Abstract
Background:
Migration of adult children may impact the health of aging parents who remain in low- and middle-income countries. Prior studies have uncovered mixed associations between adult child migration status and physical functioning of older parents; none to our knowledge has examined the impact on unmet caregiving needs.
Methods:
Data come from a population-based study of Mexican adults >50 years old. We analyzed 11806 respondents surveyed over an 11-year period. We used longitudinal targeted maximum likelihood estimation to estimate associations between having an adult child in the US and lower-body functional limitations, and both needs and unmet needs for assistance with basic or instrumental activities of daily living (ADLs/IADLs).
Results:
For women, having an adult child in the US at baseline and 2-year follow-up was associated with fewer lower body functional limitations (marginal risk difference (RD): −0.14, 95% CI: −0.26, −0.01) and fewer ADLs/IADLs (RD: −0.08, 95% CI: −0.16, −0.001) at 2-year follow-up. Having an adult child in the US at all three study waves was associated with more lower-body functional limitations at 11-year follow-up (RD: 0.04, 95% CI: 0.01, 0.06). Having an adult child in the US was associated with a higher prevalence of unmet needs for assistance at two (RD: 0.13, 95% CI: 0.04, 0.21) and 11-year follow-up for women (RD: 0.07, 95% CI: −0.02, 0.15) and 11-year follow-up for men (RD: 0.08, 95% CI: 0.00, 0.16).
Conclusion:
Having an adult child in the US had either null or modestly positive associations with physical functioning, but substantial adverse associations with unmet caregiving needs for a cohort of older adults in Mexico.
Keywords: Social Epidemiology, Longitudinal Study, Targeted Maximum Likelihood Estimation, Aging, Activities of Daily Living, Mexico
Introduction:
Many low- and middle-income countries are experiencing rapid aging and declining family size1, generating concern about who will care for older adults in these settings.2 This concern is heightened in countries with high rates of out-migration. As of 2017, 258 million individuals live outside of the country in which they were born, and the majority are young and middle-aged adults.3 Family-member migration may result in the loss of critical support for older adults who remain in places of origin, with potential impacts on physical wellbeing and needs for assistance in later life.
Research regarding the impact of family-member out-migration on older adults who remain in places of origin has been largely focused on mental health, with few studies on physical functioning.4,5 Findings have also been extremely mixed, with negative, positive, and null associations reported.4–14 Scholars suggest that family-member migration may result in poorer health for older adults who remain, possibly due to the loss of family members who might have otherwise provided social and instrumental support necessary for coping with life challenges. 6,13,15 Reduced support may impact older adults’ health-promoting behaviors (e.g. physical activity) and may contribute to greater risk for chronic disease and cognitive decline,16–19 in turn influencing physical functioning.20–24 Conversely, family members who migrate may contribute to improvements in the health of older adults who remain by way of remitting money,4,5,7,10 which may support the treatment of chronic conditions, with potentially positive influences on physical functioning.10,22
Extant research on family member migration and the physical functioning of older adults has also been largely limited to cross-sectional or short-term follow-up studies 4,5. Moreover, while cross-sectional studies have examined the impact of adult child migration on financial transfers and overall hours of care provided to elderly parents,25,26 no studies to our knowledge have examined whether or not family-member migration is associated with unmet caregiving needs among older adults who remain in low and middle-income settings. In the present study, we evaluate longitudinal associations between having an adult child in the US and physical functioning and unmet caregiving needs among a population-based prospective cohort of middle-aged and older adults in Mexico followed over an 11-year period. In the analyses, we correctly adjust for time-varying confounders affected by prior exposure27 and employ a doubly robust estimation approach that allows for data-adaptive model fitting.28–30
MATERIALS AND METHODS
Study Population
We use data from three waves of the Mexican Health and Aging Study (MHAS), a national survey of Mexican adults aged ≥ 50 years.31 Briefly, the MHAS selected households with adults ≥ 50 years in 2001 that were previously included in the nationally representative 2000 Mexican Employment Survey (ENE-2000). Households from Mexican states with historically high US out-migration were oversampled; households in remaining states were sampled with probability proportionate to size. Within each household, a target respondent was interviewed along with spouses or cohabitating partners. Proxy respondents were interviewed when target respondents could not respond on their own. The response rate was 91.8% at baseline (2001), 93.3% at 2-year follow-up (2003), and 88.1% at 11-year follow-up (2012). A total of 15186 respondents were surveyed at baseline. We excluded proxy respondents, spouses < 50 years, and respondents who had no living children, yielding a baseline analytic sample of 11806 (see flowchart in eAppendix Figure 1). This analysis was deemed exempt by the Institutional Review Board at the University of California San Francisco.
Study Measures
Adult Child Migration Status
Adult child migration status was derived from a household roster that queried respondents at each wave about the location of each non-resident child. We constructed binary indicators of whether or not respondents had at least one adult child living in the US at each wave.
Physical Functioning
Lower-body functional limitations were measured with eight questions regarding perceived difficulty with: running one mile, walking one or several blocks, climbing one or several flights of stairs, stooping, kneeling, or crouching. For each item, we contrasted those who had “no trouble” with the activity to those who reported they “have trouble, can’t do, or don’t do” the activity. Because of the high prevalence of reported difficulty with running a mile (75% of women and 55% of men), we consider our primary outcome of interest to be the sum of the remaining seven lower-body functional limitations, but report associations using the sum of all eight lower-body functional limitations in eAppendix Table 3.
Needs for assistance with activities of daily living (ADLs) were captured by asking respondents whether, because of a health problem, they needed assistance with the following basic activities: walking across a room, getting in and out of bed, eating, bathing, toileting, or dressing. Respondents who indicated they did not need help were contrasted with those who reported they need help, can’t do, or don’t do the activity or, in the case of walking across the room and getting out of bed, that they used assistive equipment to help them (e.g. a wheelchair). Respondents were similarly asked about need for assistance, because of a health problem, with instrumental activities of daily living (IADLs), including with managing money, taking medications, preparing a hot meal, or shopping for food. Basic activities and instrumental activities of daily living were summed to create a count of total needs for assistance (range: 0 – 10). We estimated models with continuous and binary measures of no versus any lower-body functional limitations or needs for assistance, respectively.
Unmet Needs for Assistance
Respondents who indicated that they needed assistance with any activity of daily living were then asked if they received help with the given activity from a spouse or another person. We classified respondents who reported not receiving help from either a spouse or another person as having “unmet” need for assistance. We generated a binary indicator of any versus no unmet needs.
Covariates
We selected covariates that may have contributed to both family-member migration decisions and outcomes of interest. For example, factors like family economic status and family composition32–34 and macro-level factors such as community-level experience with US migration have been shown to influence migration decisions.35,36 Many of these same factors have been associated with physical functioning and related needs and unmet needs for assistance among older adults.37,38,39,40
Time-invariant covariates include measures of baseline age in years, early life socio-economic status and health, and primary lifetime occupation. A time-invariant measure of prior US migration was included for men; few women reported prior US migration. Time-varying covariates included measures of cognitive function, depressive symptoms, number of self-reported chronic diseases, past-year health care utilization, health insurance status, monthly income, total household assets, employment status, marital status, total number of living children, total number of grandchildren, , whether or not respondents had a child living in another city in Mexico, whether or not an adult child lived in the same household, and whether the respondent could count on support from community members. Definitions for select covariates in eAppendix Table 1.
Statistical Analyses
We implemented longitudinal targeted maximum likelihood estimation (longitudinal TMLE)28,30 to estimate wave-specific associations between having an adult child in the US and outcomes of interest. Briefly, longitudinal TMLE models the expected outcome via a sequence of nested regressions and uses wave-specific inverse probability of treatment and censoring weights to update the resulting estimates.28,29,41,42 Implementation entailed first separately estimating the expected outcome for each of the three study waves (t = 1, 2, 3) for different exposure regimes.28,29,41 Models follow from the Directed Acyclic Graph presented in Figure 1. For example, for models of any (versus no) lower-body functional limitations at the third study wave (2012, t = 3)), we estimated the expected prevalence of having ≥ 1 lower-body functional limitation in 2012 for the following contrasting exposures of: 1) having at least one adult child migrant in 2001, 2003, and 2012 and 2) having no adult child migrants in 2001, 2003, or 2012, both conditional on a) time-invariant covariates, b) lagged time-varying covariates (including lagged functional limitations) from 2001 and 2003, and c) inclusion in the survey wave. There was only support in the data for contrasting stable regimes of adult child migration (i.e. having an adult child in the US at all waves compared to having no adult children in the US at any waves); a relatively small percentage of respondents reported shifts in adult child migration status across the study waves.
Figure 1.
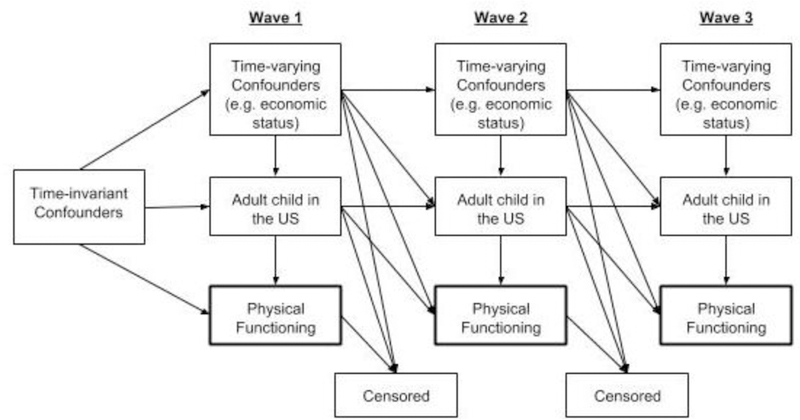
Directed Acyclic Graph Guiding Longitudinal Analyses of the Association between Adult Child US Migration Status Physical Functioning,and both Time-Varying and Time-invariant Covarities
The TMLE algorithm then updated these outcome models with cumulative inverse probability weights based on models of 1) exposure (i.e. having an adult child in the US) at each wave conditional on time-invariant covariates, lagged time-varying covariates, prior exposure, and inclusion in the survey wave, and 2) inclusion in survey wave conditional on time-invariant covariates, lagged time-varying covariates (including outcome values), and prior exposure. For analyses of lower-body functional limitations and activities of daily living, we estimated the probability of inclusion in the survey using separate models to account for attrition by the second and third follow-up waves due to 1) death, 2) having a proxy interview, or 3) loss-to-follow-up. We grouped a very small category of respondents who no longer had living children at follow-up waves with those who had a proxy interview. For analyses of unmet needs, we also generated attrition models to account for exclusion due to reporting less than one need for assistance with activities of daily living at baseline and follow-up waves. Cumulative inverse probability weights (IPWs) were truncated at the 99th percentile.43
We estimated exposure, attrition, and outcome models via SuperLearner.44 For models of continuous outcomes, the weighted convex combination of machine-learning algorithms with the lowest cross-validated mean squared error was selected among a library of three possible machine learning algorithms – LASSO,45 gradient boosting machine,46,47 and generalized linear models. Due to computational demands, we only used the gradient boosting machine algorithm for treatment and attrition models for analyses of binary outcomes. Estimation was performed using stremr 30,48 and sl349 packages for R.50
We implemented multiple imputation procedures to address missing data using the Amelia package for R.51 We created ten multiply imputed datasets for the baseline wave, and incorporated mean values from multiply imputed baseline models into the multiple imputation of time-varying measures at successive follow-up waves. We combined estimates using Rubin’s rules.52
Sensitivity Analyses
Despite including a large number of controls for respondent and family-level characteristics, we remained concerned about the potential for unmeasured confounders – particularly at the community or regional level – that might be driving both migration decisions and the health outcomes of older adults. In order to evaluate bias due to unobserved confounding, we calculated “e-values” for estimates whose 95% confidence intervals did not cross the null.53,54 E-values estimate the minimum strength of association between an unmeasured confounder and both adult child migration status and outcomes that would be required to shift observed estimates to the null, assuming the same size of association between unmeasured confounder and exposure and outcome, ly.53,54
We additionally assessed the degree to which estimates might be biased by the exclusion of respondents who had interviews completed by proxy informants in the baseline analytic sample (n = 934 respondents who were otherwise eligible based on age and having at least one living child). Proxies reported migration status of respondents’ adult children and their needs for assistance with the six basic activities of daily living (ADLs) only. We used this information to calculate bias-corrected risk ratios with the episensr package for R.55 Sample code for longitudinal TMLE and sensitivity analyses is included in the eAppendix.
RESULTS
At baseline, about a quarter of respondents reported having at least one adult child living in the US (Table 1). Nearly 70% of women and 52% of men reported at least one lower-body functional limitation and about 19% of women and 23% of men reported need for assistance with at least one activity of daily living at baseline. Of those with at least one need, 60% of women and 46% of men reported that they did not receive assistance with these needs at baseline. Additional descriptive characteristics are in eAppendix Table 2.
Table 1.
Baseline (2001) characteristics for Mexican adults > 50 years with at least one living childa
| Women | Men | |
|---|---|---|
| N | 6374 | 5432 |
| Outcomes | ||
| Number of ADLs and/or IADLs, range (0–10), mean (SD)a | 0.53 (1.51) | 0.52 (1.37) |
| ≥ 1 ADL or IADL, n (%) | 1200 (18.83) | 1225 (22.55) |
| Any unmet need, n (%)b | 725 (60.00) | 559 (45.63) |
| Number of lower-body functional limitations, range (0–7), mean (SD) | 2.32 (2.25) | 1.16 (2.04) |
| ≥ 1 lower-body functional limitation, n (%) | 4389 (68.86) | 2820 (51.91) |
| Exposure | ||
| At least one child in US, n (%) | 1532 (24.04) | 1237 (22.77) |
Source: Mexican Health and Aging Study.
Notes:
Activities of daily living (ADLs) were measured as needs for assistance (because of a health condition) with walking across a room, getting in and out of bed, eating, bathing, toileting, or dressing; instrumental activities of daily living (IADLs) were measured as needs for assistance (because of a health condition) with managing money, taking medications, preparing a hot meal, or shopping for food
Number and percent of respondents with unmet needs calculated only for respondents who reported ≥ 1 ADL or IADL.
Adjusted marginal risk differences (RDs) are presented for each study wave. In the case of binary outcomes, these results can be interpreted as the expected prevalence of the outcome at a given study wave if respondents had an adult child US migrant at that wave and all prior study waves compared to the expected prevalence of the outcome if respondents had no adult children in the US during the same time points (i.e. current study wave and all prior study waves).42 For continuous outcomes, adjusted marginal risk differences can be interpreted as the expected average difference in the outcome (e.g. number of lower body functional limitations, number of needs for assistance with activities of daily living) for the same contrasts. Baseline results are included for completeness, although lagged time-varying covariates were not available for baseline models, and estimates from these models therefore remain confounded by these factors.
For women, having at least one adult child in the US at baseline and 2-year follow-up waves was associated with fewer lower-body functional limitations (RD: −0.14, 95% CI: −0.26, −0.01), fewer needs for assistance with activities of daily living (RD: −0.08, 95% CI: −0.16, −0.001) and lower expected prevalence of reporting need for assistance with at least one activity of daily living (RD: −0.03, 95% CI: −0.05, −0.01) compared to having no adult child in the US during these two study waves (Table 2).
Table 2.
Marginal risk differences in estimated physical functioning outcomes for Mexican adults ≥ 50 years with at least one adult in the US versus no adult children in the US
| Estimated difference in the prevalence of > 1 lower-body functional limitationa | Estimated difference in average lower-body functional limitations (range: 0–7) | Estimated difference in the prevalence of > 1 ADL/IADL | Estimated difference in average ADLs/IADLs (range: 0 – 10) | |||||
|---|---|---|---|---|---|---|---|---|
| Women (n=6374) | ||||||||
| Marginal RD | 95% CI | Marginal RD | 95% CI | Marginal RD | 95% CI | Marginal RD | 95% CI | |
| 2001 | 0.02 | (−0.01, 0.04) | 0.14 | (0.03, 0.26) | 0.01 | (−0.03, 0.01) | 0.02 | (−0.06, 0.09) |
| 2003 | −0.01 | (−0.04, 0.02) | −0.14 | (−0.26, −0.01)c | −0.03 | (−0.05, −0.01)d | −0.08 | (−0.16, −0.00)e |
| 2012 | 0.04 | (0.01, 0.06)b | 0.05 | (−0.11, 0.21) | −0.02 | (−0.06, 0.01) | −0.01 | (−0.15, 0.13) |
| Men (n=5432) | ||||||||
| Marginal RD | 95% CI | Marginal RD | 95% CI | Marginal RD | 95% CI | Marginal RD | 95% CI | |
| 2001 | 0.03 | (−0.01, 0.06) | 0.10 | (−0.02, 0.22) | 0.00 | (−0.02, 0.03) | 0.02 | (−0.09, 0.14) |
| 2003 | −0.01 | (−0.04, 0.03) | −0.02 | (−0.15, 0.12) | 0.02 | (−0.01, 0.05) | 0.06 | (−0.08, 0.20) |
| 2012 | −0.01 | (−0.05, 0.03) | 0.01 | (−0.17, 0.20) | 0.01 | (−0.03, 0.05) | −0.01 | (−0.19, 0.16) |
Source: Mexican Health and Aging Study, 2001 – 2012.
Notes:
Measure of lower-body functional limitations was created from items regarding perceived difficulty with 7 different tasks (e.g. sitting, walking one or several blocks, climbing one or several flights of stairs, stooping, or kneeling). An item about perceived difficulty running a mile was excluded from this version of the outcome
e-value, or minimum strength of association that an unmeasured confounder would have to have between treatment and outcome (on the risk ratio scale) necessary to reduce observed risk differences to the null (assuming that those associations are of identical size) e-value = 1.27 (lower bound of 95% CI: 1.12)
e-value = 1.33 (lower bound of 95% CI: 1.00)
e-value = 1.58 (lower bound of 95% CI: 1.12)
e-value = 1.31 (lower bound of 95% CI: 1.00).
The e-value for the association between having an adult child in the US and need for assistance with ≥ 1 activity of daily living suggests that the observed association could be explained away by an unmeasured confounder that was associated with both the exposure and the outcome by a risk ratio of 1.58, above and beyond the set of measured confounders; the lower bound of the 95% confidence interval of the observed association could be moved to include the null by an unmeasured confounder that was associated with both exposure and outcome by a risk ratio of 1.12 (i.e. the lower bound of the 95% CI of the e-value). E-values for other associations that do not cross the null are reported in results Tables 2 and 3.
Table 3.
Marginal difference in the expected prevalence of reporting at least one unmet need with activities or independent activities of daily living for Mexican adults ≥ 50 years old with at least one adult migrant child versus no migrant children
| Women (n=1208) | ||
| Marginal RD | 95% CI | |
| 2001 | 0.04 | (−0.02, 0.10) |
| 2003 | 0.13 | (0.04, 0.21)a |
| 2012 | 0.07 | (−0.02, 0.15) |
| Men (n=1225) | ||
| Marginal RD | 95% CI | |
| 2001 | 0.00 | (−0.05, 0.06) |
| 2003 | −0.02 | (−0.11, 0.07) |
| 2012 | 0.08 | (0.00, 0.16)b |
Source: Mexican Health and Aging Study, 2001 – 2012. Note: Analyses restricted to respondents who reported > 1 ADL/IADL in a given wave
Notes:
e-value, or minimum strength of association that an unmeasured confounder would have to have between treatment and outcome (on the risk ratio scale) necessary to reduce observed risk differences to the null (assuming that those associations are of identical size) = 1.68 (lower bound of 95% CI: 1.33)
e-value: 1.56 (lower bound: 1.42).
In contrast, women with an adult child in the US across the entire study period were found to have a higher expected prevalence of ≥ 1 lower-body functional limitation at 11-year follow-up compared to their counterparts with no adult child in the US at any study wave (RD: 0.04, 95% CI: 0.01, 0.06). There were no associations between having an adult child in the US and any measures of physical functioning among men. Findings were generally similar when using an eight-item measure of lower-body functional limitations that included the indicator of difficulty running a mile (Appendix Table C).
For women with at least one need for assistance for care, having an adult child in the US was associated with greater estimated prevalence of reporting at least one unmet need for assistance at two-year follow-up (RD: 0.13, 95% CI: 0.04, 0.21) and 11-year follow-up (RD: 0.07, 95% CI: −0.02, 0.15). For men with any need for assistance in the final survey wave, having an adult child in the US at all three study waves was associated with a greater estimated prevalence of unmet needs (RD: 0.08, 95% CI: 0.00, 0.16) compared to not having an adult child in the US at all three time points (Table 3, Figure 2).
Figure 2.
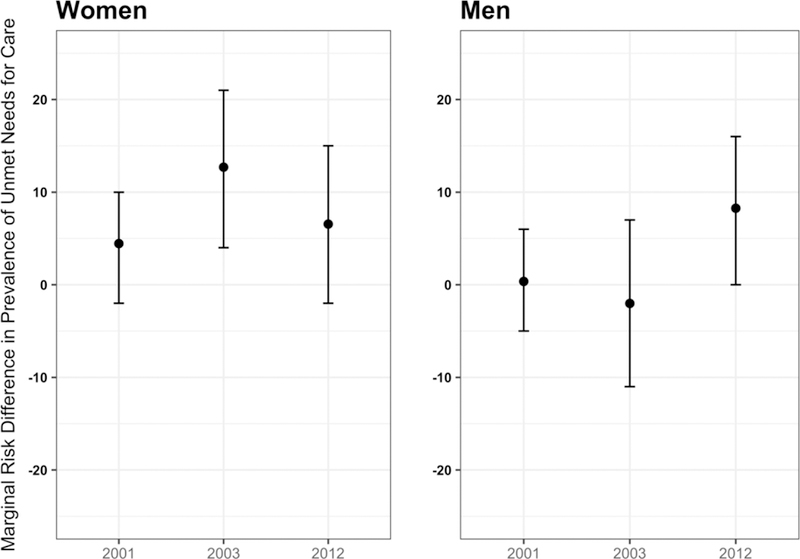
Marginal risk differences in the expected prevalence of ≥ 1 unmet need with an activity or independent activity of daily living at each time point (t) given counterfactual outcomes of having at least one adult child in the US versus having no children in the US at t plus all prior ts, restricted to respondents with need for assistance with at least one activity or independent activity of daily living (1200 women and 1225 men at baseline).
Sensitivity analyses assessing bias due to the exclusion of proxy respondents from the baseline sample indicated similar observed and selection-bias adjusted risk ratios for the relationship between having an adult child in the US and ≥ 1 need for assistance with basic activities of daily living at baseline (eAppendix Table 4).
DISCUSSION
The present study used a doubly robust estimation approach to examine longitudinal associations between having an adult child in the US and physical functioning and unmet caregiving needs among middle-age and older adults in Mexico. This study extends prior work on adult child migration status and mental health, heart disease, and cognitive function among older Mexican adults, 6,8,9 to examine physical functioning outcomes. In addition, while other studies have examined associations between adult child migration and financial and time contributions to older adults,25 this is the first study, to our knowledge, that has quantified the impact on unmet caregiving needs. Finally, this research extends the primarily cross-sectional or short-term follow-up studies used in prior research to a large cohort followed over an 11-year period.
We found select modest associations between having an adult child in the US and physical functioning for women, although the direction of these associations was inconsistent by outcome (i.e. lower body functional limitations, needs for assistance with activities of daily living) and study wave. In particular, there were positive associations between having an adult child in the US and both measures of physical functioning at the two-year follow-up for women, which is consistent with two studies in other settings reporting that having an adult child migrant and was associated with better physical functioning among older adults who remain.4,5 These protective findings have been explained by economic transfers commonly made from migrant children to parents who remain in place,5,14,25 which may allow older adults to access treatment for underlying medical conditions10,56 and to reduce physically demanding work (e.g. in agriculture or domestic occupations),5 possibly contributing to improvements in perceived and/or actual physical functioning. For example, a study5 evaluating the impact of adult child out-migration on older adults in Moldova found that those with adult migrant children had higher incomes, spent fewer hours per work laboring in the family business or farm, and spent more time sleeping and engaged in leisure activities compared to those with no migrant children.
On the other hand, we observed adverse associations between having an adult child in the US across the entire study and lower-body functional limitations at the 11-year follow-up wave for women. It may be that the long-term – but not short-term -- absence of adult children had adverse consequences for women’s physical functioning as they aged into older adulthood. On the other hand, these findings could be driven by unmeasured conditions or events that may have emerged during the 9-year gap between the second and third follow-up waves that may have also influenced exposure, outcome, and/or attrition, and may contribute to biased estimates of adverse long-run associations between adult child migration status and lower-body functional limitations.
We also found entirely null associations between having an adult child in the US and physical functioning for men. One possible explanation is that men in the MHAS had, on average, higher incomes and wealth compared to women – and over two-thirds reported at baseline that they still worked. Migrant remittances may have therefore had less of an impact on poverty alleviation, access to health care, or other factors that might have contributed to improved physical health for men with versus without migrant children. Moreover, given that men were more likely to continue to work, any financial resources gained from migrant children may not have effectively freed up time for health-promoting activities (e.g. sleep, social activities).
Finally, having an adult child in the US was associated with a substantially higher prevalence of unmet needs for assistance with basic or instrumental activities of daily living for the subsample of respondents reporting at least one need for assistance. These findings may be somewhat surprising, given that that the majority of respondents reported having at least one adult child living in the same household. Respondents otherwise had what appeared to be relatively robust family and community networks, with large average family sizes and high rates of marital status. On the other hand, these summary statistics may not reflect substantial heterogeneity in the location of these family members as well as their availability to provide care to older adult parents. The out-migration of one or more adult children may have shifted the entire distribution of labor within the household, leaving fewer family members to cover care needs for older adults as well as any young children that needed assistance. Moreover, co-residing spouses may not universally be able to provide care if they are also managing their own physical or cognitive impairments. These findings regarding unmet needs correspond with previous work25 using the baseline and two-year follow-up waves of the MHAS, which found that among older Mexican adults with any need for assistance, those with non-migrant children reported receiving 20.6 hours of care per week compared with 12.4 hours per week of care for those who had migrant children.
We note some discordance in associations observed by study wave for men. The relatively large association between having an adult child and unmet needs for care among men at the 11-year follow-up wave was not observed in the 2-year follow-up wave. This discrepancy could suggest that only the long-term, cumulative presence of an adult child in the US was associated with unmet needs for men. It could also have been that the influence of having an adult child in the US was only meaningfully associated with unmet needs for men in the cohort as they reached older age.
The results related to unmet needs could have substantial policy implications. In combination with prior findings of reduced overall time contributions to elderly parents of migrant children,25 these findings suggest that older adults should not be expected to unilaterally benefit from the out-migration of adult children – and family members who remain in place may not be able or available to cover the full range of care needs for older adults in need of assistance. This finding is particularly concerning given the lack of options for formal long-term assistance for older adults in Mexico,57 as well as declines in family size58 – possible contributing to greater vulnerability among older adults with needs for care who experience the out-migration of an adult child.
Results should be viewed in light of additional limitations. For one, the estimated strength of the relationship between possible unmeasured confounders and both exposure and outcomes that could reduce observed non-zero risk differences to the null was relatively small. We remain concerned about potential bias due to unmeasured confounding. Potential unmeasured confounders including family or community-level factors (e.g. average health of all family members, community-level socio-economic conditions) may have influenced both migration decisions and health at the individual level. Second, the third follow-up wave took place 9 years after the second follow-up wave. During such a long time between follow-up, some respondents may have had children who migrated to and returned from the US, and we would miss the potential influence of this US migration exposure. On the other hand, the percentage of respondents who reported having at least one adult child in the US remained relatively stable across each of the study waves, tempering concern about dramatic unmeasured shifts in adult child migration status within the study period.
Third, the sample size for analyses of unmet needs are quite small, precluding us from examining further nuance in the observed associations. For example, we examined differences in the relationship between having an adult child in the US and physical functioning by the gender of the migrant child, finding largely similar patterns as those reported for primary analyses (eAppendix Tables 5 and 6). The analytic sample was too small to pursue these gender-stratified analyses for the outcome of unmet needs for care. Finally, we acknowledge that future work should consider examining change or trajectories of physical functioning outcomes to further strengthen evidence on causality.
Despite these limitations, the results make important substantive contributions by examining longitudinal associations between having an adult child migrant and critical outcomes for population aging. The analyses also offer methodologic advantages over prior studies by using a doubly robust estimation approach to examining longitudinal relationships, appropriately addressing sample attrition, and accounting for time-varying covariates -- including time-varying covariates affected by prior exposure.
While out-migration to the US has fallen dramatically,59 Mexico continues to experience a rapidly aging population in a context in which there is no legal right to formal long-term care services.2 Our most important finding suggests that having an adult child migrant was associated with a higher prevalence of unmet caregiving needs for older Mexican adults who had needs for care. Older adults with care needs who have migrant family members might be targeted by efforts to provide formal long-term services and supports in Mexico. Future research might extend this work to understand whether these findings generalize to countries with distinct demographic trends and old-age policy environments.
Supplementary Material
Acknowledgments:
The Mexican Health and Aging Study (MHAS) is funded by the National Institutes of Health/National Institute on Aging (R01AG018016, R Wong, PI) and the National Institute of Statistics and Geography (INEGI) in Mexico. JMT is supported by the National Institutes of Health/National Institute on Aging (K01AG056602, J Torres, PI). KER is supported by the National Institutes of Health/National Institute on Drug Abuse (K99DA042127, K Rudolph, PI). OS is supported by the National Institutes of Health/National Institute of Allergy and Infectious Diseases (R01AI074345–07). MMG is supported by the National Institutes of Health and Aging (RF1AG05548601, MM Glymour and A Zeki Al Hazzouri, Multi-PI). LCW is supported by the National Institutes of Health/National Institute on Aging (K24AG041180).
Footnotes
No conflicts of interest to declare.
The data are publicly available for download at mhasweb.org; sample code for longitudinal Targeted Maximum Likelihood Estimation and sensitivity analysis are provided in the supplemental files. Further code (e.g. to set up all of the variables, for multiple imputation procedures) is available upon request.
References
- 1.United Nations Department of Economic and Social Affairs, Population Division. World Population Ageing 2015 New York, NY: United Nations, 2015. (ST/ESA/SER.A/390). [Google Scholar]
- 2.Scheil-Adlung X Long-term Care Protection for Older Persons: A Review of Coverage Deficits in 46 Countries Geneva, Switzerland: International Labor Organization, 2015. (ESS Paper Series (SECSOC) - ESS 50). [Google Scholar]
- 3.United Nations Department of Economic and Social Affairs, Population Division. International Migration Report 2017: Highlights New York, NY: United Nations Population Division, 2017. (ST/ESA/SER.A/404). [Google Scholar]
- 4.Kuhn R, Everett B, Silvey R. The effects of children’s migration on elderly kin’s health: a counterfactual approach. Demography 2011;48:183–209. [DOI] [PubMed] [Google Scholar]
- 5.Böhme MH, Persian R, Stöhr T. Alone but better off? adult child migration and health of elderly parents in Moldova. J Health Econ 2015;39:211–27. [DOI] [PubMed] [Google Scholar]
- 6.Antman F Adult child migration and the health of elderly parents left behind in Mexico. Am Econ Rev 2010;100(2):205–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abas M, Tangchonlatip K, Punpuing S, Jirapramukpitak T, Darawuttimaprakorn N, Prince M, Flach C. Migration of children and impact on depression in older parents in rural Thailand, southeast Asia. JAMA Psychiatry 2013;70:226–34. [DOI] [PubMed] [Google Scholar]
- 8.Antman FM. How does international migration affect the health of elderly parents left behind? evidence from Mexico Boulder, CO: Department of Economics, University of Colorado at Boulder, 2016. http://spot.colorado.edu/~antmanf/AntmanMigration&ElderlyHealth.pdf. Accessed April 25, 2018. [Google Scholar]
- 9.Downer B, González-González C, Goldman N, Pebley AR, Wong R. The effect of adult children living in the United States on the likelihood of cognitive impairment for older parents living in Mexico. Ethn Health 2018; 23(1): 57–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adhikari R, Jampaklay A, Chamratrithirong A. Impact of children’s migration on health and health care-seeking behavior of elderly left behind. BMC Public Health 2011;11:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamada K, Teerawichitchainan B. Living arrangements and psychological well-being of the older adults after the economic transition in Vietnam. J Gerontol B Psychol Sci Soc Sci 2015;70(6):957–68. [DOI] [PubMed] [Google Scholar]
- 12.Song Q. Aging, and separation from children: The health implications of adult migration for elderly parents in rural China. Demographic Research 2017;37:1761–1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.migrant-sending areas. Soc Sci Med 2012;74:135–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Torres JM, Rudolph KE, Sofrygin O, Glymour MM, Wong R. Longitudinal associations between having an adult child migrant and depressive symptoms among older adults in the Mexican Health and Aging Study. International Journal of Epidemiology 2018;ePub ahead of print. [DOI] [PMC free article] [PubMed]
- 15.Lu Y, Hu P, Treiman DJ. Migration and depressive symptoms in migrant-sending areas: findings from the survey of internal migration and health in China. Int J Public Health 2012;57:691–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ertel KA, Glymour MM, Berkman LF. Effects of social integration on preserving memory function in a nationally representative US elderly population. Am J Public Health 2008;98:1215–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav 2011;52:145–61. [DOI] [PubMed] [Google Scholar]
- 18.Yang YC, Boen C, Gerken K, Li T, Schorpp K, Harris KM. Social relationships and physiological determinants of longevity across the human life span. Proc Natl Acad Sci U S A 2016;113:578–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuiper JS, Zuidersma M, Zuidema SU, Burgerhof JG, Stolk RP, Oude Voshaar RC, Smidt N. Social relationships and cognitive decline: a systematic review and meta-analysis of longitudinal cohort studies. Int J Epidemiol 2016. 45:1169–1206. [DOI] [PubMed] [Google Scholar]
- 20.Bishop NJ, Eggum-Wilkens ND, Haas SA, et al. Estimating the co-development of cognitive decline and physical mobility limitations in older U.S. adults. Demography 2016;53:337–64. [DOI] [PubMed] [Google Scholar]
- 21.Wong E, Backholer K, Gearon E, Harding J, Freak-Poli R, Stevenson C, Peeters A. Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2013;1(2):106–14. [DOI] [PubMed] [Google Scholar]
- 22.Sousa RM, Ferri CP, Acosta D, Albanese E, Guerra M, Huang Y, Jacob KS, Jotheeswaran AT, Rodriguez JJ, Pichardo GR, Rodriguez MC, Salas A, Sosa AL, Williams J, Zuniga T, Prince M. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet 2009;374(9704):1821–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boyle PA, Buchman AS, Wilson RS, et al. Physical activity is associated with incident disability in community-based older persons. J Am Geriatr Soc 2007;55:195–201. [DOI] [PubMed] [Google Scholar]
- 24.Rist PM, Capistrant BD, Wu Q, et al. Dementia and dependence: do modifiable risk factors delay disability? Neurology 2014;82:1543–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Antman FM. Elderly care and intrafamily resource allocation when children migrate. Journal of Human Resources 2012;47(2):331–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Antman F Who cares for the elderly? Intrafamily resource allocation and migration in Mexico Vol. SIEPR Discussion Paper No. 06–31. Stanford, CA: Stanford Institute for Economic Policy Research, 2007. [Google Scholar]
- 27.Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology 2000;11:550–60. [DOI] [PubMed] [Google Scholar]
- 28.Petersen M, Schwab J, Gruber S, et al. Targeted maximum likelihood estimation for dynamic and static longitudinal marginal structural working models. J Causal Inference 2014;2:147–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schuler MS, Rose S. Targeted maximum likelihood estimation for causal inference in observational studies. Am J Epidemiol 2017;185:65–73. [DOI] [PubMed] [Google Scholar]
- 30.Sofrygin O, Zhu Z, Schmittdiel JA, et al. Targeted learning with daily EHR data 2017. https://arxiv.org/abs/1705.09874; Accessed April 24, 2018. [DOI] [PubMed]
- 31.Wong R, Michaels-Obregon A, Palloni A. Cohort profile: The Mexican Health and Aging Study (MHAS). Int J Epidemiol 2017;46:e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Massey DS, Espinosa KE. What’s driving Mexico-U.S. migration? a theoretical, empirical, and policy Analysis. Am J Sociol 1997;102:939–999. [Google Scholar]
- 33.McKenzie D, Rapoport H. Self-selection patterns in Mexico-U.S. migration: the role of migration networks. Rev Econ Stat 2010;92:811–821. [Google Scholar]
- 34.Kaestner R, Malamud O. Self-selection and international migration: new evidence from Mexico. Rev Econ Stat 2014;96:78–91. [Google Scholar]
- 35.Garip F Repeat migration and remittances as mechanisms for wealth inequality in 119 communities from the Mexican Migration Project data. Demography 2012;49:1335–1360. [DOI] [PubMed] [Google Scholar]
- 36.Massey DS, Alarcón R, Durand J, González H. Return to Aztlán: The Social Process of International Migration from Western Mexico Berkeley, CA: UC Press, 1987. [Google Scholar]
- 37.Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States. N Engl J Med 2006;355:695–703. [DOI] [PubMed] [Google Scholar]
- 38.Schoeni RF, Freedman VA, Martin LG. Why is late-life disability declining? Milbank Q 2008;86:47–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Banks LM, Kuper H, Polack S. Poverty and disability in low- and middle-income countries: A systematic review. PLoS One 2017;12(12):e0189996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Henning-Smith C, Shippee T, Capistrant B. Later-life disability in environmental context: why living arrangements matter [published online ahead of print April 3, 2017]. Gerontologist (doi: 10.1093/geront/gnx019). [DOI] [PMC free article] [PubMed]
- 41.Gruber S, van der Laan MJ. Targeted Maximum Likelihood Estimation: A Gentle Introduction. U.C. Berkeley Division of Biostatistics Working Paper Series 2009; Working Paper 252.
- 42.van der Laan MJ, Gruber S. Targeted minimum loss based estimation of causal effects of multiple time point interventions. Int J Biostat 2012;8(1):1–41 [DOI] [PubMed] [Google Scholar]
- 43.Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol 2008;168(6):656–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Polley E, LeDell E, Kennedy C, Lendle S, van der Laan M. SuperLearner: superlearner prediction 2.0–22 ed, 2017;R package. [Google Scholar]
- 45.Tibshirani R Regression shrinkage and selection via the Lasso. J Royal Stat Soc B 1996;58:267–88. [Google Scholar]
- 46.Friedman J Greedy boosting approximation: a gradient boosting machine. Annals of Statistics 2001;29:1189–1232. [Google Scholar]
- 47.Chen T, Guestrin C. XGBoost: A scalable tree boosting system Presented at Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, 2016. [Google Scholar]
- 48.Sofrygin O, van der Laan MJ, Neugebauer. stremr: Streamlined Estimation for Static, Dynamic and Stochastic Treatment Regimes in Longitudinal Data R package version 3.3.2., 2017.
- 49.Coyle J, Hejazi N, Sofrygin O, Malenica I. sl3: Pipelines for Machine Learning and Super Learning R package version 1.0.0., 2018.
- 50.R Development Core Team. R: A language and environment for statistical computing Vienna: Austria, 2017. [Google Scholar]
- 51.Honaker J, King G, Blackwell M. Amelia II: A Program for Missing Data. R package: version 1.7.3, 2014.
- 52.Rubin DB. Multiple Imputation for Nonresponse in Surveys New York, NY: Wiley, 1987. [Google Scholar]
- 53.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the e-value. Ann Intern Med 2017;167:268–274. [DOI] [PubMed] [Google Scholar]
- 54.Mathur MB, Ding P, Riddell CA, VanderWeele TJ. Website and R package for computing E-values. Epidemiology 2018; 29(5): e45–e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Haine D Basic Sensitivity Analysis of Epidemiological Results R package version 0.9.2. 2017.
- 56.Salinas JJ. Tapping healthcare resource by older Mexicans with diabetes: how migration to the United States facilitates access. J Cross Cult Gerontol 2008;23(3):301–12. [DOI] [PubMed] [Google Scholar]
- 57.Colombo F, Llena-Nozal A, Mercier J, Tjadens F. Help Wanted? Providing and Paying for Long-Term Care OECD Health Policy Studies. Paris: OECD Publishing, 2011. [Google Scholar]
- 58.United Nations Department of Economic and Social Affairs, Population Division. World Fertility Patterns 2015 - Data Booklet New York, NY: United Nations, 2015. [Google Scholar]
- 59.Passel JS, Cohn DV, Gonzalez-Barrera A. Net Migration from Mexico Falls to Zero—and Perhaps Less Washington, D. C.: Pew Research Center, 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


