Abstract
Background
Hospital readmissions after liver transplantation (LT) are common and associated with increased morbidity and cost. High readmission rates at our center motivated a change in practice with adoption of a nurse practitioner (NP)-based post-transplant care program. We sought to determine if this program was effective in reducing 30- and 90-day readmissions after LT, and to identify variables associated with readmission.
Methods
We performed a retrospective cohort study of all patients undergoing LT from 7/½014 to 6/30/2017 at a tertiary LT referral center. A nurse practitioner (NP)-based post-transplant care program with weekend in-house nurse coordination providers and increased outpatient NP clinic availability was instituted on 1/½016. Post-discharge readmission rates at 30 and 90 days were compared in the pre- and post-exposure groups, adjusting for associated risk factors.
Results
A total 362 patients were included in the analytic cohort. There were no significant differences in demographics, comorbidities, or index hospitalization characteristics between groups. In adjusted analyses, the risk of readmission in the post-exposure group was significantly reduced relative to baseline at 30 days (hazard ratio [HR] 0.60, 95% confidence interval [CI] 0.39 – 0.90; p=0.02) and 90 days (HR 0.49, 95% CI 0.34 – 0.71; p<0.001). Risk factors positively associated with 30-day readmission included peri-transplant dialysis (HR 1.70, 95% CI 1.13 – 2.58, p=0.01) and retransplant on index hospitalization (HR 10.21, 95% CI 3.39 – 30.75, p<0.001). Male sex was protective against readmission (HR 0.66, 95% CI 0.45 – 0.97; p=0.03).
Conclusion
Implementation of expanded NP-based care after LT was associated with significantly reduced 30-day and 90-day readmission rates. LT centers and other service lines using significant post-surgical resources may be able to reduce readmissions through similar programs.
Introduction
Since the inception of the Hospital Readmissions Reduction Program in 2013 there has been an increased focus on reducing 30-day hospital readmissions for an expanding range of medical and surgical diagnoses.1, 2 Liver transplantation (LT) is marked by extremely high 30-day readmission rates, with estimates ranging from 20% to 45%.3,4, 5 These readmissions are associated with significant economic burden, adding an estimated $43,785 to 90-day costs in patients who are readmitted.6 Furthermore, post-LT 30-day readmissions are independently associated with 90-day mortality (26.8% vs. 9.8% for no readmission in one study).1 Given the high frequency, costs, and morbidity associated with this prospective quality measure, several studies have sought to identify risk factors for 30-day readmissions.3–5, 7 However, to date no studies have attempted to evaluate programs aimed at reducing hospital readmissions in this patient population.
One framework to understand high readmission rates involves identifying imbalances in patient burdens (workload) and resource availability (capacity).8 Post-LT patients have significant healthcare demands (managing immunosuppressive medications, post-surgical recovery and rehabilitation, coordinating specialist care, etc.) but too often have limited hospital-based resources to support them after discharge. As such, programs that aim to reliably enhance access to post-discharge care and augment self-care are among the most effective in reducing 30-day readmissions.9 This includes transitional programs that leverage advanced healthcare professionals such as nurse practitioners (NPs).10–12 We aimed to pilot an NP-driven program focusing on increased access to outpatient care in the post-LT discharge setting, and to evaluate its impact on 30 and 90-day hospital readmissions.
Methods
Study Design and Patient Population
We performed a retrospective cohort study of liver transplant recipients at the Hospital of the University of Pennsylvania between 7/½014 and 6/30/2017. The two cohorts of interest were defined temporally (pre/post) based on the introduction of an NP-based program on 1/½016. Patients aged ≥18 years undergoing first liver transplantation for any indication were screened for inclusion. Patients receiving multi-organ transplants were excluded, as were as were those who did not survive to post-transplant discharge (n = 1), or who died within 30 or 90 days of index hospital discharge (n = 1 and 4, respectively).
Variable Collection and Outcomes of Interest
Chart reviews were performed to obtain demographics (age, sex, race), transplant data, and clinical data, including body mass index (BMI), etiology of liver disease (hepatitis C, hepatitis B, alcoholic liver disease, non-alcoholic fatty liver disease [NAFLD], autoimmune, or other), calculated model for end-stage liver disease-sodium (MELD-Na) at transplant, receipt of MELD exception points, MELD-Na score with exceptions, peritransplant hemodialysis (HD) status, transplant from inpatient versus outpatient status, need for subsequent retransplant during index hospitalization (for complications such as hepatic artery thrombosis or primary non-function), index hospitalization length of stay, post-operative length of stay, weekend discharge status, index hospitalization discharge disposition (home, rehab, or skilled nursing facility/long-term care), and distance to transplant center (in miles). In light of effective therapies for hepatitis C resulting in decreased transplantations and improved post-transplant outcomes for this group,13, 14 we also created a binary HCV-related liver disease variable to specifically address the impact of HCV over this interval. The timing and number of hospital readmissions were recorded over an observation window of 90 days for each patient. This was used to compute the primary outcome: 30- and 90-day hospital readmissions. Finally, the numbers of outpatient phone encounters as well as completed outpatient clinic visits were recorded, as were 90-day and 1-year graft and patient survival for each group.
Pre-Exposure Care Model
The implementation of an expanded NP-based care model (exposure) with a weekend in-house coordinator took effect on January 1, 2016. Prior to this (pre-exposure), liver outpatients were followed by three NPs and one registered nurse (RN) with no weekend in-house coordinator coverage. One NP managed the post-liver transplant patients from the day of discharge through post-operative day (POD) 30. This involved follow-up phones calls to assist with medication management, address laboratory abnormalities, and triage patient concerns. The two other NPs assumed patient care after POD 30 with the assistance of the RN. Clinic days were held on Tuesdays or Wednesdays and patients could be seen by any of the three NPs. The general scheduling frequency for outpatient clinic visits was weekly for the first month, every other week for the second month, and every third week for the third month. If an urgent issue arose on non-clinic days, patients would likely be sent to the emergency room or directly readmitted from home. Outpatient labs were drawn at least weekly, usually on days of clinic visits. After-hours call was divided among the three NPs and RN for both weekdays and weekends.
Post-Exposure Care Model
Beginning on January 1, 2016 (post-exposure), patients were alphabetically assigned to one of five NPs from the day of discharge through the rest of their post-transplant course. The intent of the change was to improve continuity of care, increase the patient to provider ratio, and expand access to clinic visits, phone calls, and messages to take place between the NPs and patients. Patients received phone calls from their NP on the day after discharge, any time new laboratory values resulted, or whenever medications were changed. The goal was to increase proactive phone calls in order to address potential problems and prevent emergency admissions wherever possible. As before, any urgent patient phone call would be returned by the provider on call. The frequency of scheduled clinic visits remained the same as in the pre-exposure era, however patients could now be seen on any weekday if an urgent issue arose, made possible through flexible clinic access from an increased number of providers. Outpatient labs continued to be drawn at least weekly, without change from prior practice. After-hours call was divided among the five NPs from Monday through Thursday, and the weekend in-house coordinator (a certified clinical transplant coordinator and RN) took call Friday night through Monday morning. The weekend coordinator also rounded on admitted patients with the service attending, made follow-up phone calls to recently-discharged patients, and triaged any urgent outpatient issues or concerns.
Patient Characteristics and Unadjusted Primary Analysis
Baseline demographic and clinical patient characteristics were compared between pre- and post-exposure cohorts. The proportion of patients with 30-day and 90-day readmissions were compared between cohorts as the primary analysis, and relative risks with 95% confidence intervals were computed. Time to first readmission was also evaluated, as well as differences in the numbers of phone encounters and outpatient clinic visits. Continuous data were presented as medians and interquartile ranges (IQRs), with Wilcoxon rank sum and Chi-squared tests performed for statistical inference, where applicable. Kaplan-Meier failure curves for time to first readmission were generated for both 30-day and 90-day windows and stratified by cohort, with log rank tests performed to compare distributions. A p-value <0.05 was regarded to be statistically significant, unless otherwise specified, and all data management and computations (including subsequent analyses) were performed using STATA/IC version 15.1 (College Station, TX).
Cox Proportional Hazards Regression Analysis
Univariate Cox proportional hazards regression was performed to evaluate variables potentially associated with 30- and 90-day post-transplant readmissions. A significance threshold of alpha = 0.10 was used for potential inclusion in multivariable Cox regression. Forward and clinician-driven selection methods were then used for multivariable Cox regression, with an alpha = 0.05 threshold used for variable retention and minimum Bayesian Information Criterion (BIC) used for final model selection. In order to determine if follow-up clinic visits impacted readmissions risk differently based on index hospital discharge disposition, we tested an interaction term between these variables in both 30- and 90-day models. Hazard ratios (HRs) and 95% confidence intervals were presented for all retained variables. Covariance and correlation matrices were also produced to ensure that significant collinearity was not present among variables, using a correlation coefficient threshold of +/−0.5. Post-hoc survival curves were then generated for 30-day and 90-day readmissions. Of note, ascertainment of outcomes was complete, and there was less than 4% missingness in the dataset used for regression analysis. As such, list-wise deletion was used as a treatment for missing data as opposed to multiple imputation.
Sensitivity and Exploratory Analyses
To address the possibility of selection bias induced by excluding patients who died within the follow-up period, we repeated the unadjusted Kaplan-Meier survival analyses using the outcome of death or readmission, at both 30 and 90 days after index hospitalization discharge, using the complete cohort in addition to patients who died within 90 days. As before, the log-rank test was used to assess for statistical difference in the survival distributions. Using this cohort, we also compared 90-day and 1-year patient and graft survival between exposure groups. Separately, in order to evaluate the impact of sex on short-term hospital readmissions, we compared calculated MELD/MELD-Na scores and MELD exceptions between males and females using Wilcoxon rank sum and Chi-squared tests.
Results
Patient Characteristics
A total of 362 patients were ultimately included in the analysis cohort—183 in the pre-exposure arm and 179 in the post-exposure arm (Supplemental Figure 1). There were no significant differences between groups in age, sex, race, BMI, etiology of liver disease, peri-transplant hemodialysis status, need for retransplant on index hospitalization, hospital length of stay, post-operative length of stay, weekend discharge status, or index post-hospitalization disposition (Table 1). More patients in the post-exposure arm received MELD exception points as compared to the pre-exposure group (22.9% versus 9.8%, p<0.001), primarily due to increased hepatocellular carcinoma exceptions, however there were no significant differences in MELD-Na at transplant (18 versus 20, p=0.20).
Table 1 –
Baseline Patient Characteristics by Cohort
| Variable | Pre-Exposure(n = 183) | Post-Exposure(n = 179) | p-value |
|---|---|---|---|
| Age at Transplant (years), median (IQR) | 58 (52, 64) | 58.0 (50, 63) | 0.32 |
| Male Sex | 124 (67.8%) | 130 (72.6%) | 0.31 |
| Race | 0.70 | ||
| White | 131 (71.6%) | 136 (76.0%) | |
| Black | 33 (18.0%) | 27 (15.1%) | |
| Asian | 5 (2.7%) | 6 (3.4%) | |
| Other/unknown | 14 (7.7%) | 10 (5.6%) | |
| Body Mass Index, median (IQR) | 27.5 (23.6, 32.6) | 26.6 (24.3, 30.7) | 0.48 |
| Etiology of Liver Disease | 0.07 | ||
| Hepatitis C | 75 (41.4%) | 63 (35.2%) | |
| Hepatitis B | 1 (0.6%) | 8 (4.5%) | |
| Alcoholic Liver Disease | 30 (16.6%) | 42 (23.5%) | |
| NAFLD | 24 (13.3%) | 16 (8.9%) | |
| Autoimmune | 32 (17.7%) | 32 (17.9%) | |
| Other | 19 (10.5%) | 18 (10.1%) | |
| MELD-Na, median (IQR) | 20 (15, 25) | 18 (12, 28) | 0.20 |
| MELD Exceptions Granted | 18 (9.8%) | 41 (22.9%) | <0.001* |
| Exception for Hepatocellular Carcinoma | 17 (9.3%) | 38 (21.2%) | 0.002* |
| MELD-Na with Exceptions, median (IQR) | 22 (16, 27) | 23 (15, 30) | 0.22 |
| Dialysis Status | 0.39 | ||
| No HD | 149 (81.9%) | 153 (85.5%) | |
| Peri-transplant HD | 33 (18.1%) | 26 (14.5%) | |
| Transplant type | 0.08 | ||
| Inpatient | 51 (27.9%) | 36 (20.1%) | |
| Elective | 132 (72.1%) | 143 (79.9%) | |
| Retransplant on Index Admission | 4 (2.2%) | 5 (2.8%) | 0.75 |
| Total Length of Stay (days), median (IQR) | 11 (8, 19) | 9.0 (7, 17) | 0.13 |
| Post-op Length of Stay (days), median (IQR) | 9 (7, 13) | 9.0 (7, 13) | 0.41 |
| Weekend Discharge | 22 (12%) | 26 (14%) | 0.48 |
| Index Hospitalization Disposition | 0.13 | ||
| Home | 129 (70.9%) | 137 (76.5%) | |
| Rehab | 48 (26.4%) | 33 (18.4%) | |
| Skilled Nursing Facility/Long-term Care | 5 (2.7%) | 9 (5.0%) | |
| Distance to Transplant Center (miles), median (IQR) | 30.1 (13.5, 82.4) | 33.6 (15.0, 66.3) | 0.75 |
Statistically significant at the alpha = 0.05 level
IQR = interquartile range; NAFLD = non-alcoholic fatty liver disease; MELD = model for end-stage liver disease; HD = hemodialysis
Unadjusted Primary Analysis
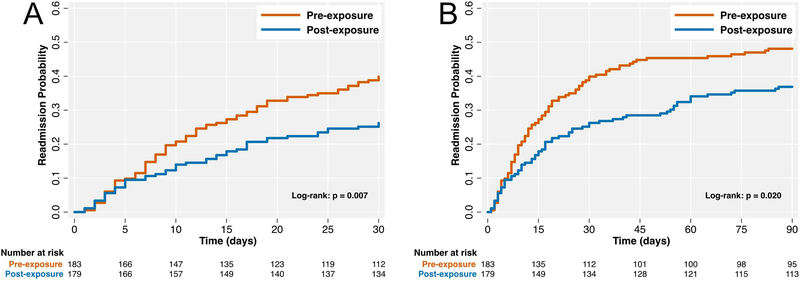
Patients in the exposure arm were less likely to be readmitted at 30- and 90-days after index hospitalization discharge (Table 2), with a 32% reduced risk of readmission at 30 days (relative risk [RR] 0.68, 95% CI 0.50 – 0.91; p=0.009) and a 22% reduced risk at 90 days (RR 0.78, 95% CI 0.61 – 0.99; p=0.04). The number of phone encounters and outpatient clinic visits were increased in the exposure group, at both 30 and 90 days (all p<0.001). There was no significant difference in median time to first readmission (p=0.26). Kaplan-Meier failure curves for 30 and 90-day readmissions, stratified by exposure arm, are presented in Figure 1. There were significant differences in time to readmission distributions between arms at 30 and 90 days (p=0.007 and p=0.02, respectively). These results were not substantively changed when performing a sensitivity analysis including patients who died during follow-up as part of the outcome (p=0.008 for 30-day analysis, and p=0.02 for 90-day analysis). Finally, there were no significant differences in patient or graft survival between groups at 90 days or 1 year (all p>0.05; Supplemental Table 1).
Table 2 –
Primary Analysis: 30-day and 90-day Readmissions by Cohort
| Variable | Pre-Exposure(n = 183) | Post-Exposure(n = 179) | p-value |
|---|---|---|---|
| Time to Readmission (days), median (IQR) | 12.0 (7.0, 26.5) | 16.5 (5.0, 40.0) | 0.26 |
| Readmitted within Thirty Days | 0.006* | ||
| No | 110 (60.1%) | 132 (73.7%) | |
| Yes | 73 (39.9%) | 47 (26.3%) | |
| Clinic Visits at 30 Days, median (IQR) | 3.0 (2.5, 4.0) | 4.0 (3.0, 4.0) | <0.001* |
| Phone Encounters at 30 Days, median (IQR) | 11.0 (8.0, 13.0) | 15.0 (11.0, 18.0) | <0.001* |
| Readmitted within Ninety Days | 0.03* | ||
| No | 95 (51.9%) | 113 (63.1%) | |
| Yes | 88 (48.1%) | 66 (36.9%) | |
| Clinic Visits at 90 Days, median (IQR) | 6.0 (5.0, 6.0) | 7.0 (6.0, 7.0) | <0.001* |
| Phone Encounters at 90 Days, median (IQR) | 23.0 (18.0, 28.0) | 30.0 (25.0, 36.0) | <0.001* |
Statistically significant at the alpha = 0.05 level
Figure 1 –
Kaplan-Meier Failure Curves for 30-day (A) and 90-day (B) Readmission
Cox Regression Analysis
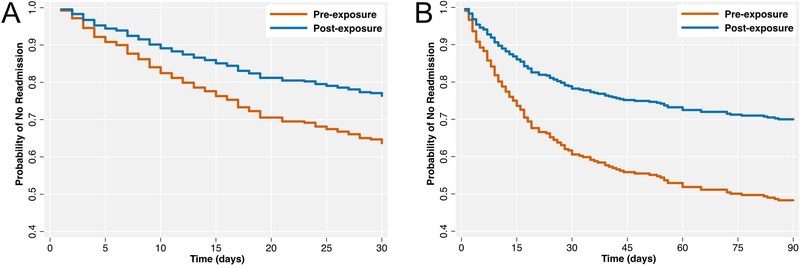
Univariate and multivariable Cox proportional hazards regression models for 30- and 90-day readmissions are presented in Table 3. In multivariable analysis, retransplant on index hospitalization and peri-transplant dialysis were strongly associated with hospital readmission at 30 days (retransplant HR 10.21, 95% CI 3.39 – 30.75; p<0.001; dialysis HR 1.70, 95% CI 1.13 – 2.58; p=0.01), but were not significantly associated with 90-day readmissions. In both models an increasing number of post-discharge phone encounters was associated with increased readmissions (30-day HR 1.08, 95% CI 1.04 – 1.13; p<0.001). Factors protective against hospital readmission in both models included male sex (30-day: HR 0.66, 95% CI 0.45 – 0.97; p=0.03), the number of outpatient clinic visits (30-day: HR 0.56, 95% CI 0.47 – 0.66; p<0.001), and exposure group status (30-day: HR 0.60, 95% CI 0.39 – 0.90; p=0.02). In the 90-day model, there was a significant interaction between index discharge disposition and number of clinic visits (p=0.0496). In particular, an increasing number of clinic visits had a stronger protective effect against readmission for patients discharged to rehab as compared to those discharged to home (HR 0.83, 95% 0.72 – 0.97; p=0.02). The associated Cox regression-adjusted survival curves demonstrating reduced 30- and 90-day readmissions with post-exposure status are presented in Figure 2. Of note, there was no indication of significant collinearity among variables in the final regression models (data not shown). Finally, in an exploratory analysis of the impact of sex on hospital readmissions, we found that females had higher calculated MELD/MELD-Na scores at the time of transplant, and males had a higher proportion of MELD exceptions and HCC exceptions (Supplemental Table 2).
Table 3 –
Univariate and Multivariable Cox Regression Analysis: Variables Associated with 30-day and 90-day Readmission
| Univariate Analysis* |
Multivariable Analysis |
|||
|---|---|---|---|---|
| Variable | Hazard Ratio (95% CI) | p-value | Hazard Ratio (95% CI) | p-value |
| 30-Day Readmission | ||||
| Male Sex | 0.67 (0.46 – 0.96) | 0.03 | 0.66 (0.45 – 0.97) | 0.03 |
| Transplant MELD-Na (per 5 points) | 1.09 (0.99 – 1.21) | 0.09 | ∙ | ∙ |
| Peri-transplant Dialysis | 2.24 (1.50 – 3.35) | <0.001 | 1.70 (1.13 – 2.58) | 0.01 |
| Retransplant | 2.23 (0.91 – 5.47) | 0.08 | 10.21 (3.39 – 30.75) | <0.001 |
| Total Length of Stay (per day) | 1.01 (1.00 – 1.01) | 0.05 | ∙ | ∙ |
| Index Hospitalization Disposition (ref = Home) | ||||
| Rehab | 2.01 (1.37 – 2.96) | <0.001 | ∙ | ∙ |
| Skilled Nursing Facility/Long-term Care | 1.22 (0.49 – 3.01) | 0.67 | ∙ | ∙ |
| Exposure Arm | 0.61 (0.42 – 0.88) | 0.008 | 0.60 (0.39 – 0.90) | 0.02 |
| Number of Clinic Visits | 0.60 (0.51 – 0.71) | 0.000 | 0.56 (0.47 – 0.66) | <0.001 |
| Number of Phone Encounters | 1.03 (1.00 – 1.07) | 0.06 | 1.08 (1.04 – 1.13) | <0.001 |
| 90-Day Readmission | ||||
| Male Sex | 0.63 (0.46 – 0.88) | 0.006 | 0.63 (0.45 – 0.88) | 0.007 |
| MELD exception granted | 0.62 (0.38 – 1.02) | 0.06 | ∙ | ∙ |
| Peri-transplant Dialysis | 1.87 (1.28 – 2.72) | 0.001 | ∙ | ∙ |
| Total Length of Stay (per day) | 1.01 (1.00 – 1.01) | 0.09 | ∙ | ∙ |
| Index Hospitalization Disposition (ref = Home) | ||||
| Rehab | 1.75 (1.24 – 2.49) | 0.002 | 4.62 (1.80 – 11.9) | 0.02 |
| Skilled Nursing Facility/Long-term Care | 0.90 (0.37 – 2.21) | 0.82 | 0.90 (0.18 – 4.49) | 0.90 |
| Disposition*Clinic Visit Interaction (ref = Home) | ||||
| Rehab | 0.81 (0.68 – 0.97) | 0.02 | 0.83 (0.72 – 0.97) | 0.02 |
| Skilled Nursing Facility/Long-term Care | 0.64 (0.44 – 0.93) | 0.02 | 0.85 (0.59 – 1.21) | 0.36 |
| Exposure Arm | 0.69 (0.59 – 0.95) | 0.02 | 0.49 (0.34 – 0.71) | <0.001 |
| Number of Clinic Visits | 0.91 (0.83 – 1.00) | 0.06 | 0.92 (0.83 – 1.02) | 0.11 |
| Number of Phone Encounters | 1.03 (1.01 – 1.04) | <0.001 | 1.06 (1.04 – 1.08) | <0.001 |
The following variables were not statistically significant at the alpha = 0.10 level: age, race, body mass index, etiology of liver disease, hepatitis C-related liver disease (binary), elective transplant, post-operative length of stay, weekend discharge, distance to transplant center, MELD exception granted (30-day model), and transplant MELD-Na (90-day model)
Figure 2 –
Cox Regression Survival Functions for 30-day (A) and 90-day (B) Readmission
Trends in Clinic Visits and Phone Encounters
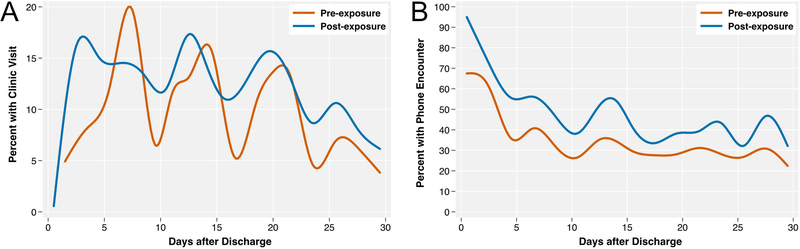
Plots of the percentages of patients with clinic visits or phone encounters through 30 days after index discharge, stratified by exposure group, are shown in Figure 3. In general, patients in the post-exposure group had earlier first clinic visits, and the subsequent visits were more evenly distributed over time. This was in contrast to the pre-exposure where clustering of clinic visits on certain days after discharge was observed. Nearly all patients in the post-exposure group had an early phone encounter, and the proportion of patients with phone encounters was uniformly higher through 30 days for this group.
Figures 3 –
Percent of Patients with a Clinic Visit (A) or Phone Encounter (B) through 30 Days Post-Discharge
Discussion
In this study of 362 post-LT patients, we found that an NP-based post-transplant program was associated with significantly decreased hazards of 30- and 90-day hospital readmission. This quality improvement was made without a reduction in transplant quantity, patient complexity, or patient survival. To date, most studies have focused on the identification of risk factors for hospital readmissions in this population,3–5 and while it has been shown that protocols can reduce readmissions while maintaining volume,15, 16 to our knowledge this is the first report of an NP-based program to accomplish this goal. We believe this is especially impactful due to the high volume of our transplant center, the novel nature of the NP-driven program, and our inclusion of high-risk patients in our analysis (e.g. those who required short-term retransplantation).
In order to isolate the impact of our program on readmission rates, we performed multivariable analysis. Adjusting for sex, peri-transplant dialysis, and discharge disposition, which are all previously-established risk factors for readmission,3, 5 we found that program exposure and an increased number of clinic visits protected against readmission. This strongly suggests that increased outpatient clinic access played a pivotal role in reducing 30- and 90-day readmissions. When evaluating the timing of outpatient clinic visits, we found that the pre-exposure group had clear clustering of visits on certain days after transplant, while the post-exposure group had more uniformly distributed visits, in addition to a shorter time to first visit. This implies that patients took advantage of the increased clinic availability, and that addressing developing outpatient issues in a timelier manner may have contributed to reduced hospital readmissions. Separately, we also found that an increased number of telephone encounters increased the hazard for readmission. Presumably, a high number of telephone encounters may have served as a signal of developing complications, and if warranted patients would have been directed to present to the hospital. Taken together, these findings arguably reflect appropriate triage of patient concerns as opposed to all patients presenting to the emergency department, from which location most transplant patients are admitted. Finally, it is interesting to note that male sex was protective against hospital readmission in our study. In an exploratory analysis, we found that males were more likely to have received MELD exceptions and HCC exceptions, consistent with prior literature.17 As such, females had higher calculated MELD and MELD-Na scores at the time of transplant, representing more severe underlying liver disease. This is a known risk factor for post-transplant readmission,18 and likely explains the impact of sex in this study. Importantly, although MELD score was not retained in any of our final multivariable models, we believe that this is due to collinearity with sex in our cohort.
Although not explicitly studied herein, reductions in post-LT hospital readmissions are expected to have a health care cost benefit. Similar to other studies,19 the majority of readmissions in our cohort (~75%) occurred within 30 days of discharge. In this time period, we noted a 33% increase in the number of clinic visits and a 36% increase in telephone encounters. Although the program required additional NPs and outpatient clinic utilization, this cost may be balanced by reduced hospital readmissions. Additionally, preventive management may mitigate escalation of complications, both in terms of cost and medical complexity. Indeed, one study which quantified the cost burden of early post-LT readmissions merged two national data sources: the University Health System Consortium and the Scientific Registry of Transplant Recipients. Their five-year analysis of more than 12,000 transplant recipients demonstrated 30- and 90-day readmission rates of 38% and 48%, respectively, each associated with approximately $43,785 in additional costs in comparison to those patients who were not readmitted.6 Furthermore, with the inception of negotiated global fees for transplant, hospitals are effectively penalized for short-term post-LT readmissions from a reimbursement standpoint.15
Work from Tapper et al highlights that further efforts in reducing post-LT readmissions should focus on high-risk patients and potentially preventable readmissions.16 To this point, an interesting and novel finding in our study was that patients who received retransplant on the index admission—most commonly due to hepatic artery thrombosis—had the most dramatically increased risk of readmission (greater than 10-fold increased hazard). This effect was only significant for 30-day readmission, as retransplant was not a significant predictor in the 90-day readmission model. Although based on a small sample size, this suggests that a particularly high-risk population that may benefit from special or tailored focus in future programs are patients who receive an early retransplantation. Because the increased risk for readmission appears to be time-limited, once these patients have cleared the 30-day post-discharge time point it may be reasonable to return them to standard protocols. Another potentially high-risk group includes patients discharged to rehab after the index hospitalization. Indeed, in our 90-day model, we identified a significant interaction between outpatient clinic visits and index discharge disposition. Patients discharged to rehab had the highest overall hazard of readmission, however each incremental clinic visit benefitted rehab patients more than patients discharged to home. From a readmission reduction perspective, this suggests that ensuring adequate outpatient follow-up is especially critical for these patients.
There are several limitations worthy of discussion in our study. First, there is possible misclassification of outcomes, as some patients may have been readmitted to other hospitals. However, this bias would be non-differential, impacting both groups equally. Furthermore, we expect these events to be rare, as our transplant patients are typically transferred to our institution if they are admitted elsewhere. Future efforts from our center will aim to prospectively track readmissions to any hospital. Second, there is a possibility of selection bias as we excluded patients who died within 90 days of discharge. However, only four patients were excluded for this reason, and the primary results were not substantively different when including these patients in a sensitivity analysis. This suggests that the impact of this bias was negligible. Third, we did not have direct cost comparison data in this study to explicitly evaluate the cost benefit of the program. This may be evaluated in future studies; however, we should highlight that significantly reducing post-transplant readmission rates is reflective of good patient care regardless of cost considerations. Fourth, as the new program involved multiple facets, it is difficult to determine which features were most critical in reducing readmissions. We performed a dedicated analysis of clinic visits and telephone encounters, and argue that wider clinical availability, made possible through an increased provider to patient ratio, may be among the most important factors. However, specifically interrogating the impact of a weekend in-house coordinator, for example, was not well codified in this study. Finally, the pre-post nature of the study design without a control group is a limitation. Given that this was a pragmatic trial as part of the Centers for Medicare & Medicaid Services (CMS)-mandated quality assurance and process improvement (QAPI) program for transplant centers, we opted to apply the program uniformly for all patients. During the study period, the post-transplantation model was static and no other systemic changes were initiated. To further address this limitation, however, we performed an adjusted analysis of factors associated with readmission, and exposure status remained strongly protective against readmission. Here it is important to note that although MELD exception points were granted more frequently in the post-exposure group, this likely reflects the known trend of increasing exception points over this time period,20 primarily from hepatocellular carcinoma exceptions as we have shown in this cohort. Furthermore, there were no significant differences between exposure groups in MELD-Na, a marker of severity of illness, and neither variable was retained as a significant predictor in our final multivariable models.
In conclusion, as we transition from fee-for-service to value-based care models, it is clear that quality, value, and volume must all be maintained in order for US healthcare to be successful. To this end, we found that an NP-based post-LT program successfully reduced 30- and 90-day readmission rates, mediated through increased outpatient clinic and phone call utilization, while maintaining patient outcomes. Programs that leverage advanced healthcare professionals may be well-suited to other transplantation centers, and future research should aim to validate similar programs in other contexts. We have also highlighted patients who are at exceptionally high risk of readmission, most notably those who receive short-term retransplantation and those who are discharged to rehab. Future programs should aim to explore alternatives to readmission for these high-risk groups. Importantly, the findings in this study are applicable not only to LT centers, but to any resource-intensive surgical cohorts who are subject to high rates of post-surgical readmissions (i.e. major surgical oncology, vascular, thoracic, cardiac surgery, etc.). As physicians and health systems become increasingly responsible for 30- and 90-day readmissions, all stakeholders, including patients, providers, health systems, and payers will benefit from a reduction in readmissions.
Supplementary Material
Supplemental Figure 1 – Patient Flow Diagram
Acknowledgments
Financial Support: Nadim Mahmud is supported by a National Institutes of Health T32 grant (2-T32-DK007740-21A1).
Abbreviations
- BMI
body mass index
- CMS
Centers for Medicare & Medicaid Services
- HD
hemodialysis
- HR
hazard ratio
- IQR
interquartile range
- LT
liver transplantation
- MELD
model for end-stage liver disease
- NAFLD
non-alcoholic fatty liver disease
- NP
nurse practitioner
- POD
post-operative day
- QAPI
quality assurance and process improvement
- RR
relative risk
Footnotes
Conflicts of Interest: The authors certify that they do not have any conflicts of interest or other disclosures that are relevant to the work in this manuscript.
References
- 1.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. Jama 2013;309:342–343. [DOI] [PubMed] [Google Scholar]
- 2.Zuckerman RB, Sheingold SH, Orav EJ, et al. Readmissions, observation, and the hospital readmissions reduction program. New England Journal of Medicine 2016;374:1543–1551. [DOI] [PubMed] [Google Scholar]
- 3.Berman K, Tandra S, Forssell K, et al. Incidence and predictors of 30-day readmission among patients hospitalized for advanced liver disease. Clinical Gastroenterology and Hepatology 2011;9:254–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pereira AA, Bhattacharya R, Carithers R, et al. Clinical factors predicting readmission after orthotopic liver transplantation. Liver Transplantation 2012;18:1037–1045. [DOI] [PubMed] [Google Scholar]
- 5.Paterno F, Wilson GC, Wima K, et al. Hospital utilization and consequences of readmissions after liver transplantation. Surgery 2014;156:871–879. [DOI] [PubMed] [Google Scholar]
- 6.Wilson GC, Hoehn RS, Ertel AE, et al. Variation by center and economic burden of readmissions after liver transplantation. Liver Transplantation 2015;21:953–960. [DOI] [PubMed] [Google Scholar]
- 7.Shankar N, Marotta P, Wall W, et al. Defining readmission risk factors for liver transplantation recipients. Gastroenterology & hepatology 2011;7:585. [PMC free article] [PubMed] [Google Scholar]
- 8.Shippee ND, Shah ND, May CR, et al. Cumulative complexity: a functional, patient-centered model of patient complexity can improve research and practice. Journal of clinical epidemiology 2012;65:1041–1051. [DOI] [PubMed] [Google Scholar]
- 9.Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA internal medicine 2014;174:1095–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.David D, Britting L, Dalton J. Cardiac acute care nurse practitioner and 30-day readmission. Journal of Cardiovascular Nursing 2015;30:248–255. [DOI] [PubMed] [Google Scholar]
- 11.Delgado‐Passler P, McCaffrey R. The influences of postdischarge management by nurse practitioners on hospital readmission for heart failure. Journal of the American Academy of Nurse Practitioners 2006;18:154–160. [DOI] [PubMed] [Google Scholar]
- 12.Coleman EA, Parry C, Chalmers S, et al. The care transitions intervention: results of a randomized controlled trial. Archives of internal medicine 2006;166:1822–1828. [DOI] [PubMed] [Google Scholar]
- 13.Cholankeril G, Li AA, March KL, et al. Improved Outcomes in HCV Patients Following Liver Transplantation During the Era of Direct-Acting Antiviral Agents. Clinical Gastroenterology and Hepatology 2018;16:452–453. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg D, Ditah IC, Saeian K, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation. Gastroenterology 2017;152:1090–1099. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Russo MW, Levi DM, Pierce R, et al. A prospective study of a protocol that reduces readmission after liver transplantation. Liver Transplantation 2016;22:765–772. [DOI] [PubMed] [Google Scholar]
- 16.Tapper EB. Early readmissions after liver transplantation and the power of quality improvement. Liver Transplantation 2016;22:717–719. [DOI] [PubMed] [Google Scholar]
- 17.Ioannou GN, Perkins JD, Carithers RL Jr. Liver transplantation for hepatocellular carcinoma: impact of the MELD allocation system and predictors of survival. Gastroenterology 2008;134:1342–1351. [DOI] [PubMed] [Google Scholar]
- 18.Volk ML, Tocco RS, Bazick J, et al. Hospital readmissions among patients with decompensated cirrhosis. The American journal of gastroenterology 2012;107:247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Serper M, Bittermann T, Rossi M, et al. Functional status, healthcare utilization, and the costs of liver transplantation. American Journal of Transplantation 2018;18:1187–1196. [DOI] [PubMed] [Google Scholar]
- 20.Goldberg DS, Olthoff KM. Standardizing MELD exceptions: current challenges and future directions. Current transplantation reports 2014;1:232–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1 – Patient Flow Diagram