Abstract
Chest radiography showed a right posterior mass on the mediastinum of an 84-year-old woman. The mass had been growing gradually for four years. Surgical excision was performed, and a pathological examination found the mass to be consistent with primary synovial sarcoma (SS) of the mediastinum. To our knowledge, this is a rare case in which follow-up imaging was able to be performed over a period of four years. This disease is aggressive, and its early diagnosis is key to achieving a cure. It is important to consider primary SS in the differential diagnosis of a primary intra-thoracic tumor, even if the tumor grows slowly.
Keywords: synovial sarcoma, mediastinum
Introduction
Synovial sarcoma (SS) mainly occurs in young adults at para-articular sites around the knee joint. Primary SS of the mediastinum is very rare (1). Imaging findings of this tumor type show a well-defined, homogeneous round or oval mass (2, 3). Calcification is identified in about 30% of cases of SS at the extremities (4) and about 5% of cases at the mediastinum (5). There are few reports about the long-term clinical course of SS.
We herein report a case of primary SS of the mediastinum with four years of follow-up. The tumor became huge, occupying approximately half of the right thorax and showing calcification. The interesting features of the case are the patient's advanced age, the site of origin, progress of calcification, and slow growth rate.
Case Report
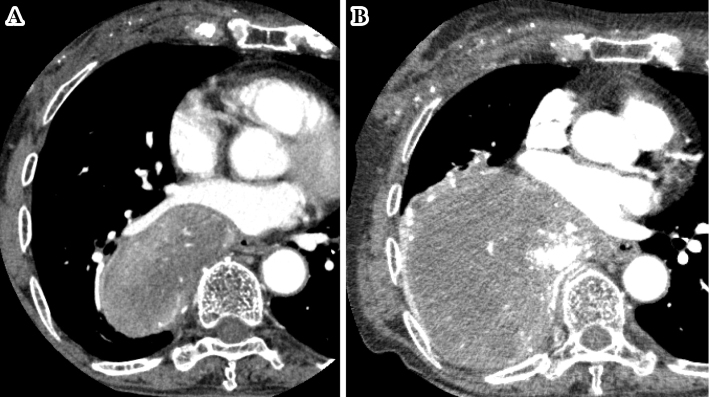
An 84-year-old woman was referred to our hospital because of discomfort in her back and edema of her left foot. Four years earlier, a right hilar mass had been detected during a routine annual medical checkup at another hospital. Chest computed tomography (CT) revealed a well-defined and heterogeneous oval mass measuring 11×8×5 cm in the right posterior mediastinum (Fig. 1A). One year later, necrotic changes and calcification appeared. However, the patient declined further investigation and treatment, and a follow-up imaging study was conducted without any treatment. Her medical and family history were unremarkable.
Figure 1.
Axial contrast-enhanced CT scan of the chest showing a large mass in the posterior mediastinum. A: initial presentation. B: four years later.
On referral to our hospital, the tumor markers SLX (sialyl SSEA-1) and ProGRP (pro-gastrin releasing peptide) were slightly elevated. Contrast-enhanced chest CT revealed a well-defined mass with heterogeneous enhancement and calcification in the right posterior mediastinum. The mass also exhibited cystic and necrotic areas. At that time, it measured 18×12×9 cm, displacing the esophagus and heart (Fig. 1B). T1-weighted magnetic resonance imaging (MRI) showed hyperintensity, which suggested hemorrhaging. On T2-weighted MRI, the tumor exhibited heterogeneous intensity, indicating necrosis and cystic degeneration. Whole-body fluororine-18 fluorodeoxyglucose positron emission tomography (FDG-PET) showed an abnormal uptake (standardized uptake value: 9.6) for this mediastinal mass. Based on these imaging findings, a solitary fibrous tumor was suspected.
The tumor parenchymal volume was measured by CT with the SYNAPSE VINCENT medical imaging system (Fujifilm Medical, Tokyo, Japan). The tumor grew slowly: the volume at the first visit was 205.9 mL, and that at the operation was 1012.1 mL. Thus, the volume doubling time (VDT) of the tumor in the present case was calculated to be 568 days. As the patient reported discomfort, she underwent surgical resection. Intraoperatively, the surface of the tumor was well circumscribed and whitish-gray in color. The tumor originated from the posterior mediastinum and firmly adhered not to the chest wall but rather to the right lower lobe of the lung. On a pathological examination, the tumor showed dense proliferation of spindle cells and traces of calcification (Fig. 2). Immunohistochemically, the tumors were diffusely positive for vimentin and bcl-2. These features suggested poorly differentiated monophasic synovial sarcoma. The SYT-SSX fusion gene transcript was detected by SYT-fluorescence in situ hybridization, leading to a final diagnosis of synovial sarcoma. We used a commercially available Vysis SS18 Break Apart Fluorescent in situ hybridization (FISH) probe Kit (Abbott, CHI, USA).
Figure 2.
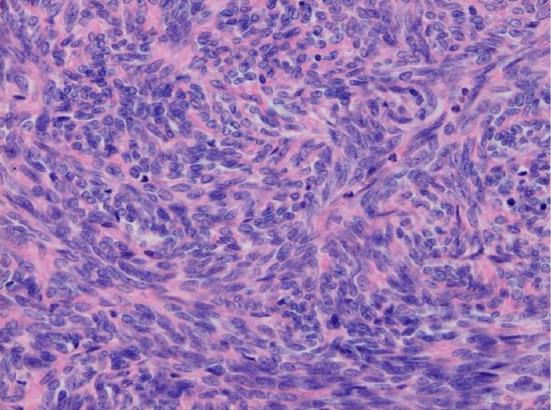
Microscopic findings showing the dense proliferation of spindle cells (Hematoxylin and Eosin staining, 200×).
The patient's postoperative course was free from complications. No adjuvant therapy was administered; only follow-up was performed. At seven months postoperatively, the patient is well without any signs of recurrence.
Discussion
Soft tissue sarcoma accounts for less than 1% of all malignancies according to surveillance in the United States (6). SS is the fourth-most common type of soft tissue sarcoma and mainly occurs in young adults at the extremities (1, 5). Thoracic cases account for <5% of SS cases, and primary SS of the mediastinum accounts for <10% of thoracic cases (1, 6, 7). The clinical course of SS is largely unclear. SS is cytogenetically characterized by a t(X;18)(p11;q11) translocation that results in the fusion of the SYT gene (8, 9).
The present case is significant for two reasons. First, we were able to perform follow-up imaging of the tumor for four years. Typically, malignant nodules have a VDT of approximately 100 days (10) compared to 568 days in the present case. Considering that the VDT of synovial sarcoma of soft tissue ranges from 50-200 days (11), the growth rate in the present case was very slow. The substantial amount of necrosis in this huge tumor might suggest that the lack of blood flow caused the slow growth. Second, CT imaging showed that the tumor exhibited progressive calcification. Calcification is identified in about 30% of SS at the extremities (4) and about 5% in cases at the mediastinum (5). In the present case, calcification appeared for one year. Calcification might have progressed because the tumor had an unusually prolonged course. Furthermore, SS of the mediastinum is rare in elderly people. The range of age at the diagnosis is wide, but the mean age is about 40 years (12). Mediastinal SS has a worse prognosis than SS in the soft tissue, lung and pleura (12). About half of patients die from this disease within 5 years, and even after surgery, local recurrence was reported to occur in over 80% of patients (7, 12). Therefore, an early diagnosis and multimodality treatment is essential to cure this disease. The slow growth of the tumor in the present case might have led to a misdiagnosis as a benign tumor. It is important to consider primary SS in the differential diagnosis of a primary intra-thoracic tumor (13).
In conclusion, we report a rare case of primary monophasic SS of the mediastinum with an unusually slow VDT and calcification progress in an elderly patient.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Cameron EWJ. Primary sarcoma of the lung. Thorax 30: 516-520, 1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang WD, Guan YB, Chen YF, Li CX. CT imaging of primary pleuropulmonary synovial sarcoma. Clin Radiol 67: 884-888, 2012. [DOI] [PubMed] [Google Scholar]
- 3.Matsuo Y, Sakai S, Yabuuchi H, et al. A case of pulmonary synovial sarcoma diagnosed with detection of chimera gene: Imaging findings. Clin Imaging 30: 60-62, 2006. [DOI] [PubMed] [Google Scholar]
- 4.Murphey MD, Gibson MS, Jennings BT, Crespo-Rodríguez AM, Fanburg-Smith JC, Gajewski DA. From the archives of the AFIP. Radiographics 26: 1543-1565, 2006. [DOI] [PubMed] [Google Scholar]
- 5.Lan T, Chen H, Xiong B, et al. Primary pleuropulmonary and mediastinal synovial sarcoma: a clinicopathologic and molecular study of 26 genetically confirmed cases in the largest institution of southwest China. Diagn Pathol 11: 1-14, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sultan I, Rodriguez-Galindo C, Saab R, Yasir S, Casanova M, Ferrari A. Comparing children and adults with synovial sarcoma in the Surveillance, Epidemiology, and End Results program, 1983 to 2005. Cancer 115: 3537-3547, 2009. [DOI] [PubMed] [Google Scholar]
- 7.Hartel PH, Fanburg-Smith JC, Frazier AA, et al. Primary pulmonary and mediastinal synovial sarcoma: a clinicopathologic study of 60 cases and comparison with five prior series. Mod Pathol 20: 760-769, 2007. [DOI] [PubMed] [Google Scholar]
- 8.Clark J, Rocques PJ, Crew AJ, et al. Identification of novel genes, SYT and SSX, involved in the t(X;18)(p11.2;q11.2) translocation found in human synovial sarcoma. Nat Genet 7: 502-508, 1994. [DOI] [PubMed] [Google Scholar]
- 9.Kawai A, Woodruff J, Healey JH, Brennan MF, Antonescu CR, Ladanyi M. SYT- SSX gene fusion as a determinant of morphology and prognosis in synovial sarcoma. N Engl J Med 338: 153-160, 1998. [DOI] [PubMed] [Google Scholar]
- 10.Revel M, Lefort C, Bissery A, et al. Pulmonary nodules: preliminary experience with three-dimensional evaluation. Radiology 231: 459-466, 2004. [DOI] [PubMed] [Google Scholar]
- 11.Nakamura T, Matsumine A, Matsubara T, Asanuma K, Uchida A, Sudo A. Clinical impact of the tumor volume doubling time on sarcoma patients with lung metastases. Clin Exp Metastasis 28: 819-825, 2011. [DOI] [PubMed] [Google Scholar]
- 12.Terra SBSP, Aesif SW, Maleszewski JJ, Folpe AL, Boland JM. Mediastinal synovial sarcoma: clinicopathologic analysis of 21 cases with molecular confirmation. Am J Surg Pathol 42: 761-766, 2018. [DOI] [PubMed] [Google Scholar]
- 13.Mirzoyan M, Muslimani A, Strrakian S, Swedeh M, Daw HA. Primary pleuropulmonary synovial sarcoma. Clin Lung Cancer 9: 257-261, 2008. [DOI] [PubMed] [Google Scholar]