Abstract
Background and objectives: Inhalers mishandling remain an important clinical issue worldwide. The aim of this study was to evaluate inhalation technique in stable COPD out-patients. The variables under study were type of inhaler device (ID), patients’ preference for an inhaler, number of IDs used by each patient, beliefs about inhaler medication and some demographic, clinical and functional patients' characteristics. We aim to assess how they are related to inhalation technique.
Methods: A cross-sectional study was conducted in a hospital outpatient respiratory care. COPD patients over 40 years old, diagnosed according to GOLD criteria, and using IDs were included consecutively. The Beliefs about Medicines Questionnaire (BMQ), a demographic and a clinical survey were applied. The number of IDs used by each patient and the patients’ preference for some IDs were recorded. Patients were asked to demonstrate the use of their prescribed inhalation devices, and inhaler technique was assessed by using previously defined checklists, including essential steps and critical errors. A statistics analysis was then performed.
Results: We studied 300 subjects performing a total of 521 inhalation manoeuvers with 10 different IDs. At least one step incorrectly performed was found in 48.2% of demonstrations and in 29.9% critical errors were observed. Misuse was related to priming/loading in 6.9%, to inhalation manoeuver in 13.1% and to both in 10%. There was a statistically significant association between critical errors and type of ID (P<0.001). No significant relationship was found between correct performance of key manoeuvers and patients’ preference or number of inhalers used per patient. Misuse due to critical errors was observed in 39.3% of patients and was positively related to female gender, age ≥65, lower education level and lower socioeconomic status (higher Graffar classification score), but not to patients’ clinical or functional characteristics. In the sub-group of patients presenting critical errors when using IDs, there was a statistically significant inverse association between BMQ Necessity score and number of critical errors.
Conclusions: Inhalers mishandling remains disappointingly common. A good inhalation technique depends on the type of ID, and failure of inhalation manoeuver was the main cause of ID misuse. It was not associated to multiple inhalers’ use nor to patient’s preference, but to the patient’s beliefs about the necessity to use them. Elderly patients, women and those with lower education level or lower socioeconomic status demonstrate a worse inhalation technique.
Keywords: COPD; Inhalation technique; Inhaler devices
Background and objectives
COPD currently represents one of the most significant health problems at an international level. Inhaled medication is the mainstay of COPD management, and therapeutic success depends on the maintenance of a correct inhalation technique. There is a growing evidence concerning inhalers misuse as a common problem worldwide.1,2 It can be associated with increased rate of severe COPD exacerbations (ECOPD),3 but the impact of inhalers misuse on COPD outcomes remains currently unknown. In a country where patients have a good access to health-care services and to effective treatment, any development in treatment outcomes must address the improvement of inhalation technique. This can be one of the main cost/benefit measures improving healthcare in COPD patients.
In 1965, Saunders published in the BMJ the first paper describing the misuse of inhaled medication.4 In fact, misuse of inhaler devices (IDs) in obstructive airway diseases is an old problem, and has not improved over the past 40 years, despite the progressive technical improvement of IDs.5 Currently, up to 94% of patients have demonstrated inhalers’ mishandling in clinical studies.6 Teaching and maintaining a correct inhalation technique has a positive impact on disease and patient outcomes.7 It should remain a constant concern of any health professional involved in the management of COPD patients.8,9
The knowledge of difficulties and barriers that hinder a correct inhalation technique is of paramount importance to develop any educational intervention regarding the correct use of IDs. However, this can be a very difficult task. Assessment of inhalation technique is complex and always somewhat subjective, and consensus is lacking between researchers regarding the definition of critical errors and standardization of inhaler technique checklists.7
The aim of this study was to evaluate the inhalation technique in stable COPD outpatients, because there was a gap of information in Portuguese population. We intended assessing whether the type of ID, the preference or number of IDs used by each patient, the demographic, clinical or functional characteristics of patients, and the patients’ beliefs about inhaled medication are associated with a correct inhalation technique. This last aspect was never studied, to the best of our knowledge.
Materials and methods
A cross-sectional study was conducted in the outpatient respiratory care of Guimarães hospital, between March 2016 and May 2017. COPD patients over 40 years old diagnosed according to GOLD criteria, without acute exacerbations for >4 weeks and using inhalation devices were consecutively included. Exclusion criteria were refusal to participate and an inability to understand simple questionnaires. No participants were at the same time enrolled in another different studies, and all gave their written informed consent. The study was approved by the Guimarães Hospital Ethics Committee, the Research Ethics Committee of Minho’s University and by the Portuguese Data Protection Agency. We followed the STROBE guidelines for reporting observational studies.10
A survey of demographic and clinical data, the Graffar Social Classification,11 validated for use in Portuguese population and the cross-cultural adaptation of the Beliefs about Medicines Questionnaire (BMQ-specific) into Portuguese were applied.12 Patients’ beliefs about inhaled medication can influence adherence to medication but we suspect they can also motivate patients to learn the correct use of inhalers. BMQ is an 11-item questionnaire with a five-item Necessity scale and a six-item Concern scale. The Necessity and the Concern scales assess, respectively, the beliefs about the necessity and the beliefs about concerns related to side-effects, dependence and toxicity of the medication. Answered on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree), the points are summed, and total scores range from 5 to 25 in the Necessity scale and 6 to 30 in the Concern scale. It was clearly detailed that questions referred to the inhaled medication, and not to the device itself. The number of ECOPD referred in the last year was evaluated. We defined ECOPD according to GOLD as an acute worsening of respiratory symptoms that results in additional therapy,13 but also requiring an unplanned medical visit, because patients have difficulty in remembering unreported exacerbations. Evaluation of symptoms was done using the Portuguese versions of the COPD assessment Test (CAT) and the Medical Research Council Dyspnoea Questionnaire (mMRC). All subjects performed spirometries according to ERS/ATS criteria, and referenced according to the Global Lung Function Initiative predict equations (GLI 2012).14,15 Inhalation technique was assessed by using previous defined checklists, as presented in Tables 1 and 2.
Table 1.
Checklist of steps for a correct inhalation technique
| 1 | Correct priming or loading (Incorrect priming or loading were considered critical error). |
| 2 | Exhalation before inhalation. |
| 3 | Correct inhalation (Incorrect inhalation were considered critical error). |
| 4 | Hold the breath a few seconds after inhalation (except when using a pMDI + spacer). |
| 5 | Finalization (clean the mouth-piece, remove used capsule after verifying that no powder remains, check color changing in control window, close ID and wash the mouth if necessary). |
Table 2.
Critical errors in different IDs
| 1 | Aeroliser®, Breezhaler®, and Handihaler®: failure to insert the capsule, failure to press and release buttons, powder remaining in the capsule after inhalation. |
| 2 | Diskus®: failure to open the cover, to slide the lever until it clicks, or not keeping inhaler horizontally. |
| 3 | Ellipta®: failure to slide cover down until a click is heard or block air vent with fingers. |
| 4 | Genuair®: failure to remove the cap, to press and release the button until the control window has changed to green, not holding inhaler horizontally, and not changing control window to red after inhalation. |
| 5 | pMDI: failure to remove cap, not shaking the inhaler (suspensions only), not holding the inhaler in the upright position, poorly synchronized hand actuation and inhalation (except using a spacer), inhalation through the nose, actuation against teeth, lips or tongue. |
| 6 | Respimat®: lack of cartridge in the device, failure to open the cap, twisting the base or pressing the dose-release button, poorly synchronized hand actuation and inhalation. |
| 7 | Spiromax®: failure to hold the inhaler in upright position, failure to open mouthpiece cover until a click is heard or blocking air vent with fingers. |
| 8 | Turbuhaler®: failure to remove cover, to hold the inhaler upright when twisting the grip (tolerance ±45º) until a click is heard. |
Abbreviation: ID, inhaler device.
They were developed according to the instructions provided by the manufactures and to previous literature,16 and included essential steps and critical errors. Errors are considered critical when they can substantially affect drug delivery to the lungs, and are related to priming/loading or inhalation manoeuver. The definition of critical errors when using inhalers is of great importance. However, there is currently a lack of consensus on their definition, deserving discussion.7
Participants were asked to demonstrate the use of their prescribed ID just as they do it at home, but demonstrations were done with inhalers containing placebo medications. Assessment of patients handling of IDs, by recording the correct steps and critical errors, were done by a single trained senior pulmonologist, to avoid inter-observer variability. The number of IDs simultaneously in use by each patient was recorded. Patients using two or more inhalers were inquired for device preference, and invited to justify their answer, clearly stated that the question is related only to inhalers’ aspects. This was an open question. Answers were then collected in 5 groups: more practical to use, easier to use, ID characteristics, accustomed to using, and others. Because of the difficulty to distinguish between “being more practical” and “easier”, these two answers were later analyzed together.
The variables under study, evaluated for potential association with incorrect inhalation technique, were the type of ID, patients’ preference, use of multiple devices, beliefs about inhaled medication and some patients’ characteristics: age, gender, monthly income, social classification, education level, CAT score, mMRC grade, number of ECOPD referred in the last year, FEV1%, and GOLD 2017 stage and classification. Because patients were using 1–4 IDs at the same time, to assess inhalation technique three different outcomes, exhibiting different aspects of the same reality were defined. Correct use rate (CUR) was defined as the ratio between the sum of the number of correct steps in all IDs used by each patient and the total possible number of steps. Critical errors rate (CER) was defined as the ratio between the sum of the number of critical errors done with all the IDs and the total number of possible critical errors. The patients’ ability (ABL) to use inhalers was defined as the ratio between the number of IDs without any critical errors and the total number of IDs used. Data were compiled in Microsoft Office Excel 2013 (Microsoft Corporation, Redmond, WA, USA).
Statistical analysis
Statistical analysis was performed with IBM SPSS Statistics for Windows, Version 23.0. (IBM Corp., Armonk, NY, USA). Group differences in the sample were analyzed with Student’s T test and Chi-square independence test. Multivariate ANOVA modeling was used to identify differences among sample groups in: CUR, CER and the patients’ ability to use inhalers. Spearman’s correlation was used to explore the association between patients’ beliefs (BMQ) and CER or the patient’s ability to use inhalers. Statistical significance was considered when P<0.05.
Results
Sample characteristics
We studied 300 subjects performing a total of 521 inhalation manoeuvers with 10 different IDs in a total of 69 (13.2%) pMDI, 132 (25.3%) single-dose inhalers (sDPI), 239 (45.8%) multiple dose inhalers (mDPI) and 81 (15.5%) SMI-Respimat®. Only 12 pMDIs (17.4%) were used together with a spacer. All participants referred using inhalers for over a month, regardless of having received prior instructions for the correct inhalers’ use. The main demographic, clinical and functional characteristics of patients are described in Table 3.
Table 3.
Demographic, clinical and functional characteristics of COPD patients
| Characteristics | n=300 |
|---|---|
| Male gender | 231 (77.0) |
| Mean age (years) | |
| Total/ male / female | 67.6 / 67.4 / 68.3 |
| Age ≥65 years | 188 (62.7) |
| Education level ≤3 school years | |
| Total; male; female | 89 (29.7); 58 (25.1); 31 (44.9) |
| Very low monthly income (<530 Euros) | |
| Total; male; female | 199 (66.8); 146 (63.5); 53 (77.9) |
| Graffar social classification | |
| I – 2 (0.7); II – 13 (4.4); III – 102 (34.5); IV – 175 (59.1); V – 4 (1.3) | |
| Mean smoking amount (pack/years) | 49.2±32.9 |
| mMRC grade ≥2 | 189 (64.3) |
| CAT score ≥10 | 156 (75.4) |
| Frequent ECOPD (≥2 / last year) | 119 (39.7) |
| Post-bronchodilator FEV1L (%) | 1.35 (53.0) |
| GOLD 2017 stage and classification | |
| I – 30 (10.0); II – 123 (41.0); III – 108 (36.0); IV – 39 (13.0) | |
| A – 62 (20.7); B – 121 (40.3); C – 7 (2.3); D – 110 (36.7) | |
Note: Data shown as mean or nº (%).
Abbreviations: mMRC, Medical Research Council Dyspnea Questionnaire; CAT, COPD Assessment Test; ECOPD, COPD exacerbations.
89.7% of patients referred living with the family, but 23.2% of women and 5.6% of men (P<0.001) referred living alone. Tobacco smoking was the most common exposure identified and 16.4% of subjects were current smokers. Participants were currently using one (38.9%), two (49.5%), three (10.6%) or four inhalers (1%). The main reasons for an ID preference were the ease of use (65.9%), ID characteristics (24.6%) and being accustomed to using (2.9%). Devices’ characteristics were frequently reported as pleasant because of the small size and feedback provided by some inhalers. Powder’s bad taste and a significant effort needed during inhalation were frequently referred as unpleasant.
Inhalation misuse by IDs
At least one incorrect step was found in 48.2% of inhalations. In 156 (29.9%) demonstrations, critical errors were observed: 53.6% with pMDIs, 24.2% with sDPIs, 26.8% with mDPIs and 28.4% with the soft-mist inhaler. There was a statistically significant association between critical errors and the type of ID (P<0.001). Misuse was related to priming or loading in 6.9%, to inhalation manoeuver in 13.1% and to both in 10%. In mDPI group, critical errors ranged from 16.1% with Ellipta® to 35.1% with Turbohaler®. No significant relationship was found between correct performance of key maneuvers and patient’s preference: 26.3% of preferred and 28.1% of non-preferred IDs presented incorrect use (P=0.120). No significant relationship was found between the correct performance of key manoeuvers and the number of inhalers currently used by patients (the incorrect use was 31.6% with one inhaler, 24.8% with two, 33.4% with three and 66.7% with four inhalers, P=0.739). The relationship between IDs and critical errors/inhalation technique is presented in Table 4. Participants showed more difficulty in inhalation maneuver with pMDI, in priming when using a Turbuhaler® and in both loading and inhalation maneuver when using the Handihaler®.
Table 4.
Inhalation misuse by inhaler devices
| Critical errors (%)a | nº | % of incorrect use | 1 | 2 | 3 |
|---|---|---|---|---|---|
| pMDI (12 with spacer) | 69 | 53.6 | 5.8 | 30.6 | 17.4 |
| SMI | 81 | 28.4 | 0 | 16 | 12.3 |
| sDPI | 132 | 24.2 | 9.1 | 5.3 | 9.8 |
| Breezhaler® | 72 | 19.4 | 6.9 | 5.6 | 6.9 |
| Handihaler® | 51 | 37.3 | 13.7 | 5.9 | 17.6 |
| Aeroliser® | 9 | 0 | 0 | 0 | 0 |
| mDPI | 239 | 26.8 | 8.4 | 11.3 | 7.1 |
| Diskus® | 75 | 29.3 | 2.7 | 16 | 10.7 |
| Genuair® | 53 | 22.6 | 11.3 | 5.7 | 5.7 |
| Spiromax® | 43 | 25.6 | 0 | 20.9 | 4.7 |
| Turbuhaler® | 37 | 35.1 | 29.7 | 2.7 | 2.7 |
| Ellipta® | 31 | 16.1 | 3.2 | 6.5 | 6.5 |
| (P<0.001) | (P<0.001) | ||||
Notes: aCritical errors related to: 1=priming/loading; 2=inhalation maneuver; 3=1+2. bIncorrect use=presence of critical errors.
Inhalation misuse by patients’ characteristics
Misuse due to critical errors was observed in 52.1% of women and 35.4% of men, in a total of 39.3% patients. The statistically significant relationship between the studied outcomes, as referred in the section on materials and methods, and patients’ characteristics are presented in Table 5.
Table 5.
Inhalers misuse by patients’ characteristics
| CUR | P-value | CER | P-value | ABL | P-value | |
|---|---|---|---|---|---|---|
| Male gender | 0.8116 | 0.1618 | 0.7454 | |||
| Female gender | 0.6899 | 0.001 | 0.3284 | 0.001 | 0.5616 | 0.001 |
| Education level <4 years | 0.7171 | 0.2591 | 0.5991 | |||
| Education level ≥4 years | 0.8117 | 0.003 | 0.1753 | 0.026 | 0.7470 | 0.004 |
| Graffar 4+5 | 0.7264 | 0.2472 | 0.6269 | |||
| Graffar 1+2+3 | 0.8654 | 0.001 | 0.1308 | 0.001 | 0.8180 | 0.001 |
Note: Data shown as mean score.
Abbreviations: CUR, correct use rate of inhalers; CER, critical errors rate; ABL, patients’ ability to use inhalers; Graffar, Graffar social classification.
A statistically significant association was also found between CUR and age <65 (<65 years: mean score=0.8264, ≥65 years: mean score=0.7581, P=0.026). No statistically significant association was found between the studied outcomes and ECOPD, CAT score, mMRC grade, FEV1% and GOLD stage or classification.
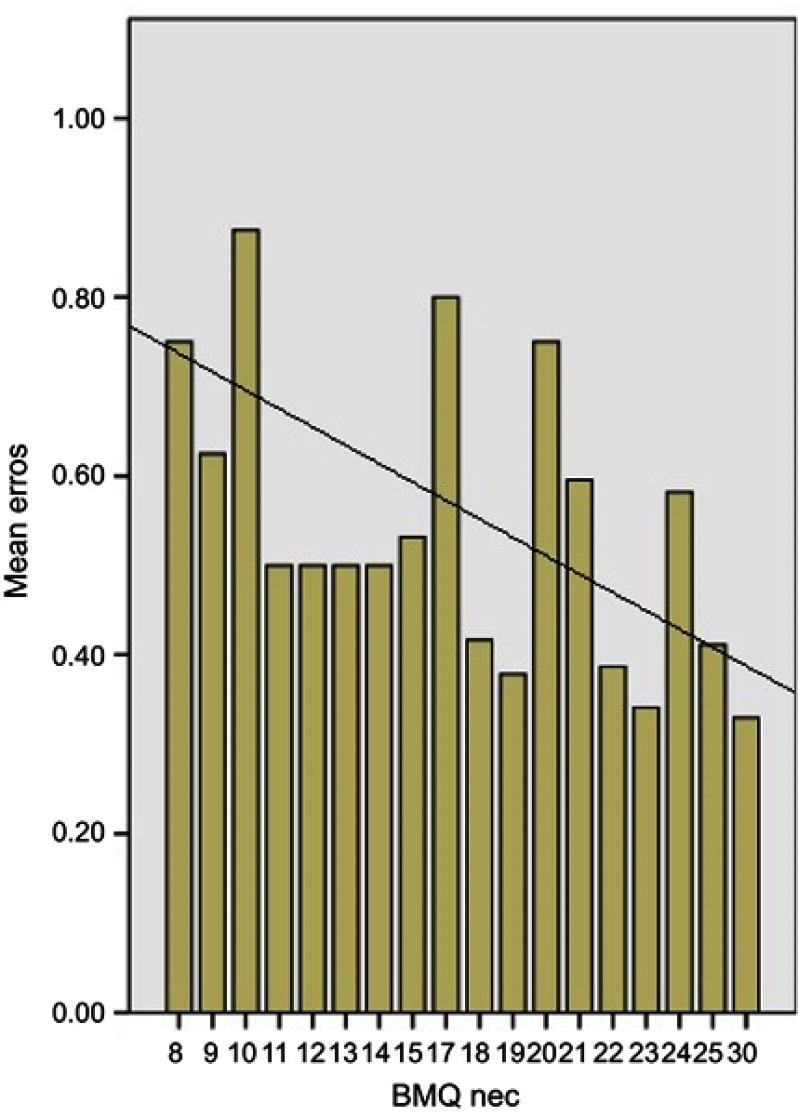
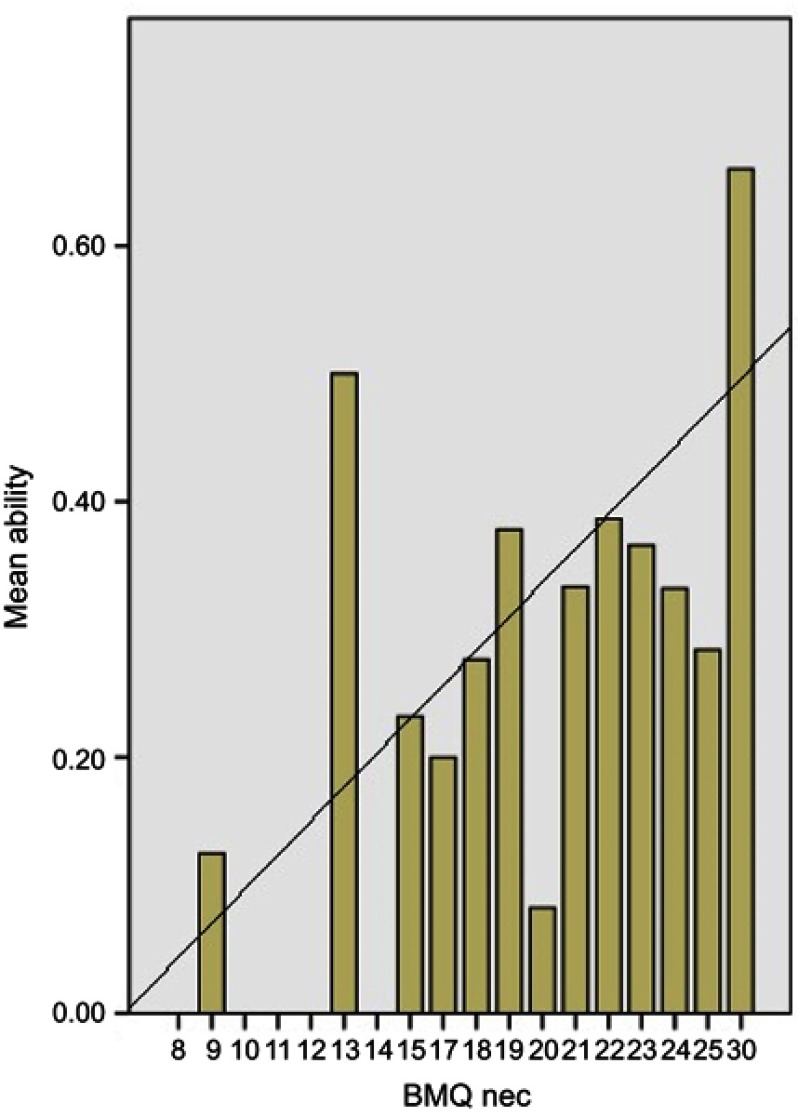
Inhalation misuse by patients’ beliefs about medicines
Only 59 (85.5%) women and 191 (82.7%) men (P=0.364), in a total of 250 (83.3%) participants were able to understand and respond to the BMQ questionnaire. Misuse due to critical errors was observed in 92 (36.8%) of them. We found no significant association between the BMQ concern score and CER or the ability to use inhalers. However, in this sub-group of patients (n=92) there was a statistically significant correlation between the BMQ Necessity score and CER (Spearman’s rho =−0.294, P=0.004) or the ability to use IDs (Spearman’s rho =0.248, P=0.017). The patients’ beliefs about the necessity to use IDs were, respectively, significant direct and inverse predictors of ability to use inhalers (β=0.310; P=0.003; r2=0.096) and misuse due to critical errors (β=−0.289; P=0.005; r2=0.084). In this group of patients, the beliefs about inhalers’ need account for 9.6% of the observed variance in the ability to use IDs. Nevertheless, there is an interaction effect between education level and response to BMQ, because responders had a significantly high education level compared to non-responders (P=0.001). Necessity beliefs as a predictor of critical errors and as a predictor of ABL to use IDs are presented in Figures 1 and 2.
Figure 1.
Necessity beliefs as a predictor of errors.
Figure 2.
Necessity beliefs as a predictor of patients’ ability.
Abbreviation: BMQ, Beliefs about Medicines Questionnaire; Nec, Necessity Score.
Discussion
In our study, the majority of patients was treated by pulmonologists for COPD, even if they were simultaneously being cared by their family physician for other co-morbidities. Even so, inhalers’ misuse was disappointingly common. This is consistent with other published studies. In a recent study on 2,935 patients, handling errors were observed in over 50% of demonstrations.3 Different studies reported different rates of misuse, using different methods and studying different populations.17 A good inhalation technique depends on the type of ID. Critical errors were observed regardless of the inhaler used, but their proportion is different according to ID. Failure of inhalation maneuver was the main cause of ID misuse. However, evaluation of inhalation maneuver was the most difficult and subjective step to evaluate, especially when using a DPI, because we do not have measure inhalation parameters. This could favor some DPIs, mainly the Turbuhaler®, Diskus®, Ellipta® and Spiromax®, for which poor inhalation flow cannot be evidenced by lack of changing of control window’s color or by powder remaining in the device. Therefore, there is a possibly a greater rate of misuse than we actually described. In patients needing >1 ID, whenever possible, we suggest the prescription of inhalers of the same type. Although differences were found between all types of inhalers, misuse related to inhalation manoeuver when using a pMDI was the most common reason for any inhaler misuse. This can be related to ID characteristics or to insufficient teaching or training. This group of inhalers is usually considered the most difficult to use, despite requiring a minimum inspiratory flow for correct airway deposition.18 Poor coordination and failure to inhale slowly and deeply are well-known causes of pMDI misuse. Their use together with a spacer, although somewhat unpopular in practice, has been recommended in certain circumstances, and may overcome some difficulties.19 In our study, only a small number of patients used pMDIs together with a spacer, which is insufficient to draw any conclusions. The soft-mist inhaler represents a more recent category of a liquid ID that can lead to high lung depositions in patients with low inspiratory flow. In our study, they represent 15.5% of the IDs evaluated, with a rate of misuse significantly lower than pMDI and comparable to DPIs. They can be a good therapeutic option, limited by the reduced number of drugs available on a SMI. DPIs were the most popular inhalers used in our study, probably because they deliver a large range of different drugs. The sub-group of sDPI presented the better rates of correct use, and Ellipta® was the mDPI easier to use.
In our survey, a good inhaler technique was not associated with patient’s preference nor to multiple inhalers’ use, unlike in previous studies.20,21 A previous study referred the importance of patients’ confidence on the use of their inhalers to improve treatment adherence.22 In our study, in the group of patients presenting critical errors when using their inhalers, the patients that believe less in the need for medication were more prone to make a higher number of critical errors. This is a new information and needs to be interpreted with caution. This is a cross-sectional study and there is an interaction effect between education level and response to BMQ.
Some patient’s characteristics are significantly related to misuse of IDs. Being older, having lower education level or lower socio-economic status was significantly related to an incorrect inhalation technique, as in other published studies.6 Therefore, the large rate of inhalers misuse in our study is not surprising, especially after considering the overall education level and socioeconomic background of the studied population. As in previous published studies,6,23females are also more prone to inhalers misuse. However, there is an interaction effect between gender and education level in the sample. Possibly, the effect observed in gender difference (ie, higher proportion of female with critical errors) may be associated with lower education level in the women subgroup. Women also exhibit a lower socioeconomic status and are more prone to live alone, without any help from family members in the use of IDs. All of this can justify the higher proportion of IDs misuse in female gender. We suggest that educational interventions could be reinforced in such patients. In our study, patients’ clinical or functional characteristics were not related to inhalers’ misuse. Again, this is consistent with other published studies.18
Although it would be expectable, the impact of inhalers misuse on ECOPD is currently unknown, and probably difficult to be proved, given the small number of studies reporting significant association between critical errors and COPD outcomes.7 We also failed to demonstrate a significant association between inhalers’ misuse and COPD acute exacerbations. Both COPD and aging process reduces inspiratory muscle function and the ability to generate sufficient inspiratory flow to allow significantly lung deposition. This is usually the limiting factor for the proper use of an inhaler, but it was not objectively measured in the present study. We understand that it could, by some extent, explain the lack of association found between inhalers’ misuse and COPD acute exacerbations. However, the aim of this study was the patient’s ability and knowledge to use IDs, and not the patient’s capacity to generate sufficient inspiratory flow.
Our study was conducted in a ‘real word’ setting, but in a single institution. Patients were mostly treated by pulmonologists and were recruited sequentially, so we cannot exclude selection bias. This may limit the generalization of results to other populations.24 However, we have studied a significant number of patients using a wide range of IDs. Subjects were recruited without prior notification and were invited to demonstrate the use of their prescribed ID by using placebo inhalers, to facilitate the evaluation of the inhalation technique. Assessing inhalation technique by using checklists is somewhat subjective, but currently, there is no ‘best’ method. Some authors suggest the need of studies based on generally accepted checklists of maneuvers affecting drug delivery, to facilitate comparisons of results.5 Previous published studies measured inhaler technique by counting the number of correct steps, counting the number of critical errors or essential steps, or classifying the quality of the inhaler technique.6,20,25–27 Our checklists were designed with full of steps and critical errors, to minimize subjective evaluation, and inhalation technique was evaluated by a single trained pulmonologist, to avoid inter-observer variability. The definition of critical errors is of great importance, because they are likely to significantly decrease delivery of medication to the lungs, impairing health-related outcomes. Nonetheless, there is currently a wide variation and a lack of consensus on their definition.7 Therefore, our defined checklist of steps for a correct inhalation technique and the choice of critical errors, although based on previous literature, deserves discussion.
Very few original studies have been developed in Portuguese populations of COPD patients, regarding misuse of IDs,23,28 and to the best of our knowledge, this is the first study relating inhalers misuse to the patients’ beliefs about inhaled medication. A correct understanding of the relationship between inhalers and some specific patient-related characteristics can be useful in clinical practice, adding value in a resource-limited community. Nevertheless, matching the adequate medications with the adequate devices for each patient will always be a challenging issue.
Conclusions
Despite significant developments in device engineering, inhalers mishandling remains an important clinical problem. A good inhalation technique depends on the type of ID. Some inhalers are more prone to critical errors, and different inhalers are susceptible to different types of critical errors. Elderly patients, women, patients with lower education level, lower socioeconomic status or less believers in the need of inhaled medication demonstrate a worse inhalation technique. Therefore, any educational intervention should be reinforced in patients with these characteristics. This knowledge can be important in clinical practice by helping the choice of IDs, in predicting difficulties and in planning educational interventions regarding the correct use of inhalers.
Acknowledgments
The abstract of this paper was partially presented in European Respiratory Society Annual Congress 2017, Milan, as an abstract presentation with interim findings. The poster’s abstract was published in “Poster Abstracts”, Eur Respir J 2017. 50: PA671; DOI:10.1183/1393003.congress-2017.PA671.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Prof. Dr. J Correia-de-Sousa report grants from Boheringer Ingelheim, Novartis, AstraZeneca and Mundipharna, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Bosnic-Anticevich S. Inhaler device handling: have we really started to address the problem? Eur Respir J. 2017;49:1700120. doi: 10.1183/13993003.00120-2017 [DOI] [PubMed] [Google Scholar]
- 2.Melani A, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105:930–938. doi: 10.1016/j.rmed.2011.01.005 [DOI] [PubMed] [Google Scholar]
- 3.Molimard M, Raherison C, Lignot S, et al. Chronic obstructive pulmonary disease exacerbations and inhaler handling: real-life assessment of 2935 patients. Eur Respir J. 2017;49:1601794. doi: 10.1183/13993003.01794-2016 [DOI] [PubMed] [Google Scholar]
- 4.Saunders K. Misuse of inhaled bronchodilators agents. Brit Med J. 1965;1:1037–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanchis J, Gich I, Pederson S, on behalf of the Aerosol Drug Management Improvement Team (ADMIT). Systematic review of errors in inhaler use: has patient technique improved over time? Chest. 2016;150(2):394–406. doi: 10.1016/j.chest.2016.03.041 [DOI] [PubMed] [Google Scholar]
- 6.Pothirat C, Chaiwong W, Phetsuk N, Pisalthanapuna S, Chetsadaphan N, Choomuang W. Evaluating inhaler use technique in COPD patients. Int J COPD. 2015;10:291–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Usmani O, Lavorini F, Marshall J, Dunlop C, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res. 2018;19:10. doi: 10.1186/s12931-017-0710-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Capstick T, Clifton I. Inhaler technique and training in people with chronic obstructive pulmonary disease and asthma. Expert Rev Respir Med. 2012;6(1):91–103. doi: 10.1586/ers.11.89 [DOI] [PubMed] [Google Scholar]
- 9.Lavorini F. Inhaled drug delivery in the hands of the patient. J Aerosol Med Pulm Drug Deliv. 2014;27(6):414–418. doi: 10.1089/jamp.2014.1132 [DOI] [PubMed] [Google Scholar]
- 10.von Elm E, Altman D, Egger M, Pocock S, Gotzche P, Vandenbroucke J. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelinis for reporting observational studies. Int J Surg. 2014;12:1495–1499. doi: 10.1016/j.ijsu.2014.07.013 [DOI] [PubMed] [Google Scholar]
- 11.Graffar M. Une méthode de classification sociale d’échantilons de population (a method of social classification of population samples). Courrier VI. 1956;6:445–459 [in French]. [Google Scholar]
- 12.Salgado T, Marques A, Geraldes L, Benrimoj S, Horne R, Fernandez-Llimos F. Cross-cultural adaptation of the beliefs about medicines questionnaire into portuguese. São Paulo Med J. 2013;131(2):88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Global Initiative for Chronic Obstructive Lung Disease (GOLD), updated; 2017. Available from: http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/. Accessed July 1, 2018.
- 14.Miller M, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Series “ATS/ERS task force: standardisation of function testing”. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805 [DOI] [PubMed] [Google Scholar]
- 15.Quanjer P, Stanojevic S, Cole T, et al. Multi-ethnic reference values for spirometry for the 3-95-year age range: the global lung function 2012 equations: report of the Global Lung Function Initiative (GLI), ERS task force to establish improved lung function reference values. Eur Respir J. 2012;40(6):1324–1343. doi: 10.1183/09031936.00080312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanchis J, Corrigan C, Levy M, Viejo J. Inhaler devices – from theory to practice. Respir Med. 2013;107:495–502. doi: 10.1016/j.rmed.2012.12.007 [DOI] [PubMed] [Google Scholar]
- 17.Crompton G, Barnes P, Broeders M, et al. The need to improve inhalation technique in Europe: a report from the aerosol drug management improvement team. Respir Med. 2006;100:1479–1494. doi: 10.1016/j.rmed.2006.01.008 [DOI] [PubMed] [Google Scholar]
- 18.Jarvis S, Ind P, Shiner R. Inhaled therapy in elderly COPD patients; time for re-evaluation? Age Aging. 2007;36:213–218. doi: 10.1093/ageing/afl174 [DOI] [PubMed] [Google Scholar]
- 19.Broeders M, Sanchis J, Levy M, Crompton G, Dekhuijzen P, on behalf of the ADMIT working group. The ADMIT series – issues in inhalation therapy. 2) improving technique and clinical effectiveness. Primary Care Respir J. 2009;18(2):76–82. doi: 10.4104/pcrj.2009.00025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Palen J, Klein J, Herwaarden C, Zielhuis G, Seydel E. Multiple inhalers confuse asthma patients. Eur Respir J. 1999;14:1034–1037. [DOI] [PubMed] [Google Scholar]
- 21.Rootmensen G, Keimpema A, Jansen H, Haan R. Predictors of incorrect inhalation technique in patients with astma and COPD: a study using a validated videotaped scoring method. J Aerosol Med Pulm Drug Deliv. 2010;23(5):1–6. doi: 10.1089/jamp.2009.0785 [DOI] [PubMed] [Google Scholar]
- 22.Price D, Keininger D, Viswanad B, Gasser M, Walda S, Gutzwiller F. Factors associated with appropriate inhaler use in patients with COPD – lessons from the REAL survey. Int J COPD. 2018;13:695–702. doi: 10.2147/COPD.S149404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chorão P, Pereira A, Fonseca J. Inhaler devices in asthma and COPD – an assessment of inhaler technique and patients’ preferences. Respir Med. 2014;108:968–975. doi: 10.1016/j.rmed.2014.04.019 [DOI] [PubMed] [Google Scholar]
- 24.Hackshaw A. Small studies: strengths and limitations. Eur Respir J. 2008;32:1141–1143. doi: 10.1183/09031936.00136408 [DOI] [PubMed] [Google Scholar]
- 25.Souza M, Meneghini A, Ferraz É, Vianna E, Borges M. Knowledge of and technique for using inhalation devices among asthma and COPD patients. J Bras Pneumol. 2009;35(9):824–831. [DOI] [PubMed] [Google Scholar]
- 26.Ovchinikova L, Smith L, Bosnic-Anticevich S. Inhaler technique maintenance: gaining an understanding from the patients’s perspective. J Asthma. 2011;48:616–624. doi: 10.3109/02770903.2011.580032 [DOI] [PubMed] [Google Scholar]
- 27.Lenney J, Innes J, Crompton G. Inappropriate inhaler use: assessment of use and patient preference of seven inhalation devices. Respir Med. 2000;94:496–500. [DOI] [PubMed] [Google Scholar]
- 28.Maricoto T, Rodrigues L, Teixeira G, Valente C, Andrade L, Saraiva A. Assessment of inhalation technique in clinical and functional control of asthma and chronic obstructive pulmonary disease. Acta Med Port. 2015;28(6):702–707. [DOI] [PubMed] [Google Scholar]