed a significant reduction in pain intensity in the first and second hours after the IV injection of dexamethasone and metoclopramide in patients with headache presenting to the emergency department. This combination therapy appears to have achieved therapeutic success with a reduction of more than 3 points in the NRS score one hour after administration and a reduction of more than 5 points two hours after administration.
The present findings support the results of other studies on the use of one of the two medications in question. The majority of studies on this subject have examined the effectiveness of one of these two medications alone or have compared their effectiveness to that of other medications. There are very few studies on the effectiveness of the combination of these two medications; one instance is the double-blind randomized clinical trial conducted by Shahrami et al., which compared the effect of administering magnesium sulfate with the concurrent administration of dexamethasone and metoclopramide on pain intensity in migraine patients and found no significant differences in the mean pain score reported 20 minutes after the administration of dexamethasone and metoclopramide and the pain score observed upon admission; nevertheless, one and two hours after the administration of dexamethasone and metoclopramide, the migraine patients reported significant pain reduction. Magnesium sulfate was found to be a more effective medication than combined dexamethasone and metoclopramide in treating acute migraine pain (17). The present study also confirms the effectiveness of dexamethasone and metoclopramide combination in pain control. Numerous studies have been conducted to date on the effectiveness of dexamethasone in controlling the intensity of pain in patients with headache. A simple randomized study by Friedman et al. on the effectiveness of incorporating dexamethasone into the therapeutic regimen of migraine patients showed that the IV administration of dexamethasone and metoclopramide is likely effective and causes few side-effects in migraine patients in the emergency department, especially in those with frequent and prolonged migraine attacks (18). These results are largely consistent with the present findings, and as already noted, a good response to treatment with no complications was an advantage of this combination of therapy. In contrast, a randomized controlled trial by Rowe et al. showed that dexamethasone fails to reduce the recurrence of headache after discharge from the emergency department and also that recurrence is associated significantly with an incomplete recovery from pain when discharged from the hospital (19). Systematic review studies and meta-analyses were conducted in response to these discrepancies; for instance, a meta-analysis by Colman et al. examined the effect of IV dexamethasone on the treatment and prevention of migraine headache recurrence and showed that adding a single dose of IV dexamethasone to the standard migraine treatment is associated with a relative reduction of 26% in the recurrence of headache within 72 hours (20). A meta-analysis conducted by Singh et al. also showed that dexamethasone is an effective medication for preventing the recurrence of headaches that can be safely added to the standard migraine treatment in emergency departments (21). Some studies have surveyed the effectiveness of metoclopramide in pain control in patients with headache. A randomized, double-blind, clinical trial conducted by Faridaalaee et al. also found acetaminophen to be more effective than IV metoclopramide in alleviating primary headaches, as the success rate of pain relief reported in the first 15 minutes of administration was 42% for acetaminophen and 0% for metoclopramide (22). In the present study, however, therapeutic success was 39.2% one hour after administering dexamethasone and metoclopramide and 84.3% in the second hour of administration; nonetheless, this study did not evaluate the patients’ pain scores 20 minutes after the treatment.
In contrast, some studies have questioned the therapeutic success of metoclopramide and proposed other available medications to be superior; these studies have also discussed other important aspects of treatment. For example, in their randomized double-blind clinical trial, Friedman et al. compared the effectiveness of the IV injection of 20-mg metoclopramide up to four times within two hours with the effectiveness of 6-mg subcutaneous sumatriptan in the treatment of primary headache in the emergency department and found the pain score to be 7.2 in the metoclopramide group and 6.3 in the sumatriptan group two hours after the treatment, which reduced to 6.1 and 5 after 24 hours. The rate of pain-free patients was 59% in the metoclopramide group and 35% in the sumatriptan group two hours after the treatment. The authors concluded that the effectiveness of metoclopramide is comparable to that of sumatriptan in the treatment of migraine in the emergency department and is even preferred given some secondary endpoints (23).
In view of the discussed issues, metoclopramide and dexamethasone can be considered readily available and cost-effective medications. The present findings thus suggest that the concurrent administration of dexamethasone and metoclopramide can be significantly effective and cause no complications when used in combination with each other. Since this study was conducted on a small sample size, the accuracy of the results should be confirmed through further studies with larger sample sizes. Systematic review studies are recommended to be conducted on the effectiveness of different medications in controlling headache, and the effectiveness of combination therapy with dexamethasone and metoclopramide should also be re-assessed.
Limitations
The present study was not randomized and had no control groups, and this fact might have affected the validity of the results. Moreover, the follow-up of the patients in terms of pain relief took place only during their hospitalization, and cases of early and late recurrence were not examined.
CONCLUSIONS
The present findings suggest that the concurrent administration of dexamethasone and metoclopramide can be effective in pain control in patients with primary headache presenting to the emergency department.
ACKNOWLEDGEMENTS
The authors would like to express their gratitude to the staff and authorities of the emergency department of Shohada-e Tajrish Hospital for their cooperation. This paper has been extracted from Dr. Erfan Shafiee’s thesis for general practitioner degree at Shahid Beheshti University of Medical Sciences, Tehran, Iran.
AUTHORS’ CONTRIBUTION
SM and HDK developed and supervised the research. SM and ES designed the study. ES collected and recorded the entire data. SM and ES analyzed the data. SM and HDK wrote the draft. All the authors finalized the final manuscript.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest with regard to this study.
FUNDING
The study was entirely funded by the authors.
References
- 1.Goldstein J, Camargo C, Pelletier A, Edlow J. Headache in United States emergency departments: demographics, work‐up and frequency of pathological diagnoses. Cephalalgia. 2006;26(6):684–90. doi: 10.1111/j.1468-2982.2006.01093.x. [DOI] [PubMed] [Google Scholar]
- 2.Bigal M, Bordini CA, Speciali JG. Headache in an emergency room in Brazil. Sao Paulo Med J. 2000;118(3):58–62. doi: 10.1590/S1516-31802000000300002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman BW, Hochberg ML, Esses D, Grosberg B, Corbo J, Toosi B, et al. Applying the International Classification of Headache Disorders to the emergency department: an assessment of reproducibility and the frequency with which a unique diagnosis can be assigned to every acute headache presentation. Ann Emerg Med. 2007;49(4):409–19. doi: 10.1016/j.annemergmed.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Balbin JEB, Nerenberg R, Baratloo A, Friedman BW. Intravenous fluids for migraine: a post hoc analysis of clinical trial data. Am J Emerg Med. 2016;34(4):713–6. doi: 10.1016/j.ajem.2015.12.080. [DOI] [PubMed] [Google Scholar]
- 5.Vinson DR. Treatment patterns of isolated benign headache in US emergency departments. Ann Emerg Med. 2002;39(3):215–22. doi: 10.1067/mem.2002.121400. [DOI] [PubMed] [Google Scholar]
- 6.Baratloo A, Bafarani SA, Forouzanfar MM, Hashemi B, Friedman BW, Abdalvand A. Intravenous caffeine versus intravenous ketorolac for the management of moderate to severe migraine headache. Bangladesh J Pharmacol. 2016;11(2):428–32. [Google Scholar]
- 7.Baratloo A, Negida A, El Ashal G, Behnaz N. Intravenous caffeine for the treatment of acute migraine: a pilot study. J Caffeine Res. 2015;5(3):125–9. [Google Scholar]
- 8.Czock D, Keller F, Rasche FM, Häussler U. Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids. Clin Pharmacokinet. 2005;44(1):61–98. doi: 10.2165/00003088-200544010-00003. [DOI] [PubMed] [Google Scholar]
- 9.Talabi S, Masoumi B, Azizkhani R, Esmailian M. Metoclopramide versus sumatriptan for treatment of migraine headache: A randomized clinical trial. J Res Med Sci. 2013;18(8):695–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Ashina S, Portenoy RK. Intravenous treatment of migraine. Tech Reg Anesth Pain Manag. 2012;16(1):25–9. [Google Scholar]
- 11.Baratloo A, Mirbaha S, Delavar Kasmaei H, Payandemehr P, Elmaraezy A, Negida A. Intravenous caffeine citrate vs magnesium sulfate for reducing pain in patients with acute migraine headache; a prospective quasi-experimental study. Korean J Pain. 2017;30(3):176–82. doi: 10.3344/kjp.2017.30.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forouzanfar MM, Mahmoudi S, Javadzadeh HR, Baratloo A, Mahdavi NS, Hashemi B, et al. The effect of haloperidol administration on relieving cluster headache, probable role of dopaminergic pathway; a double blind clinical trial. J Med Physiol. 2016;1(2):72–7. [Google Scholar]
- 13.Baratloo A, Rouhipour A, Forouzanfar M, Safari S, Amiri M, Negida A. The Role of Caffeine in Pain Management: A Brief Literature Review. Anesth Pain Med. 2016;6(3):e33193. doi: 10.5812/aapm.33193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pain Assessment Scales: University of Florida. 2017. Available from: http://pami.emergency.med.jax.ufl.edu/resources/pain-assessment-scales.
- 15.Fink R. Pain assessment: the cornerstone to optimal pain management. Proc (Bayl Univ Med Cent) 2000;13(3):236–9. doi: 10.1080/08998280.2000.11927681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andersson V, Bergman S, Henoch I, Wickström Ene K, Otterström-Rydberg E, Simonsson H, et al. Pain and pain management in hospitalized patients before and after an intervention. Scand J Pain. 2017;15(Supplement C):22–9. doi: 10.1016/j.sjpain.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 17.Shahrami A, Assarzadegan F, Hatamabadi HR, Asgarzadeh M, Sarehbandi B, Asgarzadeh S. Comparison of therapeutic effects of magnesium sulfate vs dexamethasone/metoclopramide on alleviating acute migraine headache. J Emerg Med. 2015;48(1):69–76. doi: 10.1016/j.jemermed.2014.06.055. [DOI] [PubMed] [Google Scholar]
- 18.Friedman B, Greenwald P, Bania T, Esses D, Hochberg M, Solorzano C, et al. Randomized trial of IV dexamethasone for acute migraine in the emergency department. Neurology. 2007;69(22):2038–44. doi: 10.1212/01.WNL.0000281105.78936.1d. [DOI] [PubMed] [Google Scholar]
- 19.Rowe BH, Colman I, Edmonds ML, Blitz S, Walker A, Wiens S. Randomized controlled trial of intravenous dexamethasone to prevent relapse in acute migraine headache. Headache. 2008;48(3):333–40. doi: 10.1111/j.1526-4610.2007.00959.x. [DOI] [PubMed] [Google Scholar]
- 20.Colman I, Friedman BW, Brown MD, Innes GD, Grafstein E, Roberts TE, et al. Parenteral dexamethasone for acute severe migraine headache: meta-analysis of randomised controlled trials for preventing recurrence. BMJ. 2008;336(7657):1359–61. doi: 10.1136/bmj.39566.806725.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh A, Alter HJ, Zaia B. Does the Addition of Dexamethasone to Standard Therapy for Acute Migraine Headache Decrease the Incidence of Recurrent Headache for Patients Treated in the Emergency Department? A Meta‐analysis and Systematic Review of the Literature. Acad Emerg Med. 2008;15(12):1223–33. doi: 10.1111/j.1553-2712.2008.00283.x. [DOI] [PubMed] [Google Scholar]
- 22.Faridaalaee G, Rahmani SH, Mehryar H, Shishavan SB, Merghati SZ, Hasanloei MAV, et al. Comparison of intravenous metoclopramide and acetaminophen in primary headaches: A randomized controlled trial. Emergency. 2015;3(2):70–4. [PMC free article] [PubMed] [Google Scholar]
- 23.Friedman B, Corbo J, Lipton R, Bijur P, Esses D, Solorzano C, et al. A trial of metoclopramide vs sumatriptan for the emergency department treatment of migraines. Neurology. 2005;64(3):463–8. doi: 10.1212/01.WNL.0000150904.28131.DD. [DOI] [PubMed] [Google Scholar]


