Abstract
Our aim was to examine the association of pre-treatment tumor infiltrating lymphocyte (TIL) count and PD-L1 levels with pathologic complete response (pCR) and assess immune marker changes following treatment in tumor specimens from the S0800 clinical trial which randomized patients to bevacizumab+nab-paclitaxel followed by doxorubicin/cyclophosphamide (AC) versus two control arms without bevacizumab (varying sequence of AC and nab-paclitaxel). TILs were assessed in 124 pre- and 62 post-treatment tissues (including 59 pairs). PD-L1 was assessed in 120 pre- and 43 post-treatment tissues (including 39 pairs) using the 22C3 antibody. Baseline and treatment-induced immune changes were correlated with pCR and survival using estrogen receptor (ER) and treatment adjusted logistic and Cox regressions, respectively. At baseline, the mean TIL count was 17.4% (17% had zero TIL, 9% had ≥50% TILs). Post-treatment, mean TIL count decreased to 11% (5% had no TIL, 2% had > 50% TILs). In paired samples, the mean TILs change was 15% decrease. Baseline PD-L1 was detected in 43% of cases (n=5 in tumor cells, n=29 stroma, n=18 tumor+stroma). Post-treatment, PD-L1 expression was not significantly lower, 33%. Higher baseline TIL count and PD-L1 positivity rate were associated with higher pCR rate even after adjustment for treatment and ER status (p=0.018). There was no association between TIL counts, PD-L1 expression and survival due to few events. In conclusion, TIL counts, but not PD-L1 expression, decreased significantly after treatment. Continued PD-L1 expression in some residual cancers raises the possibility that adjuvant immune checkpoint inhibitor therapy could improve survival in this patient population.
Keywords: Tumor infiltrating lymphocytes, PD-L1, neoadjuvant treatment, bevacizumab, locally advanced breast cancer
Introduction
Neoadjuvant (preoperative) chemotherapy is increasingly used in the treatment of early stage breast cancer (1) because it leads to higher breast conservation rates among locally advanced cancers, to smaller surgical resection in stage II cancers (2, 3) and the extent of residual cancer provides important prognostic information (4). Pathologic complete response (pCR), defined as no invasive cancer in the breast or lymph nodes after neoadjuvant chemotherapy, is an indicator of excellent survival, whereas extensive residual disease indicates poor prognosis. Patients with residual disease may receive additional chemotherapy which can improve survival in triple negative breast cancers (TNBC) (5) or could participate in clinical trials designed for this high-risk population (NCT02954874, NCT02445391, NCT02101385).
Tumor infiltrating lymphocytes (TIL), or immune-related gene expression signatures, are predictive of higher pCR rates (6-8) and are also associated with better survival in TNBC, HER2-positive and high-risk ER-positive breast cancers (9-12). Surprisingly, high expression of immune checkpoint molecules such as PD-1 (programmed death receptor 1) and PD-L1 (programmed death ligand 1), that down regulate anti-tumor immune effector mechanisms, is also associated with higher pCR rate and better prognosis (13-16). This is due to the strong correlation between PD-L1 expression and TIL counts and also suggests that high expression of this checkpoint molecule does not completely eliminate the benefits of anti-tumor immune surveillance in lymphocyte-rich cancers.
Several ongoing neoadjuvant clinical trials test if addition of an immune checkpoint inhibitor to standard of care chemotherapy could increase pCR rates and improve survival in early stage breast cancers, particularly TNBC (17). Understanding how chemotherapy influences the tumor immune microenvironment could assist in designing future studies and develop biomarkers. Preclinical evidence supports that some of the antitumor activity of cytotoxic agents is mediated by anti-tumor immune response (18). Tumor cell injury from chemotherapy may trigger neoantigen formation, dendritic cell activation, antigen cross-presentation and cytokine release that ultimately lead to induction of tumor-specific cytotoxic T cells (19). Some chemotherapy drugs can also inhibit myeloid-derived immune suppressor cells and FOXP3+ regulatory T cells (20). Vascular endothelial growth factor (VEGF) in the tumor microenvironment enhances expression of PD-1 and other inhibitory checkpoints involved in T cell exhaustion, and this effect can be reverted by anti-angiogenic agents such as bevacizumab (21).
S0800 (NCT00856492) was a randomized 3-arm Phase II trial that assessed if inclusion of bevacizumab with neoadjuvant chemotherapy could improve pCR rates in HER2-negative, locally advanced, or inflammatory breast cancer (IBC). The three arms of the trial were weekly nab-paclitaxel and bevacizumab followed by dose-dense doxorubicin / cyclophosphamide (ddAC) (Arm A), nab-paclitaxel followed by ddAC, (Arm B), and ddAC followed by nab-paclitaxel (Arm C). Patients were randomly allocated (2:1:1) to the three arms, but for the primary efficacy analysis the two non-bevacizumab arms (B and C) were combined. The primary efficacy results were reported earlier (22), and showed that bevacizumab increased pCR rate from 21% to 36% (p = 0.019). In TNBC, the improvement in pCR rate was even higher 29% vs. 59% (p = 0.014) while in ER-positive cancer the improvement did not reach statistical significance (18% vs. 24%; p = 0.41). There was also a trend for improved event-free survival with the addition of bevacizumab in the TNBC subset (p = 0.06). The main objectives of the current study were to (i) examine the association of pre-treatment TIL and PD-L1 levels with pCR and (ii) assess changes in TIL counts and PD-L1 expression between pre- and post-treatment tissues from the S0800 clinical trial. We also assessed associations between these immune markers and event-free and overall survival.
Material and Methods
Patients
Baseline core needle biopsies and post-treatment surgical resection specimens were collected prospectively during the trial. Formalin fixed paraffin embedded (FFPE) blocks or unstained cut sections were submitted to the SWOG tissue bank. Of the 215 patients registered for the S0800 trial, 211 were available for efficacy analysis, 134 patients had pre-treatment and 63 had post-treatment FFPE tissues with consent for research, including 59 paired pre- and post-treatment tissues (CONSORT diagram, Figure 1). TIL counts could be assessed in 124 pre- and 62 post-treatment tissues including 59 paired cases. For the remaining cases, the submitted tissue did not contain cancer or the staining procedure failed. PD-L1 immunohistochemistry (IHC) could be generated for 120 pre-treatment, 43 post-treatment and 39 paired specimens. The missing cases had no adequate tissues for IHC. Patient characteristics of the entire cohort and the current biomarker study subpopulation are shown on Table 1. Pathologic complete response was determined by the local pathologists and pCR was defined as the absence of any residual invasive cancer, with or without ductal carcinoma in situ, in the breast and axilla (ypT0/is ypN0). All surgical pathology reports were reviewed centrally for accuracy by the study chair (Z.N.) without the knowledge of treatment assignment. The current biomarker analysis was approved by the Yale Cancer Center Human Investigations Committee.
Figure 1.
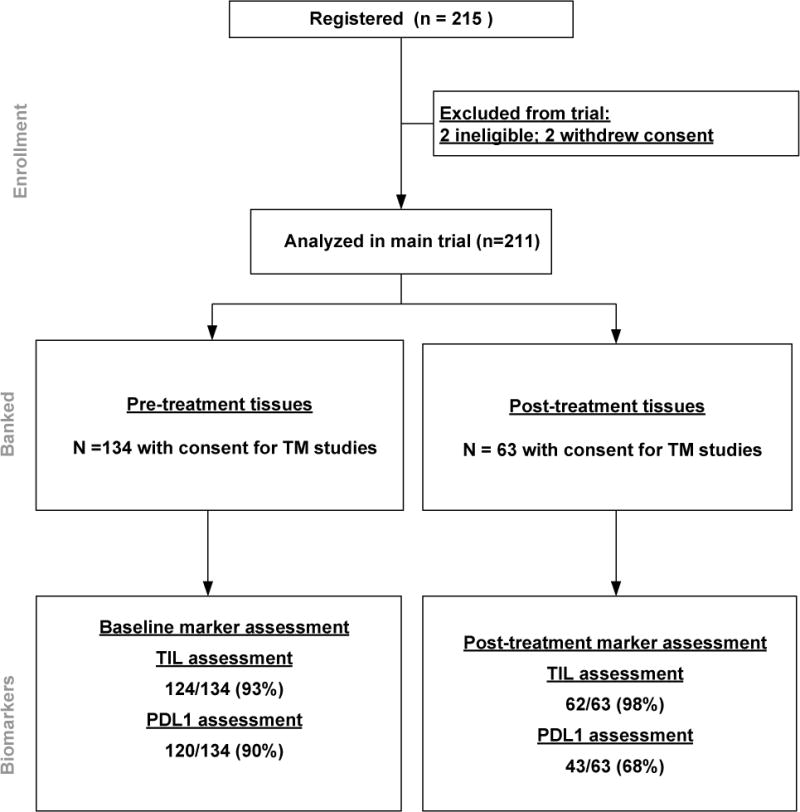
CONSORT diagram of samples used in the study.
Table 1.
Demographic and disease characteristics for the overall trial population and the immune marker subset
| S0800 Total | Immune study | |
|---|---|---|
| Eligible and Maintained Consent | 211 | 134 |
| Inflammatory Breast Cancer (IBC) or Locally Advanced Breast Cancer (LABC) | ||
| IBC | 24 (11.4%) | 12 (9.0%) |
| LABC | 187 (88.6%) | 122 (91.0%) |
| Hormone Receptor (HR) Status | ||
| HR-positive: ER+ or PR+ | 144 (68.2%) | 93 (69.4%) |
| HR-negative: ER− and PR− | 67 (31.8%) | 41 (30.6%) |
| Randomized treatment | ||
| No bevacizumab | 113 (53.5%) | 73 (54.5%) |
| Bevacizumab | 98 (46.5%) | 61 (45.5%) |
| Primary Outcome | ||
| No pCR | 152 (72.0%) | 97 (72.4%) |
| pCR | 59 (28.0%) | 37 (27.6%) |
TIL assessment
TILs were assessed by two pathologists (V.P. and B.W) on hematoxylin eosin (H&E) stained full sections following the scoring guidelines of the International TILs Working Group (23). In cases with pCR, the tumor bed was examined and scored. Stromal TIL scores were defined as the percentage of tumor stroma area that was occupied by mononuclear inflammatory cells. Inflammatory infiltrates in the stroma of noninvasive lesions and normal breast structures were excluded from TIL counts. The two scores were averaged to obtain the mean TIL percentage.
PD-L1 immunohistochemistry
PD-L1 immunohistochemistry was performed on 5-μm whole tissue sections using the FDA cleared 22C3 assay on the Dako Link 48 platform following the manufacturer’s instructions as previously reported (24). For controls, we used the control slide from DAKO 22c3 pharmDx assay that includes a PD-L1 positive (NCI-H226) and a PD-L1 negative (MCF-7) cell line (Supplemental Figure S1A) and also a tissue microarray assembled in our laboratory that contains 100 spots of randomly selected cases of placenta, tonsil, lung cancer and cell lines that express broad ranges of PD-L1 (24) (Supplemental Figure S1B). Two breast pathologists (V.P and Y-C. L) scored independently both the tumor and stromal cell compartments as a percentage of cells with PD-L1 signal at any intensity. When greater than 10% absolute difference in % positive score was observed, the pathologists jointly reviewed the case to arrive at consensus otherwise the average of the two pathologists’ scores was used as the final PD-L1 percent. PD-L1 positivity threshold was set at ≥ 1% of either tumor or stromal cells. A similar 1% threshold, using the same 22C3 antibody, was used to select PD-L1 positive metastatic TNBC for anti-PD-1 therapy in a clinical trial which reported an overall response rate of 18.5% with single agent pembrolizumab in metastatic TNBC (25).
Statistical Analysis
All available specimens were used in this study and sample size was determined by tissue availability. The primary outcome was pCR. Associations with pCR rate was evaluated either using contingency table analyses (using exact methods) or modeled with logistic regression. TIL counts were classified into approximate quartiles and the four quartile categories were tested either as an ordinal variable or as a categorical variable. The logistic regression analyses were adjusted for hormone-receptor status and randomized treatment. The secondary outcomes were overall survival (OS) defined as time from registration to death due to any cause and event-free survival (EFS). Events included progression prior to surgery, local or distant recurrence post-surgery or death from any cause. Patients without an event were censored at the last known follow-up time. OS and EFS were analyzed using Cox regression adjusting for ER status and randomized treatment assignment. Hazard ratios (HR) and 95% confidence intervals (95% CI) are presented. Changes in immune marker levels between pre- and post-treatment samples were compared by pCR outcome or hormone-receptor status using a Wilcoxon non-parametric test.
Results
TIL counts before and after chemotherapy and its association with outcome
At baseline (n=124), the mean TIL count was 17.4% (median 10%); 17% of cases had zero TILs, and 9% had ≥ 50% TILs. Baseline mean and median (15%) TIL percentages were nominally higher in ER-negative (n=39, mean 20.8%, median 15%) compared to ER-positive cancers (n=85, mean 15.8%, median 7.5%), but these differences did not reach statistical significance (Wilcoxon p=0.11). Classifying baseline TILs into approximate quartiles showed a significant association with pCR in an ordinal trend test (p=0.008), but were not significant when treated as four distinct categories (Fisher’s exact test p=0.07) (Table 2). This pattern remained in a logistic regression adjusting for treatment and ER status (trend p=0.019; categorical p=0.12). Using TIL counts as a continuous variable adjusted for ER status and bevacizumab treatment, every 10% increase in TIL increased the odds of pCR with an odds ratio (OR) of 1.21 (95% CI: 0.99-1.48, p=0.07).
Table 2.
Pathologic complete response (pCR) rates in approximate quartiles of percent tumor infiltrating lymphocyte categories.
| No pCR | pCR | Total | |||
|---|---|---|---|---|---|
| Baseline TIL Quartile | N | % | N | % | N |
| 1: < 5% | 25 | 83 % | 5 | 17 % | 30 |
| 2: 5%-10% | 27 | 75 % | 9 | 25 % | 36 |
| 3: 11%-25% | 21 | 68 % | 10 | 32 % | 31 |
| 4: 26%-90% | 14 | 52 % | 13 | 48 % | 27 |
| Total | 87 | 70 % | 37 | 30 % | 124 |
There was no significant association between EFS, OS and baseline TIL counts either as continuous variable (p=0.36, p=0.10) or as quartiles (p=0.49, p=0.32). The median follow-up of this study was only 3 years and only 24 EFS and 19 OS events occurred during this time which limits the power of the survival analyses for the entire study or for ER subsets.
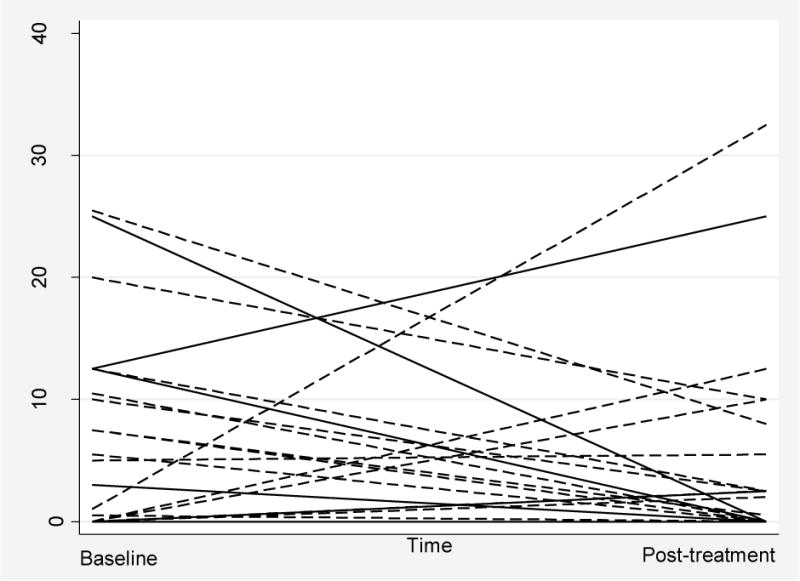
In the post-NAC samples (n=62), the mean and median TIL counts were 11% and 7.5% respectively; 5% of cases had zero TILs, and 2% had ≥ 50% TILs. In paired pre- and post-treatment samples (n=59), TIL counts decreased in 78% of cases in the post-treatment samples with a mean change of 15% decrease in TILs. In the remaining 22% of cases (n=13) TIL counts increased. Among these patients, 3 had pCR. Decrease in TIL was not associated with pCR (p=1.00), ER status (p=0.27), or bevacizumab treatment (p=0.35). Figure 2A shows the distribution of pre- and post-treatment TIL counts in paired samples. Cases with residual disease (n=44) had lesser absolute TIL decrease (Wilcoxon p=0.041) than cases with pCR (n=15) where the tumor bed was assessed (Figure 2B). The post-treatment decrease in TILs was also observed after excluding cases with pCR. Representative TIL images are shown in Figure 3A and B.
Figure 2. Tumor infiltrating lymphocyte (TIL) counts in baseline tumors and residual disease.

A. Distribution of TIL percentage counts before and after neoadjuvant chemotherapy. B. Change in TIL count before and after neoadjuvant chemotherapy in paired samples grouped by pathologic response category (pCR=pathologic complete response, n=15; no-pCR n=44). The mean change was 11% in cases with no-pCR and 26% in cases with pCR (Wilcoxon test p=0.04).
Figure 3. Representative images of tumor infiltrating lymphocytes (TIL) and PD-L1 chromogenic staining.
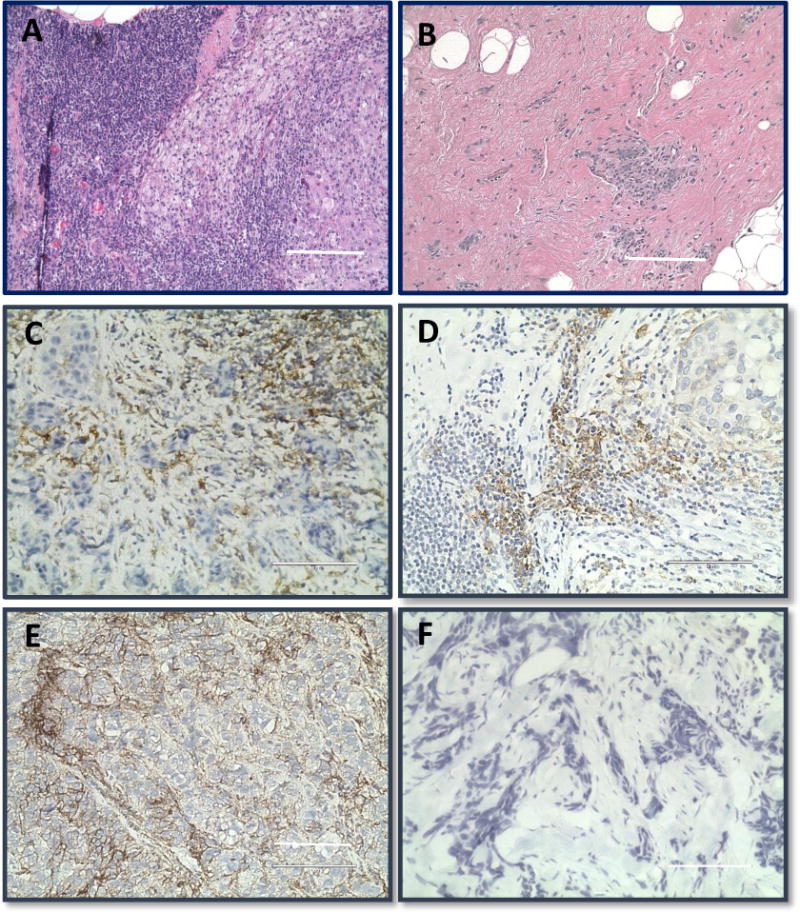
A. Baseline H&E of a case with high TIL count (40× magnification, bar represents 100μm). B. Post-treatment H&E of the same case with decrease of the TIL infiltrate. C. In this case, the PD-L1 immunostaining is mostly observed in cells morphologically compatible with macrophages or fibroblasts. D. Example of PD-L1 immunostaining that is not in lymphocytes in a tumor with high lymphocytic infiltration, staining is localized to cells that are morphologically compatible with macrophages. E. A case with baseline high PD-L1 expression in tumor cells. F. Example of a PD-L1 negative case.
PD-L1 expression before and after chemotherapy and its association with outcome
At baseline, PD-L1 expression was detected in 52 of 120 (43%) cases mostly in the stroma (n=5 PD-L1 staining in tumor only, n=29 stroma only, n=18 tumor + stroma). Stromal and tumor PD-L1 percentages were moderately but statistically significantly correlated (Pearson r=0.56; p<0.0001). Most of PD-L1 immunostaining in the stroma was observed not on TILs but macrophages and morphologically fibroblast-like cells (Figures 3C and 3D). The correlation between baseline PD-L1 expression and TIL count was weak and nonsignificant (tumor cell PD-L1 vs TILs r=0.21, p=0.27; stromal PD-L1 vs TILs r=0.21, p=0.25). Cases with PD-L1 expression at baseline, either in the stroma or in tumor cells, or both, had significantly higher pCR rates 63% vs. 37%; compared to cases lacking PD-L1 expression (Fischer’s exact test p=0.008). Examples of PD-L1 positive and negative cases are shown in Figures 3E and 3F, respectively. In ER and treatment adjusted logistic regression, every 10% increase in baseline stromal cell PD-L1 percentage had an OR of 3.02 for pCR (95% CI: 1.55-5.89, p=0.001). Baseline tumor cell PD-L1 expression was not associated with pCR (p=0.10), which may be due to the limited number of such cases (n=23). We also did not observe a significant association between baseline PD-L1 expression and EFS (p=0.93) and OS (p=0.48).
Post-treatment, PD-L1 expression was seen in 14 of 43 (33%) cases (n=6 stroma only, n=8 tumor + stroma). Post-treatment stromal (r=0.59; p=0.0002) and tumor cell (r=0.42; p=0.014) PD-L1 expression were significantly correlated with post-treatment TIL count. In the 39 paired cases, PD-L1 expression was negative in both the pre- and post-treatment samples in 20 cases, positive in 10, positive at baseline but negative in the post-treatment sample in 6, and negative at baseline but positive after chemotherapy in 3 cases. In these paired samples, post-treatment stromal PD-L1 expression decreased on average by 1% which did not reach statistical significance (p=0.44) (Figure 4). The decrease in stromal PD-L1 expression was slightly greater among those with pCR (mean 3.6%; min −12.5%; max 25.05%) than those with residual disease (mean 0.5%; min −31.5%; max 17.5%), but this difference was not statistically significant (Wilcoxon p=0.77). There was a slight, 0.3% mean, non-significant increase in tumor cell PD-L1 expression in residual disease (n=31). These results suggest that PD-L1 expression remained stable in the tumor microenvironment before and after chemotherapy with or without bevacizumab.
Figure 4. PD-L1 expression at baseline and in residual disease of paired samples.
PD-L1 decrease in expression from baseline to follow-up by residual disease of 39 paired samples. PD-L1 percent decrease from baseline to post-treatment are shown in the box plot classified by cases with pathologic complete response (pCR, n=15) or not (no pCR, n=24).
Discussion
In this study, we examined changes in TIL count and PD-L1 expression after neoadjuvant chemotherapy and assessed associations between these immune parameters at baseline and pCR rate and survival. The randomized design of the S0800 trial also allowed us to test for interaction between the immune markers and bevacizumab added to paclitaxel/ddAC chemotherapy although the small sample size limits the power of this analysis. At baseline, 17% of cancers had zero TILs and 9% were TIL predominant. These findings confirm that most breast cancers (73%) contain small but detectable number of TILs, with a median TIL count around 10%. At baseline, PD-L1 expression was observed in 43% of cases. PD-L1 signal was mainly detected in stromal cells (90%), while cancer cells stained positive in only 44% of the cases. These observations are consistent with other reports showing that in breast cancer, unlike other tumor types, stromal cells, including TILs but also macrophages and morphologically fibroblast-like cells, are the primary sites of PD-L1 expression (26-28). This suggests that in breast cancer, interruption of PD1/PD-L1 signaling between various types of immune cells, rather than (or in addition to) between tumor cells and immune cells, is an important mechanism of action of PD1/PD-L1 targeting antibodies.
We observed that higher baseline TIL counts and PD-L1 positivity were associated with increasing probability of pCR as previously reported (6-8, 13-16). This supports the hypothesis that chemotherapy response is partly mediated by activated cytotoxic T cells (18-21), and frequent PD-L1 expression provides rationale for combining immune checkpoint inhibitors with chemotherapy to increase pCR rates (29-31). One could hypothesize that PD-L1 expression is a sign of an incomplete negative feedback to a robust anti-tumor immune response. Indeed, PD-L1 expression is highly correlated with the presence of immune effector cells and immune activation signals (6, 8, 10, 11, 13).
Because of the availability of post-treatment tissues, we could examine treatment induced changes in TIL counts and PD-L1 expression. We anticipated an overall increase in these parameters since clinical (32) and preclinical studies suggested that chemotherapy can render tumor cells more immunogenic (18-21). Preclinical studies also suggested that PD-L1 expression on cancer cells is stimulated by chemotherapy and suppressed by VEGF (21, 33). However, we observed a significant decrease in TIL count, while PD-L1 expression did not change significantly from baseline to post-treatment tissues, either overall or in the bevacizumab treated arm. Other investigators have also reported chemotherapy-induced decrease of CD3 (total lymphocytes), CD4 (T cells) and CD20 (B cells) -positive cells (34) and gene expression analysis of paired pre- and post-treatment samples demonstrated depletion of immune-related mRNAs in residual cancer (35). These observations suggest that either chemotherapy has a cytotoxic effect on TILs or as the size of the primary tumor decreases in response to therapy, the immunogenic target decreases and the corresponding anti-tumor immune reaction also winds down. Our finding that the greatest decrease in TILs between matched pre-/post-treatment samples coincides with pCR supports the hypothesis that after complete eradication of the cancer from the breast the immune response also resolves.
Our small sample size and few recurrence events prevented us from assessing the prognostic impact of TILs in residual cancer. However, several studies demonstrated that higher TIL counts in the residual cancer correlate with better survival after chemotherapy (36, 37). These observations suggest that cancers that remain “immunogenic” after chemotherapy may continue to be subjected to anti-tumor immune surveillance that can reduce the risk of distant recurrence. This hypothesis provides a rational to explore adjuvant immunotherapy in breast cancers with residual disease such as the currently accruing SWOG S01418 / NRG BR006 trial (NCT02954874).
An important limitation of the S0800 trial, designed 10 years ago, is that it included both ER-positive and ER-negative patients. Because of the small sample size, no separate, adequately powered analysis could be done by ER subgroups even though today we recognize the distinct immunological and molecular characteristics (6, 10-12) and different chemotherapy sensitivities of ER-positive and -negative cancers. Sampling bias could also have influenced our pre- and post-treatment comparisons, since the pre-treatment immune marker assessments were done on core needle biopsies whereas the post-treatment samples were surgically resected tissues. However, we previously studied the impact of tumor sampling on immune markers and examined TIL subpopulation counts between biopsies from different regions of the same cancer (38). Our results showed that the average lymphocyte score across multiple fields of view from a single biopsy is reasonably representative of the whole cancer.
Our results confirm that higher pre-treatment TIL count (as quartiles) and PD-L1 expression are associated with greater probability of pCR, independently of bevacizumab administration. This finding is consistent with the hypothesis that chemotherapy-induced tumor response is partially mediated by immune cells and provides rationale for exploring immune checkpoint inhibitors in the neoadjuvant treatment setting to further increase pCR rates. Several clinical trials now test this hypothesis in the clinic. We also demonstrated that TIL counts are lower in post-chemotherapy tissues while PD-L1 expression remained the same. The continued PD-L1 expression in many residual cancers raise the possibility that anti-cancer immune surveillance persists and might be further augmented by adjuvant immune checkpoint inhibitor therapy.
Supplementary Material
Acknowledgments
Funding/Support: Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Numbers CA180888 (to C. Blanke), CA180819 (to M. LeBlanc), CA180826 (to C. Fuchs), CA180801 (to M. Zalupski) and CA180858 (to C. Eng); a grant from Gilead Sciences to D.L. Rimm; and in part by Genentech (Roche), Abraxis BioScience (Celgene), HelomicsTM (to SWOG), and the Breast Cancer Research Foundation (to D.L. Rimm, C. Hatzis and L. Pusztai) and the Susan Komen Foundation for The Cure (to L. Pusztai).
Dr Hayes reported stock ownership at Oncimmune and Inbiomotion, research funding from Merrimack Pharmaceuticals, Inc. (Parexel Intl Corp), Eli Lilly Company, Janssen R&D, LLC (J & J), Veridex (Johnson & Johnson), Puma Biotechnology, Inc., Pfizer and Astra Zeneca, royalties from licensed research from Janssen R&D, LLC (Johnson & Johnson). Dr Hortobagyi reported serving as a consultant for Agendia, Hoffman-La Roche, Lilly, Novartis, Peregrine Pharmaceuticals. He receives research funding from Novartis. Dr Gralow reported serving as a consultant for Genentech (Roche), Novartis, and Merck. Dr Rimm has served as an advisor for Astra Zeneca, Agendia, BMS, Cell Signaling Technology, Genoptix/Novartis, Merck, and Perkin Elmer. Dr Pusztai receives research funding and served as consultant for Merck.
Footnotes
Disclosure of Potential Conflict of Interest: All other authors declare no potential conflicts of interest.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Mougalian SS, Soulos PR, Killelea BK, Lannin DR, Abu-Khalaf MM, DiGiovanna MP, et al. Use of neoadjuvant chemotherapy for patients with stage I to III breast cancer in the United States. Cancer. 2015;121:2544–52. doi: 10.1002/cncr.29348. [DOI] [PubMed] [Google Scholar]
- 2.Killelea BK, Yang VQ, Mougalian S, Horowitz NR, Pusztai L, Chagpar AB, et al. Neoadjuvant chemotherapy for breast cancer increases the rate of breast conservation: results from the National Cancer Database. J Am Coll Surg. 2015;220:1063–9. doi: 10.1016/j.jamcollsurg.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Boughey JC, Peintinger F, Meric-Bernstam F, Perry AC, Hunt KK, Babiera GV, et al. Impact of preoperative versus postoperative chemotherapy on the extent and number of surgical procedures in patients treated in randomized clinical trials for breast cancer. Ann Surg. 2006;244:464–70. doi: 10.1097/01.sla.0000234897.38950.5c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Symmans WF, Peintinger F, Hatzis C, Rajan R, Kuerer H, Valero V, et al. Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2007;25:4414–22. doi: 10.1200/JCO.2007.10.6823. [DOI] [PubMed] [Google Scholar]
- 5.Toi ML-J, Lee ES, Ohtani S, Im Y-H, Im S-A, Park B-W, et al. A phase III trial of adjuvant capecitabine in breast cancer patients with HER2-negative pathologic residual invasive disease after neoadjuvant chemotherapy (CREATE-X, JBCRG-04); Proceedings of the Thirty-Eighth Annual CTRC-AACR San Antonio Breast Cancer Symposium; 2015 Dec 8-12; San Antonio. TX Philadelphia (PA): AACR; 2015. 2015. [Google Scholar]
- 6.Denkert C, Loibl S, Noske A, Roller M, Muller BM, Komor M, et al. Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2010;28:105–13. doi: 10.1200/JCO.2009.23.7370. [DOI] [PubMed] [Google Scholar]
- 7.Denkert C, von Minckwitz G, Brase JC, Sinn BV, Gade S, Kronenwett R, et al. Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2015;33:983–91. doi: 10.1200/JCO.2014.58.1967. [DOI] [PubMed] [Google Scholar]
- 8.Iwamoto T, Bianchini G, Booser D, Qi Y, Coutant C, Shiang CY, et al. Gene pathways associated with prognosis and chemotherapy sensitivity in molecular subtypes of breast cancer. Journal of the National Cancer Institute. 2011;103:264–72. doi: 10.1093/jnci/djq524. [DOI] [PubMed] [Google Scholar]
- 9.Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, et al. Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2014;32:2959–66. doi: 10.1200/JCO.2013.55.0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bianchini G, Qi Y, Alvarez RH, Iwamoto T, Coutant C, Ibrahim NK, et al. Molecular anatomy of breast cancer stroma and its prognostic value in estrogen receptor-positive and -negative cancers. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2010;28:4316–23. doi: 10.1200/JCO.2009.27.2419. [DOI] [PubMed] [Google Scholar]
- 11.Rody A, Holtrich U, Pusztai L, Liedtke C, Gaetje R, Ruckhaeberle E, et al. T-cell metagene predicts a favorable prognosis in estrogen receptor-negative and HER2-positive breast cancers. Breast Cancer Res. 2009;11:R15. doi: 10.1186/bcr2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F, et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2013;31:860–7. doi: 10.1200/JCO.2011.41.0902. [DOI] [PubMed] [Google Scholar]
- 13.Bottai G, Raschioni C, Losurdo A, Di Tommaso L, Tinterri C, Torrisi R, et al. An immune stratification reveals a subset of PD-1/LAG-3 double-positive triple-negative breast cancers. Breast Cancer Res. 2016;18:121. doi: 10.1186/s13058-016-0783-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wimberly H, Brown JR, Schalper K, Haack H, Silver MR, Nixon C, et al. PD-L1 Expression Correlates with Tumor-Infiltrating Lymphocytes and Response to Neoadjuvant Chemotherapy in Breast Cancer. Cancer Immunol Res. 2015;3:326–32. doi: 10.1158/2326-6066.CIR-14-0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schalper KA, Velcheti V, Carvajal D, Wimberly H, Brown J, Pusztai L, et al. In situ tumor PD-L1 mRNA expression is associated with increased TILs and better outcome in breast carcinomas. Clin Cancer Res. 2014;20:2773–82. doi: 10.1158/1078-0432.CCR-13-2702. [DOI] [PubMed] [Google Scholar]
- 16.Liu B, Cui J, Sun J, Li J, Han X, Guo J, et al. Immunolocalization of MMP9 and MMP2 in osteolytic metastasis originating from MDA-MB-231 human breast cancer cells. Mol Med Rep. 2016;14:1099–106. doi: 10.3892/mmr.2016.5374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pusztai L, Karn T, Safonov A, Abu-Khalaf MM, Bianchini G. New Strategies in Breast Cancer: Immunotherapy. Clinical cancer research: an official journal of the American Association for Cancer Research. 2016;22:2105–10. doi: 10.1158/1078-0432.CCR-15-1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sistigu A, Yamazaki T, Vacchelli E, Chaba K, Enot DP, Adam J, et al. Cancer cell-autonomous contribution of type I interferon signaling to the efficacy of chemotherapy. Nat Med. 2014;20:1301–9. doi: 10.1038/nm.3708. [DOI] [PubMed] [Google Scholar]
- 19.Vincent J, Mignot G, Chalmin F, Ladoire S, Bruchard M, Chevriaux A, et al. 5-Fluorouracil selectively kills tumor-associated myeloid-derived suppressor cells resulting in enhanced T cell-dependent antitumor immunity. Cancer Res. 2010;70:3052–61. doi: 10.1158/0008-5472.CAN-09-3690. [DOI] [PubMed] [Google Scholar]
- 20.Roselli M, Cereda V, di Bari MG, Formica V, Spila A, Jochems C, et al. Effects of conventional therapeutic interventions on the number and function of regulatory T cells. Oncoimmunology. 2013;2:e27025. doi: 10.4161/onci.27025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Voron T, Colussi O, Marcheteau E, Pernot S, Nizard M, Pointet AL, et al. VEGF-A modulates expression of inhibitory checkpoints on CD8+ T cells in tumors. J Exp Med. 2015;212:139–48. doi: 10.1084/jem.20140559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nahleh ZA, Barlow WE, Hayes DF, Schott AF, Gralow JR, Sikov WM, et al. SWOG S0800 (NCI CDR0000636131): addition of bevacizumab to neoadjuvant nab-paclitaxel with dose-dense doxorubicin and cyclophosphamide improves pathologic complete response (pCR) rates in inflammatory or locally advanced breast cancer. Breast Cancer Res Treat. 2016;158:485–95. doi: 10.1007/s10549-016-3889-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol. 2015;26:259–71. doi: 10.1093/annonc/mdu450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rimm DL, Han G, Taube JM, Yi ES, Bridge JA, Flieder DB, et al. A Prospective, Multi-institutional, Pathologist-Based Assessment of 4 Immunohistochemistry Assays for PD-L1 Expression in Non-Small Cell Lung Cancer. JAMA Oncol. 2017 doi: 10.1001/jamaoncol.2017.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nanda R, Chow LQ, Dees EC, Berger R, Gupta S, Geva R, et al. Pembrolizumab in Patients With Advanced Triple-Negative Breast Cancer: Phase Ib KEYNOTE-012 Study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2016;34:2460–7. doi: 10.1200/JCO.2015.64.8931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McLaughlin J, Han G, Schalper KA, Carvajal-Hausdorf D, Pelekanou V, Rehman J, et al. Quantitative Assessment of the Heterogeneity of PD-L1 Expression in Non-Small-Cell Lung Cancer. JAMA Oncol. 2016;2:46–54. doi: 10.1001/jamaoncol.2015.3638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kluger HM, Zito CR, Barr ML, Baine MK, Chiang VL, Sznol M, et al. Characterization of PD-L1 Expression and Associated T-cell Infiltrates in Metastatic Melanoma Samples from Variable Anatomic Sites. Clinical cancer research: an official journal of the American Association for Cancer Research. 2015;21:3052–60. doi: 10.1158/1078-0432.CCR-14-3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cimino-Mathews A, Thompson E, Taube JM, Ye X, Lu Y, Meeker A, et al. PD-L1 (B7-H1) expression and the immune tumor microenvironment in primary and metastatic breast carcinomas. Hum Pathol. 2016;47:52–63. doi: 10.1016/j.humpath.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nanda R, Liu MC, Yau C, Asare S, Hylton N, Van’t Veer L, et al. Pembrolizumab plus standard neoadjuvant therapy for high-risk breast cancer (BC): Results from I-SPY 2. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2017:35. [Google Scholar]
- 30.Pusztai L, Silber A, Wysong Hofstatter E, Chung GG, Horowitz NR, Lannin DR, et al. Safety of MEDI4736 (anti-PD-L1 antibody) administered concomitant with weekly nab-paclitaxel and dose dense doxorubicin/cyclophosphamide (ddAC) as neoadjuvant chemotherapy for stage I-III triple negative breast cancer (TNBC): A Phase I/II trial. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2017:35. [Google Scholar]
- 31.Schmid P, Park YH, Muñoz-Couselo E, Kim S-B, Sohn J, Im S-A, et al. Pembrolizumab (pembro) + chemotherapy (chemo) as neoadjuvant treatment for triple negative breast cancer (TNBC): Preliminary results from KEYNOTE-173. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2017:35. [Google Scholar]
- 32.Demaria S, Volm MD, Shapiro RL, Yee HT, Oratz R, Formenti SC, et al. Development of tumor-infiltrating lymphocytes in breast cancer after neoadjuvant paclitaxel chemotherapy. Clinical cancer research: an official journal of the American Association for Cancer Research. 2001;7:3025–30. [PubMed] [Google Scholar]
- 33.Zhang P, Su DM, Liang M, Fu J. Chemopreventive agents induce programmed death-1-ligand 1 (PD-L1) surface expression in breast cancer cells and promote PD-L1-mediated T cell apoptosis. Mol Immunol. 2008;45:1470–6. doi: 10.1016/j.molimm.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 34.Garcia-Martinez E, Gil GL, Benito AC, Gonzalez-Billalabeitia E, Conesa MA, Garcia Garcia T, et al. Tumor-infiltrating immune cell profiles and their change after neoadjuvant chemotherapy predict response and prognosis of breast cancer. Breast Cancer Res. 2014;16:488. doi: 10.1186/s13058-014-0488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gonzalez-Angulo AM, Iwamoto T, Liu S, Chen H, Do KA, Hortobagyi GN, et al. Gene expression, molecular class changes, and pathway analysis after neoadjuvant systemic therapy for breast cancer. Clin Cancer Res. 2012;18:1109–19. doi: 10.1158/1078-0432.CCR-11-2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dieci MV, Criscitiello C, Goubar A, Viale G, Conte P, Guarneri V, et al. Prognostic value of tumor-infiltrating lymphocytes on residual disease after primary chemotherapy for triple-negative breast cancer: a retrospective multicenter study. Ann Oncol. 2014;25:611–8. doi: 10.1093/annonc/mdt556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ladoire S, Arnould L, Apetoh L, Coudert B, Martin F, Chauffert B, et al. Pathologic complete response to neoadjuvant chemotherapy of breast carcinoma is associated with the disappearance of tumor-infiltrating foxp3+ regulatory T cells. Clinical cancer research: an official journal of the American Association for Cancer Research. 2008;14:2413–20. doi: 10.1158/1078-0432.CCR-07-4491. [DOI] [PubMed] [Google Scholar]
- 38.Mani NL, Schalper KA, Hatzis C, Saglam O, Tavassoli F, Butler M, et al. Quantitative assessment of the spatial heterogeneity of tumor-infiltrating lymphocytes in breast cancer. Breast Cancer Res. 2016;18:78. doi: 10.1186/s13058-016-0737-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


