Abstract
Introduction:
The purpose of triage in the standard Clinical Practice Guide (CPG) for multiple trauma patients is to perform the primary and secondary evaluations in the quickest and shortest possible time with minimal errors and the best quality in the emergency department (ED).
Objective:
In this study, a practical program for a coordinated management of multiple trauma patients in the ED has been provided by using the CPG guide. The impact of its implementation on the multiple trauma patients’ management was evaluated.
Methods:
This is a cross-sectional study conducted in 2014 and 2015 in Isfahan’s Al-Zahra hospital ED. Administration and management of multiple trauma patients had been prepared before the implementation of the plan based on standard clinical methods of implementation in a way that used a 12-step protocol for the practical guide. This protocol was designed as a flowchart and the results before and after its implementation were evaluated.
Results:
In this study, 100 multiple trauma patients before and after the implementation of the protocol were studied. The mean age of the patients and other baseline characteristics of studied patients in the two periods before and after implantation of the CPG were not significantly different (p > 0.05). The frequency of intubation (p = 0.016) and sent to the operating room (p < 0.001) were different in the two study periods. However, hospitalization in the ICU (p = 0.35) and death (p = 0.73) before and after implementation of the protocol were not statistically different. The time before examination by the EM physicians was significantly lower in all triage levels after CPG implementation. Meanwhile, no change in time elapsed occurred for the surgeons except for the patients in level 2 of triage.
Conclusion:
Implementation of the strategic plan of CPG lead to a significant reduction in waiting time for visits by emergency medicine services and other specialized services, increased the deployment of patients needing surgery, and reducing the time spent in the ED.
Key Words: Clinical protocols, Emergency service, hospital, Multiple trauma, Triage
INTRODUCTION
Trauma and injuries alone constitute more than 10% of the disease burden among adults in and includes more than 80% of deaths in low and middle income countries (1, 2). Available reports indicate that in 2000, more than 9 million incidents leading to trauma occurred in Iran and as a result, 4 million people underwent outpatient treatment and around 1,100,000 people were hospitalized (3). Hospital emergency departments (EDs) are responsible for providing immediate medical care 24 hours a day 7 days a week for all patients, including injured ones. In recent decades, population growth, the increased incidence of intentional and unintentional injuries and substance abuse have faced hospital EDs with increasing numbers of patients, while the number of and space in EDs has not been increased significantly (4-6). Meanwhile, the main public expectation of this department is to provide immediate medical care appropriate to the severity of the clinical status of the patients. Therefore, the patients' waiting time and length of stay in the ED are among the key factors in assessing the quality of care provided (7, 8). Prolonged length of waiting time and keeping patients in the ED may the result of inefficient workflow processes during the three-steps of patients entering the ED (input), providing care in the ED (throughput), and exiting patients from it (output) (9). This may result in the formation of a negative attitude of the community toward hospitals and health care providers, in addition to a negative impact on the expected treatment outcomes (5, 10-12).
Management of multiple trauma patients and performing timely diagnostic and therapeutic measures in preserving lives of patients and preventing complications arising from injury is an undeniable necessity. Therefore, if there is no program and protocols for management of these patients, improper and repetitive measures and lack of timely and correct diagnosis of injury results in a loss of golden times for saving patients and ultimately will be followed by increasing the complications of multiple trauma patients in the ED (13, 14).
In this context, a patient’s waiting time for diagnostic and therapeutic services is an acceptable criterion for evaluating the correct management of patients (11). Therefore, the first policy that should be implemented in the ED is the fact that patients referred to be triaged should be triaged at the earliest time possible and receive any specialized service visit required and para-clinical measures so that the patient can be sent to the relevant department in the shortest time and thus, the bed turnover rate of ED increases and the opportunity for admission of other patients is provided (9).
Generally, protocol implementation, guidelines and elaborated strategies proportional to the regional situation and the hospitals is necessary in dealing with emergency patients and managing their treatment and treatment outcome feedback; elaboration and implementation of a set of guidelines and protocols called the Clinical Practice Guide (CPG) has been proposed in the case of multiple trauma patients (5, 11, 12, 15, 16). In this study, a practical program for a coordinated management of multiple trauma patients in the ED has been provided by using the CPG guide, and the impact of its implementation on multiple trauma patients’ management was evaluated.
METHODS
Study design
This was a cross sectional study conducted in 2014 and 2015 in the ED of Al-Zahra Hospital, Isfahan, Iran. The study protocol was approved by the ethics committee of Isfahan University of Medical Sciences and the code ir.mui.res.1393.3.897 was assigned. The authors adhered to Helsinki Principles throughout the study.
Study population
Multiple trauma patients admitted to the ED during the study period were eligible. Those who were discharged against medical advice during the hospitalization in the ED and those who were referred from another medical center and rejected at least one of the doctor's orders were excluded.
CPG preparation
Following frequent meetings inviting expert professors of emergency medicine (EM), surgery, neurosurgery, orthopedic, urology and anesthesiology, a 12-step protocol for the administration and management of multiple trauma patients has been developed, the CPG. Before implementation, it was performed as a pilot on 20 multiple trauma patients during a week and necessary changes and existing shortcomings were eliminated.
Data gathering
According to the prepared CPG, a checklist including triage category, duration of clinical and para-clinical procedures, performing treatment measures including surgery, transfer of patients to the wards, performing mechanical ventilation in the ED, transfer to the intensive care unit (ICU), duration of hospitalization, and finally patient and hospital costs were provided. The prepared checklist was completed for 100 multiple trauma patients before the protocol implementation in January 2014. In the next step, the nursing staff, interns and residents working in the ED were provided training for the protocol. The mentioned protocol was also designed as a flowchart and installed in different parts of the ED. In the final phase, the prepared checklist was completed for 100 multiple trauma patients in January 2015.
Definitions
Triage was performing using Emergency Severity Index (ESI) version 4, which is a five-level ED triage algorithm that provides clinically relevant stratification of patients into five groups from 1 (most urgent) to 5 (least urgent) on the basis of acuity and resource needs. Al-Zahra hospital ED had 4 parts, and depending on the patient's triage level, they were transferred to each part. The 1st level of ESI were transferred to ED1, the 2nd level to ED2, the 3rd level to ED3, and the 4th level to fast track.
Statistical analysis
Study data were entered into SPSS software, version 23; after collection, they were analyzed with Chi-square tests, T-tests, and T-paired tests. The results before and after the implementation of the protocol were compared. A P-value less than 0.05 was considered to be significant.
RESULTS
In this study, 100 multiple trauma patients before the implementation of the protocol and 100 after that were studied. The mean age of the patients was 37.03 ± 12.48 years before CPG implementation and 38.47 ± 14.28 years after that (p = 0.112). Other baseline characteristics of the studied patients in the two periods before and after the implementation of the CPG are summarized in Table 1 and there was no statistical significance difference in this regard.
Table 1.
Baseline characteristics of studied patients before and after the protocol implementation
| Variable | Before protocol implementation | Before protocol implementation | P |
|---|---|---|---|
| number and percent | |||
| Sex | 0.820 | ||
| Male | 76 | 73 | |
| Female | 24 | 27 | |
| Mechanism of injury | 0.831 | ||
| Traffic accidents | 50 | 54 | |
| Fall from the height | 25 | 27 | |
| Assault | 15 | 9 | |
| Others | 10 | 10 | |
| Transport | 0.110 | ||
| Visitors | 23 | 39 | |
| Emergency Medicine Services | 46 | 44 | |
| Private ambulance | 27 | 11 | |
| From the prison | 4 | 6 | |
| Triage level | 0.430 | ||
| 1 | 10 | 11 | |
| 2 | 43 | 51 | |
| 3 | 47 | 38 | |
In Figure 1, the triage level of patients and appropriateness of triage level with trauma level before and after the implementation of the protocol is shown. Before CPG implementation, trauma level with triage level was inappropriate (wrong triage) in 15 people, was appropriate (correct triage, but wrong part of the ED) in 38 people and was perfectly appropriate (correct triage and correct part of the ED) in 47 people; while after CPG implementation, trauma level with triage level was inappropriate in 6 people, was appropriate in 43 people and was perfectly appropriate in 51 people and its appropriateness was not significantly different (p = 0.12).
Figure 1.
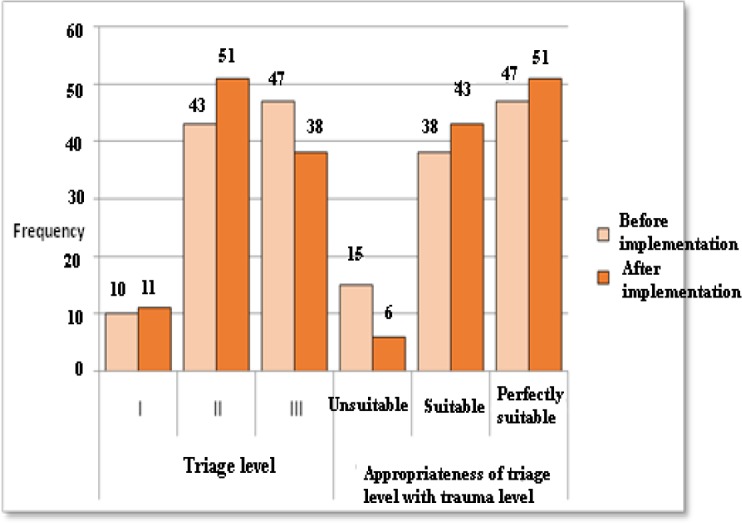
The frequency of triage level and appropriateness of triage level with trauma level before and after the implementation of the protocol
In Table 2, the mean and standard errors of the waiting time in different parts of the emergency and hospital before and after implementation of the protocol are shown. Based on the findings, the mean duration of hospitalization until the first visit by the EM physician and other physicians as well as the duration of stay in the ED department had a significant decrease after implementation of the protocol, but the mean of other time intervals and hospital costs had no significant differences between the two study periods.
Table 2.
Mean and standard errors of waiting time for obtaining services before and after protocol implementation
| Variable | Before protocol implementation | After protocol implementation | P |
|---|---|---|---|
| The average time of the first visit of emergency medicine physician (min) | 25/0 ± 19/6 | 14/6 ± 12/0 | <0.001 |
| The average time of the first visit of surgeon (min) | 29/6 ± 3/5 | 28/7 ± 4/0 | 0/87 |
| The average time of the first visit of other services (min) | 58/8 ± 5/6 | 41/1 ± 5/1 | 0/02 |
| Computed tomography scan time (min) | 57/7 ± 4/9 | 52/0 ± 5/4 | 0/45 |
| Chest X-ray time (min) | 49/5 ± 3/8 | 41/6 ± 3/7 | 0/14 |
| Hospitalization duration in emergency medicine department (hours) | 7/8 ± 1/6 | 4/2 ± 0/6 | 0/046 |
| Hospitalization duration in other services (hours) | 11/3 ± 0/9 | 9/7 ± 1/1 | 0/26 |
| Duration of hospital stay (days) | 5/0 ± 1/0 | 4/3 ± 0/5 | 0/48 |
| Hospital costs (million rials) | 3/9 ± 3/5 | 3/3 ± 3/2 | 0/18 |
The number of patients who underwent intubation in the ED before and after the CPG implementation was 12 and 3 patients, respectively, and the frequency of intubated patients after protocol implementation was significantly lower (p = 0.016). The number of patients were transferred directly from the ED to the operating room before and after protocol implementation was 11 and 53 cases, respectively; it was significantly greater after the CPG implementation (p < 0.001).
Figure 2 shows the frequency of intubation, sent to the operating room, hospitalization in the ICU, and death before and after implementation of the protocol. The number of patients admitted to intensive care units before and after implementation were 11 and 13, respectively, and there was no significant difference between before and after the implementation of the protocol (p = 0.35). The number of deceased before and after the protocol implementation was 5 and 4, respectively, and the difference between the two time periods was not significant (p = 0.73).
Figure 2.

The frequency of intubation, sent to the operating room, hospitalization in ICU and death before and after implementation of the protocol
It should be noted that 50 people (50%) were visited by the surgery service among the 100 patients studied before implementation of the protocol, but the number of surgery visits decreased to 45 people (45%) after the intervention, but the obtained difference was not statistically significant (p = 0.48).
In Table 3, the mean and standard deviation of the time before a visit based on the level of triage before and after implementation of the protocol are shown, indicating the EM and surgery physician groups. It is clear that the time before a visit by the EM physician group was significantly lessened in all triage levels. Meanwhile, the same change did not occur for the surgery physician group except for the patients in level 2 of triage.
Table 3.
Mean and standard deviation of time before a visit in terms of triage level before and after the intervention
| Group | Triage level | Waiting time before a visit | P | |
|---|---|---|---|---|
| Before protocol implementation | After protocol implementation | |||
| Emergency medicine physician | 1 | 8.3 ± 6.5 | 2 ± 2 | 0.006 |
| 2 | 23.2 ± 15.1 | 15.8 ± 10.7 | 0.006 | |
| 3 | 30.2 ± 22.8 | 16.7 ± 13.2 | 0.002 | |
| Surgery physician | 1 | 38.8 ± 25.9 | 24.9 ± 11.7 | 0.340 |
| 2 | 23.7 ± 4.5 | 25.5 ± 4.4 | 0.006 | |
| 3 | 34.8 ± 24 | 40.5 ± 29.2 | 0.620 | |
DISCUSSION
According to the results of the current study, the average time before the first visit of emergency medicine physicians and hospitalization duration in the ED decreased significantly after implementation of the protocol, which could be the result of timely actions by the emergency medicine service for patients' visits and on the other hand could represent the need for management by other specialized services with a timely presence to the patient's bedside.
In the current study, although the mean time before the first visit of patients by the EM physicians decreased after CPG implementation, the first visit by surgeons was not significantly different before and after implementation of the protocol. This might be due to the permanent presence of surgery service residents at all times before and after the implementation of the protocol in the ED, while the other services have no permanent presence and need to alter their schedules for visiting the ED.
The patients’ triage level was not significantly different before and after the implementation of the protocol, but the rate of sending patients for surgery significantly increased and the reason is that a significant number of patients before implementation of the protocol were initially transferred to the hospital wards and they were later prepared for surgery, but making a decision about the need for surgery at the earliest time possible by a specialized service in the ED was made possible by implementing the project, and patients were transferred to the operating room for surgery from there. In addition, cases requiring hospitalization in intensive care units are also envisaged in this protocol and many transfers to the intensive care unit (ICU) were also conducted by the EM physician group after consulting other specialized services.
Although the waiting time for specialized visits and waiting time to receive health services decreased after the protocol was implemented, the time for conducting para-clinical measures, including chest X-ray and CT scan time, had no significant reduction, and this is a concern due to the lack of resources, their time consuming nature, and the busyness of the mentioned units, and also because of the lack of coordination between the emergency department and such units and the impossibility of their management by the emergency medicine service. The solution to this dilemma is to provide independent imaging facilities in emergency departments, but unfortunately, such a possibility is currently not available in our country and currently, the best option is creating a single management system. Such a policy had been anticipated in the implementation protocol, but ideal results have not obtained from it due to side difficulties.
Implementation of the strategic plan of CPG, which was developed and implemented by utilizing protocols and guidelines in various specialized services and attracted the attention of experts from various fields of surgery, lead to a significant reduction in waiting time for visits by the EM physician group and other specialized services, increased deployment of patients needing surgery, and reducing the time spent in the ED, which could result in increasing ED turnover. However, the implementation of this program had no significant effect on reducing para-clinical measures including X-ray and CT scan time due to the impossibility of providing a single management for ED and para-clinical departments and a lack of coordination between the mentioned services. Therefore, we suggest that further studies should be conducted on increasing the effectiveness of the program and stemming peripheral problems leading to inefficiency of the program, in addition to continuing the proposed approach.
Limitations
Considering that Al-Zahra hospital is an educational center, despite the notification of the CPG, a number of residents managed the patients regardless of the guidelines. In addition, the protocol was only implemented for the ED, and it was better to include all other units, including laboratory, radiology and etc.
CONCLUSIONS
It is likely that implementation of the CPG lead to a significant reduction in waiting time before the first visit of the emergency medicine physicians and other specialized services to some extent, and increased deployment of patients needing for surgery and reducing the time spent in the ED.
ACKNOWLEDGEMENTS
The authors appreciate the insightful cooperation of Medical Sciences and the staff of the emergency department of Al-Zahra Hospital, Isfahan, Iran.
AUTHORS’ CONTRIBUTION
All the authors met the standards of authorship based on the recommendations of the International Committee of Medical Journal Editors.
CONFLICT OF INTEREST
None declared.
FUNDING
None declared.
References
- 1.Azami-Aghdash S, Sadeghi-Bazargani H, Shabaninejad H, Abolghasem Gorji H. Injury epidemiology in Iran: a systematic review. J Inj Violence Res. 2017;9(1):10.5249/jivr.v9i1.852. doi: 10.5249/jivr.v9i1.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sadeghi-Bazargani H, Ayubi E, Azami-Aghdash S, Abedi L, Zemestani A, Amanati L, et al. Epidemiological Patterns of Road Traffic Crashes During the Last Two Decades in Iran: A Review of the Literature from 1996 to 2014. Arch Trauma Res. 2016;5(3):e32985. doi: 10.5812/atr.32985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kobusingye OC, Hyder AA, Bishai D, Hicks ER, Mock C, Joshipura M. Emergency medical systems in low- and middle-income countries: recommendations for action. Bull World Health Organ. 2005;83(8):626–31. [PMC free article] [PubMed] [Google Scholar]
- 4.Weiss SJ, Derlet R, Arndahl J, Ernst AA, Richards J, Fernandez-Frackelton M, et al. Estimating the degree of emergency department overcrowding in academic medical centers: results of the National ED Overcrowding Study (NEDOCS) Acad Emerg Med. 2004;11(1):38–50. doi: 10.1197/j.aem.2003.07.017. [DOI] [PubMed] [Google Scholar]
- 5.Derlet RW, Kinser D, Ray L, Hamilton B, McKenzie J. Prospective identification and triage of nonemergency patients out of an emergency department: a 5-year study. Ann Emerg Med. 1995;25(2):215–23. doi: 10.1016/s0196-0644(95)70327-6. [DOI] [PubMed] [Google Scholar]
- 6.Arhami-Dolatabadi A, Maleki M, Memary E, Kariman H, Shojaee M, Baratloo A. The use of emergency department services for non-emergency conditions. Health MED. 2017;11(1):3–9. [Google Scholar]
- 7.Baratloo A, Maleki M. Iranian emergency department overcrowding. JEPT. 2015;1(2) [Google Scholar]
- 8.Hashemi B, Baratloo A, Forouzafar MM, Motamedi M, Tarkhorani M. Patient satisfaction before and after executing health sector evolution plan. Ir J Emerg Med. 2015;2(3):127–33. [Google Scholar]
- 9.Eitel DR, Rudkin SE, Malvehy MA, Killeen JP, Pines JM. Improving service quality by understanding emergency department flow: a White Paper and position statement prepared for the American Academy of Emergency Medicine. J Emerg Med. 2010;38(1):70–9. doi: 10.1016/j.jemermed.2008.03.038. [DOI] [PubMed] [Google Scholar]
- 10.Zohoor A, Pilevarzadeh M. Study of speed of offering services in emergency department at Kerman Bahonar hospital in 2000. Razi J Med Sci. 2003;10(35):413–9. [Google Scholar]
- 11.Banerjea K, Carter AO. Waiting and interaction times for patients in a developing country accident and emergency department. Emerg Med J. 2006;23(4):286–90. doi: 10.1136/emj.2005.024695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burgers JS, Grol R, Klazinga NS, Makela M, Zaat J. Towards evidence-based clinical practice: an international survey of 18 clinical guideline programs. Int J Qual Health Care. 2003;15(1):31–45. doi: 10.1093/intqhc/15.1.31. [DOI] [PubMed] [Google Scholar]
- 13.Baratloo A, Mirbaha S, Bahreini M, Banaie M, Safaie A. Outcome of Trauma Patients Admitted to Emergency Department Based on Full Outline of Unresponsiveness Score. Adv J Emerg Med. 2017;1(1):e2. doi: 10.22114/AJEM.v1i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hashemi B, Amanat M, Baratloo A, Forouzanfar MM, Rahmati F, Motamedi M, et al. Validation of CRASH Model in Prediction of 14-day Mortality and 6-month Unfavorable Outcome of Head Trauma Patients. Emergency. 2016;4(4):196–201. [PMC free article] [PubMed] [Google Scholar]
- 15.Cooke MW, Wilson S, Pearson S. The effect of a separate stream for minor injuries on accident and emergency department waiting times. Emerg Med J. 2002;19(1):28–30. doi: 10.1136/emj.19.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shaneyfelt TM, Mayo-Smith MF, Rothwangl J. Are guidelines following guidelines? The methodological quality of clinical practice guidelines in the peer-reviewed medical literature. Jama. 1999;281(20):1900–5. doi: 10.1001/jama.281.20.1900. [DOI] [PubMed] [Google Scholar]


