Abstract
Background
There are currently no approved pharmacotherapies for managing methamphetamine dependence. N-acetylcysteine (NAC) has been found to reduce the craving for methamphetamine and other drugs, but its effect on methamphetamine use and other clinically related endpoints are uncertain. The N-ICE trial is evaluating the safety and efficacy of NAC as a take-home pharmacotherapy for methamphetamine dependence.
Methods/design
This is a two-arm parallel double-blind placebo-controlled three-site randomised trial (ratio 1:1) using permuted block randomisation, with variable block sizes. It is stratified by site, sex and whether the methamphetamine is injected or not. Participants (N = 180; 60 per site) need to be dependent on methamphetamine, interested in reducing their methamphetamine use and not currently receiving treatment for substance use disorders. The trial is being conducted in outpatient settings in Melbourne, Geelong and Wollongong, Australia. Participants will receive either 2400 mg oral NAC or a matched placebo, delivered as a take-home medication for 12 weeks. Two 600 mg capsules are self-administered in the morning and two more in the evening. Adherence is being monitored using eCAP™ medication bottle lids, which record the date and time of each occasion the bottle is opened. The primary outcome is methamphetamine use during the 12-week trial medication period, measured as (a) days of use, assessed using the timeline followback, and (b) methamphetamine-positive saliva tests, taken weekly. Secondary measures include weekly assessment of methamphetamine craving, severity of methamphetamine dependence, methamphetamine withdrawal symptoms and psychiatric symptoms (depression, suicidality, psychotic symptoms and hostility). Adverse events are monitored at each weekly assessment. Tolerability is assessed using the Treatment Satisfaction Questionnaire for Medication.
Discussion
The N-ICE trial is the first clinical trial to assess whether NAC can reduce methamphetamine use. This trial will improve our understanding of the potential utility of NAC in managing methamphetamine dependence and clinically related outcomes. If found to be effective, take-home NAC could be a potentially scalable and affordable pharmacotherapy option for treating methamphetamine dependence.
Trial registration
Australian and New Zealand Clinical Trials Registry, ACTRN12618000366257. Registered on 29 May 2018.
Electronic supplementary material
The online version of this article (10.1186/s13063-019-3450-0) contains supplementary material, which is available to authorized users.
Keywords: substance use disorders, methamphetamine, N-acetylcysteine, clinical trial, craving, withdrawal, psychosis, aggression, depression, suicide
Introduction
Methamphetamine (“ice”) use has become a global health concern [1] and methamphetamine dependence is now a major contributor to the burden of disease [2]. Hence, there is an urgent need for scalable and cost-effective treatment options [3]. However, currently there are no approved pharmacotherapies for treating methamphetamine dependence or withdrawal [3, 4], or its psychiatric sequelae [5, 6], with existing treatment options entirely reliant on psychosocial interventions [3]. Although these can provide a modest benefit [7, 8], they can be resource intensive to deliver [9] and are typically accessed by only a minority of consumers, particularly in rural and resource-poor settings [10, 11]. Pharmacotherapy may be a potentially scalable and cost-effective treatment option that could dramatically increase treatment coverage.
N-acetylcysteine (NAC) is a novel non-agonist pharmacotherapy that targets changes in glutamate function in the nucleus accumbens, which are thought to underpin drug craving and drug seeking [12]. NAC has been shown to reduce cravings for various drugs, including cocaine, tobacco, cannabis and methamphetamine [13]. However, evidence of reduced substance use is mixed [14, 15] and derives mainly from preclinical research and open-label and small-scale trials [16–18]. One small-scale crossover trial has demonstrated significant reductions in the craving for methamphetamine [19], but no trials have explored whether such reductions in cravings translate into clinically meaningful reductions in methamphetamine use amongst people who are dependent on the drug.
NAC may also convey a therapeutic benefit in managing the psychiatric sequelae associated with methamphetamine dependence. In addition to its potential for reducing drug cravings, pre-exposure to NAC reduces methamphetamine-related neurotoxicity [20]. These neurotoxic changes manifest as reduced dopamine and serotonin transporter density in the frontal, striatal and limbic regions [21, 22], which correlate with psychiatric symptoms, including hostility, in chronic methamphetamine users [23, 24]. Previous clinical trials have suggested that NAC can reduce psychiatric symptoms in the context of bipolar disorder, schizophrenia and major depression [25]. However, the potential therapeutic mitigation of psychiatric symptoms amongst people who use methamphetamine [26, 27] has not been explored.
NAC’s well-established safety profile means that it can be delivered as a take-home medication [28], making it a potentially scalable and cost-effective treatment option. It is no longer under any patent restrictions, further enhancing its roll-out and take-up. Known adverse reactions include gastrointestinal upsets and rash [29], which have not been significantly elevated relative to the placebo in current NAC trials for substance use disorders [30]. The seemingly generic effect of NAC on drug craving suggests that it may also be helpful in managing polysubstance dependence.
Aims and hypotheses
The aim of the current trial is to test the safety and efficacy of NAC as a pharmacotherapy for methamphetamine dependence using a double-blindplacebo-controlled randomised controlled trial. The trial will recruit 180 participants, who will receive either 12 weeks of oral NAC (2400 mg daily) or matched placebo. This is a phase IIb trial that is powered to confirm whether NAC has a clinically relevant benefit on methamphetamine use. The comparator condition is a matched placebo, with all participants provided with a minimal form of intervention (a self-help booklet), due to the lack of readily available standardised effective treatment options for methamphetamine use.
The primary hypothesis is that daily oral NAC delivered as a take-home medication will reduce methamphetamine use measured as (a) days of methamphetamine use and (b) methamphetamine-positive weekly saliva tests, during 12 weeks of active treatment relative to the placebo. The secondary hypotheses are that daily oral NAC delivered as a take-home medication will, relative to placebo:
reduce the severity of methamphetamine dependence, the craving for methamphetamine, methamphetamine withdrawal symptoms and psychiatric symptoms (depressive symptoms, suicidality, psychotic symptoms and hostility)
have an acceptable adverse event (AE) profile
not significantly increase the use of other substances (including alcohol, tobacco, cannabis, heroin and cocaine).
Methods/design
Design
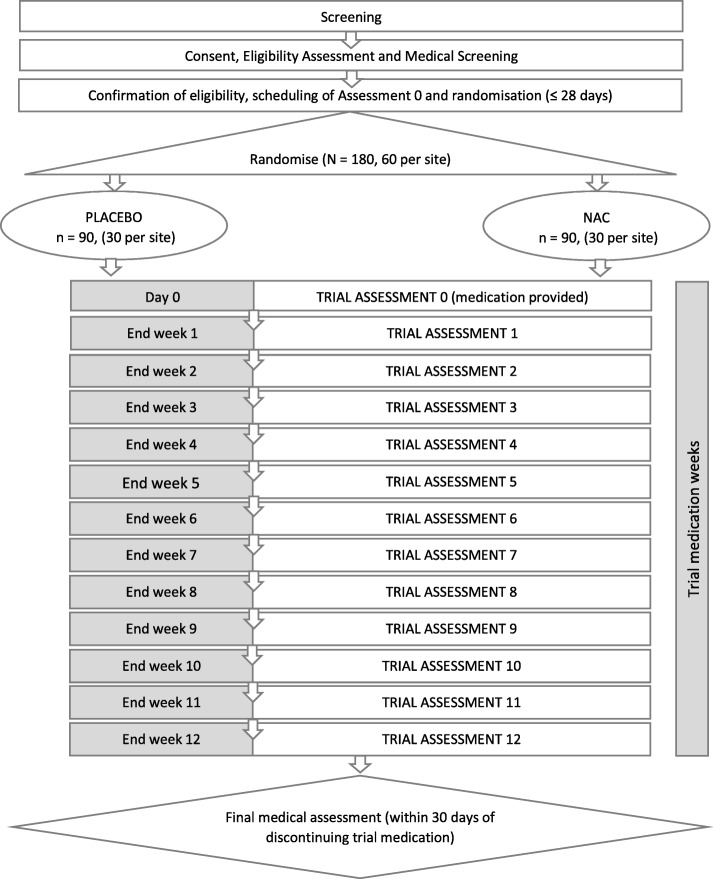
This is a three-site phase IIb randomised double-blindplacebo-controlledparallel-group trial. Participants will be recruited across three sites (N = 180; 60 per site) and randomly assigned (1:1) to receive either oral NAC 2400 mg daily or the placebo, for 12 weeks. Weekly assessments throughout the 12-week medication phase will be used to assess outcomes. The trial flow diagram is presented in Fig. 1. The trial protocol was developed in accordance with the Standard Protocol Items: Recommendations for Intervention Trials (SPIRIT) Statement (see Additional file 1 for the SPIRIT checklist).
Fig. 1.
Trial flow diagram. NAC N-acetylcysteine
Randomisation and blinding
Participants are randomised to the treatment or placebo arms in a 1:1 ratio using a permuted block randomisation schedule with variable block sizes, stratified by site (Melbourne, Geelong or Wollongong), gender (male or female) and main route of methamphetamine administration in the month prior to recruitment (injecting or not injecting). The randomisation sequence was generated a priori using an in-house custom program written by WL. A random seed, assigned by the data and safety monitoring board (DSMB) statistician, was used to generate the final randomisation schedule using this program. Allocation to treatment condition (placebo vs. NAC) is based on the participant’s unique study identifier, this being assigned by trial staff sequentially within each stratum on randomisation.
All trial staff, the trial statistician (WL) and investigators are blind to treatment allocation. The randomisation schedule is held by the trial site pharmacy and the DSMB statistician. Allocation to trial arm is done by the trial pharmacist according to the randomisation schedule (provided by the DSMB statistician) using the unique study identifier provided by the trial staff. Packaging is identical to conceal treatment allocation. A removable adhesive label indicates whether the medication is placebo or NAC.
Unblinding is done at the discretion of the DSMB, the trial investigators or the treating medical physician in a medical emergency. Trial investigators can unblind individual participants via a password-protected online portal.
Setting and study population
Participants are being recruited via outpatient settings in Melbourne (Turning Point and Eastern Health), Geelong (Barwon Health) and Wollongong (Illawarra Drug and Alcohol Service) in Australia. All participants are volunteers. They provide written informed consent prior to participation (see Additional file 2 for the participant information sheet and consent form). Inclusion criteria are that participants must be aged 18–60 years, meet DSM-IV criteria for methamphetamine dependence, be seeking to reduce their methamphetamine use but are not currently undergoing substance use treatment (including pharmacotherapy for substance use disorders), are not in need of acute care for psychiatric or other medical conditions, do not have a primary psychotic disorder, are able and willing to comply with the trial protocol, and have no contraindications for NAC. Contraindications for receiving the trial medication include: previous hypersensitivity to NAC; use of medications containing NAC or thought to be hazardous if taken with NAC (e.g. carbamazepine and nitroglycerin); a known or suspected active systemic medical disorder including cancer or other medical condition that may exacerbate the risk of AEs from NAC (recent gastrointestinal ulcers or renal stones, epilepsy or history of seizures, asthma or atopy); and, surgery within the past 28 days. Further, participants must not be pregnant (confirmed at the eligibility assessment), lactating or planning to fall pregnant during the trial.
Intervention
Randomised participants will receive 2400 mg per day of oral NAC or a matching placebo (microcrystalline cellulose), taken as two 600 mg capsules every morning and evening for 12 weeks. The trial medication is supplied by Pharmaceutical Packaging Professionals (PPP) Pty Ltd. It is encapsulated in white capsules, size 00, and bottled in identical 200 cm3 white round plastic wide-mouth packer bottles (2.3 in. in diameter and 4.3 in. in height) fitted with eCAP™ lids (see Adherence). As a minimal intervention, all randomised participants are provided with a complementary self-help booklet, On Ice (National Drug and Alcohol Research Centre, University of New South Wales).
Schedule of activities and study procedures
The trial flow diagram (Fig. 1) shows the schedule of activities.
Recruitment and screening
Participants are recruited through advertisements (e.g., Facebook, media activity, and flyers in needle and syringe programs) and word of mouth. They are screened by phone. Potentially eligible participants are consented by trial staff and then undergo a face-to-face eligibility assessment (1.5 to 2 h in total) to confirm their eligibility and to obtain information on demographics, drug use and psychiatric history. All participants undergo a medical assessment to confirm further their eligibility prior to randomisation. Randomisation must occur within 28 days of eligibility being confirmed. Eligible participants are provided with a list of local health service providers and are free to access drug treatment and other health services during the trial. Ineligible participants are offered referral to local alcohol and other drug services.
Assessments
The eligibility assessment and assessment 0 are conducted at the trial site clinic. Weekly assessments (assessments 1–12) are scheduled thereafter (with a leeway of −2 days to +4 days). These may be done at a public venue convenient to the participant (e.g., a café or shopping mall) to enhance retention. They take around 40 min each. Detailed contact information is collected on all participants and text message reminders are sent prior to appointments to enhance follow-up rates. Saliva samples are taken at each of the follow-up assessments using a Quantisal Oral Fluid Collection Device™. Participants undergo a final medical assessment within 30 days of completing the trial or on discontinuation of their medication. All participants are provided with referral information for alcohol and other drug treatment services at the close of the study.
Trial medication
Trial medication bottles are distributed to the trial site pharmacy in batches. On dispensing, the adhesive label indicating treatment allocation is removed by the pharmacist and placed in the participant’s pharmacy file. Trial medication is provided to the trial researcher who delivers the medication to the participant at assessment 0. Medication bottles are replaced at 3-week intervals. Participants are provided with feedback on their medication adherence at each assessment using eCAP™ technology (Med-ic eCAP™, Information Mediary Corp, see Adherence for details). The number of capsules remaining in each medication bottle is audited on return.
Safety monitoring
AEs are recorded by trial research staff at each assessment and reviewed by the trial physician. Face-to-face medical assessments are scheduled for all severe and serious adverse events (SAEs), and also at the discretion of the trial physician or at the request of the participant. Any ongoing AEs at the end of the trial are followed for at least 7 days, and ongoing SAEs for at least 30 days, with all AEs followed until stabilisation or resolution. All participants are entitled to compensation in accordance with the Medicines Australia Compensation Guidelines.
Discontinuation of medication and withdrawal from the trial
Participants are free to discontinue the trial medication or withdraw from the study at any time. Investigators may discontinue trial medication or withdraw a participant from the trial for the following reasons: pregnancy, no longer meeting the inclusion criteria, failing to take the medication for 7 or more days, significant non-compliance with the study protocol, disease progression that requires discontinuation of the trial medication or a clinical condition for which it would not be in the best interest of the participant to continue taking the trial medication. Follow-up assessments are completed regardless of medication discontinuation for all participants who remain consented into the study.
Endpoints and assessments
Measures and measurement time points are presented in Table 1.
Table 1.
Measures taken at each assessment
| Eligibility Assessment | Weekly trial assessments | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
| Demographics, drug use history, CIDI (methamphetamine dependence), MINI (depression, psychotic disorders and mania), DIP (family history of psychotic disorders), RCQ, BCIS, BIS items, SAPAS | x | |||||||||||||
| Saliva samples | x | x | x | x | x | x | x | x | x | x | x | x | ||
| TLFB for days of methamphetamine use | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| Days of other substance use | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| Adverse events | x | x | x | x | x | x | x | x | x | x | x | x | ||
| Concomitant medications | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Concomitant treatment | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| SDS | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| CEQ | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| AWQ | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| BPRS items | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| WPAI-GH | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| EQ-5D-5L | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Health service use and criminal justice involvement | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| TSQM | x | x | x | |||||||||||
CIDI Composite International Diagnostic Interview, MINI Mini International Neuropsychiatric Interview, DIP Diagnostic Interview for Psychosis, RCQ Readiness to Change Questionnaire, BCIS Beck Cognitive Insight Scale, BIS Birchwood Insight Scale, SAPAS Standardised Assessment of Personality – Abbreviated Scale, TLFB timeline followback, SDS Severity of Dependence Scale, CEQ Craving Experience Questionnaire, AWQ Amphetamine Withdrawal Questionnaire, BPRS Brief Psychiatric Rating Scale, WPAI-GH Work Productivity and Activity Impairment Questionnaire – General Health V2, EQ-5D-5L Five-dimension five-level version of EuroQol questionnaire, TSQM Treatment Satisfaction Questionnaire – Medication
Primary endpoint
The primary outcome is methamphetamine use. There are two measures of this endpoint:
Days of methamphetamine use during the 12-week active medication phase, assessed using the timeline followback method (TLFB) [31] and updated weekly. The outcome measure is the percentage of days on which methamphetamine is used during the 28 days prior to assessments 4, 8 and 12. The TLFB has 88% sensitivity, 96% specificity and 0.77 test–retest agreement for the use of amphetamines in the past 30 days [31].
The number of methamphetamine-positive saliva samples taken at assessments 1–12. Saliva is collected with an Alere Quantisal Oral Fluid Collection Device™ and the presence of methamphetamine confirmed using mass spectrometry with a detection cut-off of >25 mg/L.
Secondary endpoints
All secondary outcomes are assessed for the past week at assessments 0 to 12.
Methamphetamine craving
Methamphetamine craving is assessed using the total score on the Craving Experience Questionnaire (CEQ), which has been validated for various substances [32]. The original CEQ has ten items: three items corresponding to the urge to use the substance, three items corresponding to intrusive thoughts and four items corresponding to the sensory aspects of substance use (e.g., picture, taste, smell and feel). The sensory items were adapted for methamphetamine and combined into three items: (1) taste and smell combined, (2) picturing methamphetamine and (3) imagining what it would feel like to smoke or inject it. This gave a total of nine items, each with scores ranging from 0 to 10 with higher scores representing a more severe craving.
Severity of methamphetamine dependence
The severity of methamphetamine dependence is assessed using the total score on the Severity of Dependence Scale (SDS) [33]. The SDS is a five-item scale that yields scores from 0 (no dependence) to 15 (most severe dependence). It has good internal consistency for amphetamine use (Cronbach’s alpha from 0.81 to 0.89) [33] and has been validated against a diagnosis of severe amphetamine dependence using the Composite International Diagnostic Interview (CIDI) [34].
Methamphetamine withdrawal symptoms
Methamphetamine withdrawal symptoms are assessed using the total score on the Amphetamine Withdrawal Questionnaire (AWQ) [35]. The AWQ is a ten-item questionnaire that rates various symptoms associated with amphetamine withdrawal on a five-point Likert scale. Scores range from 0 to 40 with higher scores indicating higher severity. The AWQ has a test–retest reliability of 0.79 and has been validated against other measures of withdrawal [35].
Psychiatric symptoms
Psychiatric symptoms are assessed using the Brief Psychiatric Rating Scale (BPRS) [36]. Symptom domains are rated against anchor points from 1 (nil) to 7 (extremely severe). Scores of 4 or greater indicate symptoms of clinical significance or pathological intensity. The BPRS has an inter-rater reliability of 0.83 when quality assurance procedures are followed [37]. The following endpoint definitions were used:
Psychotic symptoms: A score of 4 or greater on any of the BPRS items of suspiciousness, unusual thought content and hallucinations
Hostility: A score of 6 or 7 on the BPRS hostility item
Depression: A score of 4 or greater on the BPRS depression item
Suicidality: A score of 4 or more on the BPRS suicidality item
Other assessments
Polysubstance use
The polysubstance use measure is the percentage of days using drugs from other classes (tobacco, alcohol, cannabis, cocaine, ecstasy, hallucinogens, inhalants and heroin) for the 28 days prior to assessments 0, 4, 8 and 12, assessed weekly using the TLFB, and averaged across drug types.
Adverse events
AEs will be assessed at each weekly assessment using open-ended questions and may include any other events that come to the attention of the trial staff during the trial. The outcome will be the number and percentage of participants reporting AEs and SAEs by System Organ Classification, coded according to the Medical Dictionary for Regulatory Activities. AEs will be counted once only for a given participant. The event counted will be the event with the highest severity (coded mild, moderate or severe).
Adherence
eCAP™ (Med-ic eCAP™, Information Mediary Corp) will be used as an objective measure of medication adherence. eCAP™ lids fitted to the medication bottles used record the times when a bottle is opened, which are downloaded at each assessment using a near-fieldcommunication-enabled smartphone and on bottle return using a CertiScan RFID desktop Reader (Med-ic Certiscan Version 2.5.1; Information Mediary Corp 2014–2018). Adherence will be the percentage of compliant doses, based on bottle opening, with dosing timeframes being morning (until 12 noon) and night (until midnight), or equivalent 12-h intervals.
Treatment satisfaction
The Treatment Satisfaction Questionnaire for Medication (TSQM) [38] will be completed at assessments 4, 8 and 12.
Concomitant treatments
All medications, including supplements, taken during the trial and all treatments related to either substance use or other mental health conditions received during the trial will be recorded on a template adapted from the National Institutes of Health’s concomitant medications form [39].
Health Economics
Data for costing are being collected to facilitate a subsequent economic evaluation of the intervention. These costing data include the EuroQol (EQ-5D-5L) [40] version 2.1, the Work Productivity and Activity Impairment Questionnaire – General Health V2 (WPAI-GH), and health service use and contact with the criminal justice system, which are assessed using a structured questionnaire. The data are updated weekly throughout the 12-week trial medication period.
Demographics, drug use and psychiatric history
Demographics, drug use and psychiatric history data are collected at the eligibility assessment. Demographics and drug use questions are based on the Opiate Treatment Index [41] and previous drug treatment trials [42], and include days of use for all major drug types in the past month. Current DSM-IV methamphetamine dependence is confirmed using CIDI [43]. The Mini International Neuropsychiatric Interview (MINI) [44] for Schizophrenia and Psychotic Disorders Studies, English Version 7.0.1, is used to screen for psychotic and affective disorders. Other measures include family history of psychotic disorders, assessed using the Diagnostic Interview for Psychosis (DIP) [45], the Readiness to Change Questionnaire (RCQ) [46], the Beck Cognitive Insight Scale (BCIS) [47], four items from the Birchwood Insight Scale (BIS) [48], and the Standardised Assessment of Personality – Abbreviated Scale (SAPAS) [49].
Governance and ethical considerations
Quality control
All trial researchers will receive training in the trial assessment procedures. BPRS ratings are reviewed weekly, and a selection of ratings (10%) are audio-recorded and rated by an independent trained BPRS rater to establish inter-rater reliability. Primary endpoints are double entered. Weekly researcher meetings and monthly investigator meetings are held to monitor recruitment, follow-up, data collection and other trial procedures. A delegate from the coordinating sponsor institution (Curtin University) is responsible for conducting site visits (prior to initiation, during the trial and at trial completion) to audit compliance with the protocol and the accuracy and completeness of the data.
Data safety and monitoring board
The DSMB meet at least semi-annually and include individuals with expertise in the clinical topic area (methamphetamine and other substance use disorders), randomised clinical trials and biostatistics. The current DSMB also includes a consumer/community representative. The role of the DSMB is to review participant safety, recruitment, accrual, retention and withdrawal. The DSMB can recommend trial suspension, modification or discontinuation.
Data management
Personal information obtained from participants is stored securely and separately from trial data at the trial site and is accessible only to trial staff from that site. Participants’ trial data are de-identified using a unique study identifier. Saliva samples are de-identified and destroyed after analysis. De-identified trial data are entered onto a centralised secure (password protected) online electronic database, Research Electronic Data Capture (REDCap), which is hosted on a secure Curtin University server. De-identified trial data are available to all trial investigators. All analyses are based on de-identified data and will be published in a way that participants cannot be individually identified. Trial participants will be provided with a summary of their results at the close of the study. Otherwise, trial data are confidential and will be released in identified form only with the permission of the participant or as required by law. Trial data will be stored securely for 15 years after study completion; destruction of study material thereafter will be in accordance with local ethics approvals.
Ownership and publication
The ownership and permissions relating to the trial data are managed under a multi-institutional contractual agreement between the study sponsors, which is available on request from RM. The decision to publish information from the study will be made jointly by the trial investigators. Authorship will be in accordance with the guidelines of the International Committee of Medical Journal Editors. There are no other restrictions on the publication of trial results.
Governance and ethics
The N-ICE trial (Universal Trial Number U1111–1210-1224) has been registered prospectively with the Australian and New Zealand Clinical Trials Registry (ACTRN12618000366257) and has been approved by all relevant human research ethics committees: Eastern Health (E21–2017), Barwon Health (17/202), the University of Wollongong and Illawarra Shoalhaven Local Health District Health (2017/549) and Curtin University (HRE2018–0205). The trial is funded by the National Health and Medical Research Council (NHMRC) under project grant 1128147 and is run under a co-sponsor arrangement between the participating institutions and the trial sites. The participating institutions are Curtin University, Deakin University, the University of Wollongong, Monash University, the Burnet Institute, La Trobe University and the University of Newcastle. Curtin University is the lead coordinating institution (National Drug Research Institute, Curtin University, GPO Box 1987, Perth WA 6845; phone +61 89,266 1602, facsimile +61 89,266 1611). The trial sites are in Melbourne (Turning Point and Eastern Health), Geelong (Barwon Health) and Wollongong (Illawarra Drug and Alcohol Service). Oversight is provided by an independent DSMB, which operates under a charter agreed by the DSMB members (available on request from RM). Curtin University coordinates the overall conduct of the trial, including communication with the DSMB, and monitors the study at all sites to ensure compliance with the protocol. Each site is individually responsible for ensuring compliance with good clinical practice and site-specific ethics protocols, including communicating any changes of the trial protocol to local governance authorities and participants.
Statistical considerations
Sample size estimation
The sample size of 90 participants per treatment arm is designed to detect a mean between-group difference of 3.5 days versus 6.0 days of methamphetamine use per month during the 12-week trial medication period with at least 80% power at p < 0.025 (0.05 / 2 to accommodate two primary outcome measures) and with 20% attrition (i.e., a final sample of at least 72 participants per treatment arm). The expected effect size is based on data from the Methamphetamine Treatment Evaluation Study (MATES) [42]. Participants who did not receive treatment in that cohort showed a reduction in methamphetamine use from a mean (standard deviation) of 12.8 (7.4) days per month at baseline to 6.0 (6.7) days per month at the 12-weekfollow-up. Our estimate of a minimal clinically meaningful reduction in use is based on outcomes for outpatient counselling derived from MATES: 11.2 (8.8) days per month to 3.5 (6.9) days per month at 12 weeks. Our estimate of 20% attrition is based on our previous research [42, 50, 51]. No interim analyses are planned. Statistical power was estimated using the SAMPSI command in Stata (Version 14.2, StataCorp LLC, College Station, Texas).
Efficacy analysis
All tests will be two-sided with significance set at p < .025 for each of the two primary endpoints and p < .01 for each of the secondary endpoints. Significance for all other tests will be set at p < .05. The analyses will be conducted blind to condition.
Analysis of primary outcomes
Intention-to-treat analyses will be conducted for the primary outcomes. The effect of the trial medication on days of methamphetamine use (percentage of days used in the past 28 days) will be tested using a baseline (assessment 0) vs. medication phase (three repeats: assessments 4, 8 and 12) by treatment condition (NAC vs. placebo). Unobserved days (e.g., due to hospitalisation or incarceration) will be censored. The effect of NAC on methamphetamine-positive saliva will be tested using a main effect for treatment condition (NAC vs. placebo) on saliva test results (positive vs. negative) from assessments 1–12 (12 repeats).
Analysis of secondary outcomes
Analysis of secondary outcomes will be based on a modified intention-to-treat dataset that includes only participants who completed assessment 0 and at least one follow-up assessment (i.e., assessments 1–12). The effect of NAC on each secondary outcome will be tested using a baseline (assessment 0) vs. medication phase (assessments 1–12) by treatment condition (NAC vs. placebo) interaction.
All effects will be tested with mixed effects models with repeated measures for each measurement time point. Heterogeneity in variance and treatment effect between sites will be tested for by seeing whether the model fit is significantly improved by including a random intercept for site and a random coefficient for the main effect by site, respectively. If no significant heterogeneity is found, the more parsimonious model will be retained. Missing data will be imputed using multiple imputation by chained equations implemented in Stata in the analysis of the primary outcomes only. Final details of the analysis, including methods of imputation and covariates, will be outlined in a statistical analysis plan prior to unblinding of the data. An additional statistical plan for a health economic evaluation will be developed prior to undertaking any such analysis.
Discussion
The N-ICE trial is the first randomised controlled trial to assess the efficacy of NAC as a pharmacotherapy for methamphetamine dependence. It will test whether NAC can produce a clinically meaningful reduction in methamphetamine use. It will assess whether there are any beneficial effects of NAC on related clinical endpoints, including psychiatric symptoms, and it will document adherence to NAC and the safety profile of NAC as a take-home medication in this population. Thus, the trial will improve our understanding of the potential utility of NAC in clinical practice to reduce methamphetamine use.
One clear potential benefit of NAC, if it is found to be safe and effective, is that it can be administered as a take-home medication, making it a potentially scalable and cost-effective treatment option. A significant impediment to the benefits of NAC, or any other take-home medication, would be poor compliance with dosing regimens. Thus, we are using electronic monitoring (eCAP™) to record the time and date of each occasion a bottle is opened to provide an objective measure of adherence. Electronic monitoring through devices such as eCAP™ is a relatively recent technological development [52] that has not yet been widely adopted in medication trials for illicit substance use. This technology will provide important data on the viability of prescribing take-home medications in illicit substance-using populations and it will also allow us to assess the implications of sub-optimal dosing on treatment effects and safety in this population.
Novel aspects of our trial procedures are the direct community engagement strategy to recruit participants and the outreach methods for follow-up assessments within the community, in so far as these are practical and safe. We have taken this approach because most people who are dependent on methamphetamine do not engage with specialist drug treatment services [53], and this has made recruitment to and retention in stimulant pharmacotherapy trials difficult [54]. Rather than relying on recruiting patients from existing clinical services and requiring that trial participants come to fixed sites for treatment, we use well-honed fieldwork methods that have been successfully applied in survey and cohort research involving people who use methamphetamine [42, 50, 55]. We hope that the implementation of these outreach methods within the clinical trial framework will increase engagement with consumers and improve retention.
A challenge that we faced in developing this trial protocol was the lack of standardised and readily available evidence-based treatment options for methamphetamine dependence. This precluded a treatment comparison arm or the provision of treatment as usual to trial participants. Instead, we provide all participants with a form of minimal intervention (an information booklet) and referral information for health services, which they are free to access throughout the trial period. To counter the risk of bias from concomitant treatment, we record all concomitant medications and psychosocial treatments for substance use and other mental health problems. We will compare treatment arms on these exposures and, where differences exist, we will adjust for these in the main analysis.
In summary, this trial is important because it tests a novel, affordable, available and tolerable non-agonist pharmacotherapy option for methamphetamine dependence, which, if effective, has the potential to be a much-needed, cost-effective and scalable treatment option for this population. NAC has the potential to be prescribed by primary health-care providers as a take-home medication and used as an adjunct to existing drug treatments. The lack of patent restrictions and its current availability as a prescription medication and dietary supplement will facilitate its uptake. Given the lack of approved medications currently available for managing methamphetamine dependence [3–5] and the challenges involved in translating effective psychological interventions into practice settings [56], the discovery of a safe and effective pharmacotherapy would fill an important gap in treatment options for methamphetamine use.
Trial status
The current version of the protocol that has been approved by the relevant human research ethics committees is 3.0 (29 May 2018). The first participant was randomised on 9 July 2018. By 9 May 2019, 77 participants had been randomised. It is anticipated that recruitment (N = 180) will be completed by the end of 2019.
Additional files
SPIRIT Checklist. (DOC 121 kb)
Participant information sheet and consent form. (DOCX 66 kb)
Acknowledgements
This research was funded by the Australian NHMRC (project grant 1128147). RM is supported by a Curtin senior research fellowship. OMD is a RD Wright NHMRC biomedical research fellow. MB is supported by an NHMRC senior principal research fellowship (1059660 and 1156072). PD is supported by an NHMRC research fellowship (1136908). We thank the members of our DSMB (Jason White, Matthew Spittal, Deborah Kerr, Grant Sara and Juanita Koeijers). We thank Long Nguyen for developing our online unblinding portal, Steven Shoptaw for advice on trial methods, the other trial staff (including Nicole Edwards, Lucy Saunders, Bruno Agustini, Ellie Brown and Vicky Phan), agencies and individuals who assisted with recruitment efforts, and the trial participants.
Abbreviations
- AE
Adverse event
- AWQ
Amphetamine Withdrawal Questionnaire
- BCIS
Beck Cognitive Insight Scale
- BIS
Birchwood Insight Scale
- BPRS
Brief Psychiatric Rating Scale
- CEQ
Craving Experience Questionnaire
- CIDI
Composite International Diagnostic Interview
- DIP
Diagnostic Interview for Psychosis
- DSMB
Data and safety monitoring board
- EQ-5D-5 L
Five-dimension five-level version of EuroQol questionnaire
- MATES
Methamphetamine Treatment Evaluation Study
- MINI
Mini International Neuropsychiatric Interview
- NAC
N-acetylcysteine
- NHMRC
National Health and Medical Research Council
- RCQ
Readiness to Change Questionnaire
- SAE
Serious adverse event
- SAPAS
Standardised Assessment of Personality – Abbreviated Scale
- SDS
Severity of Dependence Scale
- TLFB
Timeline followback
- TSQM
Treatment Satisfaction Questionnaire for Medication
- WPAI-GH
Work Productivity and Activity Impairment Questionnaire – General Health
Authors’ contributions
All authors read and approved the final manuscript. RM, OMD, AT, PJK, PH, PD, BQ, DIL, GC, AB and MB contributed to the design of the study, obtaining funding and implementing the research. Additionally, BS, DR, VM, NtP, RB, MK and DR contributed to the piloting and development of the trial procedures at trial sites. SA, FC, HH, BS and MB contributed their medical expertise to the trial protocol and provide medical supervision during the trial. WL developed the randomisation program and contributed statistical expertise to the trial protocol.
Funding
This trial is funded by the Australian NHMRC under project grant 1128147. The funding body played no role in the design of the study or the collection, analysis and interpretation of data, or in writing the manuscripts from the study.
Availability of data and materials
The datasets generated during the current study are not publicly available due to privacy laws but are available from the corresponding author on reasonable request and pending appropriate ethics approval and the approval of the investigator team.
Ethics approval and consent to participate
This trial has been approved by all relevant human research ethics committees: Eastern Health (E21–2017), Barwon Health (17/202), the University of Wollongong and the Illawarra Shoalhaven Local Health District Health (2017/549) and Curtin University (HRE2018–0205). All participants provide informed consent prior to participation.
Consent for publication
Not applicable.
Competing interests
OMD has received grant support from Lilly and ASBDD/Servier and in-kind support from BioMedica Nutracuticals, NutritionCare and Bioceuticals. MB has received grant support from Bristol-Myers Squibb, Eli Lilly, GlaxoSmithKline, Organon, the Meat and Livestock Board, Novartis, Mayne Pharma and Servier; has been a speaker for AstraZeneca, Bristol-Myers Squibb, Eli Lilly, GlaxoSmithKline, Janssen-Cilag, Lundbeck, Merck, Pfizer, Sanofi Synthelabo, Servier, Solvay and Wyeth; and has served as a consultant to AstraZeneca, Bristol-Myers Squibb, Eli Lilly, GlaxoSmithKline, Janssen-Cilag, Lundbeck and Servier. DIL has provided consultancy advice to Lundbeck and Indivior, and has received travel support and speaker honoraria from Astra Zeneca, Indivior, Janssen, Lundbeck, Servier and Shire. PD has received investigator-initiated funding from Gilead Sciences, an untied educational grant from Indivior and is an unpaid member of an advisory board for Mundipharma for work unrelated to this study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.United Nations Office on Drugs and Crime . World Drug Report 2017. New York: United Nations; 2017. pp. 13–20. [Google Scholar]
- 2.Degenhardt L, Baxter AJ, Lee YY, Hall W, Sara GE, Johns N, Flaxman A, Whiteford HA, Vos T. The global epidemiology and burden of psychostimulant dependence: findings from the Global Burden of Disease Study 2010. Drug Alcohol Depend. 2014;137:36–47. doi: 10.1016/j.drugalcdep.2013.12.025. [DOI] [PubMed] [Google Scholar]
- 3.Colfax G, Santos G-M, Chu P, Vittinghoff E, Pluddemann A, Kumar S, Hart C. Amphetamine-group substances and HIV. Lancet. 2010;376:458–474. doi: 10.1016/S0140-6736(10)60753-2. [DOI] [PubMed] [Google Scholar]
- 4.Bhatt M, Zielinski L, Baker-Beal L, Bhatnagar N, Mouravska N, Laplante P, Worster A, Thabane L, Samaan Z. Efficacy and safety of psychostimulants for amphetamine and methamphetamine use disorders: a systematic review and meta-analysis. Syst Rev. 2016;5:189. doi: 10.1186/s13643-016-0370-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shoptaw SJ, Kao U, Ling W. Treatment for amphetamine psychosis. [update of Cochrane Database Syst Rev. 2008;(4):CD003026; PMID: 18843639]. Cochrane Database Syst Rev. 2009. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003026.pub3/full. [DOI] [PMC free article] [PubMed]
- 6.Shoptaw SJ, Kao U, Heinzerling K, Ling W. Treatment for amphetamine withdrawal. Cochrane Database Syst Rev. 2009. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003021.pub2/full. [DOI] [PMC free article] [PubMed]
- 7.De Crescenzo F, Ciabattini M, Loreto G, De Giorgi R, Del Giovane C, Cassar C, Janiri L, Clark N, Ostacher MJ, Cipriani A. Comparative efficacy and acceptability of psychosocial interventions for individuals with cocaine and amphetamine addiction: a systematic review and meta-analysis. PLoS Med. 2018;15:e1002715. doi: 10.1371/journal.pmed.1002715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith LA, Gates S, Foxcroft D. Therapeutic communities for substance related disorder. Cochrane Database Syst Rev. 2006. https://doi.org//10.1002/14651858.CD005338.pub2. [DOI] [PubMed]
- 9.Roebuck MC, French MT, McLellan AT. DATStats: results from 85 studies using the Drug Abuse Treatment Cost Analysis Program. J Subst Abus Treat. 2003;25:51–57. doi: 10.1016/S0740-5472(03)00067-9. [DOI] [PubMed] [Google Scholar]
- 10.Pullen E, Oser C. Barriers to substance abuse treatment in rural and urban communities: counselor perspectives. Subst Use Misuse. 2014;49:891–901. doi: 10.3109/10826084.2014.891615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Degenhardt L, Glantz M, Evans-Lacko S, Sadikova E, Sampson N, Thornicroft G, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Helena Andrade L, Bruffaerts R, Bunting B, Bromet EJ, Miguel Caldas de Almeida J, de Girolamo G, Florescu S, Gureje O, Maria Haro J, Huang Y, Karam A, Karam EG, Kiejna A, Lee S, Lepine J-P, Levinson D, Elena Medina-Mora M, Nakamura Y, Navarro-Mateu F, Pennell B-E, Posada-Villa J, Scott K, Stein DJ, Ten Have M, Torres Y, Zarkov Z, Chatterji S, Kessler RC, World Health Organization’s World Mental Health Surveys c Estimating treatment coverage for people with substance use disorders: an analysis of data from the World Mental Health Surveys. World Psychiatry. 2017;16:299–307. doi: 10.1002/wps.20457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown RM, Kupchik YM, Kalivas PW. The story of glutamate in drug addiction and of N-acetylcysteine as a potential pharmacotherapy. JAMA Psychiat. 2013;70:895–897. doi: 10.1001/jamapsychiatry.2013.2207. [DOI] [PubMed] [Google Scholar]
- 13.Duailibi MS, Cordeiro Q, Brietzke E, Ribeiro M, LaRowe S, Berk M, Trevizol AP. N-acetylcysteine in the treatment of craving in substance use disorders: Systematic review and meta-analysis. Am J Addict. 2017;26:660–666. doi: 10.1111/ajad.12620. [DOI] [PubMed] [Google Scholar]
- 14.LaRowe SD, Kalivas PW, Nicholas JS, Randall PK, Mardikian PN, Malcolm RJ. A double-blind placebo-controlled trial of N-acetylcysteine in the treatment of cocaine dependence. Am J Addict. 2013;22:443–452. doi: 10.1111/j.1521-0391.2013.12034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gray KM, Watson NL, Carpenter MJ, Larowe SD. N-acetylcysteine (NAC) in young marijuana users: an open-label pilot study. Am J Addict. 2010;19:187–189. doi: 10.1111/j.1521-0391.2009.00027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mardikian PN, LaRowe SD, Hedden S, Kalivas PW, Malcolm RJ. An open-label trial of N-acetylcysteine for the treatment of cocaine dependence: A pilot study. Prog Neuro-Psychopharmacol Biol Psychiatry. 2007;31:389–394. doi: 10.1016/j.pnpbp.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 17.LaRowe SD, Myrick H, Hedden S, Mardikian P, Saladin M, McRae A, Brady K, Kalivas PW, Malcolm R. Is cocaine desire reduced by N-acetylcysteine? Am J Psychiatr. 2007;164:1115–1117. doi: 10.1176/ajp.2007.164.7.1115. [DOI] [PubMed] [Google Scholar]
- 18.Prado E, Maes M, Piccoli LG, Baracat M, Barbosa DS, Franco O, Dodd S, Berk M, Vargas Nunes SO. N-acetylcysteine for therapy-resistant tobacco use disorder: a pilot study. Redox Rep. 2015;20:215–222. doi: 10.1179/1351000215Y.0000000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mousavi SG, Sharbafchi MR, Salehi M, Peykanpour M, Karimian Sichani N, Maracy M. The Efficacy of N-Acetylcysteine in the Treatment of Methamphetamine Dependence: A Double-blind Controlled, Crossover Study. Arch Iran Med. 2015;18:28–33. [PubMed] [Google Scholar]
- 20.Hashimoto K, Tsukada H, Nishiyama S, Fukumoto D, Kakiuchi T, Shimizu E, Iyo M. Protective effects of N-acetyl-L-cysteine on the reduction of dopamine transporters in the striatum of monkeys treated with methamphetamine. Neuropsychopharmacology. 2004;29:2018–2023. doi: 10.1038/sj.npp.1300512. [DOI] [PubMed] [Google Scholar]
- 21.Volkow ND, Chang L, Wang GJ, Fowler JS, Franceschi D, Sedler M, Gatley SJ, Miller E, Hitzemann R, Ding YS, Logan J. Loss of dopamine transporters in methamphetamine abusers recovers with protracted abstinence. J Neurosci. 2001;21:9414–9418. doi: 10.1523/JNEUROSCI.21-23-09414.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chang L, Alicata D, Ernst T, Volkow N. Structural and metabolic brain changes in the striatum associated with methamphetamine abuse. Addiction. 2007;102(Suppl 1):16–32. doi: 10.1111/j.1360-0443.2006.01782.x. [DOI] [PubMed] [Google Scholar]
- 23.Sekine Y, Ouchi Y, Takei N, Yoshikawa E, Nakamura K, Futatsubashi M, Okada H, Minabe Y, Suzuki K, Iwata Y, Tsuchiya KJ, Tsukada H, Iyo M, Mori N. Brain serotonin transporter density and aggression in abstinent methamphetamine abusers. Arch Gen Psychiatry. 2006;63:90–100. doi: 10.1001/archpsyc.63.1.90. [DOI] [PubMed] [Google Scholar]
- 24.London ED, Simon SL, Berman SM, Mandelkern MA, Lichtman AM, Bramen J, Shinn AK, Miotto K, Learn J, Dong Y, Matochik JA, Kurian V, Newton T, Woods R, Rawson R, Ling W. Mood disturbances and regional cerebral metabolic abnormalities in recently abstinent methamphetamine abusers. Arch Gen Psychiatry. 2004;61:73–84. doi: 10.1001/archpsyc.61.1.73. [DOI] [PubMed] [Google Scholar]
- 25.Dean O, Giorlando F, Berk M. N-acetylcysteine in psychiatry: current therapeutic evidence and potential mechanisms of action. J Psychiatry Neurosci. 2011;36:78. doi: 10.1503/jpn.100057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Voce A, McKetin R, Calabria B, Burns R, Castle DJ. A systematic review of the symptom profile and course of methamphetamine associated psychosis. Subst Use Misuse. 2019;54:549. doi: 10.1080/10826084.2018.1521430. [DOI] [PubMed] [Google Scholar]
- 27.McKetin R, Dawe S, Burns RA, Hides L, Kavanagh DJ, Teesson M, Mc DYR, Voce A, Saunders JB. The profile of psychiatric symptoms exacerbated by methamphetamine use. Drug Alcohol Depend. 2016;161:104–109. doi: 10.1016/j.drugalcdep.2016.01.018. [DOI] [PubMed] [Google Scholar]
- 28.Grandjean EM, Berthet P, Ruffmann R, Leuenberger P. Efficacy of oral long-term N-acetylcysteine in chronic bronchopulmonary disease: a meta-analysis of published double-blind, placebo-controlled clinical trials. Clin Ther. 2000;22:209–221. doi: 10.1016/S0149-2918(00)88479-9. [DOI] [PubMed] [Google Scholar]
- 29.Anonymous. Cetylev (TM) (acetylcysteine) effervescent tablets for oral solution [Full prescribing information]. United States (U.S.). Washington, DC: Food and Drug Administration; 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/207916s003lbl.pdf.
- 30.McKetin R, Dean OM, Baker AL, Carter G, Turner A, Kelly PJ, Berk M. A potential role for N-acetylcysteine in the management of methamphetamine dependence. Drug Alcohol Rev. 2017;36:153–159. doi: 10.1111/dar.12414. [DOI] [PubMed] [Google Scholar]
- 31.Fals-Stewart W, O'Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: psychometric properties. J Consult Clin Psychol. 2000;68:134–144. doi: 10.1037/0022-006X.68.1.134. [DOI] [PubMed] [Google Scholar]
- 32.May J, Andrade J, Kavanagh DJ, Feeney GFX, Gullo MJ, Statham DJ, Skorka-Brown J, Connolly JM, Cassimatis M, Young RM, Connor JP. The Craving Experience Questionnaire: a brief, theory-based measure of consummatory desire and craving. Addiction. 2014;109:728–735. doi: 10.1111/add.12472. [DOI] [PubMed] [Google Scholar]
- 33.Gossop M, Darke S, Griffiths P, Hando J, Powis B, Hall W, Strang J. The Severity of Dependence Scale (SDS): psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction. 1995;90:607–614. doi: 10.1046/j.1360-0443.1995.9056072.x. [DOI] [PubMed] [Google Scholar]
- 34.Topp L, Mattick RP. Choosing a cut-off on the Severity of Dependence Scale (SDS) for amphetamine users. Addiction. 1997;92:839–845. doi: 10.1111/j.1360-0443.1997.tb02953.x. [DOI] [PubMed] [Google Scholar]
- 35.Srisurapanont M, Jarusuraisin N, Jittiwutikan J. Amphetamine withdrawal: I. Reliability, validity and factor structure of a measure. Aust N Z J Psychiatry. 1999;33:89–93. doi: 10.1046/j.1440-1614.1999.00517.x. [DOI] [PubMed] [Google Scholar]
- 36.Lukoff D, Nuechterlein KH, Ventura J. Manual for the expanded Brief Psychiatric Rating Scale. Schizophr Bull. 1986;12:594–602. [Google Scholar]
- 37.Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale: ‘the drift busters’. Int J Methods Psychiatr Res. 1993;3:221–244. [Google Scholar]
- 38.Atkinson MJ, Sinha A, Hass SL, Colman SS, Kumar RN, Brod M, Rowland CR. Validation of a general measure of treatment satisfaction, the Treatment Satisfaction Questionnaire for Medication (TSQM), using a national panel study of chronic disease. Health Qual Life Outcomes. 2004;2:12. doi: 10.1186/1477-7525-2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.NCCIH Clinical Research Toolbox. 2018. https://nccih.nih.gov/grants/toolbox. Accessed 27 May 2019.
- 40.Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual Life Res. 2011;20:1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Darke S, Hall W, Wodak A, Heather N, Ward J. Development and validation of a multi-dimensional instrument for assessing outcome of treatment among opiate users: the Opiate Treatment Index. Br J Addict. 1992;87:733–742. doi: 10.1111/j.1360-0443.1992.tb02719.x. [DOI] [PubMed] [Google Scholar]
- 42.McKetin R, Najman J, Baker A, Lubman D, Dawe S, Ali R, Lee N, Mattick R, Mamun A. Evaluating the impact of community-based treatment options on methamphetamine use: findings from the Methamphetamine Treatment Evaluation Study (MATES) Addiction. 2012;107:1998–2008. doi: 10.1111/j.1360-0443.2012.03933.x. [DOI] [PubMed] [Google Scholar]
- 43.Andrews G, Peters L. The psychometric properties of the Composite International Diagnostic Interview. Soc Psychiatry Psychiatr Epidemiol. 1998;33:80–88. doi: 10.1007/s001270050026. [DOI] [PubMed] [Google Scholar]
- 44.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 45.Castle DJ, Jablensky A, McGrath JJ, Carr V, Morgan V, Waterreus A, Valuri G, Stain H, McGuffin P, Farmer A. The diagnostic interview for psychoses (DIP): development, reliability and applications. Psychol Med. 2006;36:69–80. doi: 10.1017/S0033291705005969. [DOI] [PubMed] [Google Scholar]
- 46.Heather N, Rollnick S, Bell A. Predictive validity of the Readiness to Change Questionnaire. Addiction. 1993;88:1667–1677. doi: 10.1111/j.1360-0443.1993.tb02042.x. [DOI] [PubMed] [Google Scholar]
- 47.Beck AT, Baruch E, Balter JM, Steer RA, Warman DM. A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophr Res. 2004;68:319–329. doi: 10.1016/S0920-9964(03)00189-0. [DOI] [PubMed] [Google Scholar]
- 48.Birchwood M, Smith J, Drury V, Healy J, Macmillan F, Slade M. A self-report Insight Scale for psychosis: reliability, validity and sensitivity to change. Acta Psychiatr Scand. 1994;89:62–67. doi: 10.1111/j.1600-0447.1994.tb01487.x. [DOI] [PubMed] [Google Scholar]
- 49.Moran P, Leese M, Lee T, Walters P, Thornicroft G, Mann A. Standardised Assessment of Personality - Abbreviated Scale (SAPAS): preliminary validation of a brief screen for personality disorder. Br J Psychiatry. 2003;183:228–232. doi: 10.1192/bjp.183.3.228. [DOI] [PubMed] [Google Scholar]
- 50.Quinn B, Stoové M, Dietze P. Factors associated with professional support access among a prospective cohort of methamphetamine users. J Subst Abus Treat. 2013;45:235–241. doi: 10.1016/j.jsat.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 51.McKetin R, Dunlop AJ, Holland RM, Sutherland RA, Baker AL, Salmon AM, Hudson SL. Treatment outcomes for methamphetamine users receiving outpatient counselling from the Stimulant Treatment Program in Australia. Drug Alcohol Rev. 2013;32:80–87. doi: 10.1111/j.1465-3362.2012.00471.x. [DOI] [PubMed] [Google Scholar]
- 52.Ogedegbe GO, Boutin-Foster C, Wells MT, et al. A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive african americans. Arch Intern Med. 2012;172:322–326. doi: 10.1001/archinternmed.2011.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McKetin R, Voce A, Burns R. Research into methamphetamine use in the Australian Capital Territory. Perth. Australia: National Drug Research Institute; 2017. [Google Scholar]
- 54.Shearer J, Gowing LR. Pharmacotherapies for problematic psychostimulant use: a review of current research. Drug Alcohol Rev. 2004;23:203–211. doi: 10.1080/09595230410001704190. [DOI] [PubMed] [Google Scholar]
- 55.McKetin R, McLaren J, Lubman DI, Hides L. The prevalence of psychotic symptoms among methamphetamine users. Addiction. 2006;101:1473–1478. doi: 10.1111/j.1360-0443.2006.01496.x. [DOI] [PubMed] [Google Scholar]
- 56.Carroll KM. Lost in translation? Moving contingency management and cognitive behavioral therapy into clinical practice. Ann N Y Acad Sci. 2014;1327:94–111. doi: 10.1111/nyas.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SPIRIT Checklist. (DOC 121 kb)
Participant information sheet and consent form. (DOCX 66 kb)
Data Availability Statement
The datasets generated during the current study are not publicly available due to privacy laws but are available from the corresponding author on reasonable request and pending appropriate ethics approval and the approval of the investigator team.