Abstract
Introduction: During recent years, several recommendations and guidelines regarding cardiac pacing have been published in the literature. However, only a few studies have examined the implementation of these guidelines in clinical practice. The current study aimed to record and evaluate the effects of the mainstream studies, and the experience gathered by all patients who have been followed-up at the pacemaker Unit of Veroia Hospital, which is a secondary care center.
Methods and results: Epidemiological, clinical, and electrocardiographic data were collected and studied for patients with a permanent pacemaker that have been followed-up in our hospital from 2002 to 2017. The total number of patients of the study was 3,902 (2,164 men; 55.45 %) with a mean age of 73.4 ± 12.6 years. Third degree atrioventricular (AV) block was the most common cause of pacing. Dysfunction of the sinus node involved the majority of cases with bradycardia-tachycardia syndrome. At 18 patients, the cause of permanent pacemaker implantation was carotid sinus syndrome and at 13 of them, cardio-vascular type of neurocardiogenic syncope. Dizziness and syncope were the most common symptoms. Dual-chamber pacing was the most common type of pacing, which has been increasing in recent years. In follow-up visits, the most frequent examinations concerned battery condition, as the stimulation and sensing threshold. Reprogramming of the device was required in 1,434 patients (36.75 %), especially during the first year after implantation.
Conclusion: Pacing indications have been unchanged during all the years of the study and have been based on confirmed bradycardia and major symptoms. Reprogramming of the device was needed in an increased number of patients. HIPPOKRATIA 2018, 22(2): 75-79.
Keywords: Pacemaker, secondary care center, reprogramming, follow-up
Introduction
Heart rhythm disorders exist in symptomatic or asymptomatic patients, as a result of alterations in the production and transmission of an electrical stimulus to the myocardium and involve a variety of clinical scenarios that are treated every day at all levels of the healthcare system. Some of them do not necessitate special treatment; others require antiarrhythmic drugs, while a significant percentage of them require interventions with invasive methods or implantation of devices that are performed in centers equipped with a hemodynamic laboratory. Pacemaker (PM) implantation, combined with its reprogramming capabilities, is a widespread possibility of intervening in situations where life-threatening bradycardia or cardiac arrests are recorded1,2. Although several guidelines have been published in recent years on the indications of implantation of PMs3, only a few studies have been conducted to record the implementation of these guidelines in clinical practice4.
Since 2002, a Pacemaker Unit (PU) operates at the General Hospital of Veroia, in which patients from the prefecture of Hemathia who have a permanent PM are being followed-up. We aimed to evaluate the impact of international recommendations and mainstream studies on pacing, and also the recorded experience, on all patients who had been examined to the PU, over the years from 2002 to 2017.
Methods
We studied 3,902 patients; 2,164 men and 1,738 women with average age 73.4 years, who have been implanted a PM and visited the PU of our hospital for a check-up. The follow-up visit was an outpatient visit to the PU, where a cardiologist and an allied professional, if needed, advised the patient, after a predefined clinical examination. Initially, it concerned the examination of the pacing threshold stabilization and other settings. Visits were performed on a regular basis, usually every six months, and if there was a specific reason for additional monitoring (e.g., close to the battery replacement time) in any different period. If the patient reported any suspicious symptom, which could be related to the function of the device, then examinations were performed on an emergency basis. Most pacing programming devices, which measure pacing parameters, are available in the Unit, and in cases where such a device was not available, the PM was initially tested with the magnet and then by the technician of the company who owns the program. At the time of follow-up, all collected data were entered into an electronic database for future processing. The PU is staffed with two trained and experienced cardiologists, a trained nurse, and the residents who are trained in pacing and follow-up of these patients.
Epidemiological, clinical, and electrocardiographic data of patients with a PM who visited the PU were collected; the interventions that were made and the occurrence of complications related to the implantation of the device were studied.
Measurements during follow-up visits
During most follow-up visits, all routine measurements were examined, including battery status (with programmer or/and magnet test), stimulation threshold, sensing threshold, lead impedance, stimulation, and sensing of PM. In particular, the condition and adequacy of the device’s battery were checked to ensure battery replacement time before it was exhausted. The sensing and stimulation thresholds were controlled and changed in those cases where there were not producing the desired effect. At the same time, lead impedance was tested for possible complications (e.g., suspected fracture or displacement).
Data are analyzed descriptively. Continuous data are expressed as means and standard deviation and categorical parameters as percentages. The study was approved by the Scientific Committee of the General Hospital of Veroia, Hemathia (No 29/2017), and all patients signed informed consent.
Results
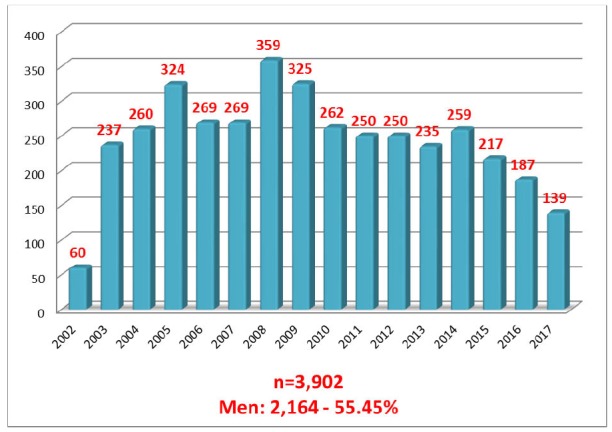
A total of 3,902 patients were cumulatively examined at the PU, either at scheduled follow-up visits or in case of emergency. Figure 1 shows the distribution of these visits per year. The majority of these 3,902 patients examined over the 16-year period, were men (2,164; 55.45 % vs 1,738 women; 44.55 %). The mean age of the patients was 73.4 years.
Figure 1. Follow-up visits per year to the pacemaker Unit of the General Hospital of Veroia during the period from 2002 to 2017.
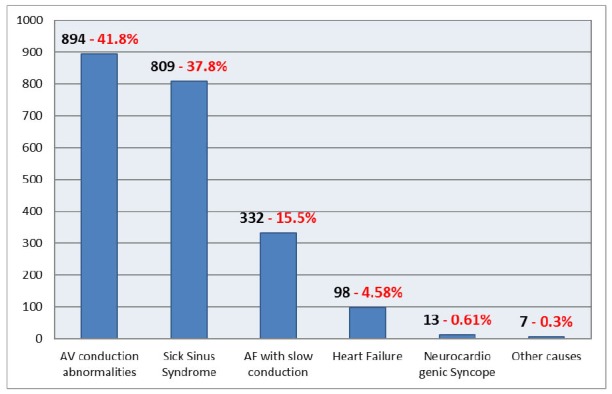
Causes of pacing
Figure 2 shows the primary indication for implantation of the PM device. The most common indication for PM implantation was conduction disturbances in the atrioventricular (AV) node, type II 2nd degree AV block - Mobitz II or 3rd degree AV block (complete heart block), concerning about 41.8 % of the cases (894 patients). Sinus node disease (including bradycardia-tachycardia syndrome) was the next in frequency concerning about 37.8 % of the cases (809 patients). Less often, the implantation of the PM was due to atrial fibrillation with slow ventricular conduction (15.5 %; 332 subjects), severe heart failure (4.58 %; 98 subjects) or cardiovascular type of neurocardiogenic syncope (0.61 %; 13 subjects). Most patients were improved immediately after the implantation of the PM.
Figure 2. Causes of initial pacemaker implantation for the cohort of patients been followed-up in the pacemaker Unit of the General Hospital of Veroia.
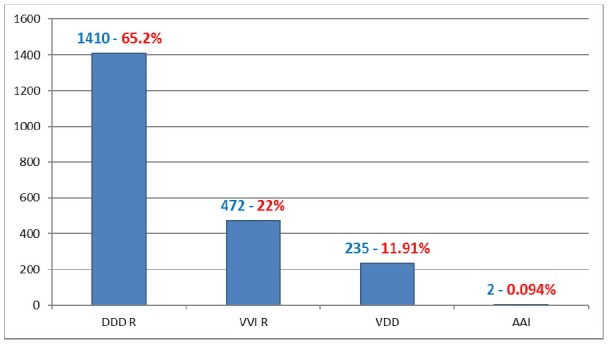
Choice of pacing mode
The pacing mode of the device was also recorded (Figure 3). About two-thirds of them concerned a dual-chamber AV pacing system, type DDD(R), in 65.2 % of the cases (1,410 subjects). The remaining one-third of the PMs were single-chamber ventricular pacing type VVI(R) in 22 % of the cases (472 subjects) and VDD type, in 11.91 % of the cases (235 subjects). Finally, there were two brothers from Sweden who had an AAI type been implanted in the early 2000s in their country.
Figure 3. Pacing type of the examined devices in the pacemaker Unit of the General Hospital of Veroia.
During these years that the PU operates, only 26 patients (0.66 %) experienced problems related to a malfunction of the device leads and were referred to the corresponding centers for correction of the problem. Finally, in all patients sensing and pacing mode were recorded at an electrocardiogram after all the other parameters had been checked.
Changes in pacemaker settings - Reprogramming
In 1,434 patients (36.75 %), their PMs had to be reprogrammed (changes in PM’s settings), using the devices available at the PU (Table 1). In those patients that we had to intervene by reprogramming their device, most cases involved changes in the stimulation threshold of either right ventricle (16.87 %) or atrium (14.05 %). Often, we also had to reprogram the sensing threshold of the PM, both ventricular (13.11 %) and atrial (12.34 %). In 183 cases, there was a need to change the mode of pacing, e.g., from DDD to VVI, when permanent atrial fibrillation was established (12.76 %). Finally, in fewer cases, changes were made to the sensor, at the time of the AV delay and the pulse duration. The majority of cases, where the device had to be reprogrammed were within the first year of implantation1,2, while less frequently reprogramming was due to symptomatic attendance of the patient at the Unit3.
Table 1. Frequency of changes in the pacemaker settings at follow-up visits.
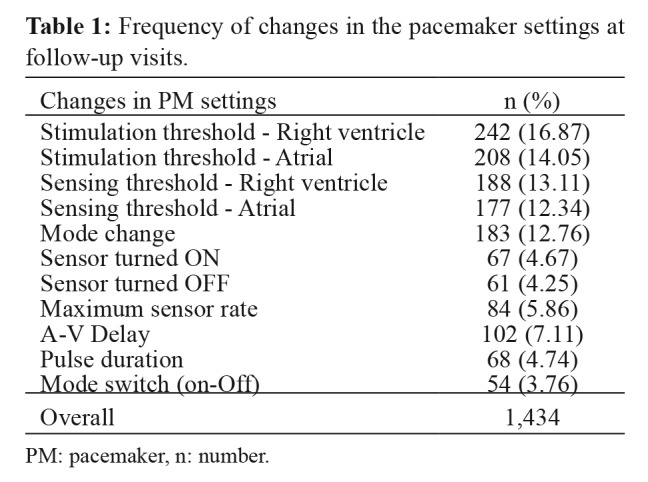
PM: pacemaker, n: number.
Discussion
Since 2002 that PU operates at the General Hospital of Veroia hundreds of patients with a permanent PM from the broader administrative region of Western Macedonia have been followed-up. Most PMs have been implanted in tertiary hospitals of the city of Thessaloniki. The Unit has been operating during these years for patients with PMs, based on the international rules and guidelines4. In every visit, the optimal functionality and longevity of the device, as well as the problems and complications of the patients with PM devices, were evaluated. Subsequent follow-up visits are planned, and the patients and their families are trained and supported on issues related to the PM5. Moreover, detailed medical data are meticulously recorded in the archive of the Unit for future assessment.
The findings of the study are in complete agreement with other recent studies. Proclemer et al6, in a large Italian study, studied patients with a permanent PM from 2003 to 2007, who were examined in several centers in the country. The data and the corresponding indications of these patients resembled those of our study. The mean age of the subjects was 77.3 years, and the leading causes of implantation were AV conduction disorders (44.2 %), followed by sick sinus syndrome (26.3 %), and atrial fibrillation with slow ventricular conduction (18.1 %). The most common type of PM was DDD(R) (53.3 %), followed by VVI(R) (33.6 %), and single-chamber VDD(R) and type AAI(R), at 11 % and 0.3 %, respectively.
Udo et al1, in a Dutch study, studied patients with a PM from 2003 to 2010, with regard to the follow-up and the need for reprogramming of their devices. Epidemiological data, indications, and type of pacing, even the need for visits to alter device settings (about 25 %), were also proportional to those of our recording. The mean age of the patients was 74 years (men: 55.4 %), the AV blocks were the leading cause of implantation (39.8 %), followed by sick sinus syndrome (37.5 %) and atrial fibrillation with slow conduction (17.8 %). The most common type of pacing was the dual-chamber type. In follow-up visits, the need for changes at stimulation and sensing threshold and PM’s mode were also the most frequent.
Similarly, van Eck et al7, in a similar publication in 2008 regarding patients with permanent PM showed comparable results: mean age of 73.8 years, 57 % men, 40 % AV blocks, 35 % sick sinus syndrome, 17 % atrial fibrillation with slow conduction, 68 % DDD type and 24 % VVI, while the parameters that were reprogrammed by physicians or technicians were the same. Also, Tuppin et al8 recorded similar results in 2011 in France: 75.4 % dual-chamber PMs, 21.5 % single-chamber, the mean age of implantation at 77 years, with men also slightly dominating over women in frequency (55 %).
In United States of America, Greenspon et al9 in a retrospective study of PM implants from 1993 to 2009, found that over the years the use of dual-chamber (DDD) PMs increased from 62 % to 82 %, while single-chamber PMs (VVI) reduced from 36 % to 14 % (we started to treat “younger” patients). As a result, patients lived longer, but with new co-morbidities, and this had an impact on their quality of life so as on the health system in general. AAI type PMs were also reported in a very small percentage of patients (0.5 %), while the cardiac resynchronization therapy PMs (CRT-P) were reported at 1.9 %. Similar reports were also published in Turkey by Bayata et al in 201010 and in Israel by Antonelli et al in 201511.
Finally, an earlier Greek recording by Styliadis et al in 200812, revealed as the leading cause of PM implantation (45.7 %) the AV conduction abnormalities, followed by sinus node disease (32.8 %) and atrial fibrillation with slow ventricular conduction (12.1 %). There was a downward trend in VVI PM implantation rates and a corresponding rise of DDD(R) mode.
In all these records as well as in ours, long-term and cross-sectional stability of the measurements was observed, concerning the patients and the reprogrammed parameters13. Τhe correct setting and operation of the PM system, beyond the unquestionable utility for the patient, also helps to extend the life expectancy of the device14,15.
The detection of atrial fibrillation through the devices, led to pharmaceutical adaptation for the patients, especially when anticoagulants were needed. This was also the most common reason for reprogramming the device, especially for changing the mode of pacing in patients with a dual-chamber system, from the DDD type to the VVI type. The finding in our Unit that the DDD(R) pacing pattern receded with the age of patients was consistent with the recorded experience in the international medical literature. Especially for patients over 80 years old, pacing type (single- or dual-chamber) did not appear to play an important role in their survival, in contrast to sex, the presence of congestive heart failure, coronary artery disease, and diabetes mellitus16. However, a recent study found that at these patients, DDD-mode of pacing is probably associated with decreased mortality and that advanced age by its own should not be an exclusion criterion for dual-chamber pacing17.
Ventricular pacing increases the likelihood of occurrence of symptoms of heart failure and atrial fibrillation over time18. Especially for patients with sick sinus syndrome, it was found that AAIR atrial pacing is associated with a significantly lower incidence of atrial fibrillation19, and we can achieve the same result by minimizing DDD pacing in patients with a dual-chamber pacing system20. While it is self-evident that pacing which maintains AV synchrony (AAI or DDD vs VVI) is preferable21 (and there are studies showing slight survival benefit)14, however, large multicentre studies such as MOST22, CTOPP23 and UKRACE24 did not show any superiority in survival associated with the type of pacing; the co-morbidities were those that ultimately defined it, anyway25.
In our study, complications involving patients with a PM were extremely low (only 26 patients) and were mainly due to device electrodes (insulation failure, lead fracture or change of lead location requiring re-implantation, etc.). They usually came with symptoms of heart failure or symptomatic bradycardia and dizziness, while in a few cases they were asymptomatic26. It is worth to be mentioned that our hospital is a secondary healthcare center where until now permanent PMs are not implanted. Therefore, patients that experience direct complications associated with the implantation of such devices (e.g., pneumothorax, cardiac perforation or tamponade, pocket hematoma, etc.) were treated locally in the centers where the device had been implanted. When there is a problem with PM’s leads, initially an attempt is made to reprogram the settings27, and if there is no therapeutic effect, then they are referred to the particular centers to be managed. In the medical literature, a percentage of such complications related to PM’s leads are reported at 2 % in the first year and 8.3 % in the first five years following implantation28. The new field of research over Leadless Cardiac PMs, if it prevails, will relieve patients of all these complications29,30.
Regarding the operation costs of the PU, one should note that the prefecture of Hemathia is mostly a lowland area allowing easy access from most settlements to the Veroia Hospital within half an hour. The nearest centers of tertiary care in the city of Thessaloniki are 80 km away. Thus, attendance to the Unit is convenient and comfortable for patients residing in the area, while at the same time reduces the workload of the tertiary centers, which serve a large number of patients from all around Northern Greece. The combination of patient benefit, with decentralization and decongestion of the healthcare system, makes the cost-effectiveness of operating a PU in a secondary care center, clearly acceptable. On this concept, we expect more studies to be published for the follow-up of patients with a permanent PM in secondary care centers.
Conclusion
During the 16 operational years of the PU of the General Hospital of Veroia and the follow-up of hundreds of patients, we observed that the indications for PM implantations remained unchanged over these years of the ongoing study and were based on confirmed bradycardias and major symptoms. Quite often, it is necessary to reprogram a device, which is directly served in our PU. We also found that in those patients co-existence of atrial fibrillation and heart failure, as well as the application of single-chamber ventricular pacing, deteriorates their quality of life. The operation of such a Unit in a secondary care center has acceptable cost-effectiveness.
Conflict of interest
Nothing to declare.
References
- 1.Udo EO, van Hemel NM, Zuithoff NP, Barrett MJ, Ruiter JH, Doevendans PA, et al. Incidence and predictors of pacemaker reprogramming: potential consequences for remote follow-up. Europace. 2013;15:978–983. doi: 10.1093/europace/eut002. [DOI] [PubMed] [Google Scholar]
- 2.Curila K, Smida J, Herman D, Osmancik P, Stros P, Zdarska J, et al. Pacemaker reprogramming rarely needed after device replacement. Herz. 2019;44:56–59. doi: 10.1007/s00059-017-4627-5. [DOI] [PubMed] [Google Scholar]
- 3.Arora S. Shortness of breath in a patient with complete heart block and permanent pacemaker: A case of effective pacemaker reprogramming. J Arrhythm. 2015;31:411–413. doi: 10.1016/j.joa.2015.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roberts PR. Follow up and optimization of cardiac pacing. Heart. 2005;91:1229–1234. doi: 10.1136/hrt.2004.054528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peal JE, Mathews IG, Runnett C, Thomas HE, Ripley DP. An update on cardiac implantable electronic devices for the general physician. J R Coll Physicians Edinb. 2018;48:141–147. doi: 10.4997/JRCPE.2018.208. [DOI] [PubMed] [Google Scholar]
- 6.Proclemer A, Ghidina M, Gregori D, Facchin D, Rebellato L, Zakja E, et al. Trend of the main clinical characteristics and pacing modality in patients treated by pacemaker: data from the Italian Pacemaker Registry for the quinquennium 2003-07. Europace. 2010;12:202–209. doi: 10.1093/europace/eup346. [DOI] [PubMed] [Google Scholar]
- 7.van Eck JW, van Hemel NM, de Voogt WG, Meeder JG, Spierenburg HA, Crommentuyn H, et al. Routine follow-up after pacemaker implantation: frequency, pacemaker programming and professionals in charge. Europace. 2008;10:832–837. doi: 10.1093/europace/eun093. [DOI] [PubMed] [Google Scholar]
- 8.Tuppin P, Neumann A, Marijon E, de Peretti C, Weill A, Ricordeau P, et al. Implantation and patient profiles for pacemakers and cardioverter-defibrillators in France (2008-2009) Arch Cardiovasc Dis. 2011;104:332–342. doi: 10.1016/j.acvd.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Greenspon AJ, Patel JD, Lau E, Ochoa JA, Frisch DR, Ho RT, et al. Trends in permanent pacemaker implantation in the United States from 1993 to 2009: increasing complexity of patients and procedures. J Am Coll Cardiol. 2012;60:1540–1545. doi: 10.1016/j.jacc.2012.07.017. [DOI] [PubMed] [Google Scholar]
- 10.Bayata S, Yeşil M, Arikan E, Postaci N, Berilğen R, Ceylan O, et al. [Retrospective analysis of 1650 permanent pacemaker implantations experience over two different consecutive time periods in a single cardiology clinic] Anadolu Kardiyol Derg. 2010;10:130–134. doi: 10.5152/akd.2010.037. [DOI] [PubMed] [Google Scholar]
- 11.Antonelli D, Ilan L, Freedberg N, Feldman A, Turgeman Y. [TRENDS OF PERMANENT PACEMAKER IMPLANTATION IN A SINGLE CENTER OVER A 20-YEAR PERIOD] Harefuah. 2015;154:288–291. [PubMed] [Google Scholar]
- 12.Styliadis IH, Mantziari AP, Gouzoumas NI, Vassilikos VP, Paraskevaidis SA, Mochlas ST, et al. Indications for permanent pacing and pacing mode prescription from 1989 to 2006. Experience of a single academic centre in Northern Greece. Hellenic J Cardiol. 2008;49:155–162. [PubMed] [Google Scholar]
- 13.Gierula J, Jamil HA, Byrom R, Joy ER, Cubbon RM, Kearney MT, et al. Pacing-associated left ventricular dysfunction? Think reprogramming first! Heart. 2014;100:765–769. doi: 10.1136/heartjnl-2013-304905. [DOI] [PubMed] [Google Scholar]
- 14.Udo EO, van Hemel NM, Zuithoff NP, Dijk WA, Hooijschuur CA, Doevendans PA, et al. Pacemaker follow-up: are the latest guidelines in line with modern pacemaker practice? Europace. 2013;15:243–251. doi: 10.1093/europace/eus310. [DOI] [PubMed] [Google Scholar]
- 15.Benkemoun H, Sacrez J, Lagrange P, Amiel A, Prakash A, Himmrich E, et al. Optimizing pacemaker longevity with pacing mode and settings programming: results from a pacemaker multicenter registry. Pacing Clin Electrophysiol. 2012;35:403–408. doi: 10.1111/j.1540-8159.2011.03318.x. [DOI] [PubMed] [Google Scholar]
- 16.Udo EO, van Hemel NM, Zuithoff NP, Kelder JC, Crommentuijn HA, Koopman-Verhagen AM, et al. Long-term outcome of cardiac pacing in octogenarians and nonagenarians. Europace. 2012;14:502–508. doi: 10.1093/europace/eur329. [DOI] [PubMed] [Google Scholar]
- 17.Krzemień-Wolska K, Tomasik A, Wojciechowska C, Barańska-Pawełczak K, Nowalany-Kozielska E, Jacheć W. Prognostic Factors in Patients with an Implanted Pacemaker after 80 Years of Age in a 4-Year Follow-Up. Gerontology. 2018;64:107–117. doi: 10.1159/000481504. [DOI] [PubMed] [Google Scholar]
- 18.Udo EO, van Hemel NM, Zuithoff NP, Doevendans PA, Moons KG. Risk of heart failure- and cardiac death gradually increases with more right ventricular pacing. Int J Cardiol. 2015;185:95–100. doi: 10.1016/j.ijcard.2015.03.053. [DOI] [PubMed] [Google Scholar]
- 19.Kristensen L, Nielsen JC, Mortensen PT, Pedersen OL, Pedersen AK, Andersen HR. Incidence of atrial fibrillation and thromboembolism in a randomized trial of atrial versus dual chamber pacing in 177 patients with sick sinus syndrome. Heart. 2004;90:661–666. doi: 10.1136/hrt.2003.016063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sweeney MO, Bank AJ, Nsah E, Koullick M, Zeng QC, Hettrick D, et al. Minimizing ventricular pacing to reduce atrial fibrillation in sinus-node disease. N Engl J Med. 2007;357:1000–1008. doi: 10.1056/NEJMoa071880. [DOI] [PubMed] [Google Scholar]
- 21.Vanerio G, Maloney JD, Pinski SL, Simmons TW, Castle LW, Trohman RG, et al. DDIR versus VVIR pacing in patients with paroxysmal atrial tachyarrhythmias. Pacing Clin Electrophysiol. 1991;14:1630–1638. doi: 10.1111/j.1540-8159.1991.tb02739.x. [DOI] [PubMed] [Google Scholar]
- 22.Lamas GA, Lee KL, Sweeney MO, Silverman R, Leon A, Yee R, et al. Ventricular pacing or dual-chamber pacing for sinus-node dysfunction. N Engl J Med. 2002;346:1854–1862. doi: 10.1056/NEJMoa013040. [DOI] [PubMed] [Google Scholar]
- 23.Connolly SJ, Kerr CR, Gent M, Roberts RS, Yusuf S, Gillis AM, et al. Effects of physiologic pacing versus ventricular pacing on the risk of stroke and death due to cardiovascular causes. Canadian Trial of Physiologic Pacing Investigators. N Engl J Med. 2000;342:1385–1391. doi: 10.1056/NEJM200005113421902. [DOI] [PubMed] [Google Scholar]
- 24.Toff WD, Camm AJ, Skehan JD, United Kingdom Pacing and Cardiovascular Events Trial Investigators Single-chamber versus dual-chamber pacing for high-grade atrioventricular block. N Engl J Med. 2005;353:145–155. doi: 10.1056/NEJMoa042283. [DOI] [PubMed] [Google Scholar]
- 25.Brunner M, Olschewski M, Geibel A, Bode C, Zehender M. Long-term survival after pacemaker implantation. Prognostic importance of gender and baseline patient characteristics. Eur Heart J. 2004;25:88–95. doi: 10.1016/j.ehj.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 26.García-Izquierdo E, Parra C, Toquero J. Dizziness in a patient with a permanent VVI pacemaker. Am J Emerg Med. 2018;36:524. doi: 10.1016/j.ajem.2017.11.051. [DOI] [PubMed] [Google Scholar]
- 27.Fuertes B, Toquero J, Arroyo-Espliguero R, Lozano IF. Pacemaker lead displacement: mechanisms and management. Indian Pacing Electrophysiol J. 2003;3:231–238. [PMC free article] [PubMed] [Google Scholar]
- 28.Bracke FA, Meijer A, van Gelder LM. Pacemaker lead complications: when is extraction appropriate and what can we learn from published data? Heart. 2001;85:254–259. doi: 10.1136/heart.85.3.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sideris S, Archontakis S, Dilaveris P, Gatzoulis KA, Trachanas K, Sotiropoulos I, et al. Leadless Cardiac Pacemakers: Current status of a modern approach in pacing. Hellenic J Cardiol. 2017;58:403–410. doi: 10.1016/j.hjc.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 30.Tjong FVY, Knops RE, Udo EO, Brouwer TF, Dukkipati SR, Koruth JS, et al. Leadless pacemaker versus transvenous single-chamber pacemaker therapy: A propensity score-matched analysis. Heart Rhythm. 2018;15:1387–1393. doi: 10.1016/j.hrthm.2018.04.027. [DOI] [PubMed] [Google Scholar]


