Abstract
Objective
Posttraumatic stress disorder (PTSD) is frequently associated with depression and anxiety, but the nature of the relationship is unclear. By removing mood and anxiety diagnostic criteria, the eleventh edition of the International Classification of Diseases (ICD-11) aims to delineate a distinct PTSD phenotype. We examine the effect of implementing ICD-11 criteria on rates of co-diagnosed depression and anxiety in survivors with recent PTSD.
Method
Participants were 1,061 survivors of traumatic injury admitted to acute care centers in Israel. ICD-10 and ICD-11 diagnostic rules were applied to the Clinician-Administered PTSD Scale for DSM-IV (CAPS). Co-occurring disorders were identified using the Structured Clinical Interview for DSM-IV (SCID). Depression severity was measured by the Beck Depression Inventory-II (BDI-II). Assessments were performed 0–60 (“Wave 1”) and 90–240 (“Wave 2”) days after trauma exposure.
Results
Participants identified by ICD-11 PTSD criteria were equally or more likely than those identified by the ICD-10 alone to meet depression or anxiety disorder diagnostic criteria (for Wave 1: depressive disorders, OR=1.98, 95% CI=[1.36, 2.87]; anxiety disorders, OR=1.04, 95% CI=[0.67, 1.64]; for Wave 2: depressive disorders, OR=1.70, 95% CI=[1.00, 2.91]; anxiety disorders, OR=1.04, 95% CI=[0.54, 2.01]). ICD-11 PTSD was associated with higher BDI scores (M=23.15 vs. 17.93, p<.001 for Wave 1; M=23.93 vs. 17.94 p<0.001 for Wave 2). PTSD symptom severity accounted for the higher levels of depression in ICD-11 PTSD.
Conclusions
Despite excluding depression and anxiety symptom criteria, the ICD-11 identified equal or higher proportion of depression and anxiety disorders, suggesting that those are inherently associated with PTSD.
Keywords: posttraumatic stress disorder, comorbidity, depressive disorders, anxiety disorders, nosology
Introduction
Posttraumatic stress disorder (PTSD) is frequently associated with mood and anxiety symptoms and disorders (Elhai, Grubaugh, Kashdan, & Frueh, 2008; Kessler, Chiu, Demler, Merikangas, & Walters, 2005; Rytwinski, Scur, Feeny, & Youngstrom, 2013). PTSD co-morbidity challenges efforts to devise disorder-specific therapy and examine the disorder’s distinct neurobiology.
The eleventh edition of the International Classification of Diseases (ICD-11), published in June 2018 and expected to come into effect in January of 2022 (World Health Organization, 2018a), reduced the number of disorder-defining symptom by excluding symptoms common to both PTSD and mood/anxiety disorders (e.g., sleep disturbances, irritability, difficulty concentrating; World Health Organization, 2018b). According to its authors, “The first reason [for this change] is the inescapable fact of the very high rates of comorbidity associated with DSM-based PTSD. This raises the question of whether comorbidity could be reduced with a more-focused symptom set” (Brewin, 2013). In line with this goal, ICD-11 PTSD criteria comprise seven symptoms ostensibly unique to PTSD: intrusive memories of the traumatic event, dissociative flashbacks, nightmares, avoidance of external reminders, avoidance of thoughts and feelings associated with the traumatic event, hypervigilance, and exaggerated startle response (World Health Organization, 2018b). The ICD-11’s use of a PTSD-specific template implies that PTSD can be reliably parsed from co-occurring depression and anxiety and simultaneously provides a unique opportunity to test that assumption.
Previous studies of the prevalence of comorbidity using the ICD-11 PTSD diagnostic criteria have produced conflicting evidence regarding the ICD-11’s tendency to reduce co-diagnoses of mood and anxiety disorders relative to DSM-IV and DSM-5 templates (e.g., Hafstad, Thorensen, Wentzel-Larsen, Maercker, & Dyb, 2017; Hyland et al., 2016; O’Donnell et al., 2014; Wisco et al., 2016). However, evaluating the ICD-11’s success in isolating PTSD from comorbid conditions is better tested against its parent symptom template, i.e., ICD-10. One study that used this comparison involved institutional abuse and World War II survivors (Gluck, Knefel, Tran, & Lueger-Schuster, 2016) and found no differences in depressive, anxious, or somatic symptomatology between ICD-10 and ICD-11-identified participants. All ICD-11 studies to date evaluated patients with chronic PTSD and employed single, cross-section evaluations. Previous research has also demonstrated that the ICD-11 PTSD criteria identify only a subset of the individuals previously identified as having PTSD by the ICD-10 criteria (Barbano et al., 2018; Gluck et al., 2016; Haravuori, Kiviruusu, Suomalainen, & Marttunen, 2016; Tay et al., 2017), allowing comparisons between participants identified by the ICD-11, the ICD-10, and the ICD-10 only.
Repeated assessments at successive stages of the response to traumatic event may better establish the consistency of the ICD-11’s ability to better separate PTSD from co-occurring disorders, as previous research shows that trauma survivors’ PTSD diagnostic statuses change over time (Bryant, O’Donnell, Creamer, McFarlane, & Silove, 2013).
This work reports two repeated assessments of ICD 10 and ICD-11 and, within each assessment, tested the following assumption: If the ICD-11 successfully separates PTSD from comorbid disorders, then individuals diagnosed using the ICD-11 template will show lower prevalence of concurrent disorders and lower depression symptom levels. We tested that hypothesis by first comparing participants identified by the ICD-10 overall with those identified by ICD-11 and, additionally, comparing those identified by ICD-11 with those meeting ICD-10 criteria alone. The former comparison examined the changes in the rates of comorbidities introduced by clinically implementing the ICD-11 template criteria, relative to the previous use of ICD-10. The latter comparison theoretically tested the assumption that more focused symptom criteria exclude individuals more prone to comorbid disorders, or those who would be better characterized as having another mental disorder.
To that end, we measured the prevalence of mood and anxiety disorders among recent survivors identified by the ICD-11 and the previous ICD-10 diagnostic templates at two time intervals from the traumatic event. The sample was comprised of emergency department (ED) patients assessed shortly after trauma exposure with follow-up assessments at three to eight months after exposure. Finally, because previous research suggests that the ICD-11 criteria identify individuals with more severe PTSD symptoms (Barbano et al., 2018; Gluck et al., 2016; Haravuori et al., 2016), we also examined the contribution of PTSD symptom severity to comorbid disorders’ prevalence and depression severity.
Method
Sources of Data
Data for this work were obtained from three studies that longitudinally evaluated adult civilians admitted to general hospital emergency departments (EDs) following potentially traumatic events in Israel (n=1061). Traumatic events were categorized as either motor vehicle accidents (MVAs), other non-interpersonal accidents (e.g., falls, burns, animal attacks), or interpersonal harm (e.g., assaults). The studies (Shalev et al., 2000; Shalev et al., 2011; Shalev et al., 2007) employed the Clinician-Administered PTSD Scale for DSM-IV (CAPS; Blake et al., 1995), the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 2002), and the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996). Detailed methodology for harmonizing item-level data, including trauma type, from these studies and others, has been previously outlined (Qi et al., 2018).
Raw, psychometric, item-level data from each study were cleaned and processed to provide standardized measures of depressive and anxiety diagnoses from the SCID. Every participant with a CAPS assessment and a SCID and/or BDI-II assessment within the same time interval was included in the analysis.
Data Collection Waves
Time periods between traumatic events and subsequent CAPS assessments were measured as number of “days since trauma.” For analyses, CAPS time interval data were grouped into two data collection waves. The first wave (“wave 1”), consisting of participants’ first assessments and extending from 0–60 days, represented an early post-exposure period following a traumatic event (mean days since trauma = 21.6, standard deviation [SD] = 8.1). The second wave (“wave 2”), consisting of participants’ first follow-up assessments and extending from 90–240 days, represented persisting, early PTSD (mean days since trauma = 138.3, SD = 29.1).
ICD Classification
The CAPS for DSM-IV was used to assess PTSD symptom severity and to infer ICD-10 and ICD-11 diagnostic status. CAPS items encompass 17 DSM-IV PTSD diagnostic criteria and quantify each symptom’s frequency and intensity on a scale of 0 to 4. Following CAPS guidelines (Weathers, Keane, & Davidson, 2001; F.W. Weathers, A. M. Ruscio, & T.M. Keane, 1999), we defined a symptom as positively endorsed if its frequency score was 1 or more and its intensity score was 2 or more.
ICD-10 and ICD-11 diagnoses were derived from CAPS symptoms aligned with the ICD-10 and ICD-11 diagnostic criteria. Though previous research has typically used six symptoms to represent the ICD-11 symptom criteria (e.g., (Gluck et al., 2016; Hyland et al., 2016)), this study employed seven symptoms to reflect the most updated ICD-11 guidelines, which state that individuals may “[re-experience] the traumatic event or events in the present in the form of vivid intrusive memories” (World Health Organization, 2018b) (as represented by CAPS item B1) as well as, separately, flashbacks (as represented by CAPS item B3) (Table 1). Avoidance and hyperarousal symptoms, though reduced in number, have remained largely unchanged in ICD revisions. As such, the ICD-11 criteria were: one out of CAPS items 1 through 3 (B1, B2, or B3); one out of items 6 and 7 (C1 and C2); and one out of items 16 and 17 (D4 and D5). For ICD-10, the criteria were: one out of CAPS items 1 through 5 (B cluster); one out of items 6 and 7 (C1 and C2); and either item 8 (C3) or two out of items 13 through 17 (D cluster).
Table 1:
CAPS and ICD-11 Re-experiencing Symptoms
| CAPS item: | CAPS question: | ICD-11 criteria: |
|---|---|---|
| B1 | Have you ever had unwanted memories of (EVENT)? What were they like? | re-experiencing the traumatic event or events in the present in the form of vivid intrusive memories, flashbacks, or nightmares, which are typically accompanied by strong and overwhelming emotions such as fear or horror and strong physical sensations, or feelings of being overwhelmed or immersed in the same intense emotions that were experienced during the traumatic event |
| B2 | Have you ever had unpleasant dreams about (EVENT)? | |
| B3 | Have you ever suddenly acted or felt as if (EVENT) were happening again? |
CAPS: Blake et al., 1995
ICD-11: World Health Organization, 2018
For analysis, the following PTSD groups were identified: an “ICD-10” group (all participants who met ICD-10 diagnostic criteria), an “ICD-11” group (all participants who met ICD-11 diagnostic criteria), an “ICD-10 only” group (participants who met ICD-10 but not ICD-11 diagnostic criteria), and a “no PTSD” group (participants meeting neither ICD-10 nor ICD-11 diagnostic criteria). The small number of participants meeting ICD-11 criteria only in each time interval (n = 8, 1.3% and n = 2, 1.3% of the samples, respectively) precluded the use of an independent ICD-11 only group for analysis.
The significant overlap between the ICD-10 and ICD-11 groups in this sample precluded direct statistical comparisons between these groups. Instead, prevalences for ICD-10 and ICD-11 comorbid disorders are presented.
PTSD Severity
The CAPS total score (sum of symptoms’ intensities and frequencies, range: 0–136) quantifies PTSD symptom severity. Following CAPS recommended severity thresholds, a score of 40 or above was considered to be indicative of threshold PTSD. Specifically, we defined PTSD severity by the following recommended classes: 0–19 = asymptomatic, 20–39 = mild PTSD/subthreshold, 40–59 = moderate PTSD/threshold, 60–79 = severe PTSD, ≥80 = extreme PTSD (F. W. Weathers, A. M. Ruscio, & T. M. Keane, 1999).
Anxiety and Depressive Disorders
The SCID is a semi-structured clinical interview that assesses DSM-IV Axis I disorders and subsequently aids clinicians in assigning diagnoses. Each disorder is rated either 1, 2, or 3: 1 represents the absence of a disorder; 2 represents a subthreshold or possible disorder; and 3 represents the presence of a disorder. In this work, we considered ‘present disorders’ and not subthreshold disorders. The “depressive disorders” variable for this work included current diagnoses of at least one the following conditions: major depressive disorder, dysthymic disorder, and depressive disorder not otherwise specified (NOS). The “anxiety disorders” variable comprised current diagnoses of at least one of the following conditions: panic disorder, agoraphobia, social phobia, specific phobia, obsessive-compulsive disorder, generalized anxiety disorder, and anxiety disorder NOS.
Depression Severity
The BDI-II is a 21-item self-report measure of depression severity. Each item evaluates common symptoms of depression and is rated on a Likert scale of 0 to 3. Items on the BDI-II were summed to create a continuous measure of depression severity.
Data Analysis
Welch’s t-tests for age, BDI scores, and CAPS scores, and Fisher’s test for gender and types of trauma were conducted to assess differences between the two ICD classifications. Welch’s t-test was also used to compare CAPS scores of participants with data points in both data collection waves to those with only an initial data point (lost to follow-up).
In order to examine the associations between diagnostic variables (i.e., results on the CAPS, BDI, and SCID) and ICD classification, nested logistic regressions for odds ratios were conducted to evaluate the relative odds of a SCID diagnosis for depression or anxiety by ICD group (ICD-11 vs. ICD-10 only). The first level was a regression of SCID diagnosis on ICD classification. The second level featured the inclusion of age, gender, and type of trauma to assess whether the association persisted after adjustment for confounders. The last level was the addition of CAPS total severity score, to investigate the role of PTSD severity in explaining the relative difference in odds of a SCID diagnosis between the two ICD classification groups. Nested linear regressions featuring BDI total score as the outcome were conducted with the same levels as the nested logistic regressions. Regressions were conducted for both data collection waves 1 and 2. All analyses were conducted in R (R Core Team, 2017).
Results
Participant Characteristics
Participants were 1,061 survivors who had experienced traumatic events that included motor vehicle accidents (82.5%), other non-interpersonal accidents (6.0%), and interpersonal harm (11.5%). Demographic information is presented in Table 2.
Table 2:
Demographic characteristics of sample participants at first evaluation
| Total† | No PTSD | ICD-10 PTSD | ICD-11 PTSD | ICD-10 only | p‡ | |
|---|---|---|---|---|---|---|
| Wave 1 | N = 1,061 | N = 464 | N = 585 | N = 421 | N = 173 | |
| Age | ||||||
| M (SD) | 34.61 (12.26) | 33.29 (11.89) | 35.72 (12.47) | 35.38 (12.38) | 36.29 (12.65) | 0.423 |
| [95% CI] | [33.88, 35.35] | [32.21, 34.37] | [34.70, 36.73] | [34.20, 36.57] | [34.40, 38.19] | |
| Female gender | n = 509 (47.97%) | n = 218 (46.78%) | n = 287 (48.89%) | n = 220 (52.26%) | n = 71 (40.80%) | 0.012 |
| Trauma type: | .003 | |||||
| MVA | n = 872 (82.50%) | n = 389 (84.01%) | n = 477 (81.40%) | n = 332 (78.86%) | n = 151 (87.28%) | |
| Non-MVA accident | n = 63 (5.96%) | n = 32 (6.91%) | n = 31 (5.29%) | n = 20 (4.75%) | n = 11 (6.36%) | |
| Interpersonal harm | n = 122 (11.54%) | n = 42 (9.07%) | n = 78 (13.31%) | n = 69 (16.39%) | n = 11 (6.36%) | |
| Symptom severity: | ||||||
| CAPS | ||||||
| M (SD) | 47.91 (28.83) | 23.70 (18.02) | 67.36 (19.90) | 71.93 (19.73) | 54.61 (15.70) | <0.001 |
| [95% CI] | [46.17, 49.64] | [22.05, 25.34] | [65.74, 68.97] | [70.04, 73.82] | [52.26, 56.96] | |
| BDI-II | N = 1,012 | N = 457 | N = 547 | N = 394 | N = 161 | |
| M (SD) | 18.30 (12.61) | 14.25 (12.05) | 21.73 (12.12) | 23.15 (12.47) | 17.93 (10.21) | <0.001 |
| [95% CI] | [17.52, 19.07] | [13.14, 15.35] | [20.72, 22.75] | [21.91, 24.38] | [16.34, 19.51] | |
| Wave 2 | N = 902 | N = 656 | N = 244 | N = 132 | N = 114 | |
| Age | 34.48 (12.17) | 13.37 (14.33) | 36.65 (12.52) | 65.95 (20.99) | 48.80 (16.53) | 0.159 |
| M (SD) | [33.69, 35.28] | [12.27, 14.47] | [35.07, 38.23] | [62.34, 69.57] | [45.73, 51.87] | |
| [95% CI] | ||||||
| Female gender | n = 444 (49.22%) | n = 307 (46.80%) | n = 136 (55.74%) | n = 69 (51.52%) | n = 68 (60.53%) | 0.16 |
| Trauma type: | 0.433 | |||||
| MVA | n = 740 (82.41%) | n = 544 (83.31%) | n = 194 (79.84%) | n = 103 (78.63%) | n = 93 (81.58%) | |
| Non-MVA accident | n = 49 (5.46%) | n = 37 (5.67%) | n = 12 (4.94%) | n = 5 (3.82%) | n = 7 (6.14%) | |
| Interpersonal harm | n = 109 (12.14%) | n = 72 (11.03%) | n = 37 (15.23%) | n = 23 (17.56%) | n = 14 (12.28%) | |
| Symptom severity: | ||||||
| CAPS | 25.54 (25.75) | 13.37 (14.33) | 58.25 (20.76) | 65.95 (20.99) | 48.80 (16.53) | <0.001 |
| M (SD) | [23.86, 27.23] | [12.27, 14.47] | [55.64, 60.87] | [62.34, 69.57] | [45.73, 51.87] | |
| [95% CI] | ||||||
| BDI-II | N = 865 | N = 635 | N = 228 | N = 126 | N = 104 | <0.001 |
| M (SD) | 13.03 (12.65) | 10.06 (11.42) | 21.30 (12.29) | 23.93 (12.71) | 17.94 (10.94) | |
| [95% CI] | [12.19, 13.88] | [9.18, 10.95] | [19.70, 22.91] | [21.69, 26.17] | [15.81, 20.07] |
Missing data: 4 participants were missing data on type of trauma.
Statistical comparisons are between ICD-10 only and ICD-11 groups. T-tests were used for age, and Fisher’s tests were used for gender and type of trauma.
Abbreviations: MVA = motor vehicle accident; CAPS = Clinician-Administered PTSD Scale; BDI-II = Beck Depression Inventory-II
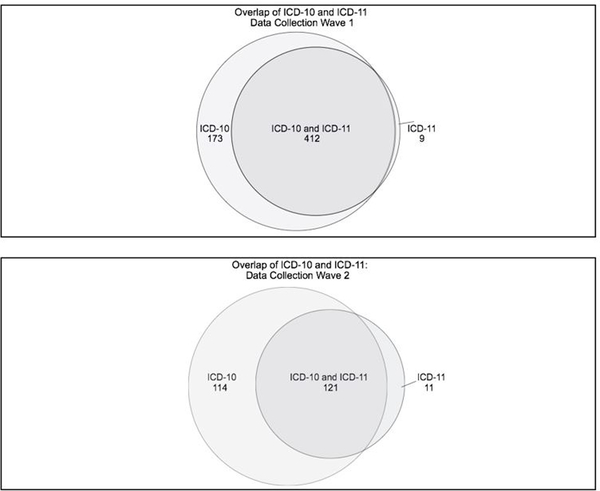
During wave 1 of data collection, 585 participants met ICD-10 PTSD diagnostic criteria, and 421 met ICD-11 diagnostic criteria. Of participants receiving an ICD-10 or ICD-11 PTSD diagnosis, 98.7% (n = 412) of participants who met ICD-11 criteria also met ICD-10 criteria. One hundred seventy-three participants (29.1%) were identified by the ICD-10 only (Figure 1).
Figure 1.
Participants meeting ICD‐10 and ICD‐11 PTSD diagnostic criteria at two data collection waves
During wave 2 of data collection, 235 participants met ICD-10 PTSD diagnostic criteria, and 132 met ICD-11 diagnostic criteria. Of participants receiving a PTSD diagnosis, 98.7% (n = 121) of participants who met ICD-11 criteria also met ICD-10 criteria. One hundred fourteen participants (46.3%) were identified by the ICD-10 only (Figure 1).
There were some notable differences between participants identified by the ICD-11 and the ICD-10 only: ICD-10 only and ICD-11 groups differed significantly on proportions of types of trauma (p = 0.003), with ICD-11-identified participants being more likely to have experienced interpersonal harm (16.4% vs. 6.4%). Additionally, the ICD-11 group had a significantly higher proportion of females than the ICD-10 only group (n = 220, 52.3% vs. n = 70, 40.5%, p = 0.011) (Table 1).
Participants lost to follow-up had significantly higher initial CAPS scores (M = 52.70, 95% CI = [48.31, 57.10]) than those not lost to follow-up (M = 46.97, 95% CI = [45.08, 48.86], p = .019).
PTSD Severity
During wave 1 of data collection, the mean CAPS score of ICD-11 participants (M = 71.93, 95% CI = [70.04, 73.82]) was significantly higher than that of ICD-10 only participants (M = 54.64, 95% CI = [52.27, 57.00], p < .0001).
At wave 2, the mean CAPS score of ICD-11 participants (M = 65.95, 95% CI = [62.34, 69.57]) was still significantly higher than that of ICD-10 only participants (M = 48.80, 95% CI = [45.73, 51.87], p < .0001).
Prevalence of Concurrent Disorders: Wave 1
In wave 1, the prevalence of depressive disorders was 46.5% (n = 264) in the ICD-10 group, 34.1% (n = 57) in the ICD-10 only group, and 50.6% (n = 207) in the ICD-11 group. The prevalence of anxiety disorders was 20.5% (n = 116) in the ICD-10 group, 19.9% (n = 33) in the ICD-10 only group and 20.6% (n = 84) in the ICD-11 group.
Prevalence of Concurrent Disorders: Wave 2
In wave 2, the prevalence of depressive disorders was 36.3% (n = 87) in the ICD-10 group, 32.3% (n = 32) in the ICD-10 only group, and 47.7% (n = 61) in the ICD-11 group. The prevalence of anxiety disorders was 18.3% (n = 44) in the ICD-10 group, 19.2% (n = 19) in the ICD-10 only group, and 19.5% (n = 25) in the ICD-11 group.
Nested Regressions: Wave 1
As presented in Table 3, the nested logistic regression model found that the odds of a comorbid SCID depressive disorder diagnosis in ICD-11 PTSD cases were 1.98 times higher than in ICD-10 only PTSD cases (95% CI = [1.36, 2.87], p < .001). When accounting for age, gender, and trauma type, ICD-11 cases had 2.12 times the odds of a comorbid SCID depressive disorder diagnosis than ICD-10 only cases (95% CI = [1.44, 3.12], p <.001). However, when additionally accounting for CAPS total severity score, ICD-11 classification became non-significant (95% CI = [.51, 1.28], p = .363).
Table 3 –
Nested Regressions with Odds Ratio or Coefficient of ICD-11 Classification, 95% Confidence Interval, and p-value
| ICD Classification | ICD with Age, Gender, and Trauma Type | ICD with Age, Gender, Trauma Type, and CAPS Score | |
|---|---|---|---|
| Wave 1 (0–60 days) | |||
| Anxiety disorder (OR) | 1.04 [.67, 1.64] .848 | 1.02 [.65, 1.62] .925 | 1.18 [.72, 1.94] .514 |
| Depressive disorder (OR) | 1.98 [1.36, 2.87] <.001 | 2.12 [1.44, 3.12] <.001 | .81 [.51, 1.28] .363 |
| Depression severity (coefficient) | 5.22 [3.04, 7.40] <.001 | 5.47 [3.24, 7.69] <.001 | −.10 [−2.20, 2.00] .924 |
| Wave 2 (90–240 days) | |||
| Anxiety disorder (OR) | 1.04 [.54, 2.01] .903 | 1.19 [.60, 2.33] .620 | .73 [.34, 1.58] .430 |
| Depressive disorder (OR) | 1.70 [1.00, 2.91] .052 | 1.68 [.97, 2.91] .065 | .50 [.24, 1.03] .061 |
| Depression severity (coefficient) | 5.99 [2.88, 9.09] <.001 | 5.67 [2.54, 8.80] <.001 | .03 [−3.00, 3.07] .983 |
Nested logistic regression models found that the odds ratio of a SCID anxiety disorder diagnosis were statistically non-significant, alone (95% CI = [.67, 1.64], p = .848), when accounting for age, gender, and type of trauma (95% CI = [.65, 1.62], p = .925), and when additionally controlling for CAPS total severity score (95% CI = [.72, 1.94], p = .514) (Table 3).
In the nested linear regression model, ICD-11 classification raised BDI scores on average by 5.22 points over ICD-10 only cases (95% CI = [3.04, 7.40], p <.001). When accounting for age, gender, and type of trauma, ICD-11 cases had on average a BDI that was 5.47 points higher than ICD-10 only cases (95% CI = [3.24, 7.69], p < .001) . However, the addition of CAPS total severity score rendered the difference between ICD classifications non-significant (95% CI = [−2.20, 2.00], p = .924) (Table 3).
Nested Regressions: Wave 2
As seen in Table 3, in the nested logistic regressions, the models found that the odds of a SCID depressive disorder diagnosis in ICD-11 PTSD cases were 1.70 times higher than in ICD-10 only cases, but were statistically non-significant (95% CI = [1.00, 2.91], p =.052). When accounting for age, gender, and type of trauma, the ICD-11 PTSD cases still had 1.68 times odds of a SCID depressive disorder diagnosis than ICD-10 only cases, but the odds ratio were again statistically non-significant (95% CI = [.97, 2.91], p = .065). After the inclusion of CAPS total severity score, the odds ratio remained statistically non-significant (95% CI = [.24, 1.03], p = .061).
In nested logistic regression models estimating the odds of anxiety disorders, the crude odds ratio for ICD classification was non-significant (95% CI = [.54, 2.01], p = .903). When accounting for age, gender, and type of trauma (95% CI = [.60, 2.33], p = .620), and when additionally accounting for CAPS total severity score (95% CI = [.34, 1.58], p = .430), the odds ratio remained non-significant (Table 3).
In the nested linear regression model, ICD-11 classification raised BDI scores on average by 5.99 points over ICD-10 only cases (95% CI = [2.88, 9.09], p <.001). When accounting for age, gender, and type of trauma, ICD-11 PTSD cases still scored on average 5.67 points higher on the BDI than ICD-10 only PTSD cases (95% CI = [2.54, 8.80], p < .001). However, the addition of CAPS total severity score to the model resulted in the coefficient of ICD-11 classification becoming non-significant (95% CI = [−3.00, 3.07], p = .983) (Table 3).
Discussion
This study used the ICD-10 and ICD-11 PTSD diagnostic criteria to examine differences in co-occurring depressive and anxiety disorders when using different operational definitions of PTSD, either including or excluding dysphoric symptoms. Participants were injury survivors assessed during two time intervals following recent trauma exposure. Our results showed that participants identified by the restricted ICD-11 criteria were equally or more likely to have a diagnosable depressive or anxiety disorder than those identified by the ICD-10 overall as well as by the ICD-10 alone. ICD-11-identified participants also reported significantly higher depression severity. Importantly, the differences in depression severity were accounted for by ICD-11 higher PTSD symptom severity.
Our results expand upon previous studies showing equal or higher rates of comorbidity in individuals identified by the ICD-11 criteria as having prolonged PTSD (Gluck et al., 2016; Hafstad et al., 2017; Wisco et al., 2016) by using repeated assessments in the early post-exposure period as well as the persistent period, which illustrates the ICD-11’s performance at successive stages following trauma exposure. Our results differ, however, from studies showing lower comorbidity among ICD-11-identified individuals (Hyland et al., 2016; O’Donnell et al., 2014; Stammel, Abbing, Heeke, & Knaevelsrud, 2015), with differences perhaps explained by differences in sample characteristics (e.g., accident survivors vs. war survivors, acute vs. chronic PTSD) and diagnostic tools (e.g., clinician-administered vs. self-report).
The ICD-11 Working Group states that “disorders specifically associated with stress have … key characteristics: they are identifiable on the basis of different psychopathology that is distinct from other mental disorders” (Maercker et al., 2013), implying that disorders associated with stress, as opposed to other anxiety and depressive disorders, are fundamentally different. Our results do not support this postulation. Participants identified by the ICD-11, a putatively more stressor-specific template, had equal depression and anxiety comorbidity and higher depression severity despite removing these symptoms from the ICD-11 PTSD diagnostic criteria.
The substantially higher PTSD severity among ICD-11 cases compared to the ICD-10 only cases presumably accounts for the heightened depression severity among the former group. Consistent with this assumption, a linear regression revealed that within the study sample, CAPS total severity was associated with depression severity after controlling for gender, trauma type, and ICD classification. This explanation is in line with previous research showing that distress is predictive of depression in individuals with PTSD: Byllesby and colleagues (Byllesby et al., 2017) found that general distress accounts for the shared variance between MDD and PTSD, rather than the Negative Alterations in Cognition and Mood (NACM) symptoms in the DSM-5. Their results also indicated that NACM symptoms (i.e., “non-specific” symptoms) were “no more related to depression than intrusion, avoidance, or arousal factors” (Byllesby et al., 2017). This finding suggests that removing affective and cognitive symptoms from the PTSD diagnostic criteria does not reduce co-occurring depressive diagnoses, as evidenced by the present study. Furthermore, a study by Mitchell and colleagues (Mitchell et al., 2017) used a network analysis to infer the most central symptoms to individuals with PTSD only and individuals with comorbid PTSD and MDD and found that persistent negative emotional state and inability to experience positive emotions were among the six most central symptoms to individuals with PTSD only. These results imply that “non-specific” symptoms are predominant in PTSD.
There were some limitations to the study. First, the participants in this study were not originally evaluated for ICD-10 or ICD-11 PTSD, and the measure used to derive these diagnoses was based on the DSM-IV dedicated questionnaire. Notably, the ICD-11 has put a greater emphasis on the sense of “nowness” compared to previous diagnostic criteria, which may affect the similarity of DSM-derived re-experiencing symptoms to those of ICD-11. In this study, we attempted to capture the sense of “nowness” with the inclusion of CAPS item B3, which asks whether patients feel or act as if the trauma were reoccurring at the time of the intrusive memory (Table 1). In order not to exclude intense intrusive memories themselves, we also included CAPS item B1, which inquires about memories specifically (Table 1). Unfortunately, we do not know to what extent participants experienced intrusive memories in the present, but rather only the reported intensity. At this point, however, items on the CAPS have been largely used and accepted in the approximation of ICD symptom criteria (e.g., Barbano et al., 2018; O’Donnell et al., 2014; Wisco et al., 2016).
Second, this study relied on available data, which in some cases were not all-inclusive. SCID data in this study did not include subthreshold disorders; the rates of co-occurring subthreshold anxiety and depressive disorders among this cohort are therefore unclear. However, available data provided a comprehensive report of those meeting criteria for co-occurring, positively endorsed disorders. Additionally, valid data on generalized anxiety severity were not available, precluding analysis of generalized anxiety severity.
Third, this study included longitudinal studies in which many participants did not fulfill the minimum three-week duration criterion for ICD-11 in the first wave of data collection. Therefore, though indicative of differences in comorbidities during the important post-trauma phase, ICD-11 diagnoses cannot be entirely validated during this time interval.
Fourth, the scope of the study sample may limit the generalizability of the findings. All participants were recruited from ERs or intensive care units, with over 80% having experienced a motor vehicle accident as their precipitating event. The rates of co-occurring depression and anxiety disorders may vary in patients with prolonged, repeated, or interpersonal traumas. Additionally, participants who were lost to follow-up had overall higher CAPS scores than those who were not lost to follow-up. Therefore, participants with more severe PTSD may have been underrepresented in the second wave of data collection.
Finally, this study did not evaluate the rate of comorbidities in participants identified as having complex PTSD, a new diagnostic category whose criteria include all ICD-11 PTSD diagnostic criteria as well as several affective, cognitive, and interpersonal dysfunctions (World Health Organization, 2018b). Complex PTSD is typically diagnosed after prolonged or repeated traumatic exposure, such as childhood abuse, slavery, captivity, or domestic violence (Cloitre, Garvert, Brewin, Bryant, & Maercker, 2013), whereas the current study sample was comprised of single traumatic events precipitating an ER visit. However, because this study did not assess lifetime trauma exposoure (including childhood trauma), it is possible that some participants meeting ICD-11 PTSD criteria would have better fit the ICD-11 definition of complex PTSD.
Despite ICD-11 attempts to simplify the diagnosis of PTSD by limiting symptoms to direct responses to the event, posttraumatic psychopathology remains a mélange of core PTSD symptoms and dysphoria. As such, clinicians may wish to note that whether or not anxiety and depressive symptoms are assessed by PTSD criteria, patients with PTSD are likely to experience these aspects of psychological distress, particularly those patients with more severe PTSD symptomatology. Our results also showed that these symptoms were present during the initial responses to trauma as well as during early persisting PTSD. Therefore, care providers may need to monitor depressive and anxiety symptoms in addition to core PTSD symptoms throughout long-term treatment plans.
Acknowledgments
We are grateful for the contributions of Paul O’Connor at the Nathan Kline Institute for his invaluable assistance in data management and quality assurance. This study was funded by the US Public Health Service research grant (MH101227) to Arieh Shalev, Ronald Kessler, and Karestan Koenen.
Footnotes
Disclosure Statement: Dr. Matsuoka reports personal fees from Morinaga Milk, Eli Lilly, and NTT Data. Over the past three years, Dr. Kessler received support for his epidemiological studies from Sanofi Aventis; was a consultant for Johnson & Johnson Wellness and Prevention, Sage Pharmaceuticals, Shire, Takeda; and served on an advisory board for the Johnson & Johnson Services Inc. Lake Nona Life Project. Kessler is a co-owner of DataStat, Inc., a market research firm that carries out healthcare research.
References
- Barbano AC, van der Mei WF, Bryant RA, Delahanty DL, deRoon-Cassini TA, Matsuoka YJ, . . . Shalev AY (2018). Clinical implications of the proposed ICD-11 PTSD diagnostic criteria. Psychol Med, 1–8. doi: 10.1017/S0033291718001101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory-II. Paper presented at the Psychological Corporation, San Antonio, TX. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a Clinician-Administered PTSD Scale. J Trauma Stress, 8(1), 75–90. [DOI] [PubMed] [Google Scholar]
- Brewin CR (2013). “I wouldn’t start from here”--an alternative perspective on PTSD from the ICD-11: comment on Friedman (2013). J Trauma Stress, 26(5), 557–559. doi: 10.1002/jts.21843 [DOI] [PubMed] [Google Scholar]
- Bryant RA, O’Donnell ML, Creamer M, McFarlane AC, & Silove D (2013). A multisite analysis of the fluctuating course of posttraumatic stress disorder. JAMA Psychiatry, 70(8), 839–846. doi: 10.1001/jamapsychiatry.2013.1137 [DOI] [PubMed] [Google Scholar]
- Byllesby BM, Elhai JD, Tamburrino M, Fine TH, Cohen G, Sampson L, . . . Calabrese JR (2017). General distress is more important than PTSD’s cognition and mood alterations factor in accounting for PTSD and depression’s comorbidity. J Affect Disord, 211, 118–123. doi: 10.1016/j.jad.2017.01.014 [DOI] [PubMed] [Google Scholar]
- Cloitre M, Garvert DW, Brewin CR, Bryant RA, & Maercker A (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: a latent profile analysis. Eur J Psychotraumatol, 4. doi: 10.3402/ejpt.v4i0.20706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Grubaugh AL, Kashdan TB, & Frueh BC (2008). Empirical examination of a proposed refinement to DSM-IV posttraumatic stress disorder symptom criteria using the National Comorbidity Survey Replication data. J Clin Psychiatry, 69(4), 597–602. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P). Paper presented at the Biometrics Research, New York: New York State Psychiatric Institute. [Google Scholar]
- Gluck TM, Knefel M, Tran US, & Lueger-Schuster B (2016). PTSD in ICD-10 and proposed ICD-11 in elderly with childhood trauma: prevalence, factor structure, and symptom profiles. Eur J Psychotraumatol, 7, 29700. doi: 10.3402/ejpt.v7.29700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafstad GS, Thorensen S, Wentzel-Larsen T, Maercker A, & Dyb G (2017). PTSD or not PTSD? Comparing the proposed ICD-11 and the DSM-5 PTSD criteria among young survivors of the 2011 Norway attacks and their parents. Psychol Med, 1. doi: 10.1017/S0033291717001568 [DOI] [PubMed] [Google Scholar]
- Haravuori H, Kiviruusu O, Suomalainen L, & Marttunen M (2016). An evaluation of ICD-11 posttraumatic stress disorder criteria in two samples of adolescents and young adults exposed to mass shootings: factor analysis and comparisons to ICD-10 and DSM-IV. BMC Psychiatry, 16, 140. doi: 10.1186/s12888-016-0849-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland P, Shevlin M, McNally S, Murphy J, Hansen M, & Elklit A (2016). Exploring differences between the ICD-11 and DSM-5 models of PTSD: Does it matter which model is used? J Anxiety Disord, 37, 48–53. doi: 10.1016/j.janxdis.2015.11.002 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry, 62(6), 617–627. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knefel M, & Lueger-Schuster B (2013). An evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse. Eur J Psychotraumatol, 4. doi: 10.3402/ejpt.v4i0.22608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maercker A, Brewin CR, Bryant RA, Cloitre M, Reed GM, van Ommeren M, . . . Saxena S (2013). Proposals for mental disorders specifically associated with stress in the International Classification of Diseases-11. Lancet, 381(9878), 1683–1685. doi: 10.1016/S0140-6736(12)62191-6 [DOI] [PubMed] [Google Scholar]
- Mitchell KS, Wolf EJ, Bovin MJ, Lee LO, Green JD, Rosen RC, . . . Marx BP (2017). Network models of DSM-5 posttraumatic stress disorder: Implications for ICD-11. J Abnorm Psychol, 126(3), 355–366. doi: 10.1037/abn0000252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell ML, Alkemade N, Nickerson A, Creamer M, McFarlane AC, Silove D, . . . Forbes D (2014). Impact of the diagnostic changes to post-traumatic stress disorder for DSM-5 and the proposed changes to ICD-11. Br J Psychiatry, 205(3), 230–235. doi: 10.1192/bjp.bp.113.135285 [DOI] [PubMed] [Google Scholar]
- Qi W, Ratanatharathorn A, Gevonden M, Bryant R, Delahanty D, Matsuoka Y, . . . Shalev A. o. b. o. t. I. (2018). Application of data pooling to longitudinal studies of early post-traumatic stress disorder (PTSD): the International Consortium to Predict PTSD (ICPP) project. Eur J Psychotraumatol, 9(1), 1476442. doi: 10.1080/20008198.2018.1476442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rytwinski NK, Scur MD, Feeny NC, & Youngstrom EA (2013). The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis. J Trauma Stress, 26(3), 299–309. doi: 10.1002/jts.21814 [DOI] [PubMed] [Google Scholar]
- Shalev A, Peri T, Brandes D, Freedman S, Orr S, & Pitman R (2000). Auditory startle response in trauma survivors with posttraumatic stress disorder: a prospective study. American Journal of Psychiatry, 157(2), 255–261. [DOI] [PubMed] [Google Scholar]
- Shalev AY, Ankri Y, Israeli-Shalev Y, Peleg T, Adessky R, & Freedman S (2011). Prevention of Posttraumatic Stress Disorder by Early Treatment: Results From the Jerusalem Trauma Outreach and Prevention Study. Archives of General Psychiatry, archgenpsychiatry. 2011.2127 v2011. [DOI] [PubMed] [Google Scholar]
- Shalev AY, Videlock EJ, Peleg T, Segman R, Pitman RK, & Yehuda R (2007). Stress hormones and post-traumatic stress disorder in civilian trauma victims: a longitudinal study. Part I: HPA axis responses. Int J Neuropsychopharmacol, 1–8. [DOI] [PubMed] [Google Scholar]
- Stammel N, Abbing EM, Heeke C, & Knaevelsrud C (2015). Applicability of the ICD-11 proposal for PTSD: a comparison of prevalence and comorbidity rates with the DSM-IV PTSD classification in two post-conflict samples. Eur J Psychotraumatol, 6, 27070. doi: 10.3402/ejpt.v6.27070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tay AK, Mohsin M, Rees S, Steel Z, Tam N, Soares Z, . . . Silove D (2017). The factor structures and correlates of PTSD in post-conflict Timor-Leste: an analysis of the Harvard Trauma Questionnaire. BMC Psychiatry, 17(1), 191. doi: 10.1186/s12888-017-1340-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2017). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; Retrieved from https://www.R-project.org/ [Google Scholar]
- Weathers FW, Keane TM, & Davidson JR (2001). Clinician-administered PTSD scale: a review of the first ten years of research. Depress Anxiety, 13(3), 132–156. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, & Keane TM (1999). Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment, 11, 124–133. [Google Scholar]
- Wisco BE, Miller MW, Wolf EJ, Kilpatrick D, Resnick HS, Badour CL, . . . Friedman MJ (2016). The impact of proposed changes to ICD-11 on estimates of PTSD prevalence and comorbidity. Psychiatry Res, 240, 226–233. doi: 10.1016/j.psychres.2016.04.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2018a). WHO releases new International Classification of Diseases (ICD 11). Retrieved from http://www.who.int/news-room/detail/18-06-2018-who-releases-new-international-classification-of-diseases-(icd-11)
- World Health Organization (2018b). ICD-11 for Mortality and Morbidity Statistics. Geneva. [Google Scholar]