Abstract
Background
It is unknown whether social anxiety disorder (SAD) has a unique association with alcohol use disorder (AUD) over and beyond that of other anxiety disorders, how the associations develop over time, and whether the associations are likely to be causal.
Methods
Diagnoses of AUD, SAD, generalized anxiety disorder, panic disorder, agoraphobia, and specific phobias were assessed twice using the Composite International Diagnostic Interview among 2,801 adult Norwegian twins. The data were analysed using logistic regression analyses and multivariate biometric structural equation modelling.
Results
SAD had the strongest association with AUD, and SAD predicted AUD over and above the effect of other anxiety disorders. In addition, SAD was prospectively associated with AUD, whereas other anxiety disorders were not. AUD was associated with a slightly elevated risk of later anxiety disorders other than SAD. Biometric modelling favoured a model where SAD influenced AUD compared to models where the relationship was reversed or due to correlated risk factors. Positive associations between AUD and other anxiety disorders were fully explained by shared genetic risk factors.
Conclusions
Unlike other anxiety disorders, SAD plausibly has a direct effect on AUD. Interventions aimed at prevention or treatment of SAD may have an additional beneficial effect of preventing AUD, whereas interventions aimed at other anxiety disorders are unlikely to have similar sequential effect on AUD.
Keywords: Anxiety disorders, Social anxiety disorder, Social phobia, Alcohol Use Disorder, Specific phobia, Agoraphobia, Twin Studies
Introduction
Alcohol use disorders (AUD) frequently occur together with social anxiety disorder (SAD) (Buckner & Schmidt, 2009; Marmorstein, 2012; Schneier et al., 2010). Up to half of individuals with SAD have a history of AUD (Grant et al., 2005), and approximately one in four with AUD have SAD (Terra et al., 2006). This combination is particularly debilitating (Schneier et al., 2010), but it is not clear how the two disorders are associated. It is possible that SAD influences AUD. In the short run, alcohol induces euphoria and reduces anxiety (Gilman, Ramchandani, Davis, Bjork, & Hommer, 2008). Since alcohol is often present at social gatherings, drinking can be used as a strategy to cope with social anxiety (Carrigan & Randall, 2003; Prescott, Cross, Kuhn, Horn, & Kendler, 2004). This ‘self-medication’ can put individuals with SAD at risk of AUD. Indeed, SAD and symptoms of social anxiety prospectively predicts AUD and substance use disorders (Buckner & Schmidt, 2009; Buckner et al., 2008; Buckner & Turner, 2009; Dahne, Banducci, Kurdziel, & MacPherson, 2014; Wolitzky-Taylor, Bobova, Zinbarg, Mineka, & Craske, 2012). The observations that SAD has a young age of onset (Boschloo et al., 2011; Lecrubier et al., 2000; Marmorstein, 2012) and occurs before AUD in 80% of comorbid cases (Buckner et al., 2008; Schneier et al., 2010) also indicate that SAD could influence AUD.
The above-mentioned studies provide less evidence for a direct effect from AUD to SAD (Buckner & Turner, 2009; Dahne et al., 2014; Wolitzky-Taylor et al., 2012). Nevertheless, from a psychopharmacological perspective it is likely that alcohol use produces anxiety, at least during withdrawal, and a few studies indicate that AUD causes anxiety (Becker, 2012; Fergusson, Boden, & Horwood, 2011). This could be true also for SAD. On the other hand, a Mendelian randomization study found alcohol use not to cause symptoms of anxiety (Chao, Li, & McGue, 2017).
Despite the temporal relationship, the association may reflect shared risk factors that affect both disorders rather than a causal relationship (confounding) (Kushner, Abrams, & Borchardt, 2000; Neale & Kendler, 1995). For instance personality, socioeconomic status, or a general tendency to psychopathology could influence SAD at a young age and later AUD. Shared genetic risk factors for AUD and anxiety disorders have been found in twin (Lahey, Krueger, Rathouz, Waldman, & Zald, 2017; Nelson et al., 2000; Tambs, Harris, & Magnus, 1997) and molecular genetic studies (Cerda, Sagdeo, Johnson, & Galea, 2010; Hodgson et al., 2016).
Finally, SAD is part of the internalizing spectrum and unlikely to be entirely distinct from other anxiety disorders (Lahey et al., 2017). AUD is also associated with other anxiety disorders (Grant et al., 2004). It could therefore be that the association between SAD and AUD reflects a broader association between AUD and anxiety disorders, rather than SAD specifically. One study has supported this hypothesis (Kushner et al., 2012). On the other hand, alcohol is likely to be particularly ‘useful’ to individuals with SAD (Bulley, Miloyan, Brilot, Gullo, & Suddendorf, 2016), and in studies that analysed all anxiety disorders together, only SAD predicted AUD in adjusted analyses (Buckner & Schmidt, 2009; Buckner et al., 2008; Buckner & Turner, 2009).
Thus, we have four possible explanations of the association: i) direct effects from SAD to AUD, ii) direct effects from AUD to SAD, iii) shared genetic and/or environmental risk factors, and iv) a general relationship between anxiety disorders and AUD. A lack of studies with diagnostic assessment of anxiety disorders and AUD has left this question unanswered. The explanatory models have different practical implications: In treatment and prevention, higher gains will be achieved by intervening on the disorder that influences the risk of developing the other disorder. In the present study, we utilize a population-based twin study with repeated diagnostic assessment of AUD, SAD and other anxiety disorders in order distinguish between the possible explanations of the association between SAD and AUD. We aim to i) test if SAD has a unique association with AUD over and beyond that of other anxiety disorders, ii) describe the longitudinal relationship between these disorders, and iii) determine whether the associations between anxiety disorders and AUD are in line with direct effects between the disorders.
Methods
Participants
The data for the current study originated from the Norwegian Institute of Public Health Twin Panel (Nilsen et al., 2013). Twins were identified through the national Medical Birth Registry, established January 1, 1967. Between 1999 and 2004 (time 1; T1), psychiatric disorders were assessed at interview in 2,801 twins born between 1967 and 1979 (44.4% response rate). Between 2010 and 2011 (time 2; T2), a second wave of interviews were conducted among 2,284 of the respondents at T1 (82.8% of the eligible; 43 had died or withdrawn consent or had unknown address). The mean age was 28.1 years (SD=3.9; range 19–35) at T1, and 37.8 years (SD=3.8; range 31–44) at T2. Combining the two waves, there were 5,085 observations with a mean age of 32.5 years (SD=3.8; range=19–44). At T1, there were 220 monozygotic (MZ) male pairs, 118 dizygotic (DZ) male pairs, 449 MZ female pairs, 263 DZ female pairs, 341 DZ opposite sex pairs, and 19 single twins. At T2, there were 154 MZ male pairs, 76 DZ male pairs, 358 MZ female pairs, 180 DZ female pairs, 219 DZ opposite sex pairs, and 310 single twins. The study was approved by The Regional Committees for Medical and Health Research Ethics and all participants provided written informed consent.
Measures
At T1 and T2, DSM-IV diagnoses of AUD, SAD, generalized anxiety disorder (GAD), panic disorder, agoraphobia, and specific phobias were assessed using the Composite International Diagnostic Interview (CIDI) (Wittchen & Pfister, 1997) in Norwegian translation. The interviewers were mainly senior clinical psychology graduate students, experienced psychiatric nurses, and experienced clinical psychologists. Most interviews at T1 were conducted face-to-face, whereas 231 (8.3%) were done by telephone. All interviews at T2 were conducted by telephone. Different interviewers assessed each twin in a pair. Ages of onset of the disorders were reported. As a compromise between recency and statistical power, we used disorders that had occurred during the last five years. In addition, lifetime diagnoses were available. The CIDI interview assigns subthreshold diagnoses in cases where individuals are one criteria short of a DSM-diagnosis. In order to increase statistical power, we included the subthreshold disorders as an intermediate category between ‘no disorder’ and ‘full disorder’ for all the anxiety disorders with the exception of specific phobias. AUD was analysed as a dichotomous variable because inclusion of subthreshold AUD led to deviation from multivariate normality in the association with SAD (χ2 = 32.72, df = 3, p < 0.001).
Statistical analyses
We first examined the associations between each anxiety disorder and AUD in logistic regression analyses adjusted for age, sex, and time, and then entered all anxiety disorders in the model simultaneously. We compared this to a model where AUD was regressed on the total load of anxiety disorders, rather than specific diagnoses, and tested whether any of the anxiety disorders predicted AUD over and above the total load of anxiety disorder. This total load was computed as an item response theory (IRT) factor score in a graded response model. We refer to this score as AnxIRT. In order to maximize power, we collapsed T1 and T2 in these analyses, so that each interview constituted an observation. The analyses were run as generalized estimating equations (GEE) to adjust for statistical dependence between siblings and repeated measures. Model fit in GEE models were compared using Quasi-likelihood Information Criterion (QIC), which is analogous to Akaike’s Information Criterion (AIC) (Pan, 2001). Lower values of QIC indicate better fit. We then described the longitudinal relationship between the SAD, AnxIRT, and AUD at the two time points with a structural equation model (SEM) for ordinal data (liability-threshold model).
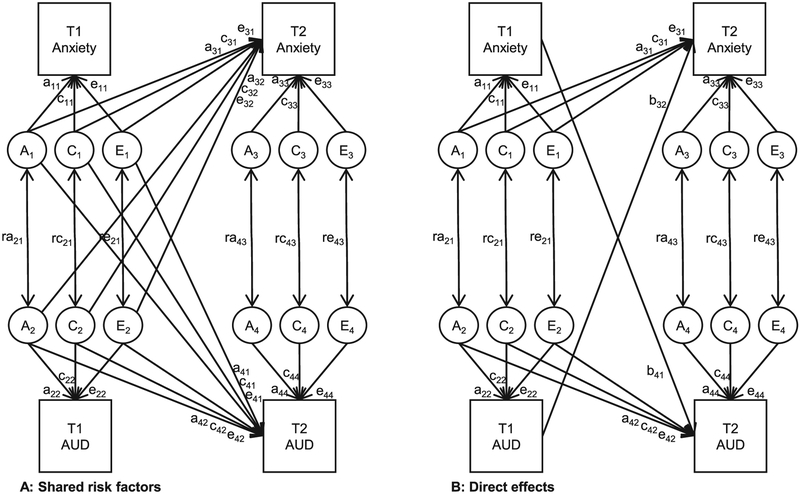
Monozygotic (MZ) twins share all their genes whereas dizygotic (DZ) twins share on average half of the genes that vary in the population. This difference can be used to divide variation in traits and associations between traits into additive genetic (A), shared environmental (C), and individual-specific environmental (E) factors (Neale & Maes, 2004). We investigated SAD and AnxIRT in separate models that both included AUD. We used a cross-lagged biometric model (left panel of Figure 1). This is a combination of the Cholesky decomposition and the correlated factors model (Torvik et al., 2017). Genetic and environmental influences on a disorder can have a directional effects on observations later in time, whereas non-directional correlations are estimated between influences on disorders observed at the same time. We tested whether there were significant effects of A and C factors by fixing their path coefficients to zero.
Figure 1.
The full model (A) for longitudinal associations between alcohol use disorder (AUD) and anxiety disorders. Genetic and environmental influences on a disorder can influence later observations, but not earlier. Influences on disorders measured at the same point in time are allowed to correlate. In the more parsimonious model B, longitudinal associations across the disorders are modelled as direct effects. If shared genetic risk factors account for the longitudinal relationship, model A would fit best. If longitudinal associations result from causal effect between the disorders, model B would fit best. If the baseline (T1) associations fully explain the future (T2) associations, b32 and b41 would be estimated at zero. We separately test the associations from anxiety to AUD (a41, c41, and e41 vs. b41) and from AUD to anxiety (a32, c32, and e32 vs. b32).
Causal associations at the phenotypic level imply direct effects between observed variables as opposed to associations between subsets of their latent risk factors. This implies a “common pathway” between phenotypes rather than independent genetic and environmental pathways (Turkheimer, Pettersson, & Horn, 2014). We can test this by modelling a direct path between the phenotypes. We thereby assume that genetic as well as environmental effects are passed on from one phenotype to the next. This resembles Mendelian randomization, but requires no explicit gene or instrument variable (Briley, Livengood, Derringer, & Kandler, 2018; Rosenstrom et al., 2019). As with discordant twin analyses, environmental associations strengthen causal hypothesis in realistic scenarios. However, unlike with discordant twin analyses, we do not assume that genetic associations represent confounding. With phenotypic causality, all the biometric influences on the exposure should be correlated with the outcome. For example, if SAD is a product of both genetic and environmental factors, and SAD phenotypically affects AUD, one would expect to find both genetic and environmental correlations between SAD and AUD. We tested the presence of direct influences by replacing separate genetic and environmental associations (e.g. a41, c41, e41) with direct paths (e.g. b41), as shown in the right panel of Figure 1. This model is simpler and fits well when direct effects explain the relationship between variables. It is important to note that a better fit of the more complex model does not preclude all types of causal effects, only phenotypic causation. We tested each of the longitudinal relationships separately.
There may be direct influences between the disorders that act on a short time-scale and that are invisible in a follow-up years later. Therefore, we tested whether we could find indications of direct influences between the disorders in cross-sectional data, using lifetime reports of the disorders at wave 1 and wave 2. The two lifetime assessments were combined in a measurement model that provides estimates of association free from measurement error. The direction of causation between two phenotypes can be approached with cross-sectional twin data when their modes of inheritance differ (Heath et al., 1993). Because effects within an individual do not affect the co-twin, different cross-twin cross-trait covariances will be expected depending on the causal direction. We compared a model with shared risk factors to models with unidirectional and reciprocal effects.
All SEM models were fitted using Full Information Maximum Likelihood (FIML) as estimation procedure to raw data in OpenMx 2.7.12 (Neale et al., 2016) within R 3.4.1. The raw data method utilizes all data, from both complete and incomplete pairs. We used the AIC (Akaike, 1987) as indices of parsimony. Models with low AIC values are preferred.
Results
Descriptive results
The prevalences of AUD and anxiety disorders the last five years are presented in Table 1. AUD was more common among men than among women, whereas all five anxiety disorders were more common among women. AUD was considerably more common among individuals with SAD. Combining T1 and T2, 15% of individuals with SAD had AUD, compared to only 6% among those with no SAD. Among men and women with SAD, 26% and 13%, respectively, had AUD. The polychoric correlation between SAD and AUD was 0.35 (95% CI 0.25, 0.46) among men and 0.34 (95% CI 0.25, 0.44) among women. The mean age of onset was reported to be 14.2 years (SD = 7.3) for SAD and 19.4 years (SD = 4.5) for AUD. Among individuals with both lifetime SAD and lifetime AUD, 33 out of 41 (81%) reported a lower age of onset for SAD than for AUD.
Table 1.
Prevalences of alcohol use disorder and anxiety disorders (including subthreshold disorders) occurring the last five years by time of measurement and sex.
| Time 1 | Time 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | |||||
| n | % | n | % | n | % | n | % | |
| Alcohol use disorder | 133 | 13.1 | 83 | 4.7 | 68 | 8.5 | 38 | 2.6 |
| Social anxiety disorder, subthreshold | 108 | 10.6 | 234 | 13.2 | 52 | 6.5 | 135 | 9.1 |
| Social anxiety disorder | 18 | 1.8 | 76 | 4.3 | 13 | 1.6 | 75 | 5.1 |
| Generalized anxiety disorder, subth. | 72 | 7.1 | 205 | 11.6 | 43 | 5.4 | 130 | 8.8 |
| Generalized anxiety disorder | 8 | 0.8 | 40 | 2.3 | 6 | 0.7 | 46 | 3.1 |
| Panic disorder, subthreshold | 33 | 3.2 | 106 | 6.0 | 9 | 1.1 | 47 | 3.2 |
| Panic disorder | 16 | 1.6 | 61 | 3.4 | 6 | 0.7 | 36 | 2.4 |
| Agoraphobia, subthreshold | 19 | 1.9 | 94 | 5.3 | 8 | 1.0 | 53 | 3.6 |
| Agoraphobia | 17 | 1.7 | 94 | 5.3 | 9 | 1.1 | 50 | 3.4 |
| Specific phobias | 85 | 8.3 | 407 | 23.0 | 35 | 4.4 | 242 | 16.3 |
Note: The median p-value for difference between men and women is 0.0006. The highest p-value equals 0.05 (subthreshold social anxiety disorder at time 1).
Which anxiety disorders are related to alcohol use disorder?
The results from logistic regression analyses are shown in Table 2. Separate analyses of each anxiety disorder showed that each of them were associated with AUD, SAD most strongly (OR=4.68, 95% CI 2.87, 7.62). This pattern persisted when we entered all the anxiety disorders in the model together (model A). In model B, we only entered AnxIRT along with the demographic variables. This model had a higher QIC than model A, indicating that model A provides a better balance between complexity and fit to the data. We further tested whether any of the anxiety disorders could explain AUD over and above AnxIRT. When SAD was entered in the model along with AnxIRT (model C1), the QIC fell to a lower level than both model A and B. Both SAD and the factor score were clearly associated with AUD. No other disorders significantly predicted AUD when included along with the factor score: in each case, the QIC was higher than both model A and B, indicating worse fit. In the following, we therefore analyse SAD and a factor score of anxiety disorders other than SAD.
Table 2.
Results of logistic regression of alcohol use disorder (AUD) on anxiety disorders occurring last five years.
| Bivariate | Model A | Model B | Model C1 | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Social anxiety, sub. | 2.72 | (1.95, 3.79) | 2.31 | (1.63, 3.27) | 2.26 | (1.60, 3.19) | ||
| Social anxiety disorder | 4.68 | (2.87, 7.62) | 2.90 | (1.68, 5.03) | 3.00 | (1.77, 5.07) | ||
| Specific phobia | 1.85 | (1.33, 2.56) | 1.45 | (1.02, 2.05) | ||||
| Agoraphobia, sub. | 1.85 | (1.05, 3.26) | 1.16 | (0.63, 2.11) | ||||
| Agoraphobia | 3.24 | (2.01, 5.22) | 1.16 | (0.62, 2.16) | ||||
| Panic disorder, sub. | 1.23 | (0.69, 2.18) | 0.73 | (0.42, 1.26) | ||||
| Panic disorder | 3.14 | (1.80, 5.47) | 1.34 | (0.71, 2.55) | ||||
| GAD, sub. | 2.52 | (1.78, 3.57) | 1.86 | (1.28, 2.71) | ||||
| GAD | 3.88 | (1.93, 7.81) | 2.00 | (0.97, 4.10) | ||||
| Anxiety disorders IRT* | 1.57 | (1.41, 1.75) | 1.57 | (1.41, 1.75) | 1.25 | (1.12, 1.40) | ||
| Time | 1.55 | (1.05, 2.28) | 1.70 | (1.15, 2.50) | 1.55 | (1.06, 2.28) | 1.61 | (1.09, 2.37) |
| Age | 0.90 | (0.87, 0.93) | 0.90 | (0.87, 0.93) | 0.90 | (0.87, 0.93) | 0.90 | (0.87, 0.93) |
| Sex (female) | 0.30 | (0.23, 0.39) | 0.24 | (0.18, 0.31) | 0.24 | (0.18, 0.31) | 0.24 | (0.18, 0.31) |
| QIC | - | 2157.4 | 2155.3 | 2153.2 |
Notes: Bivariate results are adjusted for time, age, and sex; sub. = subthreshold disorder (lacking 1 symptom to satisfy criteria); GAD = Generalized anxiety disorder; IRT = Item response theory (latent trait model);
= variable is standardized (mean = 0, sd = 1). Data is analysed in long format, combining time 1 and time 2 data. Associations statistically significant at α=0.05 shown in bold.
Longitudinal associations
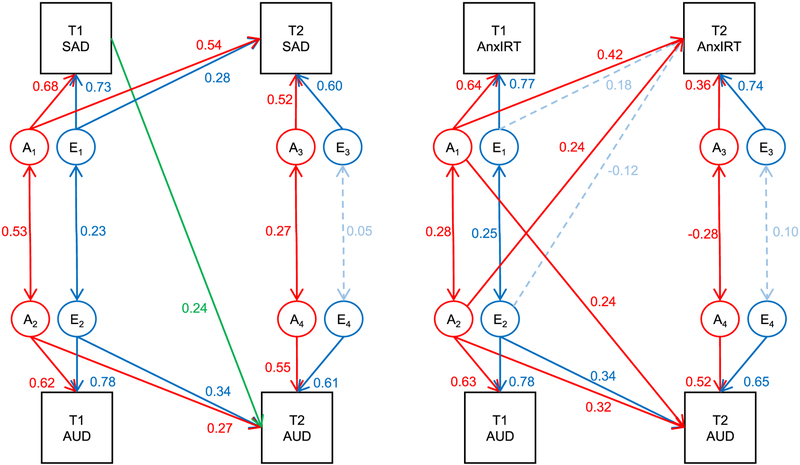
Figure 2 shows the phenotypic longitudinal associations between SAD, other anxiety disorders, and AUD. There were initial correlations between all the disorders at T1, and each disorder at T1 predicted the same disorder at T2. In addition, SAD at T1 was associated with AUD at T2. AUD at T1 had no association with SAD at T2 beyond the initial correlation. Other anxiety disorders at T1 did not predict AUD at T2 beyond the initial association, but there was a small path from AUD at T1 to other anxiety disorders at T2.
Figure 2.
Longitudinal phenotypic associations among social anxiety disorder (SAD), other anxiety disorders (AnxIRT), and alcohol use disorder (AUD) occurring within 5-year intervals assessed 10 years apart, including 95% confidence intervals.
Longitudinal biometric analyses
Shared environmental effects could be removed from the biometric model of SAD and AUD (Δ−2LL=3.14; Δdf=10; p=0.978; ΔAIC=−16.86). A model with no additive genetic effects did not have as good fit (Δ−2LL=14.76; Δdf=10; p=0.141; ΔAIC=−5.24), and a model with neither additive genetic nor shared environmental effects had poor fit (Δ−2LL=107.40; Δdf=20; p<0.001; ΔAIC=+67.40). We present the results of the biometric model fitting in the upper part of Table 3. We tested whether the longitudinal association between SAD at T1 and AUD at T2 was best explained by separate genetic and environmental associations (model 0; a41 and e41), phenotypic influences (model 1; b41), a genetic association only (model 2; a41), or no association beyond the initial correlation between the disorders (model 3). Model 1 with a direct phenotypic path had the best model fit. We tested similar models for the association between AUD at T1 and SAD at T2. As in the descriptive, longitudinal model, this relationship was best explained by the initial correlation. The difference in AIC (−5.54) between the initial and best fitting model is ‘considerable’, according to rules of thumb (Burnham & Anderson, 2004). The best fitting biometric model for SAD and AUD is shown in the left panel of Figure 3.
Table 3.
Model fit indices from biometric structural equation modelling of social anxiety disorder (SAD), other lifetime anxiety disorders (AnxIRT), and alcohol use disorder (AUD) occurring the last five years.
| Social anxiety disorder and alcohol use disorder | ||||
| Model | Δ−2LL | Δdf | p | ΔAIC |
| 0: Genetic and environmental associations | - | - | - | - |
| 1: T1 SAD → T2 AUD: Phenotypic influence | 0.01 | 1 | 0.954 | −1.99 |
| 2: T1 SAD → T2 AUD: Genetic association | 2.25 | 1 | 0.133 | 0.26 |
| 3: T1 SAD → T2 AUD: Initial association only | 7.85 | 2 | 0.020 | 3.86 |
| 4: T1 AUD → T2 SAD: Phenotypic influence | 0.26 | 1 | 0.608 | −1.73 |
| 5: T1 AUD → T2 SAD: Genetic association | 0.38 | 1 | 0.538 | −1.62 |
| 6: T1 AUD → T2 SAD: Initial association only | 0.38 | 2 | 0.827 | −3.62 |
| 7: Combination of model 1 and 6 | 0.46 | 3 | 0.927 | −5.54 |
| Other anxiety disorders and alcohol use disorder | ||||
| Model | Δ−2LL | Δdf | p | ΔAIC |
| 0: Genetic and environmental associations | - | - | - | - |
| 1: T1 AnxIRT → T2 AUD: Phenotypic influence | 4.86 | 1 | 0.027 | 2.86 |
| 2: T1 AnxIRT → T2 AUD: Genetic association | 1.15 | 1 | 0.284 | −0.85 |
| 3: T1 AnxIRT → T2 AUD: Initial association only | 8.41 | 2 | 0.015 | 4.41 |
| 4: T1 AUD → T2 AnxIRT: Phenotypic influence | 5.90 | 1 | 0.015 | 3.90 |
| 5: T1 AUD → T2 AnxIRT: Genetic association | 3.14 | 1 | 0.076 | 1.14 |
| 6: T1 AUD → T2 AnxIRT: Initial association only | 6.15 | 2 | 0.046 | 2.15 |
Note: In Model 0, genetic and environmental associations across time are estimated independently of each other. A model with a genetic association and a phenotypic path (instead of environmental association) would be algebraically equivalent and have the same fit as Model 0. Bold text indicates the best model within each block.
Figure 3.
Best fitting biometric models for the longitudinal relationship between social anxiety disorder (SAD) and alcohol use disorder (AUD) (left-hand side) and for the relationship between other anxiety disorders and AUD (right). Paths below 0.20 are drawn with dashed lines.
We then turn to the other anxiety disorders and AUD. Again, we detected no effects of shared environment (Δ−2LL=2.77; Δdf=10; p=0.986; ΔAIC=−17.23). A model with no additive genetic effects was not as good (Δ−2LL=16.23; Δdf=10; p=0.093; ΔAIC=−3.77), and the model with no familial resemblance was poor (Δ−2LL=181.29; Δdf=20; p<0.001; ΔAIC=+141.29). The results for the model fitting are shown in the lower part of Table 3. The association between AnxIRT at T1 and AUD at T2 was best explained by a genetic association. The genetic and environmental associations between AUD at T1 and AnxIRT at T2 did not converge to one direct phenotypic path, but were better explained by separate genetic and environmental associations (model 0). Genetic factors for AnxIRT at T1 seemed to be positively related to AUD at T2, whereas environmental influences at AnxIRT at T1 seemed to reduce the liability to AUD at T2. The model with a purely genetic association (model 5) was almost equally good. The best fitting model is shown in the right panel of Figure 3.
Cross-sectional ‘direction of causation’ analyses
The longitudinal models presented above are constrained by the time frame available in the data, and cannot determine the direction of associations within time. Biometric models are sometimes able to infer causal associations from cross-sectional data. In order to triangulate the modelling and to increase the number of cases, we also used ‘direction of causation’ models with the two repeated lifetime assessments of SAD and AUD as cross-sectional indicators of risk. In this model, the genetic correlation between SAD and AUD was 0.65 (95% CI 0.58, 0.95) and the environmental correlation was 0.45 (95% CI 0.16, 0.51). We compared this model with shared risk factors to models with direct effects from SAD to AUD, from AUD to SAD, and in both directions. The results are shown in the upper part of Table 4. The best fitting model included direct paths from SAD to AUD, whereas the model with a path in the opposite direction had worse fit. The difference in fit was small, possibly because SAD and AUD had similar modes of inheritance. The results are nevertheless in line with the longitudinal model with effects from SAD to AUD. In addition, the path from AUD to SAD was estimated at approximately zero in the reciprocal model. The model implies that SAD explains 30.0% of the phenotypic variance in AUD (i.e., 0.552×100%).
Table 4.
Model fit indices from biometric structural equation modelling of lifetime social anxiety disorder (SAD) and lifetime alcohol use disorder (AUD) and other lifetime anxiety disorders (AnxIRT) and AUD, with estimates of direct effects.
| Social anxiety disorder | ||||||
| Model | Δ−2LL | Δdf | p | ΔAIC | SAD → AUD | AUD → SAD |
| A: Shared risk factors | - | - | - | |||
| B: SAD to AUD | 0.01 | 1 | 0.930 | −1.99 | 0.55 | - |
| C: AUD to SAD | 1.24 | 1 | 0.265 | −0.75 | - | 0.55 |
| D: Reciprocal causation | 0.00 | 0 | 1.000 | 0.00 | 0.57 | −0.03 |
| Other anxiety disorders | ||||||
| Model | Δ−2LL | Δdf | p | ΔAIC | AnxIRT → AUD | AUD → AnxIRT |
| A: Shared risk factors | - | - | - | |||
| B: AnxIRT to AUD | 2.61 | 1 | 0.106 | 0.61 | 0.41 | - |
| C: AUD to AnxIRT | 6.33 | 1 | 0.012 | 4.33 | - | 0.41 |
| D: Reciprocal causation | 0.00 | 0 | 1.000 | 0.00 | 0.67 | −0.38 |
We also tested the ‘direction of causation’ models with the repeated lifetime assessments of other anxiety disorders and AUD. In the model with shared risk factors, the genetic correlation between other anxiety disorders and AUD was 0.66 (95% CI, 0.44, 0.88) and the environmental correlation 0.05 (95% CI −0.26, 0.30). Because both phenotypes are influenced by environmental factors, the lack of environmental association makes causal model less plausible. The lower part of Table 4 shows the fit of four models of this relationship. In line with the longitudinal analyses, the model with shared risk factors (model 4) had the best fit.
Discussion
We used a population based twin sample with two diagnostic interviews to investigate explanations of the associations between SAD, other anxiety disorders, and AUD. First, we demonstrated that SAD was associated with AUD over and beyond the association between AUD and anxiety disorders in general. Second, SAD prospectively predicted AUD, but other anxiety disorders did not. AUD did not prospectively predict SAD, but possibly other anxiety disorders. Third, two different kinds of biometric models indicated that the relationship between SAD and AUD was best explained by influences from SAD to AUD. For the other anxiety disorders, the positive correlation with AUD could be explained by shared genetic risk factors alone.
As in previous studies, all anxiety disorders were correlated with AUD (Fergusson et al., 2011). SAD had the strongest association, and the unique aspects of SAD were independently associated with AUD. This is contrary to a study (Kushner et al., 2012) finding that the overall internalizing symptom load rather than particular disorders were of importance. Differences may be related to the age of the sample – which was relatively young – or to the threshold used to define cases. More severe SAD cases are likely to avoid social gatherings altogether, rather than to participate and be exposed to alcohol (Stewart, Morris, Mellings, & Komar, 2009).
The biometric modelling favoured models with direct phenotypic paths from SAD to AUD over models with shared genetic and environmental risk factors and models with direct paths from AUD to SAD. This finding was robust to variations in modelling and timeframe. Like previous studies (Buckner & Schmidt, 2009; Buckner et al., 2008; Buckner & Turner, 2009; Dahne et al., 2014; Wolitzky-Taylor et al., 2012), we observed a temporal order where SAD was more likely to occur before AUD than vice versa. Although one should always be cautious with causal inference, we have observed specificity and temporality, which are classic signs of causality (Hill, 1965), and gathered evidence against three competing explanations for the association between SAD and AUD: i) confounding by common risk factors, ii) reverse causality, and iii) that the association is not specific to SAD. Therefore, the present study adds support to the hypothesis that AUD can develop as a consequence of SAD. A causal interpretation is in line with previous studies finding strong and independent prospective associations from SAD to AUD (Buckner et al., 2008), and resonates well with the commonsensical observation that alcohol is often served in the settings that individuals with SAD are afraid of, and that many individuals drink to cope with anxiety. Reduction in social anxiety is an important drinking motive (Terlecki & Buckner, 2015) that has been found to be associated with AUD within twin pairs (Prescott et al., 2004). Thus, the totality of evidence suggests that SAD may be a fruitful target for interventions aiming to prevent AUD.
The positive relationship between other anxiety disorders and AUD was not in line with direct influences between the phenotypes, but rather seemed to be explained by genetic background factors common to both AUD and anxiety. A genetic correlation can reflect a causal relationship (Gage, Smith, Ware, Flint, & Munafo, 2016), but for environmentally influenced disorders one would expect also to find an environmental correlation in the same direction. Previous twin studies have failed to find an environmental association (Nelson et al., 2000; Tambs et al., 1997), and the lack of effects from AUD to anxiety is also in line with a previous Mendelian randomization study (Chao et al., 2017). The model that included a small, negative environmental path from AUD to other anxiety disorders had slightly better fit than the model with only the genetic path. Taken at face value, environmental risk of AUD reduced the risk of later anxiety disorders. This contradicts previous studies and may be due to statistical fluctuations. We would therefore not emphasise this small, negative environmental correlation unless it is replicated. In any case, our results underline the special role of SAD. Interestingly, drinking with the intention of managing depression was not found to influence AUD in the above-mentioned study that found an effect of social anxiety (Prescott et al., 2004).
Some interesting implications arise if SAD, but not other anxiety disorders influence AUD. First, it is particularly important to prevent and treat SAD, because it has an additional effect of preventing AUD. There may be an underutilized potential here, because only a minority of individuals with SAD receive treatment for the condition (Schneier et al., 2010), even though SAD is a common disorder and efficacious cognitive behavioural treatments exist (Hudson, 2017). Further, in clinical settings, it is important to assess if a patient with SAD uses alcohol as a coping strategy, and to discuss the dangers of self-medication with alcohol. Although AUD does not seem to be a strong influence on new onset of SAD, AUD could worsen the course of SAD. This is particularly relevant when alcohol is naturally present in the feared situations. As therapy for SAD involves exposure to feared situations, it is important to make sure that alcohol is not used as a means of managing the exposure tasks.
The findings must be interpreted in the light of some limitations: First, we could not model environmental confounders and direct paths simultaneously. Therefore, we could only detect the most prominent of these effects. The difference in AIC was small between some of the models, but our main findings were consistent across different models and variable definitions. In addition, we could not model interactions between genetic, environmental, and direct effects. The biometric models nevertheless add information over purely phenotypic models and add to the consistent totality of evidence. Second, we could not distinguish between alcohol abuse and alcohol dependence. However, the merging of the two diagnoses as AUD is in line with the DSM-5 (American Psychiatric Association, 2013). Third, the interviews were retrospective and have measurement error. This can lead to deflated environmental correlations in twin models. However, we adjusted for this by using repeated lifetime measures in a measurement model, and obtained results that were in line with the longitudinal modelling. Fourth, many individuals identified in the Medical Birth Registry dropped out before they completed the second interview. Previous analyses on Norwegian twin data have shown that participation was predicted by female sex, monozygosity and higher educational status, but not statistically significantly by symptoms of psychiatric disorders or substance abuse (Tambs et al., 2009). Non-response can reduce statistical power and bias prevalence estimates. However, estimates of associations between variables are more robust (Nilsen et al., 2009). The use of FIML ensures that all available data are being utilized, and can sometimes correct for bias even when data are not missing completely at random (Enders & Bandalos, 2001). Finally, generalization of the results may be limited to individuals of similar age and ethnic background as the participants.
Conclusion
Our results suggest that SAD is a likely causal influence on AUD. This does not apply to other anxiety disorders. Interventions aimed at prevention and treatment of SAD are therefore likely to have an additional beneficial effect of reducing the risk for AUD. Interventions aimed at other anxiety disorders are unlikely to have similar additional effect on AUD.
Acknowledgements
This project was supported by the Research Council of Norway (RCN), grant 240061. Previous data collections were in part supported by RCN, the National Institutes of Health (grant MH-068643), the Norwegian Foundation for Health and Rehabilitation, and the Norwegian Council for Mental Health.
References
- Akaike H (1987). Factor-analysis and AIC. Psychometrika, 52(3), 317–332. doi:Doi 10.1007/Bf02294359 [DOI] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Washington, D.C.: American Psychiatric Association. [Google Scholar]
- Becker HC (2012). Effects of Alcohol Dependence and Withdrawal on Stress Responsiveness and Alcohol Consumption. Alcohol Research-Current Reviews, 34(4), 448–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boschloo L, Vogelzangs N, Smit JH, van den Brink W, Veltman DJ, Beekman ATF, & Penninx BWJH (2011). Comorbidity and risk indicators for alcohol use disorders among persons with anxiety and/or depressive disorders Findings from the Netherlands Study of Depression and Anxiety (NESDA). Journal of Affective Disorders, 131(1–3), 233–242. doi: 10.1016/j.jad.2010.12.014 [DOI] [PubMed] [Google Scholar]
- Briley DA, Livengood J, Derringer J, & Kandler C (2018). Behaviour Genetic Frameworks of Causal Reasoning for Personality Psychology. European Journal of Personality, 32(3), 202–220. doi: 10.1002/per.2153 [DOI] [Google Scholar]
- Buckner JD, & Schmidt NB (2009). Understanding social anxiety as a risk for alcohol use disorders: Fear of scrutiny, not social interaction fears, prospectively predicts alcohol use disorders. Journal of Psychiatric Research, 43(4), 477–483. doi: 10.1016/j.jpsychires.2008.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, & Lewinsohn PM (2008). Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. Journal of Psychiatric Research, 42(3), 230–239. doi: 10.1016/j.jpsychires.2007.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, & Turner RJ (2009). Social anxiety disorder as a risk factor for alcohol use disorders: A prospective examination of parental and peer influences. Drug and Alcohol Dependence, 100(1–2), 128–137. doi: 10.1016/j.drugalcdep.2008.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulley A, Miloyan B, Brilot B, Gullo MJ, & Suddendorf T (2016). An evolutionary perspective on the co-occurrence of social anxiety disorder and alcohol use disorder. J Affect Disord, 196, 62–70. doi: 10.1016/j.jad.2016.02.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnham KP, & Anderson DR (2004). Multimodel inference - understanding AIC and BIC in model selection. Sociological Methods & Research, 33(2), 261–304. doi: 10.1177/0049124104268644 [DOI] [Google Scholar]
- Carrigan MH, & Randall CL (2003). Self-medication in social phobia. Addictive Behaviors, 28(2), 269–284. doi: 10.1016/s0306-4603(01)00235-0 [DOI] [PubMed] [Google Scholar]
- Cerda M, Sagdeo A, Johnson J, & Galea S (2010). Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord, 126(1–2), 14–38. doi: 10.1016/j.jad.2009.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao M, Li X, & McGue M (2017). The Causal Role of Alcohol Use in Adolescent Externalizing and Internalizing Problems: A Mendelian Randomization Study. Alcoholism-Clinical and Experimental Research, 41(11), 1953–1960. doi: 10.1111/acer.13493 [DOI] [PubMed] [Google Scholar]
- Dahne J, Banducci AN, Kurdziel G, & MacPherson L (2014). Early Adolescent Symptoms of Social Phobia Prospectively Predict Alcohol Use. Journal of Studies on Alcohol and Drugs, 75(6), 929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, & Bandalos DL (2001). The Relative Performance of Full Information Maximum Likelihood Estimation for Missing Data in Structural Equation Models. Structural Equation Modeling-a Multidisciplinary Journal, 8(3), 430–457. doi: 10.1207/S15328007sem0803_5 [DOI] [Google Scholar]
- Fergusson DM, Boden JM, & Horwood LJ (2011). Structural models of the comorbidity of internalizing disorders and substance use disorders in a longitudinal birth cohort. Social Psychiatry and Psychiatric Epidemiology, 46(10), 933–942. doi: 10.1007/s00127-010-0268-1 [DOI] [PubMed] [Google Scholar]
- Gage SH, Smith GD, Ware JJ, Flint J, & Munafo MR (2016). G = E: What GWAS Can Tell Us about the Environment. Plos Genetics, 12(2). doi:ARTN e1005765 10.1371/journal.pgen.1005765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman JM, Ramchandani VA, Davis MB, Bjork JM, & Hommer DW (2008). Why we like to drink: a functional magnetic resonance imaging study of the rewarding and anxiolytic effects of alcohol. J Neurosci, 28(18), 4583–4591. doi: 10.1523/JNEUROSCI.0086-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Blanco C, Stinson FS, Chou SP, Goldstein RB, … Huang B (2005). The epidemiology of social anxiety disorder in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry, 66(11), 1351–1361. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, … Kaplan K (2004). Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry, 61(8), 807–816. doi: 10.1001/archpsyc.61.8.807 [DOI] [PubMed] [Google Scholar]
- Heath AC, Kessler RC, Neale MC, Hewitt JK, Eaves LJ, & Kendler KS (1993). Testing Hypotheses About Direction of Causation Using Cross-Sectional Family Data. Behavior Genetics, 23(1), 29–50. doi:Doi 10.1007/Bf01067552 [DOI] [PubMed] [Google Scholar]
- Hill AB (1965). The Environment and Disease: Association or Causation? Proc R Soc Med, 58, 295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgson K, Almasy L, Knowles EE, Kent JW, Curran JE, Dyer TD, … Glahn DC (2016). Genome-wide significant loci for addiction and anxiety. Eur Psychiatry, 36, 47–54. doi: 10.1016/j.eurpsy.2016.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JL (2017). Prevention of Anxiety Disorders Across the Lifespan. JAMA Psychiatry, 74(10), 1029–1030. doi: 10.1001/jamapsychiatry.2017.2430 [DOI] [PubMed] [Google Scholar]
- Kushner M, Abrams K, & Borchardt C (2000). The relationship between anxiety disorders and alcohol use disorders A review of major perspectives and findings. Clinical Psychology Review, 20(2), 149–171. doi: 10.1016/s0272-7358(99)00027-6 [DOI] [PubMed] [Google Scholar]
- Kushner M, Wall MM, Krueger RF, Sher KJ, Maurer E, Thuras P, & Lee S (2012). Alcohol dependence is related to overall internalizing psychopathology load rather than to particular internalizing disorders: evidence from a national sample. Alcoholism-Clinical and Experimental Research, 36(2), 325–331. doi: 10.1111/j.1530-0277.2011.01604.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychol Bull, 143(2), 142–186. doi: 10.1037/bul0000069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecrubier Y, Wittchen HU, Faravelli C, Bobes J, Patel A, & Knapp M (2000). A European perspective on social anxiety disorder. Eur Psychiatry, 15(1), 5–16. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR (2012). Anxiety disorders and substance use disorders: Different associations by anxiety disorder. J Anxiety Disord, 26(1), 88–94. doi: 10.1016/j.janxdis.2011.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neale MC, Hunter MD, Pritikin JN, Zahery M, Brick TR, Kirkpatrick RM, … Boker SM (2016). OpenMx 2.0: Extended Structural Equation and Statistical Modeling. Psychometrika, 81(2), 535–549. doi: 10.1007/s11336-014-9435-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neale MC, & Kendler KS (1995). Models of comorbidity for multifactorial disorders. Am J Hum Genet, 57(4), 935–953. [PMC free article] [PubMed] [Google Scholar]
- Neale MC, & Maes HH (2004). Methodology for genetic studies of twins and families. Dordrecht, The Netherlands: Kluwer Academic Publishers. [Google Scholar]
- Nelson EC, Grant JD, Bucholz KK, Glowinski A, Madden PAF, Reich W, & Heath AC (2000). Social phobia in a population-based female adolescent twin sample: co-morbidity and associated suicide-related symptoms. Psychol Med, 30(4), 797–804. [DOI] [PubMed] [Google Scholar]
- Nilsen RM, Vollset SE, Gjessing HK, Skjaerven R, Melve KK, Schreuder P, … Magnus P (2009). Self-selection and bias in a large prospective pregnancy cohort in Norway. Paediatr Perinat Epidemiol, 23(6), 597–608. doi: 10.1111/j.1365-3016.2009.01062.x [DOI] [PubMed] [Google Scholar]
- Nilsen TS, Knudsen GP, Gervin K, Brandt I, Roysamb E, Tambs K, … Harris JR (2013). The Norwegian Twin Registry from a public health perspective: a research update. Twin Res Hum Genet, 16(1), 285–295. doi: 10.1017/thg.2012.117 [DOI] [PubMed] [Google Scholar]
- Pan W (2001). Akaike’s Information Criterion in Generalized Estimating Equations. Biometrics, 57(1), 120–125. doi: 10.1111/j.0006-341X.2001.00120.x [DOI] [PubMed] [Google Scholar]
- Prescott CA, Cross RJ, Kuhn JW, Horn JL, & Kendler KS (2004). Is risk for alcoholism mediated by individual differences in drinking motivations? Alcoholism-Clinical and Experimental Research, 28(1), 29–39. doi: 10.1097/01.ALC.0000106302.75766.F0 [DOI] [PubMed] [Google Scholar]
- Rosenstrom T, Czajkowski NO, Ystrom E, Krueger RF, Aggen SH, Gillespie NA, … Torvik FA (2019). Genetically Informative Mediation Modeling Applied to Stressors and Personality-Disorder Traits in Etiology of Alcohol Use Disorder. Behav Genet, 49(1), 11–23. doi: 10.1007/s10519-018-9941-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneier FR, Foose TE, Hasin DS, Heimberg RG, Liu SM, Grant BF, & Blanco C (2010). Social anxiety disorder and alcohol use disorder co-morbidity in the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med, 40(6), 977–988. doi: 10.1017/S0033291709991231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Morris E, Mellings T, & Komar J (2009). Relations of social anxiety variables to drinking motives, drinking quantity and frequency, and alcohol-related problems in undergraduates. Journal of Mental Health, 15(6), 671–682. doi: 10.1080/09638230600998904 [DOI] [Google Scholar]
- Tambs K, Harris JR, & Magnus P (1997). Genetic and environmental contributions to the correlation between alcohol consumption and symptoms of anxiety and depression. Results from a bivariate analysis of Norwegian twin data. Behav Genet, 27(3), 241–250. [DOI] [PubMed] [Google Scholar]
- Tambs K, Ronning T, Prescott CA, Kendler KS, Reichborn-Kjennerud T, Torgersen S, & Harris JR (2009). The Norwegian Institute of Public Health twin study of mental health: examining recruitment and attrition bias. Twin Research and Human Genetics, 12(2), 158–168. doi: 10.1375/twin.12.2.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terlecki MA, & Buckner JD (2015). Social anxiety and heavy situational drinking: coping and conformity motives as multiple mediators. Addictive Behaviors, 40, 77–83. doi: 10.1016/j.addbeh.2014.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terra MB, Barros HM, Stein AT, Figueira I, Jorge MR, Palermo LH, … Da Silveira DX (2006). Social anxiety disorder in 300 patients hospitalized for alcoholism in Brazil: high prevalence and undertreatment. Compr Psychiatry, 47(6), 463–467. doi: 10.1016/j.comppsych.2006.02.004 [DOI] [PubMed] [Google Scholar]
- Torvik FA, Rosenstrom TH, Ystrom E, Tambs K, Roysamb E, Czajkowski N, … Reichborn-Kjennerud T (2017). Stability and change in etiological factors for alcohol use disorder and major depression. J Abnorm Psychol, 126(6), 812–822. doi: 10.1037/abn0000280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turkheimer E, Pettersson E, & Horn EE (2014). A phenotypic null hypothesis for the genetics of personality. Annu Rev Psychol, 65, 515–540. doi: 10.1146/annurev-psych-113011-143752 [DOI] [PubMed] [Google Scholar]
- Wittchen H-U, & Pfister H (1997). DIA-X interviews (M-CIDI). Frankfurt, Germany: Swets & Zeitlinger. [Google Scholar]
- Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, & Craske MG (2012). Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addictive Behaviors, 37(8), 982–985. doi: 10.1016/j.addbeh.2012.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]