Dear Editor,
A 61-year-old woman was referred to the outpatient’s department due to persistent vulvar itchiness and soreness. She had been clinically diagnosed with lichen sclerosus (LS) in primary healthcare two years before referral and was being treated with topical steroids.
One year before her presentation, she was diagnosed with breast cancer and had a lumpectomy, axillary lymph node dissection, and adjuvant radiotherapy. She had a history of hysterectomy for benign reasons, suffered from pernicious anemia and was a non-smoker.
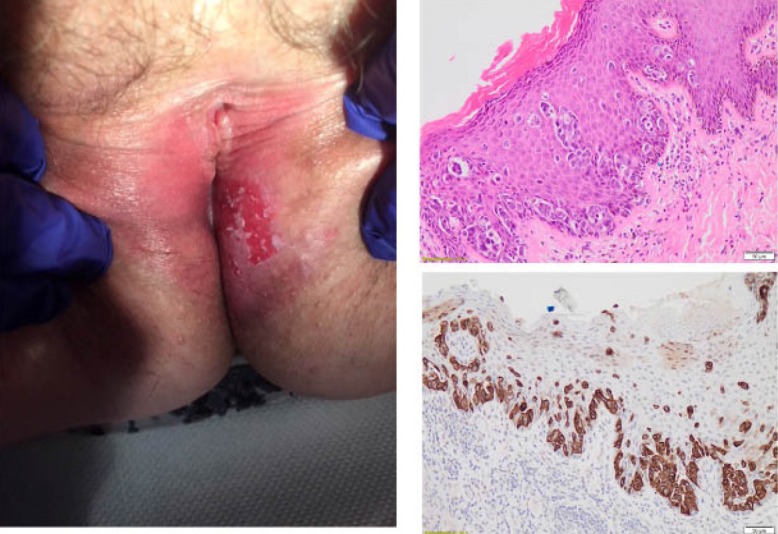
Physical examination revealed significant atrophy, resorption, and fusion of the labia minora and clitoris consistent with LS. However, on the left labium majus there was a lesion which had reportedly developed over the past few months. This was a well-demarcated 5 x 3 cm plaque of eczematous appearance with lichenification, significant erythema, and excoriations. The histopathological examination of the excisional vulvar biopsy revealed vulvar Paget’s disease (VPD) that was CK7 positive and CK20 negative (Figure 1).
Figure 1. The left-sided vulvar lesion that was excised (left image). Paget cells within the epidermis (upper right: Hematoxylin-Eosin staining, x200; lower right: CK7 positive immunostaining, x200).
Due to her breast cancer history and to exclude any secondary invasion from an underlying rectal, anal or urogenital adenocarcinoma, a computed tomography imaging of her chest, abdomen, and pelvis was performed with no abnormal findings. Urine cytology testing was negative. The tumor panel board due to the large size of the vulvar lesion suggested treatment with topical imiquimod for 16 weeks. The patient is currently asymptomatic.
Vulvar LS is a chronic pruritic skin disorder which could potentially develop into invasive squamous-cell carcinoma1. VPD is rare intraepithelial neoplasia originating either primarily from vulvar apocrine-gland bearing skin cells or is secondary to adjacent primary anal, rectal, or bladder adenocarcinomas2. There are only a few reports of LS co-existing with VPD3,4. Like in our case, due to overlapping symptoms with LS there can be a time delay before the diagnosis of VPD is established through vulvar biopsies5.
Conflict of Interest
None.
References
- 1.Fox H, Wells M. Recent advances in the pathology of the vulva. Histopathology. 2003;42:209–216. doi: 10.1046/j.1365-2559.2003.01578.x. [DOI] [PubMed] [Google Scholar]
- 2.Wilkinson EJ, Brown HM. Vulvar Paget disease of urothelial origin: a report of three cases and a proposed classification of vulvar Paget disease. Hum Pathol. 2002;33:549–554. doi: 10.1053/hupa.2002.124788. [DOI] [PubMed] [Google Scholar]
- 3.Bansal D, Bowman CA. Extramammary Paget’s disease masquerading as lichen sclerosus. Int J STD AIDS. 2004;15:141–142. doi: 10.1258/095646204322764361. [DOI] [PubMed] [Google Scholar]
- 4.Rafiei R, Eftekhari H, Granmayeh S, Nickhah N, Rafiee B. Extramammary Paget’s Disease Associated With Genital Wart and Lichen Sclerosus. Acta Med Iran. 2017;55:591–593. [PubMed] [Google Scholar]
- 5.van der Linden M, Meeuwis KA, Bulten J, Bosse T, van Poelgeest MI, de Hullu JA. Paget disease of the vulva. Crit Rev Oncol Hematol. 2016;101:60–74. doi: 10.1016/j.critrevonc.2016.03.008. [DOI] [PubMed] [Google Scholar]


