Abstract
Objectives
To identify maternal plasma protein markers for early preeclampsia (delivery <34 weeks of gestation) and to determine whether the prediction performance is affected by disease severity and presence of placental lesions consistent with maternal vascular malperfusion (MVM) among cases.
Study design
This longitudinal case-control study included 90 patients with a normal pregnancy and 33 patients with early preeclampsia. Two to six maternal plasma samples were collected throughout gestation from each woman. The abundance of 1,125 proteins was measured using high-affinity aptamer-based proteomic assays, and data were modeled using linear mixed-effects models. After data transformation into multiples of the mean values for gestational age, parsimonious linear discriminant analysis risk models were fit for each gestational-age interval (8–16, 16.1–22, 22.1–28, 28.1–32 weeks). Proteomic profiles of early preeclampsia cases were also compared to those of a combined set of controls and late preeclampsia cases (n = 76) reported previously. Prediction performance was estimated via bootstrap.
Results
We found that 1) multi-protein models at 16.1–22 weeks of gestation predicted early preeclampsia with a sensitivity of 71% at a false-positive rate (FPR) of 10%. High abundance of matrix metalloproteinase-7 and glycoprotein IIbIIIa complex were the most reliable predictors at this gestational age; 2) at 22.1–28 weeks of gestation, lower abundance of placental growth factor (PlGF) and vascular endothelial growth factor A, isoform 121 (VEGF-121), as well as elevated sialic acid binding immunoglobulin-like lectin 6 (siglec-6) and activin-A, were the best predictors of the subsequent development of early preeclampsia (81% sensitivity, FPR = 10%); 3) at 28.1–32 weeks of gestation, the sensitivity of multi-protein models was 85% (FPR = 10%) with the best predictors being activated leukocyte cell adhesion molecule, siglec-6, and VEGF-121; 4) the increase in siglec-6, activin-A, and VEGF-121 at 22.1–28 weeks of gestation differentiated women who subsequently developed early preeclampsia from those who had a normal pregnancy or developed late preeclampsia (sensitivity 77%, FPR = 10%); 5) the sensitivity of risk models was higher for early preeclampsia with placental MVM lesions than for the entire early preeclampsia group (90% versus 71% at 16.1–22 weeks; 87% versus 81% at 22.1–28 weeks; and 90% versus 85% at 28.1–32 weeks, all FPR = 10%); and 6) the sensitivity of prediction models was higher for severe early preeclampsia than for the entire early preeclampsia group (84% versus 71% at 16.1–22 weeks).
Conclusion
We have presented herein a catalogue of proteome changes in maternal plasma proteome that precede the diagnosis of preeclampsia and can distinguish among early and late phenotypes. The sensitivity of maternal plasma protein models for early preeclampsia is higher in women with underlying vascular placental disease and in those with a severe phenotype.
Introduction
Preeclampsia is a major obstetrical syndrome [1–3], classified according to the time of its clinical manifestation as “early preeclampsia” if it occurs prior to 34 weeks of gestation and, otherwise, as “late preeclampsia” [4–10]. The 34-week cut-off is most commonly used [9,11,12] given the substantial decline in maternal [6,13–17] and neonatal [8,13,18–24] morbidity compared to later gestational ages.
Early preeclampsia accounts for approximately 10% of the cases [8], and its pathophysiology involves both maternal predisposing factors and disorders of deep placentation [25,26]. Indeed, in early preeclampsia, the frequency of placental vascular lesions consistent with maternal vascular malperfusion (MVM) is higher than in late preeclampsia [27–30], suggesting that the underlying pathological processes leading to this phenotype begin in the early stages of gestation and involve an angiogenic imbalance [11,31–37]. This finding has clinical implications given that patients identified to be at risk by the end of the first trimester can benefit from treatment [38–41].
Current prediction models for preeclampsia combine maternal risk factors, Doppler velocimetry of the uterine arteries, and maternal blood proteins [32,37,42–46]. Although the detection rate of these models [12,47–50] for the identification of patients at risk for early/preterm preeclampsia is sufficient to enable preventive strategies [40], the contribution of biochemical markers in these models is limited. Moreover, Doppler velocimetry required in the current screening models [47,51–57] to compensate for the sub-optimal prediction by biochemical markers may not be available in all clinical settings.
Therefore, we used a novel high-affinity aptamer-based proteomic platform to identify longitudinal changes in maternal plasma proteins that have the potential to improve prediction of early preeclampsia and to distinguish between the early and late phenotypes. We also investigated whether the predictive performance of protein markers is impacted by disease severity and the presence of placental lesions consistent with MVM among cases.
Materials and methods
Study design
A nested case-control study was conducted, including patients diagnosed with early preeclampsia (cases, n = 33) and those with a normal pregnancy (controls, n = 90). Women were enrolled as participants of a longitudinal cohort study conducted at the Center for Advanced Obstetrical Care and Research of the Perinatology Research Branch, NICHD/NIH/DHHS, the Detroit Medical Center, and Wayne State University. Women with a multiple gestation, severe chronic maternal morbidity (i.e., renal insufficiency, congestive heart disease, and/or chronic respiratory insufficiency), acute maternal morbidity (i.e., asthma exacerbation requiring systemic steroids and/or active hepatitis), or fetal chromosomal abnormalities and congenital anomalies were excluded from the study.
Plasma samples were collected at the time of each prenatal visit scheduled at four-week intervals from the first or early second trimester until delivery. All patients provided written informed consent prior to sample collection. The plasma proteome of each patient was profiled in two to six samples collected from each patient and included, for some of the cases, the sample collected after the diagnosis of early preeclampsia. Although data collected after diagnosis are displayed in longitudinal plots, all analyses reported herein were based only on samples collected prior to the diagnosis [median (interquartile range or IQR) of 3 (2–4) for cases and 2 (2–5) for controls].
The analysis presented in this manuscript is based on data and specimens collected under the protocol entitled “Biological Markers of Disease in the Prediction of Preterm Delivery, Preeclampsia and Intra-Uterine Growth Restriction: A Longitudinal Study.” The study was approved by the Institutional Review Boards of Wayne State University (WSU IRB#110605MP2F) and NICHD/NIH/DHHS (OH97-CH-N067).
Clinical definitions
Preeclampsia was defined as new-onset hypertension that developed after 20 weeks of gestation (systolic or diastolic blood pressure ≥140 mm Hg and/or ≥90 mm Hg, respectively, measured on at least two occasions, 4 hours to 1 week apart) and proteinuria (≥300 mg in a 24-hour urine collection, or two random urine specimens obtained 4 hours to 1 week apart containing ≥1+ by dipstick or one dipstick demonstrating ≥2+ protein) [58].
Early preeclampsia was defined as preeclampsia diagnosed and delivered before 34 weeks of gestation, and late preeclampsia was defined as preeclampsia delivered at or after 34 weeks of gestation [4]. Severe preeclampsia was diagnosed as preeclampsia with systolic blood pressure ≥ 160 mmHg, or diastolic blood pressure ≥ 110 mmHg, platelet count < 100,000 per mm3, elevated liver enzymes, renal insufficiency, pulmonary edema or cyanosis, new-onset cerebral/visual disturbances, and/or right upper quadrant or epigastric pain [9,59].
Histologic placental examination
Placentas were examined according to standardized protocols by perinatal pathologists blinded to clinical diagnoses and obstetrical outcomes, as previously described [60]. Placental lesions were diagnosed using criteria established by the Perinatal Section of the Society for Pediatric Pathology [61] and the terminology was updated to be consistent with that recommended by the Amsterdam Placental Workshop Group consensus statement [62]. The definitions of lesions consistent with MVM were previously described [63].
Proteomics analysis
Maternal plasma protein abundance was determined by using the SOMAmer (Slow Off-rate Modified Aptamer) platform and reagents to profile 1,125 proteins [64,65]. Proteomics profiling services were provided by Somalogic, Inc. (Boulder, CO, USA). The plasma samples were diluted and then incubated with the respective SOMAmer mixes, and after following a suite of steps described elsewhere [64,65], the signal from the SOMAmer reagents was measured using microarrays.
Statistical analysis
Demographics data analysis
Clinical characteristics of the patient population were summarized as median and IQRs for continuous variables or as percentages for categorical variables. The comparison of demographic variables between the groups was performed using the Fisher’s exact test for binary variables and the Wilcoxon rank-sum test for continuous variables.
Proteomic data transformation
The raw protein abundance data consisted of relative fluorescence units obtained from scanning the microarrays with a laser scanner. A sample-by-sample adjustment in the overall signal within a single plate (85 samples processed per plate/run) was performed in three steps: Hybridization Control Normalization, Median Signal Normalization, and Calibration, using the manufacturer’s protocol. Outlier values (larger than 2×the 98th percentile of all samples) were set to 2×the 98th percentile of all samples (data thresholding). Protein abundance was then log2 transformed to improve normality. Linear mixed-effects models with cubic splines (number of knots = 3) were used to model protein abundance in the control group as a function of gestational age using the lme4 package [66] under the R statistical language and environment (www.r-project.org). Data for all samples were then expressed as multiple of the mean (MoM) values for the corresponding gestational age in the normal pregnancy group. Longitudinal protein abundance averages and confidence intervals in sub-groups (MVM vs non-MVM, and severe vs mild preeclampsia) were estimated using generalized additive mixed models implemented in the mgcv package and illustrated using ggplot2 package in R.
Development of multi-marker prediction models
To develop proteomics prediction models based on protein abundance collected in each gestational-age interval (8–16, 16.1–22, 22.1–28, 28.1–32, 32.1–36 weeks) and, at the same time, to obtain unbiased prediction performance estimates on the available dataset, we implemented advances in predictive modeling with omics data [67–69]. Log2 MoM values for one protein at a time were used to fit a linear discriminant analysis (LDA) model and to compute by leave-one-out cross-validation, a classification performance measure for each protein. With leave-one-out cross-validation, data from one patient at a time is left out when fitting the LDA model, and then the fitted model is applied to the data of the subject left out. The resulting predictions were combined over all patients to calculate prediction performance. The performance measure considered was the partial area under the curve (pAUC) of the receiver operating characteristic (ROC) curve (false-positive rate [FPR] <50%). Proteins that failed to reach at least a 10% change in the average MoM value between the study groups were filtered out from the analysis. Next, LDA models were fit by using increasing sets of up to five of the top proteins ranked by the pAUC. To enforce model parsimony, the inclusion of each additional protein was conditioned on the increase of 0.01 units in the pAUC statistic.
To obtain an unbiased estimate of the prediction performance of multi-marker models, we used bootstrap (200 iterations). Each iteration involved the following steps: 1) draw a random sample with the replacement of 33 cases and 90 controls to create a training set and consider all patients not selected in the bootstrap sample as a test set; 2) apply all analytical steps involved in the prediction model development described above (including the selection of predictor proteins) for each gestational-age interval using the training set; 3) apply the resulting prediction model and determine its prediction performance on data from patients in the test set. The average performance over 200 test sets was reported as a robust estimate of the prediction performance. Alternatively, instead of creating training and test partitions via bootstrap, repeated (n = 67 times) 3-fold cross-validation was used to generate 201 training and test set pairs, while keeping all other parameters of the analysis the same as described above for bootstrap.
Differential abundance analysis
The classifier development pipeline described above identifies a parsimonious set of proteins that predict early preeclampsia, yet it will not necessarily retain all proteins showing evidence of differential abundance between groups. Therefore, a complementary analysis was performed to identify all proteins with significant differences in mean log2 MoM values between the cases and controls at each gestational-age interval. Linear models with coefficient significance evaluated via moderated t-tests were applied using the limma package [70] of Bioconductor [71]. Significance was inferred based on the FDR-adjusted p-value (q-value) <0.1 after adjusting for body mass index, smoking status, maternal age, and parity.
Both prediction model development and differential abundance analyses described above were also applied, including only controls and early preeclampsia cases i) with placental MVM lesions and ii) those with a severe phenotype.
Comparison between the proteomic profiles of early and late preeclampsia
To identify protein changes specific to early onset, but not late onset, of the disease, data from the early preeclampsia (n = 33) group were compared to a combined group that included both late preeclampsia cases (N = 76) [72] and normal pregnancies (n = 90).
Gene ontology and pathway analysis
Proteins were mapped to Entrez gene identifiers [73] based on Somalogic, Inc. annotation and, subsequently, to gene ontology [74]. Biological processes over-represented among the proteins that changed with early preeclampsia were identified using a Fisher’s exact test. Gene ontology terms with three or more hits and a q-value < 0.1 were considered significantly enriched. Identification of signaling pathways from the Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway database [75] that were enriched in proteins with differential abundance was performed using a pathway impact analysis method previously described [76,77]. The analysis was conducted using the web-based implementation available in iPathwayGuide (http://www.advaitabio.com). All enrichment analyses used, as reference, the set of all 1,125 proteins that were profiled on the Somalogic platform.
Results
In the early preeclampsia group, 33% (11/33) of the women delivered a small-for-gestational-age neonate, 73% (24/33) had placental lesions consistent with MVM and 70% (23/33) were severe cases. Cases were diagnosed from 24.6 to 33.4 weeks of gestation. Other characteristics of the study population classified by outcome and presence of placental MVM lesions are shown in Table 1.
Table 1. Demographic characteristics of the study population.
| Characteristic | Normal pregnancy (n = 90) | Early PE (n = 33) With MVM (n = 24) Without MVM (n = 9) |
|
|---|---|---|---|
| With MVM (n = 24) | With MVM (n = 24) Without MVM (n = 9) | ||
| Gestational age at enrolment (weeks) | 9.1 (8.0–10.1) | 10.4 (8.3–15.2) [p = 0.024] | 13.1 (8.4–14.6) [p = 0.042] |
| Gestational age at delivery (weeks) | 39.4 (39.0–40.4) | 31.2 (28.3–33.0) [p<0.001] | 33.4 (32.1–33.6) [p<0.001] |
| Body mass index (kg/m2) | 26.5 (22.8–33.2) | 26.3 (20.5–30.6) [p = 0.27] | 28.2 (22.3–32.9) [p = 0.62] |
| Maternal age (years) | 24 (21.0–27.8) | 22 (19.0–25.5) [p = 0.05] | 24 (22.0–30.0) [p = 0.88] |
| Smoking status | 18 (20%) | 5 (20.83%) [p = 1] | 5 (55.56%) [p = 0.03] |
| Nulliparity | 26 (28.9%) | 15 (62.5%) [p = 0.004] | 1 (11.11%) [p = 0.44] |
Data are presented as median (interquartile range) or number (percentage); P-values are given for the comparison to the normal pregnancy group. Early PE: early preeclampsia; MVM: maternal vascular malperfusion.
Proteomic prediction models for early preeclampsia by gestational age at blood draw
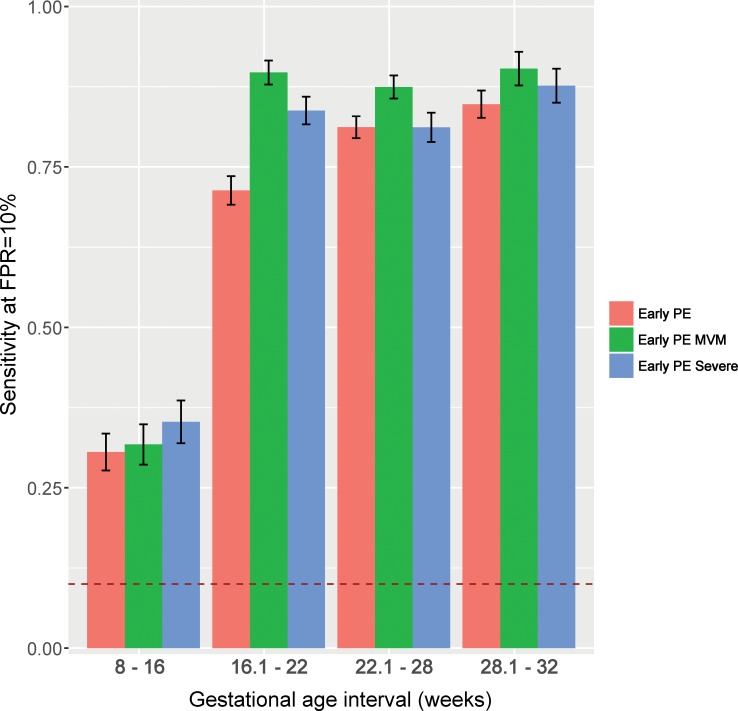
The prediction performance indices of the multi-marker models involving up to five proteins were estimated by bootstrap and are illustrated in Fig 1and Table 2. Fig 1presents the sensitivity (10% FPR) of multi-marker models for early preeclampsia at each gestational-age interval.
Fig 1. Sensitivity for early preeclampsia using multi-protein markers.
Sensitivity (y-axis) at a 10% FPR are shown by gestational-age interval (x-axis) for early preeclampsia (PE), early PE with placental lesions consistent with MVM, and severe early PE. The vertical bars represent the average (with 95% confidence intervals) of sensitivity obtained from 200 bootstrap iterations. Early PE: early preeclampsia; FPR: false-positive rate; MVM: maternal vascular malperfusion.
Table 2. Summary of bootstrap results for prediction of early preeclampsia vs normal pregnancy.
| Outcome | Sample GA | AUC | Sensitivity | Specificity | Predictor Symbols (% inclusion in best combination) |
|---|---|---|---|---|---|
| (weeks) | |||||
| 8–16 | 0.64 | 0.31 | 0.90 | MMP-7(42%), gpIIbIIIa(23%), HMG-1(10%), vWF(10%) | |
| All | 16.1–22 | 0.88 | 0.71 | 0.90 | MMP-7(90%), gpIIbIIIa(18%), Soggy-1(10%), |
| Early PE | 22.1–28 | 0.90 | 0.81 | 0.90 | Siglec-6(58%), PlGF(52%), Activin A(25%), VEGF121(18%) |
| 28.1–32 | 0.94 | 0.85 | 0.90 | ALCAM(38%), VEGF121(32%), Siglec-6(32%) | |
| 8–16 | 0.63 | 0.32 | 0.90 | MMP-7(33%), gpIIbIIIa(26%), ACE2(18%) | |
| Early PE | 16.1–22 | 0.96 | 0.90 | 0.90 | MMP-7(99%), |
| MVM | 22.1–28 | 0.95 | 0.87 | 0.92 | Siglec-6(76%), PlGF(21%), Activin A(14%) |
| 28.1–32 | 0.95 | 0.90 | 0.90 | Siglec-6(63%), VEGF121(33%), ALCAM(10%) | |
| 8–16 | 0.67 | 0.35 | 0.90 | MMP-7(44%); gpIIbIIIa(17%); Glutathione S-transferase Pi(12%); SMAC(10%); C4b(10%) | |
| Early PE | 16.1–22 | 0.94 | 0.84 | 0.90 | MMP-7(97%); gpIIbIIIa(14%) |
| Severe | 22.1–28 | 0.89 | 0.81 | 0.91 | Siglec-6(68%); PlGF(34%); VEGF121(24%); Activin A(14%) |
| 28.1–32 | 0.95 | 0.88 | 0.90 | Siglec-6(52%); VEGF121(26%); ALCAM(22%) |
The number in parentheses following the name of each protein (column Predictor Symbols) represents the percentage of bootstrap iterations in which the protein was selected in the best model. Only proteins selected in 10% or more of the 200 bootstrap iterations are listed. ACE2: angiotensin converting enzyme 2; ALCAM: activated leukocyte cell adhesion molecule; AUC: area under the receiver operating characteristic curve; GA: gestational age; gpIIbIIIa: glycoprotein IIb/IIIa; HMG-1: high-mobility group protein 1; MMP: matrix metalloproteinase; early PE: early preeclampsia; MVM: maternal vascular malperfusion; PE: preeclampsia; PlGF: placental growth factor; Siglec-6: sialic acid binding immunoglobulin-like lectin; VEGF121: vascular endothelial growth factor A, isoform 121; vWF: von Willebrand factor; SMAC: Diablo homolog, mitochondrial; C4b: Complement C4b.
At 8–16 weeks of gestation, multi-marker proteomics models predicted early preeclampsia with 31% sensitivity (FPR = 10%), which was higher than that of PlGF alone (17%). The importance of individual proteins in the prediction models was evaluated by the percentage of the 200 bootstrap iterations in which they were included in the best LDA prediction model. Matrix metalloproteinase 7 (MMP-7) and glycoprotein IIbIIIa (gpIIbIIIa) were chosen in the best model in 42% and 23% of the iterations, respectively, while high-mobility group protein 1 (HMG-1) and von Willebrand factor were selected in 10% of the iterations (Table 2). Individual patient longitudinal profiles of MMP-7 and gpIIbIIIa protein abundance are presented in Fig 2A and 2B, respectively.
Fig 2. Longitudinal maternal plasma abundance of MMP-7 and gpIIbIIIA in normal pregnancy and early preeclampsia.
Each line corresponds to a single patient (grey = normal pregnancy, red = early preeclampsia). Individual dots represent samples at 8–16 weeks (A, B) and 16.1–22 weeks (C, D) of gestation. Samples taken at the time of diagnosis with early preeclampsia are marked with an “x” and were not included in the analysis but only displayed. The thick black line represents the mean value in normal pregnancy. AUC: area under the receiver operating characteristic curve of the protein using data in the current interval; early PE: early preeclampsia; FC: fold change; gpIIbIIIa: glycoprotein IIb/IIIa; MMP-7: matrix metalloproteinase 7; MoM: multiples of the mean; p: the nominal significance p-value comparing mean MoM values between groups with a moderated t-test. Log2FC is the log (base 2) of the fold change between the cases and control groups, with negative values denoting lower MoM values in cases than in controls.
At 16.1–22 weeks of gestation, multi-marker prediction models identified women at risk to develop early preeclampsia with a sensitivity of 71% (FPR = 10%) which was again higher than the estimate for PlGF alone (18%). MMP-7, gpIIbIIIa, and Soggy-1 were selected in the best model 90%, 18%, and 10% of the time, respectively. The longitudinal profiles of MMP-7 and gpIIbIIIa, emphasizing the differences in the samples taken between 16.1 to 22 weeks of gestation, are presented in Fig 2C and 2D.
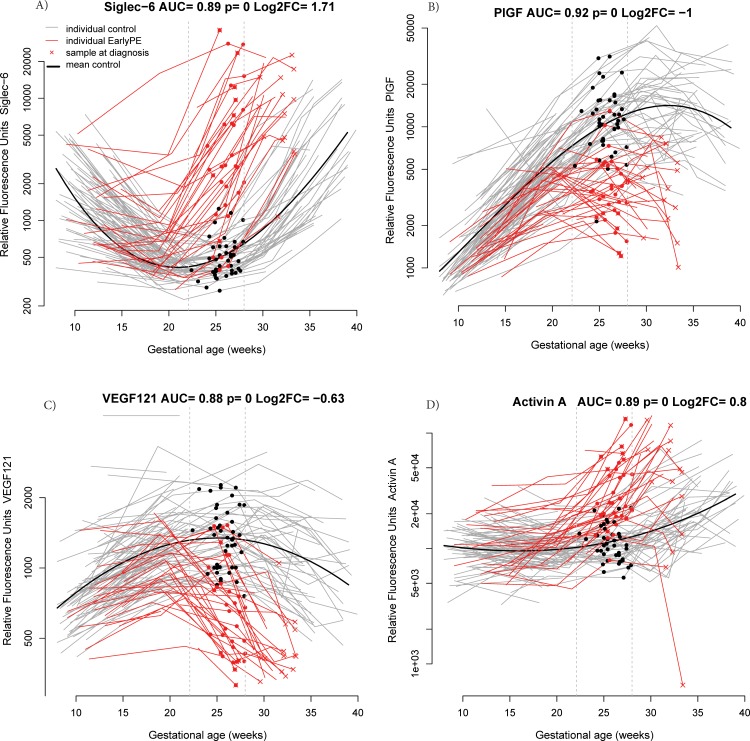
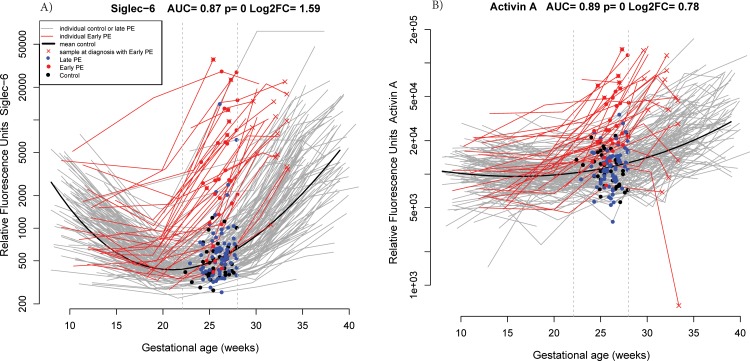
At 22.1–28 weeks of gestation, the proteins most often selected in the best risk model for early preeclampsia out of 200 bootstrap iterations were sialic acid binding immunoglobulin-like lectin 6 (siglec-6) (58%), PlGF (52%), activin-A (25%), and VEGF121 (18%). Longitudinal profiles of these four proteins emphasizing the differences in the samples taken between 22.1 and 28 weeks of gestation are shown in Fig 3.
Fig 3.
Longitudinal maternal plasma abundance of siglec−6 (A), PlGF (B), VEGF121 (C), and activin-A (D) in normal pregnancy and early preeclampsia cases, highlighting differences at 22.1–28 weeks. AUC: area under the receiver operating characteristic curve; early PE: early preeclampsia; FC: fold change; PlGF: placental growth factor; Siglec-6: sialic acid binding immunoglobulin-like lectin; VEGF121: vascular endothelial growth factor A, isoform 121.
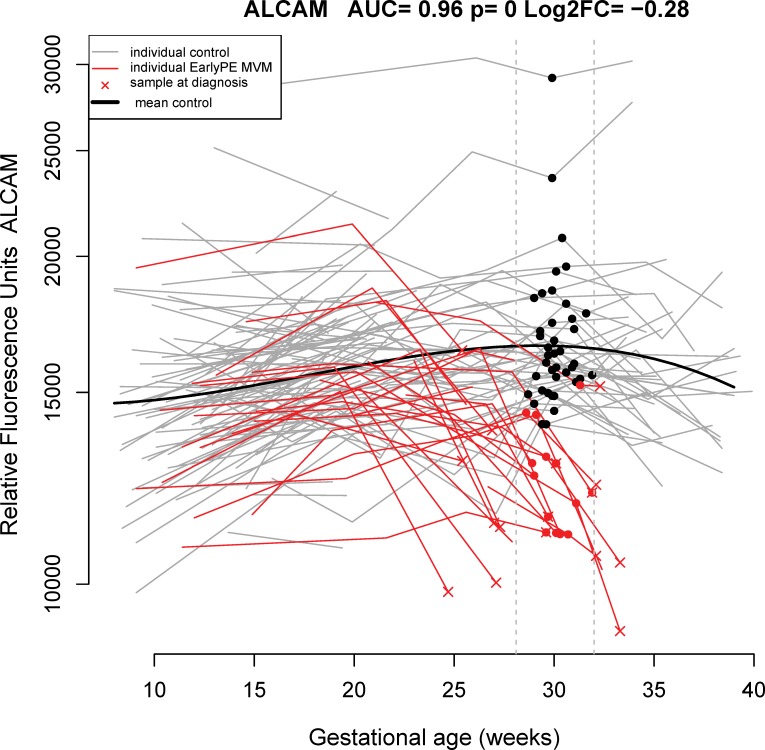
At 28.1–32 weeks of gestation, the bootstrap-estimated sensitivity of multi-marker risk models was 85% (FPR = 10%), with activated leukocyte cell-adhesion molecule (ALCAM), siglec-6, and VEGF121 being the most frequently selected markers (38%, 32%, and 32% of the bootstrap iterations, respectively). The longitudinal profiles of ALCAM are depicted in Fig 4.
Fig 4. Longitudinal maternal plasma ALCAM abundance in normal pregnancy and early preeclampsia cases, highlighting differences at 28.1–32 weeks.
ALCAM: activated leukocyte cell adhesion molecule; AUC: area under the receiver operating characteristic curve; early PE: early preeclampsia; FC: fold change; MVM: maternal vascular malperfusion.
Of note, prediction performance estimates for early preeclampsia were slightly higher when estimated by repeated cross-validation (S1 Table) than by bootstrap (Table 2), yet the variance of the estimates with the former method was somewhat higher (data not shown). The most predictive proteins retained in the prediction models were similar between the two approaches (see Tables 2and S1).
Prediction of early preeclampsia according to the presence of placental lesions consistent with maternal vascular malperfusion
To determine whether the sub-classification of early preeclampsia cases by placental lesions can lead to different protein markers and/or better prediction performance, a secondary analysis was performed that included the control group and only cases with placental lesions consistent with MVM. Bootstrap-based sensitivity estimates (at a fixed FPR of 10%) were higher for cases with MVM compared to those for the overall early preeclampsia group (16.1–22 weeks: 90% versus 71%; 22.1–28 weeks: 87% versus 81%; and 28.1–32 weeks: 90% versus 85%) (see bars in Fig 1and Table 2).
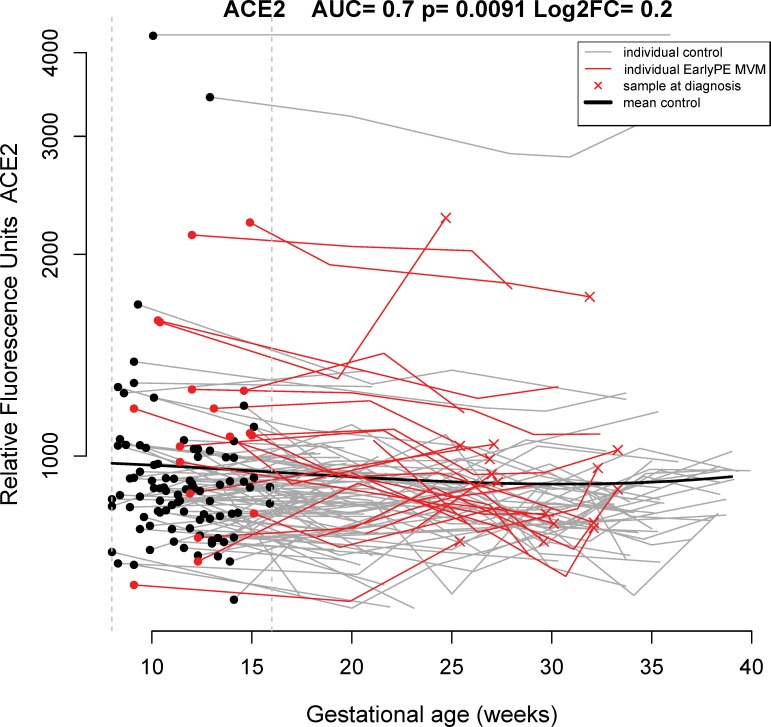
In addition to a higher sensitivity for cases with placental MVM lesions compared to the overall early preeclampsia group, differences in the sets of best predictors also emerged at particular intervals of gestation (Table 2). For example, angiotensin-converting enzyme 2 (ACE2) at 8–16 weeks (see raw data in Fig 5) and siglec-6 at 22.1–32 weeks of gestation were more frequently selected as the best markers for early preeclampsia with MVM lesions than for overall early preeclampsia (see Table 2).
Fig 5. Longitudinal maternal plasma ACE2 abundance in normal pregnancy and early preeclampsia cases, highlighting differences at 8–16 weeks of gestation.
See Fig 2 legend for more details. ACE2: angiotensin-converting enzyme 2; AUC: area under the receiver operating characteristic curve; early PE: early preeclampsia; FC: fold change; MVM: maternal vascular malperfusion.
Prediction of early preeclampsia according to disease severity
When only severe early preeclampsia cases were included in the analysis and compared to normal pregnancy cases, the sensitivity of analysis (10% FPR) was significantly higher than for overall early preeclampsia (90% vs 71%) in the 16.1–22 week interval. At this gestational-age interval, but unlike early preeclampsia with MVM that was predicted mostly by an increase in MMP-7, the prediction for severe early preeclampsia also involved the increase in gpIIbIIIa for 14% of the models trained on bootstrap samples of the original dataset. Other differences in the set of best predictors for severe early preeclampsia compared to overall early preeclampsia were noted in the 8–16 weeks gestational-age interval (see Table 2).
Proteomic markers that differentiate between early and late preeclampsia
Discrimination between early preeclampsia and both normal pregnancy and late preeclampsia was rather low in the 8-16-week and 16.1-22-week intervals (21% and 31% sensitivity, respectively, FPR = 10%) and involved different sets of proteins than those found when the comparison was only against the normal pregnancy group (Table 3). However, later in gestation, the sensitivity of multi-marker models to discriminate between early preeclampsia and both the controls and late preeclampsia increased to 77% and 82% at 16.1-22-week and 22.1-28-week intervals, respectively (FPR = 10%).
Table 3. Summary of bootstrap results for prediction of early preeclampsia versus normal pregnancy and late preeclampsia.
| Outcome | Sample GA (weeks) | AUC | Sensitivity | Specificity | Predictor Symbols (% inclusion in best combination) |
|---|---|---|---|---|---|
| Early PE | 8–16 | 0.55 | 0.21 | 0.90 | gpIIbIIIa(34%) |
| Early PE | 16.1–22 | 0.65 | 0.31 | 0.90 | Soggy-1(26%); IMDH2(20%); Siglec-6(14%); PKC-D(12%); MMP-12(10%); RBP(10%) |
| Early PE | 22.1–28 | 0.89 | 0.77 | 0.90 | Siglec-6(72%); Activin A(63%); VEGF121(34%) |
| Early PE | 28.1–32 | 0.93 | 0.82 | 0.90 | Siglec-6(72%); ALCAM(15%); FCN2(14%); VEGF121(12%) |
ALCAM: activated leukocyte cell adhesion molecule; AUC: area under the receiver operating characteristic curve; early PE: early preeclampsia; FCN2: ficolin 2; GA: gestational age; gpIIbIIIa: glycoprotein IIb/IIIa; IMDH2: inosine-5'-monophosphate dehydrogenase (IMDH2); MMP: matrix metalloproteinase; PKC-D: protein kinase C delta type; RBP: retinol binding protein; Siglec-6: sialic acid binding immunoglobulin-like lectin; VEGF121: vascular endothelial growth factor A, isoform 121. Only proteins selected in 10% or more of the 200 bootstrap iterations are listed.
Of note, discriminating early preeclampsia from both normal pregnancy and late preeclampsia cases involved more stringent cut-offs for the same proteins (see Fig 6) and also new proteins such as ficolin 2 (FCN2) (see Table 3).
Fig 6.
Longitudinal maternal plasma abundance of siglec-6 (A) and activin-A (B) in normal pregnancy and early preeclampsia, highlighting differences at 22.1–28 weeks. Blue dots correspond to samples taken from late preeclampsia cases. AUC: area under the receiver operating characteristic curve; early PE: early preeclampsia; FC: fold change; late PE: late preeclampsia; Siglec-6: sialic acid binding immunoglobulin-like lectin.
Differential protein abundance summary
In addition to the proteins included in the parsimonious models predictive of early preeclampsia at different gestational-age intervals (Table 2), other proteins (total, n = 175) had a significant differential abundance (after adjustment for body mass index, smoking status, maternal age, and parity) in at least one gestational-age interval (q-value < 0.1).
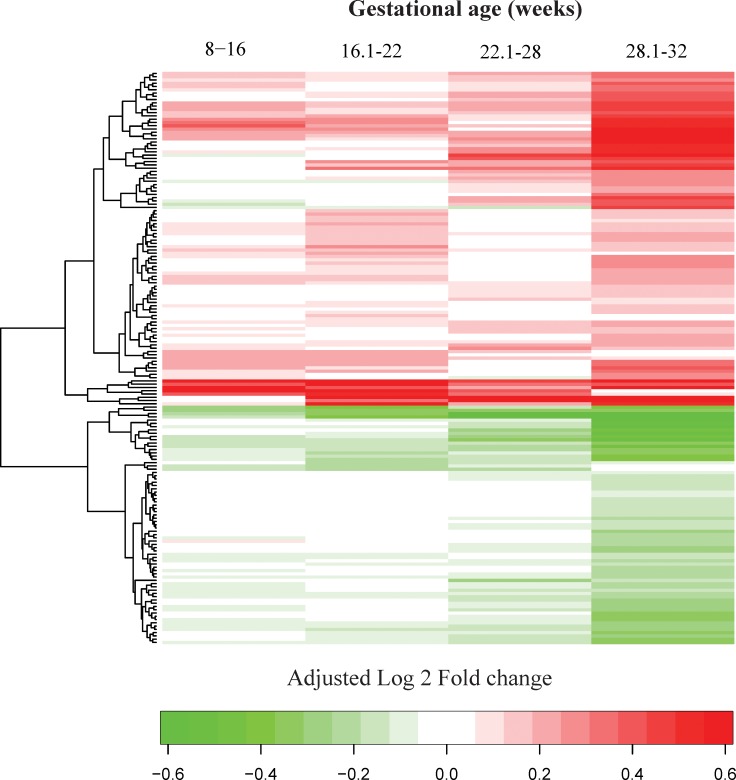
S2 Table presents the linear fold changes of MoM values between the early preeclampsia and normal pregnancy groups as well as the nominal and FDR-adjusted p-values (q-values) for each gestational-age interval. Additionally, the heatmap presented in Fig 7summarizes the differential abundance patterns across all gestational-age intervals included in this study. There were 2, 37, 20, and 153 proteins associated with early preeclampsia at 8–16, 16.1–22, 22.1–28, and 28.1–32 weeks of gestation, respectively.
Fig 7. A summary of differential protein abundance between early preeclampsia and normal pregnancy throughout gestation.
The values shown using a color scheme represent the log2 fold change in MoM values between the cases and controls (green = lower, red = higher mean MoM in cases versus controls). Fold changes >1.5 (absolute log2 fold change >0.58) were reset to 1.5 to enhance visualization of the data.
MMP-7 was elevated in three of the four gestational-age intervals. IL-1 R4 (interleukin-1 receptor-like 1), siglec-6, and activin-A were elevated while FCN2, MMP-12, VEGF121, and PlGF were lower in all three intervals from 16.1 weeks of gestation onward. Differential abundance analyses were also summarized for early preeclampsia with MVM (S3 Table and S1 Fig), as well as for severe early preeclampsia (S4 Table and S1 Fig) compared to normal pregnancy.
Biological processes and pathways perturbed in early preeclampsia during gestation
Gene ontology analysis of the proteins that changed significantly between patients with a normal pregnancy and those with early preeclampsia was performed for each gestational-age interval. At 16.1–22 weeks of gestation, there were 6; at 22.1–28 weeks, there were 7; and at 28.1–32 weeks, there were 30 biological processes significantly associated with early preeclampsia (Table 4). Biological processes associated with protein changes in at least one gestational age interval included cell adhesion, response to hypoxia, positive regulation of endothelial cell proliferation, extracellular matrix disassembly, and vascular endothelial growth factor receptor signaling pathway (all: q < 0.1) (Table 4).
Table 4. Biological processes enriched in proteins with a differential abundance between early preeclampsia and normal pregnancy.
| Interval | Name | N | OR | p | q |
|---|---|---|---|---|---|
| xenobiotic metabolic process | 3 | 47.1 | 0.000 | 0.008 | |
| negative chemotaxis | 3 | 31.5 | 0.001 | 0.008 | |
| 16.1–22 | small molecule metabolic process | 10 | 3.1 | 0.006 | 0.0485 |
| weeks | regulation of transcription from RNA polymerase II promoter | 3 | 9.5 | 0.007 | 0.0485 |
| integrin-mediated signaling pathway | 3 | 7.3 | 0.014 | 0.071 | |
| extracellular matrix disassembly | 5 | 3.7 | 0.019 | 0.0838 | |
| positive regulation of endothelial cell proliferation | 4 | 11.7 | 0.001 | 0.0128 | |
| cellular calcium ion homeostasis | 3 | 7.0 | 0.014 | 0.0866 | |
| response to hypoxia | 3 | 5.1 | 0.031 | 0.0866 | |
| 22.1–28 | cell adhesion | 5 | 3.3 | 0.033 | 0.0866 |
| weeks | response to drug | 4 | 3.7 | 0.036 | 0.0866 |
| positive regulation of angiogenesis | 3 | 4.6 | 0.040 | 0.0866 | |
| extracellular matrix disassembly | 3 | 4.1 | 0.053 | 0.0976 | |
| blood coagulation | 36 | 2.7 | 0.000 | 0.0042 | |
| platelet degranulation | 18 | 3.9 | 0.000 | 0.0045 | |
| blood coagulation, intrinsic pathway | 8 | 8.9 | 0.000 | 0.0123 | |
| sprouting angiogenesis | 6 | 13.1 | 0.000 | 0.0218 | |
| platelet activation | 22 | 2.5 | 0.001 | 0.036 | |
| vascular endothelial growth factor signaling pathway | 4 | 25.9 | 0.001 | 0.063 | |
| positive regulation of endothelial cell migration | 7 | 5.8 | 0.002 | 0.0683 | |
| response to cold | 3 | Inf | 0.002 | 0.0703 | |
| plasminogen activation | 3 | Inf | 0.002 | 0.0703 | |
| nervous system development | 12 | 3.1 | 0.003 | 0.071 | |
| blood circulation | 5 | 8.1 | 0.003 | 0.071 | |
| negative regulation of cell-substrate adhesion | 4 | 13.0 | 0.004 | 0.071 | |
| positive regulation of macrophage activation | 4 | 13.0 | 0.004 | 0.071 | |
| 28.1–32 | positive regulation of synapse assembly | 4 | 13.0 | 0.004 | 0.071 |
| weeks | liver development | 6 | 5.6 | 0.004 | 0.071 |
| fibrinolysis | 7 | 4.6 | 0.004 | 0.071 | |
| response to hypoxia | 12 | 2.9 | 0.005 | 0.071 | |
| hematopoietic progenitor cell differentiation | 4 | 8.6 | 0.008 | 0.086 | |
| response to vitamin D | 4 | 8.6 | 0.008 | 0.086 | |
| negative regulation of fat cell differentiation | 4 | 8.6 | 0.008 | 0.086 | |
| positive regulation of acute inflammatory response | 3 | 19.3 | 0.009 | 0.086 | |
| cell-substrate junction assembly | 3 | 19.3 | 0.009 | 0.086 | |
| negative regulation of ossification | 3 | 19.3 | 0.009 | 0.086 | |
| negative regulation of B cell differentiation | 3 | 19.3 | 0.009 | 0.086 | |
| cellular response to follicle-stimulating hormone stimulus | 3 | 19.3 | 0.009 | 0.086 | |
| negative regulation of angiogenesis | 7 | 3.8 | 0.009 | 0.086 | |
| negative regulation of cysteine-type endopeptidase activity involved in apoptotic process | 7 | 3.8 | 0.009 | 0.086 | |
| positive regulation of neuron differentiation | 6 | 4.4 | 0.010 | 0.0895 | |
| positive regulation of blood vessel endothelial cell migration | 5 | 5.4 | 0.010 | 0.0895 | |
| positive regulation of MAPK cascade | 9 | 3.0 | 0.011 | 0.0953 |
ID: Gene Ontology (GO) biological processes identifier; N: number of significant proteins assigned to the GO term; OR: odds ratio for enrichment; p: p-value; q: false discovery rate-adjusted p-value.
No signaling pathways documented in the KEGG database [75] were found to be perturbed given the differential protein abundance observed in each interval of gestation.
Discussion
Principal findings of the study
The principal findings of the study are as follows: 1) At 16.1–22 weeks of gestation, multi-protein models predicted early preeclampsia with a sensitivity of 71% (FPR = 10%). The most reliable predictors in this interval were an elevated MMP-7 and gpIIbIIIa complex; 2) the best predictors of the subsequent development of early preeclampsia at 22.1–28 weeks of gestation were lower PlGF and VEGF121 as well as elevated siglec-6 and activin-A (81% sensitivity, FPR = 10%); 3) at 28.1–32 weeks of gestation, the sensitivity of multi-protein models was 85% (FPR = 10%) with the most reliable predictors being ALCAM, siglec-6, and VEGF121; 4) the increase in siglec-6, activin-A, and VEGF121 at 22.1–28 weeks of gestation differentiated women who subsequently developed early preeclampsia from those who had a normal pregnancy or late preeclampsia (sensitivity 77%, FPR = 10%); 5) the sensitivity of proteomic models for early preeclampsia in women with placental lesions consistent with MVM was higher than that of the models reported for the overall early preeclampsia group from 16.1 weeks of gestation onward; and 6) the sensitivity of prediction models was higher for severe early preeclampsia than for the entire early preeclampsia group (84% versus 71% at 16.1–22 weeks).
Of note, differential protein abundance results and, hence, downstream enrichment analyses are expected to vary among the different intervals of gestation due to several factors, such as: 1) differences in the sets of patients that contributed one sample in each interval, due to sample availability or to exclusion from analysis of samples at/or past the gestational age at diagnosis (see Methods); 2) differences in the magnitude of underlying disease-specific maternal plasma protein changes with preeclampsia; and 3) differences in the level of noise in the data, contributing non-biological variability.
Proteomics prediction models for the identification of patients with preeclampsia
Biomarkers for the identification of patients at risk for obstetrical syndromes such as small-for-gestational-age neonates [34,78–82], spontaneous preterm birth [83–94], fetal death [95–105], and preeclampsia [12,47,49,50,56,72,106–113] have been proposed. For preeclampsia, prediction models have evolved from ones that used maternal background characteristics alone (e.g., obstetrical history, chronic hypertension, familial history of preeclampsia, obesity) [114,115] to those that combine maternal demographic characteristics, obstetrical history [116,117], mean blood pressure [118], uterine artery Doppler studies [52,54,119], and molecular biomarkers [56,120–122] (e.g., PAPP-A [88,123–125] and inhibin-A [124,126–128]). Some of the most predictive biochemical markers include angiogenic and anti-angiogenic factors [33,129–134] (PlGF [34,135–137], sVEGFR-1[138–142], and endoglin [143–148]), or their ratios [34,129,149–155]. A limitation of current screening methods for preeclampsia is the requirement of Doppler velocimetry, which is not readily available in middle- and low-resource populations. The detection rate for early preeclampsia drops to 77% and 57% at FPRs of 10% and 5%, respectively, in the absence of Doppler information [156]. Therefore, there would still be a benefit in developing accurate prediction models based solely on molecular information.
Discovery of molecular markers for obstetrical complications is often undertaken using “omics” technologies [157–165]: genomics [166,167], transcriptomics [168–175], proteomics [72,165,176–187], metabolomics [188–192], peptidomics [193–198], and lipidomics [199,200]. In particular, maternal proteomic profiles in preeclampsia were reported in maternal serum/plasma [175–177,180,201–210], urine [211–213], amniotic fluid [214,215], and the placenta [179,182,216–228]. However, most maternal plasma/serum proteomics studies to date did not involve samples collected longitudinally to determine how early molecular markers change their profiles prior to the disease onset and whether these changes are consistent throughout pregnancy, or the studies involved a small sample size.
The current study is one of the largest in this field and uses a new proteomics technology based on aptamers that allows the measurement of 1,125 proteins. Using this platform (Somalogic, Inc.), we and other investigators reported the stereotypic longitudinal changes of the maternal plasma proteome in normal pregnancy [229,230] and late preeclampsia [72]. Our current report observing that an increased maternal plasma abundance of MMP-7 and gpIIbIIIa is predictive of early preeclampsia during the first half of pregnancy is novel.
Increased maternal plasma MMP-7 precedes diagnosis of preeclampsia
A possible explanation for the increased maternal plasma MMP-7 in preeclampsia is that it is a marker of abnormal placentation. MMP-7 is expressed in the decidua and trophoblast [231,232] and has been proposed to play a role in the process of transformation of the spiral arteries [233,234]. There is also histological evidence to support the involvement of MMP-7 in the processes associated with the development of preeclampsia [231] and early preeclampsia [233]. Additionally, MMP-7 can act as a sheddase for syndecan-1 [235,236], a major transmembrane heparan sulfate proteoglycan expressed on the surface (glycocalyx) of epithelial, endothelial, and syncytiotrophoblast cells [237–239], which are implicated in the pathophysiology of preeclampsia [240–243]. MMP-7 may also be involved in processes leading to the formation of atherosclerotic plaques [244] that show characteristics (e.g., lipid-laden macrophages) similar to acute atherosis of the spiral arteries associated with preeclampsia [245,246]. Of note in our previous study that used the same proteomics platform, MMP-7 was found to be a sensitive biomarker during the first half of pregnancy for the detection of patients who subsequently developed late preeclampsia [72]; herein, we showed that is also the case for early preeclampsia.
The role of glycoprotein IIbIIIa in early preeclampsia
To our knowledge, this is the first study to report that changes in the abundance of gpIIbIIIa in the maternal plasma are predictive of subsequent development of early preeclampsia. In this patient population, at 8–16 weeks of gestation, gpIIbIIIa performed better than PlGF (currently used to screen for preeclampsia) [48,50,51,137] for the detection of patients who subsequently developed early preeclampsia when profiled with the Somalogic platform (AUC = 0.60 for PlGF and 0.72 for gpIIbIIIa, see Table 2and Fig 2B).
Glycoprotein IIb-IIIa is a membrane glycoprotein [247], the most common platelet receptor [247,248]. After a conformational change occurring during platelet activation [249], it interacts with ligands (e.g., von Willebrand factor and fibrinogen) to play a critical role in platelet aggregation and the cross-linkage of platelets into a hemostatic plug or thrombus [250–253]. Aspirin inhibits the expression of gpIIbIIIa by platelets [254]. This fact is important given that aspirin is currently recommended by regulatory bodies in the United States for the prevention of preeclampsia [255–257]; moreover, this medication has recently been reported to reduce the rate of preterm preeclampsia by 62% [40]. Our findings suggest that gpIIbIIIa inhibitors could be further developed for the prevention of early preeclampsia.
Presence of placental lesions of maternal vascular malperfusion and disease severity increases the sensitivity of proteomic models for early preeclampsia
The sensitivity of the proteomic models at each gestational-age interval from 16.1 weeks onward was higher for cases that had placental lesions consistent with MVM than for the overall group of women with early preeclampsia and even compared to those with severe early preeclampsia. Maternal vascular malperfusion is a prevalent placental histologic finding in patients with early preeclampsia [28], and 73% (24/33) of cases in the current study had these lesions. These results further support a previous observation that the prediction performance of angiogenic index-1 (PlGF/sVEGFR-1) for preterm delivery (<34 weeks) is higher for women with these types of placental lesions [63].
Of interest, even when only patients with lesions consistent with MVM were compared to those with a normal pregnancy, proteins of placental origin (e.g., PlGF and siglec-6) were still the most predictive of early preeclampsia, but only after 22 weeks of gestation. This finding is consistent with our earlier study in late preeclampsia [72] and with previous longitudinal studies of angiogenic and anti-angiogenic factors [35,46,151]. Moreover, the data presented herein also support our previous systems biology study in early preeclampsia showing that siglec-6 expression in the placenta increased in the second half of pregnancy due to a hypoxic-ischemic trophoblastic response to placental malperfusion [258].
Clinical implications
The current study demonstrates the potential of maternal plasma protein changes to identify women at risk of early preeclampsia based on a single blood test. The use of disease-risk models based solely on proteomic markers would be similar to first- and second-trimester aneuploidy tests [259–262]. Such an approach can be implemented in various clinical settings, especially in low-resource areas, where Doppler velocimetry of the uterine arteries is not readily available. Moreover, the proteomics biomarkers identified in this study may assist in the introduction of novel therapeutic agents (e.g., gpIIbIIIa inhibitors) for the prevention of early preeclampsia.
Strengths and limitations of the study
The major strengths of this study are its longitudinal design, the number of patients and their stratification according to placental histology, and the large number of proteins tested. In addition, best practices in terms of model development and validation were based on our award-winning classifier development pipeline [67–69]. A limitation of this study is the fact that the aptamer-based assays did not include internal standards to generate protein concentrations (as opposed to fluorescence-based abundance); hence, further studies would be needed to generate protein concentration cut-offs. Additionally, the majority of the patients included in this study were of African-American lineage, and the generalization of findings to other ethnic groups needs to be further examined. Lastly, for three of the 33 early preeclampsia cases, the information regarding 24-hour proteinuria was not available; hence, we were reliant on dipstick evaluation.
Conclusions
Aptamer-based proteomic profiling of maternal plasma identified novel as well as previously known markers for early preeclampsia. At 16.1–22 weeks of gestation, more than two-thirds of patients who subsequently develop early preeclampsia can be identified by an elevated MMP-7 and gpIIbIIIa in maternal plasma (10% FPR). High abundance of siglec-6, VEGF121, and activin-A observed in the maternal circulation at 22.1–28 weeks of gestation was more specific to early rather than late preeclampsia. Proteomic markers were more sensitive for early preeclampsia cases with placental lesions consistent with MVM as well as those with a severe phenotype.
Supporting information
The number in parentheses following the name of each protein (column Predictor Symbols) represents the percentage of folds in which the protein was selected in the best model. Only proteins selected in 10% or more of the 3x67 = 201 folds are listed. ACE2: angiotensin converting enzyme 2; ALCAM: activated leukocyte cell adhesion molecule; AUC: area under the receiver operating characteristic curve; GA: gestational age; gpIIbIIIa: glycoprotein IIb/IIIa; HMG-1: high-mobility group protein 1; MMP: matrix metalloproteinase; early PE: early preeclampsia; MVM: maternal vascular malperfusion; PE: preeclampsia; PlGF: placental growth factor; Siglec-6: sialic acid binding immunoglobulin-like lectin; VEGF121: vascular endothelial growth factor A, isoform 121; vWF: von Willebrand factor.
(XLSX)
List of 175 proteins with significantly different abundance between early preeclampsia and normal pregnancy (q < 0.1) in at least one interval, after adjustment for body mass index, maternal age, parity and smoking status. FC: linear fold change, with negative values denoting lower levels while positive values denote higher levels in cases than in controls.
(XLSX)
List of 76 proteins with significantly different abundance between early preeclampsia with MVM and normal pregnancy (q < 0.1) in at least one interval, after adjustment for body mass index, maternal age, parity and smoking status. FC: linear fold change, with negative values denoting lower levels while positive values denote higher levels in cases than in controls.
(XLSX)
List of 130 proteins with significantly different abundance between severe early preeclampsia and normal pregnancy (q < 0.1) in at least one interval, after adjustment for body mass index, maternal age, parity and smoking status. FC: linear fold change, with negative values denoting lower levels while positive values denote higher levels in cases than in controls.
(XLSX)
Protein abundance data for each sample (rows) and each of the 1125 proteins is given in this table. Note, unlike for the early preeclampsia group, data for normal pregnancy group is the same as in in [72], and included in this file for convenience. ID: anonymized identifier indicator of the patient, GA: gestational age at sample, GADiagnosis: gestational age at diagnosis for cases; EarlyPE: is 1 for early preeclampsia and 0 for normal pregnancy. EarlyPE_MVM: is 1 for early preeclampsia with maternal vascular malperfusion and 0 for normal pregnancy or early preeclampsia without maternal vascular malperfusion; EarlyPE_Severe: is 1 for severe early preeclampsia cases; Protein symbol and names provided by Somalogic, Inc, are the same as S1 File in [72].
(CSV)
Longitudinal differences in protein abundance assessed generalized additive mixed models are shown for proteins listed in Table 2. For each protein, differences are shown between early preeclampsia (PE) and controls (top left) as well as between mild or severe PE and controls (top right) and between PE with or without maternal vascular malperfusion (MVM) and controls. Thick lines show averages while grey bands give the 95% confidence interval.
(PDF)
Acknowledgments
We thank the physicians, nurses, and research assistants from the Center for Advanced Obstetrical Care and Research, Intrapartum Unit, PRB Clinical Laboratory, and PRB Perinatal Translational Science Laboratory for their help with collecting and processing samples.
Data Availability
All relevant data are included within the paper and its Supporting Information files.
Funding Statement
This research was supported, in part, by the Perinatology Research Branch, Program for Perinatal Research and Obstetrics, Division of Intramural Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, U.S. Department of Health and Human Services (NICHD/NIH/DHHS); and, in part, with federal funds from NICHD/NIH/DHHS under contract no. HHSN275201300006C. ALT was also supported by the Perinatal Initiative of the Wayne State University School of Medicine.
References
- 1.Romero R (1996) The child is the father of the man. Prenat Neonat Med 1: 8–11. [Google Scholar]
- 2.Brosens I, Pijnenborg R, Vercruysse L, Romero R (2011) The "Great Obstetrical Syndromes" are associated with disorders of deep placentation. Am J Obstet Gynecol 204: 193–201. 10.1016/j.ajog.2010.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Romero R, Lockwood C, Oyarzun E, Hobbins JC (1988) Toxemia: new concepts in an old disease. Semin Perinatol 12: 302–323. [PubMed] [Google Scholar]
- 4.von Dadelszen P, Magee LA, Roberts JM (2003) Subclassification of preeclampsia. Hypertens Pregnancy 22: 143–148. 10.1081/PRG-120021060 [DOI] [PubMed] [Google Scholar]
- 5.Vatten LJ, Skjaerven R (2004) Is pre-eclampsia more than one disease? Bjog 111: 298–302. [DOI] [PubMed] [Google Scholar]
- 6.Valensise H, Vasapollo B, Gagliardi G, Novelli GP (2008) Early and late preeclampsia: two different maternal hemodynamic states in the latent phase of the disease. Hypertension 52: 873–880. 10.1161/HYPERTENSIONAHA.108.117358 [DOI] [PubMed] [Google Scholar]
- 7.Raymond D, Peterson E (2011) A critical review of early-onset and late-onset preeclampsia. Obstet Gynecol Surv 66: 497–506. 10.1097/OGX.0b013e3182331028 [DOI] [PubMed] [Google Scholar]
- 8.Lisonkova S, Joseph KS (2013) Incidence of preeclampsia: risk factors and outcomes associated with early- versus late-onset disease. Am J Obstet Gynecol 209: 544.e541-544.e512. [DOI] [PubMed] [Google Scholar]
- 9.Tranquilli AL, Brown MA, Zeeman GG, Dekker G, Sibai BM (2013) The definition of severe and early-onset preeclampsia. Statements from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Pregnancy Hypertens 3: 44–47. 10.1016/j.preghy.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 10.Verlohren S, Melchiorre K, Khalil A, Thilaganathan B (2014) Uterine artery Doppler, birth weight and timing of onset of pre-eclampsia: providing insights into the dual etiology of late-onset pre-eclampsia. Ultrasound Obstet Gynecol 44: 293–298. 10.1002/uog.13310 [DOI] [PubMed] [Google Scholar]
- 11.Soto E, Romero R, Kusanovic JP, Ogge G, Hussein Y, Yeo L, et al. (2012) Late-onset preeclampsia is associated with an imbalance of angiogenic and anti-angiogenic factors in patients with and without placental lesions consistent with maternal underperfusion. J Matern Fetal Neonatal Med 25: 498–507. 10.3109/14767058.2011.591461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parra-Cordero M, Rodrigo R, Barja P, Bosco C, Rencoret G, Sepulveda-Martinez A, et al. (2013) Prediction of early and late pre-eclampsia from maternal characteristics, uterine artery Doppler and markers of vasculogenesis during first trimester of pregnancy. Ultrasound Obstet Gynecol 41: 538–544. 10.1002/uog.12264 [DOI] [PubMed] [Google Scholar]
- 13.Kucukgoz Gulec U, Ozgunen FT, Buyukkurt S, Guzel AB, Urunsak IF, Demir SC, et al. (2013) Comparison of clinical and laboratory findings in early- and late-onset preeclampsia. J Matern Fetal Neonatal Med 26: 1228–1233. 10.3109/14767058.2013.776533 [DOI] [PubMed] [Google Scholar]
- 14.Lisonkova S, Sabr Y, Mayer C, Young C, Skoll A, Joseph KS (2014) Maternal morbidity associated with early-onset and late-onset preeclampsia. Obstet Gynecol 124: 771–781. 10.1097/AOG.0000000000000472 [DOI] [PubMed] [Google Scholar]
- 15.Veerbeek JH, Hermes W, Breimer AY, van Rijn BB, Koenen SV, Mol BW, et al. (2015) Cardiovascular disease risk factors after early-onset preeclampsia, late-onset preeclampsia, and pregnancy-induced hypertension. Hypertension 65: 600–606. 10.1161/HYPERTENSIONAHA.114.04850 [DOI] [PubMed] [Google Scholar]
- 16.Bokslag A, Teunissen PW, Franssen C, van Kesteren F, Kamp O, Ganzevoort W, et al. (2017) Effect of early-onset preeclampsia on cardiovascular risk in the fifth decade of life. Am J Obstet Gynecol 216: 523.e521-523.e527. [DOI] [PubMed] [Google Scholar]
- 17.Christensen M, Kronborg CS, Carlsen RK, Eldrup N, Knudsen UB (2017) Early gestational age at preeclampsia onset is associated with subclinical atherosclerosis 12 years after delivery. Acta Obstet Gynecol Scand 96: 1084–1092. 10.1111/aogs.13173 [DOI] [PubMed] [Google Scholar]
- 18.Jelin AC, Cheng YW, Shaffer BL, Kaimal AJ, Little SE, Caughey AB (2010) Early-onset preeclampsia and neonatal outcomes. J Matern Fetal Neonatal Med 23: 389–392. 10.1080/14767050903168416 [DOI] [PubMed] [Google Scholar]
- 19.Kovo M, Schreiber L, Ben-Haroush A, Gold E, Golan A, Bar J (2012) The placental component in early-onset and late-onset preeclampsia in relation to fetal growth restriction. Prenat Diagn 32: 632–637. 10.1002/pd.3872 [DOI] [PubMed] [Google Scholar]
- 20.Stubert J, Ullmann S, Dieterich M, Diedrich D, Reimer T (2014) Clinical differences between early- and late-onset severe preeclampsia and analysis of predictors for perinatal outcome. J Perinat Med 42: 617–627. 10.1515/jpm-2013-0285 [DOI] [PubMed] [Google Scholar]
- 21.Madazli R, Yuksel MA, Imamoglu M, Tuten A, Oncul M, Aydin B, et al. (2014) Comparison of clinical and perinatal outcomes in early- and late-onset preeclampsia. Arch Gynecol Obstet 290: 53–57. 10.1007/s00404-014-3176-x [DOI] [PubMed] [Google Scholar]
- 22.Khodzhaeva ZS, Kogan YA, Shmakov RG, Klimenchenko NI, Akatyeva AS, Vavina OV, et al. (2016) Clinical and pathogenetic features of early- and late-onset pre-eclampsia. J Matern Fetal Neonatal Med 29: 2980–2986. 10.3109/14767058.2015.1111332 [DOI] [PubMed] [Google Scholar]
- 23.Mor O, Stavsky M, Yitshak-Sade M, Mastrolia SA, Beer-Weisel R, Rafaeli-Yehudai T, et al. (2016) Early onset preeclampsia and cerebral palsy: a double hit model? Am J Obstet Gynecol 214: 105.e101-109. [DOI] [PubMed] [Google Scholar]
- 24.Iacobelli S, Bonsante F, Robillard PY (2017) Comparison of risk factors and perinatal outcomes in early onset and late onset preeclampsia: A cohort based study in Reunion Island. J Reprod Immunol 123: 12–16. 10.1016/j.jri.2017.08.005 [DOI] [PubMed] [Google Scholar]
- 25.Moldenhauer JS, Stanek J, Warshak C, Khoury J, Sibai B (2003) The frequency and severity of placental findings in women with preeclampsia are gestational age dependent. Am J Obstet Gynecol 189: 1173–1177. [DOI] [PubMed] [Google Scholar]
- 26.van der Merwe JL, Hall DR, Wright C, Schubert P, Grove D (2010) Are early and late preeclampsia distinct subclasses of the disease—what does the placenta reveal? Hypertens Pregnancy 29: 457–467. 10.3109/10641950903572282 [DOI] [PubMed] [Google Scholar]
- 27.Sebire NJ, Goldin RD, Regan L (2005) Term preeclampsia is associated with minimal histopathological placental features regardless of clinical severity. J Obstet Gynaecol 25: 117–118. 10.1080/014436105400041396 [DOI] [PubMed] [Google Scholar]
- 28.Ogge G, Chaiworapongsa T, Romero R, Hussein Y, Kusanovic JP, Yeo L, et al. (2011) Placental lesions associated with maternal underperfusion are more frequent in early-onset than in late-onset preeclampsia. J Perinat Med 39: 641–652. 10.1515/JPM.2011.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Redman CW, Sargent IL, Staff AC (2014) IFPA Senior Award Lecture: making sense of pre-eclampsia—two placental causes of preeclampsia? Placenta 35 Suppl: S20–25. [DOI] [PubMed] [Google Scholar]
- 30.Nelson DB, Ziadie MS, McIntire DD, Rogers BB, Leveno KJ (2014) Placental pathology suggesting that preeclampsia is more than one disease. Am J Obstet Gynecol 210: 66.e61-67. [DOI] [PubMed] [Google Scholar]
- 31.Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. (2003) Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest 111: 649–658. 10.1172/JCI17189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lindheimer MD, Romero R (2007) Emerging roles of antiangiogenic and angiogenic proteins in pathogenesis and prediction of preeclampsia. Hypertension 50: 35–36. 10.1161/HYPERTENSIONAHA.107.089045 [DOI] [PubMed] [Google Scholar]
- 33.Vatten LJ, Eskild A, Nilsen TI, Jeansson S, Jenum PA, Staff AC (2007) Changes in circulating level of angiogenic factors from the first to second trimester as predictors of preeclampsia. Am J Obstet Gynecol 196: 239.e231-236. [DOI] [PubMed] [Google Scholar]
- 34.Erez O, Romero R, Espinoza J, Fu W, Todem D, Kusanovic JP, et al. (2008) The change in concentrations of angiogenic and anti-angiogenic factors in maternal plasma between the first and second trimesters in risk assessment for the subsequent development of preeclampsia and small-for-gestational age. J Matern Fetal Neonatal Med 21: 279–287. 10.1080/14767050802034545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Romero R, Nien JK, Espinoza J, Todem D, Fu W, Chung H, et al. (2008) A longitudinal study of angiogenic (placental growth factor) and anti-angiogenic (soluble endoglin and soluble vascular endothelial growth factor receptor-1) factors in normal pregnancy and patients destined to develop preeclampsia and deliver a small for gestational age neonate. J Matern Fetal Neonatal Med 21: 9–23. 10.1080/14767050701830480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gotsch F, Romero R, Kusanovic JP, Chaiworapongsa T, Dombrowski M, Erez O, et al. (2008) Preeclampsia and small-for-gestational age are associated with decreased concentrations of a factor involved in angiogenesis: soluble Tie-2. J Matern Fetal Neonatal Med 21: 389–402. 10.1080/14767050802046069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vaisbuch E, Whitty JE, Hassan SS, Romero R, Kusanovic JP, Cotton DB, et al. (2011) Circulating angiogenic and antiangiogenic factors in women with eclampsia. Am J Obstet Gynecol 204: 152.e151-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, et al. (2010) Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol 116: 402–414. 10.1097/AOG.0b013e3181e9322a [DOI] [PubMed] [Google Scholar]
- 39.Baschat AA (2015) First-trimester screening for pre-eclampsia: moving from personalized risk prediction to prevention. Ultrasound Obstet Gynecol 45: 119–129. 10.1002/uog.14770 [DOI] [PubMed] [Google Scholar]
- 40.Rolnik DL, Wright D, Poon LC, O'Gorman N, Syngelaki A, de Paco Matallana C, et al. (2017) Aspirin versus Placebo in Pregnancies at High Risk for Preterm Preeclampsia. N Engl J Med 377: 613–622. 10.1056/NEJMoa1704559 [DOI] [PubMed] [Google Scholar]
- 41.Groom KM, David AL (2018) The role of aspirin, heparin, and other interventions in the prevention and treatment of fetal growth restriction. Am J Obstet Gynecol 218: S829–s840. 10.1016/j.ajog.2017.11.565 [DOI] [PubMed] [Google Scholar]
- 42.Stampalija T, Chaiworapongsa T, Romero R, Chaemsaithong P, Korzeniewski SJ, Schwartz AG, et al. (2013) Maternal plasma concentrations of sST2 and angiogenic/anti-angiogenic factors in preeclampsia. J Matern Fetal Neonatal Med 26: 1359–1370. 10.3109/14767058.2013.784256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Baschat AA, Magder LS, Doyle LE, Atlas RO, Jenkins CB, Blitzer MG (2014) Prediction of preeclampsia utilizing the first trimester screening examination. Am J Obstet Gynecol 211: 514.e511-517. [DOI] [PubMed] [Google Scholar]
- 44.Gallo DM, Wright D, Casanova C, Campanero M, Nicolaides KH (2016) Competing risks model in screening for preeclampsia by maternal factors and biomarkers at 19–24 weeks' gestation. Am J Obstet Gynecol 214: 619 e611-619 e617. [DOI] [PubMed] [Google Scholar]
- 45.Tsiakkas A, Saiid Y, Wright A, Wright D, Nicolaides KH (2016) Competing risks model in screening for preeclampsia by maternal factors and biomarkers at 30–34 weeks' gestation. Am J Obstet Gynecol 215: 87 e81-87 e17. [DOI] [PubMed] [Google Scholar]
- 46.Romero R, Chaemsaithong P, Tarca AL, Korzeniewski SJ, Maymon E, Pacora P, et al. (2017) Maternal plasma-soluble ST2 concentrations are elevated prior to the development of early and late onset preeclampsia—a longitudinal study. J Matern Fetal Neonatal Med: 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Akolekar R, Syngelaki A, Poon L, Wright D, Nicolaides KH (2013) Competing risks model in early screening for preeclampsia by biophysical and biochemical markers. Fetal Diagn Ther 33: 8–15. 10.1159/000341264 [DOI] [PubMed] [Google Scholar]
- 48.Myers JE, Kenny LC, McCowan LM, Chan EH, Dekker GA, Poston L, et al. (2013) Angiogenic factors combined with clinical risk factors to predict preterm pre-eclampsia in nulliparous women: a predictive test accuracy study. Bjog 120: 1215–1223. 10.1111/1471-0528.12195 [DOI] [PubMed] [Google Scholar]
- 49.O'Gorman N, Wright D, Syngelaki A, Akolekar R, Wright A, Poon LC, et al. (2016) Competing risks model in screening for preeclampsia by maternal factors and biomarkers at 11–13 weeks gestation. Am J Obstet Gynecol 214: 103.e101-103.e112. [DOI] [PubMed] [Google Scholar]
- 50.Crovetto F, Figueras F, Triunfo S, Crispi F, Rodriguez-Sureda V, Dominguez C, et al. (2015) First trimester screening for early and late preeclampsia based on maternal characteristics, biophysical parameters, and angiogenic factors. Prenat Diagn 35: 183–191. 10.1002/pd.4519 [DOI] [PubMed] [Google Scholar]
- 51.Espinoza J, Romero R, Nien JK, Gomez R, Kusanovic JP, Goncalves LF, et al. (2007) Identification of patients at risk for early onset and/or severe preeclampsia with the use of uterine artery Doppler velocimetry and placental growth factor. Am J Obstet Gynecol 196: 326.e321-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Crispi F, Llurba E, Dominguez C, Martin-Gallan P, Cabero L, Gratacos E (2008) Predictive value of angiogenic factors and uterine artery Doppler for early- versus late-onset pre-eclampsia and intrauterine growth restriction. Ultrasound Obstet Gynecol 31: 303–309. 10.1002/uog.5184 [DOI] [PubMed] [Google Scholar]
- 53.Melchiorre K, Wormald B, Leslie K, Bhide A, Thilaganathan B (2008) First-trimester uterine artery Doppler indices in term and preterm pre-eclampsia. Ultrasound Obstet Gynecol 32: 133–137. 10.1002/uog.5400 [DOI] [PubMed] [Google Scholar]
- 54.Llurba E, Carreras E, Gratacos E, Juan M, Astor J, Vives A, et al. (2009) Maternal history and uterine artery Doppler in the assessment of risk for development of early- and late-onset preeclampsia and intrauterine growth restriction. Obstet Gynecol Int 2009: 275613 10.1155/2009/275613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Poon LC, Staboulidou I, Maiz N, Plasencia W, Nicolaides KH (2009) Hypertensive disorders in pregnancy: screening by uterine artery Doppler at 11–13 weeks. Ultrasound Obstet Gynecol 34: 142–148. 10.1002/uog.6452 [DOI] [PubMed] [Google Scholar]
- 56.Audibert F, Boucoiran I, An N, Aleksandrov N, Delvin E, Bujold E, et al. (2010) Screening for preeclampsia using first-trimester serum markers and uterine artery Doppler in nulliparous women. Am J Obstet Gynecol 203: 383.e381-388. [DOI] [PubMed] [Google Scholar]
- 57.Ventura W, De Paco Matallana C, Prieto-Sanchez MT, Macizo MI, Pertegal M, Nieto A, et al. (2015) Uterine and umbilical artery Doppler at 28 weeks for predicting adverse pregnancy outcomes in women with abnormal uterine artery Doppler findings in the early second trimester. Prenat Diagn 35: 294–298. 10.1002/pd.4542 [DOI] [PubMed] [Google Scholar]
- 58.(2002) ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. Obstet Gynecol 99: 159–167. [DOI] [PubMed] [Google Scholar]
- 59.Chaiworapongsa T, Chaemsaithong P, Yeo L, Romero R (2014) Pre-eclampsia part 1: current understanding of its pathophysiology. Nat Rev Nephrol 10: 466–480. 10.1038/nrneph.2014.102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Romero R, Kim YM, Pacora P, Kim CJ, Benshalom-Tirosh N, Jaiman S, et al. (2018) The frequency and type of placental histologic lesions in term pregnancies with normal outcome. J Perinat Med 46: 613–630. 10.1515/jpm-2018-0055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Redline RW, Heller D, Keating S, Kingdom J (2005) Placental diagnostic criteria and clinical correlation—a workshop report. Placenta 26 Suppl A: S114–117. [DOI] [PubMed] [Google Scholar]
- 62.Khong TY, Mooney EE, Ariel I, Balmus NC, Boyd TK, Brundler MA, et al. (2016) Sampling and Definitions of Placental Lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch Pathol Lab Med 140: 698–713. 10.5858/arpa.2015-0225-CC [DOI] [PubMed] [Google Scholar]
- 63.Korzeniewski SJ, Romero R, Chaiworapongsa T, Chaemsaithong P, Kim CJ, Kim YM, et al. (2016) Maternal plasma angiogenic index-1 (placental growth factor/soluble vascular endothelial growth factor receptor-1) is a biomarker for the burden of placental lesions consistent with uteroplacental underperfusion: a longitudinal case-cohort study. Am J Obstet Gynecol 214: 629.e621-629.e617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gold L, Ayers D, Bertino J, Bock C, Bock A, Brody EN, et al. (2010) Aptamer-based multiplexed proteomic technology for biomarker discovery. PLoS One 5: e15004 10.1371/journal.pone.0015004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Davies DR, Gelinas AD, Zhang C, Rohloff JC, Carter JD, O'Connell D, et al. (2012) Unique motifs and hydrophobic interactions shape the binding of modified DNA ligands to protein targets. Proc Natl Acad Sci U S A 109: 19971–19976. 10.1073/pnas.1213933109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bates D, Maechler M, Bolker B, Walker S (2014) lme4: Linear mixed-effects models using Eigen and S4. http://arxivorg/abs/14065823
- 67.Tarca AL, Than N. G., Romero R. (2013) Methodological approach from the Best Overall Team in the sbv IMPROVER Diagnostic Signature Challenge. Systems Biomedicine 1: 217–227. [Google Scholar]
- 68.Tarca AL, Lauria M, Unger M, Bilal E, Boue S, Kumar Dey K, et al. (2013) Strengths and limitations of microarray-based phenotype prediction: lessons learned from the IMPROVER Diagnostic Signature Challenge. Bioinformatics 29: 2892–2899. 10.1093/bioinformatics/btt492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dayarian A, Romero R, Wang Z, Biehl M, Bilal E, Hormoz S, et al. (2014) Predicting protein phosphorylation from gene expression: top methods from the IMPROVER Species Translation Challenge. Bioinformatics: 462–470. 10.1093/bioinformatics/btu490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Smyth GK (2012) Limma: linear models for microarray data In: Gentleman R, Carey VJ, Huber W, Irizarry RA, Dudoit S, editors. Bioinformatics and Computational Biology Solutions Using R and Bioconductor: Springer; pp. 397–420. [Google Scholar]
- 71.Gentleman RC, Carey VJ, Bates DM, Bolstad B, Dettling M, Dudoit S, et al. (2004) Bioconductor: open software development for computational biology and bioinformatics. Genome Biol 5: R80 10.1186/gb-2004-5-10-r80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Erez O, Romero R, Maymon E, Chaemsaithong P, Done B, Pacora P, et al. (2017) The prediction of late-onset preeclampsia: Results from a longitudinal proteomics study. PLoS One 12: e0181468 10.1371/journal.pone.0181468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Maglott D, Ostell J, Pruitt KD, Tatusova T (2005) Entrez Gene: gene-centered information at NCBI. Nucleic Acids Res 33: D54–58. 10.1093/nar/gki031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, et al. (2000) Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat Genet 25: 25–29. 10.1038/75556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ogata H, Goto S, Sato K, Fujibuchi W, Bono H, Kanehisa M (1999) KEGG: Kyoto Encyclopedia of Genes and Genomes. Nucleic Acids Res 27: 29–34. 10.1093/nar/27.1.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Draghici S, Khatri P, Tarca AL, Amin K, Done A, Voichita C, et al. (2007) A systems biology approach for pathway level analysis. Genome Res 17: 1537–1545. 10.1101/gr.6202607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tarca AL, Draghici S, Khatri P, Hassan SS, Mittal P, Kim JS, et al. (2009) A novel signaling pathway impact analysis. Bioinformatics 25: 75–82. 10.1093/bioinformatics/btn577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bobrow CS, Holmes RP, Muttukrishna S, Mohan A, Groome N, Murphy DJ, et al. (2002) Maternal serum activin A, inhibin A, and follistatin in pregnancies with appropriately grown and small-for-gestational-age fetuses classified by umbilical artery Doppler ultrasound. Am J Obstet Gynecol 186: 283–287. [DOI] [PubMed] [Google Scholar]
- 79.Melchiorre K, Leslie K, Prefumo F, Bhide A, Thilaganathan B (2009) First-trimester uterine artery Doppler indices in the prediction of small-for-gestational age pregnancy and intrauterine growth restriction. Ultrasound Obstet Gynecol 33: 524–529. 10.1002/uog.6368 [DOI] [PubMed] [Google Scholar]
- 80.Karagiannis G, Akolekar R, Sarquis R, Wright D, Nicolaides KH (2011) Prediction of small-for-gestation neonates from biophysical and biochemical markers at 11–13 weeks. Fetal Diagn Ther 29: 148–154. 10.1159/000321694 [DOI] [PubMed] [Google Scholar]
- 81.Crovetto F, Triunfo S, Crispi F, Rodriguez-Sureda V, Roma E, Dominguez C, et al. (2016) First-trimester screening with specific algorithms for early- and late-onset fetal growth restriction. Ultrasound Obstet Gynecol 48: 340–348. 10.1002/uog.15879 [DOI] [PubMed] [Google Scholar]
- 82.Parry S, Sciscione A, Haas DM, Grobman WA, Iams JD, Mercer BM, et al. (2017) Role of early second-trimester uterine artery Doppler screening to predict small-for-gestational-age babies in nulliparous women. Am J Obstet Gynecol: 30749–30744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Spencer K, Cowans NJ, Molina F, Kagan KO, Nicolaides KH (2008) First-trimester ultrasound and biochemical markers of aneuploidy and the prediction of preterm or early preterm delivery. Ultrasound Obstet Gynecol 31: 147–152. 10.1002/uog.5163 [DOI] [PubMed] [Google Scholar]
- 84.Antsaklis P, Daskalakis G, Pilalis A, Papantoniou N, Mesogitis S, Antsaklis A (2011) The role of cervical length measurement at 11–14 weeks for the prediction of preterm delivery. J Matern Fetal Neonatal Med 24: 465–470. 10.3109/14767058.2010.501124 [DOI] [PubMed] [Google Scholar]
- 85.Bakalis SP, Poon LC, Vayna AM, Pafilis I, Nicolaides KH (2012) C-reactive protein at 11–13 weeks' gestation in spontaneous early preterm delivery. J Matern Fetal Neonatal Med 25: 2475–2478. 10.3109/14767058.2012.717127 [DOI] [PubMed] [Google Scholar]
- 86.Gervasi MT, Romero R, Bracalente G, Erez O, Dong Z, Hassan SS, et al. (2012) Midtrimester amniotic fluid concentrations of interleukin-6 and interferon-gamma-inducible protein-10: evidence for heterogeneity of intra-amniotic inflammation and associations with spontaneous early (<32 weeks) and late (>32 weeks) preterm delivery. J Perinat Med 40: 329–343. 10.1515/jpm-2012-0034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Greco E, Gupta R, Syngelaki A, Poon LC, Nicolaides KH (2012) First-trimester screening for spontaneous preterm delivery with maternal characteristics and cervical length. Fetal Diagn Ther 31: 154–161. 10.1159/000335686 [DOI] [PubMed] [Google Scholar]
- 88.Goetzinger KR, Cahill AG, Kemna J, Odibo L, Macones GA, Odibo AO (2012) First-trimester prediction of preterm birth using ADAM12, PAPP-A, uterine artery Doppler, and maternal characteristics. Prenat Diagn 32: 1002–1007. 10.1002/pd.3949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stout MJ, Goetzinger KR, Tuuli MG, Cahill AG, Macones GA, Odibo AO (2013) First trimester serum analytes, maternal characteristics and ultrasound markers to predict pregnancies at risk for preterm birth. Placenta 34: 14–19. 10.1016/j.placenta.2012.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Conde-Agudelo A, Romero R (2014) Prediction of preterm birth in twin gestations using biophysical and biochemical tests. Am J Obstet Gynecol 211: 583–595. 10.1016/j.ajog.2014.07.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Parra-Cordero M, Sepulveda-Martinez A, Rencoret G, Valdes E, Pedraza D, Munoz H (2014) Is there a role for cervical assessment and uterine artery Doppler in the first trimester of pregnancy as a screening test for spontaneous preterm delivery? Ultrasound Obstet Gynecol 43: 291–296. 10.1002/uog.12465 [DOI] [PubMed] [Google Scholar]
- 92.Ekin A, Gezer C, Kulhan G, Avci ME, Taner CE (2015) Can platelet count and mean platelet volume during the first trimester of pregnancy predict preterm premature rupture of membranes? J Obstet Gynaecol Res 41: 23–28. 10.1111/jog.12484 [DOI] [PubMed] [Google Scholar]
- 93.Quezada MS, Francisco C, Dumitrascu-Biris D, Nicolaides KH, Poon LC (2015) Fetal fraction of cell-free DNA in maternal plasma in the prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol 45: 101–105. 10.1002/uog.14666 [DOI] [PubMed] [Google Scholar]
- 94.Kim SM, Romero R, Lee J, Chaemsaithong P, Lee MW, Chaiyasit N, et al. (2016) About one-half of early spontaneous preterm deliveries can be identified by a rapid matrix metalloproteinase-8 (MMP-8) bedside test at the time of mid-trimester genetic amniocentesis. J Matern Fetal Neonatal Med 29: 2414–2422. 10.3109/14767058.2015.1094049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chaiworapongsa T, Romero R, Korzeniewski SJ, Kusanovic JP, Soto E, Lam J, et al. (2013) Maternal plasma concentrations of angiogenic/antiangiogenic factors in the third trimester of pregnancy to identify the patient at risk for stillbirth at or near term and severe late preeclampsia. Am J Obstet Gynecol 208: 287.e281-287.e215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Conde-Agudelo A, Bird S, Kennedy SH, Villar J, Papageorghiou AT (2015) First- and second-trimester tests to predict stillbirth in unselected pregnant women: a systematic review and meta-analysis. Bjog 122: 41–55. 10.1111/1471-0528.13096 [DOI] [PubMed] [Google Scholar]
- 97.Akolekar R, Machuca M, Mendes M, Paschos V, Nicolaides KH (2016) Prediction of stillbirth from placental growth factor at 11–13 weeks. Ultrasound Obstet Gynecol 48: 618–623. 10.1002/uog.17288 [DOI] [PubMed] [Google Scholar]
- 98.Aupont JE, Akolekar R, Illian A, Neonakis S, Nicolaides KH (2016) Prediction of stillbirth from placental growth factor at 19–24 weeks. Ultrasound Obstet Gynecol 48: 631–635. 10.1002/uog.17229 [DOI] [PubMed] [Google Scholar]
- 99.Familiari A, Scala C, Morlando M, Bhide A, Khalil A, Thilaganathan B (2016) Mid-pregnancy fetal growth, uteroplacental Doppler indices and maternal demographic characteristics: role in prediction of stillbirth. Acta Obstet Gynecol Scand 95: 1313–1318. 10.1111/aogs.13012 [DOI] [PubMed] [Google Scholar]
- 100.Akolekar R, Tokunaka M, Ortega N, Syngelaki A, Nicolaides KH (2016) Prediction of stillbirth from maternal factors, fetal biometry and uterine artery Doppler at 19–24 weeks. Ultrasound Obstet Gynecol 48: 624–630. 10.1002/uog.17295 [DOI] [PubMed] [Google Scholar]
- 101.Kayode GA, Grobbee DE, Amoakoh-Coleman M, Adeleke IT, Ansah E, de Groot JA, et al. (2016) Predicting stillbirth in a low resource setting. BMC Pregnancy Childbirth 16: 274 10.1186/s12884-016-1061-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Khalil A, Morales-Rosello J, Townsend R, Morlando M, Papageorghiou A, Bhide A, et al. (2016) Value of third-trimester cerebroplacental ratio and uterine artery Doppler indices as predictors of stillbirth and perinatal loss. Ultrasound Obstet Gynecol 47: 74–80. 10.1002/uog.15729 [DOI] [PubMed] [Google Scholar]
- 103.Mastrodima S, Akolekar R, Yerlikaya G, Tzelepis T, Nicolaides KH (2016) Prediction of stillbirth from biochemical and biophysical markers at 11–13 weeks. Ultrasound Obstet Gynecol 48: 613–617. 10.1002/uog.17289 [DOI] [PubMed] [Google Scholar]
- 104.Yerlikaya G, Akolekar R, McPherson K, Syngelaki A, Nicolaides KH (2016) Prediction of stillbirth from maternal demographic and pregnancy characteristics. Ultrasound Obstet Gynecol 48: 607–612. 10.1002/uog.17290 [DOI] [PubMed] [Google Scholar]
- 105.Trudell AS, Tuuli MG, Colditz GA, Macones GA, Odibo AO (2017) A stillbirth calculator: Development and internal validation of a clinical prediction model to quantify stillbirth risk. PLoS One 12: e0173461 10.1371/journal.pone.0173461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Madazli R, Kuseyrioglu B, Uzun H, Uludag S, Ocak V (2005) Prediction of preeclampsia with maternal mid-trimester placental growth factor, activin A, fibronectin and uterine artery Doppler velocimetry. Int J Gynaecol Obstet 89: 251–257. 10.1016/j.ijgo.2005.02.008 [DOI] [PubMed] [Google Scholar]
- 107.Poon LC, Karagiannis G, Leal A, Romero XC, Nicolaides KH (2009) Hypertensive disorders in pregnancy: screening by uterine artery Doppler imaging and blood pressure at 11–13 weeks. Ultrasound Obstet Gynecol 34: 497–502. 10.1002/uog.7439 [DOI] [PubMed] [Google Scholar]
- 108.Conde-Agudelo A, Romero R, James MR (2015) Tests to Predict Preeclampsia In: Taylor RN, Roberts JM, Cunningham FG, Lindheimer MD, Chesley LC, editors. Chesley's Hypertensive disorders in pregnancy. Fourth Edition ed. Amsterdam; Boston: Elsevier/AP, Academic Press is an imprint of Elsevier,. pp. 221–251. [Google Scholar]
- 109.Yliniemi A, Makikallio K, Korpimaki T, Kouru H, Marttala J, Ryynanen M (2015) Combination of PAPPA, fhCGbeta, AFP, PlGF, sTNFR1, and Maternal Characteristics in Prediction of Early-onset Preeclampsia. Clin Med Insights Reprod Health 9: 13–20. 10.4137/CMRH.S21865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Brunelli VB, Prefumo F (2015) Quality of first trimester risk prediction models for pre-eclampsia: a systematic review. Bjog 122: 904–914. 10.1111/1471-0528.13334 [DOI] [PubMed] [Google Scholar]
- 111.Scazzocchio E, Crovetto F, Triunfo S, Gratacos E, Figueras F (2017) Validation of a first-trimester screening model for pre-eclampsia in an unselected population. Ultrasound Obstet Gynecol 49: 188–193. 10.1002/uog.15982 [DOI] [PubMed] [Google Scholar]
- 112.Guizani M, Valsamis J, Dutemeyer V, Kang X, Ceccoti V, Khalife J, et al. (2017) First-Trimester Combined Multimarker Prospective Study for the Detection of Pregnancies at a High Risk of Developing Preeclampsia Using the Fetal Medicine Foundation-Algorithm. Fetal Diagn Ther: 1–8. [DOI] [PubMed] [Google Scholar]
- 113.Park HJ, Kim SH, Jung YW, Shim SS, Kim JY, Cho YK, et al. (2014) Screening models using multiple markers for early detection of late-onset preeclampsia in low-risk pregnancy. BMC Pregnancy Childbirth 14: 35 10.1186/1471-2393-14-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sibai BM, Gordon T, Thom E, Caritis SN, Klebanoff M, McNellis D, et al. (1995) Risk factors for preeclampsia in healthy nulliparous women: a prospective multicenter study. The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. Am J Obstet Gynecol 172: 642–648. [DOI] [PubMed] [Google Scholar]
- 115.Sibai BM, Ewell M, Levine RJ, Klebanoff MA, Esterlitz J, Catalano PM, et al. (1997) Risk factors associated with preeclampsia in healthy nulliparous women. The Calcium for Preeclampsia Prevention (CPEP) Study Group. Am J Obstet Gynecol 177: 1003–1010. [DOI] [PubMed] [Google Scholar]
- 116.Poon LC, Kametas NA, Chelemen T, Leal A, Nicolaides KH (2010) Maternal risk factors for hypertensive disorders in pregnancy: a multivariate approach. J Hum Hypertens 24: 104–110. 10.1038/jhh.2009.45 [DOI] [PubMed] [Google Scholar]
- 117.Wright D, Syngelaki A, Akolekar R, Poon LC, Nicolaides KH (2015) Competing risks model in screening for preeclampsia by maternal characteristics and medical history. Am J Obstet Gynecol 213: 62.e61-10. [DOI] [PubMed] [Google Scholar]
- 118.Rocha RS, Alves JA, Maia EHMSB, Araujo Junior E, Peixoto AB, Santana EF, et al. (2017) Simple approach based on maternal characteristics and mean arterial pressure for the prediction of preeclampsia in the first trimester of pregnancy. J Perinat Med. [DOI] [PubMed] [Google Scholar]
- 119.Crispi F, Dominguez C, Llurba E, Martin-Gallan P, Cabero L, Gratacos E (2006) Placental angiogenic growth factors and uterine artery Doppler findings for characterization of different subsets in preeclampsia and in isolated intrauterine growth restriction. Am J Obstet Gynecol 195: 201–207. 10.1016/j.ajog.2006.01.014 [DOI] [PubMed] [Google Scholar]
- 120.Kuc S, Wortelboer EJ, van Rijn BB, Franx A, Visser GH, Schielen PC (2011) Evaluation of 7 serum biomarkers and uterine artery Doppler ultrasound for first-trimester prediction of preeclampsia: a systematic review. Obstet Gynecol Surv 66: 225–239. 10.1097/OGX.0b013e3182227027 [DOI] [PubMed] [Google Scholar]
- 121.Tobinaga CM, Torloni MR, Gueuvoghlanian-Silva BY, Pendeloski KP, Akita PA, Sass N, et al. (2014) Angiogenic factors and uterine Doppler velocimetry in early- and late-onset preeclampsia. Acta Obstet Gynecol Scand 93: 469–476. 10.1111/aogs.12366 [DOI] [PubMed] [Google Scholar]
- 122.Seravalli V, Grimpel YI, Meiri H, Blitzer M, Baschat AA (2016) Relationship between first-trimester serum placental protein-13 and maternal characteristics, placental Doppler studies and pregnancy outcome. J Perinat Med 44: 543–549. 10.1515/jpm-2015-0324 [DOI] [PubMed] [Google Scholar]
- 123.Spencer K, Yu CK, Cowans NJ, Otigbah C, Nicolaides KH (2005) Prediction of pregnancy complications by first-trimester maternal serum PAPP-A and free beta-hCG and with second-trimester uterine artery Doppler. Prenat Diagn 25: 949–953. 10.1002/pd.1251 [DOI] [PubMed] [Google Scholar]
- 124.Spencer K, Yu CK, Savvidou M, Papageorghiou AT, Nicolaides KH (2006) Prediction of pre-eclampsia by uterine artery Doppler ultrasonography and maternal serum pregnancy-associated plasma protein-A, free beta-human chorionic gonadotropin, activin A and inhibin A at 22 + 0 to 24 + 6 weeks' gestation. Ultrasound Obstet Gynecol 27: 658–663. 10.1002/uog.2676 [DOI] [PubMed] [Google Scholar]
- 125.Poon LC, Stratieva V, Piras S, Piri S, Nicolaides KH (2010) Hypertensive disorders in pregnancy: combined screening by uterine artery Doppler, blood pressure and serum PAPP-A at 11–13 weeks. Prenat Diagn 30: 216–223. 10.1002/pd.2440 [DOI] [PubMed] [Google Scholar]
- 126.Ay E, Kavak ZN, Elter K, Gokaslan H, Pekin T (2005) Screening for pre-eclampsia by using maternal serum inhibin A, activin A, human chorionic gonadotropin, unconjugated estriol, and alpha-fetoprotein levels and uterine artery Doppler in the second trimester of pregnancy. Aust N Z J Obstet Gynaecol 45: 283–288. 10.1111/j.1479-828X.2005.00412.x [DOI] [PubMed] [Google Scholar]
- 127.Akolekar R, Minekawa R, Veduta A, Romero XC, Nicolaides KH (2009) Maternal plasma inhibin A at 11–13 weeks of gestation in hypertensive disorders of pregnancy. Prenat Diagn 29: 753–760. 10.1002/pd.2279 [DOI] [PubMed] [Google Scholar]
- 128.Yu J, Shixia CZ, Wu Y, Duan T (2011) Inhibin A, activin A, placental growth factor and uterine artery Doppler pulsatility index in the prediction of pre-eclampsia. Ultrasound Obstet Gynecol 37: 528–533. 10.1002/uog.8800 [DOI] [PubMed] [Google Scholar]
- 129.Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. (2004) Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 350: 672–683. 10.1056/NEJMoa031884 [DOI] [PubMed] [Google Scholar]
- 130.Moore AG, Young H, Keller JM, Ojo LR, Yan J, Simas TA, et al. (2012) Angiogenic biomarkers for prediction of maternal and neonatal complications in suspected preeclampsia. J Matern Fetal Neonatal Med 25: 2651–2657. 10.3109/14767058.2012.713055 [DOI] [PubMed] [Google Scholar]
- 131.Villa PM, Hamalainen E, Maki A, Raikkonen K, Pesonen AK, Taipale P, et al. (2013) Vasoactive agents for the prediction of early- and late-onset preeclampsia in a high-risk cohort. BMC Pregnancy Childbirth 13: 110 10.1186/1471-2393-13-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Allen RE, Rogozinska E, Cleverly K, Aquilina J, Thangaratinam S (2014) Abnormal blood biomarkers in early pregnancy are associated with preeclampsia: a meta-analysis. Eur J Obstet Gynecol Reprod Biol 182: 194–201. 10.1016/j.ejogrb.2014.09.027 [DOI] [PubMed] [Google Scholar]
- 133.Wataganara T, Pratumvinit B, Lahfahroengron P, Pooliam J, Talungchit P, Leetheeragul J, et al. (2017) Circulating soluble fms-like tyrosine kinase-1 and placental growth factor from 10 to 40 weeks' pregnancy in normotensive women. J Perinat Med 45: 895–901. 10.1515/jpm-2017-0093 [DOI] [PubMed] [Google Scholar]
- 134.Luo Q, Han X (2017) Second-trimester maternal serum markers in the prediction of preeclampsia. J Perinat Med 45: 809–816. 10.1515/jpm-2016-0249 [DOI] [PubMed] [Google Scholar]
- 135.Wikstrom AK, Larsson A, Eriksson UJ, Nash P, Norden-Lindeberg S, Olovsson M (2007) Placental growth factor and soluble FMS-like tyrosine kinase-1 in early-onset and late-onset preeclampsia. Obstet Gynecol 109: 1368–1374. 10.1097/01.AOG.0000264552.85436.a1 [DOI] [PubMed] [Google Scholar]
- 136.Kurtoglu E, Avci B, Kokcu A, Celik H, Cengiz Dura M, Malatyalioglu E, et al. (2016) Serum VEGF and PGF may be significant markers in prediction of severity of preeclampsia. J Matern Fetal Neonatal Med 29: 1987–1992. 10.3109/14767058.2015.1072157 [DOI] [PubMed] [Google Scholar]
- 137.Tsiakkas A, Cazacu R, Wright A, Wright D, Nicolaides KH (2016) Maternal serum placental growth factor at 12, 22, 32 and 36 weeks' gestation in screening for pre-eclampsia. Ultrasound Obstet Gynecol 47: 472–477. 10.1002/uog.15816 [DOI] [PubMed] [Google Scholar]
- 138.Tsatsaris V, Goffin F, Munaut C, Brichant JF, Pignon MR, Noel A, et al. (2003) Overexpression of the soluble vascular endothelial growth factor receptor in preeclamptic patients: pathophysiological consequences. J Clin Endocrinol Metab 88: 5555–5563. 10.1210/jc.2003-030528 [DOI] [PubMed] [Google Scholar]
- 139.Koga K, Osuga Y, Yoshino O, Hirota Y, Ruimeng X, Hirata T, et al. (2003) Elevated serum soluble vascular endothelial growth factor receptor 1 (sVEGFR-1) levels in women with preeclampsia. J Clin Endocrinol Metab 88: 2348–2351. 10.1210/jc.2002-021942 [DOI] [PubMed] [Google Scholar]
- 140.Chaiworapongsa T, Romero R, Espinoza J, Bujold E, Mee Kim Y, Goncalves LF, et al. (2004) Evidence supporting a role for blockade of the vascular endothelial growth factor system in the pathophysiology of preeclampsia. Young Investigator Award. Am J Obstet Gynecol 190: 1541–1547; discussion 1547–1550. 10.1016/j.ajog.2004.03.043 [DOI] [PubMed] [Google Scholar]
- 141.Chung JY, Song Y, Wang Y, Magness RR, Zheng J (2004) Differential expression of vascular endothelial growth factor (VEGF), endocrine gland derived-VEGF, and VEGF receptors in human placentas from normal and preeclamptic pregnancies. J Clin Endocrinol Metab 89: 2484–2490. 10.1210/jc.2003-031580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Chaiworapongsa T, Romero R, Kim YM, Kim GJ, Kim MR, Espinoza J, et al. (2005) Plasma soluble vascular endothelial growth factor receptor-1 concentration is elevated prior to the clinical diagnosis of pre-eclampsia. J Matern Fetal Neonatal Med 17: 3–18. 10.1080/14767050400028816 [DOI] [PubMed] [Google Scholar]
- 143.Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, et al. (2006) Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med 355: 992–1005. 10.1056/NEJMoa055352 [DOI] [PubMed] [Google Scholar]
- 144.Stepan H, Geipel A, Schwarz F, Kramer T, Wessel N, Faber R (2008) Circulatory soluble endoglin and its predictive value for preeclampsia in second-trimester pregnancies with abnormal uterine perfusion. Am J Obstet Gynecol 198: 175 e171-176. [DOI] [PubMed] [Google Scholar]
- 145.Chaiworapongsa T, Romero R, Kusanovic JP, Mittal P, Kim SK, Gotsch F, et al. (2010) Plasma soluble endoglin concentration in pre-eclampsia is associated with an increased impedance to flow in the maternal and fetal circulations. Ultrasound Obstet Gynecol 35: 155–162. 10.1002/uog.7491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Foidart JM, Munaut C, Chantraine F, Akolekar R, Nicolaides KH (2010) Maternal plasma soluble endoglin at 11–13 weeks' gestation in pre-eclampsia. Ultrasound Obstet Gynecol 35: 680–687. 10.1002/uog.7621 [DOI] [PubMed] [Google Scholar]
- 147.Rana S, Cerdeira AS, Wenger J, Salahuddin S, Lim KH, Ralston SJ, et al. (2012) Plasma concentrations of soluble endoglin versus standard evaluation in patients with suspected preeclampsia. PLoS One 7: e48259 10.1371/journal.pone.0048259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Lai J, Syngelaki A, Poon LC, Nucci M, Nicolaides KH (2013) Maternal serum soluble endoglin at 30–33 weeks in the prediction of preeclampsia. Fetal Diagn Ther 33: 149–155. 10.1159/000343220 [DOI] [PubMed] [Google Scholar]
- 149.De Vivo A, Baviera G, Giordano D, Todarello G, Corrado F, D'Anna R (2008) Endoglin, PlGF and sFlt-1 as markers for predicting pre-eclampsia. Acta Obstet Gynecol Scand 87: 837–842. 10.1080/00016340802253759 [DOI] [PubMed] [Google Scholar]
- 150.Baumann MU, Bersinger NA, Mohaupt MG, Raio L, Gerber S, Surbek DV (2008) First-trimester serum levels of soluble endoglin and soluble fms-like tyrosine kinase-1 as first-trimester markers for late-onset preeclampsia. Am J Obstet Gynecol 199: 266.e261-266. [DOI] [PubMed] [Google Scholar]
- 151.Kusanovic JP, Romero R, Chaiworapongsa T, Erez O, Mittal P, Vaisbuch E, et al. (2009) A prospective cohort study of the value of maternal plasma concentrations of angiogenic and anti-angiogenic factors in early pregnancy and midtrimester in the identification of patients destined to develop preeclampsia. J Matern Fetal Neonatal Med 22: 1021–1038. 10.3109/14767050902994754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Cindrova-Davies T, Sanders DA, Burton GJ, Charnock-Jones DS (2011) Soluble FLT1 sensitizes endothelial cells to inflammatory cytokines by antagonizing VEGF receptor-mediated signalling. Cardiovasc Res 89: 671–679. 10.1093/cvr/cvq346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Aggarwal PK, Chandel N, Jain V, Jha V (2012) The relationship between circulating endothelin-1, soluble fms-like tyrosine kinase-1 and soluble endoglin in preeclampsia. J Hum Hypertens 26: 236–241. 10.1038/jhh.2011.29 [DOI] [PubMed] [Google Scholar]
- 154.Cim N, Kurdoglu M, Ege S, Yoruk I, Yaman G, Yildizhan R (2016) An analysis on the roles of angiogenesis-related factors including serum vitamin D, soluble endoglin (sEng), soluble fms-like tyrosine kinase 1 (sFlt1), and vascular endothelial growth factor (VEGF) in the diagnosis and severity of late-onset preeclampsia. J Matern Fetal Neonatal Med: 1–6. [DOI] [PubMed] [Google Scholar]
- 155.Perales A, Delgado JL, de la Calle M, Garcia-Hernandez JA, Escudero AI, Campillos JM, et al. (2017) sFlt-1/PlGF for prediction of early-onset pre-eclampsia: STEPS (Study of Early Pre-eclampsia in Spain). Ultrasound Obstet Gynecol 50: 373–382. 10.1002/uog.17373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.O'Gorman N, Nicolaides KH, Poon LC (2016) The use of ultrasound and other markers for early detection of preeclampsia. Womens Health (Lond) 12: 199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Romero R, Kuivaniemi H, Tromp G (2002) Functional genomics and proteomics in term and preterm parturition. J Clin Endocrinol Metab 87: 2431–2434. 10.1210/jcem.87.6.8689 [DOI] [PubMed] [Google Scholar]
- 158.Romero R, Espinoza J, Gotsch F, Kusanovic JP, Friel LA, Erez O, et al. (2006) The use of high-dimensional biology (genomics, transcriptomics, proteomics, and metabolomics) to understand the preterm parturition syndrome. Bjog 113 Suppl 3: 118–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Romero R, Tromp G (2006) High-dimensional biology in obstetrics and gynecology: functional genomics in microarray studies. Am J Obstet Gynecol 195: 360–363. 10.1016/j.ajog.2006.06.077 [DOI] [PubMed] [Google Scholar]
- 160.Blankley RT, Robinson NJ, Aplin JD, Crocker IP, Gaskell SJ, Whetton AD, et al. (2010) A gel-free quantitative proteomics analysis of factors released from hypoxic-conditioned placentae. Reprod Sci 17: 247–257. 10.1177/1933719109351320 [DOI] [PubMed] [Google Scholar]
- 161.Cox J, Mann M (2011) Quantitative, high-resolution proteomics for data-driven systems biology. Annu Rev Biochem 80: 273–299. 10.1146/annurev-biochem-061308-093216 [DOI] [PubMed] [Google Scholar]
- 162.Klein J, Buffin-Meyer B, Mullen W, Carty DM, Delles C, Vlahou A, et al. (2014) Clinical proteomics in obstetrics and neonatology. Expert Rev Proteomics 11: 75–89. 10.1586/14789450.2014.872564 [DOI] [PubMed] [Google Scholar]
- 163.Hernandez-Nunez J, Valdes-Yong M (2015) Utility of proteomics in obstetric disorders: a review. Int J Womens Health 7: 385–391. 10.2147/IJWH.S79577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Edlow AG, Slonim DK, Wick HC, Hui L, Bianchi DW (2015) The pathway not taken: understanding 'omics data in the perinatal context. Am J Obstet Gynecol 213: 59.e51-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Kolialexi A, Mavreli D, Papantoniou N (2017) Proteomics for early prenatal screening of pregnancy complications: a 2017 perspective. Expert Rev Proteomics 14: 113–115. 10.1080/14789450.2017.1275574 [DOI] [PubMed] [Google Scholar]
- 166.Nejatizadeh A, Stobdan T, Malhotra N, Pasha MA (2008) The genetic aspects of pre-eclampsia: achievements and limitations. Biochem Genet 46: 451–479. 10.1007/s10528-008-9163-9 [DOI] [PubMed] [Google Scholar]
- 167.Johnson M, Brennecke S, Iversen AC, East C, Olsen G, Kent J, et al. (2012) OS046. Genome-wide association scans identify novel maternalsusceptibility loci for preeclampsia. Pregnancy Hypertens 2: 202. [DOI] [PubMed] [Google Scholar]
- 168.Chaiworapongsa T, Romero R, Whitten A, Tarca AL, Bhatti G, Draghici S, et al. (2013) Differences and similarities in the transcriptional profile of peripheral whole blood in early and late-onset preeclampsia: insights into the molecular basis of the phenotype of preeclampsiaa. J Perinat Med 41: 485–504. 10.1515/jpm-2013-0082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Xu P, Zhao Y, Liu M, Wang Y, Wang H, Li YX, et al. (2014) Variations of microRNAs in human placentas and plasma from preeclamptic pregnancy. Hypertension 63: 1276–1284. 10.1161/HYPERTENSIONAHA.113.02647 [DOI] [PubMed] [Google Scholar]
- 170.Yong HE, Melton PE, Johnson MP, Freed KA, Kalionis B, Murthi P, et al. (2015) Genome-wide transcriptome directed pathway analysis of maternal pre-eclampsia susceptibility genes. PLoS One 10: e0128230 10.1371/journal.pone.0128230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Sober S, Reiman M, Kikas T, Rull K, Inno R, Vaas P, et al. (2015) Extensive shift in placental transcriptome profile in preeclampsia and placental origin of adverse pregnancy outcomes. Sci Rep 5: 13336 10.1038/srep13336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Whitehead CL, Walker SP, Tong S (2016) Measuring circulating placental RNAs to non-invasively assess the placental transcriptome and to predict pregnancy complications. Prenat Diagn 36: 997–1008. 10.1002/pd.4934 [DOI] [PubMed] [Google Scholar]
- 173.Luo S, Cao N, Tang Y, Gu W (2017) Identification of key microRNAs and genes in preeclampsia by bioinformatics analysis. PLoS One 12: e0178549 10.1371/journal.pone.0178549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ashar-Patel A, Kaymaz Y, Rajakumar A, Bailey JA, Karumanchi SA, Moore MJ (2017) FLT1 and transcriptome-wide polyadenylation site (PAS) analysis in preeclampsia. Sci Rep 7: 12139 10.1038/s41598-017-11639-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Than NG, Romero R, Tarca AL, Kekesi KA, Xu Y, Xu Z, et al. (2018) Integrated Systems Biology Approach Identifies Novel Maternal and Placental Pathways of Preeclampsia. Front Immunol 9: 1661 10.3389/fimmu.2018.01661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Kolla V, Jeno P, Moes S, Lapaire O, Hoesli I, Hahn S (2012) Quantitative proteomic (iTRAQ) analysis of 1st trimester maternal plasma samples in pregnancies at risk for preeclampsia. J Biomed Biotechnol 2012: 305964 10.1155/2012/305964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Myers JE, Tuytten R, Thomas G, Laroy W, Kas K, Vanpoucke G, et al. (2013) Integrated proteomics pipeline yields novel biomarkers for predicting preeclampsia. Hypertension 61: 1281–1288. 10.1161/HYPERTENSIONAHA.113.01168 [DOI] [PubMed] [Google Scholar]
- 178.Law KP, Han TL, Tong C, Baker PN (2015) Mass spectrometry-based proteomics for pre-eclampsia and preterm birth. Int J Mol Sci 16: 10952–10985. 10.3390/ijms160510952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Founds S, Zeng X, Lykins D, Roberts JM (2015) Developing Potential Candidates of Preclinical Preeclampsia. Int J Mol Sci 16: 27208–27227. 10.3390/ijms161126023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Lu Q, Liu C, Liu Y, Zhang N, Deng H, Zhang Z (2016) Serum markers of pre-eclampsia identified on proteomics. J Obstet Gynaecol Res 42: 1111–1118. 10.1111/jog.13037 [DOI] [PubMed] [Google Scholar]
- 181.Jin X, Xu Z, Cao J, Shao P, Zhou M, Qin Z, et al. (2017) Proteomics analysis of human placenta reveals glutathione metabolism dysfunction as the underlying pathogenesis for preeclampsia. Biochim Biophys Acta 1865: 1207–1214. [DOI] [PubMed] [Google Scholar]
- 182.Qi WH, Zheng MY, Li C, Xu L, Xu JE (2017) Screening of differential proteins of placenta tissues in patients with pre-eclampsia by iTRAQ proteomics techniques. Minerva Med 108: 389–395. 10.23736/S0026-4806.17.05080-7 [DOI] [PubMed] [Google Scholar]
- 183.Lynch AM, Wagner BD, Deterding RR, Giclas PC, Gibbs RS, Janoff EN, et al. (2015) The relationship of circulating proteins in early pregnancy with preterm birth. Am J Obstet Gynecol 214: 517.e511-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Myers J, Macleod M, Reed B, Harris N, Mires G, Baker P (2004) Use of proteomic patterns as a novel screening tool in pre-eclampsia. J Obstet Gynaecol 24: 873–874. 10.1080/01443610400018791 [DOI] [PubMed] [Google Scholar]
- 185.Webster RP, Myatt L (2007) Elucidation of the molecular mechanisms of preeclampsia using proteomic technologies. Proteomics Clin Appl 1: 1147–1155. 10.1002/prca.200700128 [DOI] [PubMed] [Google Scholar]
- 186.Baker PN, Myers JE (2009) Preeclamptic toxemia: a disease ripe for proteomic discovery. Expert Rev Proteomics 6: 107–110. 10.1586/epr.09.5 [DOI] [PubMed] [Google Scholar]
- 187.Carty DM, Schiffer E, Delles C (2013) Proteomics in hypertension. J Hum Hypertens 27: 211–216. 10.1038/jhh.2012.30 [DOI] [PubMed] [Google Scholar]
- 188.Bahado-Singh RO, Akolekar R, Mandal R, Dong E, Xia J, Kruger M, et al. (2012) Metabolomics and first-trimester prediction of early-onset preeclampsia. J Matern Fetal Neonatal Med 25: 1840–1847. 10.3109/14767058.2012.680254 [DOI] [PubMed] [Google Scholar]
- 189.Kuc S, Koster MP, Pennings JL, Hankemeier T, Berger R, Harms AC, et al. (2014) Metabolomics profiling for identification of novel potential markers in early prediction of preeclampsia. PLoS One 9: e98540 10.1371/journal.pone.0098540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Austdal M, Tangeras LH, Skrastad RB, Salvesen K, Austgulen R, Iversen AC, et al. (2015) First Trimester Urine and Serum Metabolomics for Prediction of Preeclampsia and Gestational Hypertension: A Prospective Screening Study. Int J Mol Sci 16: 21520–21538. 10.3390/ijms160921520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Koster MP, Vreeken RJ, Harms AC, Dane AD, Kuc S, Schielen PC, et al. (2015) First-Trimester Serum Acylcarnitine Levels to Predict Preeclampsia: A Metabolomics Approach. Dis Markers 2015: 857108 10.1155/2015/857108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Benton SJ, Ly C, Vukovic S, Bainbridge SA (2016) Andree Gruslin award lecture: Metabolomics as an important modality to better understand preeclampsia. Placenta: 1–9. [DOI] [PubMed] [Google Scholar]
- 193.de Groot CJ, Guzel C, Steegers-Theunissen RP, de Maat M, Derkx P, Roes EM, et al. (2007) Specific peptides identified by mass spectrometry in placental tissue from pregnancies complicated by early onset preeclampsia attained by laser capture dissection. Proteomics Clin Appl 1: 325–335. 10.1002/prca.200600911 [DOI] [PubMed] [Google Scholar]
- 194.Hamamura K, Nonaka D, Ishikawa H, Banzai M, Yanagida M, Nojima M, et al. (2016) Simple quantitation for potential serum disease biomarker peptides, primarily identified by a peptidomics approach in the serum with hypertensive disorders of pregnancy. Ann Clin Biochem 53: 85–96. 10.1177/0004563215583697 [DOI] [PubMed] [Google Scholar]
- 195.Kononikhin AS, Starodubtseva NL, Bugrova AE, Shirokova VA, Chagovets VV, Indeykina MI, et al. (2016) An untargeted approach for the analysis of the urine peptidome of women with preeclampsia. J Proteomics 149: 38–43. 10.1016/j.jprot.2016.04.024 [DOI] [PubMed] [Google Scholar]
- 196.Kedia K, Smith SF, Wright AH, Barnes JM, Tolley HD, Esplin MS, et al. (2016) Global "omics" evaluation of human placental responses to preeclamptic conditions. Am J Obstet Gynecol 215: 238.e231-238.e220. [DOI] [PubMed] [Google Scholar]
- 197.Dai X, Song X, Rui C, Meng L, Xue X, Ding H, et al. (2017) Peptidome Analysis of Human Serum From Normal and Preeclamptic Pregnancies. J Cell Biochem: 1–8. [DOI] [PubMed] [Google Scholar]
- 198.Qian Y, Zhang L, Rui C, Ding H, Mao P, Ruan H, et al. (2017) Peptidome analysis of amniotic fluid from pregnancies with preeclampsia. Mol Med Rep: 7337–7344. 10.3892/mmr.2017.7582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Anand S, Young S, Esplin MS, Peaden B, Tolley HD, Porter TF, et al. (2016) Detection and confirmation of serum lipid biomarkers for preeclampsia using direct infusion mass spectrometry. J Lipid Res 57: 687–696. 10.1194/jlr.P064451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Brown SH, Eather SR, Freeman DJ, Meyer BJ, Mitchell TW (2016) A Lipidomic Analysis of Placenta in Preeclampsia: Evidence for Lipid Storage. PLoS One 11: e0163972 10.1371/journal.pone.0163972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Watanabe H, Hamada H, Yamada N, Sohda S, Yamakawa-Kobayashi K, Yoshikawa H, et al. (2004) Proteome analysis reveals elevated serum levels of clusterin in patients with preeclampsia. Proteomics 4: 537–543. 10.1002/pmic.200300565 [DOI] [PubMed] [Google Scholar]
- 202.Blankley RT, Gaskell SJ, Whetton AD, Dive C, Baker PN, Myers JE (2009) A proof-of-principle gel-free proteomics strategy for the identification of predictive biomarkers for the onset of pre-eclampsia. Bjog 116: 1473–1480. 10.1111/j.1471-0528.2009.02283.x [DOI] [PubMed] [Google Scholar]
- 203.Auer J, Camoin L, Guillonneau F, Rigourd V, Chelbi ST, Leduc M, et al. (2010) Serum profile in preeclampsia and intra-uterine growth restriction revealed by iTRAQ technology. J Proteomics 73: 1004–1017. 10.1016/j.jprot.2009.12.014 [DOI] [PubMed] [Google Scholar]
- 204.Rasanen J, Girsen A, Lu X, Lapidus JA, Standley M, Reddy A, et al. (2010) Comprehensive maternal serum proteomic profiles of preclinical and clinical preeclampsia. J Proteome Res 9: 4274–4281. 10.1021/pr100198m [DOI] [PubMed] [Google Scholar]
- 205.Liu C, Zhang N, Yu H, Chen Y, Liang Y, Deng H, et al. (2011) Proteomic analysis of human serum for finding pathogenic factors and potential biomarkers in preeclampsia. Placenta 32: 168–174. 10.1016/j.placenta.2010.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Hsu TY, Hsieh TT, Yang KD, Tsai CC, Ou CY, Cheng BH, et al. (2015) Proteomic profiling reveals alpha1-antitrypsin, alpha1-microglobulin, and clusterin as preeclampsia-related serum proteins in pregnant women. Taiwan J Obstet Gynecol 54: 499–504. 10.1016/j.tjog.2014.01.007 [DOI] [PubMed] [Google Scholar]
- 207.Kolialexi A, Gourgiotis D, Daskalakis G, Marmarinos A, Lykoudi A, Mavreli D, et al. (2015) Validation of serum biomarkers derived from proteomic analysis for the early screening of preeclampsia. Dis Markers 2015: 121848 10.1155/2015/121848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Anand S, Bench Alvarez TM, Johnson WE, Esplin MS, Merrell K, Porter TF, et al. (2015) Serum biomarkers predictive of pre-eclampsia. Biomark Med 9: 563–575. 10.2217/bmm.15.21 [DOI] [PubMed] [Google Scholar]
- 209.Kim SM, Cho BK, Kang MJ, Norwitz ER, Lee SM, Lee J, et al. (2016) Expression changes of proteins associated with the development of preeclampsia in maternal plasma: A case-control study. Proteomics 16: 1581–1589. 10.1002/pmic.201500381 [DOI] [PubMed] [Google Scholar]
- 210.Kolialexi A, Tsangaris GT, Sifakis S, Gourgiotis D, Katsafadou A, Lykoudi A, et al. (2017) Plasma biomarkers for the identification of women at risk for early-onset preeclampsia. Expert Rev Proteomics 14: 269–276. 10.1080/14789450.2017.1291345 [DOI] [PubMed] [Google Scholar]
- 211.Chen G, Zhang Y, Jin X, Zhang L, Zhou Y, Niu J, et al. (2011) Urinary proteomics analysis for renal injury in hypertensive disorders of pregnancy with iTRAQ labeling and LC-MS/MS. Proteomics Clin Appl 5: 300–310. 10.1002/prca.201000100 [DOI] [PubMed] [Google Scholar]
- 212.Lee SM, Park JS, Norwitz ER, Kim SM, Kim BJ, Park CW, et al. (2011) Characterization of discriminatory urinary proteomic biomarkers for severe preeclampsia using SELDI-TOF mass spectrometry. J Perinat Med 39: 391–396. 10.1515/JPM.2011.028 [DOI] [PubMed] [Google Scholar]
- 213.Kolialexi A, Mavreli D, Tounta G, Mavrou A, Papantoniou N (2015) Urine proteomic studies in preeclampsia. Proteomics Clin Appl 9: 501–506. 10.1002/prca.201400092 [DOI] [PubMed] [Google Scholar]
- 214.Vascotto C, Salzano AM, D'Ambrosio C, Fruscalzo A, Marchesoni D, di Loreto C, et al. (2007) Oxidized transthyretin in amniotic fluid as an early marker of preeclampsia. J Proteome Res 6: 160–170. 10.1021/pr060315z [DOI] [PubMed] [Google Scholar]
- 215.Park JS, Oh KJ, Norwitz ER, Han JS, Choi HJ, Seong HS, et al. (2008) Identification of proteomic biomarkers of preeclampsia in amniotic fluid using SELDI-TOF mass spectrometry. Reprod Sci 15: 457–468. 10.1177/1933719108316909 [DOI] [PubMed] [Google Scholar]
- 216.Webster RP, Pitzer BA, Roberts VH, Brockman D, Myatt L (2007) Differences in the proteome profile in placenta from normal term and preeclamptic preterm pregnancies. Proteomics Clin Appl 1: 446–456. 10.1002/prca.200600745 [DOI] [PubMed] [Google Scholar]
- 217.Sun LZ, Yang NN, De W, Xiao YS (2007) Proteomic analysis of proteins differentially expressed in preeclamptic trophoblasts. Gynecol Obstet Invest 64: 17–23. 10.1159/000098399 [DOI] [PubMed] [Google Scholar]
- 218.Kim YN, Kim HK, Warda M, Kim N, Park WS, Prince Adel B, et al. (2007) Toward a better understanding of preeclampsia: Comparative proteomic analysis of preeclamptic placentas. Proteomics Clin Appl 1: 1625–1636. 10.1002/prca.200700034 [DOI] [PubMed] [Google Scholar]
- 219.Jin H, Ma KD, Hu R, Chen Y, Yang F, Yao J, et al. (2008) Analysis of expression and comparative profile of normal placental tissue proteins and those in preeclampsia patients using proteomic approaches. Anal Chim Acta 629: 158–164. 10.1016/j.aca.2008.09.015 [DOI] [PubMed] [Google Scholar]
- 220.Gharesi-Fard B, Zolghadri J, Kamali-Sarvestani E (2010) Proteome differences of placenta between pre-eclampsia and normal pregnancy. Placenta 31: 121–125. 10.1016/j.placenta.2009.11.004 [DOI] [PubMed] [Google Scholar]
- 221.Centlow M, Hansson SR, Welinder C (2010) Differential proteome analysis of the preeclamptic placenta using optimized protein extraction. J Biomed Biotechnol 2010: 458748 10.1155/2010/458748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Shin JK, Baek JC, Kang MY, Park JK, Lee SA, Lee JH, et al. (2011) Proteomic analysis reveals an elevated expression of heat shock protein 27 in preeclamptic placentas. Gynecol Obstet Invest 71: 151–157. 10.1159/000315162 [DOI] [PubMed] [Google Scholar]
- 223.Feng YL, Zhou CJ, Li XM, Liang XQ (2012) Alpha-1-antitrypsin acts as a preeclampsia-related protein: a proteomic study. Gynecol Obstet Invest 73: 252–259. 10.1159/000334820 [DOI] [PubMed] [Google Scholar]
- 224.Epiney M, Ribaux P, Arboit P, Irion O, Cohen M (2012) Comparative analysis of secreted proteins from normal and preeclamptic trophoblastic cells using proteomic approaches. J Proteomics 75: 1771–1777. 10.1016/j.jprot.2011.12.021 [DOI] [PubMed] [Google Scholar]
- 225.Baig S, Kothandaraman N, Manikandan J, Rong L, Ee KH, Hill J, et al. (2014) Proteomic analysis of human placental syncytiotrophoblast microvesicles in preeclampsia. Clin Proteomics 11: 40 10.1186/1559-0275-11-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Ma K, Jin H, Hu R, Xiong Y, Zhou S, Ting P, et al. (2014) A proteomic analysis of placental trophoblastic cells in preeclampsia-eclampsia. Cell Biochem Biophys 69: 247–258. 10.1007/s12013-013-9792-4 [DOI] [PubMed] [Google Scholar]
- 227.Yang JI, Kong TW, Kim HS, Kim HY (2015) The Proteomic Analysis of Human Placenta with Pre-eclampsia and Normal Pregnancy. J Korean Med Sci 30: 770–778. 10.3346/jkms.2015.30.6.770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Mary S, Kulkarni MJ, Malakar D, Joshi SR, Mehendale SS, Giri AP (2017) Placental Proteomics Provides Insights into Pathophysiology of Pre-Eclampsia and Predicts Possible Markers in Plasma. J Proteome Res 16: 1050–1060. 10.1021/acs.jproteome.6b00955 [DOI] [PubMed] [Google Scholar]
- 229.Romero R, Erez O, Maymon E, Chaemsaithong P, Xu Z, Pacora P, et al. (2017) The maternal plasma proteome changes as a function of gestational age in normal pregnancy: a longitudinal study. Am J Obstet Gynecol 217: 67.e61-67.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Aghaeepour N, Lehallier B, Baca Q, Ganio EA, Wong RJ, Ghaemi MS, et al. (2018) A proteomic clock of human pregnancy. Am J Obstet Gynecol 218: 347.e341-347.e314. [DOI] [PubMed] [Google Scholar]
- 231.Vettraino IM, Roby J, Tolley T, Parks WC (1996) Collagenase-I, stromelysin-I, and matrilysin are expressed within the placenta during multiple stages of human pregnancy. Placenta 17: 557–563. [DOI] [PubMed] [Google Scholar]
- 232.Weiss A, Goldman S, Shalev E (2007) The matrix metalloproteinases (MMPS) in the decidua and fetal membranes. Front Biosci 12: 649–659. [DOI] [PubMed] [Google Scholar]
- 233.Reister F, Kingdom JC, Ruck P, Marzusch K, Heyl W, Pauer U, et al. (2006) Altered protease expression by periarterial trophoblast cells in severe early-onset preeclampsia with IUGR. J Perinat Med 34: 272–279. 10.1515/JPM.2006.052 [DOI] [PubMed] [Google Scholar]
- 234.Smith SD, Dunk CE, Aplin JD, Harris LK, Jones RL (2009) Evidence for immune cell involvement in decidual spiral arteriole remodeling in early human pregnancy. Am J Pathol 174: 1959–1971. 10.2353/ajpath.2009.080995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Li Q, Park PW, Wilson CL, Parks WC (2002) Matrilysin shedding of syndecan-1 regulates chemokine mobilization and transepithelial efflux of neutrophils in acute lung injury. Cell 111: 635–646. [DOI] [PubMed] [Google Scholar]
- 236.Manon-Jensen T, Multhaupt HA, Couchman JR (2013) Mapping of matrix metalloproteinase cleavage sites on syndecan-1 and syndecan-4 ectodomains. FEBS J 280: 2320–2331. 10.1111/febs.12174 [DOI] [PubMed] [Google Scholar]
- 237.Jokimaa V, Inki P, Kujari H, Hirvonen O, Ekholm E, Anttila L (1998) Expression of syndecan-1 in human placenta and decidua. Placenta 19: 157–163. [DOI] [PubMed] [Google Scholar]
- 238.Stepp MA, Pal-Ghosh S, Tadvalkar G, Pajoohesh-Ganji A (2015) Syndecan-1 and Its Expanding List of Contacts. Adv Wound Care (New Rochelle) 4: 235–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Teng YH, Aquino RS, Park PW (2012) Molecular functions of syndecan-1 in disease. Matrix Biol 31: 3–16. 10.1016/j.matbio.2011.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Gandley RE, Althouse A, Jeyabalan A, Bregand-White JM, McGonigal S, Myerski AC, et al. (2016) Low Soluble Syndecan-1 Precedes Preeclampsia. PLoS One 11: e0157608 10.1371/journal.pone.0157608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Alici Davutoglu E, Akkaya Firat A, Ozel A, Yilmaz N, Uzun I, Temel Yuksel I, et al. (2018) Evaluation of maternal serum hypoxia inducible factor-1alpha, progranulin and syndecan-1 levels in pregnancies with early- and late-onset preeclampsia. J Matern Fetal Neonatal Med 31: 1976–1982. 10.1080/14767058.2017.1333098 [DOI] [PubMed] [Google Scholar]
- 242.Jokimaa VI, Kujari HP, Ekholm EM, Inki PL, Anttila L (2000) Placental expression of syndecan 1 is diminished in preeclampsia. Am J Obstet Gynecol 183: 1495–1498. 10.1067/mob.2000.107320 [DOI] [PubMed] [Google Scholar]
- 243.Szabo S, Xu Y, Romero R, Fule T, Karaszi K, Bhatti G, et al. (2013) Changes of placental syndecan-1 expression in preeclampsia and HELLP syndrome. Virchows Arch 463: 445–458. 10.1007/s00428-013-1426-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Halpert I, Sires UI, Roby JD, Potter-Perigo S, Wight TN, Shapiro SD, et al. (1996) Matrilysin is expressed by lipid-laden macrophages at sites of potential rupture in atherosclerotic lesions and localizes to areas of versican deposition, a proteoglycan substrate for the enzyme. Proc Natl Acad Sci U S A 93: 9748–9753. 10.1073/pnas.93.18.9748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Katabuchi H, Yih S, Ohba T, Matsui K, Takahashi K, Takeya M, et al. (2003) Characterization of macrophages in the decidual atherotic spiral artery with special reference to the cytology of foam cells. Med Electron Microsc 36: 253–262. 10.1007/s00795-003-0223-2 [DOI] [PubMed] [Google Scholar]
- 246.Kim YM, Chaemsaithong P, Romero R, Shaman M, Kim CJ, Kim JS, et al. (2015) The frequency of acute atherosis in normal pregnancy and preterm labor, preeclampsia, small-for-gestational age, fetal death and midtrimester spontaneous abortion. J Matern Fetal Neonatal Med 28: 2001–2009. 10.3109/14767058.2014.976198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Elangbam CS, Qualls CW Jr., Dahlgren RR (1997) Cell adhesion molecules—update. Vet Pathol 34: 61–73. 10.1177/030098589703400113 [DOI] [PubMed] [Google Scholar]
- 248.Tomer A (2004) Platelet activation as a marker for in vivo prothrombotic activity: detection by flow cytometry. J Biol Regul Homeost Agents 18: 172–177. [PubMed] [Google Scholar]
- 249.Takagi J, Petre BM, Walz T, Springer TA (2002) Global conformational rearrangements in integrin extracellular domains in outside-in and inside-out signaling. Cell 110: 599–511. [DOI] [PubMed] [Google Scholar]
- 250.Pytela R, Pierschbacher MD, Ginsberg MH, Plow EF, Ruoslahti E (1986) Platelet membrane glycoprotein IIb/IIIa: member of a family of Arg-Gly-Asp—specific adhesion receptors. Science 231: 1559–1562. [DOI] [PubMed] [Google Scholar]
- 251.Janes SL, Goodall AH (1994) Flow cytometric detection of circulating activated platelets and platelet hyper-responsiveness in pre-eclampsia and pregnancy. Clin Sci (Lond) 86: 731–739. [DOI] [PubMed] [Google Scholar]
- 252.Hodivala-Dilke KM, McHugh KP, Tsakiris DA, Rayburn H, Crowley D, Ullman-Cullere M, et al. (1999) Beta3-integrin-deficient mice are a model for Glanzmann thrombasthenia showing placental defects and reduced survival. J Clin Invest 103: 229–238. 10.1172/JCI5487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Tronik-Le Roux D, Roullot V, Poujol C, Kortulewski T, Nurden P, Marguerie G (2000) Thrombasthenic mice generated by replacement of the integrin alpha(IIb) gene: demonstration that transcriptional activation of this megakaryocytic locus precedes lineage commitment. Blood 96: 1399–1408. [PubMed] [Google Scholar]
- 254.McKenzie ME, Malinin AI, Bell CR, Dzhanashvili A, Horowitz ED, Oshrine BR, et al. (2003) Aspirin inhibits surface glycoprotein IIb/IIIa, P-selectin, CD63, and CD107a receptor expression on human platelets. Blood Coagul Fibrinolysis 14: 249–253. 10.1097/01.mbc.0000046182.72384.ab [DOI] [PubMed] [Google Scholar]
- 255.LeFevre ML (2014) Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 161: 819–826. 10.7326/M14-1884 [DOI] [PubMed] [Google Scholar]
- 256.ACOG American College of Obstetricians and Gynecologists: Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. Washington, DC: 2016. https://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations.
- 257.Seidler AL, Askie L, Ray JG (2018) Optimal aspirin dosing for preeclampsia prevention. Am J Obstet Gynecol 219: 117–118. 10.1016/j.ajog.2018.03.018 [DOI] [PubMed] [Google Scholar]
- 258.Than N, Romero R, Tarca A, Kekesi K, Xu Y, Juhasz K, et al. (2017) Systems biology identifies key molecular networks and hub factors in placental pathways of preeclampsia. Reproductive Sciences, 24(1 Suppl), 278A. [Google Scholar]
- 259.Spencer K, Macri JN, Aitken DA, Connor JM (1992) Free beta-hCG as first-trimester marker for fetal trisomy. Lancet 339: 1480. [DOI] [PubMed] [Google Scholar]
- 260.Spencer K (2000) Second-trimester prenatal screening for Down syndrome and the relationship of maternal serum biochemical markers to pregnancy complications with adverse outcome. Prenat Diagn 20: 652–656. [PubMed] [Google Scholar]
- 261.Kagan KO, Wright D, Spencer K, Molina FS, Nicolaides KH (2008) First-trimester screening for trisomy 21 by free beta-human chorionic gonadotropin and pregnancy-associated plasma protein-A: impact of maternal and pregnancy characteristics. Ultrasound Obstet Gynecol 31: 493–502. 10.1002/uog.5332 [DOI] [PubMed] [Google Scholar]
- 262.Colosi E, D'Ambrosio V, Periti E (2016) First trimester contingent screening for trisomies 21,18,13: is this model cost efficient and feasible in public health system? J Matern Fetal Neonatal Med: 1–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The number in parentheses following the name of each protein (column Predictor Symbols) represents the percentage of folds in which the protein was selected in the best model. Only proteins selected in 10% or more of the 3x67 = 201 folds are listed. ACE2: angiotensin converting enzyme 2; ALCAM: activated leukocyte cell adhesion molecule; AUC: area under the receiver operating characteristic curve; GA: gestational age; gpIIbIIIa: glycoprotein IIb/IIIa; HMG-1: high-mobility group protein 1; MMP: matrix metalloproteinase; early PE: early preeclampsia; MVM: maternal vascular malperfusion; PE: preeclampsia; PlGF: placental growth factor; Siglec-6: sialic acid binding immunoglobulin-like lectin; VEGF121: vascular endothelial growth factor A, isoform 121; vWF: von Willebrand factor.
(XLSX)
List of 175 proteins with significantly different abundance between early preeclampsia and normal pregnancy (q < 0.1) in at least one interval, after adjustment for body mass index, maternal age, parity and smoking status. FC: linear fold change, with negative values denoting lower levels while positive values denote higher levels in cases than in controls.
(XLSX)
List of 76 proteins with significantly different abundance between early preeclampsia with MVM and normal pregnancy (q < 0.1) in at least one interval, after adjustment for body mass index, maternal age, parity and smoking status. FC: linear fold change, with negative values denoting lower levels while positive values denote higher levels in cases than in controls.
(XLSX)
List of 130 proteins with significantly different abundance between severe early preeclampsia and normal pregnancy (q < 0.1) in at least one interval, after adjustment for body mass index, maternal age, parity and smoking status. FC: linear fold change, with negative values denoting lower levels while positive values denote higher levels in cases than in controls.
(XLSX)
Protein abundance data for each sample (rows) and each of the 1125 proteins is given in this table. Note, unlike for the early preeclampsia group, data for normal pregnancy group is the same as in in [72], and included in this file for convenience. ID: anonymized identifier indicator of the patient, GA: gestational age at sample, GADiagnosis: gestational age at diagnosis for cases; EarlyPE: is 1 for early preeclampsia and 0 for normal pregnancy. EarlyPE_MVM: is 1 for early preeclampsia with maternal vascular malperfusion and 0 for normal pregnancy or early preeclampsia without maternal vascular malperfusion; EarlyPE_Severe: is 1 for severe early preeclampsia cases; Protein symbol and names provided by Somalogic, Inc, are the same as S1 File in [72].
(CSV)
Longitudinal differences in protein abundance assessed generalized additive mixed models are shown for proteins listed in Table 2. For each protein, differences are shown between early preeclampsia (PE) and controls (top left) as well as between mild or severe PE and controls (top right) and between PE with or without maternal vascular malperfusion (MVM) and controls. Thick lines show averages while grey bands give the 95% confidence interval.
(PDF)
Data Availability Statement
All relevant data are included within the paper and its Supporting Information files.