Abstract
Objective:
Drug-induced deaths, defined as intentional or unintentional consumption of illicit substances or diverted medications leading to death, are the leading cause of death for reproductive age women in the United States. Our objective was to describe pregnancy-associated deaths attributed to drug-induced causes in order to identify opportunities for intervention.
Methods:
Using the Utah Perinatal Morality Review Committee database, we performed a retrospective cohort study of all pregnancy-associated deaths - death of a woman during pregnancy or within one year from the end of pregnancy - from 2005 to 2014. We performed a detailed descriptive analysis of women with drug-induced deaths. We compared characteristics of women with drug-induced and other pregnancy-associated deaths.
Results:
From 2005 to 2014, 136 pregnancy-associated deaths were identified. Drug-induced death was the leading cause of pregnancy-associated death (n=35, 26%) and 89% occurred in the postpartum period. More specifically, those with a drug-induced death were more likely to die in the late postpartum period, defined as death occurring within 43 days to one year of the end of the pregnancy, (n=28/35, 80%) compared to women whose deaths were from other pregnancy-associated causes (n=34/101, 34%) (p<0.001). The majority of drug-induced deaths were attributed to opioids (n=27/35, 77%), prescription opioids (n=21/35, 60%) and polysubstance use (n=29/35, 83%). From 2005 to 2014, the pregnancy-associated mortality ratio increased 76%, from 23.3 in 2005 to 41.0 in 2014. During this same time period, the drug-induced pregnancy-associated mortality ratio increased 200%, from 3.9 in 2005 to 11.7 in 2014.
Conclusion:
Drug-induced death is the leading cause of pregnancy-associated death in Utah and occurs primarily in the late postpartum period. Interventional studies focused on identifying and treating women at risk of drug-induced death are urgently needed.
PRÉCIS:
Drug-induced deaths are the leading cause of pregnancy-associated death in Utah, and 89% occur in the postpartum period.
Introduction
Drug-induced deaths, defined as intentional or unintentional consumption of illicit substances or diverted medications leading to death, are the leading cause of death for reproductive age women in the United States.1–3 Sixty-one percent of drug overdose deaths involved opioids.4 Increasing drug use endangers every segment of the population including pregnant and postpartum women. From 1999 to 2014, the rate of deliveries complicated by maternal opioid use disorder, defined as a problematic pattern of opioid use leading to serious impairment or distress, more than quadrupled (from 1.5 per 1000 deliveries in 1999 to 6.5 in 2014).5 These rates do not include women using opioids as prescribed for medical indications. National estimates suggest that 14–40% of pregnant women will receive an opioid prescription at some time during their pregnancy.6,7 The most common reasons for opioid prescriptions during pregnancy are back pain, abdominal pain, headache or migraine, joint pain or other pain diagnosis6,7 From 2013–2015, Utah ranked seventh among all states in drug-induced age-adjusted death rates (23.4 per 100,000).4,8,9 In Utah, 42% of pregnant women insured by Medicaid are prescribed opioids, the highest rate of any state in the nation.7
Pregnancy and the postpartum period are particularly vulnerable times for drug use, drug relapse and drug-induced mortality. The vast majority (70–90%) of pregnant women who use illicit drugs will attempt and achieve drug abstinence by the second trimester.10–12 However, some conditions such as co-existing mood disorders increase the risk of relapse during pregnancy.13 Postpartum, women are at heightened risk of relapse and overdose, possibly due to decreased tolerance from periods of abstinence combined with hormonal changes, loss of insurance, and stress of caring for an infant.10,14 Among reproductive age women, the majority of drug-induced deaths (84.2%) are accidental,1 however, less is known about whether drug-induced pregnancy-associated deaths are accidental or intentional. Additionally, knowledge gaps exist regarding the circumstances surrounding drug use, drug relapse and drug-induced deaths among pregnant and postpartum women.15–17 Closing these gaps is critical to developing effective prevention strategies.
Our objective was to estimate the proportion and timing of pregnancy-associated deaths attributed to drug-induced causes in Utah from 2005–2014. We compared characteristics of women whose deaths were drug-induced compared to those whose deaths were not. Among women with drug-induced deaths, we compared characteristics of women whose drug-induced deaths were determined to be accidental, intentional or could not be determined. To better understand the circumstances surrounding drug-induced deaths, we aimed to identify the class(es) of drug(s) involved in the death, presence of polysubstance use and mental health conditions, intimate partner violence or history of abuse and involvement with drug treatment, and mental health and social services.
Methods
We conducted a retrospective cohort study of all pregnancy-associated deaths in Utah from January 2005 to December 2014 using the Utah Perinatal Mortality Review Committee (PMRC) database. Established in 1995, the Utah PMRC, an interdisciplinary committee of obstetrical and pediatric providers, public health officials, and epidemiologists, identifies and reviews all pregnancy-associated deaths occurring in Utah. Consistent with the Centers for Disease Control and Prevention (CDC) Pregnancy Mortality Surveillance System definitions, the PMRC defines pregnancy-associated death as the death of a woman while pregnant or within one year of the end of pregnancy, regardless of the cause.18,19 Pregnancy-associated, but not related, deaths were defined as occurring during pregnancy or within one year of the end of pregnancy, but not related to pregnancy (for example, a motor vehicle accident). A pregnancy-related death was defined as the death of a woman during pregnancy or within one year of the end of pregnancy, from a pregnancy complication, a chain of events initiated by pregnancy, or the aggravation of an unrelated condition by the physiologic effects of pregnancy.19 A pregnancy-associated death includes all deaths during pregnancy and within one year of the termination of pregnancy, including those that are pregnancy-related. Pregnancy-associated mortality ratio is the number of pregnancy-associated deaths per 100,000 live births.
For this study, we calculated the drug-induced pregnancy-associated mortality ratio. For the purposes of epidemiological reporting and quality improvement, state law grants the Utah Department of Health (UDOH) access to relevant data sources for all women with a pregnancy-associated death. These sources include medical records (inpatient, outpatient, prenatal, delivery and emergency room records), psychiatric and social work notes (when available), birth and death certificates, autopsy and toxicology reports, law enforcement reports, and other relevant sources. Cause of death was determined based on reviews of medical records, death certificates and medical examiner’s reports. The PMRC database contains information about maternal age, race, geographic location, number of prenatal visits and cause of death.
The UDOH identifies maternal deaths from death certificates using: 1) International Classification of Diseases 9 and 10 codes indicating that the death was related to or aggravated by pregnancy, childbirth or puerperium; 2) selection of pregnancy timing field including ‘pregnant at time of death’, ‘not pregnant, but pregnant within 42 days of death’ or ‘not pregnant, but pregnant within 43 days to one year before death;’ and 3) cross-referencing death certificates of women of reproductive age with live birth and fetal death certificates. For this study, we defined early postpartum death as death within 42 days and late postpartum death as occurring within 43 days to one year of the end of the pregnancy. UDOH reviews all possible deaths and forwards those meeting pregnancy-associated death criteria to the PMRC for further review.
The PMRC considers each death for its pregnancy-relatedness, contributing factors and preventability.20 Preventability was determined by the expert opinion of the PMRC by reviewing all available documents. A death is considered preventable if the committee determines that there was at least some chance of the death being averted by one or more reasonable changes to patient, family, provider, facility, system, and/or community factors.
To describe women’s drug use history, we used definitions published by the US Office of the Surgeon General.21 Drug use was defined as the use of any psychoactive drug with the potential to cause health or social problems including alcohol, opioids, stimulants, benzodiazepines, sedative/hypnotics, muscle relaxants, inhalants and cannabinoids. Drug use includes use of prescribed medications used appropriately. Drug relapse was defined as return to drug use after significant period of abstinence. Drug misuse was defined as any drug use in a manner, situation, amount or frequency that can cause harm to the user or to those around them. For specific populations including pregnant women, any drug use is synonymous with misuse with the exception of medications (e.g. opioids, benzodiazepines, stimulants) used as prescribed. Substance use disorder (SUD) is a primary brain disorder characterized by repeated misuse and clinically significant impairment in health, social functioning and impaired control over drug use. In this study, we combine drug misuse and SUD into one category as precise diagnostic criteria were usually not specified in the medical records.
Based on the Centers for Disease Control and Prevention guidelines, drug-induced deaths were defined as deaths from poisoning and medical conditions caused by use of legal or illegal drugs, as well as deaths from poisoning due to medically prescribed drugs and other drugs.22 Drugs implicated in pregnancy-associated deaths were determined based on the autopsy and toxicology reports. Drugs were grouped into opioids (including methadone, fentanyl, oxycodone, codeine, hydromorphone, heroin, tramadol), alcohol, benzodiazepines, sedative/hypnotics, muscle relaxants, acetaminophen, amphetamines, cannabinoids, antidepressants, cocaine and other (inhalants). Prescription opioids included methadone, fentanyl patches, oxycodone, codeine, hydrocodone, tramadol and hydromorphone. Illicit drugs included heroin, cocaine, methamphetamine/amphetamines and marijuana.
Based on Utah medical examiner’s assessments, deaths were defined as intentional (i.e. suicide), accidental, or could not be determined. Intentional deaths are those in which there is clear evidence that the individual intended to end her life either through written or verbal means (e.g. suicide note, social media post, endorsing active suicidal ideation or plan to someone prior to death). Accidental deaths were defined as those which lacked any evidence of intentional drug overdose or desire to end life. Deaths labeled “could not be determined” are those for which there is some evidence of intentional overdose but not enough to clearly define the death as intentional.
We assessed the proportion of pregnancy-associated deaths from 2005–2014 attributed to drug-induced reasons using the PMRC database. We chose this time period for two reasons: 1) drug-induced deaths were systematically cross-referenced with delivery records beginning in 2005 and 2) pregnancy-associated deaths after 2015 had not yet been fully analyzed.
Descriptive statistics (frequencies, percentages) were used to describe demographics and characteristics of women with drug-induced and non-drug-induced deaths available in the PMRC database. Fisher’s exact test and Kruskal-Wallis tests were used as appropriate. To assess geographical distribution of drug-induced pregnancy-associated death, we assessed the county of death and classified the location as urban, rural or frontier. As defined by the Utah Office of Primary Care and Rural Health, urban counties are defined as those with ≥100 persons/square mile, rural counties, 6–99 persons/square mile, and frontier counties, <6 persons/square mile.23
Because detailed information about drug use, mental health and referral to treatment had not been previously abstracted in the PMRC database, we performed a detailed review of all available data sources for each woman with pregnancy-associated drug-induced death. Sources were reviewed to determine if drug-related concerns were noted in prenatal/postpartum records and delivery records (depending on timing of death). A drug-related concern was defined as any documentation of illicit drug use, misuse of prescribed medications or referral to substance use treatment. We noted any evidence of co-existing co-morbidities (e.g. chronic pain, obesity, asthma), mental health conditions (e.g. depression, anxiety, schizophrenia, bipolar disorder), domestic violence/intimate partner violence, or history of abuse/trauma. Among women with postpartum deaths, all records were reviewed for a notation of involvement of the Department of Child and Family Services (DCFS) and the custody of the child at the time of death. We assessed for DCFS involvement for two reasons: 1) prenatal illicit drug use or prescribed drug misuse triggers a mandatory referral for DCFS investigation in Utah once delivery occurs and 2) removal of an infant from maternal custody is considered a major destabilizing event that could lead to drug overdose and death. We further assessed characteristics based on whether the death was determined to be accidental (including organ failure exacerbated by drug use), intentional or could not be determined.
P values of < 0.05 were considered statistically significant. Analyses were performed using Stata 14.0 (College Station, Texas). The Institutional Review Boards of the University of Utah and the Utah Department of Health reviewed and approved this study.
Results
During the ten-year span of this study (January 2005 - December 2014), a total of 136 pregnancy-associated deaths, of which 69 were pregnancy-related deaths, were identified in Utah. During the same time interval, there were 526,333 live births and 2776 fetal deaths. From 2005–2014, the three most common causes of pregnancy-associated deaths were drug-induced death (n=35/136, 26%), thromboembolic disease (n=18/136, 13%) and motor vehicle accidents (n=17/136, 12%). The remainder of pregnancy-associated deaths (n=66, 49%) were due to cardiac conditions, hypertension, infection, homicide/suicide, hemorrhage, malignancy and other causes. The annual proportion of pregnancy-associated deaths that were drug-induced ranged from 17 – 47%, with nadir in 2007 (8%) and peak (47%) in 2010. The pregnancy-associated mortality ratio increased 76%, from 23.3 in 2005 to 41.0 in 2014. During this same time period, the drug-induced pregnancy-associated mortality ratio increased 200%, from 3.9 in 2005 to 11.7 in 2014.
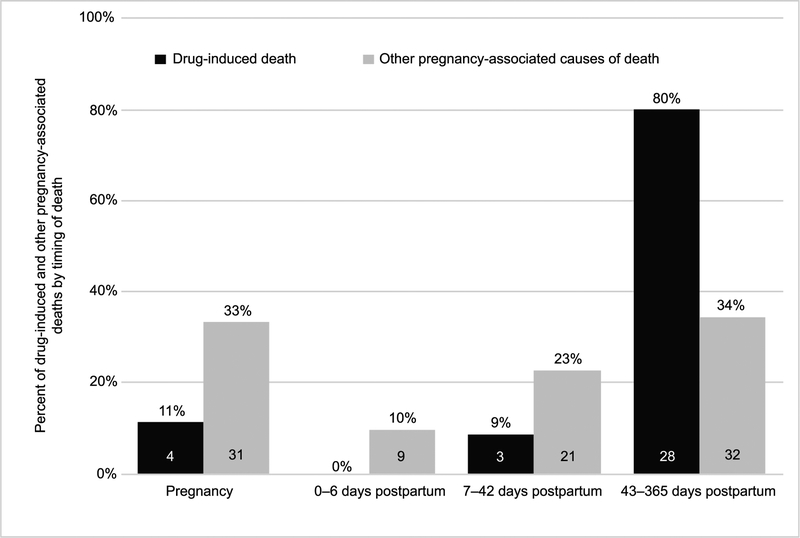
There were no significant differences in age, race/ethnicity, education level, parity, geographical location or number of prenatal visits between women with drug-induced and other pregnancy-associated deaths (Table 1). The distribution of the location of death was significantly different between drug-induced and other pregnancy-associated deaths (p<0.001); the majority of women with drug-induced deaths died at home (n=20/35, 57%) while women with other pregnancy-associated deaths died most frequently in the hospital (n=64/101, 63%). Women whose deaths were drug-induced were more likely to have died after delivery (n=31/35, 89%) compared to those whose deaths were from other pregnancy-associated causes (n=62/101, 61%) (p=0.01). More specifically, those with a drug-induced death were more likely to die in the late postpartum period (n=28/35, 80%) compared to women whose deaths were from other pregnancy-associated causes (n=34/101, 34%) (p<0.001) (Figure 1).
Table 1:
Characteristics of women with drug-induced deaths compared to women with other pregnancy-associated causes of death in Utah, 2005–2014
| Drug-induced (n=35) |
Other Pregnancy-Associated Causes (n=101) |
p-value* | |
|---|---|---|---|
| Race/Ethnicity | 0.08 | ||
| White, non-Hispanic | 29 (82.9) | 64 (63.4) | |
| Other, non-Hispanic | 3 (8.6) | 11 (10.9) | |
| Hispanic | 3 (8.6) | 25 (24.8) | |
| Unknown | 0 | 1 (1.0) | |
| Age (years) | 0.54 | ||
| 15–19 | 2 (5.7) | 5 (4.9) | |
| 20–34 | 28 (80.0) | 72 (71.3) | |
| ≥35 | 5 (14.3) | 23 (22.8) | |
| Unknown | 0 | 1 (1.0) | |
| Education | 0.34 | ||
| Less than high school | 6 (17.1) | 17 (16.8) | |
| High school graduate | 16 (45.7) | 31 (30.7) | |
| Some College | 9 (25.7) | 31 (30.7) | |
| College graduate | 4 (11.4) | 22 (21.8) | |
| Parity | 0.66 | ||
| 0 | 12 (34.3) | 25 (24.8) | |
| >=1 | 18 (51.4) | 62 (61.4) | |
| Unknown | 5 (14.3) | 14 (13.9) | |
| Initiation of Prenatal Care | 0.14 | ||
| Trimester (< 13 weeks) | 20 (57.1) | 57 (56.4) | |
| Trimester (13–27 weeks) | 8 (22.9) | 20 (19.8) | |
| Trimester (≥28 weeks) | 3 (8.6) | 1 (1.0) | |
| No Prenatal Care | 1 (2.9) | 6 (5.9) | |
| Unknown | 3 (8.6) | 17 (16.8) | |
| Number of prenatal visits (median, IQR) | 7 (4,11) | 10 (6,11) | 0.16 |
| Unknown n (%) | 4 (11.4) | 21 (20.8) | |
| Geographical region of death | 0.52 | ||
| Urban | 28 (80.0) | 86 (85.2) | |
| Rural | 6(17.1) | 12 (11.8) | |
| Frontier | 1 (2.9) | 1 (1.0) | |
| Unknown | 0 (0) | 2 (2.0) | |
| Location of death | <0.001 | ||
| Home | 20 (57.1) | 16 (15.8) | |
| Hospital | 9 (25.7) | 64 (63.4) | |
| Outpatient Clinic | 0 (0) | 3 (3.0) | |
| Unknown | 6 (17.1) | 18 (17.8) | |
| Timing of Death | 0.01 | ||
| During pregnancy | 4 (11.4) | 31 (30.7) | |
| Postpartum | 31 (88.6) | 62 (61.4) | |
| Unknown | 0 (0) | 8 (7.9) |
IQR, interquartile range
Figure 1:
Proportion of pregnancy-associated drug-induced deaths compared to all pregnancy-associated deaths 2005-–2014, n=136.
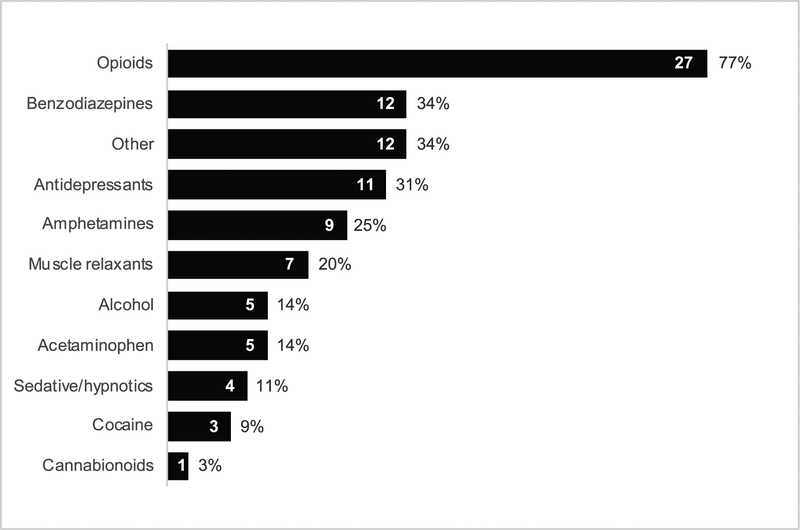
Of the 35 women with drug-induced deaths, 54% (19/35) were accidental overdoses, 26% (9/35) were intentional overdoses and 20% (7/35) could not be determined (Table 2). Four women died while pregnant: 2 during the first trimester (one accidental, one intentional) and 2 during the second trimester (both accidental). The majority of women had an autopsy performed (n=30/35, 85%), which confirmed drug-induced causes of death. Medical examiner’s reports and toxicology reports identified a variety of drugs (Figure 2). Nearly three-quarters of deaths (n=27/35, 77%) were opioid-related; 60% (n=21/35) were prescription opioid-related. Illicit drugs were present in 40% (n=14/35) of drug-induced deaths. Methadone was attributed to the cause of death among six women (17%); 2 women were receiving methadone for chronic pain and 4 women apparently obtained it illicitly. Polysubstance use was involved in 83% (n=29/35) of women with a drug-induced death (Table 3). The majority of women (n=29/35, 83%) had more than one substance identified: 17% of women had two substances noted (n=6/35) and 66% of women had three or more substances (n=23/35) (range 3–7 substances).
Table 2:
Characteristics of women with drug-induced pregnancy-associated deaths in Utah (n=35), 2005–2014
| Characteristics | Total | Accidental | Intentional | Could Not Be Determined |
|---|---|---|---|---|
| N =35 | N=19 | N=9 | N=7 | |
| Age (years) | ||||
| 15–19 | 2 (5.7) | 1 (5.3) | 1 (11.1) | 0 (0) |
| 20–34 | 28 (80.0) | 16 (84.2) | 7 (77.8) | 5 (71.4) |
| ≥35 | 5 (14.3) | 2 (10.5) | 1 (11.1) | 2 (28.6) |
| Married | 17 (48.6) | 9 (47.4) | 5 (55.6) | 3 (42.9) |
| Medicaid at delivery | 16 (45.7) | 7 (36.8) | 7 (77.8) | 2 (28.6) |
| Drug misuse or substance use disorder | 19 (54.2) | 9 (47.4) | 6 (66.7) | 4 (44.4) |
| Chronic pain | 15 (42.9) | 11 (57.9) | 3 (33.3) | 1 (14.2) |
| Obesity | 13 (37.1) | 11 (57.9) | 0 (0) | 2 (28.6) |
| Mental health diagnosis | 27 (77.1) | 14 (73.7) | 9 (100.0) | 4 (57.1) |
| Depression | 24 (69) | 12 (63.2) | 9 (100.0) | 3 (42.9) |
| Anxiety | 19 (54.2) | 10 (52.6) | 7 (77.8) | 2 (28.6) |
| Schizophrenia | 1 (2.9) | 0 (0) | 0 (0) | 1 (14.3) |
| Bipolar | 2 (5.7) | 1 (5.3) | 0 (0) | 1 (14.3) |
| Prior suicide attempt | 8 (22.9) | 3 (15.8) | 5 (55.6) | 0 (0) |
| Prior overdose | 9 (25.7) | 6 (31.6) | 3 (33.3) | 0 (0) |
| Prior mental health hospitalization | 6 (17.1) | 1 (5.3) | 4 (44.4) | 1 (14.3) |
| History of lifetime abuse (emotional, mental, physical, sexual) | 9 (25.7) | 4 (21.1) | 4 (44.4) | 1 (14.3) |
| Intimate partner violence | 6 (17.1) | 2 (11.1) | 3 (33.3) | 1 (14.3) |
| Mental health services documented | 9 (25.7) | 4 (21.1) | 4 (44.4) | 1 (14.3) |
| Social work referral documented | 14 (40.0) | 8 (42.1) | 5 (55.6) | 1 (14.3) |
| Prenatal care record | N=26 | N=14 | N=8 | N=4 |
| Drug-related concern in prenatal chart | 21 (60.0) | 11 (57.9) | 7 (77.8) | 3 (42.9) |
| Delivery care record | N=24 | N=13 | N=7 | N=4 |
| Drug-related concern in delivery record (n=24) | 18 (75.0) | 10 (76.9) | 5 (71.4) | 3 (75.0) |
| Number of infants | N=31 | N=17 | N=9 | N=5 |
| Department of Child and Protective Services involvement | 7 (22.5) | 2 (11.8) | 5 (55.6) | 0 (0) |
| Maternal custody of infant at delivery | 17 (54.8) | 11 (64.7) | 4 (44.4) | 2 (40.0) |
Figure 2:
Frequency of drugs attributed to maternal deaths in Utah. Opioids includes morphine (heroin metabolite), methadone, oxycodone, hydrocodone. Other includes dextromethorphan, inhaled gas, salicylate, non-steroidal anti-inflammatory medications, antihistamines (doxylamine, promethazine, diphenhydramine), caffeine. Categories are not mutually exclusive.
Table 3:
Drug types identified among women with more than one drug identified at death
| Drug type | Polysubstance use (n=29) |
|---|---|
| N (%) | |
| Opioids | 25 (86) |
| Benzodiazepines | 12 (41) |
| Anti-depressants | 11 (38) |
| Muscle relaxants | 7 (24) |
| Acetaminophen | 4 (14) |
| Amphetamines | 8 (28) |
| Alcohol | 5 (17) |
| Z drugs | 4 (14) |
| Other | 10 (34) |
Z drugs are non-benzodiazepine drugs including zolpidem, zaleplon, eszoplicone and zopiclone. Other includes dextromethorphan, non-steroidal anti-inflammatory medications, antihistamines (doxylamine, promethazine, diphenhydramine), caffeine.
The majority of women had known drug misuse (illicit drug use or misuse of prescription drugs during pregnancy) or substance use disorder (n=19/35, 54%) (Table 1). Most also had a mental health condition (n=27, 77%), most frequently depression (n=24, 69%) and/or anxiety (n=19, 54%). More than one in five women had a prior suicide attempt (n=8/35, 22%) and among those with an intentional death, over half had a history of suicide attempt (n=5/9, 56%. In the prenatal (n=26) and delivery records (n=24) that were available, no woman was documented as having been screened for drug use with a validated screening tool during prenatal, delivery or postpartum care. The majority of women did have drug-related concerns (e.g. active use, concern for relapse if in recovery or concerns regarding prior drug use history) noted in their prenatal (60%) and delivery (75%) records. Information about drug-related concerns was primarily based on self-disclosure, prior DCFS case notes, criminal justice system involvement, or drug-related health complications (e.g., endocarditis due to intravenous drug use). Despite active or previous drug use, fewer than half received a social work consultation (n=14/35, 40%) or mental health services (n=9/35, 26%). None of the women received pharmacotherapy (buprenorphine or methadone) for opioid use disorder. Alarmingly, while a quarter of women with a drug-induced death had a previous history of overdose, none of the women with drug-induced deaths had documented either counseling regarding prevention of overdose or prescription for naloxone rescue medication. More than one in five women who died due to drug-induced causes had a prior suicide attempt, although suicide prevention and crisis hotline counseling was not documented in the prenatal or delivery records.
Of the 31 women who died in the postpartum period, fewer than a quarter had DCFS involvement and more than half of infants were discharged to their mother’s custody (n=17, 55%). The majority of women did not have a postpartum visit (n=18, 58%). Of those 13 who did have a postpartum visit, all died at least two months after their last contact with their obstetrical provider.
After case review at the Utah PMRC, 85% (n=30/35) of the drug-induced pregnancy-associated deaths were deemed not preventable typically because they occurred after the six week postpartum visit. For those deaths that were deemed preventable, the PMRC recommended systematic screening for substance use and clearer linkage to mental health and substance use treatment as strategies to prevent these deaths.
Discussion
Drug-induced death is the leading cause of pregnancy-associated death in Utah. It accounts for the same proportion of pregnancy-associated deaths as the next two most frequent causes, thromboembolic disease and motor vehicle accidents, combined. Nearly three-quarters of drug-induced deaths were opioid-related and the majority involved polysubstance use and prescription opioids. In 2010, the peak of drug-induced pregnancy-associated deaths in Utah corresponded to an increase in heroin-related deaths nationwide.4 During our study period, the pregnancy-associated mortality ratio increased 76% and the drug-induced pregnancy-associated mortality ratio increased 200%. Detailed review of available records demonstrated that 1) women were not systematically screened for drug use using validated screening tools, 2) despite known mental health and drug misuse, most women did not receive mental health or drug treatment, 3) none were receiving pharmacotherapy (buprenorphine or methadone) for opioid use disorder, and, 4) women with a drug-induced pregnancy-associated death died primarily in the late postpartum period, after they had stopped seeing their obstetrical providers.
Our results corroborate other studies that have found that the highest risk of drug-induced death is in the late postpartum period.14,16,24,25 In Georgia (2010–2012), all 26 women who died due to drug toxicity died in the postpartum period and 77% died in the late postpartum period.25 In Maryland, all deaths in 2015 attributable to drug-induced causes were in the postpartum period.24 Schiff et al. found that among pregnant and postpartum women with opioid use disorder, those receiving pharmacotherapy had reduced rates of overdose deaths, particularly in the late postpartum period.14 In our cohort, most women with a drug-induced death were not receiving any kind of drug or mental health treatment, representing a missed opportunity for potentially life-saving interventions.
From 2005–2014, the Utah PMRC deemed 85% of drug-induced pregnancy-associated deaths unpreventable. However, there is recognition that pregnancy and the postpartum period are associated with either new onset or exacerbation of underlying health conditions including depression, anxiety, chronic pain and substance use disorders. Based on the results of this study, and the evolving recognition that mental health conditions appear to be aggravated by pregnancy and delivery, the Utah PMRC has elected to classify drug-induced deaths as pregnancy-related from 2015 onward. The evolving definition of pregnancy-related deaths to include those that are drug-induced is currently undergoing evaluation at national maternal mortality meetings and may be implemented among other states with Maternal Mortality Review Committees.20 This may impact the determination of preventability of these drug-induced deaths, including increased awareness of and screening for drug use in pregnancy and postpartum, improved access to mental health and addiction services and increased support of new mothers extending past the standard six-week postpartum visit.
Recently, the American College of Obstetricians and Gynecologists (ACOG) and the Council on Patient Safety in Women’s Health safety bundle committee have published recommendations for the care of pregnant and postpartum women with opioid use disorders.26,27 A parallel committee opinion was recently published by ACOG on reconceptualization of postpartum care as the extended “fourth trimester.”28 ACOG stresses that continued engagement and coordinated care for women with pre-existing conditions, including substance use disorder and mental health conditions, is imperative for reduction of severe maternal morbidity and mortality.29 Our findings highlight that the postpartum period is a critical period for women with substance use disorders. For postpartum women struggling with drug use, the demands of a newborn, loss of continuity with trusted providers, loss of insurance, increased risk of postpartum depression and anxiety, and sleep deprivation may result in the ‘perfect storm’ leading to drug use, relapse, overdose and death.26,30,31
The strength of our study is the detailed analysis of all records available for women with drug-induced deaths. The proportion of women with drug-induced deaths with prior suicide attempt or previous overdose was higher than reported in other studies.14,30,31 Many of these events did not occur in the hospital and women did not seek immediate treatment, and therefore would not appear in administrative databases.14 One unique contribution of our study is assessment of obstetrical provider awareness of drug misuse prior to a drug-induced death. Indeed, the majority of women had known drug misuse or substance use disorder, however, a substantial proportion (46%) of women with drug-induced deaths had no known drug use noted during obstetrical care. Systematic screening for drug use may have been able to identify these women and represents another missed opportunity for intervention.26,27,32
Our study has notable limitations. We were not able to capture insurance status or coverage lapses systematically. We were also not able to determine whether women had insurance at time of their death, or if insurance status was a barrier in accessing mental health or addiction specialists. In our cohort, abuse and intimate partner violence were lower than other populations of women with substance use disorders,33 likely representing a lack of systematic screening in prenatal and postpartum care and another opportunity of intervention. Classification bias (changing definitions or understandings over time) and missed cases (not capturing all maternal deaths due to emigration or unknown pregnancy status) may exist. Maternal deaths linked to unreported miscarriage or abortions may not have been identified in this process. Comprehensive records were not available for all women. Additionally, women may have sought care from providers we were unable to identify. However, our chart review likely provides more detailed information about drug-related concerns in prenatal and delivery care, referral to DCFS and attempts to link women with mental health services than is typically available in administrative data.
Our results support the mounting evidence that pregnant, and particularly postpartum, women with history of drug use and overdose, psychiatric co-morbidities, prior suicide attempt, and polysubstance use need enhanced and ongoing care. Our results, and those of others, provide an impetus to explore interventions in this vulnerable time to reduce pregnancy-associated deaths, including systematic screening for drug use during pregnancy and postpartum period, relapse prevention counseling, naloxone prescription, and ensuring transition to and continuity of care with substance use and mental health care specialists. Prospective studies are needed to understand the context in which drug use, relapse and overdose occurs among pregnant and postpartum women. These studies are urgently needed to develop effective strategies to reduce the catastrophic event of maternal death.
Supplementary Material
Acknowledgments
Marcela C. Smid is supported by Women’s Reproductive Health Research (WRHR K12, 1K12 HD085816) Career Development Program.
Footnotes
Presented in part as a poster at the Society of Maternal Fetal Medicine January 29-February 3, 2018 meeting (Dallas, TX).
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has confirmed compliance with the journal’s requirements for authorship.
Peer Review History
Peer reviews and author correspondence are available at http://links.lww.com/xxx.
References
- 1.Center for Disease Control and Prevention. Annual Surveillance Report of Drug-Related Risks and Outcomes — United States, 2017 . In. Vol Surveillance Special Report 1. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2017. [Google Scholar]
- 2.Murphy SL, Xu J, Kochanek KD, Curtin SC, Arias E. Deaths: Final Data for 2015. Natl Vital Stat Rep. 2017;66(6):1–75. [PubMed] [Google Scholar]
- 3.Hedegaard H, Warner M, Minino AM. Drug Overdose Deaths in the United States, 1999–2015. NCHS data brief. 2017(273):1–8. [PubMed] [Google Scholar]
- 4.Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(5051):1445–1452. [DOI] [PubMed] [Google Scholar]
- 5.Haight SC. Opioid Use Disorder Documented at Delivery Hospitalization—United States, 1999–2014. MMWR Morbidity and mortality weekly report. 2018;67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bateman BT, Hernandez-Diaz S, Rathmell JP, et al. Patterns of opioid utilization in pregnancy in a large cohort of commercial insurance beneficiaries in the United States. The Journal of the American Society of Anesthesiologists. 2014;120(5):1216–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desai RJ, Hernandez-Diaz S, Bateman BT, Huybrechts KF. Increase in prescription opioid use during pregnancy among Medicaid-enrolled women. Obstet Gynecol. 2014;123(5):997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Center for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) (2013–2015). . In: National Center for Injury Prevention and Control, CDC; January. [Google Scholar]
- 9.Program UVIP. Prescription Drug Overdoses. In: Utah Department of Health; 2018. [Google Scholar]
- 10.Forray A, Merry B, Lin H, Ruger JP, Yonkers KA. Perinatal substance use: a prospective evaluation of abstinence and relapse. Drug Alcohol Depend. 2015;150:147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ebrahim SH, Gfroerer J. Pregnancy-related substance use in the United States during 1996–1998. Obstet Gynecol. 2003;101(2):374–379. [DOI] [PubMed] [Google Scholar]
- 12.Massey SH, Lieberman DZ, Reiss D, Leve LD, Shaw DS, Neiderhiser JM. Association of clinical characteristics and cessation of tobacco, alcohol, and illicit drug use during pregnancy. The American journal on addictions. 2011;20(2):143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fitzsimons HE, Tuten M, Vaidya V, Jones HE. Mood disorders affect drug treatment success of drug-dependent pregnant women. J Subst Abuse Treat. 2007;32(1):19–25. [DOI] [PubMed] [Google Scholar]
- 14.Schiff DM, Nielsen T, Terplan M, et al. Fatal and Nonfatal Overdose Among Pregnant and Postpartum Women in Massachusetts. Obstet Gynecol. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gemmill A, Kiang MV, Alexander MJ. Trends in pregnancy-associated mortality involving opioids in the United States, 2007–2016. Am J Obstet Gynecol. 2019;220(1):115–116. [DOI] [PubMed] [Google Scholar]
- 16.Metz TD, Rovner P, Hoffman MC, Allshouse AA, Beckwith KM, Binswanger IA. Maternal Deaths From Suicide and Overdose in Colorado, 2004–2012. Obstet Gynecol. 2016;128(6):1233–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bagley SM, Cabral H, Saia K, et al. Frequency and associated risk factors of non-fatal overdose reported by pregnant women with opioid use disorder. Addict Sci Clin Pract. 2018;13(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reviewtoaction.org. Definitions. http://www.reviewtoaction.org/learn/definitions. Published 2018. Accessed August 8th, 2018.
- 19.Prevention CfDCa. Pregnancy Mortality Surveillance System. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-mortality-surveillance-system.htm. Published 2018. Accessed August 8th 2018.
- 20.Prevention CfDCa. Report from Maternal Mortality Review Commitees: A View Into Their Critical Roles. In:2017.
- 21.Health UDo, Services H. Facing addiction in America: The Surgeon General’s report on alcohol, drugs, and health. Washington, DC: HHS; 2016:6. [PubMed] [Google Scholar]
- 22.Murphy SL, Xu J, Kochanek KD, Curtin SC, Arias E. Deaths: final data for 2015. 2017. [PubMed]
- 23.Health UOoPCaR. Shortage Area Designations. In: Health UDo, ed 2018. [Google Scholar]
- 24.Administration MDoHaMHPaHP. Maryland Maternal Mortality Review: 2016 Annual Report. 2016.
- 25.Platner M, Loucks TL, Lindsay MK, Ellis JE. Pregnancy-Associated Deaths in Rural, Nonrural, and Metropolitan Areas of Georgia. Obstet Gynecol. 2016;128(1):113–120. [DOI] [PubMed] [Google Scholar]
- 26.Committee Opinion No. 711: Opioid Use and Opioid Use Disorder in Pregnancy. Obstet Gynecol. 2017;130(2):e81–e94. [DOI] [PubMed] [Google Scholar]
- 27.Obstetric Care for Women with Opioid Use Disorder. 2017. http://safehealthcareforeverywoman.org/patient-safety-bundles/obstetric-care-for-women-with-opioid-use-disorder/. Accessed Novermber 25th, 2017.
- 28.ACOG Committee Opinion No. 736: Optimizing Postpartum Care. Obstet Gynecol. 2018;131(5):e140–e150. [DOI] [PubMed] [Google Scholar]
- 29.Declercq ER, Sakala C, Corry MP, Applebaum S, Herrlich A. Major Survey Findings of Listening to MothersSM III: Pregnancy and Birth: Report of the Third National US Survey of Women’s Childbearing Experiences. The Journal of perinatal education. 2014;23(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Terplan M, Smith EJ, Kozloski MJ, Pollack HA. Methamphetamine use among pregnant women. Obstet Gynecol. 2009;113(6):1285–1291. [DOI] [PubMed] [Google Scholar]
- 31.Wright TE, Schuetter R, Tellei J, Sauvage L. Methamphetamines and pregnancy outcomes. J Addict Med. 2015;9(2):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Madsen AM, Stark LM, Has P, Emerson JB, Schulkin J, Matteson KA. Opioid Knowledge and Prescribing Practices Among Obstetrician–Gynecologists. Obstet Gynecol. 2018;131(1):150–157. [DOI] [PubMed] [Google Scholar]
- 33.Brogly SB, Saia KE, Werler MM, Regan E, Hernández-Díaz S. Prenatal Treatment and Outcomes of Women With Opioid Use Disorder. Obstet Gynecol. 2018;132(4):916–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.