Abstract
This study uses Medicare Parts A and B claims data to compare hospitalizations for and spending on traumatic injury vs heart failure, pneumonia, stroke, and acute myocardial infarction in older adults between 2008 and 2014.
The burden of traumatic injury among older adults is underappreciated, as it is the predominant cause of death among children and younger adults and therefore often thought to be primarily a disease of the young.1 However, traumatic injury in older adults is increasing in prevalence as the US population ages.2 Older patients present unique care challenges because they have decreased physiologic reserve, have more comorbid conditions, and are at risk of specific complications such as delirium.3 Our objective was to quantify occurrence of and spending on traumatic injury in comparison with other common medical diseases resulting in acute hospitalization among Medicare beneficiaries.
Methods
We evaluated Centers for Medicare & Medicaid Services Parts A and B claims data for inpatient hospitalizations among adults aged 65 years or older with fee-for-service Medicare coverage from 2008 to 2014 (the most recent data available to our research group) using a nationally representative 20% sample. We computed all index hospitalization, readmission, and postacute care (skilled nursing facility, long-term acute care facility, inpatient rehabilitation, and outpatient Part B) payments within 90 days of discharge. Payments were categorized according to primary indication for hospitalization based on the first International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code listed for each episode. Traumatic injury was defined as a first-position ICD-9-CM code from 800 to 959.9, excluding late effects, superficial injuries, or foreign bodies entering through orifice.4 Additional ICD-9-CM diagnosis groupings were created for congestive heart failure, pneumonia, stroke, and acute myocardial infarction. These diagnosis groupings were chosen because they represent common acute diseases among Medicare beneficiaries.
Analyses were performed using SAS version 9.4 (SAS Institute Inc). Proportions of inpatient hospitalizations and Medicare payments were compared between disease categories using 2-sided z tests or t tests. 95% Wald confidence intervals were constructed. Statistical significance was set at P < .005 to account for multiple comparisons. Payment data are presented in real dollars (not inflation adjusted). The Michigan Medicine Institutional Review Board approved this study with a waiver of informed consent.
Results
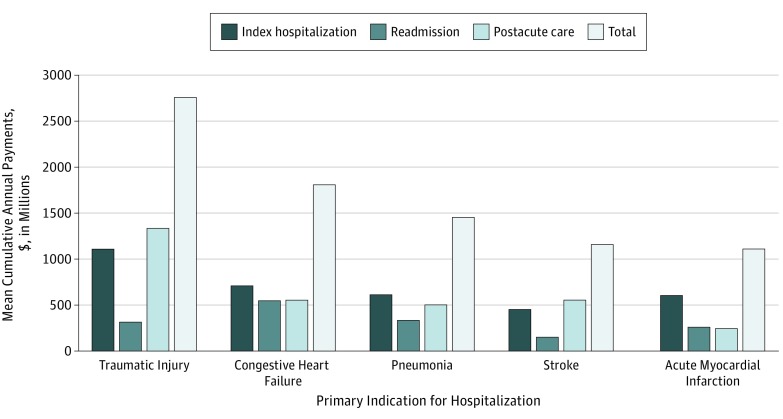
Of 11 766 922 inpatient hospitalizations, 42.4% were for men, and the median age at admission was 78 (interquartile range, 71-85) years. Traumatic injury was the primary indication for hospitalization in 5.6% of admissions in fee-for-service Medicare–covered patients (Table). This proportion was statistically significantly smaller than for congestive heart failure (5.9%) and statistically significantly greater than for pneumonia (4.9%), stroke (2.7%), or acute myocardial infarction (2.7%) (P < .001 for all). The mean cumulative annual Medicare payment for hospitalization and care within 90 days of discharge after traumatic injury was $2760 million (95% CI, $2755-$2766 million) (Figure). These annual payments were statistically significantly greater than the annual spending for congestive heart failure ($1811 million; 95% CI, $1806-$1816 million), pneumonia ($1454 million; 95% CI, $1450-$1459 million), stroke ($1159 million; 95% CI, $1155-$1163 million), and acute myocardial infarction ($1109 million; 95% CI, $1105-$1114 million) (P < .001 for all). The distribution of annual Medicare payments due to traumatic injury was as follows: for index hospitalization, $1113 million (40.3%); for postacute care, $1335 million (48.4%); and for readmission, $313 million (11.3%).
Table. Demographic Data for Acute Medical Conditions in Adults With Fee-for-Service Medicare Coverage, 2008-2014 (20% Sample)a.
| Demographics | Traumatic Injuryb | Congestive Heart Failurec | Pneumoniad | Strokee | Acute Myocardial Infarctionf |
|---|---|---|---|---|---|
| Total hospitalizations, 2008-2014, No. | 653 413 | 692 031 | 571 389 | 316 606 | 313 022 |
| Age, median (interquartile range), y | 83 (76-88) | 81 (74-87) | 81 (73-87) | 80 (73-87) | 78 (71-85) |
| Male, % (95% CI) | 29.9 (29.8-30.0) | 44.8 (44.7-44.9) | 45.2 (45.1-45.4) | 41.4 (41.2-41.5) | 51.1 (50.9-51.3) |
| Percentage of overall hospitalizations (95% CI)g | 5.6 (5.6-5.6) | 5.9 (5.9-5.9) | 4.9 (4.8-4.9) | 2.7 (2.7-2.7) | 2.7 (2.7-2.7) |
Data are presented for the 20% sample only and are not projected to 100% of the population.
Traumatic injury: International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 800-959.9, excluding late effects (codes 905-909.9), superficial injuries (codes 910-924.9), or foreign bodies entering through orifice (codes 930-939.9).
Congestive heart failure: ICD-9-CM codes 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 428.0, 428.1, 428.20, 428.21, 428.22, 428.23, 428.30, 428.31, 428.32, 428.33, 428.40, 428.41, 428.42, 428.43, or 428.9.
Pneumonia: ICD-9-CM codes 480-480.99, 481, 482-482.99, 483-483.99, 484-484.99, 485, 486, or 487.0.
Stroke: ICD-9-CM codes 430, 431, 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, 434.91, or 436.
Acute myocardial infarction: ICD-9-CM codes 410.00, 410.01, 410.10, 410.11, 410.20, 410.21, 410.30, 410.31, 410.40, 410.41, 410.50, 410.51, 410.60, 410.61, 410.70, 410.71, 410.80, 410.81, 410.90, or 410.91.
Comparisons were performed for traumatic injury vs other conditions for percentage of overall hospitalizations; P < .001 for all comparisons.
Figure. Mean Cumulative Annual 90-Day Payments Associated With Inpatient Hospitalizations Among Medicare Beneficiaries by Condition, 2008-2014 (20% Sample).
Data represent mean overall annual expenditures in dollars for index hospitalization, readmission, postacute care, and total 90-day payments associated with inpatient hospitalization by condition for fee-for-service Medicare beneficiaries. Postacute care includes skilled nursing facility, inpatient rehabilitation, Part B expenses, and long-term care. Home health care payment data were not available. Data are presented for the 20% sample only and are not projected to 100% of the population. Error bars indicate 95% CIs. P < .001 for traumatic injury vs all other conditions and payment categories.
Discussion
Between 2008 and 2014, traumatic injury was among the most common and costly reasons for hospitalization in Medicare beneficiaries. More was spent on trauma than on each of the other acute diseases studied in this population. Forty-eight percent of spending went toward postacute care, while the index hospitalization accounted for 40% of total payments. The National Trauma Data Bank 2016 report showed that 31% of patients experiencing injury are at least 65 years old and that Medicare was the primary payer for 27% of all traumatic injuries.5 These numbers will likely increase in the coming years, as adults aged 65 years or older are expected to increase from 14.5% of the total US population in 2014 to 23.6% in 2060.6
This study was limited by use of a 20% sample and noninclusion of home health spending. Different types of traumatic injury were not investigated. The prevalence and payments may differ by type of trauma diagnosis given the breadth and heterogeneity of trauma as a disease. The data are from 2008 through 2014, and it is unknown if prevalence or payments have changed more recently. Injury prevention efforts to reduce incidence and payment reform linked to quality initiatives, especially focusing on postacute care, to optimize value in Medicare spending should be priorities.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Heron M. Deaths: leading causes for 2016. Natl Vital Stat Rep. 2018;67(6):1-77. [PubMed] [Google Scholar]
- 2.DeGrauw X, Annest JL, Stevens JA, Xu L, Coronado V. Unintentional injuries treated in hospital emergency departments among persons aged 65 years and older, United States, 2006-2011. J Safety Res. 2016;56:105-109. doi: 10.1016/j.jsr.2015.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American College of Surgeons ACS TQIP Geriatric Trauma Management Guidelines https://www.facs.org/~/media/files/quality%20programs/trauma/tqip/geriatric%20guide%20tqip.ashx. Accessed December 22, 2018.
- 4.Hemmila MR, Nathens AB, Shafi S, et al. The Trauma Quality Improvement Program: pilot study and initial demonstration of feasibility. J Trauma. 2010;68(2):253-262. doi: 10.1097/TA.0b013e3181cfc8e6 [DOI] [PubMed] [Google Scholar]
- 5.American College of Surgeons National Trauma Data Bank 2016: Annual Report https://www.facs.org/~/media/files/quality%20programs/trauma/ntdb/ntdb%20annual%20report%202016.ashx. Accessed December 22, 2018.
- 6.Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060 March 2015. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. Accessed December 22, 2018.